Abstract
Introduction
Natalizumab (NTZ), a monoclonal antibody against the integrin α4β1 (VLA-4) found on activated T cells and B cells, blocks the interaction of this integrin with adhesion molecules of central nervous system (CNS) endothelial cells and lymphocyte migration through the blood–brain barrier, effectively preventing new lesion formation and relapses in multiple sclerosis (MS). Whether NTZ treatment has additional effects on the peripheral immune system cells, and how its actions compare with other MS disease-modifying treatments, have not been extensively investigated. In particular, its effect on the proportions of circulating regulatory T cells (Treg) is unclear.
Methods
In this study, we investigated the effect of NTZ treatment in 12 patients with relapsing MS, at 6 and 12 months after the start of treatment. We evaluated the proportions of regulatory T cells (Treg), defined by flow cytometry as CD4+ CD25++ FoxP3+ cells and CD4+ CD25++ CD127– cells at these intervals. As an exploratory study, we also investigated the NTZ effects on the proportions of bulk T and B lymphocyte populations, and of those expressing novel the markers CD195 (CCR5), CD196 (CCR6), or CD161 (KLRB1), which are involved in MS pathogenesis but have been studied less in the context of MS treatment. The effects of NTZ were compared to those obtained with 11 patients under interferon-beta-1a (IFN-β1a) treatment, and against 9 healthy volunteers.
Results
We observed a transient increment in the proportion of Treg cells at 6 months, which was not sustained at 12 months. We observed a reduction in the proportion of T cells expressing CD195 (CCR5) and CD161 (KLRB1) subsets of T cells.
Conclusion
We conclude that NTZ does not have an effect on the proportion of Treg cells over 1 year, but it may affect the expression of molecules important for some aspects MS pathogenesis, in a manner that is not shared with IFN-β1a.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40120-023-00539-9.
Keywords: CCR5, Foxp3, Multiple sclerosis, Natalizumab, Regulatory T cells
Key Summary Points
| Why carry out this study? |
| Multiple sclerosis (MS) affects 1 million people in the USA. Natalizumab (NTZ) is among the most effective disease-modifying treatments, acting by blocking lymphocyte (e.g. T cell) migration to the central nervous system (CNS). |
| It is not known whether NTZ affects the long-term phenotype and function of T cells, and in particular whether regulatory T cells (Treg) are affected by long-term NTZ treatment. This has implications for situations whereby NTZ is stopped (e.g. out of safety concerns) |
| What did the study ask?/What was the hypothesis of the study? |
| Does NTZ alter the proportion of Treg cells? The hypothesis is that long-term sequestration may lead to changes in Treg phenotypic markers. |
| What were the study outcomes/conclusions? |
| NTZ treatment for 1 year did not alter the proportion of T cells bearing Treg phenotypic markers. Some changes in pro-inflammatory T cell markers were noted, and need further confirmation. |
| What was learned from the study? |
| NTZ does not induce long-term Treg cells. This indicates that discontinuation of NTZ is not followed by long-term immune regulation and may explain rebounds of MS activity seen after NTZ discontinuation. |
| Other effector T cell surface markers are regulated by NTZ. These may represent markers of NTZ response, but need further confirmation, as these phenotypic markers were not the primary outcome of this study. |
Introduction
Migration of lymphocytes into the central nervous system (CNS) is an essential process in the pathogenesis of the inflammatory demyelinating disease, multiple sclerosis (MS) [1].
Trans-endothelial migration of lymphocytes in inflammatory conditions involves a complex series of event whereby inflamed endothelium interacts with activated lymphocytes. A crucial such interaction occurs between the α4β1 integrin (VLA-4) on lymphocytes and VCAM-1 on endothelial cells [1]. Natalizumab (NTZ) is a humanised monoclonal antibody that binds to and blocks the α4 component on the VLA-4 integrin and thus effectively suppresses transmigration of inflammatory cells into the CNS of people with MS. NTZ is among the most effective disease-modifying treatments for relapsing MS. It leads to a reduction of > 90% in the number of new inflammatory lesions on magnetic resonance imaging (MRI) [2, 3]. The ability of natalizumab to reduce immune cell entry into the CNS is also reflected in a reduction in immune surveillance within the CNS, and in the development of progressive multifocal leukoencephalopathy (PML), a rare, severe opportunistic infection caused by the JC polyomavirus, the reactivation of which occurs in immunosuppressed states [4].
Whether, in addition to its effects on immune cell migration, natalizumab exerts other long-term effects on immune cell function is not entirely clear. The fact that a rebound of MS disease activity and concomitant CNS inflammation can occur after discontinuation of natalizumab argues against long-term immunomodulatory effects of natalizumab on the effector T cells and possibly B cells in MS in the periphery [5]. This phenomenon also suggests that the proportion of circulating effector to regulatory T cells remains in favour of the former, and thus that NTZ does not enhance T reg cells. Indeed, Kimura and colleagues [6] have shown that NTZ down-regulates CD49 on Treg cells more than on effector cells; thus, the ability of Treg cells to migrate to the CNS during rebound is lower than that of effector cells.
Whether NTZ changes the proportion of Treg cells has been investigated in only a few studies. Kivisakk and colleagues [7] and Stenner and colleagues [29] found no change in the proportion of circulating Treg cells under short-term (3–6-months) NTZ treatment. It is unknown whether regulation occurs over longer periods.
