Abstract
Histotripsy is an emerging non-invasive, non-thermal, and non-ionizing focused ultrasound (US) therapy that can be used to destroy targeted tissue. Histotripsy has evolved from early laboratory prototypes to clinical systems which have been comprehensively evaluated in the preclinical environment to ensure safe translation to human use. This review summarizes the observations and results from preclinical histotripsy studies in the liver, kidney, and pancreas. Key findings from these studies include the ability to make a clinically relevant treatment zone in each organ with maintained collagenous architecture, potentially allowing treatments in areas not currently amenable to thermal ablation. Treatments across organ capsules have proven safe, including in anticoagulated models which may expand patients eligible for treatment or eliminate the risk associated with taking patients off anti-coagulation. Treatment zones are well-defined with imaging and rapidly resorb, which may allow improved evaluation of treatment zones for residual or recurrent tumor. Understanding the effects of histotripsy in animal models will help inform physicians adopting histotripsy for human clinical use.
Keywords: histotripsy, ablation, abdomen, liver, kidney, renal, pancreas, tumor
Introduction
Histotripsy is an emerging non-thermal, non-invasive, and non-ionizing focused ultrasound (US) therapy that can be used to destroy targeted tissue. In recent years, histotripsy devices have rapidly progressed from early laboratory prototypes to clinical systems being evaluated for use in humans. There is now an extensive body of preclinical work which demonstrates that histotripsy has the potential to non-invasively destroy tissue with a high degree of accuracy and precision. This manuscript is a summary of observations and results from large animal preclinical histotripsy studies in the liver, kidney and pancreas with particular emphasis on destruction of targeted tissue, tissue selectivity, side effects, and imaging findings. Understanding the bioeffects of histotripsy in in vivo large animal models should help inform physicians pursuing the translation of the technology for human clinical use.
The term histotripsy was coined at the University of Michigan in 2004 and comes from the Greek root words ‘histo’, meaning soft tissue, and ‘tripsy’, meaning breakdown. [1] Focused, high amplitude, short duration, low duty cycle US pulses are applied to target tissue to create high peak negative pressures. When pressures exceed a tissue-specific threshold, cavitation is produced which results in the rapid expansion and collapse of nanometer-scale endogenous gas bubbles, causing high stress and strain and eventual rupture of cell membranes. [1-4] This type of histotripsy is called “cavitation” or “cavitation cloud” histotripsy (intrinsic/shock-scattering mechanism) and contrasts boiling histotripsy which uses longer (1-10 ms) pulses and has a larger bubble cloud. [5] Boiling histotripsy pulses are still much shorter than those used in thermal High Intensity Focused Ultrasound (HIFU) and also results in non-thermal mechanical histotripsy. [6] More information regarding specific parameters of various forms of histotripsy can be found in this special issue by Williams et al. To destroy a targeted tissue volume with cavitation histotripsy, the focal point is swept through a pre-planned pathway using mechanical (micropositioners), robotic, or electronic (beam steering) methods. The result is a treatment volume that corresponds to the prescribed plan with millimeter-level accuracy and is composed of an acellular liquid homogenate consisting of extracellular fluid, cellular debris, and newly aggregated red blood cells. [7,8] Most in vivo abdominal studies and all human clinical trials to date have used cavitation histotripsy, which will be termed ‘histotripsy’ in this work, unless specifically denoted.
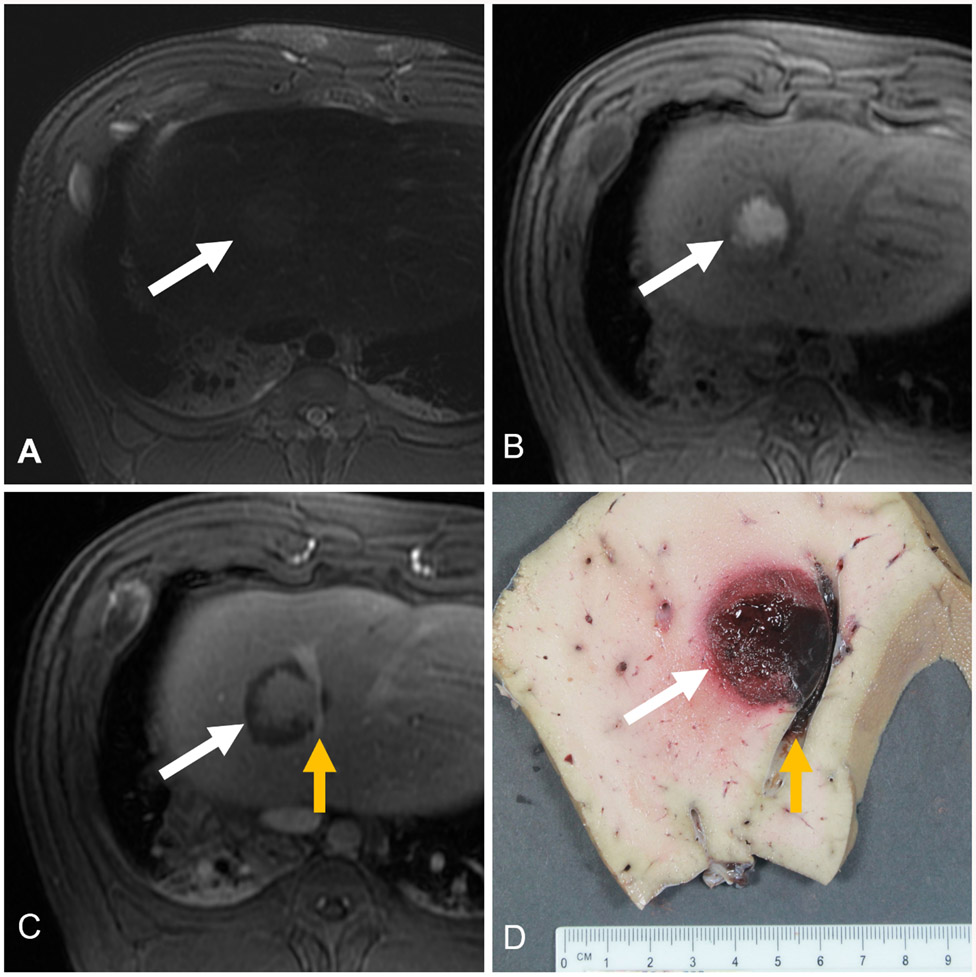
There are technical differences between histotripsy and other minimally or non-invasive ablation techniques (Figure 1). Histotripsy uses high-amplitude, short duration ultrasound pulses at a low duty-cycle to induce rapid expansion and collapse of microbubbles to cause mechanical destruction of cell membranes. The mechanical nature of cavitation histotripsy starkly contrasts the clinically used thermal based modalities of HIFU, microwave (MW), radiofrequency (RF), and cryoablation. HIFU is a focused ultrasound technique which uses long duration, relatively low-amplitude focused ultrasound pulses at a high duty-cycle to generate heat at the focal point, resulting in thermal destruction. [9-12] Microwave (MW) and radiofrequency (RF) ablation use percutaneous probes and different energy sources to heat tissue to temperatures >60 ° . [13-19] Cryoablation uses similar probes but instead destroys tissue through many freeze-thaw cycles (temperatures < −40°) which result in ice crystal formation, cell membrane rupture, and osmotic imbalances. [14,16,20] Histotripsy has potential advantages over these thermal ablation modalities. Although rare, severe side effects in thermal ablation can occur in adjacent anatomy due to heat diffusion, including bile duct strictures and chronic thrombosis of blood vessels during liver or pancreas treatments, as well as hydronephrosis and strictures in the collecting system and ureter during renal treatments. [21-29] Disadvantages of cryoablation are the lack of control of treatment zone, bleeding post procedure, and the potential for cryoshock, a life-threatening syndrome of multi organ failure and coagulopathy. [30,31] Finally, cavitation histotripsy differs from irreversible electroporation (IRE), which is a minimally invasive technique that uses low-energy, high-voltage electrical impulses to induce cellular apoptosis through electroporation. [32-34] The applied electric field alters the electrochemical gradient across cell membranes, forming instabilities and pores through which cell contents leak. [34,35] IRE also has disadvantages, including a frequent need to place multiple electrodes in precise patterns, synchronization with the cardiac cycle to avoid dysrhythmias, small irregular and unpredictable ablation zones, an inability to prescribe specific treatment sizes and shapes, and a higher disease recurrence with larger tumor volumes. [33,36,37]
Figure 1:
Histopathologic comparison of tissue destruction modalities. Differences in procedural application and mechanism of action between histotripsy, high intensity focused ultrasound (HIFU), microwave ablation (MW), radiofrequency ablation (RF), cryoablation, and irreversible electroporation (IRE) are illustrated in the pictograms under each modality. Histotripsy uses cavitation to mechanically destroy tissue. HIFU, MW, RF and cryoablation use thermal mechanisms to create coagulative necrosis and IRE uses electricity to disrupt the cell membrane potential. Pathologic differences are illustrated below each modality. Images have been reprinted with permission and license numbers can be found in the Acknowledgements section.
