Abstract
Objectives
Food insecurity in the United States is a stubborn public health issue, affecting more than one in five households with children and disproportionately impacting racial and ethnic minority women and their children. Past research and policy has focused on household predictors of food insecurity, but neglected broader factors, such as perceived neighborhood social cohesion, that might protect those most vulnerable to food insecurity.
Methods
We use a racially and ethnically diverse data set from the Geographic Research on Wellbeing study (N = 2847) of women and their young children in California to investigate whether social cohesion influences food insecurity and whether it moderates the relationship between race/ethnicity and food insecurity.
Results
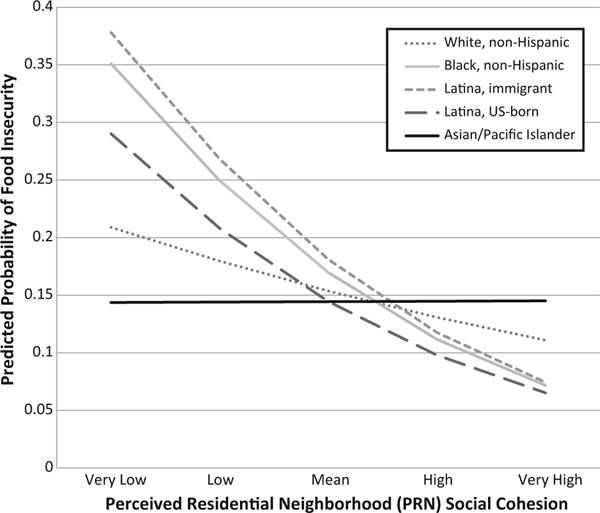
We find that lower levels of perceived residential neighborhood social cohesion associate with higher odds of food insecurity even after considering important household socioeconomic factors. In addition, our results suggest that social cohesion is most relevant for reducing the risk of food insecurity among racial and ethnic minority mothers. For example, the probability of food insecurity for immigrant Latina mothers is nearly 0.40 in neighborhoods where mothers perceive little to no cohesion and less than 0.10 in neighborhoods where mothers perceive high cohesion.
Conclusions for Practice
Higher levels of neighborhood perceived social cohesion are protective against food insecurity in households with children and especially so for racial and ethnic minority households who are at a heightened risk of food insecurity. Supporting programs that focus on building closer knit communities may be a key to reducing food insecurity overall and for reducing disparities in food insecurity by race and ethnicity.
Keywords: Food insecurity, Social cohesion, Race, Ethnicity
Introduction
Food insecurity, a household indicator of limited or uncertain access to adequate food, impacts over 14 % of all households in the United States, a rate which has increased more than 30 % since 2007, the start of the Great Recession (Nord et al. 2010). More troubling, over 20 % of all households with children in the U.S. experience food insecurity (Wight et al. 2010). As with the risks for many outcomes related to healthy development, food insecurity is not equally distributed among children. Specifically, children of immigrant mothers, and children in Hispanic and non-Hispanic black households, have levels of food insecurity nearly twice as high as those of native-born mothers, and children in non-Hispanic white households, respectively (Nord et al. 2010; Kalil and Chen 2008; Chilton et al. 2009). A number of other household and individual characteristics, such as household poverty and low socio-economic status (SES)–particularly low maternal education and participation in food assistance programs such as the Supplemental Nutrition Assistance Program (SNAP; formerly known as Food Stamps), WIC, or free/reduced breakfast and lunch–are known to be associated with household food insecurity (Kalil and Chen 2008; Rose and Richards 2004; Casey et al. 2001; Jones et al. 2003; Alaimo et al. 1998).
Background
Disparities in household food insecurity are particularly troubling given the clearly established consequences of food insecurity for children’s health and development (Gundersen et al. 2011; Alaimo et al. 2001b; Cook et al. 2004). Indeed, the frequency and duration of food insecure intervals throughout childhood, as well as their intensity, are related to well-being during important developmental periods (Kirkpatrick et al. 2010). And the consequences are wide ranging, from physical and mental health to academic performance. Studies have shown that children who live in food insecure households perform worse in math and reading, and more often miss school, repeat grades, have behavior and attention problems, and need special education services and mental health counseling (Jyoti et al. 2005; Alaimo et al. 2001a, 2002; Whitaker et al. 2006; Kleinman et al. 1998; Murphy et al. 1998). On the whole, food insecurity in households with children may be playing an important role in the pervasive health, development, and academic achievement disparities documented across racial and ethnic groups from infancy into adulthood.