There are few detailed longitudinal investigations of T and B cells phenotype changes over the course of natalizumab treatment, and few direct comparisons with other disease-modifying treatments in MS [6–12]. Relevant to the risk of rebound of disease activity, and of immune reconstitution syndrome (IRIS) after treatment cessation, natalizumab has direct, albeit mild, signalling effects with induction of a pro-inflammatory phenotype of T cells [13]. In particular, the effects of natalizumab on immune cell expression of the surface markers CD195 (CCR5) [14], CD196 (CCR6) and CD161 (KLRB1) are of great interest, as subsets of cells expressing these molecules have been associated with inflammatory activity in childhood-onset MS, and may provide clues to the first echelon of pathogenic immune cells in MS [15].
CCR5 is expressed on various cell types and has a role in directing cells to sites of inflammation [16], and it may contribute to the activation and recruitment of the immune cells in MS. CCR5 is expressed by the immune cells in the MS inflammatory lesions, or present in the cerebrospinal fluid (CSF) during a MS relapse [17], The proportion of CCR5+ CD19+ B cells in the blood is not altered during natalizumab treatment [11], but the effect of natalizumab on CCR5 expressed by T cells in MS has not been extensively explored.
Genetic variations of KLRB1 are associated with susceptibility to MS [18]. CD161 is a marker of interleukin 17 (IL-17) producing immune cells, and in MS its surface expression is increased on circulating CD8+ T cells [19] and CD8+ T cell subtypes that are recruited to MS lesions [20]. Recently, a specific pathogenic T cell population expressing CD161 and lymphotoxin beta was described in the brain tissue of progressive MS patients; its passage into the brain is blocked by natalizumab [21].
CCR6 is highly expressed on pro-inflammatory T cells (Th17, Thelper-1-like-Th17 cells, and cytotoxic T-cells), and also on myelin-reactive T cells in the blood and CSF from people with MS [22]. In the animal model of MS, CCR6 acts as a homing receptor, allowing inflammatory cells to access the uninflamed CNS [23, 24].
The primary aim of this study was to assess the effect of NTZ treatment on the proportion of circulating Treg over a 12-month period. As an exploratory study, we also examined T and B cell expression of CD161, CD195, and CD196 under treatment with natalizumab, at the start of treatment and 6 and 12 months after the start of treatment. We also compared the effects of NTZ to those of interferon-beta-1a (IFN-β-1a) at the same time points after the initiation of treatment, and volunteer controls with no MS or other neurological or inflammatory disease at one time point.
Methods
Patients
Patients with the diagnosis of MS according to the McDonald criteria [25], with a relapsing clinical course [26], were recruited between 2012 and 2015 from the MS Clinic at the University Hospitals Nottingham, UK. Patients were deemed on clinical grounds to qualify for disease-modifying treatment with either NTZ (Tysabri®) intravenously monthly or IFN-β-1a (Rebif® 44 μg subcutaneously 3 times weekly or Avonex® 30 mg intramuscularly once weekly). Patients had not received systemic glucocorticoid or other disease-modifying treatment and had not had clinical relapses in the 3 months preceding the initiation of the treatment.
The study was approved by the East Midlands Research Committee, UK (11/EM/0341). All patients gave written informed consent. The study was conducted in accordance with the Declaration of Helsinki.
At each visit, interval history was obtained, with particular attention to side effects, missed treatments, and relapses. The patients underwent a neurological examination with estimation of their expanded disability status scale (EDSS) scores [27].
Sample Collection
Blood samples were taken at baseline (visit 1, V1), month 6 (V2) and month 12 (V3) from patients with relapsing–remitting MS treated with NTZ (n = 12) or IFN-β (n = 11) and from controls with no MS ©) (n = 9). Samples from C were obtained at a single time point.
Peripheral blood mononuclear cells (PBMC) from patients and C were isolated by a density gradient centrifugation according to a standard protocol using Histopaque® 1077 (Sigma-Aldrich, St Louis, MO, USA). PBMC were frozen at a density of 5–10 × 106 cell/mL, using cryoprotective freezing medium [90% foetal calf serum (FCS) + 10% dimethyl sulfoxide] and storage in liquid nitrogen until completion of sample collection.
Flow Cytometry Staining
For cell identification and flow cytometry analysis, PBMCs were thawed, washed, and cultured overnight in RPMI 1640 with 10% FCS, 100 units/mL of penicillin, 0.1 mg/mL of streptomycin, and 2 mM of glutamine (all from Sigma-Aldrich). The following day, the cells were washed twice with phosphate buffered saline (PBS), counted, and resuspended at 1 × 106 cells/100 µL. Cells were incubated with LIVE/DEAD near-IR (Invitrogen) 1:100 cell stain and kept in darkness for 30 min. Then, they were washed once in fluorescence-activated cell sorting buffer (PBS + 2% FCS) and stained for extracellular markers CD3, CD4, CD8, CD25, CD127, CD161, CD195, CD196, and CD20 by standard procedures. For the FoxP3 marker, intracellular staining was performed using the Human FoxP3 buffer set (BD Biosciences) according to the manufacturer’s instructions.
