Abstract
Biceps tendinopathy is a common cause of chronic anterior shoulder pain characterized by altered joint mechanics with considerable deficits in range of motion secondary to pain. The benefits of in-office nano-arthroscopy (IONA) include the ability to diagnosis and treat biceps tendinopathy, quicker patient recovery, reduced cost, and improved patient satisfaction. The purpose of this technical report is to describe the technique for performing IONA for biceps tendinopathy (biceps tenotomy/biceps tenodesis), with special consideration for obtaining adequate local anesthesia, proper indications, adequate visualization, and the advantages of performing these procedures in the office rather than the operating room.
Technique Video
Operative technique demonstrating in-office biceps tenodesis with nano-arthroscopy of the left shoulder. Patient is supine with the head of the bed at 70 degrees.
Biceps tendinopathy is a common cause of chronic anterior shoulder pain. Long head of biceps tendon (LHBT) pathology is often caused by tendon degeneration resulting from persistent inflammation or microtearing, tendon anchors disorders (SLAP lesions), and LHBT instability.1 Following failure of conservative management, biceps tenodesis and tenotomy are 2 surgical treatment options for relief of LHBT pathology.2 The gold-standard procedure for LHBT pathology is still widely debated, and both techniques have shown comparable results regarding pain reduction and functional improvements.3,4 Similarly, multiple techniques for long head of biceps (LHB) tenodesis have been described—including both open and arthroscopic with comparable results.5,6 Recent advances with in-office nano-arthroscopy (IONA) have allowed for wide-awake arthroscopic procedures in the office setting7, 8, 9, 10, 11, 12, 13, 14 without the need for either an operating room or anesthesiologists and resulting in high patient satisfaction with high rates of return to work and sport.10
Building on prior IONA designs, the system uses a 1.9-mm arthroscope with an optic chip at the tip of the camera with no inner-rod lenses. The scope and malleable sheath provide a durable construct that allows providers to visualize into the glenohumeral joint and to perform procedures under a local anesthetic in an office or bedside setting. Above all, the system produces an image that is similar in quality to conventional arthroscopy. Furthermore, this IONA technology includes various burrs, punches, graspers, scissors, probes, shavers, and resectors to permit direct intervention on identified pathology.
The purpose of the technical report is to describe a reproducible and effective biceps tenodesis method using IONA for the treatment of biceps tendinopathy with special consideration for obtaining adequate local anesthesia, proper indications, adequate visualization, and the advantages of performing these procedures in the office rather than the operating room (Video 1). Indications and contradictions of this procedure can be found in Tables 1 and 2. Additionally, a step-by-step guide can be found in Table 3.
Table 1.
Advantages and Disadvantages of the Proposed Technique
| Advantages | Disadvantages |
|---|---|
| Reduced operating room utilization, avoidance of anesthesia complications | Potential for patient pain or discomfort |
| Potential for true patient-physician education and shared decision-making | Learning curve |
| Potential for improved patient satisfaction | |
| Improved ability to diagnose anatomic variants compared to magnetic resonance imaging | |
| Reduced cost and resource utilization | |
| Less swelling and pain |
Table 2.
Pearls and Pitfalls of the Proposed Technique
| Pearls | Pitfalls |
|---|---|
| Patient selection is critical | Failure to provide adequate preprocedural local anesthesia or adequate time for anesthesia to take effect |
| At least 10 minutes between portal and intra-articular local anesthetic injection and procedure | Improper placement of trocar, leading to articular cartilage damage |
| Familiarity of office staff with room setup, instrument turnover, workflow | Poor indications of patients with excessive expectations |
| Thorough preprocedure discussion with patient in regard to mental readiness and expectations for wide-awake procedures | Inadequate time between local anesthetic and procedure |
| At least 10 minutes between portal and intra-articular local anesthetic injection and procedure | Poor portal placement given 0° needle scope |
| 5 cc of epinephrine in 1 L of normal saline for hemostasis and visualization |
Table 3.
