Abstract
Background
As developing countries experience the epidemiologic transition to chronic diseases, morbidity and mortality from stroke is expected to rise. Stroke and other non-communicable diseases are increasing in Ethiopia but prospective data are scarce and there are not enough data regarding the characteristics, risk factors and mortality of stroke.
Objective
Aimed at determining the risk factors, clinical profiles and treatment outcomes of stroke admissions in Ayder Comprehensive Specialized Hospital, Tigray, Ethiopia.
Methods
This is a prospective cross-sectional study of all adult stroke patients admitted over consecutive 12 months period in medical ward and ICU of Ayder Comprehensive sSpecialized Hospital, northern Ethiopia. Medical residents through a pre-designed questionnaire collected data. Monovariate analysis, bivariate analysis and multivariate analysis to control for confounder variables were done using software SPSS version 26. P < 0.05 was considered statistically significant.
Results
There were 272 stroke admissions to medical ward and ICU over the 1-year period. Stroke comprised 13.05% of total medical admissions. Ischemic stroke accounted for 62.9% of stroke admissions. Stroke in the young accounted for 14.7% of all stroke admissions. Hypertension was the most common risk factor identified, found in 51.8%. Diabetes mellitus and atrial fibrillation were the other common risk factors. The in-hospital mortality was 13.6%. The only independent predictor of mortality identified was presence of complications, AOR [95% CI] of 2.4 [1.4, 5.3], P-value of 0.028. Aspiration pneumonia was the most common complication.
Conclusion
This study showed a high burden of stroke among medical admissions in northern Ethiopia. Being the most common risk factor for stroke, the high burden of undiagnosed and untreated hypertension needs special attention and efforts on community awareness should be enhanced. The relatively higher mortality illustrates the need to establish stroke centers to enhance the quality of stroke care.
Keywords: ischemic stroke, hemorrhagic stroke, risk factors, mortality, northern Ethiopia
Introduction
As developing nations, such as Ethiopia, experience the health transition to chronic non-communicable diseases, the morbidity and mortality from stroke is expected to rise.1 In 2005, of the estimated 5.7 million global stroke deaths, 87% occurred in low and middle-income countries.2 The American Heart Association (AHA) reported in 2016, stroke accounted for 11.8% of total deaths and ranked as the second leading cause of death next to heart disease in 2013.3 First-time incidence of stroke occurs almost 17 million times per year worldwide, which is approximately one every 2 seconds.4
Non-communicable diseases (NCDs) are increasing in Ethiopia5 and other sub-Saharan African (SSA) nations, but prospective data are scarce. One of the major NCDs is stroke, which is usually classified under cardiovascular diseases, which are the most common NCDs. The patterns of medical admissions to a given institution can be used to study the morbidity and mortality of the community it serves and used as an input for better large community-based studies. The amount of available data on stroke characteristics, risk factors and predictors of mortality is very limited in Ethiopia.
Ischemic stroke is the commonest type of stroke, far more common than hemorrhagic stroke worldwide.6 However, there have been reports that there is a disproportionally high incidence of hemorrhagic stroke in nations of Africa and other developing nations.7 In a study done in Tikur anbessa hospital of Addis Ababa, Ethiopia, hemorrhagic stroke was the predominant type of stroke accounting for 55.3%.7 In addition, several prior studies done in Ethiopia reported unusually higher proportions of hemorrhagic stroke,7–9 suggesting that there may be distinctive factors affecting the dynamics of stroke in this population. However, this was not seen uniformly across other health institutions of Ethiopia where studies were done, where ischemic stroke was found to be rather more common10,11 even if the ratio of hemorrhagic stroke looks relatively higher than seen worldwide.
The common risk factors for stroke such as diabetes mellitus and hypertension are known to increase with age worldwide and so does stroke. However, in Africa, risk factors such as obesity, hypertension, diabetes mellitus, dyslipidemia, and chronic rheumatic heart disease tend to occur at younger ages than in many developed countries according to the WHO 2014 Africa Regional Health Report.12,13 In a retrospective study done in western Africa, the commonest risk factors were hypertension (84.3%), tobacco smoking (35.9%), and alcohol (31.4%).14 However, in a retrospective study done in our institution in 2016, 38.0% of patients had hypertension and 4.9% had diabetes, and most were not on any treatment and the incidence of tobacco smoking and alcohol was much lower.10 There is a scarcity of prospective studies assessing the risk factors of stroke in Ethiopia.