FITC Mouse Anti-Human CD4, PE Mouse Anti-Human CD25, PE-Cy™ 7 Mouse Anti-Human CD127 and Alexa Fluor 647 Mouse anti-Human FoxP3 were from BD Biosciences.
Brilliant Violet 421™ anti-human CD195 (CCR5), Brilliant Violet 510™ anti-human CD3, Brilliant Violet 605™ anti-human CD161, Brilliant Violet 711™ anti-human CD196 (CCR6), Brilliant Violet 785™ anti-human CD8 and PerCPCy5.5 anti-human CD20 were from BioLegend.
Isotype controls for each antibody were included and ‘fluorescence minus one’ samples were used to set gating parameters.
For gating strategy, please see supplementary Fig. 1.
Flow Cytometry Analysis
The cells were analysed on a Beckman Coulter MoFlo Astrios Cell Sorter and using Kaluza 2.1 software (Beckman Coulter).
The following cell populations were analysed in the MS and C samples: T Reg (defined as CD4+ CD25++ CD127− and CD4+ CD25++ FoxP3+); CD3+ CD161+, CD3+ CD195+, CD3+ CD196+, B cells (defined as CD20+), CD20+ CD196+, and CD20+ CD195+, CD20+ CD3+, CD4+, CD8+ and CD8+ CD161+. The respective percentage of these cells were determined at V1, V2 and V3, in both NTZ and IFN-β groups.
Statistical Analysis
Statistical analysis was performed using GraphPad Prism 7.04 (GraphPad Software, La Jolla, CA, USA). The Mann–Whitney test was applied for comparisons (nonparametric test). Significance was set as p ≤ 0.05 without correction for multiple measurements, due to the exploratory nature of the study and potential collinearity of the novel markers.
Results
Participants
A total of 32 participants were recruited in the study. Of these, 12 patients with MS had been assigned on clinical grounds to NTZ, and 11 to IFN-β-1a. The patients receiving NTZ or IFN-β-1a had a second blood sample collected at month 6 after initiation of treatment (V2), and a third at month 12 (V3). A group of 9 healthy volunteers matched for age and sex (C) served as controls and provided blood samples at one time point (V1). In the NTZ group, there were 7 females and 5 males (Table 1).
Table 1.
Demographics of the participants
| NTZ | IFN | C | p | |
|---|---|---|---|---|
| N (F) | 12 (7) | 11 (9) | 9 (7) | ns |
| Age in years (SD) | 34 (7) | 42 (11) | 42 (10) | ns |
| EDSS | 3.5 (1.8) | 2.4 (1.9) | n/a | ns |
| MS duration | 3.4 (4.6) | 3.5 (1.8) | n/a | ns |
N number, F number of females, p significance (≤ 0.05 is significant), ns not significant, SD standard deviation, n/a = not applicable
Mean age was 34.2 years [range 21–45 years, standard deviation (SD) 7.25]. The mean EDSS in this group at V1 was 3.5 (range 1–7, SD 1.8). The mean disease duration was 3.4 years, range 1–7, SD 4.6, median 3). In the IFN-β group, there were 9 females and 2 males. Mean age was 42 years (range 25–59 years, SD 11.6). The mean EDSS in this group at V1 was 2.4 (range 0–6, SD 1.9). The mean disease duration was 3.5 years, range 2–7, SD 1.8, median 3). The C group comprised 7 females and 2 males. Mean age was 41.8 (range 31–58, SD 10.4). There were no significant differences in terms of sex distribution and age between the groups.
Clinical Course of MS During the Observation Period
Over the course of the 1 year of observation, none of the patients assigned to natalizumab experienced a clinical relapse. The EDSS score improved in three patients between V1 and V3 (3 to 1.5; 5 to 4; and 7 to 2). In the IFN-β group, one patient had a relapse with an increase in the EDSS score from 2.5 to 4 from V1 to V3. while another patient had a clinical relapse with EDSS remaining at 6 between V1 and V3.
There was no sustained meaningful change in bulk lymphocyte population throughout the study (supplementary Fig. 2).
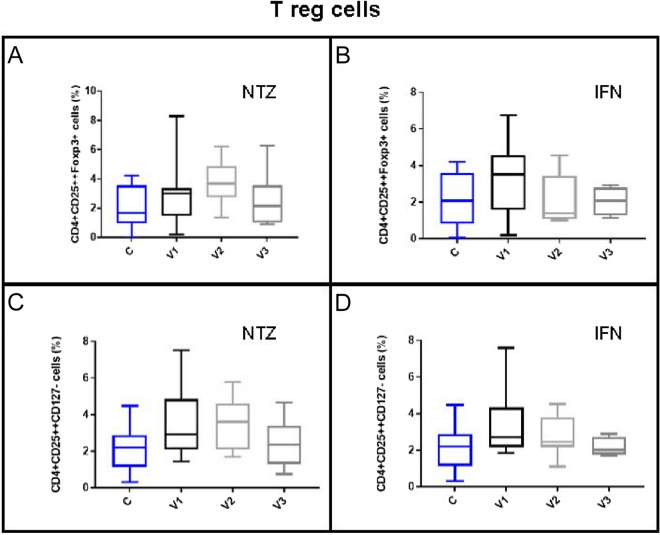
Natalizumab treatment was associated with an increase in the proportion of CD4+ CD25++ Foxp3+ cells at 6 months (V2) compared to C, which was paralleled by a non-significant increase in the CD4+ CD25+ CD127– cells. Otherwise, the proportion of regulatory T cells, defined as CD4+ CD25++ CD127– or CD4+ CD25++ Foxp3+ cells, did not differ at baseline between the MS patients and the C, or between visits during the course of the study, in either the NTZ or the IFN-β group (Fig. 1).