Even with the documentation of these relationships, the issue of food insecurity–and particularly its solutions–have proved complex (Nord et al. 2010; Gundersen et al. 2011), suggesting that social and physical environmental factors outside of households may contribute importantly to the differentiation of risk. Given the orientation of existing research efforts, strategies and implemented policies to address food insecurity among children have largely focused on individual and household attributes. While these policies help individual families, to date they have struggled to curtail this enduring problem that disproportionately impacts minority and immigrant families. One reason behind stalled progress may be failing to consider the community correlates of food insecure families, limiting our knowledge of potentially effective intervention strategies.
Social cohesion reflects the degree of connectedness and solidarity among individuals in geographic space, most often, neighborhood of residence, with the notion that more cohesive neighborhoods display a collective capacity to translate social ties into goals for the common good (Sampson et al. 1997; Sampson 2003). The relevance of feeling connected to others in the community to securing adequate food supplies and being aware of social services to assist in that process is apparent. Indeed, a small body of work has emerged examining the relevance of community attachment, social capital, and social cohesion for the risk of food insecurity (Chung et al. 2012; Dean and Sharkey 2011; Dean et al. 2011; Carter 2013; Kirkpatrick and Tarasuk 2010; Brisson 2012; Carter et al. 2012). For example, Carter et al. (2012) used data gathered on the children of Quebec mothers to show that low social cohesion predicted higher food insecurity. Brisson (2012) used longitudinal data from Boston, Chicago, and San Antonio to show that more positive assessments of cohesion at time 1 predicted lower food insecurity at time 2.
Put simply, this recent evidence suggests that more cohesive communities possess dense and supportive social networks that can be leveraged to mitigate food insecurity risk. If so, the relevance of social cohesion may be most apparent in the highest risk populations. No work to date, however, has assessed whether social cohesion is particularly important for racial and ethnic groups most at risk of food insecurity.
Objectives
This paper has two primary objectives. First, we examine the association between perceived residential neighborhood social cohesion (PRN social cohesion) in participants’ neighborhood of residence and food insecurity among a racially and ethnically diverse sample of women in California after accounting for important socioeconomic and sociodemographic characteristics. Second, we estimate models with interactions between racial and ethnic identity of mother and PRN social cohesion to determine if social cohesion is more important for households of different race/ethnicities.
Methods
We use data from the Geographic Research on Wellbeing (GROW) study collected in 2012–2013. GROW is a population-based follow-up study of mothers initially interviewed as part of the California Maternal and Infant Health Assessment (MIHA) between 2003 and 2007. MIHA, which is very similar to CDC’s Pregnancy Risk Assessment Monitoring System, is an ongoing, statewide-representative mail or telephone survey of mothers delivering live infants in California during February through May annually, linked with birth certificate data. During 2003–2007, MIHA data included surveys from about 3500 women annually; data were weighted to be representative of the approximately 500,000 women who gave birth in California each year. Response rates for MIHA exceeded 70 % each year between 2003 and 2007; 71 % of the surveys were completed in English and 29 % in Spanish. The maternal characteristics of the MIHA sample are representative of all eligible births statewide (California Department of Public Health 2013). Additional details about the MIHA survey have been reported elsewhere (Cubbin et al. 2002; Heck et al. 2006; Braveman et al. 2004).
Women were eligible for GROW if they lived in one of six largely urbanized counties and had agreed to be re-contacted for future studies. Respondents in these 6 counties represented 55 % of all respondents in MIHA from 2003 to 2007. The administration for GROW was similar to that for MIHA and women were asked to respond to approximately 80 questions regarding demographic, socioeconomic, neighborhood, psychosocial, and health-related characteristics pertaining to herself and her index child (her infant from the MIHA survey). Of the 4026 sample of eligible women who were able to be located, 74.9 % responded (N = 3016). The large majority of respondents (90.3 %) still lived in one of the six GROW counties. Fifty-six percent completed the survey by phone, and 73 % completed it in English. For all items except income (9.8 %), missing values were less than 8 %. Weights were created (multiplying the estimated weighting factors of non-coverage, sampling fraction, and non-response to produce a final weight) to produce data that were representative of the birth file and original MIHA sample in the six GROW counties, and a sampling fraction file was created to make a minor finite population correction to the standard errors for analyses.
The analytic dataset excluded women whose race/ethnicity was reported as American Indian/Alaska Native, missing, or “other” (N = 29); and whose data was missing on any of the variables in the analyses, resulting in 2847 records (94 % of the GROW sample).
