Abstract
AIM
To assess the visual correction of patients with different degrees of astigmatism with toric soft contact lenses (TSC).
METHODS
It was a real-world study with prospective and single-arm design. A total of 384 patients with astigmatism who came for TSC fitting and alignment from November 2022 to January 2023 were included. According to the difference in astigmatism, patients were divided into groups A (cylinder degree: -0.75 to -0.50 D), B (cylinder degree: -1.75 to -1.00 D) and C (cylinder degree ≤ -2.00 D), and followed up on the day of wear, 1wk, 1 and 3mo, mainly to observe visual acuity, refraction, lens fit, visual quality and comfort at 1wk after wear. The visual acuity success rate and the overall success rate of the fitting were evaluation indicators (taking into account the four dimensions of visual acuity, fitting, quality of vision and comfort). The visual acuity success rate was calculated by taking “corrected visual acuity with contact lenses is no less than 1 line or better than best spectacle-corrected visual acuity” (i.e. corrected visual acuity with contact lenses is 1 line below, equal to, one line above or more than best spectacle-corrected visual acuity) as the criterion for visual success, and the the overall success rate of the fitting was calculated by using the comprehensive indicators (visual acuity, fit, visual quality, comfort) to meet certain conditions as the judgment criteria for successful fitting.
RESULTS
After 1wk of wearing TSC, the visual acuity success rates of patients were 100% (207/207), 98.58% (139/141) and 97.22% (35/36) in the three groups, respectively, with residual cylinder closed to 0. The acceptability of the lens fitting was over 95%; the incidence of adverse visual symptoms was within 10% and the comfort acceptability was over 97%. The overall success rate of fitting for patients with high, medium and low astigmatism was 93.72% (194/207), 90.78% (128/141) and 88.89% (32/36), respectively.
CONCLUSION
TSC (model: G&G POP·CT) are effective in correcting astigmatism in patients with different degrees of astigmatism.
Keywords: toric soft contact lenses, astigmatism, visual acuity
INTRODUCTION
According to epidemiological trends in myopia, nearly 5 billion and 1 billion people worldwide will be affected by myopia and high myopia by 2050, respectively[1]. There is a growing market demand for myopia correction products. Soft contact lenses have been applied to the tear layer of the cornea directly and are physiologically compatible with the human eye for the purpose of vision correction[2]. Soft contact lenses, in a “safe, convenient and aesthetic” way, overcome the reduction of the image of objects and the trigeminal effect, which is caused by glasses. It has become an important means of refractive error correction[3]–[4].
However, astigmatism correction is a huge challenge for soft contact lenses. According to Holden's[5] study, the average astigmatism of contact lens wearers is 0.83 D, of which about 62% have an astigmatism of 0.50 D or more, about 45% have an astigmatism of 0.75 D or more, and 35% have an astigmatism of 1.00 D or more[6]–[7]. The uncorrected astigmatism is associated with reduced visual acuity, visual fatigue, poor quality of vision etc[8]. The inability to tolerate the visual impact of residual astigmatism is an important factor for many patients to give up on spherical soft contact lenses[9].
To solve the problem of residual astigmatism after wearing lenses, the first clinical use of toric soft contact lenses dates back to 1979[10]. With the development of society and the change in consumer awareness in recent years, the demand for toric soft contact lenses has been increasing gradually, and their design and the selection of parameters have been improving constantly[11]. Toric soft contact lenses are for the correction of full-eye astigmatism. In clinical practice, there are differences in the degree of astigmatism of the wearer. There are no clear reports on whether these differences can lead to limitations of vision correction in patients with high degrees of astigmatism, which may affect subsequently the visual acuity and fitting success rate of patients with different degrees of astigmatism. Therefore, the evaluation of visual acuity, diopter, lens fit, visual quality and comfort after wearing toric soft contact lenses for subjects with low, medium and high astigmatism can provide a reference for patients with different astigmatism degrees when choosing the treatment of astigmatism.
This study aimed to compare the visual acuity correction of patients with different degrees of astigmatism with toric soft contact lenses, and to determine the visual acuity success rate and overall success rate of fitting with toric soft contact lenses. The results help to understand whether the toric soft contact lenses can provide the same astigmatism correction effect for patients with different astigmatism degrees.
SUBJECTS AND METHODS
Ethical Approval
It was a real-world study with prospective and single-arm design. The Medical Ethics Committee of Xi'an People's Hospital (Xi'an Fourth Hospital) has reviewed and approved the medical study project (No.20220146). Written informed consent was obtained from all of the patients after explaining the purpose and possible consequences of the study.
Subjects
Totally 384 patients with astigmatism, who came to the hospital for toric soft contact lenses fitting from November 2022 to January 2023, were chosen. Inclusion criteria: 1) Eighteen years of age or older, regardless of gender; 2) By subjective refraction, both eyes have spherical degree between 0.00 and -10.00 D (contains 0.00 and -10.00 D), astigmatism between -0.50 and -3.75 D (contains -0.50 and -3.75 D) and astigmatism axis between 0° to 180°; 3) Best spectacle-corrected visual acuity (BSCVA) should be no more than 0.1 (logMAR visual acuity) in either eye. Exclusion criteria: 1) Suffering from various eye diseases, e.g. acute or chronic inflammation of the eye, glaucoma, abnormal corneal perception, corneal epithelial defects, corneal endothelial cell reduction, xerophthalmia etc., or judged by an ophthalmologist not fit for soft contact lenses; 2) Suffering from a systemic disease which may affect the eye, or judged by an ophthalmologist not fit for soft contact lenses; 3) History of contact lens allergy or care product allergy. Depending on the degree of astigmatism in the whole eye, there were three groups as follows: Group A (cylinder degree of -0.75 to -0.50 D), Group B (cylinder degree of -1.75 to -1.00 D) and Group C (cylinder degree ≤-2.00 D).