Our study’s aim is to bridge the gap in the lack of data concerning the contribution of stroke admissions in developing nations such as Ethiopia. We hypothesized that the contribution of stroke admissions is increasing and the mortality pattern is largely unknown. To the best knowledge of the authors, this is the first prospective study to assess stroke characteristics, risk factors and mortality not only in this hospital but also in northern Ethiopia. Hence, the main objectives of this study were to assess the characteristics and risk factors of stroke admissions in Ayder Comprehensive Specialized Hospital (ACSH) and the in-hospital mortality.
Methods and Materials
Study Area and Setting
The study was conducted in Ayder Comprehensive Specialized Hospital (ACSH), a teaching university hospital located in Mekelle. ACSH is located in Tigray region, the most northern part of Ethiopia. It is under the University of Mekele, College of Health Sciences that was established in 2008. It gives services to people from Tigray, Afar and neighboring Amhara regions with a catchment area of more than 10 million. It is the most advanced tertiary hospital in Tigray with around 500 inpatient beds.
The Department of Internal Medicine has more than 30 internists working under it. The department has 108 inpatient beds in two medical wards in addition to a medical ICU with 8 beds. The department provides outpatient services with its different subspecialty units. The hospital is equipped with a CT scanner and MRI. It has also Electroencephalogram (EEG), nerve conduction test, Echocardiography, stress ECG machines, Bronchoscopy, Spirometry, Upper and lower Gastrointestinal Endoscopy and Cardiac catheterization set up comprising primary coronary angiography and percutaneous coronary intervention (PCI). ACSH is a teaching hospital for both undergraduate and postgraduate students with some subspecialty training as well.
Study Design and Data Collection
This study was done prospectively on all stroke patients admitted to medical ICU and ward at ACSH from November 1, 2017 until October 31, 2018. It included only those with stroke admission of age 18 and above. Data were collected after development of a structured questionnaire. Medical residents collected the data, as they were part of the treating team, which was led by senior consultant physicians including a neurologist. Patients were followed as part of the routine treatment and data taken from the medical records after settling the final diagnosis. The final diagnosis was made by attending physicians in addition to consultations from a neurologist. None of the patients with ischemic stroke received thrombolytics (t-PA). The final diagnosis was recorded at patient discharge by the resident. A patient could have more than one problem and the major reason for the patients’ current admission was taken as final diagnosis and others as comorbidity.
Medical residents collected data for sociodemographic characteristics, final diagnosis, risk factors, comorbidities, duration of hospital stay, complications, outcome of hospitalization and status at discharge.
Inclusion Criteria
All patients above 18 years of age with a diagnosis of stroke.
Exclusion Criteria
Patients less than 18 years of age.
Patients with TIA (transient ischemic attack).
AV malformations.
Trauma (head injury).
Coagulation disorders.
Patients not admitted to ward or ICU.
Data Quality Control
A quality control system was in place together with recording data for all patients admitted starting from the initial study period. The resident using the questionnaire at the time of discharge or death recorded data. The investigating team then reviewed for accuracy all of the discharge information.
Discharge diagnosis and information was crosschecked weekly with the nurses’ discharge logs to ensure every eligible stroke patient was recorded. The residents and nurses of ACSH were communicated with regularly about the correct recording of final and comorbid conditions. The medical record was reviewed for any ambiguity.
Operational Definitions
Stroke
An episode of acute neurological dysfunction presumed to be caused by ischemia or hemorrhage, persisting ⩾24 h or until death.15 The diagnosis of stroke was made with CT scan/ MRI imaging or clinical diagnosis by the treating physicians, consultant seniors or neurologist.
Ischemic Stroke
A stroke caused by focal cerebral, spinal, or retinal infarction.15
Hemorrhagic Stroke
A stroke that happens due to bleeding to the brain parenchyma.
Risk Factors
Conditions which are known to cause or increase the possibility of developing stroke, which include diabetes mellitus, hypertension, smoking, dyslipidemia, atrial fibrillation, etc.
Comorbidity
A concurrent disease present in addition to the final/primary diagnosis.
Data Analysis
Descriptive analysis was done with percentage, frequency, pie chart, and graph for categorical variables. Combinations of measure for central tendency and measure of dispersion were used for description of continuous variables.
Independent predictors of death among stroke patients were identified using multivariable logistic regression. Odds ratio with 95% confidence interval and significance value was utilized to study association between death and its predictors. Statistical significance was defined as P-value < 0.05 and all tests were two-sided. Significance Goodness of fit (GOF) of the multivariable model was analyzed using Hosmer-Lemeshow test. Multicollinearity was analyzed using Variance Inflation Factor (VIF). Data were analyzed using SPSS version 26.
