Abstract
Objective
This study aimed to determine the magnitude of occupational exposure to sharp injuries and identify its associated factors among nurses.
Design
Institution-based cross-sectional study design was conducted from 1 to 30 November 2022.
Analysis
The collected data were entered into EpiData V.4.2; then, exported to Stata V.14 for analysis. Variables with a p value of <0.05 at 95% CI were considered significantly associated with occupational exposure to sharp injuries.
Setting
The study was conducted in South Gondar zone public hospitals.
Participants
Nurses working in South Gondar zone public hospitals.
Results
Of the total respondents, 213 (56.65%) were between the ages of 25 and 34 with the mean±SD of age 30.22±6.63 years. Similarly, 202 (53.72%) of the respondents were women. This study finding showed that the magnitude of occupational exposure to sharp injuries among nurses was 52.39% (95% CI: 47.92% to 56.37%). Moreover, this study finding showed that year of service >10 years (adjusted OR (AOR)=2.35, 95% CI: 1.21 to 4.57), lack of infection prevention training (AOR=1.85, 95% CI: 1.09 to 3.45), job-related stress (AOR=2.24, 95% CI: 1.27 to 3.89) and presence of contaminated sharps at the workplace (AOR=2.76, 95% CI: 1.67 to 4.72) were significantly associated with occupational exposure to sharp injuries among nurses.
Conclusions
Generally, this study finding reported that the magnitude of occupational exposure to sharp injuries among nurses was high. This study finding also showed that years of service >10 years, lack of infection prevention training, job-related stress and the presence of contaminated sharps at the workplace were independent predictors of occupational exposure to sharp injuries among nurses. Hence, all the concerned bodies should strengthen regular provision of infection prevention training to nurses at all levels. Nurses should practice proper use of safety box more than ever in order to avoid the presence of contaminated needles and other sharp materials at the workplace.
Keywords: Risk management, infectious diseases, Infection control, Safety
Strengths and limitations of this study.
The findings could be strong evidence as a result of using census method.
The study might be subjected to recall and social desirability biases.
The study also might not show cause and effect relationships.
Background
A sharp injury is ‘an accidental penetrating wound with an instrument that is potentially contaminated with the body fluid of another person’.1–10 Sharp injuries occur when healthcare providers perform their clinical activities in the healthcare facilities, such as hospitals, health centres and clinics.3 The majority of sharp injuries occur during administering injections, securing intravenous lines, drawing blood, checking blood sugar, recapping needles, poor handling and disposing of needles and transferring blood or body fluids from a syringe to a specimen container.3 4
Globally, of the total of 35 million healthcare providers, it is estimated that 3 million experience sharp injuries every year; of these, nurses are at the greatest risk, with up to 50% of all sharp injuries being sustained by nurses.11 12 Because nurses have the highest rate of encountering sharp injuries among healthcare providers due to their prolonged exposure to needles and other sharp devices.13 Most of these sharp injuries (90%) occur in developing countries, where the burden of blood borne infections in the general population is high and access to safety devices and personal protective equipments (PPEs) is limited, specifically more common in sub-Saharan African countries.14
On average, healthcare providers in Africa suffer two to four sharp injuries every year.15 In sub-Saharan Africa, the magnitude of sharp injuries and their associated factors are not clearly understood among healthcare providers.16 A study conducted in Jimma University Specialized Teaching Hospital, Ethiopia reported that the magnitude of occupational exposure to sharp injuries among nurses was 61.76%.3 Sharp injuries are markedly the most common and preventable occupational hazards that healthcare providers are exposed to and become high risk for the transmission of a variety of blood borne infections, such as hepatitis B virus, hepatitis C virus and HIV (AIDS).17 18
Blood-borne infections following sharp injuries have serious consequences, including long-term illness, psychological stress to the victims, colleagues and family, disability and death.19 In addition to the potential risks for infectious diseases, they also suffer for direct costs required for laboratory tests, including tests for HIV antibodies, hepatitis B serology and a baseline test for hepatitis C as well as any treatments for these infections.20 The implementation of education, universal precautions, elimination of needle recapping and use of sharp containers for safe disposal have reduced the chance of getting sharp injuries by 80%.6 21
Healthcare providers who followed universal precautions were 66% less likely to have needle sticks and sharp injuries than those who did not follow.22 Training of handling objects, using instruments to grasp needles, reduction of the use of sharp devices, avoiding hand-to-hand passing of sharp instruments, decreasing of direct contact with needles, an appropriate disposal and using safety boxes properly can decrease the risk of getting sharp injuries.23
In Ethiopia, where primary healthcare services are covered by nurses, it is important to develop their knowledge and practice on universal precautions since the risks of getting infections following sharp injuries are high in their day-to-day activities.4 However, there is limited information in the study area that describes the magnitude of sharp injuries and its predictors among nurses. Therefore, this study aimed to determine the magnitude of occupational exposure to sharp injuries and identify its associated factors.