Product Information
The parameters of the product used in this study are shown in Table 1.
Table 1. Lens parameters.
D: Diopter.
Inspection Indicators
The follow-up period was 3mo, with visits at 5 follow-up time points: screening phase, initial lens wearing, 1wk, 1 and 3mo. At each follow-up visit, a specialist ophthalmic examination was carried out. Visual acuity was examined through the E Standard Logarithm Eyesight Table, including uncorrected distance visual acuity (UDVA), corrected visual acuity with contact lenses (CVA) and BSCVA, statistical analysis was performed using logMAR visual acuity. Obtain spherical and cylinder degree in both eyes by subjective refractive examination with phoroptor (TOPCON). Slit lamp was used to assess lens fitting, lens coverage, tightness, mobility and centration. Moreover, the overall comfort was evaluated by asking patients if they had any adverse visual symptoms, like halos, double vision etc.
The evaluation indicators were visual acuity success rate and the overall success rate of the fitting. “CVA with contact lenses is no less than 1 line or better than BSCVA” (i.e. CVA with contact lenses is 1 line below, equal to, one line above or more than BSCVA) as a criterion for visual acuity success; The overall success rate of the fitting was comprehensively judged from the four dimensions of visual acuity, lens fitting (coverage, tightness, mobility, center positioning), visual quality (halo, ghosting) and comfort at the 1-week follow-up, and the “four indicators achieved at the same time” in Table 2 was used as the judgment standard for successful fitting to calculate the overall success rate.
Table 2. The criterion for overall success rate of fitting.
| No. | Index | Evaluation criteria |
| 1 | Visual acuity | No less than 1 line of CVA compared to the BSCVA |
| 2 | Lens fitting | The coverage, tightness, mobility, and centration are within an acceptable range |
| 3 | Visual quality | No halo, ghosting or mild symptoms |
| 4 | Comfort | The comfort level is evaluated as “good”, “very good” and “excellent” |
CVA: Corrected visual acuity with contact lenses; BSCVA: Best spectacle-corrected visual acuity.
Statistical Analysis
Statistical analysis of the data was performed by SPSS 22.0 (International Business Machines Corporation, IBM, https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-22). All statistical tests were two-tailed, and if P<0.05, it would be considered statistically significant for the differences tested. The measurement data were described by mean±standard deviation (SD), and were described by the Kruskal-Wallis H test. The numerical or hierarchical data were described in the form of percentage, and the difference analysis was performed by using the Kruska-Wallis H method.
RESULTS
Subjects' Profile
Totally 384 subjects participated in the study including 60 males and 324 females, with an age range of 18 to 52, a spherical diopter range of -0 to -10 D and a cylinder degree range of -0.5 to -3.5 D. At the time of dispensing, 207, 141 and 36 patients were in Groups A, B, and C, respectively. The baseline information of the three groups is detailed in Table 3.
Table 3. Basic information of the three groups at baseline.
| Groups | Age | Sexual distribution |
UDVA | Spherical diopter (D) | Cylinder degree (D) | |
| Male, n (%) | Female, n (%) | |||||
| Group A | 30.29±7.33 | 28 (13.53) | 179 (86.47) | 0.84±0.37 | -4.02±2.03 | -0.60±0.12 |
| Group B | 30.08±7.45 | 24 (17.02) | 117 (82.98) | 0.90±0.40 | -4.28±2.43 | -1.24±0.26 |
| Group C | 31.11±7.88 | 8 (22.22) | 28 (77.78) | 1.00±0.38 | -5.04±1.48 | -2.38±0.44 |
| H | 0.495 | 2.088 | 4.287 | 9.300 | 320.575 | |
| P | 0.781 | 0.352 | 0.117 | 0.010 | <0.001 | |
Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D; D: Diopter; UDVA: Uncorrected distance visual acuity; H: Test statistics for Kruskal-Wallis H test.
All of the subjects attended the 1-week follow-up visit. For dropout, at the 1-month follow-up visit, there were 14 in Group A, 10 in Group B and 3 in Group C; at the 3-month follow-up, there were 13 in Group A, 14 in Group B and 3 in Group C. A total of 327 subjects completed all follow-up visits, 180 in Group A, 117 in Group B and 30 in Group C.
Visual Acuity
The changes in visual acuity over time in the three groups are shown in Table 4. There was no statistical difference for UDVA in baseline among the three groups (H=4.287, P=0.117). The difference in the CVA among the three groups was statistically significant (all P<0.05) at initial lens wearing and at 1-week follow-up visit, when Group A had the best visual acuity and Group C had the lowest visual acuity. However, with the extension of the wearing time, patients' visual acuity in Group C improved gradually, and Group C could reach the same level as Group A and Group B at 1-month and 3-month follow-up visits, with no statistically significant difference among the three groups (all P>0.05).