Step-by-Step Guide to Performing the Proposed Technique
| Step 1: Position the patient comfortably seated on an examination table, with the back of the bed to set approximately 70° to 80° and the ipsilateral shoulder positioned so that the posterior, lateral, and anterior aspects of the shoulder are unobstructed (Fig 1). |
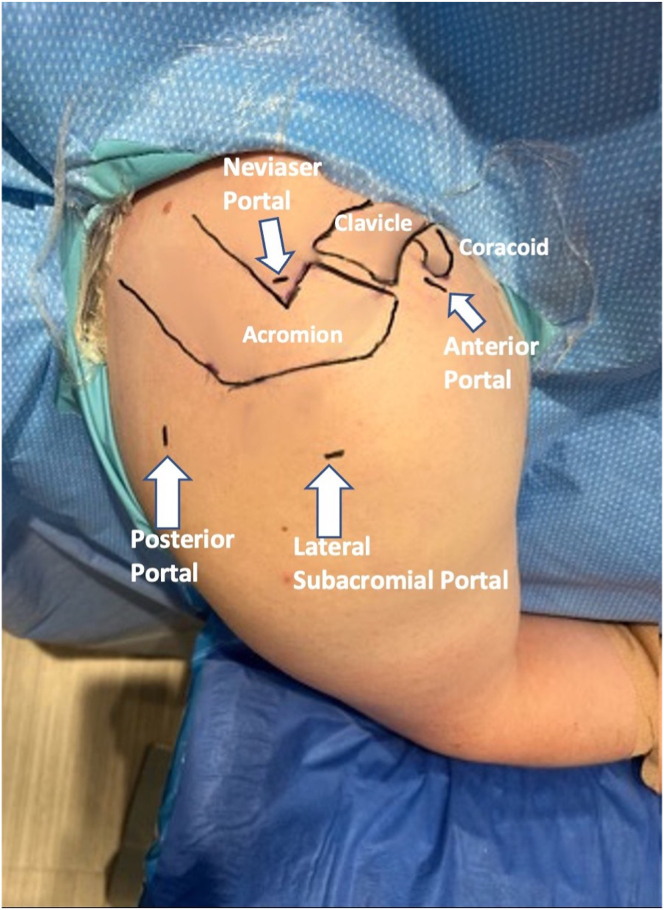
| Step 2: The ipsilateral arm should be supported on a padded mayo stand in slight forward flexion and abduction to allow for optimum entry in the glenohumeral joint. Mark out relevant surface anatomy and anticipated portals, including anterior, posterior, and lateral portals (Fig 2). |
| Step 3: Prior to the procedure, the planned arthroscopy portal sites are injected with 5 mL of a 1:1 ratio of 0.5 ropivacaine and 1% lidocaine with epinephrine. After 5 to 10 minutes, another 20 mL of a 1:1 ratio of lidocaine with epinephrine and ropivacaine is then used to infiltrate the joint one more time and establish that the portals can adequately gain access to the joint. |
| Step 4: A standard posterior arthroscopy portal is made using a No. 11 blade. A small 2-mm stab incision is made. |
| Step 5: Under direct visualization, the anterosuperior portal is established by passing a spinal needle just inferior to the biceps tendon in the rotator interval. A diagnostic arthroscopy is then performed using an 18-gauge spinal needle as both a probe and an outflow. Once confirmed that our anterosuperior portal site (working portal) is adequate, a small 3- to 4-mm stab incision is made. |
