Abstract
The posterior cruciate ligament (PCL) is an important restraint to posterior tibial translation. PCL reconstruction is one of the most challenging procedures, with the literature having described many techniques for reconstruction. Protecting the neurovascular structures, overcoming the “killer turn,” preserving bone, and reducing morbidity and postoperative pain are a few of the technical challenges that surgeons often encounter during PCL reconstruction. We describe a technique using a graft-link construct through the anteromedial portal for all-inside PCL reconstruction with remnant preservation that protects the graft from the killer turn of the tibia by smooth passage of the graft over the remnant and improves proprioception, thereby reducing postoperative pain and morbidity and achieving excellent functional outcomes.
Technique Video
All-inside posterior cruciate ligament reconstruction with remnant preservation using anteromedial portal technique.
The posterior cruciate ligament (PCL) is an important restraint to posterior tibial translation.1 Most PCL injuries are successfully treated nonoperatively.2 Refractory injuries (symptomatic grade III injuries) or multiligamentous injuries are often treated with surgery.3, 4, 5 PCL reconstruction is one of the most challenging procedures, with the literature having described many techniques for reconstruction6 (ie, tibial tunnel technique, tibial inlay technique, single-bundle technique, double-bundle technique, remnant-sacrificing technique, and remnant-preservation technique). Recent advances in implants and instruments including retro-reamers (FlipCutter; Arthrex) and adjustable-loop devices (TightRope; Arthrex), as well as the development of the graft-link technique, allow us to perform reconstruction using sockets instead of tunnels.7,8
We describe a technique using a graft-link construct through the anteromedial (AM) portal for all-inside PCL reconstruction with remnant preservation that protects the graft from the “killer turn” of the tibia by smooth passage of the graft over the remnant and improves proprioception, thereby reducing postoperative pain and morbidity and achieving excellent functional outcomes.
Surgical Technique
Patient Positioning
The patient is operated on while under spinal anesthesia in the supine position; the affected knee hangs from the side of the operating table and remains in 90° of flexion throughout the surgical procedure (Video 1).
Graft Harvest and Preparation
A padded tourniquet is applied, and PCL laxity is appreciated clinically. Arthroscopic confirmation (sloppy anterior cruciate ligament [ACL] sign) is performed using a 30° arthroscope after standard anterolateral and AM portals are created. An isolated semitendinosus graft is harvested and quadrupled to achieve an 8-mm thickness, and a graft link is created using 2 adjustable loops on each side (Fig 1, Video 1). A graft length of 8 cm is achieved. Because remnant preservation is planned, a graft thickness of 8 mm is considered adequate to avoid overstuffing and allow smooth passage of the graft. The planned intraosseous socket length over the femoral side is 15 mm, with 30 mm on the tibial side.
Fig 1.
Quadrupled semitendinosus (Semi-T) graft-link construct, with graft thickness of 8 mm and graft length of 80 mm.
Arthroscopic Approach
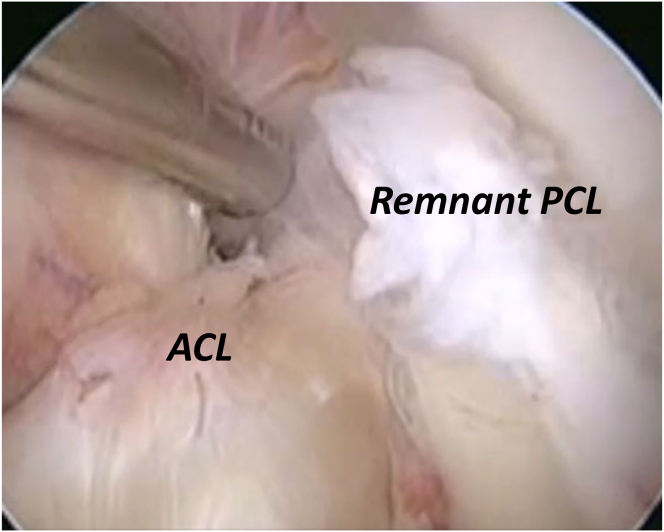
For improved visualization, 2 windows are created: one between the ACL and the remnant PCL (lateral window) and the other between the remnant PCL and the medial femoral condyle (medial window) (Fig 2, Video 1). The posteromedial (PM) portal is created in standard fashion by use of a spinal needle and switching stick through the medial window (Fig 3). A shaver is introduced through the PM portal, and adhesions from behind the remnant PCL are released. Similarly, viewing from the PM portal and bringing the shaver and radiofrequency probe from the AM portal, the surgeon removes adhesions from the remnant PCL; thereby, a clear cleavage plane is developed to protect the neurovascular structures during creation of the tibial retro-socket. The endpoint of clearance is achieved when reaching underneath the popliteus muscle (Fig 4). The FlipCutter retro-reamer is used for socket creation.