Table 4. Visual acuity of the three groups at each follow-up visit.
| Groups | UDVA, baseline | CVA |
|||
| Initial lens wearing | 1wk | 1mo | 3mo | ||
| Group A | 0.84±0.37 | 0.02±0.04 | 0.01±0.04 | 0.02±0.04 | 0.01±0.04 |
| Group B | 0.90±0.40 | 0.03±0.07 | 0.03±0.06 | 0.03±0.06 | 0.03±0.06 |
| Group C | 1.00±0.38 | 0.04±0.08 | 0.03±0.07 | 0.03±0.06 | 0.02±0.06 |
| H | 4.287 | 8.238 | 6.393 | 3.964 | 4.633 |
| P | 0.117 | 0.016 | 0.041 | 0.138 | 0.099 |
Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D; UDVA: Uncorrected distance visual acuity; CVA: Corrected visual acuity with contact lenses; H: Test statistics for Kruskal-Wallis H test.
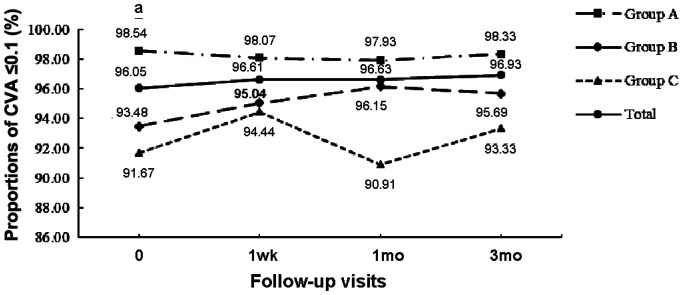
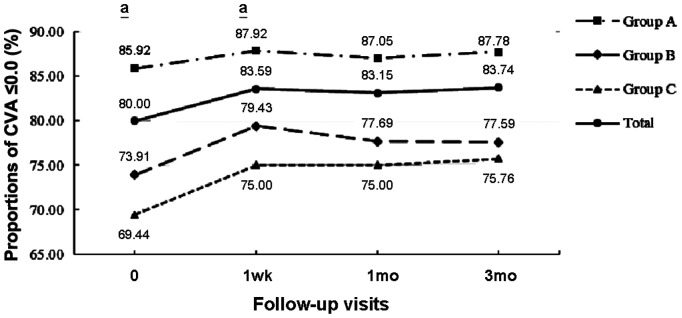
logMAR visual acuity of 0.1 can meet people's daily work, life and social needs. The proportion of patients in the three groups whose CVA could achieve 0.1 or better at different follow-up periods is shown in Figure 1. At initial lens wearing time, there was a statistically significant difference among the three groups in the proportion of patients with visual acuity of 0.1 or better (H=7.590, P=0.022), and Group A had a significantly higher proportion of patients with visual acuity of 0.1 than Group C. There was no significant difference among the three groups in the proportion of patients with visual acuity of 0.1 or better in the rest of the follow-up visits (all P>0.05). For further analysis, the proportion of patients in each of the three groups achieving a CVA of 0.0 or better at each follow-up visit is shown in Figure 2. The distribution of CVA≤0.0 at each follow-up visit among the three groups was generally consistent with that of CVA≤0.1, and there were no significant differences among groups at all follow-up visits (all P>0.05) except for the initial lens wearing time and the 1-week follow-up visit (both P>0.05). In addition, Group A had the highest proportions of CVA≤0.1 and 0.0 at each follow-up visit, with the best visual acuity correction, and both were higher than the proportions of CVA≤0.1 and 0.0 for all patients at the corresponding follow-up points.
Figure 1. The proportion of visual acuity achieving 0.1 or better in each group at various follow-up visits.
aP<0.05, representing a statistically significant difference among the three groups; X-axis: The proportion of visual acuity achieving 0.1 or better; Y-axis: Various follow-up visits; CVA: Corrected visual acuity with contact lenses; Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D.
Figure 2. The proportion of visual acuity achieving 0.0 or better in each group at various follow-up visits.
aP<0.05, representing a statistically significant difference among the three groups; X-axis: The proportion of visual acuity achieving 0.0 or better; Y-axis: Various follow-up visits; CVA: Corrected visual acuity with contact lenses; Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D.
CVA is a visual indicator of visual acuity correction. If “CVA is no less than 1 line or better than BSCVA” (i.e. CVA is 1 line below, equal to, one line above or more than BSCVA) is used as the criterion for visual acuity success. The visual acuity success rates for the three groups at each follow-up visit are shown in Table 5. There was no significant difference in visual acuity success rate among the three groups at the follow-up visits (all P>0.05), except for the initial lens wearing time (H=12.056, P=0.002). At 1-week follow-up visit, the visual acuity success rates for the three groups were 100% (207/207), 98.58% (139/141) and 97.22% (35/36), respectively (H=4.209, P=0.122). This shows that patients with different degrees of astigmatism can achieve visual acuity of 0.1 or more with toric soft contact lenses, with a visual acuity success rate of 97% or more.
Table 5. Visual acuity success rate of three groups at various follow-up visits.
| Groups | Initial lens wearing | 1wk | 1mo | 3mo |
| Group A | 100.00 (206/206) | 100.00 (207/207) | 100.00 (193/193) | 100.00 (180/180) |
| Group B | 99.28 (137/138) | 98.58 (139/141) | 99.23 (129/130) | 99.14 (115/116) |
| Group C | 94.44 (34/36) | 97.22 (35/36) | 96.97 (32/33) | 100.00 (30/30) |
| H | 12.056 | 4.209 | 4.777 | 1.810 |
| P | 0.002 | 0.122 | 0.092 | 0.404 |
Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D; H: Test statistics for Kruskal-Wallis H test.
