Abstract
Background
After the widespread of coronavirus disease (COVID-19) around the globe, it was imperative to establish preventative measures to restrict the virus's transmission. The purpose of this research was to present an overview of the awareness, knowledge, attitude, and abilities of Syrian physicians about telemedicine technology.
Methods
An online cross-sectional study was conducted from April 1 to May 15, 2022. The questionnaire was taken from published study, and the inclusion criteria consist the Syrian doctors who worked in hospitals during the COVID-19 pandemic, mainly those who had direct contact with patients.
Results
Among 385 responses, 52.72% of them were females, 83.9% of them were aged less than 30 years old, and 66% were working in the governmental sector; 66% of participants have moderate knowledge about using computers and the internet, 80% have heard about telemedicine. Despite that, 95.1% of participants have not attended any training workshop on telemedicine, and most of them have reported no availability of a telemedicine unit in their department. Only 31.7% participants have shown high awareness of telemedicine. Furthermore, no significant correlation was identified between the academic level with the age and telemedicine awareness, knowledge, attitude, or computer skills. Despite that, there was an obvious correlation between age and computer skills (P-value < 0.05). There was a significant correlation between the medical specialty and awareness, and computer abilities, especially the anesthesiology (88.5 ± 5.2), (84 ± 8.7), respectively. Spearman's rho test showed mild positive significant association in various subscales (awareness and experience, experience and skills, knowledge and attitude, knowledge and skills, and attitude and skills).
Conclusion
The study results demonstrate that most of the participating clinical doctors have a neutral view of telemedicine, even though they do not know much about it and do not have considerable experience with it. It is practical to educate and train academic staff, practicing physicians, residents and medical students within the clinical stages about telemedicine.
Keywords: Telemedicine, health intelligence, management and policy, public health
Background
Coronavirus disease (COVID-19), caused by coronavirus 2 (SARS-CoV-2), was declared a new pandemic by the World Health Organization (WHO) on March 11, 2020. 1 The first outbreak of the novel SARS-CoV-2 was reported in Wuhan, China, in December 2019. 2 According to WHO, until May 20, 2021 there were over 160 million confirmed cases and more than 3 million deaths. 3 Many preventive measures have decreased the risk of patients’ exposure to the COVID-19 infection. Education, isolation, prevention, control of transmission, and treatment of infected people are critical in controlling infectious diseases, especially COVID-19. 4 The following recommendations it is possible to reduce the spread of infection: staying at home and avoiding close communication with sick people; avoiding unnecessary travel; social separation such as avoiding busy public areas and keeping at least 2 meters between people, also, hands should be washed for at least 20 s with soap and water or with a hand sanitizer containing at least 60% alcohol after contacting joint surfaces, using the bathroom, or shaking hands.5, 6 In the context of COVID-19 pandemic, telemedicine, including video consultations, has been supported to limit the risk of infection transmission between the individuals. 7 This technique provides video teleconsultations from a patient's home because of technological advancements, cost reductions in telemedicine technologies, and the widespread availability of high-speed internet and smartphones. 8 Telemedicine services have evolved beyond phone assessment and digital visits, including mental health, post-surgical follow-up, and specialist consultations. 9 Also, WHO has recommended this method, because of its potential to decrease the transmission of COVID-19 among population. 10 During the COVID-19 crisis, the United States Health Systems were expanding their telemedicine services to support initiatives to socially separate medical care. 11 Telemedicine uses telecommunications technology to offer healthcare information and services. Telemedicine is considered a promising option for acute, chronic, and preventative care, especially with the advancement of internet services.12, 13 Healthcare providers employ telemedicine to aid their patients, protect their personnel, and save resources by limiting physical human interaction, providing healthcare remotely, and contacting patients at home.11, 14 However, clinical physicians who use telemedicine services should be evaluated for their awareness, knowledge, attitude, and competence. Several studies have recommended that telemedicine should be used in the healthcare system to improve efficiency, manage long wait times, and reduce the risk of illness development.15, 16 Syria's overall health spending is among the lowest in the area, and state healthcare institutions offer poor quality treatment and are inefficient. Syria's healthcare system has been seriously affected, and many doctors and healthcare professionals have departed the country throughout the war, increasing the demand on surviving healthcare institutions. The tele-ICU was established in Syria, where persistent conflict has put a strain on resources, utilizing affordable technology including webcams, cell phone cameras, and instant messaging via free social media programs. 17 Furthermore, COVID-19 has shown that Syria's health status is worsening and that it is vital to provide sufficient medical equipment and a large number of medical specialists.1 Due to the implementation of curfew rules, many Syrian clinical doctors were forced to conduct patient diagnosis and treatment by phone during COVID-19; however, there has been no previous study that assesses Syrian clinical doctors’ attitudes toward telemedicine and determines its benefits and disadvantages. The purpose of this research is to evaluate the Syrian doctors’ telemedicine awareness, knowledge, attitude, and abilities in light of their poor economic and educational status after 11 years of civil war.