Fig 2.
Arthroscopic view of left knee showing creation of medial window (between remnant posterior cruciate ligament [PCL] and medial femoral condyle) and lateral window (between anterior cruciate ligament [ACL] and remnant PCL).
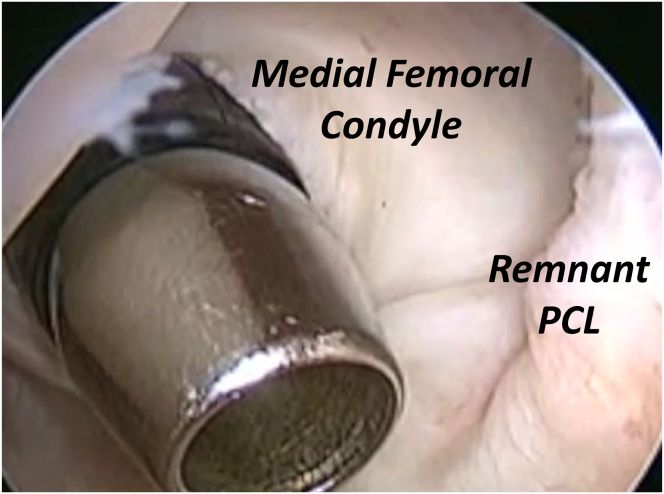
Fig 3.
Arthroscopic view of left knee showing creation of posteromedial portal through medial window between remnant posterior cruciate ligament (PCL) and medial femoral condyle.
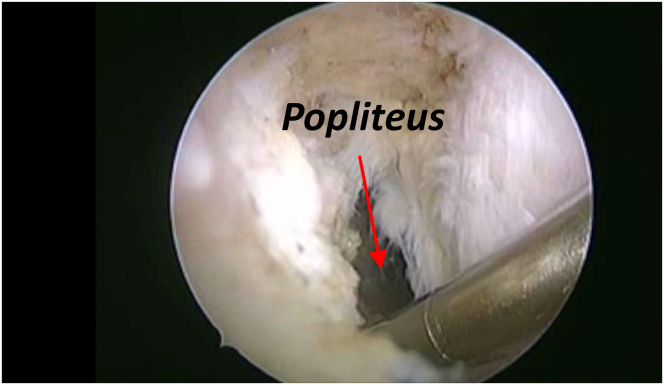
Fig 4.
Identification of popliteus as final level of clearance of adhesions (with posteromedial portal as viewing portal and anteromedial portal as working portal).