Cylinder Degree
The changes of refractive error over time in the three groups are shown in Table 6. Before lens wearing, there was a statistical difference among the three groups in terms of cylinder degree with naked eye (H=320.575, P<0.001), with Group A having the lowest cylinder degree and Group C having the highest cylinder degree. After wearing, the residual cylinder degree were close to 0 in all three groups and were stable at all follow-up visits, with no significant difference among the three groups (P>0.05). It shows that patients with different degrees of astigmatism have achieved good correction with toric soft contact lenses.
Table 6. Cylinder degree of three groups at various follow-up visits.
| Groups | Naked cylinder degree, initial lens wearing | Residual cylinder degree |
|||
| 1wk | 1mo | 3mo | Initial lens wearing | ||
| Group A | -0.60±0.12 | -0.11±0.23 | -0.12±0.25 | -0.11±0.22 | -0.12±0.23 |
| Group B | -1.24±0.26 | -0.13±0.27 | -0.13±0.29 | -0.14±0.31 | -0.17±0.31 |
| Group C | -2.38±0.44 | -0.13±0.40 | -0.13±0.39 | -0.09±0.35 | -0.18±0.39 |
| H | 320.575 | 0.635 | 0.364 | 0.183 | 3.268 |
| P | <0.001 | 0.728 | 0.834 | 0.913 | 0.195 |
Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D; H: Test statistics for Kruskal-Wallis H test.
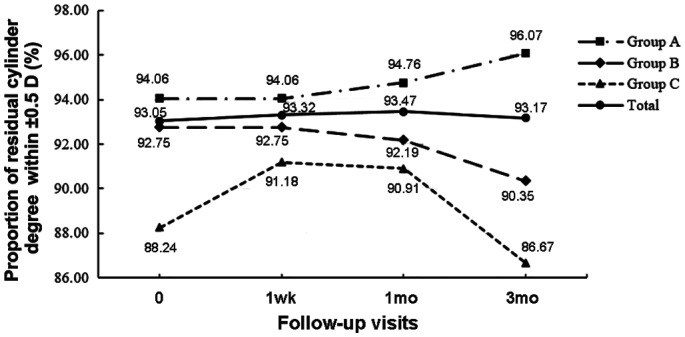
Statistically, the proportion of patients with a residual cylinder degree of ±1.0 D was higher in all three groups after lens wearing, approaching 100%. At 1-week follow-up visit, Group A, Group B and Group C had 201 eyes (99.50%), 136 eyes (98.55%) and 33 eyes (97.06%) with a residual cylinder degree of ±1.0 D, respectively, and all achieved 97% or more. The proportion of patients in the three groups with a residual cylinder degree of ±0.5 D at each follow-up visit is shown in Figure 3. There was no statistical difference among the three groups in the proportion of patients with a residual cylinder degree of ±0.5 D (all P>0.05). At 1-week follow-up visit, 190 eyes (94.06%), 128 eyes (92.75%) and 31 eyes (91.18%) in groups A, B, and C, respectively, had a residual cylinder degree of ±0.5 D.
Figure 3. The proportion of residual cylinder degree within ±0.5 D for each group at various follow-up visits.
X-axis: The proportion of residual cylinder degree within ±0.5 D; Y-axis: Various follow-up visits; Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D.
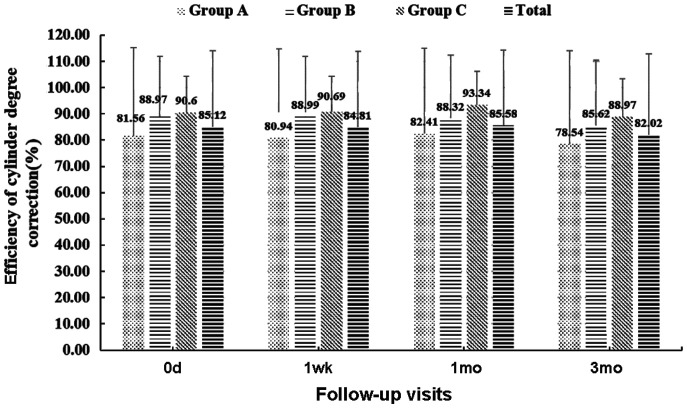
In order to further investigate the effect of the correction of cylinder degree in the three groups of patients after lens wearing, the ratio of the reduction of cylinder degree in each patient to the cylinder degree before lens wearing was defined as the efficiency of cylinder degree correction. Statistically, at 1-week follow-up visit, the cylinder degree correction efficiency of Group A, Group B, and Group C were 80.94%, 88.99% and 90.69% respectively, and all reached over 80% (Figure 4). There was no statistical difference among the three groups in terms of the efficiency of cylinder degree correction at each follow-up visit (P>0.05).
Figure 4. The efficiency of cylinder degree correction in different groups at various follow-up visits.
X-axis: The efficiency of cylinder degree correction; Y-axis: Various follow-up visits; Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D.