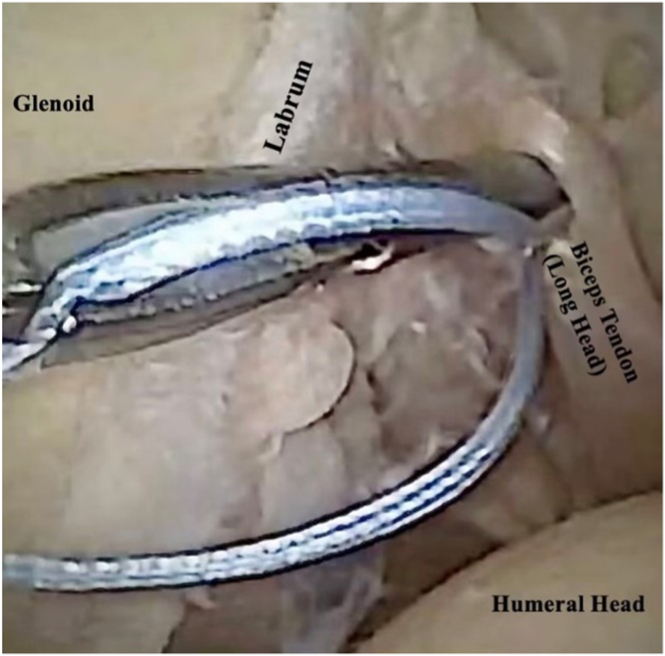
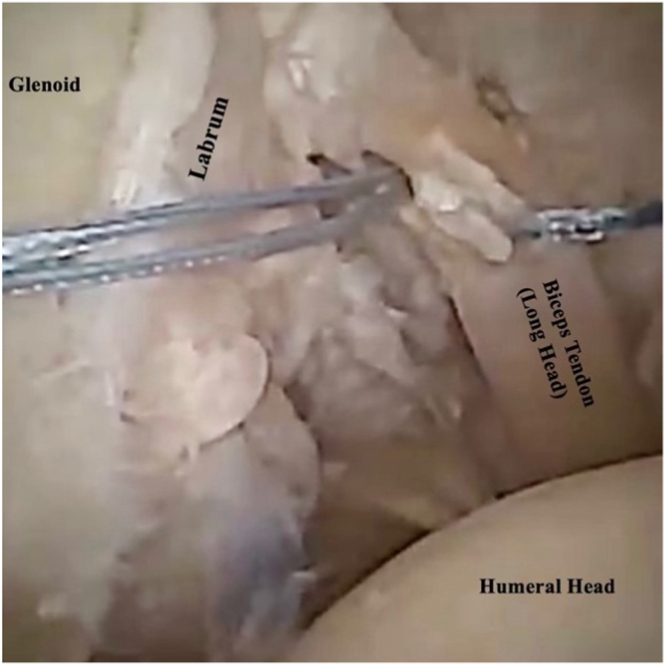
| Step 6: Using a 2.75-mm BirdBeak Suture Passer (Arthrex), a 1.3-mm SutureTape is passed through the biceps tendon approximately 1 to 1.5 cm (Fig 3) from the bicep-labral anchor and then again approximately 5 mm to 1 cm from the long head of biceps origin (Fig 4). |
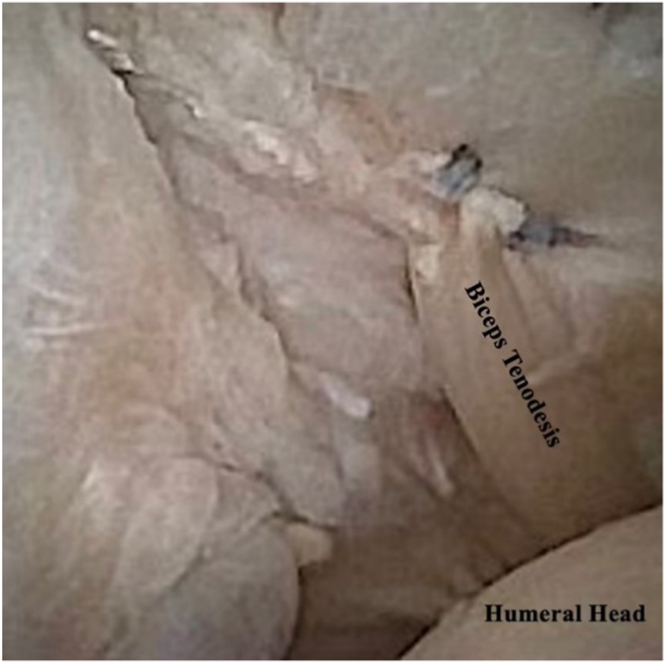
| Step 7: A nanobiter is then used to tenotomize the biceps tendon at its labral junction. |
| Step 8: A 2.0-mm shaver can then be used to shave down any remnant of the remaining bicep at its previous origin. |
| Step 9: Finally, the 2 limbs of the SutureTape are tied to the overlying shoulder capsule, at the level of the rotator interval, with an arthroscopic knot pusher—ensuring adequate cinching of the knot (Fig 5). |
| Step 10: Apply wound closure and soft dressing as indicated. |
Surgical Technique
Preoperative Planning/Positioning
With the back of the examination table positioned at approximately 70° to 80°, the patient is comfortably seated to mimic the beach-chair positioning. The ipsilateral shoulder is positioned so that the posterior, lateral, and anterior aspects of the shoulder are unobstructed (Fig 1).
