Abstract
Background
An association between heart rate variability (HRV) and cardiac events in certain diseases has been demonstrated. However, the association with new-onset atrial fibrillation (AF) after coronary artery bypass grafting (CABG) is still controversial. This study aimed to investigate the association between HRV and new-onset AF in patients undergoing CABG during a 6-month follow-up.
Methods
This prospective study included 119 consecutive patients who underwent off-pump CABG. All patients were assessed using 24-hour Holter recordings 2 days before CABG and 1 week, 3 months, and 6 months postoperatively. HRV was analyzed, and AF was detected from its recordings.
Main results
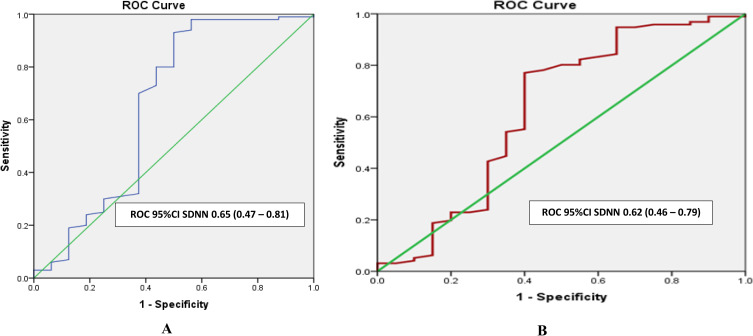
In patients undergoing CABG, NYHA III increased the AF rate 7 days postoperatively, and advanced age and diabetes were associated with AF 6 months postoperatively. A reduction in time-domain measurements before surgery was significantly associated with a higher risk of developing AF seven days postoperatively; no association between preoperative HRV and AF was found at six months. Reduced preoperative HRV (SDNN (standard deviation of all normal-to-normal intervals [) < 50 ms) was an independent predictor of AF at 3 (AUC = 0.65) and 6 months (AUC = 0.62) following surgery.
Conclusion
A reduction in the time domain measurements before CABG was associated with a higher risk of new-onset AF at 7 days postoperatively but not at 6 months. An SDNN <50 ms was a weak independent predictor of a higher incidence of AF at 3 and 6 months post-surgery.
Keywords: heart rate variability, coronary artery bypass graft, atrial fibrillation, standard deviation of all normal-to-normal intervals
Introduction
Stenting is the mainstay therapy for coronary artery disease. But when this therapy is not feasible, coronary artery bypass grafting (CABG) is the main choice. However, several cardiac events, including cardiac arrhythmias, are still recorded after surgery.1 CABG is associated with increased autonomic instability of the heart, and the autonomic nervous system may play an important role as a trigger and risk marker for developing atrial fibrillation (AF) after surgery.2 The occurrence of postoperative AF has been associated with hospitalization,3 longer length of stay, short-term mortality (one-year mortality),4 and long-term mortality (four-year mortality).5 Cerebral stroke occurs in approximately 10% of postoperative AF patients.4 Early identification of patients who are likely to develop postoperative AF may allow targeted prophylaxis. Heart rate variability (HRV) analysis is widely used to assess the cardiovascular autonomic activity.6
There are several predictors of AF following CABG surgery. Several parameters have been suggested to predict the incidence of atrial fibrillation.7 HRV parameters are very important tools for a healthy lifestyle and are a good indicator of a healthy cardiovascular system.8
The relationship between HRV and AF after coronary artery bypass surgery has been investigated with divergent results.9–11 Some authors have found an association between new-onset AF and both preoperative12,13 and postoperative HRV. Other studies have found no association between AF and HRV.14 Therefore, there are no specific recommendations regarding the clinical use or implications of HRV in patients undergoing CABG. In most previous studies, new-onset AF and HRV were evaluated only during hospitalization, which was significantly affected by the factors of acute surgery, and may explain the controversy regarding the association between AF and HRV. This study aimed to determine the association between (preoperative and postoperative) HRV and the occurrence of AF after off-pump CABG 7 days, 3 months, and 6 months postoperatively. To the best of our knowledge, this is the first study to assess this association 3 times after CABG during a 6-month follow-up period.
Patients and Methods
Between June 2016 and August 2018, we selected consecutive patients who underwent isolated off-pump CABG with cardiopulmonary bypass at Hanoi Heart Hospital, one of Vietnam’s largest heart operation centers. This prospective descriptive study was approved by the ethics committee of our hospital. Patients were advised of the study protocol and written informed consent was obtained from all patients. All the patients had previously been granted permission to use their medical records for research purposes.
The inclusion criteria were stable coronary artery disease patients indicated for CABG, according to the ESC of Cardiology guidelines 2013, with a stable sinus rhythm.
The exclusion criteria were patients had AF history of AF before CABG, acute coronary syndrome, acute heart failure, or other acute diseases; medical conditions where HRV could not be evaluated, such as preoperative atrial fibrillation, frequent ventricular ectopic activity, sinus node syndrome, or second- or third-degree atrioventricular block; cardiac pacing; concomitant cardiac surgery–implanted artificial valves; severe postoperative complications, such as infection or bleeding requiring reoperation; patients needing inotropes after 3 days postoperatively; and significant artifacts or duration of Holter ECG recordings of less than 18 hours. Patients requiring vasopressor agents over the first 3 days were excluded from this study.