Fig. 1.
Effect of NTZ and IFNb1a on T reg cell populations from MS patients. Evaluation of CD4+ CD25++ FoxP3+ (A and B) and CD4+ CD25++ CD127– (C and D) cell percentages in PBMCs from MS patients treated either with NTZ or IFNb1a. C controls (non-MS), V1 baseline, V2 visit at 6 months, V3 visit at 12 months. Boxes represent interquartile range, median value is indicated as the central box line, and whiskers represent min to max range
We investigated the effect of NTZ, in comparison with IFN-β-1a, on a small set of lymphocytes that are of increasingly recognised importance in MS pathogenesis: those bearing the surface markers CD195 (CCR5), CD196 (CCR6), and CD161 (KLRB1).
We found that NTZ treatment significantly reduces the percentage of CD3+ cells expressing CD195 (CCR5). While this proportion was not different at baseline between patients and C, the reduction was significant already at 6 months between V1 and V2, and was more pronounced at V3, where it was significantly lower than in C. IFN-β-1a did not modulate CD195 (CCR5) expression. The CD20+ cell expression of CD195 was not affected by either treatment.
We found no effect of either NTZ or IFN-β-1a on the CD196 (CCR6) expression by CD3+ T cells. However, we did find an increased proportion of CD20+ cells expressing this chemokine receptor at month 6 (V2) which was significant compared to baseline and 12 months of NTZ treatment, as well as to C (not shown). Of note, this corresponded to the overall increase in B cells at 6 months. As in the T cell population, IFN-β-1a had no significant effect on this marker in the B cell population either.
The proportion of CD3+ CD161+ cells was significantly reduced by NTZ treatment, whereas IFN-β-1a did not modify it significantly. Within the T cell subsets, the percentage of CD8+ CD161+ T cells, which are thought to be particularly pathogenic [28], was significantly increased at baseline compared with C, and was significantly reduced after 1 year of NTZ treatment. IFN-β-1a had no significant effect on this subpopulation.
For results of the above and additional cell markers, please see supplementary Fig. 2.
As expected for the NTZ mechanism of action, there was an increase in the total number circulating lymphocytes (absolute lymphocyte count), and in the T cell (CD3+), CD4+ cell count and CD20+ cell count (B cells) under treatment with NTZ, whereas no significant, sustained, or relevant change in these populations was observed under treatment with IFN-β-1a (slight reduction in absolute CD20+ and CD8+ cells at V2 and increased absolute CD4+ count at V3). These absolute changes were not accompanied by changes in the relative proportions of Treg in either group (see supplementary Fig. 3).
Discussion
In this study, we have shown that NTZ does not have long-term effect on the proportion of Treg cells. However, it may affect the expression of molecules relevant to MS pathogenesis, in a way that is not shared with IFN-β1a.
The primary mechanism of action of NTZ in MS is interference with leukocyte trafficking into the CNS. The extent of this inhibition makes NTZ a highly effective disease-modifying therapeutic for MS. The binding and blockade of the VLA-4 integrin on immune cells prevents the interaction of this molecule with adhesion molecules on the vascular endothelium of the blood–brain barrier [2]. However, this interaction of the monoclonal antibody or cognate endogenous ligands such as VCAM-1 with the target integrin has other effects on immune cells. It can induce signalling pathways in the T cells and thus potentially modulates them [7]. Moreover, the ligation leads to the down-regulation of VLA-4 expression, which may differentially affect different T and B cell populations [6, 29]. It is therefore important to investigate the effects of NTZ on circulating immune cell subsets, and to compare them to those of other disease-modifying treatments, including those that do not primarily or specifically target leukocyte migration. In addition, it is now clear that discontinuation of NTZ can be followed by a return, and even a rebound, of inflammatory activity in MS [5], suggesting that the inflammatory potential of immune cells is preserved during NTZ treatment, and can become manifest once migration is unblocked. Studies have shown peripheral sequestration of inflammatory cells in the circulating compartments and increases in inflammatory cytokines [7].
In addition to integrins like α4β1 and their interaction with binding partners, the complex process of migration and crossing of the blood–brain barrier involves other molecular interactions, for example those between chemokines and their receptors [30]. The effect of NTZ treatment on chemokine receptors that are markers of pathogenic lymphocyte populations has been studied [7, 11], although not extensively, and it was worth revisiting in this small pilot study, in particular in comparison with IFN-β1a.