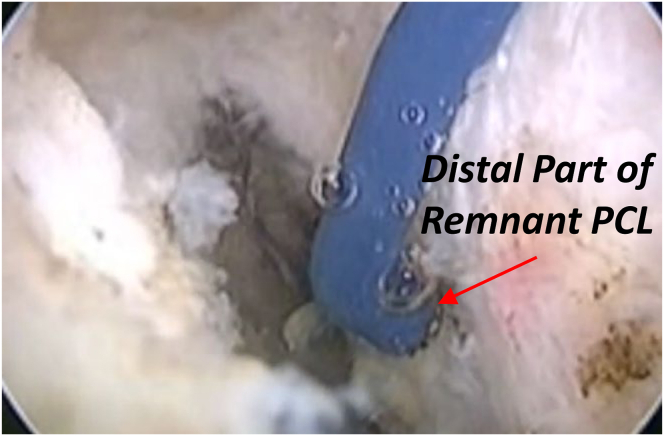
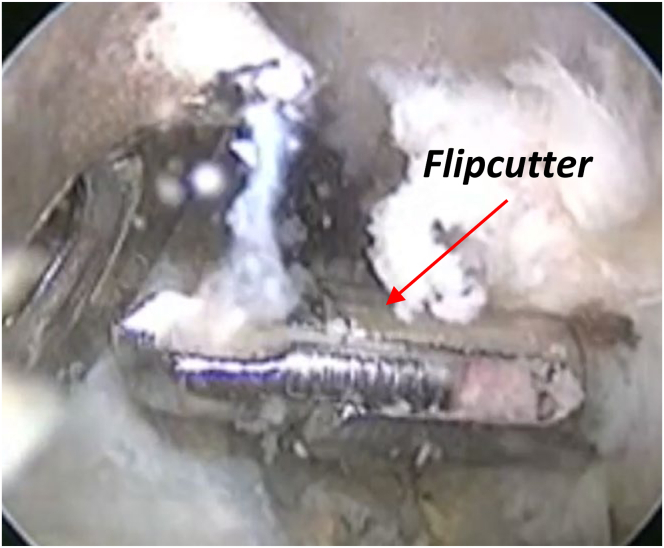
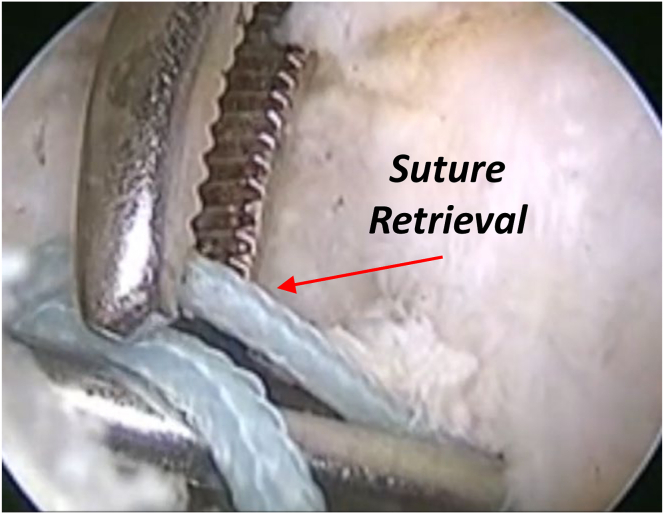
The tibial exit point of the FlipCutter is marked by identifying the distal-most part of the remnant PCL tissue to avoid damage to the native PCL (Fig 5). The tibial zig is inserted through the lateral window and kept over the mark; the FlipCutter is introduced (Fig 6) and flipped flush with the bone, followed by the creation of a tibial socket 30 mm in size. A Beath pin along with No. 2 FiberWire (Arthrex) is passed through the socket and retrieved through the lateral window in the anterior compartment (Fig 7).
Fig 5.
Arthroscopic view of left knee showing marking of distal part of remnant posterior cruciate ligament (PCL) as tibial footprint of graft.
Fig 6.
Arthroscopic view of left knee showing FlipCutter and tibial jig for creation of tibial retro-socket.
Fig 7.
Arthroscopic view of left knee showing retrieval of suture from lateral window between anterior cruciate ligament and remnant posterior cruciate ligament.
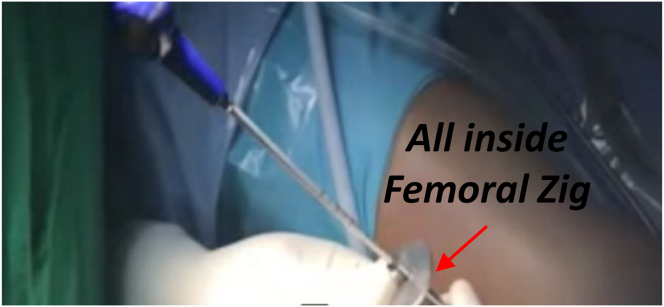
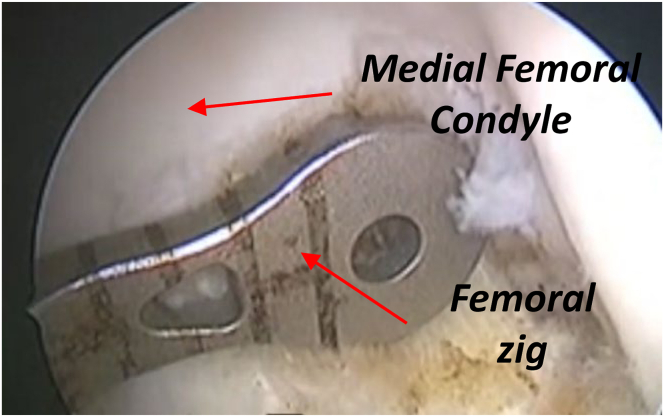
The PCL femoral retro-socket is prepared using an all-inside femoral zig (Fig 8). Initially, the PCL femoral point is marked, the PCL femoral zig is placed over the mark (Fig 9), and the retro-reamer is passed through the zig from outside into the joint. The retro-reamer is flipped, and creation of the retro-socket is achieved once retro-reamer is flush with the bone. A femoral retro-socket 15 mm in size is created. After clearance of debris, a Beath pin along with suture is passed into the joint. To prevent the intertwining of suture, a PassPort cannula (Arthrex) is passed. First, the tibial leading suture is retrieved, followed by retrieval of the femoral suture outside.