Holter recordings were made using 3-channel SEER LIGHTS Digital Holter recorders for healthcare purposes. An MSC 8800 Holter monitoring system with Medical System International (MSI) software version 5.02 was used. Twenty-four-hour Holter recordings were performed four times. The first recording was made two days before CABG, and three other recordings were made at one week, three months, and six months postoperatively. HRV was analyzed using the Holter monitoring system and was then manually overread. The Holter ECG was reviewed by a single cardiologist, all artifacts were cleaned, and the beats were modified as needed. AF was defined as at least 6 minutes duration of an irregular pattern of QRS waves from the recordings. The corrected data were processed and HRV was computed in recordings with less than 4 h of AF. Most HRV variables were calculated as recommended by the Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology.15
For time-domain analysis, ASDNN (the mean of the standard deviations of all normal-to-normal intervals for 5 minutes of recording), SDNN (standard deviation of all normal-to-normal intervals), SDANN (the mean of the standard deviations of all normal-to-normal intervals for 5 minutes of recording), rMSSD (root mean square of successive RR interval differences), and pNN50 (number of times that successive RR intervals differed by 50% from the index RR interval) were calculated. Frequency domain analysis covered VLF (magnitude of the HRV in the VLF range, 0.0033 to 0.04 Hz), LF (magnitude of the HRV in the LF range, 0.04 to 0.15 Hz), and HF (magnitude of the HRV in the HR range, 0.15 to 0.04 Hz), with LF/HF: low to high-frequency ratio apart from the 24-hour Holter ECG.
Perioperative Management
None of the patients had undergone preoperative amiodarone treatment. Most patients were extubated on the day of surgery and oral medication was initiated on postoperative day 1. Patients requiring vasopressor agents over the first 3 days were excluded from this study. We are carefully following up with the patients who are prescribed drugs that affect HRV (such as calcium channel blockers, beta-blockers, and antiarrhythmic drugs). If drugs affecting HRV were prescribed preoperative and postoperative in patients, these patients will selected in this study. If drugs affecting HRV were prescribed preoperative only, we excluded them from this study to prevent bias. Blood tests were performed daily for seven days postoperatively to ensure that all electrolyte disorders were corrected. The blood potassium levels were adjusted using oral potassium to obtain a target blood potassium level of 4.0 to 5.0 mEq/L.
Statistical Analysis
The results are expressed as the mean ± standard deviation. Pearson’s 2 test was used to analyze the differences between certain observed proportions and categorical data, and Fisher’s exact test was used if the variable was < 5. For continuous variables, the normality of the distribution of the variables was checked using the Kolmogorov–Smirnov test. Unpaired t-tests for normally distributed variables; Mann–Whitney U-test for skewed variables. Variables that were statistically significant in univariate comparisons were entered into the multivariate Cox model. In the Cox Proportional Hazard Model, RR and 95% confidence intervals (CI) for the association between reduced HRV and postoperative new-onset AF were examined. The significance of reduced HRV measurement in explaining postoperative AF was evaluated by ROC (receiver operating characteristic (ROC) curves with determination of the areas under the curves. A statistic of 0.5 represents poor predictive ability; a value of 0.60 indicates good predictive ability; a value of 0,8–0,9 shows very good prediction and perfect ability; a value of 1.0. All analyses were performed using the SPSS statistical package, version 11.0.
Results
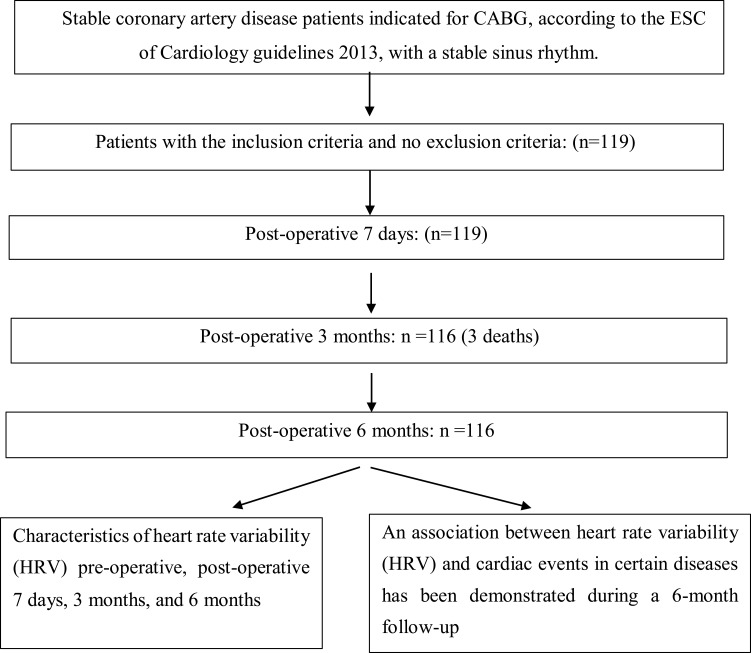
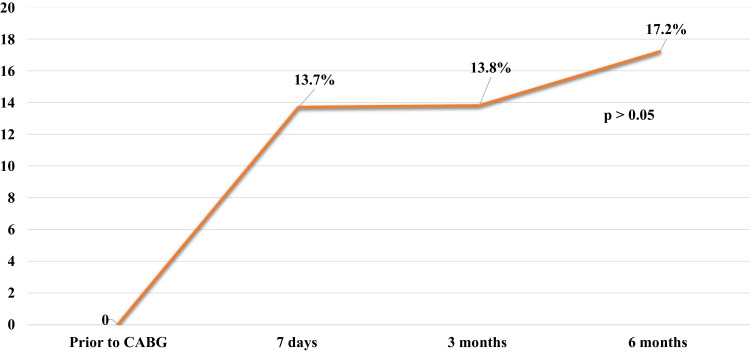
In total, 119 patients were recruited for this study. Seven days after surgery, with 2 cases of death, the number of patients was 117. After 2 months, one death occurred; the number of patients was 116 at 3 and 6 months postoperatively (Figure 1: Flowchart of study). The total number of patients with completed follow-up was 116 (Table 1). The AF rates during the follow-up period were 13.7%, 13.8%, and 17.2%, respectively (Figure 2).
Figure 1.
Flowchart of study.
Table 1.