General objective
To assess the magnitude of occupational exposure to sharp injuries among nurses working in South Gondar zone public hospitals, Northcentral Ethiopia from 01 to 30 November 2022.
Specific objectives
To determine the magnitude of occupational exposure to sharp injuries among nurses working in South Gondar zone public hospitals, Northcentral Ethiopia from 1 to 30 November 2022.
To identify the predictors of occupational exposure to sharp injuries among nurses working in South Gondar zone public hospitals, Northcentral Ethiopia from 1 to 30 November 2022.
Methods
Study design, area and period
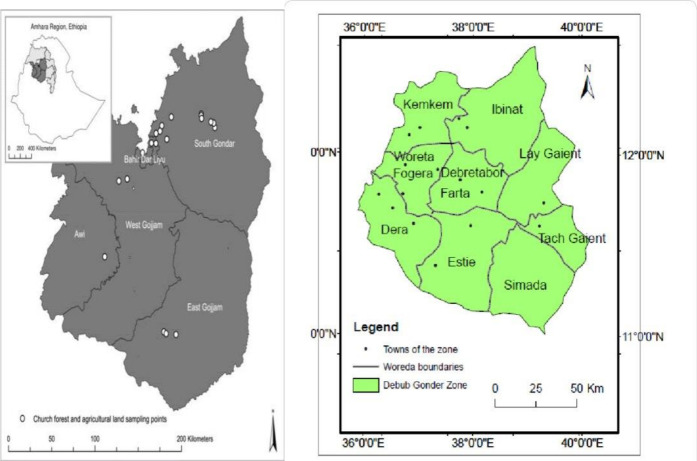
Institution-based cross-sectional study design was conducted among nurses working in South Gondar zone public hospitals from 1 to 30 November 2022. South Gondar is one of the zonal administrations in Amhara region, Northern Ethiopia with an estimated area of 14 095.19 square kilometres. It is located by South and North Wollo zones in the East, Bahirdar Liyu zone and Lake Tana in the West, Central Gondar in the North, Waghimra zone in the Northeast and East and West Gojjam zones in the South (figure 1). There are 10 public hospitals in the zone, namely Debre Tabor comprehensive specialised hospital, Addis Zemen, Ebnat, Mekane-Eyesus, Andabet, Wogeda, Woreta, Nefas Mewucha, Dr Ambachew Makonnen and Migbaru Kebede primary hospitals.
Figure 1.
Map of South Gondar zone (Source; Ethio GIS, 1994).
Source population
All nurses working in all South Gondar zone public hospitals.
Study population
All nurses working in all South Gondar zone public hospitals.
Inclusion and exclusion criteria
All nurses working in all South Gondar zone public hospitals at the time of the data collection period were included in the study; whereas nurses who were on sick leave, maternity leave, annual leave and training at the time of data collection period were excluded from the study.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of the research.
Sample size determination
The sample size (n) was calculated by computer-based Epi Info 7 software using a single population proportion at 95% CI, with a 5% margin of error, and by assuming the burden of occupational exposure to sharp injuries among nurses to be 61.76%.3
Where: n=the minimum sample size required for the study
Z=standard normal distribution (Z=1.96) with a 95% CI
P=burden of occupational exposure to sharp injuries among nurses (61.76%=0.6176)
d=is a tolerable margin of error (d=5%=0.05)
n=363. Then, by adding a 10% (0.1) non-response rate, the final sample size (n) was calculated to be 400. But, since it was the minimum sample size required, and the source population was only 402, the source population (402) was taken as a sample size for this study (census method was used).
Dependent variable
Occupational exposure to sharp injuries.
Independent variables
Socio-demographic characteristics
Age, sex, marital status, level of education and years of service.
Behavioural characteristics
Sleeping disturbance, following of standard precaution guideline, use of PPE, knowledge of standard precautions and job-related stress.
Work environment characteristics
Length of stay/shift, health and safety information access, infection prevention training, work load, availability of safety box, availability of standard precaution guidelines and presence of contaminated sharps.