Lens Fitting (Coverage, Looseness, Mobility, Centration)
At 1-week follow-up visit, the percentages of patients whose lens fitting assessment was within the acceptable range in the three groups were 98.07%, 98.58% and 97.22%, respectively (P>0.05). In terms of lens coverage and tightness, all three groups were acceptable; in terms of lens mobility, one eye in Group A was unacceptable and the rest were acceptable; in terms of centration, there were four, two and one eyes, which was unacceptable, in Groups A, B, and C, with acceptability levels of 98.07%, 98.58% and 97.22%, respectively. At the 3-month follow-up visit, the percentages of patients whose lens fitting assessment was within the acceptable range in all three groups were still over 95%, and there was no statistical difference in lens fitting assessment (all P>0.05).
Visual Quality (Halos, Ghosting) and Comfort
At 1-week follow-up visit, the proportions of patients with no halos or mild halos symptoms in three groups were 99.04%, 99.29% and 94.44%, respectively, and the proportions with no double vision or mild double vision symptoms were 97.10%, 95.74%, and 91.67%, respectively. There was lower visual quality in Group C. However, there was no significant difference among three groups (all P>0.05). The percentages of comfort ratings of “good”, “very good” and “excellent” were 97.58%, 97.16% and 100% in the three groups, respectively (all P>0.05). At the 3-month follow-up visit, the performance of the three groups in terms of visual quality and comfort was almost the same as that at the 1-week follow-up visit.
Overall Success Rate of Fitting
According to Table 2, the overall success rates of fitting were calculated, and the values were 93.72% (194/207), 90.78% (128/141) and 88.89% (32/36) for the three groups, respectively, with the highest for Group A and the lowest for Group C. There was no statistical difference among the groups (H=1.602, P=0.449). The analysis of cases of the fitting failure in each group is shown in Table 7. It presents that poor visual quality was the main reason for fitting failure in the three groups, with 43.75% (7/16), 46.67% (7/15) and 66.67% (4/6) of the failures related to visual quality in the three groups, respectively. Moreover, failed cases in Groups A and B were more affected by comfort, while Group C was more impacted by visual acuity and fitting.
Table 7. Main causes of fitting failure.
| Groups | Dimension 1, visual acuity | Dimension 2, lens fitting | Dimension 3, visual quality | Dimension 4, comfort |
| Group A | 0 | 4 (25.00%) | 7 (43.75%) | 5 (31.25%) |
| Group B | 2 (13.33%) | 2 (13.33%) | 7 (46.67%) | 4 (26.67%) |
| Group C | 1 (16.67%) | 1 (16.67%) | 4 (66.67%) | 0 |
Group A: Cylinder degree range of -0.75 to -0.50 D; Group B: Cylinder degree range of -1.75 to -1.00 D; Group C: Cylinder degree ≤-2.00 D;
DISCUSSION
Astigmatism is a state of refraction that occurs when parallel light is refracted through the eye and instead of forming a clear focal point, two focal lines and a minimum dispersion circle are imaged on the retina at different locations in space. Astigmatism can occur alone or in combination with myopia or hyperopia, and affects approximately 13% of the population[12]. However, the prevalence of astigmatism tends to increase with age. In Indonesia, there are 18.5% of people over 21 years of age having astigmatism ≥1.0 D[13], 36.1% of people aged more than 40 having astigmatism≥1.0D in Korea[14], and 45.6% of people aged more than 50 having astigmatism ≥1.0 D in California[15]. The increase in astigmatism is often accompanied by an increase in higher-order aberrations such as coma[16], which in turn affects visual quality. Harvey[17] realized that astigmatism reduced the implementation capacity of tasks with high visual demands. Astigmatism can also reduce the speed and fluency of reading for adults and children[18]–[19]. Moreover, astigmatism may cause abnormal regulatory function, which is more likely to lead to the development of myopia[20]. Astigmatism not only affects vision, but also affects visual development. Children with oblique axis astigmatism are more likely to develop amblyopia[21]. Therefore, astigmatism correction is not only conducive to improving the visual quality of patients, improving their quality of life, but also conducive to visual development.
Currently, the commonly used methods for correcting astigmatism include wearing frame spectacles, corneal contact lenses, and refractive surgery[17]. Frame spectacles are a safe and reliable method of refractive correction that has been in use for many years. However, one major limitation of the frame glasses is that they cannot rotate with the eyeball, which limits the visual field, affects the appearance, and can cause the visual object to become smaller and deformed[22]–[23]. Refractive surgery is a surgical procedure that changes the refractive state of the eye, including LASIK surgery[24]–[25], lens implantation[26]–[27], and limbal relaxing incisions[28], etc. Although these surgeries can achieve certain astigmatism correction effects, they have the characteristics of trauma, long-term recovery of vision and medication, certain requirements for eye parameters, problems with postoperative dry eyes, nighttime glare, and refractive regression. The pathophysiological changes that occur after surgery are uncertain[29]–[30].
Soft corneal contact lenses, also known as contact lenses, are directly attached to the tear layer of the cornea and are physiologically compatible with the human eye, achieving the goal of vision correction[31]. As a “safe, convenient, and beautiful” method, soft corneal contact lenses overcome the narrowing effect and the prism effect of frame spectacles on the object image, and continue to be active in the fields of refractive error correction, beauty, and other fields. The toric design of toric soft contact lenses is to correct astigmatism and the product has been used clinically for over 40y. However, a European study showed that among all soft contact lens wearers, about 25% of them wear toric soft contact lenses (among them, Russia has the lowest proportion, accounting for 6%, and Portugal has the highest proportion, accounting for 48%)[6], which is far lower than the proportion of astigmatism patients in the contact lens wearers (astigmatism ≤-0.50 D 62%, astigmatism ≤-0.75 D 45%, and astigmatism ≤-1.00 D 35%)[7]. The main factors contributing to the low popularity of toric soft contact lenses are as follows: 1) More difficult fitting requires more time and advanced technology; 2) The axial instability of astigmatism affects the visual effect; 3) Uneven lens thickness caused by toric design negatively affects wearing comfort; 4) Patient's lack of understanding of the product, etc.