Univariate Variables Comparisons Between Patients with and without Postoperative AF During Follow-Up
| Timing Variables |
Postoperative AF at 7 Days | p-value | Postoperative AF at 3 Months | p-value | Postoperative AF at 6 Months | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n=16) | No (n=101) | Yes (n=16) | No (n=100) | Yes (n=20) | No (n=96) | |||||
| Age | 65.94 ± 10.45 | 64.62 ± 6.77 | > 0.05 | 67.50 ± 8.53 | 64.27 ± 7.04 | > 0.05 | 68.35 ± 7.10 | 63.96 ± 7.15 | <0.05* | |
| BMI | 23.41 ± 3.23 | 22.94 ± 2.83 | >0.05 | 23.63 ± 3.21 | 22.90 ± 2.84 | > 0.05 | 23.49 ± 2.68 | 22.90 ± 2.93 | >0.05 | |
| eGFR | 67.88 ± 22.40 | 63.30 ± 18.82 | > 0.05 | 64.19 ± 28.40 | 64.34 ± 17.11 | > 0.05 | 57.85 ± 16.53 | 65.67 ± 19.16 | >0.05 | |
| Sex | Male | 13 (13.4) | 84 (86.6) | >0.05 | 13 (13.4) | 84 (86.6) | > 0.05 | 18 (18.6) | 79 (81.4) | > 0.05 |
| Female | 3 (15.0) | 17 (85.0) | 3 (15.8) | 16 (84.2) | 2 (10.5) | 17 (89.5) | ||||
| Diabetes | Yes | 3 (7.7) | 36 (92.3) | >0.05 | 4 (10.5) | 34 (89.5) | > 0.05 | 2 (5.3) | 36 (94.7) | <0.05* |
| No | 13 (16.7) | 65 (83.3) | 12 (15.4) | 66 (84.6) | 18 (23.1) | 60 (76.9) | ||||
| Smoking | Yes | 8 (14.8) | 46 (85.2) | >0.05 | 7 (13.0) | 47 (87) | > 0.05 | 7 (13.0) | 47 (87.0) | > 0.05 |
| No | 8 (12.7) | 55 (87.3) | 9 (14.5) | 53 (85.5) | 13 (21.0) | 49 (79.0) | ||||
| Hypertension | Yes | 14 (14) | 87 (86.1) | > 0.05 | 14 (14.0) | 86 (86) | >0.05 | 19 (19.0) | 81 (81.0) | >0.05 |
| No | 2 (12.5) | 14 (87.5) | 2 (12.5) | 14 (87.5) | 1 (6.2) | 15 (93.8) | ||||
| PAD | Yes | 3 (21.4) | 11 (78.6) | > 0.05 | 2 (14.3) | 12 (85.7) | >0.05 | 3 (21.4) | 11 (78.6) | >0.05 |
| No | 13 (12.6) | 90 (87.4) | 14 (13.7) | 88 (86.3) | 17 (16.7) | 85 (83.3) | ||||
| Previous MI | Yes | 0 (0.0) | 10 (100) | >0.05 | 1 (10.0) | 9 (90) | > 0.05 | 2 (20.0) | 8 (80.0) | > 0.05 |
| No | 16 (15.0) | 91 (85.0) | 15 (14.2) | 91 (85.8) | 18 (17.0) | 88 (83.0) | ||||
| NYHA (≥ 3) | Yes | 3 (42.9) | 4 (57.1) | <0.05* | 3 (42.9) | 4 (57.1) | >0.05 | 1 (14.3) | 6 (85.7) | >0.05 |
| No | 12 (11.0) | 97 (89.0) | 13 (11.9) | 96 (88.1) | 19 (17.4) | 90 (82.6) | ||||
| Chronic kidney failure ≥stage 4 | Yes | 6 (10.7) | 50 (89.3) | > 0.05 | 9 (16.4) | 46 (83.6) | >0.05 | 12 (21.8) | 43 (78.2) | > 0.05 |
| No | 10 (16.4) | 51 (83.6) | 7 (11.5) | 54 (88.5) | 8 (13.1) | 53 (86.9) | ||||
| Euro score ≥ 3% | Yes | 2 (28.6) | 5(71.4) | >0.05 | 4 (57.1) | 3 (42.9) | >0.05 | 3 (42.9) | 4 (57.1) | >0.05 |
| No | 14 (12.7) | 96 (87.3) | 12 (11.0) | 97 (89.0) | 17 (15.6) | 92 (84.4) | ||||
| Preoperative EF | 66.75 ± 8.31 | 63.38 ± 12.05 | >0.05 | 65.56 ± 10.56 | 63.6 ± 11.88 | > 0.05 | 65.2 ± 9.53 | 63.59 ± 12.11 | >0.05 | |
| CPB duration (min) | 93.15 ± 29.55 | 94.05 ± 26.25 | >0.05 | 95.25 ± 29.05 | 94.0 ± 26.15 | >0.05 | 94.25 ± 27.35 | 94.05 ± 26.5 | >0.05 | |
| Aortic clamp time (min) | 72.05 ± 24.50 | 74.05 ± 23.45 | > 0.05 | 73.05 ± 25.50 | 74.05 ± 23.95 | >0.05 | 73.05 ± 24.10 | 74.05 ± 23.15 | >0.05 | |
Notes: *(The bold values): Statistically significant difference. Entries are means±SD or numbers of patients. P -values are nominal.
Abbreviations: AF, atrial fibrillation; BMI, body mass index; GFR, Glomerular Filtration Rate; PAD, Peripheral artery disease; MI, Myocardial infarction; CPB, Cardiopulmonary bypass.
Figure 2.
New onset AF rate during the follow-up.
The clinical and operative characteristics of the patients with and without postoperative AF are presented in Table 1. Univariate analysis showed that heart failure NYHA class ≥3 was associated with a higher incidence of AF 7 days postoperatively. No variable was found to be associated with AF occurrence 3 months post-surgery. The AF rate increased with advanced age and decreased in the presence of diabetes six months postoperatively. Because the results of the univariate analysis showed that only 1–2 variables were associated with AF, multivariate analysis was not used.
As shown in Table 2, most preoperative HRV time-domain measurements (rMSSD, pNN50, and SDNN) were associated with new-onset AF 7 days postoperatively. Three months after surgery, only the preoperative SDANN was lower in the AF group. At six months, no difference in preoperative HRV was observed between the AF and non-AF groups.
Table 2.