Ethical Considerations
Institutional Review Board of Mekelle University, College of Health Sciences provided ethical clearance (Ref No. ERC 1136/2017) as part of a study: pattern and causes of medical admissions, morbidity and mortality in Ayder hospital. This study complies with the Declaration of Helsinki. This article involves review of medical charts while patients were admitted and followed. Data were de-identified and stored in a password-secured computer. There is no cost to patients in the study and no compensation or consent was necessary to subjects as we were registering the findings from the patient chart before patients’ discharge. The study involved only data from medical reviews and there was no direct communication with patients. Ethics committee waived informed consent and the main reason for it was that as data were collected from medical reviews only, no direct contact with the patients occurred and some data were collected after discharge. In addition, there was no plan for intervention and there is no benefit or risk to the patients during the study.
Results
Demographic Characteristics
During the 1-year study period, there were 272 stroke admissions which were 13.05% of the 2084 total medical admissions in medical ward and ICU of Ayder Comprehensive Specialized Hospital. The majority (57.4%) of patients were females. Patients from urban areas were 146 (53.7%) and 126 (46.3%) were from rural areas. There were 6 patients (2.2%) with stroke under the age of 25 years (Table 1). Stroke in the young, which can be defined as stroke occurring under the age of 45 years, was seen in 40 patients which was 14.7% of all stroke. Stroke under the age of 65 years accounted for 47.5% of all stroke.
Table 1.
Demographic and Baseline Characteristics of Stroke Patients Admitted TO ACSH from November 1, 2018 - October 31, 2019
| Frequency (n=272) | Percent | 95% CI | ||
|---|---|---|---|---|
| Lower Limit | Upper Limit | |||
| Age Category | ||||
| <25 Years | 6 | 2.2% | 0.9 | 4.5 |
| 25–34 Years | 9 | 3.3% | 1.6 | 6.0 |
| 35–44 Years | 25 | 9.2% | 6.2 | 13.1 |
| 45–54 Years | 35 | 12.9% | 9.3 | 17.2 |
| 55–64 Years | 54 | 19.9% | 15.4 | 24.9 |
| 65–74 Years | 73 | 26.8% | 21.8 | 32.3 |
| 75 Years & above | 70 | 25.7% | 20.8 | 31.2 |
| Gender | ||||
| Male | 116 | 42.6% | 36.9 | 48.6 |
| Female | 156 | 57.4% | 51.4 | 63.1 |
| Residence | ||||
| Urban | 146 | 53.7% | 47.7 | 59.5 |
| Rural | 126 | 46.3% | 40.5 | 52.3 |
| Duration of Hospital Stay | ||||
| <= 5 days | 100 | 36.8% | 31.2 | 42.6 |
| 6–10 days | 102 | 37.5% | 31.9 | 43.4 |
| 11–15 days | 41 | 15.1% | 11.2 | 19.7 |
| >15 days | 29 | 10.7% | 7.4 | 14.7 |
| Number of Comorbidities | ||||
| No Comorbidity | 206 | 75.7 | 70.4 | 80.5 |
| One Comorbidity | 54 | 19.9 | 15.4 | 24.9 |
| Two or more comorbiditIES | 12 | 4.4 | 2.4 | 7.4 |
| Type of Stroke | ||||
| Ischemic stroke | 171 | 62.9% | 57.0 | 68.4 |
| Hemorrhagic stroke | 101 | 37.1% | 31.6 | 43.0 |
Ischemic stroke was the most common type of stroke with 171 patients, accounting for 62.7% of all stroke. Hemorrhagic stroke was seen in 101 patients (37.1%). Sixty-six patients (24.3%) had comorbidities (Table 1).
