Abstract
Background
The majority of English literature has reported on the somewhat conflicted outcomes of the effect of radiotherapy on immediate breast reconstruction. However, data specifically related to patients of Asian descent has been scarce. This retrospective study aims to shed light on this topic to aid in the management of this group of patients.
Methods
All patients who received immediate free perforator flap-based breast reconstruction under a single surgeon over a 10-year period were included in the study. Patient characteristics, oncological and surgical data were collected. Patients were divided into post-mastectomy radiotherapy (PMRT) and non-PMRT groups. The final aesthetic outcome was assessed by a surgeon-reported outcome questionnaire. Patient satisfaction and psychological outcomes were assessed using validated patient-reported outcome (PRO) questionnaire (BREAST-Q), breast reconstruction, and postoperative module.
Results
A total of 101 women, with an average age of 44.7 ± 8.4 underwent perforator flap-based reconstruction. Fifteen patients received PMRT, with remaining 86 patients in the non-PMRT group. The mean duration of follow-up was over 5 years (p = 0.514). The recurrence rate was acceptable in the PMRT group (3/15, p = 0.129). There were no significant differences in complication rates between the two groups (p = 1.000). The aesthetic outcomes were comparable (p = 0.342). PRO appears to be lower in the PMRT group.
Conclusions
Immediate breast reconstruction with PMRT in the local patient cohort is oncologically safe, acceptable complication profile, revision rate, and aesthetic outcome. PRO showed lower scores in several categories, which differ from normative data generated in the Western population. Further studies will need to examine the confounding effects of radiation in this specific population.
Keywords: Immediate autologous breast reconstruction, Post-mastectomy radiation therapy, Patient-reported outcomes, BREAST-Q
Introduction
There are two schools of thought regarding the timing of breast reconstruction when post-mastectomy radiotherapy (PMRT) is required. The decision depends on the belief in the extent of radiotherapy's influence on the outcomes of the surgery, especially on the final aesthetics achieved over the psychological benefit of immediate reconstruction.1 In the senior author's (JJH) practice, the multidisciplinary oncology team did not discourage patients from undergoing immediate breast reconstruction when PMRT is required. This is partly based on recent systematic reviews2,3 demonstrating no significant differences in outcomes between delay and immediate reconstruction and good outcomes in using perforator flap-based free flap options.4 In addition, similar to the prevalence and broader indications of digital replantation in Asia,5 a culture influenced by Confucianism placed significant emotional significance on the loss of body parts.
Despite this, the outcomes of surgery and the patient perceived experience still requires substantiation. A survey of the literature reveals a paucity of information for Asian women in the English literature undergoing perforator flap-based breast reconstruction. The differences in attitude of Asians toward reconstruction and deficiency of data in this aspect have been noted,6,7 particularly in relation to patient-reported outcomes (PRO). Several studies utilized non-validated tools for this purpose.6,8,9 To date, only Chao et al10 performed a comprehensive review of the changes in the PRO between women receiving various types of breast reconstruction. However, the specific issue of outcomes differences in perforator flap-based reconstruction receiving PMRT was only looked at by He et al11 utilized the current gold standard in PRO (BREAST-Q). However, the outcomes were not reported in its entirety and the primary reconstruction option were pedicled transverse rectus abdominis musculocutaneous (TRAM) with only small numbers of perforator-based free flaps. This article thus intends to shed more light on this topic.
The current study retrospectively evaluates differences in the postoperative journey between Asian female patients who have undergone immediate free perforator flap-based reconstruction with and without PMRT. Oncological outcomes, significant surgical and radiation-related complications, subjective aesthetic outcome from the surgeon's perspective, and PRO were assessed.
Patients and methods
Institutional review board committee (IRB No. 201900634B0) approval was obtained. This is a retrospective cohort study. Patients were divided into two groups: Immediate breast reconstruction with or without PMRT. All patients who received immediate breast reconstruction for cancer treatment by the senior author (JJH) between July 2008 and December 2018 were identified. Patients who had recurrence, previous radiation therapy, or lost to follow-up were excluded from the study. To avoid the confounding effect of flap vascular complications, this group of patients was also excluded (Supplementary Table 1).
