Abstract
Background
Facial rejuvenation is becoming more and more popular, particularly among middle‐aged persons. There are currently many techniques for improving the aforementioned situations, but each has its drawbacks. Our study aimed to discuss the treatment effect of a composited technique for reversing both lower eyelid and midface aging.
Methods
The patient's face was designed and measured before surgery. During surgery, a traditional lower blepharoplasty incision was made. The layer between the orbital septum and the orbicularis oculi muscle was separated to approximately 4‐5 mm below the infraorbital, then the orbital septum and orbicularis retaining ligament were found to be released. A self‐made suspension curving needle subconsciously passed through the brim of the superficial cheek fat pad via the “U‐type” path and raised them to the proper location. Then sutured them to the infraorbital rim periosteum, as well as the suborbicularis oculi fat (SOOF) and the orbital septum fat. Secured the outside canthus to keep the lower lid position stable.
Results
From February 2020 to November 2022, 106 patients underwent the new surgical procedure and were successfully followed up for 20 ± 6.5 months postoperatively. The mean GAIS score was 2.42 ± 0.78, patient satisfaction rate was 95%. All of the Barton grades were decreased. The nasal base level suspension points were elevated to a level of 5 ± 2 mm. 3D measurement data revealed significant improvements.
Conclusions
The composited technique is a safe and effective way to reverse the aging of the lower eyelid and midface.
Keywords: Chagas disease reactivation, endomyocardial biopsy, heart transplantation
1. INTRODUCTION
People are increasingly concerned about how to improve facial aging. At the moment, the trend of middle facial aging shows a younger age. The sagging midface could give people an aged appearance and make them appear tired or depressed. Human aging is an extremely complex process that includes changes in the skin, fat, muscle, ligament, and bone. The superficial muscular aponeurotic system (SMAS) divides the facial fat into a superficial layer and a deep layer, and the deep layer supports the superficial layer. With age, the deep fat atrophies and collapses, causing the superficial fat to lose support and droop under the influence of gravity. Facial ligaments fixed soft tissue to bone or fascia of deep muscles, but the ligaments aged slower than the soft tissue, causing grooves and pouches. 1
Currently, the techniques for reversing mid‐facial aging include traditional rhytidectomy, injection of fillers such as autologous fat and hyaluronic acid, various suture suspensions, and photoelectric therapy. Traditional rhytidectomy mainly works on the SMAS and is associated with a high‐level surgical technique, a high degree of trauma, and a high risk of complications. Hyaluronic acid fillers have a temporary lifting effect due to their need for repeated injections. Photoelectric therapy, such as laser and radiofrequency, only has beneficial effects on mild skin aging but is ineffective in treating moderate to severe age‐related sagging. In the treatment of mid‐facial aging, multiple treatments might be required sequentially. Others were not improved vertical aging. So we developed a composited surgical method based on the aging mechanism for the symptomatic treatment of facial aging, to kill two birds with one stone.
1.1. Patients and methods
1.1.1. Inclusions
Patients who met the following inclusion criteria were enrolled: (1) Tear trough deepening, eye bag creation (Barton grades II‐III). (2) Low, flat zygomatic area. (3) Lax lower eyelid skin. (4) Nasolabial fold deepening.
1.1.2. Exclusions
Exclusion criteria: (1) Serious systemic disease; (2) Local skin infection; (3) A history of similar mid‐facial lift surgeries; (4) Zygomatic trauma; (5) The bony collapse of the midface; (6) Taking hormones or anticoagulant medicines within 2 weeks; (7) Pregnancy or lactation; (8) Too high expectations.
1.1.3. Design
The patients' facial aging was evaluated while they were standing. Patients were placed in a horizontal position and routinely disinfected and draped in towels. Drawing line: first, patients were asked to turn their eyes upwards as far as they could and then hold them still, the lower eyelid skin is tense at this point. To determine the initial amount of skin removed, use tweezers to clamp the skin until no lower eyelid ectropion occurs. The incision line extended outwards to the appropriate length from point A along the lower eyelid edge to point B. (determined by skin relaxation of the lower eyelid). The AC line was drawn according to the degree of skin relaxation, and ABC was the width of the skin to be removed. A horizontal line along the nasal base and the vertical line of the pupil center point were crossed to point D, A point E was made approximately 5 mm below the inner canthus, A point F was made approximately 5 mm below the lateral canthal ligament, and connected each point as shown in Figure 1. The distance from point D to the midpoint of the pupil was measured in a horizontal sight.