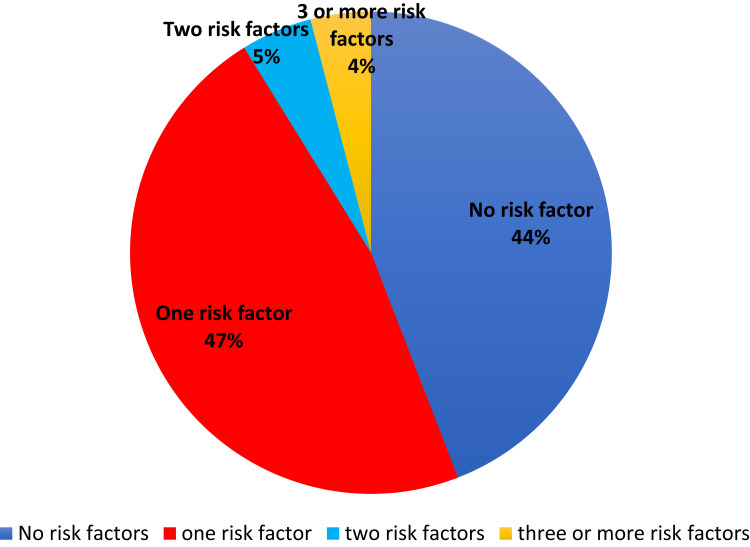
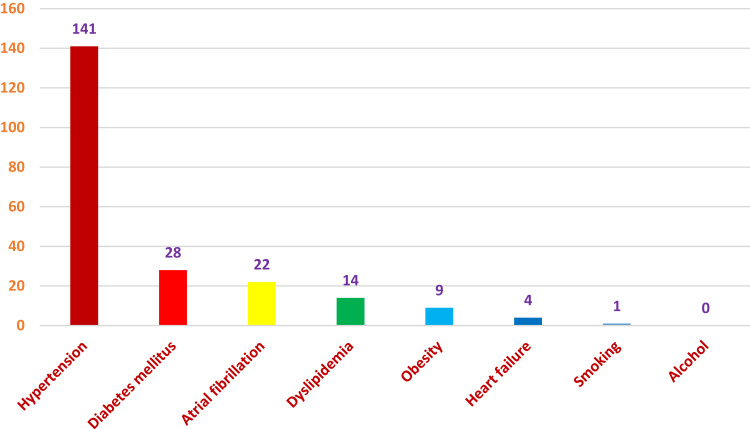
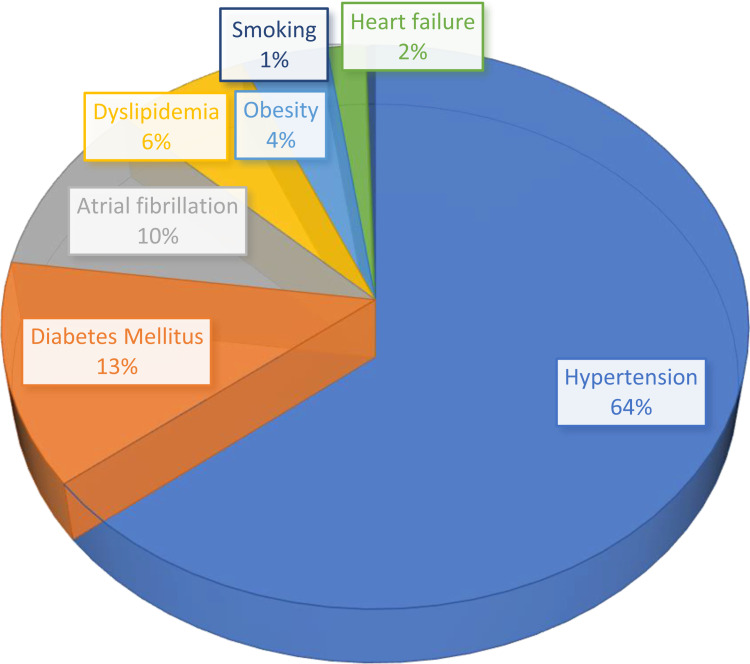
Most of our patients have at least one risk factor for stroke. Even excluding old age which can be a sole risk factor for stroke, 152 (55.9%) had at least one or more risk factors. 4.8% had two risk factors and 4.0% had high risk factors for stroke with at least three known predisposing factors (Figure 1). Without including the risk of old age on stroke, 120 (44.1%) patients, however, had no known other risk factors identified. The most common single risk factor in our patients was hypertension which was seen in 141 patients, which is 51.8% of all patients (Figure 2). Diabetes mellitus, atrial fibrillation, and dyslipidemia were the other common risk factors identified. On the contrary, our patients had an extremely low smoking, alcohol and other drug use history profile (Figure 3).
Figure 1.
Proportion of Risk factors among patients with at least one identified risk factor in ACSH.
Figure 2.
Numbers of identified risk factors in stroke patients admitted to ACSH, November 1, 2018 -October 2019.
Figure 3.
Identified risk factors among 272 stroke patients admitted to ACSH from November 1, 2018 -October 31, 2019.
Our study showed most stroke patients stay more than 5 days, with 63.3% staying for 6 days or more. 10.7% of all stroke patients stayed in the hospital for more than 15 days contributing highly to shortages of beds in the hospital. The mean length of inpatient stay was 8.6 (SD 6.1) and median of 7 days (IQR 7 days). Complications associated with either hospitalization or complications associated with disease progression occurred in 49 patients, 18% of all stroke patients. Aspiration pneumonia was the most common complication which was seen in 32 patients (11.8%) followed by hospital-acquired pneumonia and acute kidney injury.