Data collection
Data concerning patient's demographics, including age, body mass index (BMI) and the type of free flap used for reconstruction were collected. Flaps used for reconstruction included deep inferior epigastric perforator (DIEP) flaps, muscle-sparing transverse rectus abdominis musculocutaneous (ms-TRAM) flaps and profunda artery perforator (PAP) flaps.
Oncological profile and treatments, including tumour staging, oestrogen and progesterone receptor status, human epidermal growth factor receptor 2 (HER2) status, neoadjuvant and adjuvant chemo-radiotherapy, and the type of mastectomy were recorded.
To assess if the reconstruction impacted the oncological outcomes of the patients, all medical records were assessed throughout the duration of follow-up (up until April 2021) to document any signs of recurrence, including locoregional or metastasis that developed after the completion of treatment. The interval between reconstruction and radiotherapy were examined to assess if the reconstruction delayed the treatment of any patients that developed recurrence.
To obtained information to compare postoperative recovery between the two groups, early (within a month postoperatively) and late (over a month postoperatively) complications were collected. Early complications include mastectomy skin flap necrosis, infection, haematoma, partial necrosis of the primary flap, and nipple areolar complex necrosis. Late complications include fat necrosis and chronic persistent wounds that required surgical intervention. Any complications related to radiation therapy were recorded.
Surgeon-reported aesthetic outcome (SrAO)
To compare subjective aesthetic outcome of the two groups, a panel of six board certified plastic surgeons (not included in the authors list) were recruited for the assessment. With the panel blinded to the two groups, they were first provided the standard postoperative photographs of the patients for a 3 minute assessment. These photographs were taken at least 1 year post-breast reconstruction (non-PMRT group) or at least 6 months postradiotherapy (PMRT group). After the designated time, each surgeon from the panel is required to rate the aesthetic outcomes using a visual analogue scale that consists of five items which include 1) the shape of the reconstructed breast; 2) the symmetry of the inframammary fold (IMF); 3) the symmetry of the bilateral breast volume; 4) the symmetry of the bilateral breast shape; and 5) the overall reconstructive appearance. Each of the five items was rated on a numerical scale from 1 to 5, ranging from 1, which is “very unsatisfactory” to 5 being “very satisfactory.”
Patient-reported outcome (BREAST-Q)
Subjective PRO was evaluated using BREAST-Q12,13 at least 1 year after immediate breast reconstruction (non-PMRT group) or at least 6 months postradiotherapy (PMRT group). The breast reconstruction module with the life of the quality and satisfaction domains (psychosocial well-being, physical well-being, sexual well-being, satisfaction with breasts, and satisfaction with care) were used. Each domain, items are summed and translated to a 0 to 100 scale, with greater values indicating higher satisfaction and better health-related quality of life. As the questionnaire was prescribed retrospectively, only the postoperative part of the module was used.
Radiotherapy
A dose to 5000–5040 cGy divided into 25–28 fractions was provided. Besides, the detailed protocol was modified at the discretion of the radiation oncologists on an individual-case basis, accounting for factors such as the involvement of internal mammary nodes and other factors.
Surgical technique
Preoperative marking was done with the patients in standing position, the markings included the midline, anterior axillary line, IMF, and the upper border of bilateral breasts. The surgery was started in a two-team approach, with breast surgeons performing the mastectomy and the reconstructive surgeon harvesting the flap. The recipient vessels were prepared after the mastectomy was finished before the pedicle of the flaps was divided. After microvascular anastomosis, the redundant flap was excised. De-epithelialization was partially done before the inset to confirm the final monitor skin flap location. The IMF and lateral border of the breast were reinforced by suturing the mastectomy skin flap to the chest wall. After completing the de-epithelialization of the buried part of the flap, the wounds were closed primarily.
Statistics
All data are presented as mean ± standard deviation (SD) and range. All statistical analyses were performed using SPSS software (IBM SPSS Statistics for Mac, version 21, IBM Corp., Armonk, USA); t-tests were conducted to compare the cohorts with regard to continuous variables, and chi-square tests were conducted for categorical variables. A p-value of less than 0.05 was considered a statistically significant difference.