The GROW study was approved by the Institutional Review Boards at the University of Texas at Austin, the University of California, San Francisco, and the California Department of Public Health; all participants gave informed consent. Additional details about the GROW study have been reported elsewhere (Cubbin 2015).
Our dependent variable was food insecurity. We use a 6-item Household Food Security scale developed by researchers at the National Center for Health Statistics (NCHS) and that include questions referencing the last 12 months and querying mothers on issues such as: “The food I bought just didn’t last, and I didn’t have money to get more”, “I couldn’t afford to eat balanced meals”, and “Cut size of meals or skipped meals because there wasn’t enough money for food” (Blumberg et al. 1999). We coded mothers who answer affirmatively to at least 2 of the items as food insecure (vs. food secure).
For PRN social cohesion, our primary independent variable, we followed the method of Sampson et al. (1997) using 5 questions asking agreement with the following statements: “My neighbors feel connected to each other,” “People in my neighborhood are willing to help their neighbors,” “People in my neighborhood generally get along with each other,” “People in my neighborhood share the same values,” and “People in my neighborhood can be trusted.” Modifications from Sampson et al. (1997) included slight variations in wording. For example, in GROW, “my neighbors feel connected to each other” was used instead of the original wording, “this is a close-knit neighborhood,” because of concerns that some immigrants would not understand “close-knit.” In addition, instead of “in this neighborhood,” GROW used “in my neighborhood.” Responses range from strongly agree (Chilton et al. 2009) to strongly disagree (Nord et al. 2010), while Sampson et al. (1997) used a 5-point Likert scale. The original items have been demonstrated to have high internal consistency and test–retest reliability among a sample of women (Pruitt et al. 2012). The construct validity of social cohesion is supported in that it has been found to be associated with crime and informal social control, as would be expected theoretically (Sampson et al. 1997). For GROW respondents with at least 3 of the 5 items answered (97 % of the sample), we reverse code so that high values represent low social cohesion, averaged the values, and standardized the measure.
We control for a host of individual-level factors associated with food insecurity. These include age, race/ethnicity, relationship status, number of children in the household, duration at current residence, self-rated health of mother, educational attainment, and family income. Race/ethnicity data are from birth certificates. For 40 respondents with missing race/ethnicity information, we imputed race/ethnicity from self-reported data on the MIHA survey (2003–2006). Annual family income was measured as the total pretax income in 2011 from all sources combined with the number of people supported on that income, converted into increments of the federal poverty level. Preliminary analyses also examined employment status and tract-level poverty and population density. No significant associations between these items and food insecurity were observed so, for parsimony, these items were excluded from the final analyses.
Statistical Analysis
For the analyses, we first examined means or proportions on all of our covariates for the full sample, and prevalence of food insecurity for all of our covariates. Chi square tests of significance, comparing means or proportions between food insecure and food secure mothers for all covariates were highly significant (p < 0.0001, results not shown). Next, we use weighted logistic regression to investigate the odds of food insecurity for mothers and their children. In accordance with our objectives, we first examine PRN social cohesion after accounting for important individual and household predictors of food insecurity. Finally, we estimate interaction models between race/ethnicity of mother and PRN social cohesion to examine if the potential protective effects of social cohesion are most relevant for groups with the highest odds of food insecurity. We illustrate these interaction results by calculating and displaying fully adjusted predicted probabilities of food insecurity for each racial/ethnic group across categories of higher and lower PRN social cohesion. All analyses were weighted, accounted for the complex sample design, and were conducted using SAS version 9.
Results
The overall level of food insecurity in the sample is 22.7 %. Table 1 shows that food insecure mothers with children are younger, more often previously or never married, have more children in the home, have lived in their current home for a shorter period, are in worse health, are less educated, and are poorer than the average mother with children in the GROW sample. We also see varying rates of food insecurity by race of mother. For example, only 10.9 % of white mothers are food insecure compared to 30.7 % of black mothers and 36.0 % of Latina, immigrant mothers. Finally, while only 13.1 % of the sample report particularly low PRN social cohesion, 44.3 % of these mothers are food insecure.
Table 1.