Results of Preoperative HRV Analysis in Patients with and without Postoperative AF During the Follow-Up
|
Timing Preoperative HRV |
Postoperative AF at 7 Days | p-value | Postoperative AF at 3 Months | p-value | Postoperative AF at 6 Months | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| Yes (n=16) | No (n=101) | Yes (n=16) | No (n=100) | Yes (n=20) | No (n=96) | ||||
| ASDNN (ms) | 38.44 ± 25.24 | 46.27 ± 18.97 | >0.05 | 40.44 ± 30.12 | 46.27 ± 17.79 | >0.05 | 41.75 ± 25.80 | 46.24 ± 18.47 | >0.05 |
| Rmssd (ms2) | 19.63 ± 8.14 | 28.02 ± 12.30 | <0.05* | 24.25 ± 12.35 | 27.47 ± 12.04 | >0.05 | 23.30 ± 11.43 | 27.80 ± 12.13 | >0.05 |
| pNN 50 (%) | 3.23 ± 3.30 | 7.48 ± 7.57 | <0.05* | 5.88 ± 6.55 | 7.13 ± 7.40 | >0.05 | 4.58 ± 5.44 | 7. ± 7.53 | >0.05 |
| SDNN (ms) | 85.94 ± 40.95 | 104.50 ± 32.06 | <0.05* | 85.13 ± 45.23 | 105.23 ± 30.66 | >0.05 | 91.50 ± 42.81 | 104.74 ± 31.05 | >0.05 |
| SDANN (ms) | 74.00 ± 34.02 | 90.69 ± 31.02 | >0.05 | 73.31 ± 36.57 | 91.29 ± 30.28 | <0.05* | 81.25 ± 39.12 | 90.38 ± 29.88 | >0.05 |
| VLF (ms2) | 23.37 ± 19.32 | 25.74 ± 10.76 | >0.05 | 23.26 ± 21.63 | 25.93 ± 9.96 | >0.05 | 23.92 ± 18.23 | 25.90 ± 10.55 | >0.05 |
| LF (ms2) | 15.43 ± 19.53 | 16.55 ± 10.94 | >0.05 | 15.19 ± 19.77 | 16.73 ± 10.83 | >0.05 | 16.24 ± 17.48 | 16.58 ± 11.10 | >0.05 |
| HF (ms2) | 9.42 ± 8.74 | 11.75 ± 6.95 | >0.05 | 10.62 ± 9.15 | 11.65 ± 6.89 | >0.05 | 10.49 ± 8.40 | 11.72 ± 6.96 | >0.05 |
| LF/HF | 1.45 ± 0.55 | 1.44 ± 0.37 | >0.05 | 1.30 ± 0.51 | 1.47 ± 0.37 | >0.05 | 1.48 ± 0.53 | 1.44 ± 0.36 | >0.05 |
Notes: *(The bold values): Statistically significant difference. Entries are means±SD. P -values are nominal. Student’s unequal variance unpaired t-tests were used.
The cut-off for each measurement of the reduced HRV time domain was defined as recommended.15 However, in general cardiology, reduced HRV is determined when the SDNN is ≤93 ms.16 In this study, the two cutoffs used for SDNN with reduced HRV were 50 ms and 93 ms, respectively (Tables 3 and 4). Seven days after surgery, the most reduced pre-operative HRV in the time domain was related to new-onset AF. Three months post-surgery, ASDNN <30 ms, rMSSD <15 ms, and SDNN <50 ms were related to increased AF. Six months post-surgery, ASDNN <30 ms and SDNN <50 ms increased the incidence of AF. In multivariate analysis, SDNN <50 ms was the only independent predictor of postoperative AF at 3 and 6 months post-surgery (Table 5).
Table 3.
Results of Reduced Pre-Operative HRV Analysis in Patients with and without Postoperative AF During the Follow-Up
| Time Reduced Pre-Operative HRV |
Postoperative AF at 7 Days | p-value (CI 95%) | Postoperative AF at 3 Months | p-value (CI 95%) | Postoperative AF at 6 Months | p-value (CI 95%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| AF (+) (n =16) | AF (-) (n= 101) | AF (+) (n=16) | AF (-) (n=100) | AF (+) (n= 20) | AF (-)(n=96) | |||||
| ASDNN (n.%) | < 30 ms | 5 (22.70) | 17 (77.30) | > 0.05 (0.69–7.29) | 8 (38.10) | 13 (61.90) | <0.05* (2.14–20.92) | 7 (33.30) | 14 (66.70) | < 0.05* (1.0–9.28) |
| ≥ 30 ms | 11 (11.60) | 84 (88.40) | 8 (8.40) | 87 (91.60) | 13 (13.70) | 82 (86.30) | ||||
| rMSSD (n.%) | < 15 ms | 7 (41.20) | 10 (58.80) | <0.05* (2.16–23.12) | 5 (31.20) | 11 (68.80) | <0.05* (1.07–12.56) | 4 (25.00) | 12 (75.00) | >0.05 (0.50–6.11) |
| ≥ 15 ms | 9 (9.00) | 91 (91.00) | 11 (11.00) | 89 (89.00) | 16 (16.00) | 84 (84.00) | ||||
| pNN 50 (n.%) | < 0.75% | 7 (28.00) | 18 (72.00) | <0.05* (1.18–10.89) | 5 (20.80) | 19 (79.20) | > 0.05(0.60–6.23) | 6 (25.00) | 18 (75.00) | >0.05 (0.62–5.49) |
| ≥ 0.75% | 9 (9.80) | 83 (90.2) | 11 (12.00) | 81 (88.00) | 14 (15.20) | 78 (84.80) | ||||
| SDNN (n.%) | < 50 ms | 4 (44.40) | 5 (55.60) | <0.05* (1.50–27.15) | 6 (75.00) | 2 (25.00) | < 0.01* (5.22–16.4) | 4 (50.00) | 4 (50.00) | < 0.05* (1.30–25.36) |
| ≥ 50 ms | 12 (11.1) | 96 (88.9) | 10 (9.30) | 98 (90.70) | 16 (14.80) | 92 (85.20) | ||||
| SDNN (n.%) | ≥ 93 ms | 11 (20.8) | 42 (79.2) | <0.05* (1.0–9.56) | 10 (19.2) | 42 (80.8) | >0.05 (0.77–6.82) | 12 (23.1) | 40 (76.9) | >0.05 (0.78–5.60) |
| < 93 ms | 5 (7.8) | 59 (92.2) | 6 (9.4) | 58 (90.6) | 8 (12.5) | 56 (87.5) | ||||
| SDANN (n.%) | < 40 ms | 3 (60.00) | 2 (40.00) | <0.05* (1.74–74.88) | 2 (40.00) | 3 (60.00) | >0.05 (0.70–30.11) | 2 (40.00) | 3 (60.00) | >0.05 (0.53–2210) |
| ≥ 40 ms | 13 (11.60) | 99 (88.40) | 14 (12.60) | 97 (87.40) | 18 (16.20) | 93 (83.80) | ||||
Notes: *(The bold values): Statistically significant difference. Entries are numbers of patients. P -values are nominal. The cut-off for each index of reduced HRV time domain as recommended.