To assess the visual acuity correction of patients with different degrees of astigmatism with toric soft contact lenses and to determine the visual acuity success rate and overall success rate of fitting with toric soft contact lenses.
As a real-world study with a prospective and single-arm design, this study assessed the visual acuity success rate and overall success rate of patients with different degrees of astigmatism with toric soft contact lenses through a large sample size clinical tracking in a real-world environment. This study covers a wide range of people, with 384 cases screened for inclusion and completing initial wearing, with an astigmatism range of -0.50 to -3.00 D. There are 207, 141, and 36 patients with high, medium, and low degree astigmatism, respectively, with a ratio of about 6:4:1, which is basically consistent with the true distribution characteristics of whole eye astigmatism. The results of this study indicate that after wearing toric soft contact lenses with different degrees of astigmatism, the visual acuity of all patients reaches above 0.03 and the residual cylindrical is close to 0.
The overall success rate of fitting (visual acuity, lens fitting, visual quality, and comfort) for patients with high, medium and low astigmatism was 88.89% to 93.72%, higher than the reported 70% to 80%[9]. This indicates that the corrective effect of G&G POP·CT toric soft contact lenses is universal and applicable to the correction of vision in patients with different degrees of astigmatism, with a success rate that can meet expectations. Consistent with the ideal indications mentioned in previous studies with an astigmatism range of 1.0 to 2.5 D[32] or 1.0 to 3.0 D[33].
Although patients with different degrees of astigmatism can achieve the goal of correcting astigmatism and improving vision after wearing toric soft contact lenses, the clinical manifestations of patients with different astigmatism in this study are different. The efficiency of cylinder degree correction in patients with high degree astigmatism is higher than that in patients with low degree astigmatism. However, in the early stage of wearing lenses, the visual acuity of patients with low degree astigmatism can improve to 0.02, while the improvement of the visual acuity of patients with high degree astigmatism is relatively slow. In addition, patients with low degree astigmatism have the highest rates of visual acuity reaching 0.1 and above 0.0. It has been clearly pointed out in the literature that patients with oblique axis simple astigmatism exceeding 2.50 D are more difficult to correct[34].
In the process of astigmatism correction, the astigmatic axis of the toric soft contact lenses needs to be consistent with that of the entire eye. The balance between biological mechanical force and lens stability is an important factor affecting the effectiveness of astigmatism correction, and any axial deviation will generate additional astigmatism. The shape of the lens and ocular surface, blink movement, and lens mobility can all affect the position and stability of the lens[35]. Therefore, this study uses lens fitting as one of the evaluation criteria for the overall fitting success rate. In this study, all patients were acceptable for lens coverage, tightness, and mobility, but there were patients with different astigmatism who were not acceptable for centration with a proportion of about 2%. This may be related to factors such as lens design, eyelid tension, and inconsistency in axial position between corneal astigmatism and total astigmatism.
In this study, visual quality was used as another evaluation criterion for the overall fitting success rate. Patients with different degrees of astigmatism have different proportions of halos and ghosting, and patients with high degrees of astigmatism have relatively poor visual quality. Poor visual quality is the main reason for fitting failure in the three groups of failed cases. There are 43.75% (7/16), 46.67% (7/15) and 66.67% (4/6) of the failures related to visual quality in the three groups, respectively. This may be due to the fact that the toric soft contact lenses typically require the lens to align with the corresponding position in the astigmatic axis after blinking, and each blink may cause a small rotation of the lens, resulting in fluctuations in visual quality[36]–[37].
Chaudhry et al[38] compared visual acuity, comfort, and patient preference in a soft toric contact lens versus soft spherical contact lens in low astigmatic subjects (0.75 to 1.25 D) and found that wearing toric contact lens had better vision and visual quality, and significantly lower fatigue scores. Therefore, it is considered that patients with low to moderate astigmatism should prefer soft toric contact lens. However, chaudhry's study did not evaluate patients with higher degrees of astigmatism. In this study, according to the results of real-world studies, patients with different degrees of astigmatism who wear toric soft contact lenses (model: G&G POP·CT) can effectively improve their visual acuity and significantly reduce their residual cylinder. The visual acuity success rates of patients with high, medium, and low astigmatism were 100% (207/207), 98.58% (139/141) and 97.22% (35/36), respectively. The overall success rate of fitting (considering the four dimensions of visual acuity, lens fitting, visual quality, and comfort) of patients was 93.72% (194/207), 90.78% (128/141) and 88.89% (32/36), respectively. This provides a theoretical basis and data support for the fitting of toric soft contact lenses. However, there are still certain limitations in this study. The low number of subjects in the high astigmatism group may result in an uneven population among the three groups, which may have a certain impact on the statistical results.
Acknowledgments
Foundation: Supported by Key R&D Plan of Shaanxi Province: Key Industrial Innovation Chain (Cluster) - Social Development Field (No.2022ZDLSF03-10).