Characteristics of women and prevalence of food insecurity, Geographic Research on Wellbeing study, 2012–2013, N = 2847
| Full sample distribution % (95 % CI) | Prevalence of food insecurity % (95 % CI) | |
|---|---|---|
| Age | ||
| 20–29 years | 18.5 (16.8–20.2) | 29.9 (24.9–34.9) |
| 30–39 years | 48.8 (46.7–50.8) | 24.1 (21.6–26.7) |
| 40 years or more | 32.7 (30.9–34.5) | 16.3 (13.9–18.7) |
| Race/ethnicity | ||
| Black, non-Hispanic | 6.4 (6.1–6.8) | 30.7 (25.0–36.3) |
| Latina, immigrant | 35.7 (34.0–37.5) | 36.0 (32.5–39.6) |
| Latina, US-born | 16.1 (14.6–17.5) | 21.6 (17.4–25.8) |
| Asian/Pacific Islander | 15.6 (13.9–17.3) | 9.5 (5.2–13.8) |
| White | 26.2 (24.7–27.7) | 10.9 (8.8–13.1) |
| Relationship status | ||
| Married/cohabiting | 83.7 (82.2–85.2) | 20.0 (18.1–21.8) |
| Previously/never married | 16.3 (14.8–17.8) | 36.5 (31.6–41.4) |
| Number of children in household | ||
| 0–1 | 11.1 (9.8–12.5) | 21.6 (15.7–27.4) |
| 2–3 | 64.4 (62.4–66.4) | 18.9 (16.9–20.9) |
| 4 or more | 24.4 (22.6–26.2) | 33.1 (29.0–37.1) |
| Duration at residence (%) | ||
| <1 year | 11.7 (10.3–13.0) | 39.8 (33.6–46.1) |
| 1 year or longer | 88.3 (87.0–89.7) | 20.4 (18.6–22.2) |
| Self-rated health | ||
| Poor/fair | 21.6 (19.9–23.3) | 40.5 (36.0–45.1) |
| Good/excellent | 78.4 (76.7–80.1) | 17.7 (15.9–19.5) |
| Educational attainment | ||
| Less than high school graduate | 20.0 (18.5–21.4) | 37.9 (33.2–42.7) |
| High school graduate or GED | 22.1 (20.3–24.0) | 32.2 (27.8–36.6) |
| Some college | 22.9 (21.3–24.6) | 23.1 (19.4–26.8) |
| College graduate | 34.9 (33.2–36.6) | 7.6 (5.9–9.3) |
| Family income | ||
| ≤100 % of federal poverty level | 30.9 (29.0–32.7) | 41.2 (37.4–45.0) |
| 101–200 % of federal poverty level | 18.1 (16.5–19.8) | 28.3 (23.9–32.8) |
| 201+ % of federal poverty level | 40.8 (39.1–42.6) | 5.4 (3.8–7.1) |
| Missing | 10.2 (8.9–11.4) | 25.3 (19.5–31.1) |
| Perceived social cohesion | ||
| <1 standard deviation (high cohesion) | 16.0 (14.6–17.4) | 9.6 (6.5–12.6) |
| Within 1 standard deviation | 71.0 (69.1–72.8) | 21.6 (19.5–23.7) |
| >1 standard deviation (low cohesion) | 13.1 (11.7–14.5) | 44.3 (38.6–50.0) |
CI confidence interval
Table 2 shows results for the association between race and ethnicity of mother and the risk of food insecurity. Model 1 adjusts for mother’s age, her relationship status, number of children in the household, duration at the residence, and her self-rated health. After adjusting for these risk factors, black and Latina mothers, compared to white mothers, have 1.5 (US born Latina) to over 3 (immigrant Latina) times higher odds of food insecurity. Model 2 shows that these higher racial and ethnic minority odds are largely explained by mother’s educational attainment and family income. Indeed, the poorest families, compared to the wealthiest GROW families, have odds of food insecurity that are 4.4 times higher. After adjusting for education and income, the odds of food insecurity for black and US born Latina mothers are statistically similar to white mothers. Foreign born Latina mothers, however, still have 1.45 times higher odds of food insecurity than do white mothers.
Table 2.