Stroke in the Young, Subgroup Analysis
On separate analysis of patients with stroke in the young, which can be defined as stroke occurring in people with age <45 years, a total of 40 cases were seen over the 1-year period. Stroke in the young accounted for 14.7% of cases of all stroke admissions. It occurred among 19 male patients while 21 cases were females, with no significant difference statistically. The incidence of ischemic stroke (21 patients) was similar to those of hemorrhagic stroke (19 patients). Hypertension, likely secondary hypertension, was the commonest risk factor identified in those with stroke in the young, occurring in 19 patients out of the total 40 cases, 47.5%. The other relatively common risk factors identified were atrial fibrillation, seen in 5 patients (12.5%), diabetes mellitus (5 patients, 12.5%) and obesity which was seen in 3 patients, 7.5%. Heart failure without atrial fibrillation was seen in 2 patients, 5% and there was 1 patient with dyslipidemia. There were no patients with smoking and alcohol intake among these groups of patients. The in-hospital mortality rate among stroke in the young was 20%, 8 patients died of the 40.
In Hospital Mortality, Outcome and Discharge Condition of the Patients
The in-hospital mortality was 13.6%, there were 37 deaths from the total 272 patients. The mortality of hemorrhagic stroke (18.7%) appears to be higher than ischemic stroke (11.1%) but it was not statistically significant with AOR [95% CI] of 1.8 [0.9, 3.8], P-value of 0.108. The majority of patients (84.6%) were discharged from the hospital although there was a high proportion of patients who left against medical advice. There were 43 patients, which is 15.8% of all stroke patients, who left against medical advice which usually happens for many reasons including when patients deteriorate and family relatives opt for holy water as well as to decrease cost of the expensive transport of those who are deceased (Table 2).
Table 2.
Outcome and Complications of Stroke Patients Admitted to ACSH from November 1, 2018–October 31, 2019
| Frequency (n=272) | Percent | 95% CI of Percent | ||
|---|---|---|---|---|
| Lower Limit | Upper Limit | |||
| Outcome of Hospitalization | ||||
| Death | 37 | 13.6 | 9.9 | 18.1 |
| Discharge | 230 | 84.6 | 79.9 | 88.5 |
| Referred to better set-up | 2 | 0.7 | 0.2 | 2.3 |
| Transferred to continue same treatment | 3 | 1.1 | 0.3 | 2.9 |
| Condition at Discharge (n=230) | ||||
| Improved | 173 | 75.2 | 69.3 | 80.5 |
| Same condition | 14 | 6.1 | 3.5 | 9.7 |
| Left Against Medical Advice | 43 | 18.7 | 14.1 | 24.1 |
| Types of Complication | ||||
| No complications | 223 | 82.0 | 77.1 | 86.2 |
| Aspiration pneumonia | 32 | 11.8 | 8.3 | 16.0 |
| Hospital-acquired pneumonia | 3 | 1.1 | 0.3 | 2.9 |
| Acute kidney injury | 3 | 1.1 | 0.3 | 2.9 |
| Other complications of hospitalization | 2 | 0.7 | 0.2 | 2.3 |
| Electrolyte abnormalities | 1 | 0.4 | 0.0 | 1.7 |
| Other complications of disease progression | 4 | 1.5 | 0.5 | 3.5 |
| Complications from both Hospitalization & Disease progression | 4 | 1.5 | 0.5 | 3.5 |
Predictors of In-Hospital Mortality
Predictors of death among patients admitted with the diagnosis of stroke were identified by fitting binary logistic regression. During multivariable analysis, only complications were found to be significantly related with increased in-hospital mortality. Accordingly, in comparison to patients with no complications, the adjusted odds of death were 2.4 times higher in patients with complications of hospitalization and/or disease progression (Table 3). The final multivariable logistic model was a good fit for the data (Hosmer-Lemeshow test: χ2 (df=7, n=272) =11.0, p=0.139). There was no multicollinearity issue (maximum VIF= 1.05, mean VIF=1.03). Age and comorbidities were not significantly associated with increased in-hospital mortality.
Table 3.