Results
A total of 151 patients were first identified, of which 101 patients fulfilled the inclusion criteria. Fifteen out of the 101 patients (14.8%) underwent PMRT. The average follow-up were 5.2 ± 2.48 years (range 2.4–10.5) in the PMRT group and 5.73 ± 2.73 years (range 2.3–12.8) in the non-PMRT groups (p = 0.514).
Baseline characteristics and flap choices
The mean age of all patients was 44.7 ± 8.4 years old, with the PMRT group being statistically significantly younger than the non-PMRT group with a mean age of 40.0 ± 7.5 and 45.5 ± 8.3, respectively (p = 0.019). Twelve of the 15 (80%) PMRT patients were in the 30 to 49-year-old age group, while there were more patients (31.4%) over 50 years of age in the non-PMRT group. The mean BMI of our patient cohort was 24.2 ± 4.1. 92.9% of patients in both groups were under BMI of 30, suggesting our cohort of patients were lean females. Despite this, the most commonly utilized free flap was the DIEP flap with PAP flap or conversion to ms-TRAM secondary option when sizable perforators were not available (Table 1). The mean flap volume used in our patients was 460.3 ± 191.2 gm, with the PMRT group 458.4 ± 187.0 and non-PMRT group was 471.7 ± 222.6, respectively (p = 0.810) (Supplementary Table 2).
Table 1.
Clinical characteristics and perforator flap choices between PMRT and non-PMRT groups.
| Non-PMRT group (n = 86) | PMRT group (n = 15) | p | |
|---|---|---|---|
| Age (years) | 45.5 ± 8.3 (24–65) | 40.0 ± 7.5 (29–53) | 0.019⁎ |
| between 20–29 | 3 (3.5) | 1 (6.7) | 0.259 |
| 30–49 | 56 (65.1) | 12 (80.0) | |
| > 50 | 27 (31.4) | 2 (13.3) | |
| BMI (kg/m2) | 24.2 ± 4.2 (17.3–40.1) | 24.5 ± 3.7 (19.5–32.0) | 0.770 |
| < 30 | 78 (92.9) | 13 (92.9) | 0.621 |
| > 30 | 6 (7.1) | 2 (13.3) | |
| Perforator flap used | 0.208 | ||
| DIEP | 75 (87.2) | 11 (73.3) | |
| PAP | 6 (7.0) | 2 (13.3) | |
| Free ms-TRAM | 5 (5.8) | 2 (13.3) |
Values are presented as mean ± SD (range) or number (%). PMRT: post-mastectomy radiotherapy; BMI: body mass index; DIEP: deep inferior epigastric artery perforator flap; PAP: profunda artery perforator flap; ms-TRAM: muscle-sparing transverse rectus abdominis myocutaneous flap.
Significant statistical difference.
Oncological profile and safety
The patients in the PMRT group have more advanced stage breast cancer (p = 0.002), thus more axillary lymph node involvement (p = 0.010) (Table 2), more patients underwent neoadjuvant (p = 0.004), and adjuvant chemotherapy (p = 0.005).
Table 2.
Oncological profile and outcome between the non-PMRT group and the PMRT group.
| Non-PMRT group (n = 86) | PMRT group (n = 15) | p | |
|---|---|---|---|
| Type of mastectomy | 0.010⁎ | ||
| SSM/NSM ALND (-) | 26 (30.2) | 0 (0.0) | |
| SSM/NSM ALND (+) | 60 (69.8) | 15 (100.0) | |
| TNM staging | |||
| Stage 0 (DCIS) | 21 (24.4) | 0 (0.0) | 0.002⁎ |
| Stage I | 28 (32.6) | 2 (13.3) | |
| Stage II | 37 (43.0) | 5 (33.3) | |
| Stage III | 0 (0.0) | 8 (53.3) | |
| ER status | 0.489 | ||
| Positive | 70 (81.4) | 11 (73.3) | |
| Negative | 16 (18.6) | 4 (26.7) | |
| PR status | 0.115 | ||
| Positive | 65 (75.6) | 8 (53.3) | |
| Negative | 21 (24.4) | 7 (46.7) | |
| HER2 status | 0.665 | ||
| Positive | 35 (40.7) | 7 (46.7) | |
| Negative | 51 (59.3) | 8 (53.3) | |
| Neoadjuvant chemotherapy | 7 (8.1) | 6 (40.0) | 0.004⁎ |
| Adjuvant chemotherapy | 55 (64.0) | 15 (100.0) | 0.005⁎ |
| Time, surgery to RT (months) | N/A | 5.16 ± 2.62 (1.6–8.4) | N/A |
| Oncological outcomes | 0.129 | ||
| Disease free | 80 (93.0) | 12 (80.0) | |
| Locoregional recurrence | 0 | 0 | |
| Distant metastasis | 6 (7.0) | 3 (20.0) | |
| Follow-up (months) | 69.30 ± 33.25 (28.4–155.4) | 63.28 ± 30.16 (28.8–127.4) | 0.514 |
Values are presented as number (%) or mean ± SD (range). PMRT: post-mastectomy radiotherapy; SSM: skin-sparing mastectomy; NSM: nipple-sparing mastectomy; ALND: axillary lymph node dissection, RT: radiotherapy; TNM: tumor-node-metastasis; DCIS: Ductal carcinoma in situ; ER: Estrogen receptor; PR: progestrone recentor; HER2: human epidermal growth factor receptor 2.