With regard to Treg cells, defined by two sets of markers, we have not found significant effects of NTZ treatment. While the proportion of Treg cells increased at V2 to levels that were significantly higher than those in C, the proportion was not significantly different from the baseline at V1. This indicates that blockade of lymphocyte migration into the CNS over 1 year does not affect the proportion of Treg cells, as defined by robust phenotypic markers that have been shown to correlate with Treg suppressive activity, and to respond to other MS treatments [31]. It is possible that the effect of NTZ on Treg was at the level of other cell surface molecules, including CD49/VLA-4, as has been shown previously, and, thus, despite no sustained changes in Treg functional markers, NTZ may affect the transmigration properties of these cells [6, 7]. Of note, in our study, the effect of NTZ on Treg was investigated over a longer period of time (12 months) than in previous studies (3–6 months). In this study, the lack of effect of NTZ on Treg cell phenotypic markers was shared with IFN-β1a.
In this exploratory study, the proportion of T cells expressing CCR5 (CD195) was reduced from baseline to visit 2, and further significantly decreased to visit 3, at which point it was lower than that seen in healthy volunteers. This indicates that NTZ had additional effects of relevance to the trans-endothelial migration of T cells by suppressing CCR5 expression. Traditionally, CCR5 was thought to be expressed preferentially on Th1 cells [32], but it is also known to be expressed on other cell types, including a recently identified subgroup of T cells that shares transcriptomics profiling with the Th17.1 cells [14]. These are cells that express both IFN-γ and IL-17 and are pathogenic in MS [33] through enhanced ability to cross the blood–brain barrier [34] and up-regulation in relapses [35]. CCR5 is relevant for MS, as maraviroc, a CCR5 antagonist, suppresses the murine model of MS, experimental autoimmune encephalomyelitis (EAE) [36]. It is reassuring, from the MS therapeutics point of view, that, alongside the blockade of VLA-4, NTZ treatment appears to reduce CCR5, thus preventing a potential compensatory increase in a molecule that could allow alternative lymphocyte migration pathways. On the other hand, this finding sheds light on the phenomenon of rebound MS activity and immune reconstitution inflammatory syndrome (IRIS) described after discontinuation of NTZ, in particular in the setting of positivity for JCV or development of PML [5]. Our findings support a role of CCR5 in the pathogenesis of these conditions, whereby discontinuation of NTZ releases not only α4β1 integrin (VLA-4) but also CCR5 (CD195) from blockade. CCR5, a receptor for the human immunodeficiency virus (HIV), has been implicated in HIV-associated PML and IRIS resulting from antiretroviral therapy, and maraviroc has been advocated, and used in this setting, as well as in NTZ-associated PML [37–39].
Another interesting effect of NTZ seen in this preliminary study was a reduction in the proportion of T cells expressing CD161, or KLRB1, a C-type lectin expressed specifically on memory T cells, particularly on those with a Th17 phenotype. These cells have pro-inflammatory activity and pathogenic potential in MS and are stimulated by the pro-inflammatory cytokine interleukin (IL)-12 [28]. These cells also express EOMES [28], a molecule implicated in the genetic susceptibility and pathogenesis of MS and EAE and a potential determinant of MS progression [40, 41]. Moreover, we show that the CD8+ T cell population expressing the CD161 marker is also reduced by NTZ treatment. A subgroup of these CD8+ cells has been implicated in paediatric-onset MS and represent one of the earliest cell types mediating MS, theoretically the nearest to the putative MS-inciting event and thus a possible therapeutic target [15]. Interestingly, CCR5 on a subgroup of CD4+ T cells is also an effector T cell population in paediatric-onset MS, and also, as discussed above, down-regulated by NTZ [15]. The fact that NTZ treatment for MS led to a reduction in these pathogenic cells underscores an immunoregulatory role for NTZ, not shared by IFN-β1a, that is not confined to its migration inhibition properties. Further studies, powered specifically to look at these molecules, are needed to elucidate the role of these cells and their regulation by NTZ.
We also investigated the effect of NTZ treatment on the proportion of lymphocytes expressing CCR6 (CD196), a molecule associated with proinflammatory, predominantly Th17, responses, and with CNS migration. We did not observe an overall effect, confirming previous studies that did not find an overall effect of NTZ treatment on CCR6+ B cells [42].
In conclusion, neither NTZ nor IFN- β1a altered the proportion of Treg over 12 months of treatment. This finding, together with the previous suggestion [7] and the recent demonstration [43] of enhanced pathogenicity of peripheral Th17 cells via co-expression of CCR6 and MCAM, may explain the MS rebound after NTZ discontinuation.
We found that the above-described changes in the exploratory study of newer markers may be specific to NTZ, as the IFN- β1a-treated patients did not show any of these changes.
There are limitations to our study. Although we followed the patients for a longer period of time than in other studies, the number of patients in both the NTZ and in the IFN- β1a arm were relatively small. The main aim is to determine changes in the proportion of Treg cells, using markers that are responsive to immunoregulation and correlate with suppressive activity.
Although the proportion of Treg did not change, the absolute number of Treg increased, in parallel with the expected increase observed in the absolute circulating lymphocyte count. The proportion of CD20+ cells also increased under NTZ treatment. However, the proportions of CD3+ cells and CD4+ cells were not altered (supplementary Fig. 2). As the proportion of effector cells to Treg is likely to be more relevant to Treg cell activity than the absolute number [15], we do not think the increase in Treg cell number and the slight reduction in the proportion of cells with the above-discussed T effector cell phenotype translates into an enhanced Treg suppressor potential.