Conflicts of Interest: Zhang GY, None; Ye L, None; Wang WJ, None; Guo YM, None; Wei JH, None; Ren MX, None.
REFERENCES
- 1.Fricke TR, Jong M, Naidoo KS, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050:systematic review, meta-analysis and modelling. Br J Ophthalmol. 2018;102(7):855–862. doi: 10.1136/bjophthalmol-2017-311266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morgan PB, Sulley AL. Challenges to the new soft contact lens wearer and strategies for clinical management. Cont Lens Anterior Eye. 2023;46(3):101827. doi: 10.1016/j.clae.2023.101827. [DOI] [PubMed] [Google Scholar]
- 3.Waghmare SV, Jeria S. A review of contact lens-related risk factors and complications. Cureus. 2022;14(10):e30118. doi: 10.7759/cureus.30118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhee MK, Jacobs DS, Dhaliwal DK, Szczotka-Flynn L, Prescott CR, Jhanji V, Steinemann TL, Koffler BH, Jeng BH. Contact lens safety for the correction of refractive error in healthy eyes. Eye Contact Lens. 2022;48(11):449–454. doi: 10.1097/ICL.0000000000000938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holden BA. The principles and practice of correcting astigmatism with soft contact lenses. Clin Exp Optom. 1975;58(8):279–299. [Google Scholar]
- 6.Efron N, Morgan PB, Helland M, Itoi M, Jones D, Nichols JJ, van der Worp E, Woods CA. Soft toric contact lens prescribing in different countries. Cont Lens Anterior Eye. 2011;34(1):36–38. doi: 10.1016/j.clae.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Lim CHL, Stapleton F, Mehta JS. Review of contact lens-related complications. Eye Contact Lens. 2018;44(Suppl 2):S1–S10. doi: 10.1097/ICL.0000000000000481. [DOI] [PubMed] [Google Scholar]
- 8.Schallhorn SC, Hettinger KA, Pelouskova M, Teenan D, Venter JA, Hannan SJ, Schallhorn JM. Reply: effect of residual astigmatism on uncorrected visual acuity and patient satisfaction in pseudophakic patients. J Cataract Refract Surg. 2021;47(11):1493–1494. doi: 10.1097/j.jcrs.0000000000000806. [DOI] [PubMed] [Google Scholar]
- 9.Sulley A, Young G, Lorenz KO, Hunt C. Clinical evaluation of fitting toric soft contact lenses to current non-users. Ophthalmic Physiol Opt. 2013;33(2):94–103. doi: 10.1111/opo.12028. [DOI] [PubMed] [Google Scholar]
- 10.Maltzman BA. Soft toric lenses. Curr Opin Ophthalmol. 1992;3(1):117–119. doi: 10.1097/00055735-199202000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Chao C, Skidmore K, Tomiyama ES, Wolffsohn JS, Richdale K. Soft toric contact lens wear improves digital performance and vision-a randomised clinical trial. Ophthalmic Physiol Opt. 2023;43(1):25–34. doi: 10.1111/opo.13053. [DOI] [PubMed] [Google Scholar]
- 12.Zhang J, Wu YF, Sharma B, Gupta R, Jawla S, Bullimore MA. Epidemiology and burden of astigmatism: a systematic literature review. Optom Vis Sci. 2023;100(3):218–231. doi: 10.1097/OPX.0000000000001998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saw SM, Gazzard G, Koh D, Farook M, Widjaja D, Lee J, Tan DTH. Prevalence rates of refractive errors in Sumatra, Indonesia. Invest Ophthalmol Vis Sci. 2002;43(10):3174–3180. [PubMed] [Google Scholar]
- 14.Rim TH, Kim SH, Lim KH, Choi M, Kim HY, Baek SH, Epidemiologic Survey Committee of the Korean Ophthalmological Society Refractive errors in koreans: the Korea national health and nutrition examination survey 2008-2012. Korean J Ophthalmol. 2016;30(3):214–224. doi: 10.3341/kjo.2016.30.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Varma R, Torres M, McKean-Cowdin R, Rong F, Hsu C, Jiang XJ, Group CAES Prevalence and risk factors for refractive error in adult Chinese Americans: the Chinese American eye study. Am J Ophthalmol. 2017;175:201–212. doi: 10.1016/j.ajo.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohammadpour M, Heidari Z, Mohammad-Rabei H, et al. Correlation of higher order aberrations and components of astigmatism in myopic refractive surgery candidates. J Curr Ophthalmol. 2016;28(3):112–116. doi: 10.1016/j.joco.2016.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harvey EM. Development and treatment of astigmatism-related amblyopia. Optom Vis Sci. 2009;86(6):634–639. doi: 10.1097/OPX.0b013e3181a6165f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wills J, Gillett R, Eastwell E, Abraham R, Coffey K, Webber A, Wood J. Effect of simulated astigmatic refractive error on reading performance in the young. Optom Vis Sci. 2012;89(3):271–276. doi: 10.1097/OPX.0b013e3182429c6b. [DOI] [PubMed] [Google Scholar]