Abbreviation: CI, the confidence of interval.
Table 4.
Hazard Ratios for Association Between Variables and Postoperative Atrial Fibrillation
| Timing Reduced HRV | RR | p-value (CI 95%) | RR | p-value (CI 95%) | RR | p-value (CI 95%) |
|---|---|---|---|---|---|---|
| At 7 Days | At 3 Months | At 6 Months | ||||
| SDNN ≤ 50 ms | 3.502 | >0.05 (0.708–17.322) | 30.882 | < 0.001 * (4.503–211.777) | 5.404 | <0.05 * (1.078–27.087) |
| rMSSD ≤ 15 ms | 3.444 | >0.05 (0.987–12.015) | 0.906 | > 0.05 (0.170–4.835) | 1.138 | > 0.05 (0.304–4.259) |
Notes: *(The bold values): Statistically significant difference. Multivariate was used to find the predictor of postoperative AF.
Abbreviation: CI, confidence of interval.
Table 5.
Results of HRV Analysis at 7 Days’ Post-Surgery in Patients with and without Postoperative AF During the Follow-Up
|
Timing HRV at 7 Days Postoperatively |
AF at 3 Months | p | AF at 6 Months | p | ||
|---|---|---|---|---|---|---|
| Yes (n=12) | No (n=97) | Yes (n=16) | No (n=93) | |||
| ASDNN (ms) | 29.75 ± 19.32 | 35.34 ± 21.49 | > 0.05 | 35.56 ± 23.48 | 34.58 ± 20.97 | > 0.05 |
| rMSSD (ms2) | 19.92 ± 7.93 | 22.40 ± 13.37 | > 0.05 | 24.56 ± 15.92 | 21.71 ± 12.34 | > 0.05 |
| pNN 50 (%) | 3.08 ± 3.49 | 5.16 ± 9.25 | > 0.05 | 7.07 ± 10.06 | 4.56 ± 8.60 | > 0.05 |
| SDNN (ms) | 66.17 ± 38.97 | 78.48 ± 34.27 | > 0.05 | 80.75 ± 39.22 | 76.51 ± 34.22 | > 0.05 |
| SDANN (ms) | 58.08 ± 35.49 | 65.42 ± 28.63 | >0.05 | 68.81 ± 33.84 | 63.89 ± 28.67 | >0.05 |
| VLF (ms2) | 15.66 ± 12.17 | 18.81 ± 11.80 | > 0.05 | 17.69 ± 13.29 | 18.60 ± 11.63 | > 0.05 |
| LF (ms2) | 10.45 ± 9.11 | 13.37 ± 12.25 | >0.05 | 11.82 ± 10.84 | 13.26 ± 12.17 | >0.05 |
| HF (ms2) | 7.06 ± 3.69 | 8.98 ± 6.43 | > 0.05 | 9.14 ± 8.24 | 8.71 ± 5.84 | > 0.05 |
| LF/HF | 1.40 ± 0.86 | 1.50 ± 0.60 | >0.05 | 1.41 ± 0.74 | 1.50 ± 0.61 | >0.05 |
Notes: Entries are means ± SD. P -values are nominal. Student’s unequal variance unpaired t-tests was used.
HRV frequency and time-domain measurements at 7 days after surgery were not related to AF occurrence at 3 and 6 months after surgery. HRV at 3 months postoperatively was also not related to AF rate at 6 months (Table 5).
In multi-analysis, only SDNN <50 ms was shown to increase AF at 3 and 6 months post-surgery, with an AUC of 0.65 and 0.62, (Figure 3)
Figure 3.
ROC curves for predicting atrial fibrillation at 3 months (A) and 6 months (B) postoperatively. ROC: Receiver operator characteristic. The significance of reduced HRV measurement in explaining postoperative AF was evaluated by ROC (receiver operating characteristic (ROC) curves with determination of the areas under the curves. A statistic of 0.5 represents poor predictive ability; a values of 0.60 indicate good predictive ability; a value of 0.8–0,9 shows and very good prediction and perfect ability; a value of 1.0.
Abbreviations: AUC, area under curve; CI, confidence interval.
Discussion
The main findings of this study focused on the HRV before and post-surgery AF. These results provide new insights into Vietnam’s population. In most previous studies, new-onset AF was assessed from the time of cardiac surgery to hospital discharge or until postoperative day 103,13 and was detected by continuous ECG telemetry monitoring. The new-onset AF rate after CABG has been variable, ranging from 16.1% to 47.7%.17–19 The incidence of paroxysmal AF has increased from the day of surgery to a peak on postoperative day 2 and has declined steadily thereafter.3,13 Atrium injury caused by cutting and cautery, cardioplegia, atrial stretch, postoperative metabolic changes, and inflammation are all contributing factors to early postoperative AF, usually manifesting on the 2nd or 3rd postoperative day.3 The divergence in the new-onset AF rate can be explained by the postoperative timing, duration of AF recording, CABG protocol, and pre-existing features.3 In contrast to previous studies, in which the rate of new-onset AF was recorded only during cardiac rehabilitation, the AF rate in this study was evaluated using 24-hour Holter monitoring at 7 days, 3 months, and 6 months after surgery. No significant difference was observed in the AF rate recorded 3 times postoperatively. The AF rate was probably steadier after 7 days post-surgery when some main acute factors were resolved.