Fig. 1.
An in-office nano-arthroscopy standard shoulder setup. With the back of the examination table positioned at approximately 70° to 80°, the patient is comfortably seated to mimic the beach-chair positioning. The ipsilateral shoulder (right) is positioned so that the posterior, lateral, and anterior aspects of the shoulder are unobstructed. The operative arm is rested on a well-padded mayo stand with arm in slight forward flexion and abduction. This positioning will help facilitate entry into the glenohumeral joint.
Using sterile technique, the patient’s extremity is prepped, using a mixture of chlorhexidine gluconate with isopropyl alcohol and draped. The operative arm is supported on a padded mayo stand in slight forward flexion and abduction to allow for optimal entry into the glenohumeral joint. The relevant surface anatomy is marked out on the shoulder (Fig 2), including the anterior, posterior, and lateral portals.
Fig. 2.
The patient is in an upright, beach-chair position, with the bed set at approximately 70° to 80°. Using sterile technique, the patient’s extremity (right shoulder) is prepped, using a mixture of chlorhexidine gluconate with isopropyl alcohol and draped. Standard portal sites are marked with respect to relevant surface anatomy markings, which include the acromion, clavicle, and coracoid. The posterior portal, which is the primary viewing portal, is made approximately 2 cm inferior and 2 cm medial to the posterolateral border of the acromion. The anterior, working portal is made 1 cm laterally to the coracoid process.
Prior to the procedure, the planned arthroscopy portal sites are injected with 5 mL of a 1:1 ratio of 0.5 bupivacaine and 1% lidocaine with epinephrine. After 5 to 10 minutes, another 20 mL of a 1:1 ratio of lidocaine with epinephrine and ropivacaine is then used to infiltrate the joint one more time and establish that the portals can adequately gain access to the joint. In the case of subacromial impingement and the need for arthroscopic debridement, the subacromial space is also infiltrated with an additional 10-mL 1:1 ratio of lidocaine with epinephrine and bupivacaine. A 13-in. high-definition monitor with an integrated HDMI output to extend the video signal to the in-room display allows the patient to watch their procedure while their procedure and pathology is narrated in real time by the lead surgeon.
Portal Placement/Operative Technique
A standard posterior arthroscopy portal is made using a No. 11 blade. A small 2-mm stab incision is made to accommodate the 1.9-mm 0° nano arthroscope (NanoScope; Arthrex). A blunt trocar is then used to enter intra-articularly. The camera is exchanged over the trocar and connected to the integrated inflow and outflow fluid management system at a pressure of 35 mm Hg (DualWave; Arthrex). Fluid inflow consists of 1 L of 0.9% normal saline mixed with 5 cc of epinephrine. It is our experience that the addition of epinephrine allows for improved hemostasis and visualization. Under direct visualization, the anterosuperior portal is established by passing a spinal needle just inferior to the biceps tendon in the rotator interval. A diagnostic arthroscopy is then performed using an 18-gauge spinal needle as both a probe and an outflow. Once confirmed that our anterosuperior portal site (working portal) is adequate, a small 3- to 4-mm stab incision is made. A blunt trocar is then used to enter intra-articularly, then replaced by a probe.