Predictors of in-Hospital Mortality Among Patients Admitted with the Diagnosis of Stroke, ACSH, n=272
| Variables | Death, n (row %) | COR [95% CI] | AOR [95% CI] | P value | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Age in years | |||||
| ≤40 | 28 (82.4) | 6 (17.6) | 1 | 1 | |
| >40 | 207 (87.0) | 31 (13.0) | 0.7 [0.3, 1.8] | 0.9 [0.3, 2.5] | 0.847 |
| Gender | |||||
| Male | 98 (84.5) | 18 (15.5) | 1.3 [0.7, 2.7] | 1.4 [0.7, 2.9] | 0.354 |
| Female | 137 (87.8) | 19 (12.2) | 1 | 1 | |
| Comorbidity | |||||
| Yes | 53 (80.3) | 13 (19.7) | 1.9 [0.9, 3.9] | 2.0 [0.9, 4.4] | 0.074 |
| No | 182 (88.4) | 24 (11.6) | 1 | 1 | |
| Complication | |||||
| Yes | 37 (75.5) | 12 (24.5) | 2.5 [1.2, 5.6] * | 2.4 [1.1, 5.3] * | 0.028 |
| No | 198 (88.8) | 25 (11.2) | 1 | 1 | |
| Type of stroke | |||||
| Ischemic | 152 (88.9) | 19 (11.1) | 1 | 1 | |
| Hemorrhagic | 83 (82.2) | 18 (17.8) | 1.7 [0.9, 3.5] | 1.8 [0.9, 3.8] | 0.108 |
Notes: *(Bold text)- result showing significant association.
Discussion
As the first prospective study in the region, this study should provide valuable data regarding stroke burden, risk factors and in-hospital mortality, which have been missing dearly. This study was done in the largest hospital in northern Ethiopia but still lacking a stroke center and IV thrombolytics. In this study stroke accounted for 13.05% of all medical admissions. This admission rate was higher than findings from Gambia in which stroke patients constituted 5%,16 Sierra Leone (9.8%) as well as Nigeria in which stroke accounted for 4.5% of all medical admissions.17 Similar to our study, stroke admissions in Ethiopia constituted a higher burden than those African countries based on other studies done in Ethiopia, in Hawassa (13.7%) and Jimma (16.5%).8,14 The higher number of stroke admissions in Ethiopia might be due to lack of awareness on NCDs such as stroke, poor risk factor control especially poor follow up on hypertension and diabetes mellitus. Being a tertiary hospital-based study, referral bias also might increase the admission rate of stroke.
This study demonstrated that the commonest type of stroke even in a tertiary hospital of the region is ischemic stroke accounting for 62.7% of all stroke. This was similar with most studies done in Ethiopia10,18,19 and abroad;14,20 but against a study done in Tikur Anbessa Hospital (TAH), the largest hospital of the country, where one study showed predominance of hemorrhagic stroke.7 What should be emphasized here is that the proportion of hemorrhagic stroke in our setup is a lot higher than seen in most developed nations, where it accounts for only 20% of all strokes,6 but in our study it contributed for 37.3% of all stroke admissions. This high rate of hemorrhagic stroke is mainly due to the high prevalence of uncontrolled and unknown hypertension in the country, as our study also showed the most common risk factor identified being hypertension. Being a tertiary hospital, an associated referral bias also contributes for higher proportion of hemorrhagic stroke.
The commonest risk factor in our study was hypertension by far which was present in 51.5% of all stroke patients, this is in line with most prior studies in Ethiopia7,10 and other African studies.14 In those studies, hypertension was seen in 69% of all stroke patients in one study in Ethiopia, 85% in Sierra Leone14 and 48% in India.21 The increasing conditions of diabetes mellitus and atrial fibrillation contributed to only around 10% each which is lower than seen in studies done in other parts of Africa and the world.6,14,21 Alcohol use and tobacco smoking as a risk factor was very much lower in our patients, much lower than seen in other studies done in Africa and India,21 where tobacco chewing (26.01%), smoking (19.51%), and dyslipidemia (8.94%) were relatively common. However, similar to our study, hypertension, diabetes mellitus and atrial fibrillation were the three most common risk factors identified in other studies done in Ethiopia;7 whereas hypertension and tobacco chewing and smoking were the three commonest in India.21
The mean and median length of stay in our study is found to be shorter than seen in most African studies.14,17 The median length of stay of 7 days was shorter than 10 days in Sierra Leone and 10–19 days in many African studies14,17 even if one study in Ethiopia showed a shorter stay with 5 days.19 The relatively shorter length of stay in our study may be due partly to the early mortality after admission and the relatively earlier practice of patient transferral to nearby hospitals.