In addition to technical differences, cavitation histotripsy also has histopathologic differences from other ablation modalities (Figure 1). As stated, the treated zone with histotripsy is comprised of a homogenous acellular eosinophilic slurry or liquid with fragments of pyknotic cell debris and erythrocytes due to foci of hemorrhage. [7,38] Heat-based thermal tissue destruction (HIFU, MW, RF) occurs via coagulative necrosis which is characterized by protein denaturation and irreversible damage to cellular structures. [11,12,15,18,39-41] Microscopic analysis of the thermally ablated tissue generally shows maintenance of cellular shape and an intact membrane with reduced cytoplasmic detail, cytoplasmic hypereosinophilia and nuclear changes that include pyknosis (shrinkage/condensation), karyorrhexis (fragmentation), and eventually karyolysis (dissolution). In the peracute to acute phase of thermal destruction, tissue architecture is maintained, and histopathologic changes may be quite subtle, necessitating immunohistochemical staining to demonstrate non-viability (eg. Negative NADH staining). [42] Histotripsy differs pathologically from cryoablation, where instantaneous cell necrosis leaves remnants of cellular outlines, foci of cell loss and loss of cytoplasmic and nuclear detail with karyhorhexis. [16,43] Calcium deposition (dystrophic mineralization) is often encountered adjacent to or within the cryoablated region. With time, the ablated foci across modalities are generally rimmed by a pseudocapsule of granulation tissue, collagen with admixed inflammatory cells (neutrophils, lymphocytes, plasma cells and histiocytes). IRE treatment has maintained tissue architecture in the acute phase and later showing pyknosis, which is a characteristic feature of cells having undergone apoptosis. [35,44,45] Other cellular injuries such as swelling, vacuolation, and cytoplasmic eosinophilia have been reported, but in general, apoptosis occurs later which may make acute pathological confirmation of tissue destruction difficult in transitional zones at the edges of the ablated regions. [35] Similar to histotripsy, structures with abundant collagen, such as the ureter, bile ducts, and large blood vessels are relatively resistant to damage from IRE. [45-49]
Tissue selectivity is a potentially important feature of cavitation histotripsy. Different tissues have different intrinsic thresholds, which results in a dose-dependence of destruction. Anatomical structures with high collagen content such as large blood vessels, bile ducts and urothelial structures appear relatively resistant to damage from histotripsy due to high intrinsic mechanical strength (high Young’s Modulus) compared to parenchymal organs and most tumors. [4,50,51] The differences in the vulnerability of various tissues to cavitation can be exploited to preserve critical normal structures in and around the histotripsy treatment zone. Damage to collagenous structures can be achieved eventually with a higher dose (increasing number of pulses) compared to liver, kidney, or pancreas parenchyma. [4,50-52]
Although not yet tested in large animals, histotripsy appears to provoke activation of an immunologic response in small animal tumor models. The suggested mechanism of action is the release of non-denatured intracellular proteins and neoantigens due to the mechanical fracture of cell membranes. Early work in murine models suggests that this response is more robust than after external beam radiation or thermal ablation. [53-55] Histotripsy has also been shown to induce an increased immune recognition of abscopal tumors and may have synergy with checkpoint inhibitors. [53,54,56] Of note, IRE has been noted to create a potential immune response due to the lack of protein denaturation. [35,47] Further discussion of the immunological effects of histotripsy is provided in a separate issue in this volume (Imran KM, Cho CS, Allen CA).
Preclinical Histotripsy Studies in the Liver, Kidney, and Pancreas
Liver
The possibility of using histotripsy for treatment of liver tumors was first described at the University of Michigan in 2013 using an early prototype system and an in vivo swine model. [7] In this initial study, histotripsy was used to destroy small volumes of normal hepatic tissue safely, accurately, and reproducibly. [7] Since then, human-scale swine models have been used to assess histotripsy’s safety and efficacy [7,57-62], outcomes with and without anticoagulation [63,64], ability to treat across costal blockage [60,65], and tissue selectivity. [50] A list of the in vivo, large animal, transcutaneous liver histotripsy studies can be found in Table 1.
Table 1:
Summary of Large Animal Preclinical Transcutaneous Liver Histotripsy Studies in Swine
| Author | Year | Organ Treated |
Objective | Number of Swine |
Survival Period |
Size of Treatment |
Imaging Modality |
Imaging Findings | Conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Vlaisavljevich [7] | 2013 | Liver | Proof of concept | 6 | Acute (6 swine) | 1 cm cube (12 treatments) | MRI of ex vivo liver | Hyperintense lesion on T2 weighted MRI | Creation of non-invasive lesions with tissue selective properties was possible. |
| Vlaisavljevich [50] | 2014 | Liver | Tissue selectivity | 2 | Acute (2 swine) | 3 x 2 x 2 cm3 (1 treatment) and 3 x 3 x 2 cm3 (1 treatment) | MRI of ex vivo liver | T1 and T2 weighted images showed major hepatic vessels structurally intact inside of the treatment zone | Large vessels with increased mechanical strength are more resistant to treatment. |
| Kim [65] | 2014 | Liver | Transcostal treatment | 8 | Acute (8 swine) | 5 cm cube (8 treatments) | MRI of ex vivo liver and ribs | Hyperintense lesions on T2 weighted MRI. No damage to ribs | Transcostal hepatic treatment without aberration correction is possible. |
| Vlaisavljevich [63] | 2017 | Liver | Safety profile with and without heparinization | 22: 11 heparinized, 11-non heparinized | Acute (22) | Parenchyma: 5 x 3 mm rectangle (22 treatments) xVessel: single bubble cloud |
Parenchyma: Ultrasound Vessel: Doppler Ultrasound |
Parenchyma: Hypo-echoic lesions were observed in the treated regions for both groups Vessel: continuous blood flow, some with an altered flow pattern |
Treatment near and inside of large hepatic veins can be safely and effectively accomplished without systemic heparinization. |
| Smolock [57] | 2018 | Liver | Feasibility of creating a clinically relevant zone and 1 month survival study | 10 | Acute (3 swine), 28 Days (7 swine) |
3 cm sphere (10 treatments) |
MRI | Acute: -3/3 body wall injury -3/3 portal vein thrombus -1/3 hepatic vein thrombus -no bile duct injuries 28 Days: -1/7 body wall injury -6/7 portal vein thrombus -1/7 hepatic vein thrombus -no bile duct injuries -treatment volume decreased by 64% |
Destruction of liver tissue with clinically relevant treatment zone sizes are possible with sparing of vessels and bile ducts |
| Longo [58] | 2019 | Liver | Body wall damage mitigation | 6 | Acute (6 swine) |
3 cm sphere (6 treatments) |
MRI | -3/6 portal vein thrombus (2 were nonocclusive) -4/6 hepatic vein thrombus (3 were nonocclusive) |
Thermal injury to body wall can be mitigated with an altered pulse sequence. |
| Khokhlova* [62] | 2019 | Liver and Kidney | Feasibility and safety of boiling histotripsy for subcostal liver lesions | 6 | Acute (6 swine) | ~1 cm treatment zone | Ultrasound | -4/6 livers were treated -treatments showed homogenized voids and full liquefaction on histology -difficult to view treatments due to respiratory motion and US aberrations -3/4 livers had mechanical and thermal damage noted on the fatty layer of the body wall |
It was feasible to destroy liver and renal tissue with boiling histotripsy but some side effects were identified. |
| Longo [59] | 2020 | Liver | Altered treatment shape | 6 | Acute (6 swine) |
2.5 cm sphere (6 treatments), 2.5 cm ellipsoid (6 treatments) |