Operational definitions
Occupational exposure to sharp injuries
Any kind of needle stick and/or other sharp injury which occurred among nurses in relation to his/her job in the healthcare facility.4
Knowledge
Nurses who have scored ≥75% (9) of 12 knowledge-related questions were considered to have adequate knowledge; whereas nurses who have scored below 75% were also considered to have inadequate knowledge towards sharp injuries.24
Job-related stress
Nurses who scored above or equal to the mean score (32.78) of the Likert-scale questions that used to assess nurses’ job-related stress were considered they have a job-related stress, whereas nurses who scored below the mean score were also considered they did not have job-related stress.25
Workload
When one trained intensive care unit (ICU) nurse provides nursing care services for more than two patients in the ICU, and when one nurse provides nursing care services for more than six patients in inpatient departments per shift.25
Sleeping disturbance
The presence of sleeping problems while the healthcare provider is at the workplace.25
Data collection tool and procedure
A structured and pretested self-administered English version questionnaire was used to collect the data. The questionnaire was prepared by reviewing different literatures,3 4 25 and using standardised Expanded Nursing Stress Scale Likert-scale questions to assess job-related stress of the respondents.3 4 25
The questionnaire contains nurses’ socio-demographic, behavioural, environmental characteristics, knowledge questions related to standard precaution and standardised Likert-scale questions to assess job-related stress of the respondents. Reliability of the tool was established with an overall Cronbach’s alpha score (0.74 for knowledge questions related to standard precaution, and 0.79 for job-related stress Likert-scale questions). Training was given to the data collectors, and before giving the questionnaire, the data collectors informed the nurses about the aims/purposes, risks and possible benefits of the study, the right and refusal to participate in the study and that the collected information would be kept confidential.
After all, those nurses who were willing and have signed the informed voluntary consent form were requested to fill out the questionnaire. The data collection was held for four consecutive weeks (from 1 to 30 November 2022).
Data quality control
Five per cent of the questionnaire was pre-tested from 23 to 27 October 2022 in Koladiba primary hospital to assess the reliability, clarity, consistency, understandability and the total time that it would take to complete the questionnaire prior to the actual data collection. Then, the necessary comments and feedback were incorporated in the final tool to improve its quality. Training was given for the data collectors regarding the objective of the study, data collection tool, ways of data collection, checking the completeness of the collected data and how to maintain confidentiality.
The collected data were checked for completeness, cleaned, edited, coded manually and entered into EpiData V.4.2. Double data entry was done for its validity, and compared with the original data. Outliers were checked, and simple frequencies and cross tabulation were done for missing values and variables.
Data processing and analysis
Then after, the data were exported to Stata V.14 for analysis. Descriptive analysis was done by computing proportions and summary statistics. The information was presented using simple frequencies, summary measures, tables and figures. Binary logistic regression was used to identify the associated factors of occupational exposure to sharp injuries. Bivariate and multivariate analyses were used to see the association between the outcome variable, and each independent variable. The assumptions for binary logistic regression were checked. The goodness of fit was tested by Hosmer-Lemeshow statistics and Omnibus tests.
All variables with p<0.2 in the bivariate analysis were included in the final multivariable analysis model in order to control all the possible confounders, and the variables were selected using enter method. The adjusted OR (AOR) along with a 95% CI was estimated to identify the associated factors of occupational exposure to sharp injuries. In this study, variables with a p value of <0.05 were considered significantly associated with occupational exposure to sharp injuries.
Results
Of the total of 402 respondents, 376 were included in the final analysis, giving a response rate of 93.53%.
Socio-demographic and working environment-related attributes
Of the total respondents, 213 (56.65%) were between the ages of 25 and 34 with the mean±SD of age 30.22±6.63 years. Similarly, 202 (53.72%) of the respondents were women. Additionally, only 89 (23.67%) of the respondents got infection prevention training. Moreover, 271 (72.07%) of them had safety boxes at the workplace to dispose of needles and other sharp materials after use, and 214 (56.91%) of respondents also stated that there were contaminated needles and sharp materials at the workplace (table 1).
Table 1.