FIGURE 1.
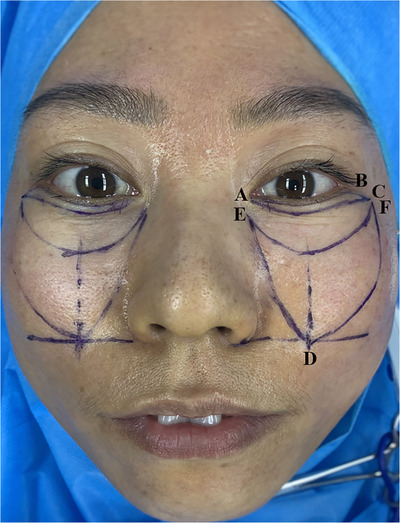
A: inner canthus B: outer canthus ABC: area to be resected D: point of the horizontal line at the base of the nose and the vertical line at the pupil midpoint; E: about 5 mm below the inner canthus F: about 5 mm below the outer canthal ligament.
1.1.4. Separation
Infraorbital foramen block anesthesia was performed with 1 mL of a 0.75% lidocaine mixture containing 1:200,000 epinephrine, the local infiltration anesthesia in the ABEF point region (1 mL suborbital nerve block could avoid midfacial enlargement from excessive anesthetics). After adequate anaesthesia, the skin was incised and removed along the ABC line segment, and the orbital septum was exposed by dissecting the orbicularis oculi. Electrocoagulation was used to achieve hemostasis. With the skin‐muscle flap in place, ophthalmic scissors were used to separate the orbicularis oculi muscle and the orbital septum to about 4–5 mm below the infraorbital margin. The orbital septal fat and orbicularis retaining ligament were released, and electrocoagulation was repeated to control the bleeding.
1.1.5. Suspension and suture
A self‐made suspension curving needle was inserted at point F. A 2‐0 non‐absorbable silk thread (Hangzhou Huawei Medical Appliance Co., Ltd., Hangzhou, Zhejiang Province, China) was passed through the brim of the superficial middle cheek fat and medial cheek fat in the direction of the drawn line, and the needle was withdrawn at point D. It was ensured that the thread in the suspension needle invariably traveled into the fat layer because if the thread at the end of the needle passed through the dermis or was accidentally placed into part of the dermis, local adhesions could occur and a small depression could be formed.
The needle continued to pass through the nasolabial fat chamber, and finally exited from point E. The suture lifted the fat area via the “U‐type” path. After pulling both ends of the suture to adjust the degree of midface lift and reduce the nasolabial folds to the proper location, the ends of the sutures were fixed with toothless pliers(Figure 2). The suture was then continued to pass through the orbital septum fat and the deep fat SOOF, all of which were continuously sutured to the periosteum at 4–5 mm of the infraorbital rim. After fixation, the patient was told to look up once more and check for eyelid malposition and retraction in the event of skin tension. If there is no problem, lateral canthopexy (the lateral portion of the orbicularis oculi was sutured to the lateral periosteal orbital rim) should be performed to avoid risk factors for lower eyelid malposition, palpebral fissure rounding, scleral show, or frank ectropion. Then the lower eyelid incision was sutured with continuous intradermal absorbable sutures, and a non‐absorption line of 7‐0 was sutured with several sutures outside the outermost layer to reduce the cross‐layer scar. The distance from point D to the pupil midpoint was measured again and the data were recorded. The same method was performed on the other side(Figures 3 and 4). We uploaded a video demonstrating the steps.
FIGURE 2.

Adjust the degree of midface lift and reduce the nasolabial folds.
FIGURE 3.