MRI | Treatment zones were slightly larger than prescribed in all dimensions. No adverse events reported |
Decreasing prescribed cranial-caudal diameter helps correct for effects of respiratory motion. |
| Knott [60] | 2021 | Liver | Transcostal treatment | 6 | Acute (6 swine) |
3 cm sphere (6 treatments) |
MRI | -5/5 intercostal muscle edema -4/5 portal vein thrombus (nonocclusive) -no bile duct injuries (one animal did not receive MRI) |
Transcostal hepatic treatments are safe and possible. |
| Knott [38] | 2022 | Liver | Comparison to microwave ablation | 14 (8 histotripsy, 6 MW) |
28 Days (14 swine) |
2-3 cm sphere (10 histotripsy treatments, 6 MW ablations) |
CT | Histotripsy: 7/8 portal vein thrombus (4 resolved by day 28), 0/8 hematoma, 0/8 galbladder injury. MW: 6/6 portal vein thrombus (none resolved), 2/6 hematoma, 1/6 gallbladder injury |
Histotripsy has a similar safety and efficacy profile to microwave ablation. |
| Thomas* [73] | 2022 | Liver and Kidney | Aberration Correction in Subcostal Treatment | 4 | Acute (4 swine) | Single boiling bubble (5 areas in liver, 3 in kidney) | Ultrasound | The acoustic power to create a boiling bubble was reduced by at least 45% with aberration correction compared to without aberration correction | Aberration correction effectively lowers acoustic power needed to achieve a boiling histotripsy bubble in vivo |
| Mauch [64] | 2023 | Liver and Kidney | Treatment with anticoagulation | 8 (all anticoagulated with warfarin) | 7 Day (8 swine) |
2.5 cm sphere (7 liver), 2 cm sphere (8 kidney) |
CT | Liver: No hemorrhage. 4/8 portal vein thrombus (3 resolved by day 7). Kidney: No hemorrhage. 3/8 transient hematuria, 2/8 urine leak |
No increase in bleeding risk in an anticoagulated swine |
denotes study done with boiling histotripsy
The safety and efficacy of cavitation histotripsy treatments in the liver has been explored in multiple preclinical animal studies. The initial feasibility study consisted of treating two 1 cm3 cubes in the liver of a porcine model and acutely showed successful fractionation of liver while preserving major vessels and the gallbladder. [7] To expand the clinical relevance, a proof-of-concept study was later performed with 3 cm spherical diameters, acute and chronic arms, and evaluation of body wall damage. [57] MR Imaging and histopathology demonstrated successful treatments with complete destruction of cellular hepatic parenchyma within the treatment zone. [57,59] The additional findings of this study (larger craniocaudal dimension of the treatment zone than planned, some local body wall damage, and vessel thrombi) laid the groundwork for the subsequent studies.
The first of Smolock et al’s additional findings was a significant difference in the diameter of the treatment zone in the craniocaudal dimension (elongation of up to 8 mm when creating a 3 cm sphere) from planned to actual in a porcine model, which was likely due to respiratory motion of the liver during treatment. [57] Respiratory motion has also posed difficulty when treating the liver with boiling histotripsy. [62] Avenues to overcome respiratory motion have been explored: use of robotic arm in ex vivo boiling histotripsy [66] and the change in the prescribed geometry [59] and use of high frequency jet ventilation in in vivo cavitation histotripsy. [67] Using a motion compensating robotic arm with skin tracking showed promising results to improve treatment size accuracy ex vivo. [66] In the in vivo study compensating for respiratory motion with geometry, a lens prescription with the short axis in the craniocaudal dimension (2.5 cm x 2.5 cm x 1.7 cm) resulted in a more spherical treatment than the sphere prescription, which created an ovoid shape with craniocaudal elongation as in prior studies. [59] Each prescription resulted in uniform tissue destruction within the treatment zone and there was no significant difference in transition zone from normal to treated tissue between the prescriptions. [59] More recently, high frequency jet ventilation (HFJV), which utilizes relatively rapid (~120 breaths/minute) low tidal volume breaths to minimize diaphragmatic movement and therefore decrease liver motion, has been trialed in swine with more spherical treatment zones achieved compared with conventional ventilation. [67]
The initial proof of concept study also reported local body wall damage (via MR imaging) immediately after treatment (3/3) and in 1/7 chronic animals. [57] Authors suggested the damage was due to a poor acoustic window and a nonoptimized prototype pulse sequence which resulted in pre focal energy deposition causing local heating. [57] To address this limitation, a subsequent study with an optimized pulse sequence to mitigate heat deposition and body wall injury was used to treat 3 cm treatment zones in the right liver. [58] With the optimized pulse sequence, there was no body wall damage (0/6) seen on MRI and necropsy. [58] Using the optimized pulse sequence, the same group explored the efficacy of a transcostal treatment, determining that clinical size treatments were possible with an increase in ultrasound power and increased time of energy delivery relative to subcostal treatments. [60] Although intercostal muscle edema was identified on post-treatment MRI, there was no histopathological evidence of injury to the chest wall. [60] Another transcostal study used subcutaneous thermocouples in a swine model and measured the temperature change when treating entirely transcostal with subsequent ex vivo imaging and pathology. Though there was no substantial increase in temperature nor rib damage with transcostal treatments, the prescribed treatment zone was smaller than a typical clinical treatment with any currently available modality by 5 mm3. [65] Therefore, although safe and feasible, the accuracy of treating beneath the ribs remains to be determined.
Finally, vascular thrombosis, particularly portal venous thrombosis, has been noted with histotripsy. The original clinical proof of concept study demonstrated portal vein (9/10) and hepatic vein thrombi (2/10) acutely post treatment, with all thrombi resolving during a 4 week follow-up period. [57] Similar acute results were found in the study with the pulse sequence optimized to mitigate body wall damage, where thrombi in the main portal vein (2/6, both nonocclusive), peripheral portal vein (1/6, distally occlusive), main hepatic vein (4/6, 1 occlusive), were seen. [58] However, since no chronic data was reported in this second study, the results currently suggest the majority of thrombi are nonocclusive and/or resolve. [57]
Although most in vivo histotripsy research focuses on destroying liver parenchyma, a porcine study was developed to determine the outcome of treating on or within a hepatic vein and if prophylactic heparin was necessary. [63] After 22 treatments involving hepatic veins of healthy swine, authors concluded that heparinization before treatment was not necessary to perform safe and effective treatments near hepatic vessels and also noted no significant bleeding events when heparinized. [63] Inversely, a porcine study was performed to determine if anticoagulation before a procedure would pose a challenge to abdominal histotripsy, as it does with other invasive ablation procedures. In this study, eight healthy swine were anticoagulated with warfarin and survived for 7 days post liver treatment. [64] No hemorrhage or hematoma was seen despite the treatment extending to or across the liver capsule in 5/7 cases and 6 of the swine having supratherapeutic warfarin levels on post-procedure day 7. [64] Portal vein thrombus was observed in 4/7 cases, where 3 cases resolved by day 7. [64] Notably, the liver and renal capsule were intact following treatment, presumably due to their collagenous architecture. [64] These reported anticoagulation results only refer to histotripsy treatment in abdominal organs and may not generalize to other areas of the body.