Methods
Study design
This cross-sectional study was conducted in Syria from April 1 to May 15, 2022, where we sent an online questionnaire to Syrian doctors via social media apps and emails. We did not ask for any personal information in the responses (name, religion, and political attitude). Our target was Syrian doctors who worked in hospitals during the COVID-19 pandemic, especially those in direct contact with COVID-19 patients. Age, gender, years of experience, job status, department of work, and computer skills were all obtained in the first phase of the survey; also, many general telemedicine questions were asked. Four specific subsections were included in the second part of the questionnaire that had already been created by Zayapragassarazan et al. 18 To verify participants’ understanding of the questionnaire, it was translated into Arabic by language experts who were healthcare professionals and had great expertise in biomedical research and then retranslated to English for data analysis. Specific collaborators from many medical Syrian colleges (Data Collection Group) collected the data by disrupting the online survey, which was generated at the Google form website, on social media platforms such as WhatsApp, Telegram, and Facebook. Also, the data collection group was mentored by a supervisor who has access to the Google form website. To acquire the required data from the respondents, we employed convenience and snowball tactics. The research was open to all clinical doctors, and participation was completely optional, with personal data being stored in a secure database. We calculated the required sample size for this study by using the Calculator.net tool available at https://www.calculator.net/sample-size-calculator.html (population size (the number of the Syrian doctors according to the latest report from the Syrian Ministry of Health (http://calcuator.com/) (PS) = 282,141, the proportion of the population who are aware of colorectal cancer (PP) = 50%, confidence level (CL) = 95%, and the margin error (ME) = 5%). When the previous formula was used, the requested sample size was 264.The total number of participating clinical doctors was 389, 4 have declined to complete the survey, and the final sample size was 385.
Sample size calculation
Sample size = Z1-a/2 2 P(1 - P)/d2; 1.962 0.16 (1 - 0.16)/0.052 = 385
Z1-a/2 = In our study P value is considered significant under 0.05 so Z1-a/2, which equals 1.96
P = Predicted proportion in Indian population who have perceptive toward telemedicine as useful method during COVID-19; 50%
d = Absolute precision; 0.05
Measures
1. Sociodemographic variables
Respondents were requested to give details about their personal and professional backgrounds. Their name, age, sex, position, computer skills, and the subject (pre-clinical, para-clinical, and clinical) were all included in the data.
2. Measurement subscales
• Awareness subsection: This subsection included 12 telemedicine-related questions that were used to evaluate awareness. Each item was evaluated on a three-point scale ranging from 0 to 2 (0 = don’t know, 1 = heard of it, 2 = know about it). The total score might vary from a minimum of 0 to a maximum of 24.
• Knowledge subsection: This subsection consists of twelve questions that tested the physician's knowledge of telemedicine. Each item was evaluated on a two-point scale of 0 to 1 (0 = yes, 1 = no). The total score might vary from a minimum of 0 to a maximum of 11.
• Attitude subsection: This subsection included 11 questions intended to determine respondents’ attitudes toward telemedicine. Each question was evaluated on a 5-point Likert scale ranging from 0 to 4 (0 = strongly disagree, 1 = disagree, 2 = undecided, 3 = agree, 4 = strongly agree). The total score might vary from a minimum of 0 to a maximum of 44.
• Computer skills subsection: This subsection had 13 questions meant to assess the doctor's degree in computer and information technology knowledge. A 4-point scale with values ranging from 0 to 3 was used to evaluate each question (0 = unskilled, 1 = learner, 2 = mediocre, 3 = expert). The total score might vary from a minimum of 0 to a maximum of 39.
Statistical analysis
The statistical analysis of the data was performed using the IBM SPSS V. 25.0 package program (IBM Corporation, Armonk, NY, USA). A P-value less than 0.05 was considered for statistical significance. Categorical variables on sociodemographic characteristics of the participants were expressed using descriptive statistics and frequencies, whereas Continuous data were described using mean and standard deviation. For the statistical analysis, the awareness-knowledge-attitude-skill questionnaire's raw scores were adjusted to percentages and compared to other group factors. Scores of 49% were regarded poor, 50% to 70% were considered medium, and 71% were considered high. The survey was performed using the Checklist for Reporting Results of Internet E-Surveys. 19 Using Kolmogorov–Smirnov test, we didn’t identify any normally distributed for continuous outcomes including survey scores. Thus, we conducted a Mann–Whitney U test to see whether there were significant differences between the two groups and the scores of each segment. The Kruskal–Wallis H test was used to compare groups with three independent variables. A correlation between the category groups was examined using the Chi-squared test. Moreover, we conducted a Spearman test to detect if there was a significant correlation between the used subscales.
Ethical consideration
Ethical approval and research clearance were obtained from the ethical committee at the University of Aleppo and Damascus, and the study was conducted in line with the Declaration of Helsinki. All participants were informed of the study's objectives, including the research group's identity, their right to withdraw from the study, privacy, and data protection, and that only fully registered data will be analyzed.
Pilot study
To ensure the validity and reliability of the questionnaire, we set up a pilot study involving 25 of the medical doctors randomly chosen. We made modifications in light of the results of the pre-test study and depending on the suggested feedback. After conducting a pilot study and ensuring high levels of internal consistency (Cronbach's alpha ranged from 0.712 to 0.861), we disseminated the questionnaire.
Results
Baseline demographic characteristics
Three hundred and eighty-nine clinical doctors have received the survey on Google form, four have declined to complete the survey, and the final sample size was 385 out of which 52.72% of them were female. The majority of participants were aged below 30 (83.9%), and 66% of them were working in the governmental sector, with a predominance of Internal medicine (27%). Most participants have a master's academic degree (66.2%). Furthermore, 66% of participants have moderate knowledge about using computers and the internet (Table 1). However, 366 (95.1%) of them have not attended any formal training or training Workshop on telemedicine, and the majority of the participants revealed no significant availability of a telemedicine unit in their department 364 (89.9%). There was a significant correlation between the gender and only three variables, including medical specialty, knowledge of computers and the internet and academic degree, which the P-values were <0.001, <0.001 and 0.03, respectively (Table 1).