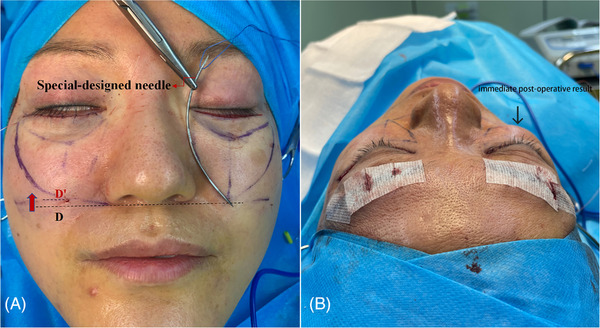
A self‐designed curving needles needle, the needle is a little over 5 cm long, and both ends are pointed (right of A). Immediate post‐operative results (left of A). Unilateral immediate postoperative effect (B).
FIGURE 4.
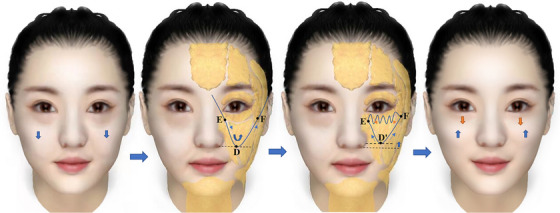
A simple diagram of the surgical procedure.
1.2. Subjective evaluations
Two plastic doctors not engaged in the procedure performed subjective evaluations. The Global Aesthetic Improvement Scale (GAIS) was utilized to rate patients' lid‐cheek, malar, and nasolabial improvements based on preoperative and 24‐month postoperative pictures (Table 1). At the 24‐month postoperative follow‐up, patients were asked to self‐evaluate the time to recovery, pain level, complications (super satisfied 4, very satisfied 3, satisfied 2, slightly satisfied 1, or dissatisfied 0), and self‐perceived age; patients were asked to estimate how many years younger (0‐10 years) they felt they were than their chronological age.
TABLE 1.
The global aesthetic improvement scale (GAIS).
| Score | Grade | Delineation |
|---|---|---|
| −1 | Worse | Appearance worse than original condition |
| 0 | No change | Appearance essentially the same as original condition |
| 1 | Improved | Obvious improvement but touch‐up or retreatment in indicated |
| 2 | Much improved | Marked improvement in condition, but not optimal for the subject; touch‐up would slightly improve the result |
| 3 | Very much improved | Optimal cosmetic result for the subject |
| GAIS, global aesthetic improvement scale. | ||
1.3. Objective evaluations
Preoperative and postoperative distance from point D to pupil midpoint was evaluated. Images were obtained using the Artec EVA 3D scanner (Artec Europe Sarl, Luxembourg). Each postoperative image was fused and overlaid on the respective preoperative image to create a three‐dimensional structure of each treated area. The blue color represents decreased height and the red color represents increased height. The fixed‐point curve measurement function of EVA was used to assess changes in the zygomatic region(Figures 5 and 6).
FIGURE 5.
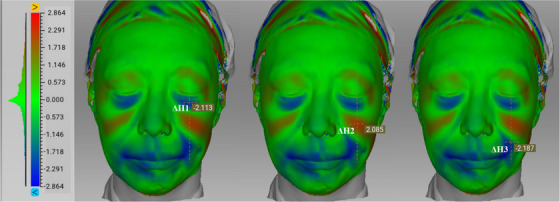
A vertical line was drawn along the midpoint of the eye fissure, and the midpoints of intersection with the lid‐cheek segment, malar segment, and nasolabial segment were denoted as ΔH1, ΔH2, and ΔH3, respectively.
FIGURE 6.
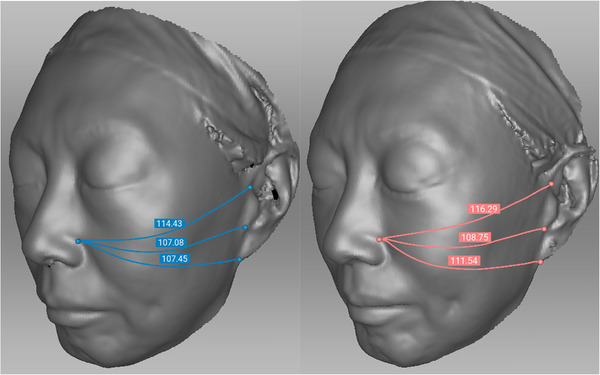
Lines between the alae nasi point and the upper tragus, lower tragus, and earlobe point were denoted as L1, L2, and L3, respectively.