The in-hospital mortality was 13.6% which is lower than studies done in Ethiopia and the rest of African countries. In-hospital mortality was 21.6% in Jimma, Ethiopia and a lot higher in western African countries such as Sierra Leone (34.8%) as well as Asian countries such as Kazakhstan (37%). Similar to our study, a meta-analysis showed the in-hospital mortality was lower in eastern African countries (15%) than seen in Western Africa (37%) and Southern Africa (18%).22 The mortality rate in our study was similar to a previous study done in the same hospital a few years ago where it was 12.0%.10 The in-hospital mortality in our setup however is very high as compared with studies done in developed countries, the mortality was 7.13% in Spain to mention one.23 However, the relatively lower in-hospitality mortality in our study might be increased if we consider the high rate of patients who left against medical advice (15.8%), which is mostly comprised of severely ill and non-responding patients. As expected, aspiration pneumonia and other chest infections were the most common complications seen in our study which was also similar to most previous studies.10,14,19,23
Our study showed a slightly higher, though not statistically significant, in-hospital mortality with hemorrhagic stroke as compared with ischemic stroke. This is similar with a few studies done abroad where the mortality was similar across stroke types20 while more studies showed hemorrhagic stroke having a higher in-hospital mortality.10,14,22 Our study also shows a similar trend of increased mortality with hemorrhaging and with a larger sample it might be even more significant. Our study showed increased mortality with presence of complications during in-patient stay and this was similar in many previous studies14,19,20,22 and it was the expected finding. However, our study did not show significant increment of mortality with presence of comorbidities and this was similarly seen in previous local studies.19
Limitations of the Study
Even if this study is one of the few studies in this area regionally, it has also limitations. First, this study was not a large community-based study, rather it was a tertiary hospital-based study. It is known that a hospital-based study may not reflect an accurate picture of stroke as extremely critical patients die before hospitalization and mild cases may have not been admitted to hospital. Additionally, a hospital-based study is subject to referral bias. This referral bias, being a single set-up as well as a convenience sampling approach might not accurately reflect the burden and outcome of stroke in the community. Hence, extrapolations and generalization to the rest of the community should be done with caution. On the contrary, this pioneer prospective study in the region will give a clue about the actual magnitude of stroke and will be an input for future studies.
Finally, sample size was relatively small to assess some predictors of mortality and risk factors. However, this has the largest sample among studies done in the region and is bigger than most previous similar studies in the country. In addition, being the first prospective stroke study in Northern Ethiopia, this study would give valuable data to fill the gap and will encourage further community-based prospective cohort studies.
Conclusions and Recommendations
The epidemiologic transition from communicable diseases to non-communicable diseases in low-income countries such as Ethiopia poses a challenge to the health system, as it has long been more inclined towards communicable diseases. Hypertension is the commonest risk factor of stroke patients in our set-up as our study showed. The high burden of undiagnosed and untreated hypertension needs special attention; efforts on community awareness should be enhanced.
There is a relatively high mortality rate as well as excess numbers of patients who left against medical advice, which can be a reflection of the quality of the health care. Establishing stroke units, availing IV thrombolytics, increasing trained personnel (e.g. neurologists, neurosurgeons) as well as availing well-equipped instruments are very much needed to improve the health care and reduce mortality.
The health system of the country needs to be redirected to encourage health education focusing on NCDs at the public level. The health system needs to promote identification of lifestyle-related risk factors, include regular screening of NCD risk factors at all levels of care, and facilitate consistent and continuous follow up of chronic non-communicable conditions. Saying this, prospective community-based studies are needed to identify burden, risk factors and outcomes of stroke in the general population for a better intervention.
Acknowledgment
We are thankful to staff of the medical ward as well as ICU nurses and residents especially those who were involved in data collection and quality check for their support towards the success of this study. In addition to the patients who were admitted in the study period, we are also grateful to Mekelle University College of Health Sciences.
Funding Statement
Authors have received no funding for the preparation and/or writing of the manuscript.
Abbreviations
ACSH, Ayder Comprehensive Specialized Hospital; CT, Computed tomography; HS, Hemorrhagic stroke; ICU, Intensive care unit; IS, Ischemic stroke; MRI, Magnetic resonance imaging; MU, Mekelle University; NCD, Non-communicable diseases; TIA, Transient ischemic attack; WHO, World Health Organization.
Data Sharing Statement
Data ARE available from the corresponding author on accepted request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
We declare no competing interests.
References
- 1.Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746–2753. doi: 10.1161/hc4601.099487 [DOI] [PubMed] [Google Scholar]
- 2.Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6(2):182–187. doi: 10.1016/S1474-4422(07)70031-5 [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke Statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360. doi: 10.1161/CIR.0000000000000350 [DOI] [PubMed] [Google Scholar]
- 4.United Kingdom. State of the nation stroke statistics; 2016. Available from: https://www.stroke.org.uk. Accessed October 5, 2017.