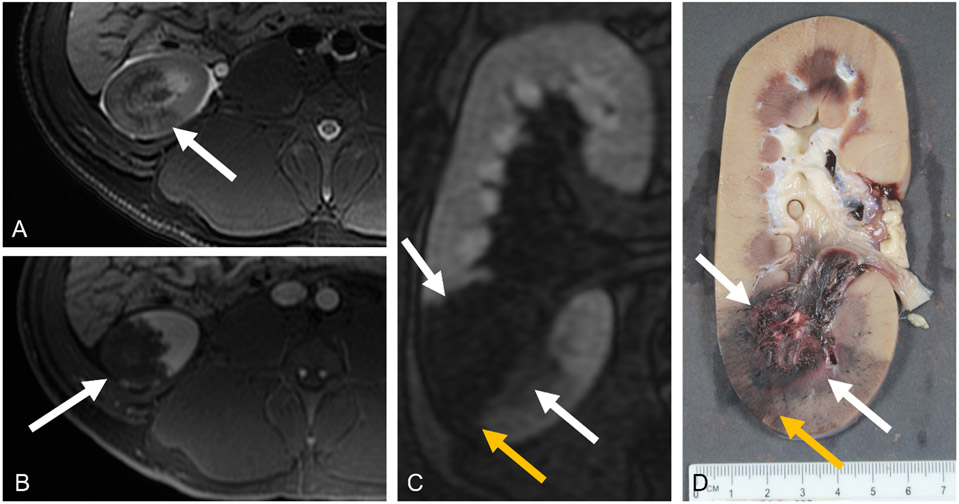
The lack of vascular damage or side effects with histotripsy demonstrate that large blood vessels, and other collagenous structures, such as intact bile ducts, are more resistant to histotripsy compared to other critical structures. [4,50,51] In a study of ten acute and chronic swine undergoing liver treatments, there was notable sparing of collagenous structures such as intact bile ducts traversing the treatment zone (2/2) on radiographic and histologic analysis. [57] Figure 2 shows a hepatic porcine treatment with post-treatment MRI and gross histology illustrating the tissue selective and tissue sparing nature of histotripsy. A varying degree of tissue selectivity may be leveraged depending upon the tissue properties of both the target tissue and the specific critical structure of interest. [4,50-52]
Figure 2:
MRI and gross pathology images of a histotripsy treatment (white arrows) in a porcine liver. A) Axial T2-weighted fat-saturated MRI following histotripsy of a healthy swine liver. B) Axial T1 weighted MRI before the administration of IV contrast. C) Axial T1 weighted MRI after the administration of a gadolinium-based contrast, shown in the portal venous phase. A patent vessel runs through the treatment zone (yellow arrow). D) Corresponding gross pathology of histotripsy treatment with patent vessel.
In the liver, the histotripsy treatment zone has been reported to involute. There was a 64% volume involution reported at post-treatment day 28 in a swine, which trends with other published work in a rodent model where near 100% involution was reported. [57,68,69] The rapid involution of treatment zones may be beneficial for assessing local treatment success and failures on follow-up imaging. In addition to cavitation histotripsy, wound healing from boiling histotripsy in rat livers was reported to follow normal wound healing of extracellular matrix remodeling, angiogenesis, and finally hepatocyte regeneration. [69] Immunologic effects of histotripsy for liver cancer have been recently explored in small-animal model experiments. Partial (goal of treating only 50-80% of the tumor) and complete histotripsy treatments have resulted in tumor regression and statistically significant improved survival outcomes in orthotopic rat hepatocellular carcinoma models. [70,71] Large-animal tumor models for histotripsy are being explored but have yet to become widely used. [72] For a detailed description of current knowledge on histotripsy immune effects readers are referred to another article within this issue (Imran KM, Cho CS, Allen CA).
Finally, the most recent safety study of histotripsy in a hepatic model compared it with the clinical standard of care, microwave ablation (MW). In this study histotripsy created more spherical treatment zones and demonstrated similar efficacy of tissue destruction compared to MW ablation. [38] There was less chronic damage to vessels and bile ducts created by histotripsy when compared to microwave ablation, particularly there was evidence for biliary damage in 0/8 histotripsy treatments and 5/6 microwave treatments. [38]
Boiling histotripsy has also been shown feasible in invasive and transcutaneous liver treatments. [61,62] Similar results to the above studies in cavitation histotripsy were reported: full liquefaction based on histologic analysis, some damage to the body wall, respiratory motion disruption of treatment zone, and US aberrations from the body wall. [62] Further work on boiling histotripsy to mitigate aberrations has also been done in vivo with success. [73]
Beyond liver tumors, histotripsy has been studied preclinically for disinfection of abdominal abscesses and decellularization of liver parenchyma for cell transplantation. [74-76] Even if drug resistant, bacteria are still susceptible to thermal and mechanical damage. Both boiling and cavitation histotripsy were used in a pilot study to treat abdominal abscesses in a porcine model. Authors found that histotripsy treatments were successful at decreasing the amount of bacteria colonies in these abscesses. [74] Boiling histotripsy has also been studied in vivo to decellularize a section of a porcine and rat livers to create a cavity for implantation of healthy hepatocytes. [75,76] Cells injected into this cavity proliferated and integrated into the recipient liver, highlighting this method for future cell therapy. [75,76]
Kidney
In addition to focal tumor treatments of the liver, renal applications are also promising. The first use of histotripsy in the kidney was reported by the University of Michigan in 2006 demonstrating the feasibility of using transcutaneous focused ultrasound to destroy renal tissue in a normal rabbit kidney. [77] Shortly thereafter, the same group studied the tissue pathological appearance after renal treatments in 29 rabbits at 0, 1, 2, 7, 21, 60 days. [78] The tissue transitioned from finely disrupted tissue with no cellular components (day 0) to a gradual inflammatory response with steadily decreasing area of cellular and architectural disruption and finally to a small fibrous scar by day 60. [78] To evaluate concerns of systemic spread of tumor from a mechanical treatment, the group at the University of Michigan performed a rabbit study of histotripsy in a VX-2 tumor model. This demonstrated that the number of metastatic lung lesions from a renally implanted tumor did not increase with histotripsy treatment. [79]
Although less in number compared with liver, human scale swine models have been used for renal histotripsy treatments. There are currently three preclinical studies evaluating the safety and efficacy of renal cavitation histotripsy in a human scale swine model. [64,80,81] The first was an evaluation of the efficacy and safety of renal histotripsy in a swine model [80], the second an evaluation of the safety of treatments in a swine model with anticoagulation [64], and the third a comparison study performed between cryoablation and renal histotripsy. [81]
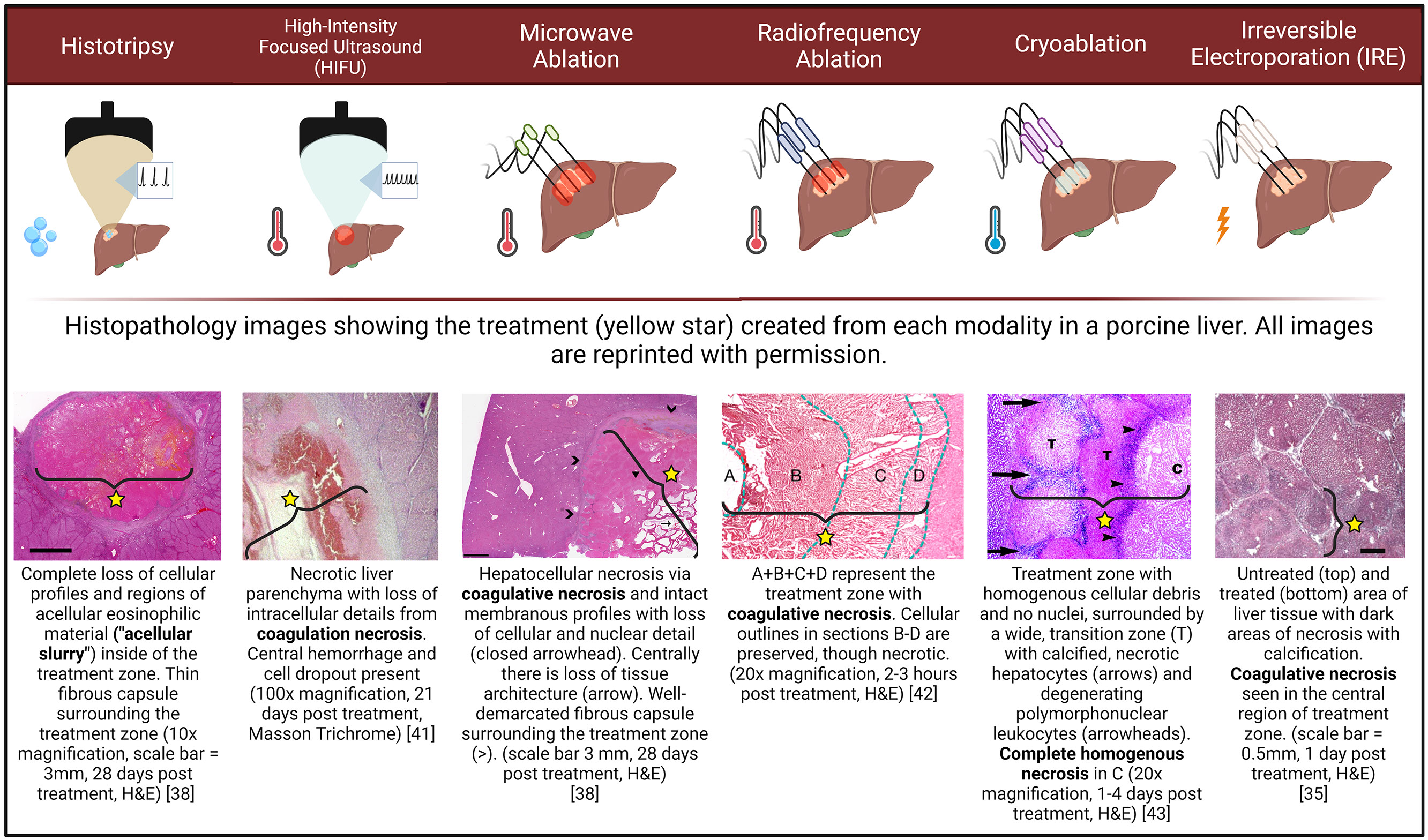