Attention is then directed to the biceps tendon. Using a 2.75-mm BirdBeak Suture Passer (Arthrex), a 1.3-mm SutureTape is passed through the biceps tendon approximately 1 to 1.5 cm (Fig 3) from the bicep-labral anchor and then again approximately 5 mm to 1 cm from the LHB origin (Fig 4). A nanobiter is then used to tenotomize the biceps tendon at its labral junction. A 2.0-mm shaver can then be used to shave down any remnant of the remaining bicep at its previous origin. Finally, the 2 limbs of the SutureTape are tied to the overlying shoulder capsule, at the level of the rotator interval, with an arthroscopic knot pusher—ensuring adequate cinching of the knot (Fig 5).
Fig. 3.
This is an arthroscopic view of the left shoulder through the posterior portal. Through the anterior portal, using a BirdBeak suture passer, the SutureTape is first passed approximately 1 to 1.5 cm from the bicep-labral anchor. Through the anterior portal, the BirdBeak suture passer is then once again passed approximately 1 cm lateral to the biceps tendon, through the capsule, to retrieve the suture tape. The 2 limbs are tied over the capsule at the level of the rotator interval using an arthroscopic knot pusher.
Fig. 4.
This is an arthroscopic view of the left shoulder through the posterior portal. Through the anterior portal, using a BirdBeak suture passer, SutureTape is passed a second time approximately 5 mm to 1 cm from the long head of biceps origin. Through the anterior portal, the BirdBeak suture passer is then once again passed approximately 1 cm lateral to the biceps tendon, through the capsule, to retrieve the suture tape. The 2 limbs are tied over the capsule at the level of the rotator interval using an arthroscopic knot pusher.
Fig. 5.
This is an arthroscopic view of the left shoulder through the posterior portal, demonstrating tenodesis of the biceps tendon to the rotator cuff interval, followed by tenotomy at the long head of biceps origin. The portals can be sealed primarily using adhesive wound closure strips or with simple nylon sutures if the surgeon feels they are necessary. A dry, sterile dressing is applied that facilitates early shoulder range of motion.
Portals can be sealed primarily using adhesive wound closure strips (Steri-Strip; 3M) or with simple nylon sutures if the surgeon feels they are necessary. A dry, sterile dressing is applied that facilitates early shoulder range of motion.
Postoperative Protocol
Postoperatively, the patient is allowed to mobilize the joint as tolerated and given a sling for comfort. The patient is encouraged to come out of their sling on postoperative day 2 in order to mobilize their shoulder and prevent stiffness. Ice and elevation are encouraged for 24 to 36 hours. Acetaminophen and anti-inflammatories are sufficient for postoperative pain control. The patient returns on day 5 following the procedure. Formal physical therapy is started on day 5 postoperatively.
Discussion
Biceps tenodesis and tenotomy are 2 surgical procedures commonly performed during shoulder arthroscopy for the treatment of various pathologies of the LHBT, including tendinosis, tenosynovitis, complete or partial rupture, subluxation or dislocation, or SLAP tear.15 In this technical note, we describe the use of IONA for the treatment of biceps tendinopathy. This simple 2-portal technique has proved effective at allowing the senior author the ability to perform an in-office biceps tenodesis that is reproducible and safe for the treatment of anterior shoulder pain related to proximal biceps tendon pathology. Additionally, we have found that our cohort of patients is very interested in the procedure, experience virtually no pain, and feel that watching the camera feed is a positive experience.