Odds ratios and 95 % confidence intervals for food insecurity, Geographic Research on Wellbeing study, 2012–2013, N = 2847
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Age | 0.98 (0.96–1.00)* | 1.00 (0.98–1.02) | 1.00 (0.98–1.02) | 1.00 (0.98–1.02) |
| Race/ethnicity (%) | ||||
| Asian/Pacific Islander | 0.89 (0.51–1.57) | 0.95 (0.52–1.76) | 0.93 (0.50–1.75) | 0.93 (0.50–1.74) |
| Black, non-Hispanic | 2.02 (1.37–2.99)*** | 1.29 (0.85–1.96) | 1.19 (0.78–1.83) | 1.13 (0.72–1.76) |
| Latina, immigrant | 3.29 (2.44–4.42)*** | 1.45 (1.00–2.16)* | 1.32 (0.90–1.91) | 1.22 (0.83–1.78) |
| Latina, US-born | 1.51 (1.04–2.19)* | 1.03 (0.69–1.54) | 0.97 (0.64–1.46) | 0.93 (0.61–1.41) |
| White, non-Hispanic | 1.00 | 1.00 | 1.00 | 1.00 |
| Relationship status (%) | ||||
| Married/cohabiting | 1.00 | 1.00 | 1.00 | 1.00 |
| Previously/never married | 1.84 (1.39–2.44)*** | 1.38 (1.03–1.84)* | 1.34 (1.00–1.81) | 1.35 (1.00–1.82) |
| Number of children in household | 1.14 (1.06–1.23)*** | 1.07 (0.99–1.15) | 1.07 (0.99–1.16) | 1.08 (1.00–1.16) |
| Duration at residence (%) | ||||
| <1 year | 2.52 (1.87–3.40)*** | 2.48 (1.80–3.40)*** | 2.31 (1.67–3.18)*** | 2.31 (1.67–3.20)*** |
| 1 year or longer | 1.00 | 1.00 | 1.00 | 1.00 |
| Self-rated health (%) | ||||
| Poor/fair | 2.36 (1.85–3.03)*** | 2.07 (1.61–2.67)*** | 1.99 (1.53–2.58)*** | 2.01 (1.54–2.61)*** |
| Good/very good/excellent | 1.00 | 1.00 | 1.00 | 1.00 |
| Educational attainment (%) | ||||
| Less than high school graduate | 1.67 (1.04–2.67)* | 1.56 (0.97–2.50) | 1.67 (1.05–2.65)* | |
| High school graduate or GED | 1.52 (0.96–2.42) | 1.45 (0.91–2.31) | 1.54 (0.98–2.42) | |
| Some college | 1.79 (1.18–2.72)** | 1.62 (1.07–2.47)* | 1.71 (1.14–2.56)** | |
| College graduate | 1.00 | 1.00 | 1.00 | |
| Family income (%) | ||||
| ≤100 % of federal poverty level | 4.40 (2.85–6.81)*** | 4.09 (2.63–6.37)*** | 4.10 (2.66–6.31)*** | |
| 101–200 % of federal poverty level | 3.00 (1.95–4.59)*** | 2.84 (1.84–4.38)*** | 2.85 (1.85–4.39)*** | |
| 201+ % of federal poverty level | 1.00 | 1.00 | 1.00 | |
| Missing | 2.65 (1.70–4.12)*** | 2.65 (1.70–4.14)*** | 2.59 (1.67–4.01)*** | |
| Perceived social cohesion | 1.50 (1.32–1.71)*** | 1.21 (0.95–1.54) | ||
| Social cohesion × Asian/Pacific Islander | 0.83 (0.41–1.68) | |||
| Social cohesion × Black, non-Hispanic | 1.35 (0.89–2.03) | |||
| Social cohesion × Latina, immigrant | 1.38 (1.01–1.87)* | |||
| Social cohesion × Latina, US-born | 1.29 (0.86–1.93) |
Social Cohesion is standardized and reversed so that large values represent low perceived social cohesion
CI confidence interval
p < 0.001;
p < 0.01;
p < 0.05
Model 3 adds a standardized measure of PRN social cohesion (higher values represent lower social cohesion) and shows that one standard deviation decrease in PRN social cohesion is associated with 50 % higher odds of food insecurity, even after accounting for the other important social, demographic, and economic covariates. Accounting for PRN social cohesion further lowers the odds of food insecurity for the racial/ethnic groups such that Latina immigrant mother’s odds are statistically similar to white mothers.
Finally, Model 4 tests whether PRN social cohesion is more relevant for those who are already at higher odds of food insecurity. The interaction ORs are consistently positive (i.e. greater than 1.0) for non-Hispanic black, US born Latina, and immigrant Latina mothers, suggesting that lower social cohesion is particularly problematic for the odds of food insecurity among these racial and ethnic minority women. The interaction ORs for non-Hispanic black (p = 0.15) and US born Latina (p = 0.21) mothers do not reach significance. The interaction OR for immigrant Latina mothers does reach significance (p = 0.04).
Figure 1 uses the regression estimates in Model 4 and displays predicted probabilities of food insecurity for the racial and ethnic groups at varying levels of PRN social cohesion. The figure suggests a stepwise reduction in the probability of food insecurity with each increase in social cohesion for all groups except Asian/Pacific Islanders. Consistent with the results from Table 2, the reduction is most pronounced for Latina and non-Hispanic black mothers.