Although there were no statistically significant differences in age, EDSS at baseline, and disease duration between the two patient groups, these were not perfectly matched. For example, the baseline mean EDSS was numerically lower by almost 1 step in the IFN-β1a group (though ranges were similar), perhaps reflecting the clinical practice of selecting more active patients for NTZ treatment. Similarly, the disease duration was more variable in the NTZ group. These differences may have reflected different stages of MS, such as proximity to secondary progressive disease. Some of these baseline differences may have influenced the immunological results.
Conclusion
As in previous, shorter studies, we found that, over 1 year of treatment, NTZ does not alter the proportion of Treg cells. In this small group of patients we avoided analyzing a large number of cell markers to avoid false positive findings. However, we decided to explore more recently implicated markers of early immunopathogenesis of MS, which had not previously been thoroughly investigated with regard to NTZ or in comparison to other disease-modifying treatments. In these preliminary studies, we detected changes that can provide hints to the pathogenesis of MS and, if confirmed, to the widening spectrum of action of NTZ.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank all the participants in this study.
Author Contributions
Radu Tanasescu: conceptualization, formal analysis, funding support, recruitment, data acquisition, project administration, writing original draft and review and editing; Nanci Frakich: methodology, formal analysis, data acquisition, project administration, writing original draft and review and editing; software, data curation; I-Jun Chou: project administration, recruitment, data acquisition, funding support; Perla Filippini: methodology, data acquisition, formal data analysis; Giulio Podda: recruitment, data acquisition; Gao Xin: methodology, formal analysis; Ranjithmenon Muraleedharan: methodology, data acquisition; Oltita P Jerca: conceptualization, recruitment, data acquisition; David Onion: conceptualization, methodology, resources, data acquisition, formal analysis; Cris S Constantinescu: conceptualization, formal analysis, funding support, resources, recruitment, data acquisition, project administration, data curation, supervision writing original draft and review and editing. All authors have read and agreed to the final manuscript.
Funding
This study was supported in part by an unrestricted grant from Biogen to C.S.C. Radu Tanasescu received in part support from MRC (CARP MR/T024402/1). I-Jun Chou was funded by Chang Gung Memorial Hospital, Taoyuan, Taiwan (Research Grants: CMRPG4A0121-0124, CORPG3G0461, CORPG3G0471, CORPG3G0481). The journal’s fee was waived.
Data Availability
Data obtained during this study are available upon request. Interested researchers are advised to contact the corresponding author.
Declarations
Conflict of Interest
Radu Tanasescu received support for attending scientific meetings from AbbVie, Biogen Idec, Teva and Genzyme, and consultancy fees from Johnson & Johnson. Cris S Constantinescu received research grant support, support for attending scientific meetings, and consultancy fees from Biogen Idec, Bayer Schering, Genzyme, Merck Serono, Morphosys, Novartis, Roche, Sanofi Pasteur and Merck Sharp and Dohme & EMD Serono. Dr Constantinescu is on the editorial board of Neurology and Therapy. Nanci Frakich, I-Jun Chou, Giulio Podda, Xin Gao, Ranjithmenon Muralledharan, Olita P Jerca and David Onion have nothing to disclose.
Ethical Approval
The study was approved by the East Midlands Research Committee, England (11/EM/0341). All patients gave written informed consent. The study was conducted in accordance with the Declaration of Helsinki.
References
- 1.Takeshita Y, Ransohoff RM. Inflammatory cell trafficking across the blood-brain barrier: chemokine regulation and in vitro models. Immunol Rev. 2012;248(1):228–239. doi: 10.1111/j.1600-065X.2012.01127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polman CH, O'Connor PW, Havrdova E, Hutchinson M, Kappos L, Miller DH, et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med. 2006;354(9):899–910. doi: 10.1056/NEJMoa044397. [DOI] [PubMed] [Google Scholar]
- 3.O'Connor P, Goodman A, Kappos L, Lublin F, Polman C, Rudick RA, et al. Long-term safety and effectiveness of natalizumab redosing and treatment in the STRATA MS Study. Neurology. 2014;83(1):78–86. doi: 10.1212/WNL.0000000000000541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho PR, Koendgen H, Campbell N, Haddock B, Richman S, Chang I. Risk of natalizumab-associated progressive multifocal leukoencephalopathy in patients with multiple sclerosis: a retrospective analysis of data from four clinical studies. Lancet Neurol. 2017;16(11):925–933. doi: 10.1016/S1474-4422(17)30282-X. [DOI] [PubMed] [Google Scholar]
