Introduction
Falling is the most frequent cause of injury in older adults in the United States, leading to substantial disability and mortality. A variety of studies have found that approximately one-third of older adults fall each year, but there have been no nationally representative longitudinal studies that examine falling across the population over time.1 Falling is anticipated to increase in the United States owing to changing demography. However, a prior statewide study showed a temporal increase (1999–2001) in the annual rate of falls requiring medical care, independent of age.2 We investigated temporal trends in falling on a national scale from 1998 to 2010, hypothesizing that any increase in prevalence would be due to changes in the age structure of the population.
Methods
We used data from 7 biennial waves (1998–2010) of the Health and Retirement Study, a nationally representative longitudinal health interview survey of a cohort of middle-aged and older adults in the United States.3,4 The Health and Retirement Study is sponsored by the National Institute on Aging, is performed by the Institute for Social Research (University of Michigan), and was approved by the University of Michigan Health Sciences Institutional Review Board. The practice of the Health and Retirement Study (for both telephone and in-person interviews) is for respondents to be read a confidentiality statement when first contacted; respondents provide oral or implied consent by agreeing to the interview. The study sample for each wave included all adults 65 years or older (≥10 590 for each wave).
We defined falling as at least 1 self-reported fall in the preceding 2 years. We also examined fall frequency and fall injuries. Covariates included sociodemographic characteristics (eg, age, sex, race and ethnicity, marital status, educational level), chronic diseases (eg, hypertension, heart disease, chronic lung disease, diabetes mellitus, musculoskeletal conditions, stroke), other geriatric conditions (eg, dementia, urinary incontinence, vision impairment, hearing impairment), and body mass index.5 We also investigated the effect of participation in prior interview waves on the self-report of falls. We used age-stratified cross-sectional and longitudinal logistic analyses to investigate falling across interview waves.
Results
Among all adults 65 years or older, the 2-year prevalence of self-reported falls increased from 28.2% in 1998 to 36.3% in 2010 (Figure). Stratifying by age, fall prevalence increased for adults aged 65 to 89 years (Table) and was most marked at the younger end of the age range (analysis of 1-year age cohorts). Using unadjusted age-stratified logistic models across all 7 waves, linear time predicted increased fall prevalence for all but 4 ages from 65 to 88 years. In fully adjusted models, linear time predicted increased fall prevalence for all but 6 ages from 65 to 82 years (P < .05); prevalence differences were smaller or nonexistent for older ages in fully adjusted models, and therefore no longer statistically significant. We could not find any significant effects for disease-by-time interaction (eg, diabetes with time), suggesting that the increase in fall prevalence is always observed, regardless of the presence of disease. The increased self-report of falls across interview waves was not associated with respondents’ participation in the immediately preceding interview wave; the increase was likewise not associated with the total number of preceding interviews in which respondents participated. There was no increase in disability across interview waves, and the increased self-report of falls was found with older adults with and without a disability. There was no concomitant increase in the prevalence of injury from falls at the population level or with age stratification.