Fig. 1.
Predicted probabilities of food insecurity, by race/ethnicity and PRN social cohesion
Discussion
Food insecurity in households with children is a detrimental and stubborn public health issue. It is at the highest level of severity ever measured in the U.S. and has increased over 30 % since 2007 in spite of federal food and nutrition assistance programs aimed at its elimination (Nord et al. 2010).
Our results, adding to other recent studies (Chung et al. 2012; Dean and Sharkey 2011; Dean et al. 2011; Martin et al. 2004), suggest that mothers’ perceived high levels of connectedness in their neighborhoods of residence has important implications for their families’ risk of food insecurity. Significantly, we find evidence that social cohesion may be especially relevant for those households most at risk. To put Fig. 1 into perspective, the probability of food insecurity for immigrant Latina mothers (almost 0.40) is nearly twice as high as that of white mothers (0.21) in neighborhoods where mothers feel little to no connectedness or solidarity with others. At the mean level of PRN social cohesion, the twofold difference is reduced substantially. And for mothers who feel a strong social connection to others in their neighborhood, the probability of food insecurity for immigrant Latina mothers drops to less than 0.10, lower than that of white mothers.
Optimistically, enhancing social cohesion in communities could help hundreds of thousands of women and their children avoid food insecurity. High levels of perceived social cohesion bring social capital to communities and residents, building trust among neighbors and encouraging norms of reciprocity which translate to shared resources, which might include food or strategies to mitigate food insecurity. Though not as often a research focus, scholars have documented coordinated strategies among residents in disadvantaged communities, often racial and ethnic minority neighborhoods, to overcome seemingly overwhelming adversity (Seccombe 2002; Small et al. 2010) in part by building relationships and resources through collective action.
Our results support research efforts and policy strategies that develop innovative ways to target neighborhoods rather than (or in addition to) households. Moving beyond simply addressing issues of food access (Sadler et al. 2013) and instead focusing attention on building social capital and cohesion in communities might have additional unanticipated advantages, such as reaching families who might need, but may not be knowledgeable about, existing assistance programs such as SNAP or WIC. For example, some research has shown that child care centers, schools, and other neighborhood institutions, in addition to providing specific services, also build strong networks of social support, trust, and cohesion (Small 2009; Sherman 2006). So while providing parents with needed services, these neighborhood institutions can also create informal networks that might be used to mitigate food insecurity. Put simply, social services that can address food insecurity do not have to be social services focused solely on providing access to food.
Limitations
The GROW study provides an effective follow-up to MIHA respondents, resulting in a unique population-based survey sample representative of women with young children in California (Cubbin 2015). However, the limited sample size of GROW restricts the level of racial and ethnic detail that we can investigate here. In addition, with a relatively small number of mothers in each race/ethnic group, nested in even fewer neighborhoods, our analyses of other neighborhood indicators that might modify relationships between PRN social cohesion, race, and food insecurity are limited. Finally, that the GROW study includes measures of social cohesion and food insecurity make it a valuable source of data, though we are limited to just a subset of the potential indicators used to understand links between social cohesion and well-being (Sampson et al. 1997). More nationally representative data sets which include assessments of food security and include measures of social cohesion are needed.
Conclusion
Prior evidence and the findings presented here support the idea that unique social processes may allow some disadvantaged residents to overcome food insecurity, but more work is needed. Specifically, how might building social cohesion work to reduce food insecurity and what sorts of policies can support those efforts? As a start, we might turn to a limited number of studies which document the building of social capital and cohesion via school-based intervention programs (Terrion 2006; Noguera 2001). Designed to encourage parents to engage with their children’s academic life, these programs have the added benefit of expanding social networks and creating strong links to other vulnerable families. This, in addition to after-school programs which feed families dinner could be expanded, particularly in high disadvantage communities. Such programs harness and nurture community social cohesion (Berkman 2000), can reduce food insecurity among children, and might close the gap in food insecurity risks by race and ethnicity.
Significance.
What is already known on this subject?
More than 1 in 5 households with children under the age of 18 in the United States are food insecure. Past research has identified heightened risks for food insecurity for racial and ethnic minority households and that food insecurity has robust negative associations with health and development.
What does this study add?
We know far less about how communities shape food insecurity. The current study focuses on the role of perceived social cohesion in the residential neighborhood and finds that as feelings of social connectedness increase, the odds of food insecurity decrease even after accounting for household predictors. Further, we find that perceived social cohesion is most relevant for those at the highest risk, racial and ethnic minority mothers and their children.