1.4. Statistical analysis
The quantitative data that met the assumption of normality is represented as the mean (SD), and the changes in values before and after surgery were compared by the paired samples t‐test. All statistical analyses were performed using SPSS software, version 25.0, and p < 0.05 was considered statistically significant.
2. RESULTS
2.1. General results
From February 2020 to November 2022, 106 patients underwent the surgical procedure and 86 received a successful 24‐month postoperative follow‐up. A total of 98 women (92.5%) and 8 men (7.5%) with ages ranging from 37 to 66 years (46 ± 7.61), and Fitzpatrick skin type III‐IV were included. The dressing was changed 3 days after surgery, and the sutures were removed 5 days later; Detumescence mostly subsided one month after surgery. Figures 7, 8, 9 represent a comparison between pre‐surgery and post‐surgery.
FIGURE 7.

Case 1: A 51‐year‐old woman, pre‐surgery (A) compared with post‐surgery (B) at 12 months.
FIGURE 8.
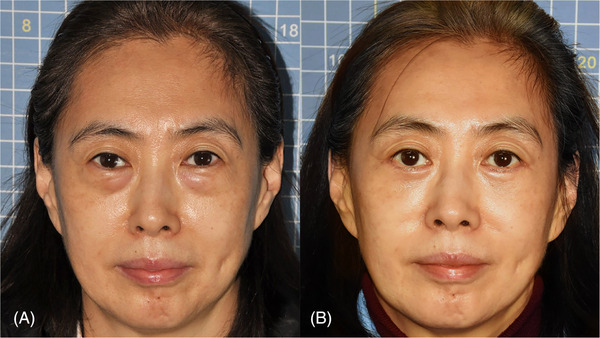
Case 2A 52‐year‐old woman, pre‐surgery (A) compared with post‐surgery (B) at 24 months.
FIGURE 9.
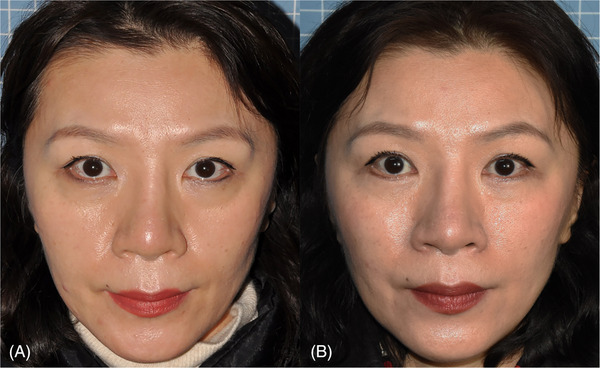
Case 3A 48‐year‐old woman, pre‐surgery (A) compared with post‐surgery (B) at 24 months.
2.2. Subjective results
In the subjective evaluation of GAIS in 86 patients 24 months after the operation by two physicians who were not present during the procedure, the eyelid‐cheek, zygomatic, and nasolabial areas had mean scores of 2.48 ± 0.78, 2.43 ± 0.75, and 2.35 ± 0.79 (range from −1 to 3), respectively (Figure 10). The average self‐satisfaction score in patients was 3.12 ± 1.06, the satisfaction rate was 95%, and the average self‐perceived age of patients was 7.3 ± 2.5 years younger than their chronological age (Table 2). Before surgery, 47 patients were classified as Barton II; two years later, 40 were classified as Barton 0, and seven as Barton I. Simultaneously, 39 patients who were graded Barton III preoperatively were all graded Barton I postoperatively.
FIGURE 10.