Socio-demographic characteristics of the respondents working in South Gondar zone public hospitals, Northcentral Ethiopia, 2022 (n=376)
| Variables | Category | Frequency | Percentage (%) |
| Age | ≤24 | 68 | 18.09 |
| 25–34 | 213 | 56.65 | |
| 35–44 | 71 | 18.88 | |
| ≥45 | 24 | 6.38 | |
| Sex | Male | 174 | 46.28 |
| Female | 202 | 53.72 | |
| Marital status | Single | 171 | 45.48 |
| Married | 183 | 48.67 | |
| Divorced | 17 | 4.52 | |
| Widowed | 5 | 1.33 | |
| Educational level | Diploma | 132 | 35.11 |
| BSc | 244 | 64.89 | |
| Years of service | <5 | 136 | 36.17 |
| 5–10 | 128 | 34.04 | |
| >10 | 112 | 29.79 | |
| Sleeping disturbance problem | Yes | 274 | 72.87 |
| No | 102 | 27.13 | |
| Use of PPEs | All of the time | 185 | 49.20 |
| Most of the time | 102 | 27.13 | |
| Sometimes | 73 | 19.41 | |
| Never use | 16 | 4.26 | |
| Workload in the unit | Yes | 212 | 56.38 |
| No | 164 | 43.62 | |
| Length of stay/shift at work | ≤8 hours | 193 | 51.33 |
| 9–14 hours | 35 | 9.31 | |
| ≥15 hours | 148 | 39.36 | |
| Health and safety information access | Yes | 291 | 77.39 |
| No | 85 | 22.61 | |
| Training on IP | Yes | 89 | 23.67 |
| No | 287 | 76.33 | |
| Availability of safety box at workplace | Yes | 271 | 72.07 |
| No | 105 | 27.93 | |
| Availability of universal precaution guideline | Yes | 212 | 56.38 |
| No | 164 | 43.62 | |
| Following universal precaution guideline | Yes | 93 | 43.87 |
| No | 119 | 56.13 | |
| Presence of contaminated sharps at workplace | Yes | 214 | 56.91 |
| No | 162 | 43.09 | |
| Knowledge of standard precaution | Adequate knowledge | 134 | 35.64 |
| Inadequate knowledge | 242 | 64.36 | |
| Job-related stress | Stressed | 237 | 63.03 |
| Not stressed | 139 | 36.97 |
BSc, Bachelor of Science; IP, infection prevention; PPEs, personal protective equipments.
Magnitude of occupational exposure to sharp injuries
This study finding showed that the magnitude of occupational exposure to sharp injuries among nurses was 52.39% (95% CI: 47.92% to 56.37%) (197).
The occurrence of occupational exposure to sharp injuries was the highest among respondents with the age of 45 years and above (62.50). Likewise, the majority of men, 108 (62.07) also got occupational exposure to sharp injuries. Occupational exposure to sharp injuries was also the highest among diploma nurses, and nurses having more than 10 years of service (59.85% and 62.50%), respectively. Moreover, the occurrence of sharp injuries was also the highest among nurses working along with the presence of contaminated sharps at workplace (63.55%) (table 2).
Table 2.
Distribution of sharp injuries among nurses working in South Gondar zone public hospitals, Northcentral Ethiopia, 2022 (n=376)
| Variables | Categories | Occupational exposure to sharp injuries | |
| Yes (%) | No (%) | ||
| Age | ≤24 | 32 (47.06) | 36 (52.94) |
| 25–34 | 111 (52.11) | 102 (47.89) | |
| 35–44 | 39 (54.93) | 32 (45.07) | |
| ≥45 | 15 (62.50) | 9 (37.50) | |
| Sex | Male | 108 (62.07) | 66 (37.93) |
| Female | 89 (44.06) | 113 (55.94) | |
| Marital status | Single | 87 (50.88) | 84 (49.12) |
| Married | 96 (52.46) | 87 (47.54) | |
| Divorced | 11 (64.71) | 6 (32.29) | |
| Widowed | 3 (60.0) | 2 (40.0) | |
| Educational level | Diploma | 79 (59.85) | 53 (40.15) |
| BSc | 118 (48.36) | 126 (51.64) | |
| Year of service | <5 | 59 (43.38) | 77 (56.62) |
| 5–10 | 68 (53.13) | 60 (46.87) | |
| >10 | 70 (62.50) | 42 (37.50) | |
| Sleeping disturbance problem | Yes | 141 (51.46) | 133 (48.54) |
| No | 56 (54.90) | 46 (45.10) | |
| Use of PPEs | All of the time | 89 (48.11) | 96 (51.89) |
| Most of the time | 56 (54.90) | 46 (45.10) | |
| Sometimes | 41 (56.16) | 32 (43.84) | |
| Never use | 11 (58.75) | 5 (31.25) | |
| Workload | Yes | 125 (58.96) | 87 (41.04) |
| No | 72 (43.90) | 92 (56.10) | |
| Length of stay/shift at work | ≤8 hours | 95 (49.22) | 98 (50.78) |
| 9–14 hours | 19 (54.29) | 16 (45.71) | |
| ≥15 hours | 83 (56.08) | 65 (43.92) | |
| Health and safety information access | Yes | 148 (50.86) | 143 (49.14) |
| No | 49 (57.65) | 36 (42.35) | |
| Training on IP | Yes | 38 (42.70) | 51 (57.30) |
| No | 159 (55.40) | 128 (44.60) | |
| Availability of safety box | Yes | 129 (47.60) | 142 (52.40) |
| No | 68 (64.76) | 37 (35.24) | |
| Availability of universal precaution guideline | Yes | 99 (46.70) | 113 (53.30) |
| No | 98 (59.76) | 66 (40.24) | |
| Following universal precaution guideline | Yes | 42 (45.16) | 51 (54.84) |
| No | 155 (54.77) | 128 (45.23) | |
| Presence of contaminated sharps at workplace | Yes | 136 (63.55) | 78 (36.45) |
| No | 61 (37.65) | 101 (62.35) | |
| Knowledge of standard precaution | Adequate knowledge | 59 (44.03) | 75 (55.97) |
| Inadequate knowledge | 138 (57.02) | 104 (42.98) | |
| Job-related stress | Stressed | 149 (62.87) | 88 (37.13) |
| Not stressed | 48 (34.53) | 91 (65.47) | |
BSc, Bachelor of Science; IP, infection prevention; PPEs, personal protective equipments.