Significant statistical difference.
In a mean follow-up duration of 5 years (ranging from 2.4 to 10.5 years) in the PMRT group, only 3/15 (20%) developed distant metastasis, with no cases of locoregional recurrences (Table 2). 12/15 (80%) subjects remained disease free. In the non-PMRT group, 6/86 subjects (7%) developed locoregional recurrence or distant metastasis.
The mean overall interval between time of surgery to radiotherapy for the PMRT group was 5.16 months (range 1.6–8.4 months) (Table 2). In a sub analysis of the patients who developed recurrence or metastasis, two patients had radiation therapy within 6 months (at 3 months and 6 months, respectively), while one other patient received radiation therapy at 7 months (Table 3). These three patients did not suffer from any complications from the reconstruction prior to radiation therapy, and the late delivery of radiotherapy was because of ongoing adjuvant chemotherapy.
Table 3.
The list of patients with post-mastectomy radiation therapy (n = 15).
| Patient number | Age | bmi | Tumour staging | Neoadjuvant chemotherapy | Adjuvant chemotherapy | Radiotherapy dose | Interval† | Recurrence | Complications after RT | Revisions (frequency) | SrOA | Photo assessed | Breast Q-1 | Breast Q-2 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 34 | 21.3 | IA | Yes | No | 6640 | 133 | No | None | 0 | 3.83 | 1183 | 78 | 64 |
| 2 | 53 | 28.7 | IIIA | No | Yes | 6250 | 202 | No | None | 0 | 3.50 | 493 | N/A | N/A |
| 3 | 31 | 26.2 | IIIA | No | Yes | 5040 | 236 | No | None | 0 | 4.33 | 406 | 57 | 55 |
| 4 | 43 | 30.7 | IIB | No | Yes | 5040 | 218 | No | None | 1 | 3.83 | 120 | 48 | 48 |
| 5 | 33 | 21.6 | IIIC | Yes | Yes | 6000 | 185 | Yes | None | 0 | 4.17 | 1024 | N/A | N/A |
| 6 | 48 | 21.9 | IIB | No | Yes | 5040 | 229 | No | None | 4 | N/A | N/A | N/A | N/A |
| 7 | 51 | 22.3 | IIIA | Yes | Yes | 6250 | 83 | Yes | Radiation dermatitis, gr1 | 0 | 3.50 | 255 | 55 | 93 |
| 8 | 37 | 26.2 | IB | Yes | Yes | 5000 | 54 | No | None | 1 | 4.00 | 236 | 71 | 47 |
| 9 | 42 | 24.4 | IIA | Yes | Yes | 5000 | 64 | No | Skin pigmentation change | 1 | 3.67 | 228 | 54 | 43 |
| 10 | 37 | 32.0 | IIIC | No | Yes | 6500 | 221 | Yes | Radiation dermatitis, gr1 | 0 | 4.67 | 130 | N/A | N/A |
| 11 | 37 | 19.5 | IIIA | No | Yes | 6250 | 236 | No | None | 1 | 3.50 | 417 | 71 | 93 |
| 12 | 29 | 20.8 | IIIC | No | Yes | 6250 | 48 | No | Radiation dermatitis, gr1 | 0 | 4.00 | 186 | N/A | N/A |
| 13 | 46 | 26.2 | IIIB | No | Yes | 5000 | 252 | No | None | 0 | 3.83 | 475 | N/A | N/A |
| 14 | 45 | 23.7 | IIB | Yes | Yes | 7000 | 71 | No | None | 1 | N/A | N/A | 55 | 87 |
| 15 | 34 | 22.2 | IIA | Yes | Yes | 5000 | 89 | No | Radiation dermatitis, gr1 | 0 | N/A | N/A | 52 | 66 |
Interval between surgery and RT (days), SrOA: surgeon-reported aesthetic outcome; BMI: body mass index; RT: radiotherapy; OP to Photo being assessed (days); Breast Q-1 (Satisfaction with breast); Breast Q-2 (Psychosocial well-being)
Complication profile