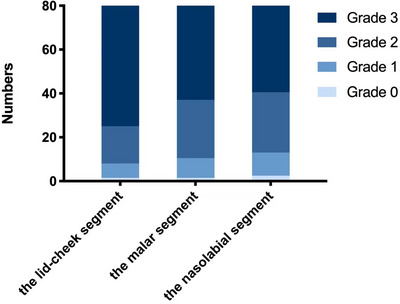
GAIS score results.
TABLE 2.
Patients self‐evalution.
| Satisfaction | N = 86 | |
|---|---|---|
| Range | 0‐4 | |
| Mean value (SD) | 3.12 ± 1.06 | |
| Ages decreases | N = 86 | |
| Range | 0‐10 | |
| Mean value (SD) | 7.3 ± 2.5 |
2.3. Objective results
In the objective evaluation, the range of elevation at the horizontal suspension point of the nasal base after surgery was 5 ± 2 mm, this was the lift distance of the middle facial fat chamber in the vertical direction, and it was adjusted according to the extent of facial skin sagging in patients. EVA3D measurements showed that the average changes in height of ∆H1, ∆H2, and ∆H3 were −1.987 ± 0.82 mm, 2.018 ± 0.78, and −2.025 ± 0.76 mm, respectively. To determine zygomatic changes, we measured three zygomatic curves on 3D images before surgery and compared them to one year later, the average increase in the zygomatic region curves of L1, L2, and L3 was 2.37 ± 0.80 mm, 2.57 ± 0.64 mm, and 3.22 ± 0.75 mm, respectively, with p‐values < 0.05 considered statistically significant (Figure 11). The change in midface volume is shown in Figure 12.
FIGURE 11.
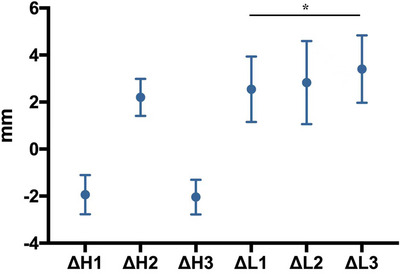
Changes in the height and curve under EVA 3D measurement.
FIGURE 12.
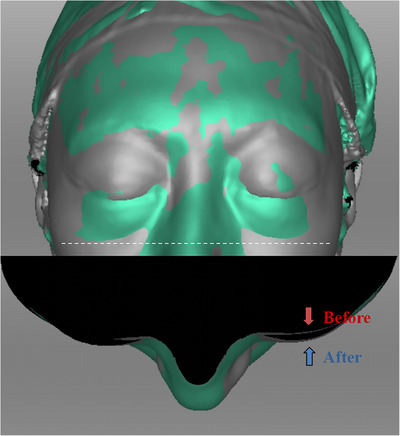
Volume change under cross section.
2.4. Complications
In these 106 patients, we did not observe any unfavorable consequences such as severe lower lid malposition and retraction, abnormal facial shape, facial numbness, facial markings, local skin depression, or suture rejection. In addition, not one of the 106 patients needed additional treatment for secondary repair. Six patients experienced mild lower eyelid ectropion in the early postoperative period. This is due to excessive swelling in the early postoperative period, which subsided two months after surgery. There was also three cases of mild scar growth one month after surgery that improved significantly after five months of silicone gel dressing and did not necessitate surgical repair.
3. DISCUSSION
The midface fat compartment is divided into two layers: deep fat and superficial fat. The superficial fat compartment comprises the following five sections: infraorbital fat, nasolabial fat, superficial medial cheek fat, middle cheek fat, and lateral temporal cheek fat. The deep fat compartment comprises the following four parts: medial SOOF, lateral SOOF, deep medial cheek fat, and buccal fat. 2 The SOOF is a suborbicularis oculi fat pad located on the deep surface of the orbicularis oculi muscle and the surface of the periosteum, which is divided into internal and external parts. The medial part of the SOOF is covered by nasolabial fat and superficial medial cheek fat, whereas the lateral part of the SOOF is located on the deep surface of the lateral orbital fat and middle cheek fat, and its volume loss is closely related to “V‐deformity”. 3 , 4 (Figure 13). Tear trough deformity refers to the presence of the lower eyelid from the inner canthus to the lower portion of the pupil's central line. The tear trough triad includes orbital fat herniation, strong attachment of the orbicularis to the arcus marginalis, and malar rim retrusion. 5
FIGURE 13.