With the advent of needle arthroscopy and improving technology, a multitude of techniques have been reported.16 Recently, Lavender et al.17, 18, 19 have demonstrated the versatility and functionality of nano-arthroscopy in the full operating room arthroscopy suite for both the knee and the shoulder. Similarly, in a recent technique guide, Peach et al.20 demonstrate the utilization of a wide-awake biceps tenotomy in the operating room. As opposed to the operating room, we have seen firsthand how integrating IONA into our practice has resulted in decreased patient morbidity, increased patient satisfaction, and high rates of return to sport and work when used appropriately.10,21 This has been further corroborated by the recent case series by Gauci et al.,22 who successfully performed an in-office needle arthroscopic biceps tenotomy under local anesthesia. Gauci et al.22 further concluded that needle arthroscopy confers several advantages over conventional arthroscopy, including that it facilitates confirmation or correction of radiologic diagnoses and permits evaluation of the intra-articular structures under direct vision.
As IONA becomes more widely available, several studies have demonstrated its benefit.10,16,18,21 Colasanti et al.,10 in their retrospective study, demonstrated that more than 94% of their cohort of patients undergoing IONA expressed a willingness to undergo the same procedure again, as they felt that being awake and coherent allowed them to ask questions and learn about their condition from the operative surgeon in real time. Furthermore, the authors demonstrated that IONA resulted in significantly higher accuracy, sensitivity, and specificity when compared to magnetic resonance imaging.10 The benefit of the 1.9-mm arthroscope, as opposed to the standard 4-mm arthroscope, is it reduces the risk of causing iatrogenic nerve injury and chondral damage when entering the joint.10 Additionally, the advantage of using a smaller scope allows less damage to the skin and subcutaneous tissue, reducing postoperative pain, and theoretically has the advantage of limiting bacterial entry and the potential subsequent infection.
Conclusions
With the latest advances in IONA technology, it has become possible to perform diagnostic and therapeutic procedures in the wide-awake office setting. Patients can now be active members of the procedures and learn about their pathology in real time, establishing a patient-physician relationship. Our patients have been pleased with their experience and highly satisfied. Furthermore, IONA has the potential to reduce cost and increased efficiency. The ability to treat biceps tendon pathology in the office provides a unique tool for orthopaedic surgeons.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.G.K. received support from Ohnell Family Foundation and Winston Fisher. J.G.K. is a consultant for Arteriocyte Industries (Isto Biologics) and Arthrex.
Supplementary Data
Operative technique demonstrating in-office biceps tenodesis with nano-arthroscopy
References
- 1.Wilk K.E., Hooks T.R. The Painful long head of the biceps brachii: Nonoperative treatment approaches. Clin Sports Med. 2016;35:75–92. doi: 10.1016/j.csm.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 2.Hsu A.R., Ghodadra N.S., Provencher M.T., Lewis P.B., Bach B.R. Biceps tenotomy versus tenodesis: A review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326–332. doi: 10.1016/j.jse.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 3.Castricini R., Familiari F., De Gori M., et al. Tenodesis is not superior to tenotomy in the treatment of the long head of biceps tendon lesions. Knee Surg Sports Traumatol Arthrosc. 2018;26:169–175. doi: 10.1007/s00167-017-4609-4. [DOI] [PubMed] [Google Scholar]
- 4.Belk J.W., Kraeutler M.J., Houck D.A., Chrisman A.N., Scillia A.J., McCarty E.C. Biceps tenodesis versus tenotomy: A systematic review and meta-analysis of level I randomized controlled trials. J Shoulder Elbow Surg. 2021;30:951–960. doi: 10.1016/j.jse.2020.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Golish S.R., Caldwell P.E., III, Miller M.D., et al. Interference screw versus suture anchor fixation for subpectoral tenodesis of the proximal biceps tendon: A cadaveric study. Arthroscopy. 2008;24:1103–1108. doi: 10.1016/j.arthro.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Werner B.C., Evans C.L., Holzgrefe R.E., et al. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: A comparison of minimum 2-year clinical outcomes. Am J Sports Med. 2014;42:2583–2590. doi: 10.1177/0363546514547226. [DOI] [PubMed] [Google Scholar]