In the first feasibility study, renal histotripsy intentionally including the central collecting system was performed in acute and chronic porcine models. [80] There was complete histological destruction of the targeted renal parenchyma with predictable and spherical treatment zone sizes. [80] There was involution of the treatment zone over time (96% over 4 weeks), similar to that noted in the liver studies. Bilateral treatments were performed in a portion of the animals (n=4) demonstrating safety of this approach as there was no evidence of renal decompensation. [80] Temporary bladder and ureteral debris occasionally resulting in ureteral obstruction was noted in a small number of animals with this debris resolving by 1 week in each case. [80] Importantly, there was no urine leak, main vessel thrombosis, or mortality. [80] On CT imaging, histotripsy treatment zones in the cortical kidney were noted to be well demarcated and non-enhancing post contrast administration with small, peripheral wedge-shaped perfusion defects. [80] Similar results have been seen on MRI. Figure 3 illustrates a well demarcated wedge-shaped perfusion defect on a treated porcine kidney.
Figure 3:
MRI and gross pathology images of a histotripsy treatment (white arrow) in a porcine kidney. A) Axial T2-weighted fat-saturated MRI following histotripsy of a healthy swine kidney. B) Axial T1 weighted MRI with IV contrast (gadobenate dimeglumine) in the corticomedullary phase after treatment (white arrow). C) Coronal MRI with contrast 13 minutes after administering IV contrast. Note the wedge-shaped perfusion defect (yellow arrow) extending peripheral to the treatment zone (white arrows), causing the treatment zone to appear larger. D) Corresponding gross image demonstrating the central area of treatment (white arrows) with adjacent perfusion deficit (yellow arrow).
The second study evaluated the risk of hemorrhage from renal histotripsy in a warfarin anticoagulated swine model. Eight therapeutically anticoagulated swine underwent histotripsy treatments to the renal parenchyma and were survived 7 days post treatment while continuing anticoagulation. There were no cases of retroperitoneal hemorrhage, even with all eight treatments extending to the kidney capsule and 6/8 swine being supratherapeutic on warfarin at day 7. [64] The authors proposed that this finding may be explained by histologic mechanisms that involve endothelial injury of vessels at the periphery and within the treatment zone resulting in thrombosis. [64]
The third study is a comparison between renal histotripsy and a current clinical standard, renal cryoablation. [81] Similar efficacy, safety profile, and predictability of treatment zone size was achieved with histotripsy and cryoablation. Debris was noted in the collecting system of both treatment arms, 9/9 with histotripsy and 5/9 with cryoablation, without resultant obstruction. Additionally, more perirenal hematomas (8/9) were identified after cryoablation treatments than with histotripsy (1/9). [81]
Similar to the liver, histotripsy treatments in the kidney exhibited tissue selectivity. First described by Lake et al, there is a differential histotripsy treatment effect in the renal cortex versus collecting system when treating in-vitro renal tissue. [82] This aligns with histology from another paper, where there was patchy urothelium disruption in the ureter but no injury to underlying connective tissue. [80] Similar results were seen when treating the kidneys with boiling histotripsy. [62,83] The tissue selective properties of histotripsy may be useful for centrally located renal tumors and those adjacent to the ureter, locations challenging or not typically accessible with current ablation modalities. [84]
Pancreas
Recent studies have investigated the feasibility of histotripsy for the treatment of healthy pancreas and pancreatic tumors in both small and large animal models in vivo. [85] Results from histotripsy studies in an immunocompetent subcutaneous mouse model of pancreatic cancer showed that histotripsy could effectively ablate Pan02 pancreatic tumors and stimulate immune pathways through the release of tumor-associated proteins and DNA. [86,87] This work matches previous studies of histotripsy that have demonstrated effective ablation and immune-stimulation in multiple tumor types [53,54], and suggests that histotripsy may have multiple roles in the treatment of pancreatic cancer including ablation, palliation, immune-modulation, and enhancing drug delivery.
In addition to these feasibility studies in small animals, in vivo large animal swine models have been investigated for histotripsy ablation of the pancreas. [85,88] In one of these studies, the safety and feasibility of using histotripsy for the non-invasive ablation of the pancreas was tested in 11 healthy pigs using a custom 500kHz histotripsy transducer mounted on a prototype clinical histotripsy system. [88] Results from this study demonstrated that the pancreas could be successfully visualized and treated with histotripsy when the pigs were fed a specialty diet consisting of sweetened custard with simethicone and bisacodyl designed to minimize the intestinal contents and gas present on the day of treatment. To illustrate the importance of this diet to minimize intestinal gas, a separate group of pigs were fasted for 12 hours prior to histotripsy and were not fed the specialty diet. Ultrasound imaging of the pancreas was not feasible in any of these pigs.[88] Despite the lack of proper visualization of the pancreas on ultrasound prior to treatment, histotripsy was still performed and resulted in off-target injury to the intestines due to extensive pre-focal cavitation. In contrast, precise bubble clouds were safely generated in the pancreas of pigs that received the specialty diet without inducing any clinically relevant injuries to overlying tissue structures. [88] This finding matches prior clinical studies using thermal HIFU for the treatment of pancreatic cancer, which have shown a strong safety profile when applying HIFU through an acoustic window without gas blockage in the stomach and bowel. [89-92] It is also worth noting that four pigs in the initial histotripsy pig study were survived for 1-week post-treatment, with results showing that the treatments were well-tolerated with no signs of complications, behavioral changes, or changes in blood markers that might indicate other complications such as pancreatitis. [88] Additional studies are needed to confirm this finding in a larger number of animals and over longer time periods.