Occupational exposure to sharp injuries-related attributes
Of the respondents who encountered occupational exposure to sharp injuries, 114 (57.87%) had encountered sharp injuries one to two times. Additionally, 69 (35.03%) of injuries occurred during abrupt movement of patients, and 86 (43.65%) sharp injuries were slight skin penetration. Moreover, 93 (47.21%) of injuries were from unknown status, and only 92 (46.70%) sharp injuries were reported to the concerned body (table 3).
Table 3.
Occupational exposure to sharp injuries-related attributes among nurses working in South Gondar zone public hospitals, Northcentral Ethiopia, 2022 (n=376)
| Variables | Values | Frequency | Percentage (%) |
| Frequency of injuries occurred | 1–2 times | 114 | 57.87 |
| 3–4 times | 71 | 36.04 | |
| ≥5 times | 12 | 6.09 | |
| Condition of sharps | Dirty needles/sharps | 74 | 37.56 |
| Sterile needles/sharps | 58 | 29.45 | |
| Both dirty and sterile needles/sharps | 65 | 32.99 | |
| How sustaining injuries | During abrupt movement of patients | 69 | 35.03 |
| During recapping needle after use | 63 | 31.98 | |
| During sharp collection | 46 | 23.35 | |
| Others | 19 | 9.64 | |
| Type of injuries sustained | Deep injury | 54 | 27.41 |
| Slight skin penetration | 86 | 43.65 | |
| Superficial injury | 57 | 28.94 | |
| Health status of the source patients | Known HIV/AIDS positive | 37 | 18.78 |
| Clinically suspected HIV/AIDS | 40 | 20.30 | |
| Clinically diagnosed patient with hepatitis B | 27 | 13.17 | |
| Unknown status | 93 | 47.21 | |
| Report of the injuries | Yes | 92 | 46.70 |
| No | 105 | 53.30 |
Distribution of sharp injuries by their type
The types of sharps that cause injuries to nurses were intravenous needles, 64 (32.49%), intramuscular needles, 42 (21.32%), suturing needles, 36 (18.27%), lancets, 29 (14.72%), surgical blades, 17 (8.63%) and scalpels, 9 (4.57%).
Factors associated with occupational exposure to sharp injuries
Nurses having above 10 years of service were 2.35 times more likely to encounter occupational exposure to sharp injuries than nurses having less than 5 years of service (AOR=2.35, 95% CI: 1.21 to 4.57). On the other hand, nurses who did not get infection prevention training were 1.85 times more likely to encounter occupational exposure to sharp injuries (AOR=1.85, 95% CI: 1.09 to 3.45). Additionally, nurses having job-related stress were also 2.24 times more likely to be exposed for sharp injuries (AOR=2.24, 95% CI: 1.27 to 3.89), and nurses who were working in the area with the presence of contaminated sharps were 2.76 times more likely to get the chance of occupational exposure to sharp injuries (AOR=2.76, 95% CI: 1.67 to 4.72) (table 4).
Table 4.