- 7.Mercer N.P., Gianakos A.L., Kaplan D.J., et al. Achilles paratenon needle tendoscopy in the office setting. Arthrosc Tech. 2022;11:e315–e320. doi: 10.1016/j.eats.2021.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mercer N.P., Azam M.T., Davalos N., et al. Anterior talofibular ligament augmentation with internal brace in the office setting. Arthrosc Tech. 2022;11:e545–e550. doi: 10.1016/j.eats.2021.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colasanti C.A., Kaplan D.J., Chen J.S., et al. In-office needle arthroscopy for anterior ankle impingement. Arthrosc Tech. 2022;11:e327–e331. doi: 10.1016/j.eats.2021.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Colasanti C.A., Mercer N.P., Garcia J.V., Kerkhoffs G., Kennedy J.G. In-office needle arthroscopy for the treatment of anterior ankle impingement yields high patient satisfaction with high rates of return to work and sport. Arthroscopy. 2022;38:1302–1311. doi: 10.1016/j.arthro.2021.09.016. [DOI] [PubMed] [Google Scholar]
- 11.Kanakamedala A., Chen J.S., Kaplan D.J., et al. In-office needle tendoscopy of the peroneal tendons. Arthrosc Tech. 2022;11:e365–e371. doi: 10.1016/j.eats.2021.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dankert J.F., Mercer N.P., Kaplan D.J., et al. In-office needle tendoscopy of the tibialis posterior tendon with concomitant intervention. Arthrosc Tech. 2022;11:e339–e345. doi: 10.1016/j.eats.2021.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaplan D.J., Chen J.S., Colasanti C.A., et al. Needle arthroscopy cheilectomy for hallux rigidus in the office setting. Arthrosc Tech. 2022;11:e385–e390. doi: 10.1016/j.eats.2021.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen J.S., Kaplan D.J., Colasanti C.A., et al. Posterior hindfoot needle endoscopy in the office setting. Arthrosc Tech. 2022;11:e273–e278. doi: 10.1016/j.eats.2021.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Creech M.J., Yeung M., Denkers M., Simunovic N., Athwal G.S., Ayeni O.R. Surgical indications for long head biceps tenodesis: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:2156–2166. doi: 10.1007/s00167-014-3383-9. [DOI] [PubMed] [Google Scholar]
- 16.Burt J., Smith V., Gee C.W., Clarke J.V., Hall A.J. The role of outpatient needle arthroscopy in the diagnosis and management of musculoskeletal complaints: A systematic review of the Arthrex NanoScope. Knee. 2023;42:246–257. doi: 10.1016/j.knee.2023.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Lavender C., Lycans D., Sina Adil S.A., Berdis G. Single-incision rotator cuff repair with a needle arthroscope. Arthrosc Tech. 2020;9:e419–e423. doi: 10.1016/j.eats.2019.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lavender C., Lycans D., Kopiec A., Sayan A. Nanoscopic single-incision anterior labrum repair. Arthrosc Tech. 2020;9:e297–e301. doi: 10.1016/j.eats.2019.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lavender C., Flores K., Patel T., Berdis G., Blickenstaff B. Nanoscopic medial meniscus repair. Arthrosc Tech. 2021;10:e1943–e1947. doi: 10.1016/j.eats.2021.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peach C., Davies R., Phillips N. Wide-awake shoulder nanoscopic long head of biceps tenotomy. Arthrosc Tech. 2021;10:e909–e912. doi: 10.1016/j.eats.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mercer N.P., Samsonov A.P., Dankert J.F., et al. Improved clinical outcomes and patient satisfaction of in-office needle arthroscopy for the treatment of posterior ankle impingement. Arthrosc Sports Med Rehabil. 2022;4:e629–e638. doi: 10.1016/j.asmr.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gauci M.-O., Monin B., Rudel A., Blasco L., Bige B., Boileau P. In-office biceps tenotomy with needle arthroscopy: A feasibility study. Arthrosc Tech. 2021;10:e1263–e1268. doi: 10.1016/j.eats.2021.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Operative technique demonstrating in-office biceps tenodesis with nano-arthroscopy of the left shoulder. Patient is supine with the head of the bed at 70 degrees.
Operative technique demonstrating in-office biceps tenodesis with nano-arthroscopy