- 5.Prosperini L, Kinkel RP, Miravalle AA, Iaffaldano P, Fantaccini S. Post-natalizumab disease reactivation in multiple sclerosis: systematic review and meta-analysis. Ther Adv Neurol Disord. 2019;12:1756286419837809. doi: 10.1177/1756286419837809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kimura K, Nakamura M, Sato W, Okamoto T, Araki M, Lin Y, et al. Disrupted balance of T cells under natalizumab treatment in multiple sclerosis. Neurol (R) Neuroimmunol Neuroinflamm. 2016;3(2):e210. doi: 10.1212/NXI.0000000000000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kivisakk P, Healy BC, Viglietta V, Quintana FJ, Hootstein MA, Weiner HL, et al. Natalizumab treatment is associated with peripheral sequestration of proinflammatory T cells. Neurology. 2009;72(22):1922–1930. doi: 10.1212/WNL.0b013e3181a8266f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carotenuto A, Scalia G, Ausiello F, Moccia M, Russo CV, Sacca F, et al. CD4/CD8 ratio during natalizumab treatment in multiple sclerosis patients. J Neuroimmunol. 2017;309:47–50. doi: 10.1016/j.jneuroim.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Sellebjerg F, Cadavid D, Steiner D, Villar LM, Reynolds R, Mikol D. Exploring potential mechanisms of action of natalizumab in secondary progressive multiple sclerosis. Ther Adv Neurol Disord. 2016;9(1):31–43. doi: 10.1177/1756285615615257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meira M, Sievers C, Hoffmann F, Rasenack M, Kuhle J, Derfuss T, et al. Unraveling natalizumab effects on deregulated miR-17 expression in CD4+ T cells of patients with relapsing-remitting multiple sclerosis. J Immunol Res. 2014;2014:897249. doi: 10.1155/2014/897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saraste M, Penttila TL, Airas L. Natalizumab treatment leads to an increase in circulating CXCR3-expressing B cells. Neurol Neuroimmunol Neuroinflamm. 2016;3(6):e292. doi: 10.1212/NXI.0000000000000292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maier S, Simu M, Hutanu A, Barcutean L, Voidazan S, Bajko Z, et al. Clinical immunological correlations in patients with multiple sclerosis treated with natalizumab. Brain Sci. 2020;10(11):802. doi: 10.3390/brainsci10110802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benkert TF, Dietz L, Hartmann EM, Leich E, Rosenwald A, Serfling E, et al. Natalizumab exerts direct signaling capacity and supports a pro-inflammatory phenotype in some patients with multiple sclerosis. PLoS ONE. 2012;7(12):e52208. doi: 10.1371/journal.pone.0052208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herich S, Schneider-Hohendorf T, Rohlmann A, KhaleghiGhadiri M, Schulte-Mecklenbeck A, Zondler L, et al. Human CCR5high effector memory cells perform CNS parenchymal immune surveillance via GZMK-mediated transendothelial diapedesis. Brain: J Neurol. 2019;142(11):3411–3427. doi: 10.1093/brain/awz301. [DOI] [PubMed] [Google Scholar]
- 15.Mexhitaj I, Nyirenda MH, Li R, O'Mahony J, Rezk A, Rozenberg A, et al. Abnormal effector and regulatory T cell subsets in paediatric-onset multiple sclerosis. Brain: J Neurol. 2019;142(3):617–632. doi: 10.1093/brain/awz017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vangelista L, Vento S. The expanding therapeutic perspective of CCR5 blockade. Front Immunol. 2017;8:1981. doi: 10.3389/fimmu.2017.01981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sorensen TL, Tani M, Jensen J, Pierce V, Lucchinetti C, Folcik VA, et al. Expression of specific chemokines and chemokine receptors in the central nervous system of multiple sclerosis patients. J Clin Invest. 1999;103(6):807–815. doi: 10.1172/JCI5150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sondergaard HB, Sellebjerg F, Hillert J, Olsson T, Kockum I, Linden M, et al. Alterations in KLRB1 gene expression and a Scandinavian multiple sclerosis association study of the KLRB1 SNP rs4763655. Eur J Hum Genet. 2011;19(10):1100–1103. doi: 10.1038/ejhg.2011.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Annibali V, Ristori G, Angelini DF, Serafini B, Mechelli R, Cannoni S, et al. CD161(high)CD8+T cells bear pathogenetic potential in multiple sclerosis. Brain. 2011;134(Pt 2):542–554. doi: 10.1093/brain/awq354. [DOI] [PubMed] [Google Scholar]
- 20.Nicol B, Salou M, Vogel I, Garcia A, Dugast E, Morille J, et al. An intermediate level of CD161 expression defines a novel activated, inflammatory, and pathogenic subset of CD8(+) T cells involved in multiple sclerosis. J Autoimmun. 2018;88:61–74. doi: 10.1016/j.jaut.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Kaufmann M, Evans H, Schaupp AL, Engler JB, Kaur G, Willing A, et al. Identifying CNS-colonizing T cells as potential therapeutic targets to prevent progression of multiple sclerosis. Med (N Y) 2021;2(3):296–312.e8. doi: 10.1016/j.medj.2021.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cao Y, Goods BA, Raddassi K, Nepom GT, Kwok WW, Love JC, et al. Functional inflammatory profiles distinguish myelin-reactive T cells from patients with multiple sclerosis. Sci Transl Med. 2015;7(287):287ra74. doi: 10.1126/scitranslmed.aaa8038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liston A, Kohler RE, Townley S, Haylock-Jacobs S, Comerford I, Caon AC, et al. Inhibition of CCR6 function reduces the severity of experimental autoimmune encephalomyelitis via effects on the priming phase of the immune response. J Immunol. 2009;182(5):3121–3130. doi: 10.4049/jimmunol.0713169. [DOI] [PubMed] [Google Scholar]