Table 1.
Baseline demographic characteristics of the study sample (n = 385).
| Variables | Total, n (%) | Females (n = 203) | Males (n = 182) | P-Value |
|---|---|---|---|---|
| Age range (years), n (%) | 0.152 | |||
| Below 30 | 323 (83.9) | 175 (86.2) | 148 (81.3) | |
| 31–40 | 30 (7.8) | 15 (7.4) | 15 (8.2) | |
| 41–50 | 16 (4.2) | 9 (4.4) | 7 (3.8) | |
| 51–60 | 12 (3.1) | 4 (2) | 8 (4.4) | |
| Above 60 | 4 (1) | 0 (0) | 4 (2.2) | |
| Work sector, n (%) | 0.62 | |||
| Government | 254 (66) | 135 (66.5) | 119 (65.4) | |
| Private | 47 (12.2) | 27 (13.3) | 20 (11) | |
| Corporate | 84 (21.8) | 41 (20.2) | 43 (23.6) | |
| Medical specialty, n (%) | <0.001b | |||
| Anesthesiology | 4 (1) | 0 (0) | 4 (2.2) | |
| Dermatology | 24 (6.2) | 18 (8.9) | 6 (3.3) | |
| Family medicine | 5 (1.3) | 4 (2) | 1 (0.5) | |
| Gynecology and obstetrics | 37 (9.6) | 30 (14.8) | 7 (3.8) | |
| Internal medicine (including all subspecialties) | 104 (27) | 53 (26.1) | 51 (28) | |
| Laboratory medicine | 6 (1.6) | 4 (2) | 2 (1.1) | |
| Ophthalmology, otolaryngology | 35 (9.1) | 19 (9.4) | 16 (8.8) | |
| Pediatrics | 27 (7) | 25 (12.3) | 2 (1.1) | |
| Psychiatry | 6 (1.6) | 2 (1.1) | 4 (2.2) | |
| Surgery (including all subspecialties) | 70 (18.2) | 5 (2.5) | 65 (35.7) | |
| Other | 67 (17.4) | 43 (21.2) | 24 (13.2) | |
| Knowledge of computer and internet, n (%) | <0.001 b | |||
| Beginner | 41 (10.6) | 29 (14.3) | 12 (6.6) | |
| Average | 254 (66) | 143 (70.4) | 111 (61) | |
| Advanced learner | 90 (23.4) | 31 (15.3) | 59 (32.4) | |
| Academic degree, n (%) | 0.03 a | |||
| Diploma | 6 (1.6) | 6 (3) | 0 (0) | |
| Bachelor | 103 (26.8) | 52 (25.6) | 51 (28) | |
| Master | 255 (66.2) | 138 (68) | 117 (64.3) | |
| PhD | 11 (2.9) | 2 (1) | 9 (4.9) | |
| Fellowship | 9 (2.3) | 5 (2.5) | 4 (2.2) | |
| Assistant professor | 1 (0.3) | 0 (0) | 1 (0.5) | |
| Experience (years), mean (SD) | 4.1 (5.2) | 3.5 (4) | 4.8 (6.2) | 0.056 |
| Have you ever heard of term telemedicine, n (%) | 0.71 | |||
| Yes | 310 (80.5) | 162 (79.8) | 148 (81.3) | |
| No | 75 (19.5) | 41 (20.2) | 34 (18.7) | |
| Have you attended any formal training in telemedicine, n (%) | 0.16 | |||
| Yes | 19 (4.9) | 7 (3.4) | 12 (6.6) | |
| No | 366 (95.1) | 196 (96.6) | 170 (93.4) | |
| Availability of a telemedicine unit in your department, n (%) | 0.23 | |||
| Yes | 39 (10.1) | 17 (8.4) | 22 (12.1) | |
| No | 346 (89.9) | 186 (91.6) | 160 (87.9) |
P < 0.05.
P < 0.001.
Awareness, knowledge, attitude, and skills among health care workers in Syria
31.7% of respondents had a high level of telemedicine awareness, 50.4% had a high level of telemedicine knowledge, and 57.7% had a favorable attitude toward telemedicine. However, 11.9% have poor comprehension of telemedicine, whereas just 3.9% have a negative attitude toward it. Moreover, 18.4% have advanced telemedicine skills (Table 2).
Table 2.
The description of the awareness, knowledge, attitude, and skills among health care workers in Syria (n = 385).