Agreement regarding the variables associated with new-onset AF after CABG has not yet been reached. In the multivariate model, the statistically significant variables were age, diabetes mellitus, supraventricular non-sustained tachycardia, preoperative statin use, and operative duration.13 Akintoye et al identified only two independent factors (increased age and BMI) as predictors of postoperative AF using multivariate analysis.3 Different variables associated with AF may be explained by the effects of acute surgery due to the mechanism.20 Therefore, it may be more consistent to assess the association between variables and AF at least 7 days postoperatively when the patient is much less affected by surgery. Table 1 shows that at 7 days postoperatively, only heart failure with an NYHA class ≥3 was associated with a higher incidence of AF. Six months after surgery, in agreement with previous studies, advanced age and diabetes were associated with AF. Structural changes in the heart increase with age, including loss of nodal fibers, ventricular fibrosis, and decreased ventricular compliance, which establish an anatomic substrate susceptible to the development of AF.21,22 In agreement with the results of this study, other studies have demonstrated a lower incidence of postoperative AF in patients undergoing CABG.23,24 There should be a scoring system in order to precisely detect patients with potential AF.25 Artificial intelligence systems are being used in routine clinical practice which can easily detect AF patients.26
The major finding of our study was that a reduction in the time-domain measurements of 24-hour HRV was associated with a higher risk of postoperative AF 7 days after surgery, but no association was found at 6 months. Some investigators have reported controversy on the relationship between preoperative HRV and AF after CABG.9–11 Frost et al studied preoperative 24-hour Holter monitoring in 102 patients with non-diabetic CABG. They concluded that an isolated reduction in basic vagal modulation (calculated as the percentage of successive normal-to-normal interval differences greater than 6%, positively correlated with rMSSD) was significantly associated with a higher risk of postoperative AF.11 However, Kinoshita et al found that reduced time-domain factors in preoperative 24-hour HRV were independently associated with a lower risk of AF after off-pump CABG.13 This may be because patients with diabetes, who are likely to have a lower AF rate, were excluded by Frost et al but accounted for 55% of Kinoshita’s sample.13 In contrast, Chamchad et al concluded that preoperative 24-hour HRV (SDNN and RMSSD) did not significantly predict postoperative AF in CABG patients.9 It may be due to measurements of vagal activity, such as rMSSD and SDANN, being of particular interest for brief intervals of 5 minutes or less. Separating the values based on day and night would be an effective and simple method for assessing the vagotonia level in patients. To measure the autonomic nervous system’s baseline state more precisely, deceleration capacity is preferred.25,26 Controversy has also existed on the association between frequency domain and AF; Ksela et al identified frequency measures as predictive of postoperative AF in patients undergoing CABG.27 Other authors have stated that in patients undergoing CABG, the LF/HF ratio predicts postoperative AF,28,29 whereas Hakala et al showed that none of the preoperative spectral analysis measures differed significantly between the AF and non-AF groups10 and that diabetic autonomic neuropathy may affect HRV dynamics.30 Hakala’s study included 17 patients with diabetes; however, excluding these patients from the analysis did not significantly affect the results.10
Hogue et al performed HRV analysis before AF onset in patients after CABG. They observed either lower or higher measures of HRV before AF and hypothesized that either a higher vagal tone or dysfunctional autonomic heart rate control is present before AF onset.31 They hypothesized that changes in autonomic tone occurred within minutes to an hour before AF onset; these changes cannot be recognized when analyzing HRV a day before surgery.10
In most studies, only the difference in mean HRV between groups with and without AF was assessed, and the correlation between reduced HRV and new-onset AF was not evaluated, which may have led to inconsistent results. Kinoshita used the median as a cutoff point to define preoperative reduced HRV; SDNN <99 ms or rMSSD <20 ms was independently associated with a lower risk of AF.13
According to the recommendations, SDNN >100 ms was considered normal HRV, and SDNN <50 ms reduced HRV.16 Milicevic et al conducted a study of more than 2500 patients and concluded that in the “general cardiologic population”, SDNN >93 ms indicated borderline normal HRV, whereas SDNN values of 59–92 ms indicated mildly to moderately decreased HRV.16 Lakusic et al32 used this cut-off point to define reduced HRV (SDNN <93 ms); 36% of patients with SDNN <93 ms following CABG were found to have higher mortality, but no data on AF were reported. In the present study, reduced HRV was defined as recommended with SDNN <50 ms or rMSSD <15 ms considered reduced HRV.16 Another cutoff for SDNN (<93 ms) was used, as stated by Milicevic. Table 3, with Univariate analysis, showed that most indices of reduced preoperative HRV (sMSSD and SDNN) increased the AF rate 7 days and 3 months post-surgery. In multi-analysis, only SDNN <50 ms was shown to increase AF at 3 and 6 months post-surgery, with an AUC of 0.65 and 0.62. No previous study has shown an association between preoperative reduced HRV and postoperative AF in patients undergoing CABG during a 6-month follow-up period.
According to some reports, unlike decreased HRV in patients after myocardial infarction, decreased postoperative HRV does not increase mortality in CABG patients.14,33 However, several investigators have reported an association between HRV and AF following CABG. Dimmer et al analyzed HRV in 4 sequential 15-minute intervals preceding the onset of AF in 64 patients undergoing elective CABG and showed that patients with AF had higher postoperative SDNN than those without postoperative AF in the first 45 min.34 Bettoni and Zimmermann also concluded that paroxysmal AF is preceded by increased adrenergic drive, followed by vagal predominance (time-domain and spectral analyses).35 No previous studies have reported an association between postoperative HRV and subsequent AF development during follow-up. In addition to comorbidities, HRV fluctuations after CABG might be related to the combined effects of surgical manipulation of the heart, prolonged anesthesia, cardioplegia, and extracorporeal circulation.36 In this study, postoperative HRV was evaluated at 7 days and 3 months to overcome the acute effects of surgery on AF; however, no association was found with AF development.