- 5.Memirie ST, Dagnaw WW, Habtemariam MK, et al. Addressing the impact of noncommunicable diseases and injuries (NCDIs) in Ethiopia: findings and recommendations from the Ethiopia NCDI commission. Ethiop J Health Sci. 2022;32(1):161–180. doi: 10.4314/ejhs.v32i1.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120(3):439–448. doi: 10.1161/CIRCRESAHA.116.308413 [DOI] [PubMed] [Google Scholar]
- 7.Alemayehu CM, Birhanesilasie SK. Assessment of stoke patients: occurrence of unusually high number of haemorrhagic stroke cases in tikur anbessa specialized hospital, Addis Ababa, Ethiopia. Clin Med Res. 2013;2(5):94–100. doi: 10.11648/j.cmr.20130205.11 [DOI] [Google Scholar]
- 8.Deresse B, Shaweno D. Epidemiology and in-hospital outcome of stroke in South Ethiopia. J Neurol Sci. 2015;335(1):138–142. doi: 10.1016/j.jns.2015.06.001 [DOI] [PubMed] [Google Scholar]
- 9.Zenebe G, Alemayehu M, Asmera J. Characteristics and outcomes of stroke at tikur anbessa teaching hospital Ethiopia. Ethiop Med J. 2005;43(4):251–259. [PubMed] [Google Scholar]
- 10.Gebremariam Sennay A, Yang Hannah S. Types, risk profiles, and outcomes of stroke patients in a tertiary teaching hospital in northern Ethiopia. ENeurologicalSci. 2016;3. doi: 10.1016/j.ensci.2016.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agazhe M, Eshetu D, Arsicha A, et al. Incidence and pattern of stroke among patients admitted to medical ward at yirgalem general hospital, sidama regional State, Southern-Ethiopia. SAGE Open Med. 2021;9:1–7. doi: 10.1177/20503121211001154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mensah G. Epidemiology of stroke and high blood pressure in Africa. Heart. 2008;94:697–705. doi: 10.1136/hrt.2007.127753 [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization Regional Office for Africa. The health of the people- What works: the Africa regional health report 2014. World Health Organization; 2014.
- 14.Russell JBW, Charles E, Conteh V, et al. Risk factors, clinical outcomes and predictors of stroke mortality in Sierra Leoneans: a retrospective hospital cohort study. Anna Med Surg. 2020;60:293–300. doi: 10.1016/j.amsu.2020.10.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sacco RL, Kasner SE, Broderick JP, et al. A statement for healthcare professionals from the American heart association/American stroke association. Stroke. 2013;44(7):2064–2089. doi: 10.1161/STR.0b013e318296aeca [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walker RW, Rolfe M, Kelly PJ, George MO, James OF. Mortality and recovery after stroke in the Gambia. Stroke. 2003;34(7):1604–1609. doi: 10.1161/01.STR.0000077943.63718.67 [DOI] [PubMed] [Google Scholar]
- 17.Desalu OO, Wahab KW, Fawale B, et al. A review of stroke admissions at a tertiary hospital in rural southwestern Nigeria. Ann Afr Med. 2011;10(2):80–85. doi: 10.4103/1596-3519.82061 [DOI] [PubMed] [Google Scholar]
- 18.Fekadu G, Chelkeba L, Kebede A. Burden, clinical outcomes and predictors of time to in hospital mortality among adult patients admitted to stroke unit of Jimma university medical center: a prospective cohort study. BMC Neurol. 2019;19:213. doi: 10.1186/s12883-019-1439-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kefale B, Ewunetei A, Molla M, et al. Clinical pattern and predictors of stroke treatment outcome among hospitalised patients who had stroke at Felege Hiwot comprehensive specialized hospital, northwest Ethiopia: a retrospective cross-sectional study. BMJ Open. 2020;2020:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Viderman D, Issanov A, Temirov T, Goligher E, la Fleur P. Outcome predictors of stroke mortality in the neurocritical care unit. Front Neurol. 2020;11:579733. doi: 10.3389/fneur.2020.579733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patne SV, Chintale KN. Study of clinical profile of stroke patients in rural tertiary health care centre. Int J Adv Med. 2016;3:666–670. doi: 10.18203/2349-3933.ijam20162514 [DOI] [Google Scholar]
- 22.Siraj Mohammed A, Degu A, Alemayehu Woldekidan N, et al. In-hospital mortality and its predictors among stroke patients in sub-Saharan Africa: a systemic review and meta-analysis. SAGE Open Med. 2021;9:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kortazar‐Zubizarreta I, Pinedo‐ Brochado A, Azkune‐Calle I, Aguirre‐Larracoechea U, Gomez‐ Beldarrain M, Garcia‐Monco JC. Predictors of in‐hospital mortality after ischemic stroke: a prospective, single‐center study. Health Sci Rep. 2019;2:e110. doi: 10.1002/hsr2.110 [DOI] [PMC free article] [PubMed] [Google Scholar]