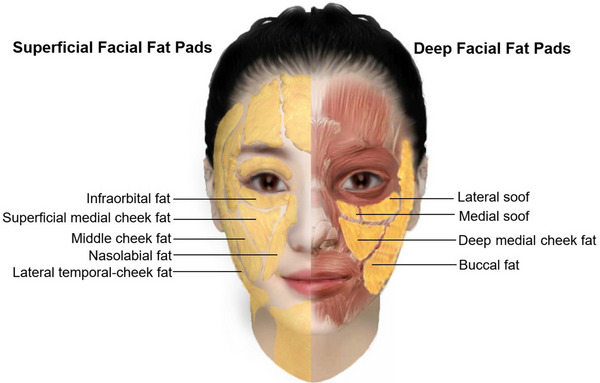
Deep and superficial facial fat compartments in the midface.
Lower blepharoplasty was described for the first time in 1923. The traditional management of this condition is based upon clinical analysis of the severity and a graded approach which ranges from transconjunctival isolated resection of lower eyelid fat to the transcutaneous release of the tear trough and orbicularis retaining ligament with caudal transposition of lower eyelid fat. Furthermore, an inside‐outside approach has also been described notably by Hidalgo combining a transconjunctival approach to release the ligament and redrape the fat and skin‐only flap to address skin redundancy. 6 Sam Hamra has developed the “composite rhytidectomy” where the arcus marginalis release, zygote‐orbicular dissection, and an orbicularis oculi suspension flap are used to blend the lid cheek junction and improve the midface. 7 In 1985, Shorr and Fallor first described that a transeyelid midface lift could be used for cosmetic and functional repair in patients with lower eyelid retraction. Since then, various scholars have studied and suggested different ways to perform midface lift procedures on different planes including temporal incisions, transconjunctival incisions, and transcutaneous incisions. In 2001, Jon 8 proposed elevating the SOOF to the infraorbital rim and intermittently suturing it to the periosteum below the orbital rim. In 2004, Patipa 9 proposed a method to tighten the orbicularis oculi muscle in the external superior direction and suture it to the lateral orbital periosteum to achieve midface lift. In 2012, Jeffrey 10 used a carbon dioxide laser to perform lysis of the orbicularis retaining ligament and lower orbicularis oculi insertion to achieve midface rejuvenation. In 2013, Bryan 11 proposed bone fixation to achieve midface lift through the conjunctiva. In 2015, Quatela 12 achieved elevation of two vectors, including the temporal area and midface, through a temporal incision. In addition, midface lift has been achieved through an endoscope. 13 , 14 Yuguang Zhang recently published Vertical “V‐Y” Advancement Lifting Based on Fat Compartments. This method can also be used to rejuvenate the lower eyelids and the midcheek. 15
Our surgical was is a composited technique, the ability to improve multiple problems such as lower eyelid skin laxity, eye bags, tear troughs, nasolabial folds, and cheek flattening through a single incision gives it a significant advantage over other procedures. Via a lower eyelid subciliary incision, we can effectively improve extension to the lateral tear groove and feel the needle during the procedure; if the needle is too deep or too shallow, it can be adjusted in time. All structures can also be precisely fixed to the infraorbital rim periosteum under direct vision via an incision, reducing the potential of lower eyelid ectropion due to intraorbital fat pulling.
The “U‐type” lift has the ability to cover the three main superficial fat chambers in the middle face, allowing for a more precise lift. Furthermore, when suturing the edges of cellulite, we can pass through part of the fascia, reducing the possibility of suture slippage within the fat. Moreover, our surgery can also improve other problems of facial aging, such as midcheek grooves and modiolus aging. The main reason behind the formation of a midcheek groove may be the abnormal fibrous connection between zygomatic skin and subcutaneous soft tissue. 16 The modiolus is a complex area located at the angle of the mouth. It has been defined as a tendon‐like structure in which muscle fibers extending from vertical and horizontal directions converge at the angle of the mouth, and it is connected with the SMAS. 17 During the postoperative follow‐up, we found that some patients showed improvement with respect to these problems.