Limitations
The major findings of this study were weak, modest, and significant. A larger sample size was required to perform logistic regression or Cox regression modeling.
Conclusion
A reduction in the time domain measurements before CABG increased the risk of AF seven days postoperatively. An SDNN <50 ms was a weak independent predictor of a higher incidence of AF at 3 and 6 months post-surgery.
Acknowledgments
We thank our staff for collecting the samples and supporting the study.
Funding Statement
There is no funding to report.
Ethics
This prospective descriptive study was approved by the Institutional Review Board of 108 Military Central Hospital and the Research Ethics Committee of Hanoi Heart Hospital. This study complies with the Declaration of Helsinki. Patients were advised of the study protocol and written informed consent was obtained from all patients. All the patients had previously been granted permission to use their medical records for research purposes.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas, took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no potential conflicts of interest regarding this article’s research, authorship, and/or publication.
References
- 1.Kandaswamy E, Zuo L. Recent advances in treatment of coronary artery disease: role of science and technology. Int J Mol Sci. 2018;19(2):424. doi: 10.3390/ijms19020424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hogue CW Jr, Creswell LL, Gutterman DD, Fleisher LA. Epidemiology, mechanisms, and risks: American College of Chest Physicians guidelines for the prevention and management of postoperative atrial fibrillation after cardiac surgery. Chest. 2005;128(2):9S–16S. doi: 10.1378/chest.128.2_suppl.9S [DOI] [PubMed] [Google Scholar]
- 3.Bandar AG. Arrhythmias post coronary artery bypass surgery. Coronary Artery Bypass Graft Surgery INTECH. 2018;107–147. [Google Scholar]
- 4.Akintoye E, Sellke F, Marchioli R, Tavazzi L, Mozaffarian D. Factors associated with postoperative atrial fibrillation and other adverse events after cardiac surgery. J Thorac Cardiovasc Surg. 2018;155(1):242–251. doi: 10.1016/j.jtcvs.2017.07.063 [DOI] [PubMed] [Google Scholar]
- 5.Rubin DA, Nieminski KE, Monteferrante JC, Magee T, Reed GE, Herman MV. Ventricular arrhythmias after coronary artery bypass graft surgery: incidence, risk factors and long-term prognosis. J Am Coll Cardiol. 1985;6(2):307–310. doi: 10.1016/s0735-1097(85)80165-0 [DOI] [PubMed] [Google Scholar]
- 6.Villareal RP, Hariharan R, Liu BC, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol. 2004;43(5):742–748. doi: 10.1016/j.jacc.2003.11.023 [DOI] [PubMed] [Google Scholar]
- 7.Hayıroğlu Mİ, Çınar T, Selçuk M, et al. The significance of the morphology-voltage-P-wave duration (MVP) ECG score for prediction of in-hospital and long-term atrial fibrillation in ischemic stroke. J Electrocardiol. 2021;69:44–50. doi: 10.1016/j.jelectrocard.2021.09.006 [DOI] [PubMed] [Google Scholar]
- 8.Çinar T, Hayiroğlu Mİ, Selçuk M, et al. Evaluation of electrocardiographic P wave parameters in predicting long-term atrial fibrillation in patients with acute ischemic stroke. Arq Neuropsiquiatr. 2022;80(9):877–884. doi: 10.1055/s-0042-1755322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chamchad D, Djaiani G, Jung HJ, Nakhamchik L, Carroll J, Horrow JC. Nonlinear heart rate variability analysis may predict atrial fibrillation after coronary artery bypass grafting. Anesth Analg. 2006;103(5):1109–1112. doi: 10.1213/01.ane.0000239330.45658.76 [DOI] [PubMed] [Google Scholar]
- 10.Hakala T, Vanninen E, Hedman A, Hippeläinen M. Analysis of heart rate variability does not identify the patients at risk of atrial fibrillation after coronary artery bypass grafting. Scand Cardiovasc J. 2002;36(3):167–171. doi: 10.1080/cdv.36.3.167.171 [DOI] [PubMed] [Google Scholar]
- 11.Frost L, Mølgaard H, Christiansen EH, Jacobsen CJ, Allermand H, Thomsen PE. Low vagal tone and supraventricular ectopic activity predict atrial fibrillation and flutter after coronary artery bypass grafting. Eur Heart J. 1995;16:825–831. doi: 10.1093/oxfordjournals.eurheartj.a061002 [DOI] [PubMed] [Google Scholar]
- 12.De Godoy MF, Takakura IT, Correa PR, et al. Preoperative nonlinear behavior in heart rate variability predicts morbidity and mortality after coronary artery bypass graft surgery. Med Sci Monit. 2009;15(3):CR117–22. [PubMed] [Google Scholar]
- 13.Kinoshita T, Asai T, Ishigaki T, et al. Preoperative heart rate variability predicts atrial fibrillation after coronary bypass grafting. Ann Thorac Surg. 2021;91:1176–1182. doi: 10.1016/j.athoracsur.2010.12.042 [DOI] [PubMed] [Google Scholar]
- 14.Milicevic G, Fort L, Majsec M, et al. Heart rate variability decreased by coronary artery surgery has no prognostic value. Eur J Cardiovasc Prev Rehabil. 2004;11(3):228–232. doi: 10.1097/01.hjr.0000129743.53464.c0 [DOI] [PubMed] [Google Scholar]
- 15.Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17(3):354–381. [PubMed] [Google Scholar]
- 16.Milicević G, Lakusić N, Szirovicza L, Cerovec D, Majsec M. Different cut-off points of decreased heart rate variability for different groups of cardiac patients. J Cardiovasc Risk. 2001;8(2):93–102. doi: 10.1177/174182670100800206 [DOI] [PubMed] [Google Scholar]