Fig 8.
Intraoperative view of left knee showing creation of femoral retro-socket by all-inside femoral zig.
Fig 9.
Arthroscopic view of medial femoral condyle in left knee with placement of femoral zig close to articular cartilage.
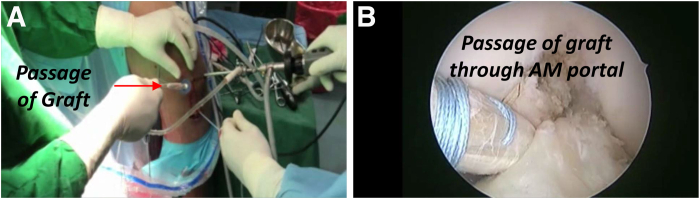
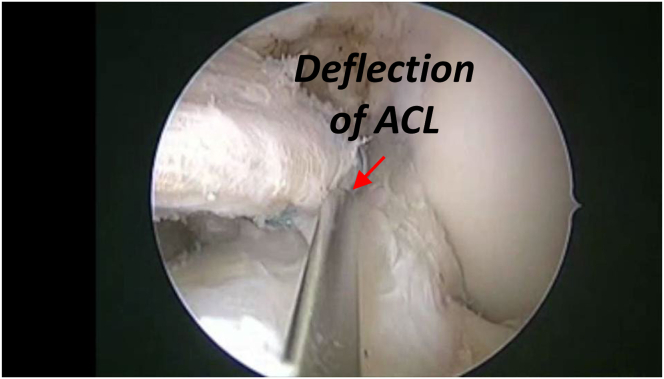
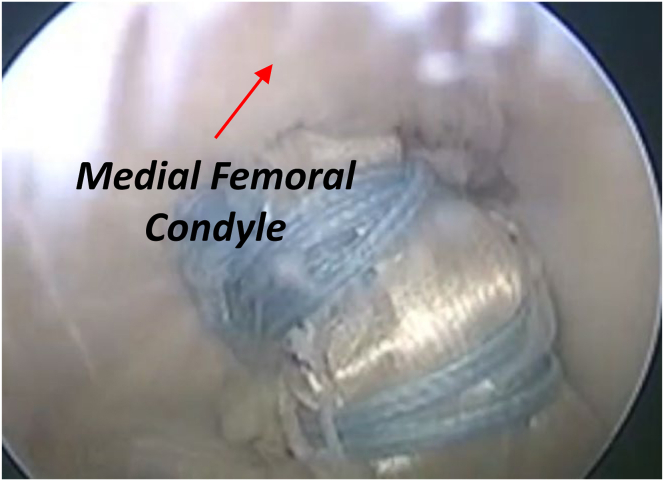
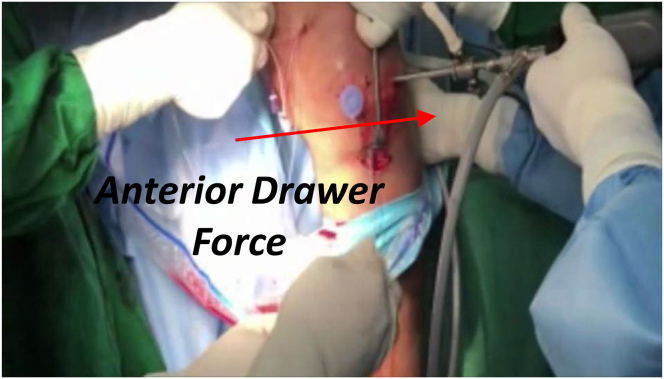
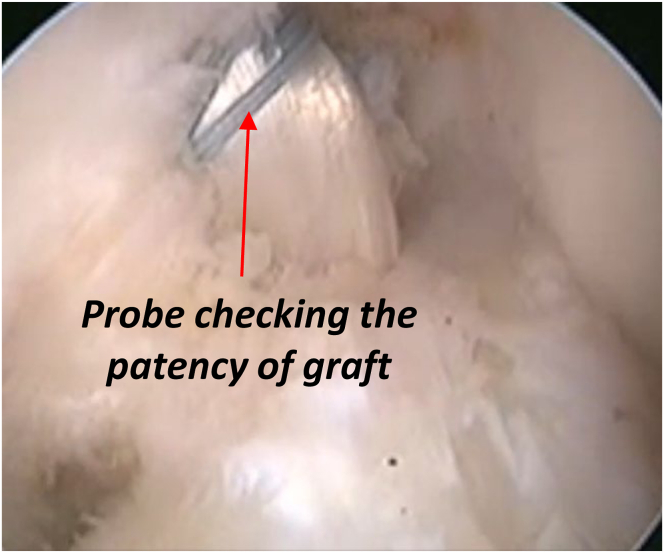
The adjustable-loop graft-link construct is loaded over the tibial leading suture and pulled inside; the tibial retro-socket is then taken outside. Through the AM portal, the graft is delivered inside the tibial retro-socket (Fig 10). The graft is passed by a toggling movement of the sutures and simultaneous deflection of the ACL with a probe (Fig 11). This allows the graft to slide over the remnant PCL. The quadrupled semitendinosus graft is placed over the native PCL remnant. Similarly, the femoral sutures along with the adjustable loop are pulled out of the femoral retro-socket until the EndoButton (Smith & Nephew) is delivered outside the cortex through the AM portal (Fig 12); again by a toggling movement, the graft is passed into the femoral socket and adequately tensioned. All of these steps are achieved under continuous vision through the PM portal. A strong anterior drawer force is placed on the tibial side until the tibial step-off is re-created, after which final tensioning of the graft is performed (Fig 13). Final patency and tension are assessed with a probe before closure (Fig 14).
Fig 10.
(A) Intraoperative view of passage of graft through anteromedial portal by PassPort cannula. (B) Arthroscopic view of left knee showing passage of graft through anteromedial (AM) portal by PassPort cannula