| Degree | Awareness | Knowledge | Attitude | Skills |
|---|---|---|---|---|
| Low (≤49%), n (%) | 109 (28.3) | 46 (11.9) | 15 (3.9) | 218 (56.6) |
| Average (50%–70%), n (%) | 154 (40) | 145 (37.7) | 148 (38.4) | 96 (24.9) |
| High (≥71%), n (%) | 122 (31.7) | 194 (50.4) | 222 (57.7) | 71 (18.4) |
Differences in the awareness, knowledge, the attitude, and computer skills
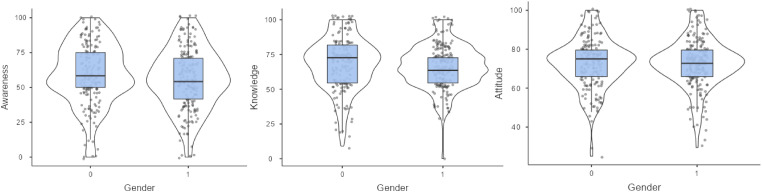
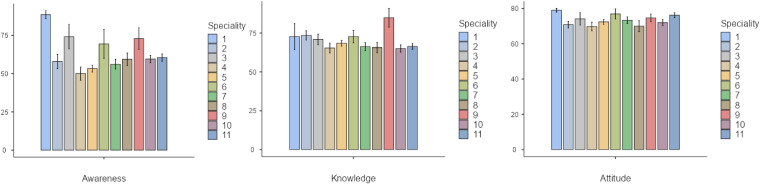
The Mann–Whitney U test revealed the differences between males and females in awareness, knowledge, attitude, and computer skills. According to our results in Table 3, there was no significant correlation between participant age and awareness (P-value = 0.089), knowledge (P-value = 0.679), or attitude (P-value = 0.182) toward telemedicine. In contrast, there was an obvious association the age and computer skills (P-value < 0.05), especially in the age group above 60. However, no significant association between gender and awareness (P-value = 0.112), knowledge (P-value = 0.185), and attitude (P-value = 0.89) toward telemedicine. In addition, males have shown higher mean computer skills than females (P-value < 0.001). The Kruskal–Wallis H test evaluated the difference in awareness, knowledge, attitude, and skill scores across various categories, including employment status, computer abilities, and work departments. There was no definite correlation between the academic level and telemedicine awareness (P-value = 0.784), knowledge (P-value = 0.73), attitude (P-value = 0.2), or computer skills (P-value = 0.27). Furthermore, health care workers in the government sector have demonstrated a greater mean in awareness (P-value < 0.001) and computer skills (P-value < 0.001). However, we identified a correlation between medical specialty and awareness (P-value < 0.001), as well as computer abilities (P-value < 0.05), especially the anesthesiology (mean = 88.5, SD = 5.2), (mean = 84, SD = 8.7), respectively. We found no significant correlation between the place of residence and awareness (P-value = 0.96), knowledge (P-value = 0.98), attitude (P-value = 0.31), and computer skill (P-value = 0.98). Furthermore, participants with advanced computer utilizing ability had a greater levels of awareness (mean = 63.4, SD = 22.2) (P-value = 0.001) and computer skills (mean = 68.2, SD = 22.3) (P-value = 0.001) (Table 3). Figure 1 shows no considerable difference between gender, awareness, and attitude toward telemedicine, and the values of the three assessed subscales were equal approximately among females and males (Figure 1). Figure 2 demonstrates the difference between the medical specialties and awareness, knowledge, and attitude toward telemedicine. The anesthesiologists have shown a higher awareness and attitude toward telemedicine, whereas the psychiatrists have demonstrated more outstanding knowledge of telemedicine (Figure 2).
Table 3.
Differences in the awareness, knowledge, the attitude, and computer skill scores of the study participants based on baseline demographic characteristics (n = 385).
| Variables | Total, N (%) | Awareness scores (range 0–100) | Knowledge scores (range 0–100) | Attitude scores (range 0–100) | Computer skill scores (range 0–100) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | H a Or U b Value | P-Value | Mean (SD) | H a Or U b Value | P-Value | Mean (SD) | H a Or U b Value | P-Value | Mean (SD) | H a Or U b Value | P-Value | ||
| Age | 8.067344 a | 0.089 | 2.309695 a | 0.679 | 6.232539 a | 0.182 | 11.036027 a | 0.026 c | |||||
| Below 30 | 323 (38.9) | 56.6 (21.6) | 66.9 (16.4) | 72.3 (12.3) | 48 (21.3) | ||||||||
| 31–40 | 30 (7.8) | 63.3 (24.3) | 68.2 (24.1) | 72.7 (16.3) | 60.9 (23.6) | ||||||||
| 41–50 | 16 (4.2) | 56.7 (22.9) | 75 (19.8) | 76.1 (11.3) | 44.7 (20.5) | ||||||||
| 51–60 | 12 (3.1) | 64.6 (24.7) | 71.2 (15.9) | 76.5 (15.5) | 48.5 (27.1) | ||||||||