In 86 patients, the lid‐cheek, malar, and nasolabial GAIS scores were 2.48 ± 0.78, 2.43 ± 0.75, and 2.35 ± 0.79. The average self‐satisfaction score was 3.12 ± 1.06 points, the satisfaction rate was 95%, and the average self‐perceived age of patients was 7.3 ± 2.5 years younger than their chronological age. At the two‐year postoperative follow‐up, the Barton grade decreased in all patients, indicating that both doctors and patients thought the surgical effect was ideal. The range of elevation at the horizontal suspension point of the nasal base after surgery was 5 ± 2 mm. The data is intended to objectively demonstrate the immediate post‐operative lifting effect. We used 3D measurements to objectively assess the long‐term effects of the enhancements: The average changes in lid‐cheek, malar, and nasolabial height were −1.987 ± 0.82 mm, 2.018 ± 0.78, and −2.025 ± 0.76 mm, respectively, the average increase in the zygomatic region curves of L1, L2, and L3 was 2.37 ± 0.80 mm, 2.57 ± 0.64 mm, and 3.22 ± 0.75 mm, respectively, with p < 0.05 considered statistically significant. Zygomatic changes in two aspects were measured in 3D measurements, proving objectively that our surgery can create high cheek mass.
Transconjunctival lower blepharoplasty may not significantly improve this condition because all of the patients chosen had lax orbicularis oculi and lower eyelid skin. However, the subciliary lower eyelid approach is a risk factor for lower eyelid malposition, scleral show, or frank ectropion, so we performed repeated measurements and evaluations before and after surgery. To further prevent the occurrence of various complications, a canthopexy was carried out as an add‐on to the transcutaneous approach with special attention paid to the suture incision. For individuals with keloidal hyperplasia, we recommend topical anti‐scar medication for six months after surgery.
Patients should be fully informed that this type of surgery can improve both lower eyelid and midface aging, but in patients with coexisting severe upper eyelid aging, we recommend that surgery for upper eyelid rejuvenation be performed simultaneously with surgery for lower eyelid and midface rejuvenation, as improving only the lower eyelid and midface can provide a visual impression of increased upper eyelid aging. Some of our patients have undergone upper lid rejuvenation at the same time as their midface lift, however this has no bearing on the midface lift evaluation and results. Meanwhile, in patients with very severe age‐related changes and sagging skin, we still recommend traditional rhytidectomy to achieve the most optimal results. In addition, this new surgical procedure only resets the sagging fat compartments; thus, it is recommended that it be performed with autologous fat grafting in patients with severe midface volume loss. To this end, the doctor should fully evaluate the patient before surgery to choose the best surgical plan.
It is critical to emphasise that our homemade needles are only for intraoperative manipulation and are not specific. We believe that any needle capable of passing through the superficial fat chamber in accordance with our design can achieve the same surgical result.
In addition, it should be noted that after the lift of the facial fat compartment, occasionally, it may be necessary to remove the excess skin and orbicularis oculi muscle again, and the data should be measured again to ensure the same degree of lift on both sides. Previous research found early improvement but long‐term disappointment in the midface region. Immediately following our surgery, the patient's pouch and tear groove were significantly improved, and a fuller cheek mass was achieved; good results were maintained during the two‐year post‐surgery follow‐up. We will continue to monitor the patients to see if there is a longer‐term postoperative effect.
4. CONCLUSIONS
The absence of the eyelid‐cheek junction and a high cheek mass are essential features of a youthful face, the surgical procedure outlined in this research is an efficient method for addressing both of the issues that exist in the vertical direction. Because it is consistent with the natural principles of facial aging, it is suitable for use as a reference procedure to address problems associated with midfacial aging.
Supporting information
Supporting Information
Li M, Xu H, Tian Y, Li R, Hao L. U‐type soft tissue lifting: A new composited technique for reversing lower eyelid and midfacial aging. Skin Res Technol. 2023;29:e13511. 10.1111/srt.13511
DATA AVAILABILITY STATEMENT
The datasets generated during and analyzed during the current study are publicly available.