Acknowledgments
We thank the Urban Health Program at Rice University for administrative support. This work was supported by a Research Scholar Grant from the American Cancer Society (RSGT-11-010-01-CPPB) to C. Cubbin and a Foundation for Child Development Young Scholars Program Grant (YSP Rice 10-2014) to J. Denney.
References
- Alaimo K, Briefel RR, Frongillo EA, et al. (1998). Food insufficiency exists in the United States: Results from the third National Health and Nutrition Examination Survey (NHANES III). American Journal of Public Health, 88(3), 419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alaimo K, Olson CM, & Frongillo EA Jr. (2001a). Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics, 108(1), 44–53. [PubMed] [Google Scholar]
- Alaimo K, Olson CM, & Frongillo EA (2002). Family food insufficiency, but not low family income, is positively associated with dysthymia and suicide symptoms in adolescents. Journal of Nutrition, 132(4), 719–725. [DOI] [PubMed] [Google Scholar]
- Alaimo K, Olson CM, Frongillo EA Jr., et al. (2001b). Food insufficiency, family income, and health in US preschool and school-aged children. American Journal of Public Health, 91(5), 781–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman LF (2000). Social support, social networks, social cohesion and health. Social Work in Health Care, 31(2), 3–14. [DOI] [PubMed] [Google Scholar]
- Blumberg SJ, Bialostosky K, Hamilton WL, et al. (1999). The effectiveness of a short form of the Household Food Security Scale. American Journal of Public Health, 89(8), 1231–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Egerter SA, Cubbin C, et al. (2004). An approach to studying social disparities in health and health care. American Journal of Public Health, 94(12), 2139–2148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brisson D. (2012). Neighborhood social cohesion and food insecurity: A longitudinal study. Journal of the Society for Social Work and Research, 3(4), 268–279. [Google Scholar]
- California Department of Public Health. (2013). California Maternal and Infant Health Assessment (MIHA) Technical Documenta-tion. http://www.cdph.ca.gov/data/surveys/MIHA/Documents/MIHATechnicalDocument.pdf. [Google Scholar]
- Carter MA (2013). Do childhood excess weight and family food insecurity share common risk factors in the local environment? An examination using a Quebec birth cohort. Applied Physiology, Nutrition and Metabolism, 39(3), 404. [Google Scholar]
- Carter MA, Dubois L, Tremblay MS, et al. (2012). Local social environmental factors are associated with household food insecurity in a longitudinal study of children. BMC Public Health, 12(1), 1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey PH, Szeto K, Lensing S, et al. (2001). Children in food-insufficient, low-income families: Prevalence, health, and nutrition status. Archives of Pediatrics and Adolescent Medicine, 155(4), 508–514. [DOI] [PubMed] [Google Scholar]
- Chilton M, Black MM, Berkowitz C, et al. (2009). Food insecurity and risk of poor health among US-born children of immigrants. American Journal of Public Health, 99(3), 556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung WT, Gallo WT, Giunta N, et al. (2012). Linking neighborhood characteristics to food insecurity in older adults: The role of perceived safety, social cohesion, and walkability. Journal of Urban Health, 89(3), 407–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JT, Frank DA, Berkowitz C, et al. (2004). Food insecurity is associated with adverse health outcomes among human infants and toddlers. Journal of Nutrition, 134(6), 1432–1438. [DOI] [PubMed] [Google Scholar]
- Cubbin C. (2015). Survey methodology of the Geographic Research on Wellbeing (GROW) study. BMC Research Notes, 8, 402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cubbin C, Braveman PA, Marchi KS, et al. (2002). Socioeconomic and racial/ethnic disparities in unintended pregnancy among postpartum women in California. Maternal and Child Health Journal, 6(4), 237–246. [DOI] [PubMed] [Google Scholar]
- Dean WR, & Sharkey JR (2011). Food insecurity, social capital and perceived personal disparity in a predominantly rural region of Texas: An individual-level analysis. Social Science and Medicine, 72(9), 1454–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean WR, Sharkey JR, & Johnson CM (2011). Food insecurity is associated with social capital, perceived personal disparity, and partnership status among older and senior adults in a largely rural area of central Texas. Journal of Nutrition in Gerontology and Geriatrics, 30(2), 169–186. [DOI] [PubMed] [Google Scholar]