Fig 11.
Arthroscopic image of left knee showing passage of graft through lateral window with deflection of anterior cruciate ligament (ACL) with probe.
Fig 12.
Arthroscopic image of left knee showing passage of graft in femoral tunnel with outside toggling of femoral adjustable sutures.
Fig 13.
Intraoperative image showing simultaneous tensioning of graft on both femoral side and tibial side with anterior drawer force, thereby re-creating tibial step-off.
Fig 14.
Arthroscopic image of left knee showing assessment of final patency of graft with probe.
Postoperative Care
A knee brace with posterior tibial support is applied for 3 weeks, followed by passive range-of-motion exercises. Toe-touch weight bearing is started immediately postoperatively, with a progressive increment after 3 weeks. Sporting activities are restricted for 6 months.
Discussion
Arthroscopic PCL reconstruction is a technically demanding surgical procedure. Various technical challenges have been described in the past, which have led to the development of different techniques for its management.
Our technique for all-inside PCL reconstruction with remnant preservation has various advantages (Tables 1 and 2), in addition to the benefits of all-inside PCL reconstruction previously described by Adler3 and further substantiated by Vasdev et al.8 Because there is a risk of damaging the posterior neurovascular structures during the creation of tibial tunnels,7 retro-sockets are created using a FlipCutter to minimize this risk. The creation of retro-sockets preserves the intervening bone bridge and helps in achieving cortical fixation of the graft.8
Table 1.