| Above 60 | 4 (1) | 67.1 (12.4) | 63.6 (31.5) | 81.8 (8.5) | 65.4 (43.6) | ||||||||
| Gender | 16743 b | 0.112 | 17050.5 b | 0.185 | 18322 b | 0.89 | 14677.5 b | <0.001 d | |||||
| Male | 182 (47.3) | 59.3 (22.1) | 68.3 (19.1) | 72.7 (12.9) | 53.1 (23.3) | ||||||||
| Female | 203 (52.7) | 55.9 (21.8) | 66.8 (15.7) | 72.7 (12.5) | 45.5 (20.5) | ||||||||
| Academic degree | 2.451850 a | 0.784 | 2.807302 a | 0.73 | 7.290755 a | 0.2 | 6.396684 a | 0.27 | |||||
| Diploma | 6 (1.6) | 68.1 (22.5) | 69.7 (9.4) | 76.9 (3.3) | 64.1 (25.4) | ||||||||
| Bachelor | 103 (26.8) | 56.2 (21.2) | 65.8 (15.6) | 73.7 (13.2) | 48.2 (22.7) | ||||||||
| Master | 255 (66.2) | 57.9 (22.3) | 67.7 (17.8) | 71.7 (12.3) | 49.7 (22) | ||||||||
| PhD | 11 (2.9) | 58.33 (26.7) | 72.7 (26.7) | 77.7 (17.2) | 45.2 (22) | ||||||||
| Fellowship | 9 (2.3) | 56 (18.4) | 17.7 (16) | 78 (12.2) | 36.18 (13.1) | ||||||||
| Assistant professor | 1 (0.3) | NA | NA | NA | NA | ||||||||
| Work sector | 20.132950 a | <0.001 d | 5.235877 a | 0.07 | 8.721956 a | 0.013 c | 14.419506 a | <0.001 d | |||||
| Government | 254 (66) | 53.9 (21.9) | 66.25 (17.3) | 71.6 (12.9) | 46 (21.6) | ||||||||
| Private | 47 (12.2) | 64.5 (19.2) | 71.2 (18.9) | 76.8 (9.9) | 54.7 (22.1) | ||||||||
| Corporate | 84 (21.8) | 64.6 (21.5) | 69.2 (16.5) | 73.9 (13.1) | 55.2 (22.3) | ||||||||
| Medical specialty | 25.741078 a | <0.001 d | 12.184293 a | 0.27 | 13.446470 a | 0.2 | 19.909390 a | 0.03 c | |||||
| Anesthesiology | 4 (1) | 88.5 (5.2) | 72.7 (16.6) | 79 (2.1) | 84 (8.7) | ||||||||
| Dermatology | 24 (6.2) | 58 (23.3) | 73.5 (14.7) | 70.8 (9) | 50 (22.1) | ||||||||
| Family medicine | 5 (1.3) | 74.1 (17.8) | 70.9 (7.6) | 74.1 (7.8) | 63.6 (23.3) | ||||||||
| Gynecology and obstetrics | 37 (9.6) | 50 (26.1) | 65.4 (19) | 69.8 (14.5) | 42.6 (21.9) | ||||||||
| Internal medicine (including all subspecialties) | 104 (27) | 53.3 (22.6) | 68.4 (18.4) | 72.3 (12.9) | 46.9 (23.1) | ||||||||
| Laboratory medicine | 6 (1.6) | 69.4 (23.1) | 72.7 (9.9) | 76.9 (7.1) | 61.1 (19.6) | ||||||||
| Ophthalmology, otolaryngology | 35 (9.6) | 56.2 (18.9) | 66.2 (15.5) | 73.3 (11.1) | 50.6 (21.9) | ||||||||
| Pediatrics | 27 (7) | 59.4 (21.4) | 65.7 (17.1) | 70 (16) | 45.6 (17.4) | ||||||||
| Psychiatry | 6 (1.6) | 72.9 (17.2) | 84.9 (14.8) | 74.6 (5.1) | 62.4 (21.6) | ||||||||
| Surgery (including all subspecialties) | 70 (18.2) | 59.6 (20.4) | 65.1 (19.6) | 72 (13.7) | 51.2 (22.1) | ||||||||
| Other | 67 (17.4) | 60.51 (19.8) | 66.35 (14.7) | 76.2 (11.7) | 48.8 (21.4) | ||||||||
| Residence | 10099.5 b | 0.96 | 10128 b | 0.98 | 9321.5 b | 0.31 | 10126 b | 0.98 | |||||
| City | 322 (83.6) | 57.3 (22.5) | 67.4 (17.3) | 73.1 (12.8) | 49.2 (22.2) | ||||||||
| Countryside | 63 (16.4) | 58.7 (19.5) | 68.1 (17.9) | 71 (12) | 49 (22.1) | ||||||||
| Ability to use the computer | 15.505352 a | <0.001 d | 2.949681 a | 0.23 | 4.277243 a | 0.12 | 82.341890 a | <0.001 d | |||||
| Beginner | 41 (10.6) | 47 (22.4) | 67.9 (21.1) | 72 (12.4) | 33.3 (19.7) | ||||||||
| Average | 254 (66) | 57.2 (21.3) | 66.6 (16.9) | 72.1 (12.4) | 44.9 (17.9) | ||||||||
| Advanced learner | 90 (23.4) | 63.4 (22.2) | 69.8 (16.9) | 74.7 (13.5) | 68.2 (22.3) | ||||||||
Kruskal–Wallis H test for multiple-group comparison of independent variables.
Mann–Whitney U test for pairwise comparison of independent variables.
P < 0.05.
P < 0.001.
Figure 1.
The difference between gender and awareness, knowledge, and attitude toward telemedicine (0 = male, 1 = female).
Figure 2.
Demonstrates the difference between the medical specialties and awareness, knowledge, and attitude toward telemedicine (1. Anesthesiology, 2. Dermatology, 3. Family medicine, 4. Gynecology and obstetrics, 5. Internal medicine (including all subspecialties), 6. laboratory medicine, 7. Ophthalmology, otolaryngology, 8. Pediatrics, 9. Psychiatry, 10. Surgery (including all subspecialties), 11. other).