REFERENCES
- 1. Farkas JP, Pessa JE, Hubbard B, Rohrich RJ. The science and theory behind facial aging. Plast Reconstr Surg Glob Open. 2013;1(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119:2219‐2227. [DOI] [PubMed] [Google Scholar]
- 3. Rohrich RJ, Pessa JE. The anatomy and clinical implications of perioral submuscular fat. Plast Reconstr Surg. 2009;124:266‐271. [DOI] [PubMed] [Google Scholar]
- 4. Gierloff M, Stöhring C, Buder T, Gassling V, Açil Y, Wiltfang J. Aging changes of the midfacial fat compartments: a computed tomographic study. Plast Reconstr Surg. 2012;129:263‐273. [DOI] [PubMed] [Google Scholar]
- 5. Barton FE Jr., Ha R, Awada M. Fat extrusion and septal reset in patients with the tear trough triad: a critical appraisal. Plast Reconstr Surg. 2004;113(7):2115‐2121. discussion 2122‐3. [DOI] [PubMed] [Google Scholar]
- 6. Hidalgo DA. An integrated approach to lower blepharoplasty. Plast Reconstr Surg. 2011;127(1):386‐395. [DOI] [PubMed] [Google Scholar]
- 7. Hamra ST. Building the composite face lift: a personal odyssey. Plast Reconstr Surg. 2016;138(1):85‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Turk JB, Goldman A. SOOF lift and lateral retinacular canthoplasty. Facial Plast Surg. 2001;17:037‐048. [DOI] [PubMed] [Google Scholar]
- 9. Patipa M. Transblepharoplasty lower eyelid and midface rejuvenation: part II. Functional applications of midface elevation. Plast Reconstr Surg. 2004;113:1469‐1474. discussion 1475‐1467. [DOI] [PubMed] [Google Scholar]
- 10. Schiller JD. Lysis of the orbicularis retaining ligament and orbicularis oculi insertion: a powerful modality for lower eyelid and cheek rejuvenation. Plast Reconstr Surg. 2012;129:692e‐700e. [DOI] [PubMed] [Google Scholar]
- 11. Correa BJ, Eisemann B, Eisemann M. Transconjunctival midface lift: a "hole" different fixation. J Craniofac Surg. 2013;24:987‐991. [DOI] [PubMed] [Google Scholar]
- 12. Quatela VC, Antunes MB. Transtemporal midface lifting to blend the lower eyelid‐cheek junction. Clin Plast Surg. 2015;42:103‐114. [DOI] [PubMed] [Google Scholar]
- 13. Ramirez OM. Three‐dimensional endoscopic midface enhancement: a personal quest for the ideal cheek rejuvenation. Plast Reconstr Surg. 2002;109:329‐340. discussion 341‐329. [DOI] [PubMed] [Google Scholar]
- 14. Mittelman H, Hershcovitch M. Management of the midface during rhytidectomy. Facial Plast Surg Clin North Am. 2015;23:195‐200. [DOI] [PubMed] [Google Scholar]
- 15. Sun X, Chen X, Zhang L, et al. Vertical “V‐Y” advancement lifting based on fat compartments: a new approach for lower eyelid and midcheek rejuvenation. Plast Reconstr Surg. 2022;150(3):550‐557. [DOI] [PubMed] [Google Scholar]
- 16. Du Y, Zhong Y, Wang Z, Sui H, Luo S. Anatomic characteristics and treatment of the midcheek groove by deep filling. Dermatol Surg. 2021;47:e47‐e52. [DOI] [PubMed] [Google Scholar]
- 17. Yu SK, Lee M‐H, Kim H‐S, Park J‐T, Kim H‐J, Kim H‐J. Histomorphologic approach for the modiolus with reference to reconstructive and aesthetic surgery. J Craniofac Surg. 2013;24:1414‐1417. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Data Availability Statement
The datasets generated during and analyzed during the current study are publicly available.