Showing the association between independent variables with occupational exposure to sharp injuries among nurses working in South Gondar zone public hospitals, Northcentral Ethiopia, 2022 (n=376)
| Variables | Categories | Sharp injuries | COR (95% CI) | AOR (95% CI) | |
| Yes (%) | No (%) | ||||
| Sex | Male | 108 (54.82) | 66 (36.87) | 2.15 (1.32 to 3.07) | 1.98 (0.91 to 4.21) |
| Female | 89 (45.18) | 113 (63.13) | 1.00 | 1.00 | |
| Year of service | <5 | 59 (29.95) | 77 (43.02) | 1.00 | 1.00 |
| 5–10 | 68 (34.52) | 60 (33.52) | 1.46 (0.87 to 2.42) | 1.38 (0.72 to 2.64) | |
| >10 | 70 (35.53) | 42 (23.46) | 2.12 (1.26 to 3.49) | 2.35 (1.21 to 4.57) *** | |
| Workload in the unit | Yes | 125 (63.45) | 87 (48.60) | 1.73 (1.15 to 2.52) | 1.42 (0.83 to 2.45) |
| No | 72 (36.55) | 92 (51.40) | 1.00 | 1.00 | |
| Training | Yes | 38 (19.29) | 51 (28.49) | 1.00 | 1.00 |
| No | 159 (80.71) | 128 (71.51) | 2.08 (1.49 to 3.13) | 1.85 (1.09 to 3.45) **** | |
| Nurses’ knowledge of standard precaution | Adequate knowledge | 59 (29.95) | 75 (41.90) | 1.00 | 1.00 |
| Inadequate knowledge | 138 (70.05) | 104 (58.10) | 1.96 (1.31 to 2.94) | 1.42 (0.79 to 2.39) | |
| Nurses’ job stress level | Stressed | 149 (75.63) | 88 (49.16) | 2.45 (1.62 to 3.67) | 2.24 (1.27 to 3.89) ** |
| Not stressed | 48 (24.37) | 91 (50.84) | 1.00 | 1.00 | |
| Presence of contaminated sharps | Yes | 136 (69.04) | 78 (43.58) | 2.71 (1.79 to 4.09) | 2.76 (1.67 to 4.72) |
| No | 61 (30.96) | 101 (56.42) | 1.00 | 1.00 | |
*Significant at p=0.000, **significant at p=0.005, ***significant at p=0.011 and ****significant at p=0.018.
AOR, adjusted OR; COR, Crude Odd Ratio.
Discussion
This study finding showed that the magnitude of occupational exposure to sharp injuries among nurses was 52.39%. This study finding also reported that years of service >10 years, lack of infection prevention training, job-related stress and the presence of contaminated sharps at the workplace were significantly associated with the occurrence of occupational exposure to sharp injuries among nurses.
In this study, the magnitude of occupational exposure to sharp injuries among nurses was 52.39%. This finding was higher than a study conducted in three hospitals, Izmir, Turkey (44.3%),18 but lower than studies conducted in Public Sector Tertiary Care Hospitals of Pakistan (67%),26 and JUSH, Southwest Ethiopia (61.76%).3 This variation might be due to the difference in study setting and period, as well as due to the difference in infection prevention training and knowledge level of the respondents towards standard precaution across study settings.
In this study, year of service >10 years was significantly associated with the occurrence of occupational exposure to sharp injuries among nurses at p<0.05. This finding was similar with studies conducted in three hospitals, Izmir, Turkey18 and a secondary care hospital, Gaza Strip,27 which showed that year of service had shown significant association with the occurrence of occupational exposure to sharp injuries among nurses at p<0.05. It might be due to the fact that as years of service increases, the chance of getting occupational exposure to sharp injuries also increases.
This study finding also indicated that nurses who did not get infection prevention training were 1.85 times more likely to get the chance of occupational exposure to sharp injuries compared with nurses who got the training. This finding was in line with a study conducted in public hospitals of Jimma Zone, Southwest Ethiopia,4 which showed that nurses who did not get infection prevention training were 8.33 times more likely to get the chance of occupational exposure to sharp injuries compared with nurses who got the training. It is due to the fact that getting infection prevention training helps to understand and practice the standard precaution guideline easily, which in turn reduces the chance of getting occupational exposure to sharp injuries.
Similarly, this study finding also showed that job-related stress was significantly associated with the occurrence of occupational exposure to sharp injuries among nurses. This finding was comparable with a study conducted in JUSH, Southwest Ethiopia which reported that job-related stress had shown significant association with the occurrence of occupational exposure to sharp injuries among nurses.14 It could be explained that job-related stress might make nurses lose their concentration and practice their daily activities unsafely.
Moreover, this study finding also showed that the presence of contaminated needles and sharp materials at the workplace was also significantly associated with the occurrence of occupational exposure to sharp injuries among nurses at p<0.05. This finding was congruent with a study conducted in JUSH, Southwest Ethiopia which reported that the presence of contaminated needles and sharp materials at the workplace was significantly associated with the occurrence of occupational exposure to sharp injuries among nurses at p<0.05.3 The presence of contaminated needles and sharp materials at the workplace increases the chance of getting occupational exposure to sharp injuries among nurses in their day-to-day workplace activities.