Correlation matrix between the experience (years) and awareness, knowledge, attitude, and skills scores
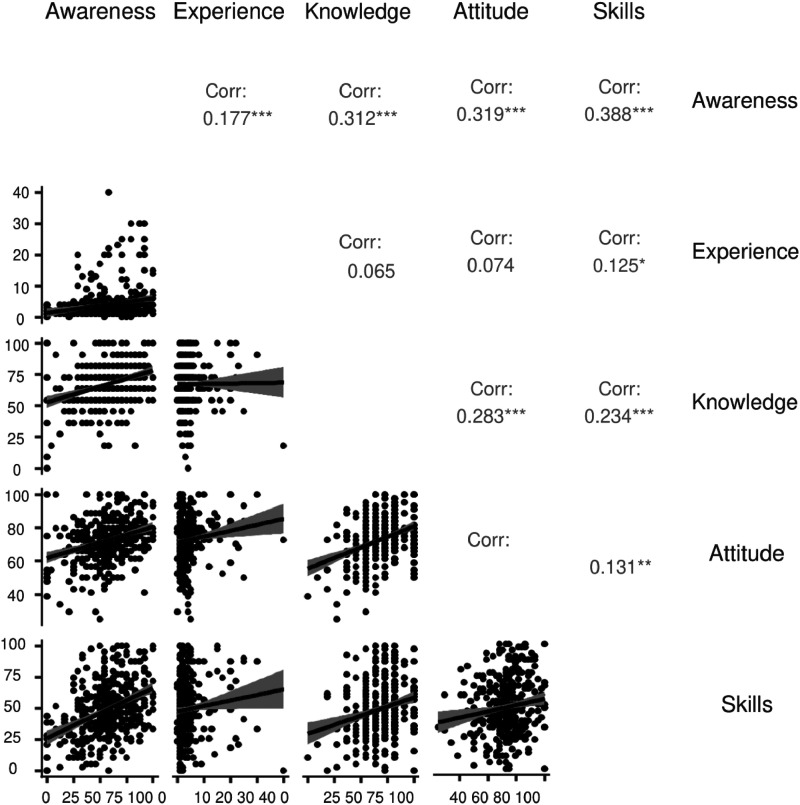
We used a Spearman's rho test to establish the relationship between the used subscales. We observed a mild positive significant correlation between the following subscales (Awareness & Experience, Experience & Skills, Knowledge & Attitude, Knowledge & Skills, and Attitude & Skills), and a moderate positive significant relationship between awareness subscale and the other subscales except experience subscale (Table 4 and Figure 3).
Table 4.
Correlation matrix between the experience (years) and awareness, knowledge, attitude, and skills scores.
| Subscales | Awareness | Experience | Knowledge | Attitude | Skills | |
|---|---|---|---|---|---|---|
| Awareness | Spearman's rho | — | ||||
| P-Value | — | |||||
| N | — | |||||
| Experience | Spearman's rho | 0.177*** | — | |||
| P-Value | <0.001 | — | ||||
| N | 385 | — | ||||
| Knowledge | Spearman's rho | 0.312*** | 0.065 | — | ||
| P-Value | <0.001 | 0.200 | — | |||
| N | 385 | 385 | — | |||
| Attitude | Spearman's rho | 0.319*** | 0.074 | 0.283*** | — | |
| P-Value | <0.001 | 0.146 | <0.001 | — | ||
| N | 385 | 385 | 385 | — | ||
| Skills | Spearman's rho | 0.388*** | 0.125 | 0.234*** | 0.131** | — |
| P-Value | <0.001 | 0.014 | <0.001 | 0.010 | — | |
| N | 385 | 385 | 385 | 385 | — | |
* P < 0.05.
** P < 0.01.
*** P < 0.001.
Figure 3.
Scatter plot and Spearman's correlation coefficient matrix. The upper panel above the diagonal shows Spearman's correlation coefficients with flagging for significant results. The lower panel below the diagonal gives their scatter plots.
Discussion
Principal findings
The pandemic of COVID-19 has stressed the importance of increased awareness of telemedicine as in the rest of the world, 20 especially in low- and low-intermediate-income countries. Where, the utilization of remote working technology assisted in early detection and reduced healthcare personnel’ burnout during the epidemic. Because of the limitations in infrastructural and skilled human resources, it is essential to assess health care providers’ acceptance and motivation toward telemedicine to tailor future modalities. 21 Our study revealed only 31.7% of the participants had a good awareness level toward telemedicine, 50.4% of them had high knowledge about telemedicine, and 57.7% had a high attitude toward telemedicine. Otherwise, the findings are not suitable for Syrian physicians because of the present horrible circumstances in Syria, but they are regarded as encouraging results since numerous past studies in lower-income countries such as Ethiopia and Libya recognized attitude as a key important component that contributes to the seamless adoption of technology in the health sector.22–24 Moreover, recent Chinese study has also backed the use of telemedicine, reporting that it is acceptable, and successful in Western China, with 76.7% of participants admitting that it has enhanced healthcare quality. 10 Telemedicine has increased, especially in developed countries, due to positive evidence during previous epidemics/pandemics and new advancements in technology. 25 However, telemedicine is unique to transitional countries like Syria, and sparse research has been done on this topic. When assessing the success of any relatively new system, we should consider that facilitators and barriers greatly influence the system's uptake. In Syria, where radiology equipment did not permit electronic image transmission, physicians were able to capture ultrasound scans and take photos of hardcopy radiograph films thanks to the functionality of mobile phones. Where videoconferencing would not have been feasible due to restricted internet connection, instant messaging, such as WhatsApp, was available. 26 Positive facilitators can be either internal or external; external factors refer to the facilities that enable the appropriate system's usage and the system itself. Internal factors refer to the user's behavior and motivation to use the system. It is crucial to identify these factors. 27 Our study has many strengths, including taking a snapshot of these factors; The questionnaires used assessed the physicians’ awareness, knowledge, attitude, and telemedicine skills and revealed positive internal facilitators from the physicians’ side. On the other side, the external facilitator factors showed that 95.1% of the participants had not attended any formal training or training workshop on telemedicine. According to a research conducted in Saudi Arabia, a lack of training may have played an essential role in the reality that over 50% of the doctors had no experience with telemedicine tools, apps, or medical technology. 28 However, a Peruvian research found no correlation between prior training and experience and the depth of telemedicine expertise. 29 This discovery may have several of reasons, including the possibility that although working in the field of telemedicine, doctors are not exposed to the requisite lectures or meetings on the subject, leaving them with inadequate awareness of this service. This result indicates that medical schools need to encourage and support the use of telemedicine teaching programs in undergraduate and medical specialty programs. Unfortunately, most participants revealed no significant availability of a telemedicine unit in their department 89.9%. Similar findings showed in French study where only 14% of participants reported having previously used telemedicine. 