Advantages of All-Inside PCL Reconstruction
| Bone-preserving surgery is achieved owing to the creation of sockets instead of tunnels. |
| Pain and morbidity are decreased. |
| The technique is ideal for multiligamentous reconstruction because it is a bone-preserving procedure. |
| The graft-link construct with suspensory fixation helps in tensioning the graft from both sides even after passage into the sockets. |
| Retrograde reaming with the FlipCutter avoids the risk of injury to the neurovascular bundle. |
PCL, posterior cruciate ligament.
Table 2.
Advantages of Remnant-Preserving PCL Reconstruction
| Passage of the graft over the remnant helps achieve a smooth excursion, thereby negating the killer-turn effect. |
| Only an 8-mm-thick graft is required; hence, semitendinosus graft alone suffices, which helps reduce morbidity. |
| Passage of the graft above the remnant helps achieve a better intra-articular length and preserves graft isometry. |
| The presence of mechanoreceptors in the remnant provides more proprioception, thereby allowing early rehabilitation. |
PCL, posterior cruciate ligament.
In our technique, the graft-link construct is passed above the PCL remnant, thereby aiding in smooth passage of the graft and avoiding the killer-turn effect. The graft is delivered through the AM portal, hence helping to achieve continuous visualization of graft passage into the sockets through the PM portal.
The limitations of our technique include inadequacy of graft thickness when using isolated semitendinosus graft, which can be overcome by gracilis supplementation (Table 3). There is a risk of intertwining of suture during retrieval, which is prevented by using a PassPort cannula (Video 1). Furthermore, there is a possibility of overstuffing owing to the presence of the remnant PCL; this is avoided by using 8 mm of graft as opposed to previously described techniques.8 To summarize, the described technique provides a reproducible way to perform all-inside PCL reconstruction with remnant preservation and graft passage via the AM portal, which has multiple advantages over previously described methods.
Table 3.
Limitations of Technique
| A smaller semitendinosus graft can result in a thickness < 8 mm when tripled; this pitfall can be overcome by combining gracilis with the graft. |
| There is a risk of intertwining of suture during retrieval, which is prevented by using a PassPort cannula. |
| There is a possibility of overstuffing of graft owing to the presence of the remnant PCL; this is avoided by using 8 mm of graft. |
PCL, posterior cruciate ligament.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
All-inside posterior cruciate ligament reconstruction with remnant preservation using anteromedial portal technique.
References
- 1.Campbell R.B., Jordan S.S., Sekiya J.K. Arthroscopic tibial inlay for posterior cruciate ligament reconstruction. Arthroscopy. 2007;23:1356.e1–1356.e4. doi: 10.1016/j.arthro.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 2.Kim S.J., Kim T.E., Jo S.B., Kung Y.P. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am. 2009;91:2543–2549. doi: 10.2106/JBJS.H.01819. [DOI] [PubMed] [Google Scholar]
- 3.Adler G.G. All-inside posterior cruciate ligament reconstruction with a GraftLink. Arthrosc Tech. 2013;2:e111–e115. doi: 10.1016/j.eats.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Slullitel D., Galan H., Ojeda V., Seri M. Double-bundle “all-inside” posterior cruciate ligament reconstruction. Arthrosc Tech. 2012;1:e141–e148. doi: 10.1016/j.eats.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matava M.J., Ellis E., Gruber B. Surgical treatment of posterior cruciate ligament tears: An evolving technique. J Am Acad Orthop Surg. 2009;17:435–446. doi: 10.5435/00124635-200907000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Prince M.R., Stuart M.J., King A.H., Sousa P.L., Levy B.A. All-inside posterior cruciate ligament reconstruction: GraftLink technique. Arthrosc Tech. 2015;4:e619–e624. doi: 10.1016/j.eats.2015.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGuire D.A., Hendricks S.D. Protection of posterior structures during transtibial tunnel creation for posterior cruciate ligament reconstruction. Arthroscopy. 2006;22:1254–1255. doi: 10.1016/j.arthro.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Vasdev A., Rajgopal A., Gupta H., Dahiya V., Tyagi V.C. Arthroscopic all-inside posterior cruciate ligament reconstruction: Overcoming the “killer turn.”. Arthrosc Tech. 2016;5:e501–e506. doi: 10.1016/j.eats.2016.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
All-inside posterior cruciate ligament reconstruction with remnant preservation using anteromedial portal technique.
All-inside posterior cruciate ligament reconstruction with remnant preservation using anteromedial portal technique.