Strengths and limitations of this study
The study used a census method, as a result, the findings could be strong evidence for the problem. However, the study might be subjected to recall and social desirability biases. The study also might not show cause and effect relationships while the study design was cross-sectional.
Conclusions
Generally, this study finding reported that the magnitude of occupational exposure to sharp injuries among nurses was high. Moreover, this study finding also showed that years of service >10 years, lack of infection prevention training, job-related stress and the presence of contaminated sharps at the workplace were independent predictors of occupational exposure to sharp injuries among nurses.
Prevention and control strategies
Continually educate the healthcare team: To achieve the desired infection prevention and control goals, training on infection prevention and control should be given to the staff on a continual basis covering the standard infection prevention and control precautions.
Conducting regular clinical audits: It used to ensure best practice of the standard infection prevention and control precautions such as proper use of PPE, disposal of used needles and other sharps and hand hygiene.
Creating a cleanliness culture: By building a clean culture, staff are aware of the benefits of infection prevention and control.
Recommendations
All the concerned bodies should strengthen regular provision of infection prevention training to the nurses at all levels. Stakeholders, including nursing staff, should also strengthen their efforts to work together to identify and manage the possible job-related stressors among nurses. Furthermore, safety boxes should be available in each working unit, and nurses should also practice proper use of safety box more than ever in order to avoid the presence of contaminated needles and other sharp materials at the workplace.
Supplementary Material
Acknowledgments
First and foremost, we would like to extend our deepest gratitude to Debre Tabor University, college of health science, for giving us the opportunity to conduct this study. Second, we would like to thank hospital administrators for their permission and unlimited support. Lastly, we also give our heartfelt thanks to all nurses who have participated in this study.
Footnotes
Twitter: @yes
Contributors: TMA conceptualised the study and was involved in the design, analysis, interpretation, report and manuscript writing. TMA and YTK made a substantial contribution to the conception, analysis and interpretation of data. SDK contributes to critical revision of the manuscript. TM is responsible for the overall content as the guarantor. All the authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographical or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical clearance was obtained from Debre Tabor University, College of Health Sciences, ethical review board (Ref No.CHS/048/2022). Participants gave informed consent to participate in the study before taking part.
References
- 1.Adola SG. The status of sharp injury and risk factors among health care staffs in the Bule Hora hospital, South Ethiopia, 2020. SCRI 2022;5:13–20. 10.33140/SCRI.05.01.03 [DOI] [Google Scholar]
- 2.Bazie GW. Factors associated with needle stick and sharp injuries among Healthcare workers in North East Ethiopia. Risk Manag Healthc Policy 2020;13:2449–56. 10.2147/RMHP.S284049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beker J, Bamlie T. Needle stick and sharp injuries and associated factors among nurses working in Jimma University specialized hospital, South West Ethiopia. J Nurs Care 2015:2167–1168. [Google Scholar]
- 4.Bidira K, Woldie M, Nemera G. Prevalence and predictors of Needlestick injury among nurses in public hospitals of Jimma zone, South West Ethiopia. Int J Nurs Midwifery 2014:90–6. [Google Scholar]
- 5.Getie A, Wondmieneh A, Tesfaw G. The prevalence of Needlesticks and sharp injuries, and the associated factors among midwives and nurses in North Wollo zone public hospitals, North East Ethiopia: an institution-based cross-sectional study. Drug Healthc Patient Saf 2020;12:187–93. 10.2147/DHPS.S273669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yesuf JH, Bayou NB, Agde ZD. n.d. Magnitude of needle stick and sharp injuries and associated factors among health care workers in Werabe comprehensive specialized hospital, Southwest Ethiopia: A cross-sectional study. medRxiv;2022:2022–11. [Google Scholar]
- 7.Legesse WT, Anemaw W, Mekonen T, et al. Prevalence of needle sticks injury and its associated factors among health care workers in Bahir Dar city health centers, Northwest Ethiopia. Int j Infect Control 2015;11. 10.3396/IJIC.v11i2.014.15 [DOI] [Google Scholar]