30 Only 23.4% of the participants showed advanced computer and internet skills, while 10.6% and 66% showed beginner and average computer skill levels. Therefore, the physicians’ overall computer skills and information technology skills were inadequate. Such skills are very crucial for the production of a successful telemedicine system. Consequently, we recommend formal training programs and workshops in telemedicine and software computer skills in transitional countries. However, we should consider that low-income countries affected by wars, such as Syria, have unstable electricity and internet connection; thus, the internet companies need to address these challenges as well. Our findings were in line with another study conducted in Libya, which revealed a positive attitude and high awareness of telemedicine among the physicians, but they lack the infrastructure in their healthcare system for its implementation. 31
Limitations
Our study is limited to the Syrian physicians in Syria. Furthermore, reporting a bias in studies is essential; however, in this study, we excluded sampling bias, response bias, non-response bias, acquiescence bias, and order bias, which is a potential limitation of this study. Another significant limitation is that the cross-sectional design of our study does not allow for drawing concrete conclusions regarding correlation causation between the variables. Our study was limited to physicians’ surveys; we didn’t study patients’ attitudes toward telemedicine. Additionally, participants were not particularly questioned about their understanding of and attitudes regarding all the many facets of telemedicine and the departments connected to it. Future research is needed to evaluate patients’ perception, accessibility, and beneficially to these patients from the telemedicine technology in transitional countries. Also, they should concentrate on the use of telemedicine to treat persistent illnesses and mental problems. Furthermore, a thorough examination of the many variables that may obstruct the use of telemedicine should be conducted. Finally, more doctors from urban areas with internet access and computer knowledge may have participated as it was a convenience sample.
Conclusion
According to our results, there is a significant need to raise awareness, knowledge, attitude, and computer skills about telemedicine in Syria. Additionally, there is a need to urge medical professionals to learn more about this technology and undertake additional training programs for telemedicine in Syria.
Footnotes
Availability of data and materials: The data that support the findings of this study are available from the corresponding author but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the corresponding author.
Contributorship: Sarya Swed has done conceptualization, methodology, formal analysis, writing-original draft, review and editing.
- Eyas Idrees, Faculty of Medicine, Tishreen University, Latakia, Syria
- Mohamed Wahedi, Department of Orthopedic Surgery, Aleppo University Hospital, Aleppo, Syria
- Haidara Kherbek, Faculty of Medicine, Tishreen University, Latakia, Syria
- Hiba Haj Saleh, Faculty of Medicine, Aleppo University, Aleppo, Syria
- Khedr Layka, Faculty of Medicine, Tishreen University, Latakia, Syria
- Daiana Karkouti, Faculty of Medicine,Tartus University, Tartus, Syria
- Jawa Nasser Mohammad Shareef, Faculty of Medicine, Tishreen University, Lattakia, Syria
- Huda Alhejazi, Faculty of Medicine, Aleppo Universit, Aleppo, Syria
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval and consent to participant: All experimental protocols were approved by Aleppo and Damascus institutional review boards. All methods were carried out in accordance with relevant guidelines and regulations or Declaration of Helsinki.
Written informed consent was obtained from all participants.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Guarantor: Sarya Swed.
ORCID iDs: Sarya Swed https://orcid.org/0000-0002-9983-2020
Basel Abdelazeem https://orcid.org/0000-0002-2919-6196
Sheikh Shoib https://orcid.org/0000-0002-3739-706X
References
- 1.Swed S, Alibrahim H, Sawaf B, et al. COVID-19, war and poverty in Syria. Ann Med Surg 2022; 75, Available from: /pmc/articles/PMC8860774/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abbas M, Alibrahim H, Hasan M, et al. Subcutaneous emphysema and spontaneous pneumomediastinum in non-intubated COVID-19 patient: the first case report in Syria. Ann Med Surg 2021; 72, Available from: /pmc/articles/PMC8603424/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus disease (COVID-19) [Internet]. [cited 2023 Apr 23]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQjwi46iBhDyARIsAE3nVrbmb5b4o431OzqcsssgQOViHzPsHbad5kATn9Sj052yEJhoKbvrR3MaArn1EALw_wcB.
- 4.WHO Director-General’s opening remarks at the media briefing on COVID-19–11 March 2020 [Internet]. [cited 2023 Apr 23]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020.