Ongoing work is underway to optimize histotripsy therapy methods for targeting the pancreas and to explore the differential thresholds for tissue selectivity to damage pancreatic tumors but preserve critical structures such as blood vessels, bile ducts, stomach, and bowel. Additional studies are needed to characterize these findings and develop improved computational models that can predict the level of tissue selectivity for specific clinical applications. [93]
Finally, the newest set of histotripsy studies on the pancreas has investigated the potential of histotripsy for treating pancreatic tumors in a novel SCID-like orthotopic pig tumor model. [94] This model, which grows human pancreatic tumors in the pancreas of immunocompromised pigs, has been used in initial pilot studies showing that histotripsy could effectively target and ablate pancreatic tumors in vivo, consistent with results from the healthy pig studies described above. [88,94]
Conclusion
Histotripsy is a non-invasive, non-thermal, non-ionizing focused ultrasound treatment that has benefits over previous minimally and non-invasive tissue destruction techniques by creating mechanical cell death versus thermal coagulative necrosis. preclinical work on the liver, kidney, and pancreas has spanned small and large animals through feasibility studies and tumor models. Although the liver has been most extensively studied both preclinically and clinically for tumor treatment with histotripsy, exploration of treatments in the kidney and pancreas are increasing. Preclinical studies have explored safety and efficacy of cavitation histotripsy treatments in abdominal organs through highly acoustic impeding structures, varying treatment sizes, with and without anticoagulation, and around critical structures. These important studies are instrumental to helping physicians understand the intricacies and nuances of histotripsy treatment in the abdomen which will lead to better clinical translatability and ultimately, patient care.
Acknowledgments
The pathology images were re-printed with permission (license numbers: 5518820073359, 5518820073359, 5518401223932, 5523070678784). The radiofrequency pathology image in Figure 1 was cited and reprinted with slight modifications under the Creative Commons Attribution License https://creativecommons.org/licenses/by/4.0/. Figure 1 was created using Biorender and published with agreement number JX25YLZX9E.
Funding
Research reported in this publication was supported by National Cancer Institute and National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health under award numbers R01CA262474 and R01EB031007, respectively. Funding support was received for author KF from the National Institute of General Medical Sciences under award number T32GM140935.
Footnotes
Disclosure Statement
Conflict of interest. Author PL is a consultant and stockholder with HistoSonics, Inc., a consultant with NeuWave/Ethicon, Inc., and receives research support from Siemens Healthineers. Author AS is a consultant and speaking faculty for NeuWave Medical, on the Advisory Board for AstraZeneca, a consultant for Varian, and advisor and shareholder of HistoSonics, Inc. Author EV is a consultant, stock- holder, and receives research support from HistoSonics, Inc. Author FL is a consultant, stockholder, receives research support, and is on the board of directors at HistoSonics, Inc., is a consultant with Ethicon, Inc., is on the Canon Medical Advisory Board, and has patents and royalties with Medtronic, Inc. Author TZ is a consultant, stockholder, receives research support from HistoSonics, Inc. and is a consultant with Ethicon, Inc.). KF, MK, AZ, EK, CB do not have anything to disclose.
Data Availability Statement
Data sharing not applicable – no new data generated.
References
- [1].Xu Z, Ludomirsky A, Eun LY, et al. Controlled ultrasound tissue erosion. Proc IEEE Ultrason Symp. 2004;51:726–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Vlaisavljevich E, Maxwell A, Mancia L, et al. Visualizing the Histotripsy Process: Bubble Cloud–Cancer Cell Interactions in a Tissue-Mimicking Environment. Ultrasound Med Biol. 2016;42:2466–2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Maxwell AD, Yuldashev PV, Kreider W, et al. A Prototype Therapy System for Transcutaneous Application of Boiling Histotripsy HHS Public Access. IEEE Trans Ultrason Ferroelectr Freq Control. 2017;64:1542–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Vlaisavljevich E, Maxwell A, Warnez M, et al. Histotripsy-induced cavitation cloud initiation thresholds in tissues of different mechanical properties. IEEE Trans Ultrason Ferroelectr Freq Control. 2014;61:341–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Khokhlova TD, Canney MS, Khokhlova VA, et al. Controlled tissue emulsification produced by high intensity focused ultrasound shock waves and millisecond boiling. J Acoust Soc Am. 2011;130:3498–3510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Maxwell A, Sapozhnikov O, Bailey M, et al. Disintegration of Tissue Using High Intensity Focused Ultrasound: Two Approaches That Utilize Shock Waves. Acoust Today. 2012;8:24. [Google Scholar]
- [7].Vlaisavljevich E, Kim Y, Allen S, et al. Image-Guided Non-Invasive Ultrasound Liver Ablation Using Histotripsy: Feasibility Study in an In-Vivo Procine Model. Ultrasound Med Biol. 2013;39:1398–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Xu Z, Hall TL, Vlaisavljevich E, et al. Histotripsy: the first noninvasive, non-ionizing, non-thermal ablation technique based on ultrasound. Int J Hyperth. 2021;38:561–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Illing RO, Kennedy JE, Wu F, et al. The safety and feasibility of extracorporeal high-intensity focused ultrasound (HIFU) for the treatment of liver and kidney tumours in a Western population. Br J Cancer. 2005;93:890–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kennedy JE. High-intensity focused ultrasound in the treatment of solid tumors. Nat Rev Cancer. 2005;5:321–327. [DOI] [PubMed] [Google Scholar]
- [11].Wu F, Wang ZB, Cao Y De, et al. A randomised clinical trial of high-intensity focused ultrasound ablation for the treatment of patients with localised breast cancer. Br J Cancer. 2003;89:2227–2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wu F, Chen WZ, Bai J, et al. Pathological changes in human malignant carcinoma treated with high-intensity focused ultrasound. Ultrasound Med Biol. 2001;27:1099–1106. [DOI] [PubMed] [Google Scholar]
- [13].Brace CL. Microwave tissue ablation: Biophysics, technology, and applications. Crit Rev Biomed Eng. 2010;38:65–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Brace CL. Thermal Tumor Ablation in Clinical Use. IEEE Pulse. 2011;2:28–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ahmed M. Image-guided tumor ablation: Standardization of terminology and reporting Criteria-A 10-year update. Radiology. 2014;273:241–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Nikfarjam M, Muralidharan V, Christophi C. Mechanisms of focal heat destruction of liver tumors. J Surg Res. 2005;127:208–223. [DOI] [PubMed] [Google Scholar]
- [17].Decadt B, Siriwardena AK. Radiofrequency ablation of liver tumours: Systematic review. Lancet Oncol. 2004;5:550–560. [DOI] [PubMed] [Google Scholar]
- [18].Huang SKS. Advances in Applications of Radiofrequency Current to Catheter Ablation Therapy. Pacing Clin Electrophysiol. 1991;14:28–42. [DOI] [PubMed] [Google Scholar]
- [19].Lubner MG, Brace CL, Hinshaw JL, et al. Microwave Tumor Ablation: Mechanism of Action, Clinical Results and Devices. J Vasc Interv Radiol. 2010;21:S192–S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Weber SM, Lee FT, Chinn DO, et al. Perivascular and intralesional tissue necrosis after hepatic cryoablation: Results in a porcine model. Surgery. 1997;122:742–747. [DOI] [PubMed] [Google Scholar]
- [21].Livraghi T, Meloni F, Solbiati L, et al. Complications of microwave ablation for liver tumors: Results of a multicenter study. Cardiovasc Intervent Radiol. 2012;35:868–874. [DOI] [PubMed] [Google Scholar]