- 19.Harvey EM, Miller JM, Twelker JD, Davis AL. Reading fluency in school-aged children with bilateral astigmatism. Optom Vis Sci. 2016;93(2):118–125. doi: 10.1097/OPX.0000000000000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harvey EM, Miller JM, Apple HP, Parashar P, Twelker JD, Crescioni M, Davis AL, Leonard-Green TK, Campus I, Sherrill DL. Accommodation in astigmatic children during visual task performance. Invest Ophthalmol Vis Sci. 2014;55(8):5420–5430. doi: 10.1167/iovs.14-14400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chou YS, Tai MC, Chen PL, Lu DW, Chien KH. Impact of cylinder axis on the treatment for astigmatic amblyopia. Am J Ophthalmol. 2014;157(4):908–914.e1. doi: 10.1016/j.ajo.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 22.Leung TW, Li RWH, Kee CS. Blue-light filtering spectacle lenses: optical and clinical performances. PLoS One. 2017;12(1):e0169114. doi: 10.1371/journal.pone.0169114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh H, Singh H, Latief U, Tung GK, Shahtaghi NR, Sahajpal NS, Kaur I, Jain SK. Myopia, its prevalence, current therapeutic strategy and recent developments: a Review. Indian J Ophthalmol. 2022;70(8):2788–2799. doi: 10.4103/ijo.IJO_2415_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yao L, Zhang MH, Wang DQ, et al. Small incision lenticule extraction (SMILE) and laser in situ keratomileusis (LASIK) used to treat myopia and myopic astigmatism: a systematic review and meta-analysis of randomized clinical trials. Semin Ophthalmol. 2023;38(3):283–293. doi: 10.1080/08820538.2022.2107399. [DOI] [PubMed] [Google Scholar]
- 25.Goes S, Delbeke H. Posterior chamber toric implantable collamer lenses vs LASIK for myopia and astigmatism: systematic review. J Cataract Refract Surg. 2022;48(10):1204–1210. doi: 10.1097/j.jcrs.0000000000001007. [DOI] [PubMed] [Google Scholar]
- 26.Sigireddi RR, Weikert MP. How much astigmatism to treat in cataract surgery. Curr Opin Ophthalmol. 2020;31(1):10–14. doi: 10.1097/ICU.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 27.Goggin M. Toric intraocular lenses: evidence-based use. Clin Exp Ophthalmol. 2022;50(5):481–489. doi: 10.1111/ceo.14106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.González-Cruces T, Cano-Ortiz A, Sánchez-González MC, Sánchez-González JM. Cataract surgery astigmatism incisional management. Manual relaxing incision versus femtosecond laser-assisted arcuate keratotomy. A systematic review. Graefes Arch Clin Exp Ophthalmol. 2022;260(11):3437–3452. doi: 10.1007/s00417-022-05728-0. [DOI] [PubMed] [Google Scholar]
- 29.Yu XW, Wang JW, Lin XQ, Xu DJ, Ni S, Sheng ST, Xu W. Effect of two different preoperative calculation schemes on visual outcomes of patients after toric intraocular lens implantation. Int Ophthalmol. 2023;43(2):491–501. doi: 10.1007/s10792-022-02447-7. [DOI] [PubMed] [Google Scholar]
- 30.Song JX, Cao HZ, Chen X, et al. Small incision lenticule extraction (SMILE) versus laser assisted stromal in situ keratomileusis (LASIK) for astigmatism corrections: a systematic review and meta-analysis. Am J Ophthalmol. 2023;247:181–199. doi: 10.1016/j.ajo.2022.11.013. [DOI] [PubMed] [Google Scholar]
- 31.Wolffsohn J, Hall L, Young G. Clinical comparison of optimum and large diameter soft contact lenses. Cont Lens Anterior Eye. 2018;41(5):405–411. doi: 10.1016/j.clae.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 32.Richdale K, Berntsen DA, Mack CJ, Merchea MM, Barr JT. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci. 2007;84(10):969–975. doi: 10.1097/OPX.0b013e318157c6dc. [DOI] [PubMed] [Google Scholar]
- 33.Edrington TB. Toric soft contact lenses: they're not hard to fit. Contact Lens Spec. 1999;(6):46–48. [Google Scholar]
- 34.Hewett L. Contact lenses and astigmatism. Clin Exp Optom. 1962;45:202–205. [Google Scholar]
- 35.Young G, Hunt C, Covey M. Clinical evaluation of factors influencing toric soft contact lens fit. Optom Vis Sci. 2002;79(1):11–19. doi: 10.1097/00006324-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Maldonado-Codina C, Navascues Cornago M, Read ML, Plowright AJ, Vega J, Orsborn GN, Morgan PB. The association of comfort and vision in soft toric contact lens wear. Cont Lens Anterior Eye. 2021;44(4):101387. doi: 10.1016/j.clae.2020.11.007. [DOI] [PubMed] [Google Scholar]
- 37.Logan AK M, Datta A, Skidmore K, Tomiyama ES, Hu C, Chandler MA, Procopio B, Bhadane M, Benoit JS, Ritchey ER, Wolffsohn JS, Richdale K. Randomized clinical trial of near visual performance with digital devices using spherical and toric contact lenses. Optom Vis Sci. 2020;97(7):518–525. doi: 10.1097/OPX.0000000000001540. [DOI] [PubMed] [Google Scholar]
- 38.Chaudhry M, Sah SP, Sharma IP, Mondal S. Does offering only the spherical contact lens trial to the low astigmats mislead the practitioners? Int J Ophthalmol. 2021;14(8):1281–1284. doi: 10.18240/ijo.2021.08.21. [DOI] [PMC free article] [PubMed] [Google Scholar]