- 5.Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta 2020; 508: 254–266. https://pubmed.ncbi.nlm.nih.gov/32474009/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jin Y, Yang H, Ji W, et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses 2020; 12. Available from: https://pubmed.ncbi.nlm.nih.gov/32230900/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenhalgh T, Wherton J, Shaw Set al. et al. Video consultations for COVID-19. BMJ 2020; 368, Available from: https://www.bmj.com/content/368/bmj.m998. [DOI] [PubMed] [Google Scholar]
- 8.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: A call to action. JMIR Public Health Surveill 2020; 6. https://pubmed.ncbi.nlm.nih.gov/32238336/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iancu AM, Kemp MT, Alam HB. Unmuting medical students’ education: utilizing telemedicine during the COVID-19 pandemic and beyond. J Med Internet Res 2020; 22. https://pubmed.ncbi.nlm.nih.gov/32614776/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hong Z, Li N, Li D, et al. Telemedicine during the COVID-19 pandemic: experiences from Western China. J Med Internet Res 2020; 22. https://pmc/articles/PMC7212818/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med 2020; 382: 1679–1681. https://pubmed.ncbi.nlm.nih.gov/32160451/. [DOI] [PubMed] [Google Scholar]
- 12.Zundel KM. Telemedicine: history, applications, and impact on librarianship. Bull Med Libr Assoc 1996; 84: 71. https://pmc/articles/PMC226126/?report=abstract. [PMC free article] [PubMed] [Google Scholar]
- 13.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ 2000; 320: 1517–1520. https://pubmed.ncbi.nlm.nih.gov/10834899/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir J Med Sci 2021; 190. https://pubmed.ncbi.nlm.nih.gov/32642981/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anthony B, Jnr. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst 2020; 44. https://pubmed.ncbi.nlm.nih.gov/32542571/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hur J, Chang MC. Usefulness of an online preliminary questionnaire under the COVID-19 pandemic. J Med Syst 2020; 44. https://pmc/articles/PMC7235540/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parkes P, Pillay TD, Bdaiwi Y, et al. Telemedicine interventions in six conflict-affected countries in the WHO eastern Mediterranean region: A systematic review. Confl Health 2022; 16: 1–18. https://conflictandhealth.biomedcentral.com/articles/10.1186/s13031-022-00493-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zayapragassarazan Z, Kumar S. Awareness, knowledge, attitude and skills of telemedicine among health professional faculty working in teaching hospitals. J Clin Diagn Res 2016; 10: JC01–JC04. https://pubmed.ncbi.nlm.nih.gov/27134899/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004; 6. https://pubmed.ncbi.nlm.nih.gov/15471760/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Omboni S, Padwal RS, Alessa T, et al. The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connected Health. 2022; 1: 7. https://pmc/articles/PMC7612439/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiferaw KB, Mengiste SA, Gullslett MK, et al. Healthcare providers’ acceptance of telemedicine and preference of modalities during COVID-19 pandemics in a low-resource setting: an extended UTAUT model. PLoS One 2021; 16: e0250220. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0250220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yehualashet G, Asemahagn M, Tilahun B. The attitude towards and use of electronic medical record system by health professionals at a referral hospital in northern Ethiopia: cross-sectional study. J Health Inform Afr 2015; 3: 19–29. https://www.jhia-online.org/index.php/jhia/article/view/124. [Google Scholar]
- 23.Tilahun B, Fritz F. Comprehensive evaluation of electronic medical record system use and user satisfaction at five low-resource setting hospitals in Ethiopia. JMIR Med Inform 2015; 3. https://pmc/articles/PMC4460264/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McClellan SR, Casalino LP, Shortell SMet al. et al. When des adoption of health information technology by physician practices lead to use by physicians within the practice? J Am Med Inform Assoc 2013; 20: e26. https://pmc/articles/PMC3715336/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Galiero R, Pafundi PC, Nevola R, et al. The importance of telemedicine during COVID-19 pandemic: A focus on diabetic retinopathy. J Diabetes Res 2020; 2020. https://pmc/articles/PMC7584941/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parkes P, Pillay TD, Bdaiwi Y, et al. Telemedicine interventions in six conflict-affected countries in the WHO Eastern Mediterranean region: A systematic review. Confl Health 2022; 16: 1–18. https://conflictandhealth.biomedcentral.com/articles/10.1186/s13031-022-00493-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Almathami HKY, Than Win K, Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J Med Internet Res 2020; 22. https://pubmed.ncbi.nlm.nih.gov/32130131/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Albarrak AI, Mohammed R, Almarshoud N, et al. Assessment of physician’s knowledge, perception and willingness of telemedicine in Riyadh region, Saudi Arabia. J Infect Public Health 2021; 14: 97–102. [DOI] [PubMed] [Google Scholar]
- 29.García-Gutiérrez FM, Pino-Zavaleta F, Romero-Robles MA, et al. Self-reported perceptions and knowledge of telemedicine in medical students and professionals who enrolled in an online course in Peru. BMC Med Educ 2023; 23: 1–8. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-023-04058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yaghobian S, Ohannessian R, Iampetro T, et al. Knowledge, attitudes and practices of telemedicine education and training of French medical students and residents. J Telemed Telecare 2022; 28: 248–257. https://pubmed.ncbi.nlm.nih.gov/32517545/. [DOI] [PubMed] [Google Scholar]
- 31.Elhadi M, Elhadi A, Bouhuwaish A, et al. Telemedicine awareness, knowledge, attitude, and skills of health care workers in a low-resource country during the COVID-19 pandemic: cross-sectional study. J Med Internet Res 2021; 23. https://pubmed.ncbi.nlm.nih.gov/33600350/ [DOI] [PMC free article] [PubMed] [Google Scholar]