- Gundersen C, Kreider B, & Pepper J. (2011). The economics of food insecurity in the United States. Applied Economic Perspectives and Policy, 33(3), 281–303. [Google Scholar]
- Heck KE, Braveman P, Cubbin C, et al. (2006). Socioeconomic status and breastfeeding initiation among California mothers. Public Health Reports, 121(1), 51–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SJ, Jahns L, Laraia BA, et al. (2003). Lower risk of overweight in school-aged food insecure girls who participate in food assistance: Results from the panel study of income dynamics child development supplement. Archives of Pediatrics and Adolescent Medicine, 157(8), 780–784. [DOI] [PubMed] [Google Scholar]
- Jyoti DF, Frongillo EA, & Jones SJ (2005). Food insecurity affects school children’s academic performance, weight gain, and social skills. Journal of Nutrition, 135(12), 2831–2839. [DOI] [PubMed] [Google Scholar]
- Kalil A, & Chen JH (2008). Mothers’ citizenship status and household food insecurity among low-income children of immigrants. New Directions for Child and Adolescent Development, 121, 43–62. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick SI, McIntyre L, & Potestio ML (2010). Child hunger and long-term adverse consequences for health. Archives of Pediatrics and Adolescent Medicine, 164(8), 754. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick SI, & Tarasuk V. (2010). Assessing the relevance of neighbourhood characteristics to the household food security of low-income toronto families. Public Health Nutrition, 13(7), 1139–1148. [DOI] [PubMed] [Google Scholar]
- Kleinman RE, Murphy JM, Little M, et al. (1998). Hunger in children in the United States: Potential behavioral and emotional correlates. Pediatrics, 101(1), E3. [DOI] [PubMed] [Google Scholar]
- Martin KS, Rogers BL, Cook JT, et al. (2004). Social capital is associated with decreased risk of hunger. Social Science and Medicine, 58(12), 2645–2654. [DOI] [PubMed] [Google Scholar]
- Murphy JM, Wehler CA, Pagano ME, et al. (1998). Relationship between hunger and psychosocial functioning in low-income American children. Journal of the American Academy of Child and Adolescent Psychiatry, 37(2), 163–170. [DOI] [PubMed] [Google Scholar]
- Noguera PA (2001). Transforming urban schools through investments in the social capital of parents . In S. Saegert, J. [Google Scholar]
- Thompson P, & Warren MR (Eds.), Social capital and poor communities (pp. 189–212). New York: Russell Sage. [Google Scholar]
- Nord M, Coleman-Jensen A, Andrews M, et al. (2010). Household food security in the United States, 2009. Washington, DC: US Department of Agriculture. [Google Scholar]
- Pruitt SL, Jeffe DB, Yan Y, et al. (2012). Reliability of perceived neighborhood conditions and the effects of measurement error on self-rated health across urban and rural neighborhoods. Journal of Epidemiology and Community Health, 66(4), 342–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose D, & Richards R. (2004). Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public Health Nutrition, 7(8), 1081–1088. [DOI] [PubMed] [Google Scholar]
- Sadler RC, Gilliland JA, & Arku G. (2013). A food retail-based intervention on food security and consumption. International Journal of Environmental Research and Public Health, 10(8), 3325–3346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ (2003). The neighborhood context of well-being. Perspectives in Biology and Medicine, 46(3), S53–S64. [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, & Earls F. (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277(5328), 918–924. [DOI] [PubMed] [Google Scholar]
- Seccombe K. (2002). “Beating the odds” versus “changing the odds”: Poverty, resilience, and family policy. Journal of Marriage and Family, 64(2), 384–394. [Google Scholar]
- Sherman J. (2006). Coping with rural poverty: Economic survival and moral capital in rural America. Social Forces, 85(2), 891–913. [Google Scholar]
- Small ML (2009). Unanticipated gains: origins of network inequality in everyday life. New York: Oxford University Press. [Google Scholar]
- Small ML, Harding DJ, & Lamont M. (2010). Reconsidering culture and poverty. Annals AAPSS, 629, 6–26. [Google Scholar]
- Terrion JL (2006). Building social capital in vulnerable families: Success markers of a school-based intervention program. Youth & Society, 38(2), 155–176. [Google Scholar]
- Whitaker RC, Phillips SM, & Orzol SM (2006). Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics, 118(3), e859–e868. [DOI] [PubMed] [Google Scholar]
- Wight VR, Thampi K, & Briggs J. (2010). Who are America’s poor children? Examining food insecurity among children in the United States. Columbia University, Mailman School of Public Health: National Center for Children in Poverty. [Google Scholar]