Figure.
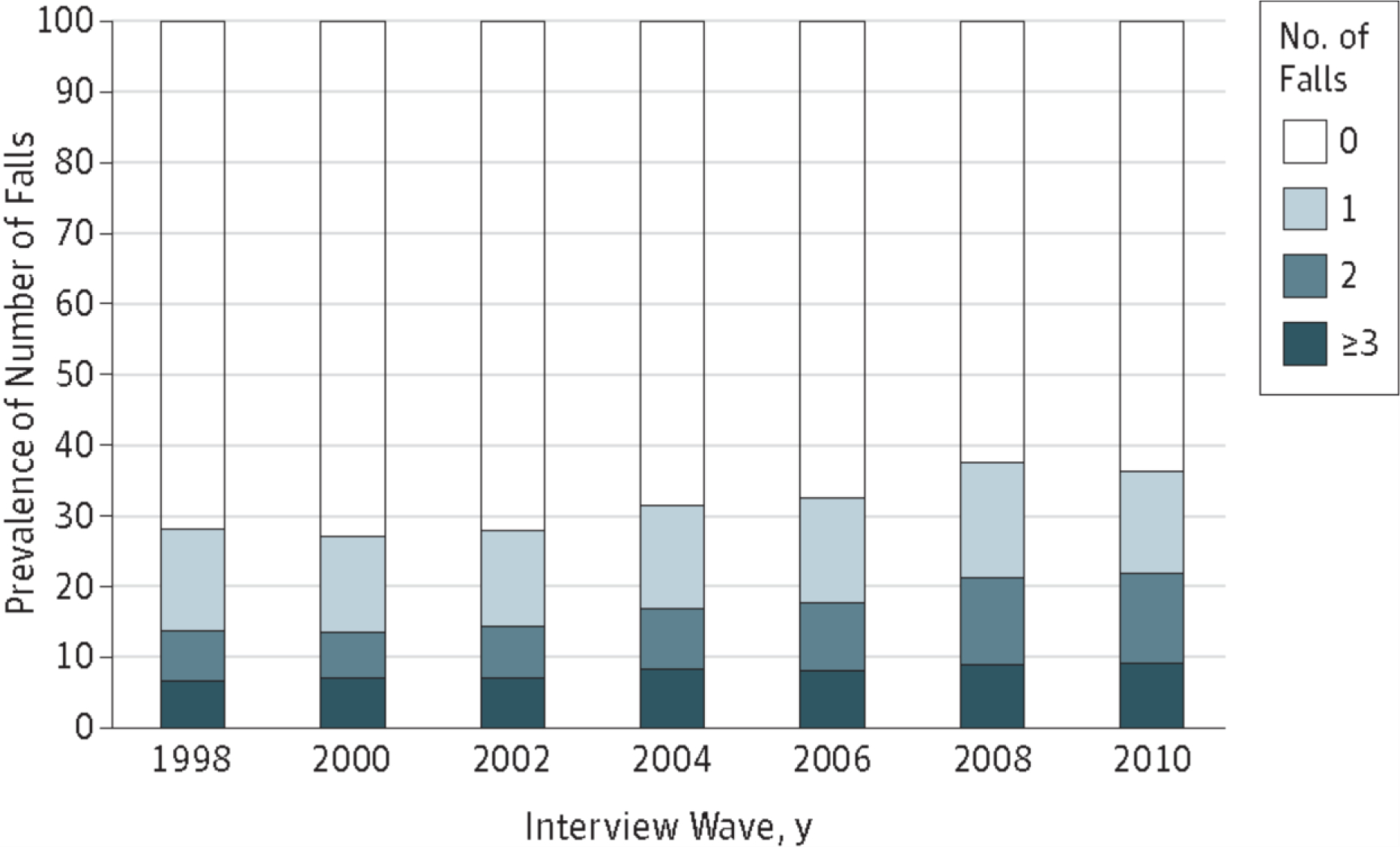
Two-Year Prevalence of Number of Falls Across Interview Waves of the Health and Retirement Study (1998–2010)
Respondents replied to the question “Have you fallen down in the last 2 years/since respondent’s last interview?” Weighted percentages were derived using Health and Retirement Study respondent population weights to adjust for differential probability of selection into the sample and differential nonresponse.
Table.
Two-Year Prevalence of at least one fall, stratified by age, 1998 and 2010.
| Age at interview, y | 2-year prevalence (%)a |
P value | |
|---|---|---|---|
| 1998 | 2010 | ||
| 65–69 | 22.3 | 32.0 | <.01 |
| 70–74 | 25.3 | 34.5 | <.01 |
| 75–79 | 30.5 | 38.4 | <.01 |
| 80–84 | 37.6 | 44.3 | <.01 |
| 85–89 | 45.8 | 46.7 | 0.68 |
| ≥90 | 55.8 | 56.7 | 0.79 |
Weighted percentages were derived using Health and Retirement Study respondent population weights to adjust for differential probability of selection into the sample and differential non-response.
Discussion
Contrary to our hypothesis, we observed an increase in fall prevalence among older adults that exceeds what would be expected owing to the increasing age of the population. Programs such as Matter of Balance focus on making older adults aware of balance and fall risk and provide strategies to reduce fall risk; these programs may improve reporting.6 Alternatively, if a true increase in falling is occurring, then further research is needed to identify possible reasons, such as an increase in fall risk factors (eg, cardiovascular and psychiatric medications) or an increase in fall risk behavior.
Acknowledgements
Funding/Support: Dr Cigolle is supported by grant K08 AG031837 from the National Institute on Aging.
Role of the Sponsor: The National Institute on Aging had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: No disclosures pertinent to the study.
References
- 1.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. [DOI] [PubMed] [Google Scholar]
- 2.Murphy TE, Tinetti ME, Allore HG. Hierarchical models to evaluate translational research: Connecticut collaboration for fall prevention. Contemp Clin Trials. 2008;29(3):343–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Juster FT, Suzman R. An overview of the Health and Retirement Study. Journal of Human Resources. 1995;30:S7–S56. [Google Scholar]
- 4.Soldo BJ, Hurd MD, Rodgers WL, Wallace RB. Asset and Health Dynamics Among the Oldest Old: an overview of the AHEAD Study. J Gerontol B Psychol Sci Soc Sci. 1997;52 Spec No:1–20. [DOI] [PubMed] [Google Scholar]
- 5.Cigolle CT, Langa KM, Kabeto MU, Tian Z, Blaum CS. Geriatric conditions and disability: the Health and Retirement Study. Ann Intern Med. 2007;147:156–64. [DOI] [PubMed] [Google Scholar]
- 6.Zijlstra GA, van Haastregt JC, Ambergen T, van Rossum E, van Eijk JT, Tennstedt SL, Kempen GI. Effects of a multicomponent cognitive behavioral group intervention on fear of falling and activity avoidance in community-dwelling older adults: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57(11):2020–8. [DOI] [PubMed] [Google Scholar]