- 8.Liyew B, Sultan M, Michael M, et al. Magnitude and determinants of Needlestick and sharp injuries among nurses working in Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. Biomed Res Int 2020;2020:6295841. 10.1155/2020/6295841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mekonnen R, Yosef H, Teklegiorgis K, et al. Magnitude and impact of occupational related needle stick and sharp injuries and associated factors among health care workers in dire Dawa, Eastern Ethiopia. Med Saf Glob Health 2018;07:2574–0407. 10.4172/2574-0407.1000141 [DOI] [Google Scholar]
- 10.Sharew NT, Mulu GB, Habtewold TD, et al. Occupational exposure to Sharps injury among Healthcare providers in Ethiopia regional hospitals. Ann Occup Environ Med 2017;29:7.:7. 10.1186/s40557-017-0163-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gebremariyam BS. Determinants of occupational exposure to blood and body fluids, Healthcare workers’ risk perceptions and standard precautionary practices: a hospital-based study in Addis Ababa, Ethiopia. Ethiopian Journal of Health Development 2019;33. [Google Scholar]
- 12.Tadesse M, Meskele M, Boltena AT. Needle-stick and Sharps injuries among health care workers in Wolaita zone, Southern Ethiopia. Med Safe Glo Heal 2016;05:1–7. 10.4172/2574-0407.1000130 [DOI] [Google Scholar]
- 13.Manzoor I, Daud S, Hashmi NR, et al. Needle stick injuries in nurses at a tertiary health care facility. J Ayub Med Coll Abbottabad 2010;22:174–8. [PubMed] [Google Scholar]
- 14.Sahiledengle B, Tekalegn Y, Woldeyohannes D, et al. Occupational exposures to blood and body fluids among Healthcare workers in Ethiopia: a systematic review and meta-analysis. Environ Health Prev Med 2020;25:58. 10.1186/s12199-020-00897-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mbaisi EM, Ng’ang’a Z, Wanzala P, et al. Prevalence and factors associated with percutaneous injuries and splash exposures among health-care workers in a provincial hospital. Pan Afr Med J 2010;14. 10.11604/pamj.2013.14.10.1373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Isara AR, Oguzie KE, Okpogoro OE. Prevalence of Needlestick injuries among Healthcare workers in the accident and emergency Department of a teaching hospital in Nigeria. Ann Med Health Sci Res 2015;5:392–6. 10.4103/2141-9248.177973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jahangiri M, Rostamabadi A, Hoboubi N, et al. Needle stick injuries and their related safety measures among nurses in a University hospital. Safety and Health at Work 2016;7:72–7. 10.1016/j.shaw.2015.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akyol AD. Needle stick and sharp injuries among nurses. Glob J Nurs Forensic Stud 2016;01:109. 10.4172/2572-0899.1000109 [DOI] [Google Scholar]
- 19.Markovic-Denic L, Maksimovic N, Marusic V, et al. Occupational exposure to blood and body fluids among health-care workers in Serbia. Med Princ Pract 2015;24:36–41. 10.1159/000368234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho E, Lee H, Choi M, et al. Factors associated with Needlestick and sharp injuries among hospital nurses: a cross-sectional questionnaire survey. Int J Nurs Stud 2013;50:1025–32. 10.1016/j.ijnurstu.2012.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lemessa D, Solomon T. Occupational exposure of health care workers to blood and body fluids in West Shewa zone, Oromia, Ethiopia, 2018: A cross-sectional study. J Environ Public Health 2021;2021:2944158. 10.1155/2021/2944158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bekele T, Gebremariam A, Kaso M, et al. Factors associated with occupational needle stick and Sharps injuries among hospital Healthcare workers in bale zone, Southeast Ethiopia. PLoS One 2015;10:e0140382. 10.1371/journal.pone.0140382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geravandi S, Alavi SM, Yari AR, et al. Epidemiological aspects of needle stick injuries among health care workers in Razi hospital Ahvaz, Iran, in 2015. Archives of Hygiene Sciences 2016. [Google Scholar]
- 24.Tebeje B, Hailu C. Assessment of HIV post-exposure prophylaxis use among health workers of governmental health institutions in Jimma zone, Oromiya region, Southwest Ethiopia. Ethiop J Health Sci 2010;20:55–64. 10.4314/ejhs.v20i1.69429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aderaw Z. Assessment on magnitude of needle stick and sharp injuries and associated factors among health care workers in East Gojjam zone health institutions, Amahara regional state, Ethiopia. Global Journal of Medical Research 2013;13:41–9. [Google Scholar]
- 26.Habib H, Khan EA, Aziz A. Prevalence and factors associated with needle stick injuries among registered nurses in public sector tertiary care hospitals of Pakistan. International Journal of Collaborative Research on Internal Medicine & Public Health 2011:124–30. [Google Scholar]
- 27.Elsous A, Ouda M, Mohsen S, et al. Needle stick injuries among nurses of secondary care hospital: A cross-sectional study from Gaza strip. Annals of International Medical and Dental Research 2016;2. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.