- 24.Reboldi A, Coisne C, Baumjohann D, Benvenuto F, Bottinelli D, Lira S, et al. C-C chemokine receptor 6-regulated entry of TH-17 cells into the CNS through the choroid plexus is required for the initiation of EAE. Nat Immunol. 2009;10(5):514–523. doi: 10.1038/ni.1716. [DOI] [PubMed] [Google Scholar]
- 25.Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17(2):162–173. doi: 10.1016/S1474-4422(17)30470-2. [DOI] [PubMed] [Google Scholar]
- 26.Lublin FD, Reingold SC, Cohen JA, Cutter GR, Sorensen PS, Thompson AJ, et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. 2014;83(3):278–286. doi: 10.1212/WNL.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33(11):1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 28.Fergusson JR, Fleming VM, Klenerman P. CD161-expressing human T cells. Front Immunol. 2011;2:36. doi: 10.3389/fimmu.2011.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stenner MP, Waschbisch A, Buck D, Doerck S, Einsele H, Toyka KV, et al. Effects of natalizumab treatment on Foxp3+ T regulatory cells. PLoS ONE. 2008;3(10):e3319. doi: 10.1371/journal.pone.0003319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luster AD. Chemokines–chemotactic cytokines that mediate inflammation. N Engl J Med. 1998;338(7):436–445. doi: 10.1056/NEJM199802123380706. [DOI] [PubMed] [Google Scholar]
- 31.Tanasescu R, Tench CR, Constantinescu CS, Telford G, Singh S, Frakich N, et al. Hookworm treatment for relapsing multiple sclerosis: a randomized double-blinded placebo-controlled trial. JAMA Neurol. 2020;77(9):1089–1098. doi: 10.1001/jamaneurol.2020.1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loetscher P, Uguccioni M, Bordoli L, Baggiolini M, Moser B, Chizzolini C, et al. CCR5 is characteristic of Th1 lymphocytes. Nature. 1998;391(6665):344–345. doi: 10.1038/34814. [DOI] [PubMed] [Google Scholar]
- 33.Moser T, Akgun K, Proschmann U, Sellner J, Ziemssen T. The role of TH17 cells in multiple sclerosis: therapeutic implications. Autoimmun Rev. 2020;19(10):102647. doi: 10.1016/j.autrev.2020.102647. [DOI] [PubMed] [Google Scholar]
- 34.Kebir H, Ifergan I, Alvarez JI, Bernard M, Poirier J, Arbour N, et al. Preferential recruitment of interferon-gamma-expressing TH17 cells in multiple sclerosis. Ann Neurol. 2009;66(3):390–402. doi: 10.1002/ana.21748. [DOI] [PubMed] [Google Scholar]
- 35.Edwards LJ, Robins RA, Constantinescu CS. Th17/Th1 phenotype in demyelinating disease. Cytokine. 2010;50(1):19–23. doi: 10.1016/j.cyto.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 36.Karampoor S, Zahednasab H, Amini R, Esghaei M, Sholeh M, Keyvani H. Maraviroc attenuates the pathogenesis of experimental autoimmune encephalitis. Int Immunopharmacol. 2020;80:106138. doi: 10.1016/j.intimp.2019.106138. [DOI] [PubMed] [Google Scholar]
- 37.Stork L, Bruck W, Bar-Or A, Metz I. High CCR5 expression in natalizumab-associated progressive multifocal leukoencephalopathy immune reconstitution inflammatory syndrome supports treatment with the CCR5 inhibitor maraviroc. Acta Neuropathol. 2015;129(3):467–468. doi: 10.1007/s00401-015-1391-6. [DOI] [PubMed] [Google Scholar]
- 38.Giacomini PS, Rozenberg A, Metz I, Araujo D, Arbour N, Bar-Or A, et al. Maraviroc and JC virus-associated immune reconstitution inflammatory syndrome. N Engl J Med. 2014;370(5):486–488. doi: 10.1056/NEJMc1304828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hodecker SC, Sturner KH, Becker V, Elias-Hamp B, Holst B, Friese MA, et al. Maraviroc as possible treatment for PML-IRIS in natalizumab-treated patients with MS. Neurol (R) Neuroimmunol Neuroinflamm. 2017;4(2):e325. doi: 10.1212/NXI.0000000000000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raveney BJ, Oki S, Hohjoh H, Nakamura M, Sato W, Murata M, et al. Eomesodermin-expressing T-helper cells are essential for chronic neuroinflammation. Nat Commun. 2015;6:8437. doi: 10.1038/ncomms9437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oki S. Eomes-expressing T-helper cells as potential target of therapy in chronic neuroinflammation. Neurochem Int. 2019;130:104348. doi: 10.1016/j.neuint.2018.11.023. [DOI] [PubMed] [Google Scholar]
- 42.van Langelaar J, Rijvers L, Janssen M, Wierenga-Wolf AF, Melief MJ, Siepman TA, et al. Induction of brain-infiltrating T-bet-expressing B cells in multiple sclerosis. Ann Neurol. 2019;86(2):264–278. doi: 10.1002/ana.25508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Janoschka C, Lindner M, Koppers N, Starost L, Liebmann M, Eschborn M, et al. Enhanced pathogenicity of Th17 cells due to natalizumab treatment: Implications for MS disease rebound. Proc Natl Acad Sci U S A. 2023;120(1):e22. doi: 10.1073/pnas.2209944120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data obtained during this study are available upon request. Interested researchers are advised to contact the corresponding author.