- [22].Schmitz JJ, Schmit GD, Viers BR, et al. Renal Microwave Ablation Resulting in Ureteropelvic Junction Stricture Remote from the Ablation Site. J Vasc Interv Radiol. 2017;28:1278–1280.e1. [DOI] [PubMed] [Google Scholar]
- [23].Ziemlewicz TJ, Hinshaw JL, Lubner MG, et al. Percutaneous Microwave Ablation of Hepatocellular Carcinoma with a Gas-Cooled System: Initial Clinical Results with 107 Tumors. J Vasc Interv Radiol. 2015;1:62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Marchal F, Elias D, Leroux A, et al. Biliary Lesions during Radiofrequency Ablation in Liver. Eur Surg Res. 2004;36:88–94. [DOI] [PubMed] [Google Scholar]
- [25].Teratani T, Yoshida H, Shiina S, et al. Radiofrequency ablation for hepatocellular carcinoma in so-called high-risk locations. Hepatology. 2006;43:1101–1108. [DOI] [PubMed] [Google Scholar]
- [26].Pinkhasov GI, Raman JD. Management and prevention of renal ablative therapy complications. World J Urol. 2010;28:559–564. [DOI] [PubMed] [Google Scholar]
- [27].Orsi F, Zhang L, Arnone P, et al. High-intensity focused ultrasound ablation: Effective and safe therapy for solid tumors in difficult locations. Am J Roentgenol. 2010;195:245–252. [DOI] [PubMed] [Google Scholar]
- [28].Nabi G, Goodman C, Melzer A. High intensity focused ultrasound treatment of small renal masses: Clinical effectiveness and technological advances. Indian J Urol. 2010;26:331–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Cheung TT, Ma KW, She WH. A review on radiofrequency, microwave and high-intensity focused ultrasound ablations for hepatocellular carcinoma with cirrhosis. Hepatobiliary Surg Nutr. 2021;10:193–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hinshaw JL, Lee FT. Cryoablation for Liver Cancer. Tech Vasc Interv Radiol. 2007;10:47–57. [DOI] [PubMed] [Google Scholar]
- [31].Llovet JM, De Baere T, Kulik L, et al. Locoregional therapies in the era of molecular and immune treatments for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2021;18:293–313. [DOI] [PubMed] [Google Scholar]
- [32].Hsiao CY, Huang KW. Irreversible Electroporation: A Novel Ultrasound-guided Modality for Non-thermal Tumor Ablation. J Med Ultrasound. 2017;25:195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wagstaff PGK, Buijs M, van den Bos W, et al. Irreversible electroporation: State of the art. Onco Targets Ther. 2016;9:2437–2446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Davalos RV., Mir LM, Rubinsky B. Tissue ablation with irreversible electroporation. Ann Biomed Eng. 2005;33:223–231. [DOI] [PubMed] [Google Scholar]
- [35].Rubinsky B, Onik G, Mikus P. Irreversible electroporation: A new ablation modality - Clinical implications. Technol Cancer Res Treat. 2007;6:37–48. [DOI] [PubMed] [Google Scholar]
- [36].Cornelis FH, Durack JC, Kimm SY, et al. A Comparative Study of Ablation Boundary Sharpness After Percutaneous Radiofrequency, Cryo-, Microwave, and Irreversible Electroporation Ablation in Normal Swine Liver and Kidneys. Cardiovasc Intervent Radiol. 2017;40:1600–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Niessen C, Igl J, Pregler B, et al. Factors associated with short-term local recurrence of liver cancer after percutaneous ablation using irreversible electroporation: A prospective single-center study. J Vasc Interv Radiol. 2015;26:694–702. [DOI] [PubMed] [Google Scholar]
- [38].Knott EA, Zlevor AM, Hinshaw JL, et al. A comparison study of microwave ablation vs. histotripsy for focal liver treatments in a swine model. Eur Radiol. 2022;33:1050–1062. [DOI] [PubMed] [Google Scholar]
- [39].Scudamore CH, Lee SI, Patterson EJ, et al. Radiofrequency ablation followed by resection of malignant liver tumors. Am J Surg. 1999;177:411–417. [DOI] [PubMed] [Google Scholar]
- [40].Kasper HU, Bangard C, Gossmann A, et al. Pathomorphological changes after radiofrequency ablation in the liver. Pathol Int. 2010;60:149–155. [DOI] [PubMed] [Google Scholar]
- [41].Kopelman D, Inbar Y, Hanannel A, et al. Magnetic resonance-guided focused ultrasound surgery ( MRgFUS ): Ablation of liver tissue in a porcine model. Eur J Radiol. 2006;59:157–162. [DOI] [PubMed] [Google Scholar]
- [42].Hensen B, Drenkmann U, Frericks B, et al. Detection of Ablation Boundaries Using Different MR Sequences in a Swine Liver Model. Cardiovasc Intervent Radiol. 2022;45:1010–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Lee FT, Chosy SG, Littrup PJ, et al. CT-monitored percutaneous cryoablation in a pig liver model: Pilot study. Radiology. 1999;211:687–692. [DOI] [PubMed] [Google Scholar]
- [44].Lee EW, Loh CT, Kee ST. Imaging guided percutaneous irreversible electroporation: Ultrasound and immunohistological correlation. Technol Cancer Res Treat. 2007;6:287–293. [DOI] [PubMed] [Google Scholar]
- [45].Edd JF, Horowitz L, Davalos RV., et al. In vivo results of a new focal tissue ablation technique: Irreversible electroporation. IEEE Trans Biomed Eng. 2006;53:1409–1415. [DOI] [PubMed] [Google Scholar]
- [46].Ben-David E, Ahmed M, Faroja M, et al. Irreversible Electroporation : Treatment Effect Is Susceptible to Local Environment and Tissue Properties. Radiology. 2013;269:738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Lee EW, Chen C, Prieto VE, et al. Advanced hepatic ablation technique for creating complete cell death: Irreversible electroporation. Radiology. 2010;255:426–433. [DOI] [PubMed] [Google Scholar]
- [48].Kingham TP, Karkar AM, D’Angelica MI, et al. Ablation of perivascular hepatic malignant tumors with irreversible electroporation. J Am Coll Surg. 2012;215:379–387. [DOI] [PubMed] [Google Scholar]
- [49].Silk MT, Wimmer T, Lee KS, et al. Percutaneous ablation of peribiliary tumors with irreversible electroporation. J Vasc Interv Radiol. 2014;25:112–118. [DOI] [PubMed] [Google Scholar]
- [50].Vlaisavljevich E, Kim Y, Owens G. Effects of tissue mechanical properties on susceptibility to histotripsy-induced tissue damage. Phys Med Biol. 2014;59:253–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Vlaisavljevich E, Xu Z, Arvidson A, et al. The Effects of Thermal Preconditioning on Tissue Susceptibility to Histotripsy. Ultrasound Med Biol. 2015;41:2938–2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Hendricks-Wenger A, Schwenker H, Meduri C, et al. Determing Dose Effects of Critical Structures for Intra-abdominal Histotripsy Ablation. Histotripsy Symp. 2022; [Google Scholar]
- [53].Hendricks-Wenger A, Hutchison R, Vlaisavljevich E, et al. Immunological Effects of Histotripsy for Cancer Therapy. Front Oncol. 2021;11:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Qu S, Worlikar T, Felsted AE, et al. Non-thermal histotripsy tumor ablation promotes abscopal immune responses that enhance cancer immunotherapy. J Immunother Cancer. 2020;8:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Pepple AL, Guy JL, Mcginnis R, et al. Spatiotemporal local and abscopal cell death and immune responses to histotripsy focused ultrasound tumor ablation. Front Immunol. 2023;14:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Worlikar T, Vlaisavljevich E, Gerhardson T, et al. Histotripsy for Non-Invasive Ablation of Hepatocellular Carcinoma (HCC) Tumor in a Subcutaneous Xenograft Murine Model. IEEE Eng Med Biol Soc Annu Int Conf. 2018;2018:6064–6067. [DOI] [PubMed] [Google Scholar]
- [57].Smolock AR, Cristescu MM, Vlaisavljevich E, et al. Robotically assisted sonic therapy as a noninvasive nonthermal ablation modality: Proof of concept in a porcine liver model. Radiology. 2018;287:485–493. [DOI] [PubMed] [Google Scholar]