- 17.Abdel-Salam Z, Nammas W. Incidence and predictors of atrial fibrillation after coronary artery bypass surgery: detection by event loop recorder monitoring from a contemporary multicentre cohort. Acta Cardiol. 2017;72(3):311–317. doi: 10.1080/00015385.2017.1304716 [DOI] [PubMed] [Google Scholar]
- 18.Memetoglu ME, Kehlibar T, Yılmaz M, et al. Serum uric acid level predicts new-onset atrial fibrillation after coronary artery bypass graft operation. Eur Rev Med Pharmacol Sci. 2015;19(5):784–789. [PubMed] [Google Scholar]
- 19.Tatsuishi W, Adachi H, Murata M, et al. Postoperative hyperglycemia and atrial fibrillation after coronary artery bypass graft surgery. Circ J. 2015;79(1):112–118. doi: 10.1253/circj.CJ-14-0989 [DOI] [PubMed] [Google Scholar]
- 20.Leventopoulos G, Koros R, Travlos C, et al. Mechanisms of Atrial Fibrillation: how Our Knowledge Affects Clinical Practice. Life. 2023;13(6):1260. doi: 10.3390/life13061260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mao Z, Zhong X, Yin J, Zhao Z, Hu X, Hackett ML. Predictors associated with stroke after coronary artery bypass grafting: a systematic review. J Neurol Sci. 2015;357(1–2):1–7. doi: 10.1016/j.jns.2015.07.006 [DOI] [PubMed] [Google Scholar]
- 22.Creswell LL, Schuessler RB, Rosenbloom M, Cox JL. Hazards of postoperative atrial arrhythmias. Ann Thorac Surg. 1993;56(3):539–549. doi: 10.1016/0003-4975(93)90894-n [DOI] [PubMed] [Google Scholar]
- 23.Mathew JP, Parks R, Savino JS, et al. Atrial fibrillation following coronary artery bypass surgery: predictors, outcomes, and resource utilization. JAMA. 1996;276:300–306. doi: 10.1001/jama.1996.03540040044031 [DOI] [PubMed] [Google Scholar]
- 24.Halkos ME, Puskas JD, Lattouf OM, et al. Elevated preoperative hemoglobin A1c level is predictive of adverse events after coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2008;136(3):631–640. doi: 10.1016/j.jtcvs.2008.02.091 [DOI] [PubMed] [Google Scholar]
- 25.Bauer A, Kantelhardt JW, Barthel P, et al. Deceleration capacity of heart rate as a predictor of mortality after myocardial infarction: cohort study. Lancet. 2006;367(9523):1674–1681. doi: 10.1016/S0140-6736(06)68735-7 [DOI] [PubMed] [Google Scholar]
- 26.Bauer A, Barthel P, Müller A, Kantelhardt J, Schmidt G. Bivariate phase-rectified signal averaging-a novel technique for cross-correlation analysis in noisy nonstationary signals. J Electrocardiol. 2009;42(6):602–606. doi: 10.1016/j.j [DOI] [PubMed] [Google Scholar]
- 27.Ksela J, Suwalski P, Kalisnik JM, Avbelj V, Suwalski G, Gersak B. Assessment of nonlinear heart rate dynamics after beating-heart revascularization. Heart Surg Forum. 2009;12(1):E10–6. doi: 10.1532/HSF98.20081116 [DOI] [PubMed] [Google Scholar]
- 28.Chamchad D, Horrow JC, Samuels LE, Nakhamchik L. Heart rate variability measures poorly predict atrial fibrillation after off-pump coronary artery bypass grafting. J Clin Anesth. 2011;23(6):451–455. doi: 10.1016/j.jclinane.2010.12.016 [DOI] [PubMed] [Google Scholar]
- 29.Jideus L, Ericson M, Stridsberg M, Nilsson L, Blomstrom P, Blomstrom-Lundqvist C. Diminished circadian variation in heart rate variability before surgery in patients developing postoperative atrial fibrillation. Scand Cardiovasc J. 2001;35:238–244. doi: 10.1080/14017430152581341 [DOI] [PubMed] [Google Scholar]
- 30.Dimitropoulos G, Tahrani AA, Stevens MJ. Cardiac autonomic neuropathy in patients with diabetes mellitus. World J Diabetes. 2014;5(1):17–39. doi: 10.4239/wjd.v5.i1.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hogue CW, Domitrovich PP, Stein PK, et al. RR interval dynamics before atrial fibrillation in patients after coronary artery bypass graft surgery. Circulation. 1998;98(5):429–434. doi: 10.1161/01.cir.98.5.429 [DOI] [PubMed] [Google Scholar]
- 32.Lakusic N, Mahovic D, Sonicki Z, Slivnjak V, Baborski F. Outcome of patients with normal and decreased heart rate variability after coronary artery bypass grafting surgery. Int J Cardiol. 2013;166(2):516–518. doi: 10.1016/j.ijcard.2012.04.040 [DOI] [PubMed] [Google Scholar]
- 33.Stein PK, Domitrovich PP, Kleiger RE; CAST Investigators. Including patients with diabetes mellitus or coronary artery bypass grafting decreases the association between heart rate variability and mortality after myocardial infarction. Am Heart J. 2004;147(2):309–316. doi: 10.1016/s0002-8703(03)00520-9 [DOI] [PubMed] [Google Scholar]
- 34.Dimmer C, Tavernier R, Gjorgov N, Van Nooten G, Clement DL, Jordaens L. Variations of autonomic tone preceding onset of atrial fibrillation after coronary artery bypass grafting. Am J Cardiol. 1998;82(1):22–25. doi: 10.1016/s0002-9149(98)00231-8 [DOI] [PubMed] [Google Scholar]
- 35.Bettoni M, Zimmermann M. Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation. 2002;105(23):2753–2759. doi: 10.1161/01.cir.0000018443.44005.d8 [DOI] [PubMed] [Google Scholar]
- 36.Lakusic N, Mahovic D, Kruzliak P, Cerkez Habek J, Novak M, Cerovec D. Changes in heart rate variability after coronary artery bypass grafting and clinical importance of these findings. Biomed Res Int. 2015;2015:680515. doi: 10.1155/2015/680515 [DOI] [PMC free article] [PubMed] [Google Scholar]