- [58].Longo KC, Knott EA, Watson RF, et al. Robotically Assisted Sonic Therapy (RAST) for Noninvasive Hepatic Ablation in a Porcine Model: Mitigation of Body Wall Damage with a Modified Pulse Sequence. Cardiovasc Intervent Radiol. 2019;42:1016–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Longo KC, Zlevor AM, Laeseke PF, et al. Histotripsy Ablations in a Porcine Liver Model: Feasibility of Respiratory Motion Compensation by Alteration of the Ablation Zone Prescription Shape. Cardiovasc Intervent Radiol. 2020;43:1695–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Knott EA, Longo KC, Vlaisavljevich E, et al. Transcostal Histotripsy Ablation in an In Vivo Acute Hepatic Porcine Model. Cardiovasc Intervent Radiol. 2021;44:1643–1650. [DOI] [PubMed] [Google Scholar]
- [61].Khokhlova TD, Wang YN, Simon JC, et al. Ultrasound-guided tissue fractionation by high intensity focused ultrasound in an in vivo porcine liver model. Proc Natl Acad Sci U S A. 2014;111:8161–8166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Khokhlova TD, Schade GR, Wang YN, et al. Pilot in vivo studies on transcutaneous boiling histotripsy in porcine liver and kidney. Sci Rep. 2019;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Vlaisavljevich E, Owens G, Lundt J, et al. Non-Invasive Liver Ablation Using Histotripsy: Preclinical Safety Study in an In-Vio Porcine Model. Ultrasound Med Biol. 2017;43:1237–1251. [DOI] [PubMed] [Google Scholar]
- [64].Mauch SC, Zlevor AM, Knott EA, et al. Hepatic and Renal Histotripsy in an Anticoagulated Porcine Model. J Vasc Interv Radiol. 2023;34:386–394.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Kim Y, Vlaisavljevich E, Owens GE, et al. In vivo transcostal histotripsy therapy without aberration correction. Phys Med Biol. 2014;59:2553–2568. [DOI] [PubMed] [Google Scholar]
- [66].Thomas GPL, Khokhlova TD, Khokhlova VA. Partial Respiratory Motion Compensation for Abdominal Extracorporeal Boiling Histotripsy Treatments with a Robotic Arm. IEEE Trans Ultrason Ferroelectr Freq Control. 2021;68:2861–2870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Winterholler J, Kisting M, Falk K, et al. Reduction of respiratory motion effect on Histotripsy ablation in porcine liver models by use of jet ventilation. Soc Interv Radiol Conf. 2023; [Google Scholar]
- [68].Vlaisavljevich E, Greve J, Cheng X, et al. Non-Invasive Ultrasound Liver Ablation Using Histotripsy: Chronic Study in an In Vivo Rodent Model. Ultrasound Med Biol. 2016;42:1890–1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Heo J, Joung C, Pahk K, et al. Investigation of the long-term healing response of the liver to boiling histotripsy treatment in vivo. Sci Rep. 2022;12:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Worlikar T, Mendiratta-Lala M, Vlaisavljevich E, et al. Effects of Histotripsy on Local Tumor Progression in an in vivo Orthotopic Rodent Liver Tumor Model. BME Front. 2020;1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Worlikar T, Zhang M, Ganguly A, et al. Impact of Histotripsy on Development of Intrahepatic Metastases in a Rodent Liver Tumor Model. Cancers (Basel). 2022;14:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Hendricks-Wenger A, Nagai-Singer MA, Uh K, et al. Employing Novel Porcine Models of Subcutaneous Pancreatic Cancer to Evaluate Oncological Therapies. Biomed Eng Technol. 2022. p. 883–895. [DOI] [PubMed] [Google Scholar]
- [73].Thomas GPL, Khokhlova TD, Sapozhnikov OA, et al. In Vivo Aberration Correction for Transcutaneous HIFU Therapy Using a Multielement Array. IEEE Trans Ultrason Ferroelectr Freq Control. 2022;10:2955–2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Matula TJ, Wang YN, Khokhlova T, et al. Treating Porcine Abscesses with Histotripsy: A Pilot Study. Ultrasound Med Biol. 2021;47:603–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Froghi S, de Andrade MO, Hadi LM, et al. Liver Ultrasound Histotripsy: Novel Analysis of the Histotripsy Site Cell Constituents with Implications for Histotripsy Application in Cell Transplantation and Cancer Therapy. Bioengineering. 2023;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Pahk KJ, Mohammad GH, Malago M, et al. A Novel Approach to Ultrasound-Mediated Tissue Decellularization and Intra-Hepatic Cell Delivery in Rats. Ultrasound Med Biol. 2016;42:1958–1967. [DOI] [PubMed] [Google Scholar]
- [77].Roberts WW, Hall TL, Ives K, et al. Pulsed Cavitational Ultrasound : A Noninvasive Technology for Controlled Tissue Ablation ( Histotripsy ) in the Rabbit Kidney. J Urol. 2006;175:734–738. [DOI] [PubMed] [Google Scholar]
- [78].Hall TL, Ph D, Kieran K, et al. Histotripsy of Rabbit Renal Tissue in Vivo : Temporal Histologic Trends. J Endourol. 2007;21:1159–1165. [DOI] [PubMed] [Google Scholar]
- [79].Styn NR, Hall TL, Fowlkes JB, et al. Technology and Engineering Histotripsy of Renal Implanted VX-2 Tumor in a Rabbit Model : Investigation of Metastases. Urology. 2012;80:724–729. [DOI] [PubMed] [Google Scholar]
- [80].Knott EA, Swietlik JF, Longo KC, et al. Robotically-Assisted Sonic Therapy for Renal Ablation in a Live Porcine Model: Initial Preclinical Results. J Vasc Interv Radiol. 2019;30:1293–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Couillard AB, Kisting MA, Rossebo AE, et al. A Comparison Study of Histotripsy and Cryoablation for Renal Ablation in a Porcine Model. Soc Interv Radiol Conf. 2022; [Google Scholar]
- [82].Lake AM, Xu Z, Wilkinson JE, et al. Renal Ablation by Histotripsy—Does it Spare the Collecting System? J Urol. 2008;179:1150–1154. [DOI] [PubMed] [Google Scholar]
- [83].Schade GR, Wang YN, D’Andrea S, et al. Boiling Histotripsy Ablation of Renal Cell Carcinoma in the Eker Rat Promotes A Systemic Inflammatory response. Ultrasound Med Biol. 2019;45:137–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].El Dib R, Touma NJ, Kapoor A. Cryoablation vs radiofrequency ablation for the treatment of renal cell carcinoma : a meta- analysis of case series studies. BJU Int. 2012;110:510–516. [DOI] [PubMed] [Google Scholar]
- [85].Hendricks-Wenger A, Arnold L, Gannon J, et al. Histotripsy Ablation in Preclinical Animal Models of Cancer and Spontaneous Tumors in Veterinary Patients: A Review. IEEE Trans Ultrason Ferroelectr Freq Control. 2022;69:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Hendricks-Wenger A, Zeher A, Sereno J, et al. Histotripsy is an effective pancreatic tumor ablation strategy that relesaes immunostimulatory molecules and promoted anti-tumor immunity. Focus Ultrasound Found Symp Virtual Conf. 2020; [Google Scholar]
- [87].Hendricks A, Brock RM, Gannon J, et al. Determining the mechanism of the immune response to histotripsy ablation of pancreatic cancer. Am Assoc Immunol Virtual Conf. 2020; [Google Scholar]
- [88].Gannon J, Khan I, Edwards M, et al. Histotripsy for the Treatment of Pancreatic Tumors: Feasibility Study in an in vivo Porcine Model. 21st Annu Int Symp Ther Ultrasound. 2021; [Google Scholar]
- [89].Khokhlova TD, Hwang JH. HIFU for palliative treatment of pancreatic cancer. J Gastroinestional Oncol. 2011. p. 175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Vidal-jove J, Perich E, Alvarez de Castillo M. Ultrasonics Sonochemistry Ultrasound Guided High Intensity Focused Ultrasound for malignant tumors : The Spanish experience of survival advantage in stage III and IV pancreatic cancer. Ultrason Sonochem. 2015;27:703–706. [DOI] [PubMed] [Google Scholar]
- [91].Wu F. High intensity focused ultrasound : A noninvasive therapy for locally advanced pancreatic cancer. World J Gastroenterol. 2014;20:16480–16488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Ning Z, Xie J, Chen Q, et al. HIFU is safe, effective, and feasible in pancreatic cancer patients: A monocentric retrospective study among 523 patients. Onco Targets Ther. 2019;12:1021–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Mancia L, Vlaisavljevich E, Yousefi N, et al. Modeling tissue-selective cavitation damage. Phys Med Biol. 2019;64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Hendricks-Wenger A, Aycock KN, Nagai-Singer MA, et al. Establishing an immunocompromised porcine model of human cancer for novel therapy development with pancreatic adenocarcinoma and irreversible electroporation. Sci Rep. 2021;11:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable – no new data generated.