There were no significant differences in the acute complication rates between the two groups (Table 4). For long-term complications, to allow of comparable period, the non-PMRT group long-term complications were represented as overall complications and complications that occur after 48 days. This period was chosen as the earliest time when the PMRT group patients received irradiation was 48 days. In this group, there were only three patients who required removal of clinically significant fat necrosis. In comparison, there were no surgical complications in the PMRT group after radiotherapy. However, 4/15 patients in the PMRT group suffered from grade 1 radiation dermatitis post-radiation therapy that eventually recovered, while 1/15 in the PMRT group developed permanent radiation-related skin pigmentation changes (Table 4).
Table 4.
A comparison of post-operative and post-radiotherapy complications between non-PMRT and PMRT.
| Non-PMRT group (n = 86) | PMRT group (n = 15) | p | |||
|---|---|---|---|---|---|
| Acute surgical complications (< 30 days) | |||||
| Mastectomy skin flap necrosis | 0 | 0 | |||
| Haematoma required evacuation | 0 | 1 (6.7) | 1.000 | ||
| Infection requiring admission | 0 | 0 | |||
| Partial flap failure | 2 (2.3) | 0 | 1.000 | ||
| NAC necrosis | 1 (1.2) | 0 | 1.000 | ||
| Radiation specific complication | |||||
| Acute dermatitis | N/A | 4 (26.7) | |||
| Permanent pigmentation change | N/A | 1 (6.7) | |||
| Long-term surgical complications (> 30 days) | |||||
| Overall | After 48 days | Overall | After RT | ||
| Wound required surgical intervention | 1 (1.2) | 0 | 0 | 0 | |
| Fat necrosis required surgical intervention | 3 (3.5) | 3 (3.5) | 0 | 0 | |
Values are presented as number (%). PMRT: post-mastectomy radiotherapy; NAC: nipple-areolar complex; RT: radiotherapy
Rate of revision surgeries
The requirement for revisional surgery was 0.6 times in the PMRT group as opposed to 0.5 times per patient in the non-PMRT group (Table 5). Most of the revisional surgery were scar revision, in 33.7% of non-PMRT group and 40% in the PMRT group (p = 0.637). Fat grafting rate to improve breast contour tend to be higher but without statistical difference in the PMRT group (26.7%) than in the non-PMRT group (12.8%) (p = 0.230). Other revisional surgeries for asymmetrical IMF, breast symmetrizing procedure and liposuction also did not show significant differences, with PMRT group having a lower rate in each of these categories (Table 5).
Table 5.
A comparison between the two groups the total revisional surgeries required between non-PMRT group and PMRT group.
| Non-PMRT group (n = 86) | PMRT group (n = 15) | p | |
|---|---|---|---|
| Revision / person (times) | 0.5 | 0.6 | 0.905 |
| Types of revisional surgery | |||
| Breast scar revision | 29 (33.7) | 6 (40) | 0.637 |
| Symmastia correction | 1 (1.2) | 0 | 1 |
| IMF position adjustment | 6 (7.0) | 1 (6.7) | 1 |
| Liposuction of flap | 8 (9.3) | 2 (13.3) | 0.641 |
| Fat grafting for volume loss | 11 (12.8) | 4 (26.7) | 0.230 |
| Symmetrization procedure (i.e. ptosis) | 1 (1.2) | 0 | 1 |
Values are presented as mean or number (%). All PMRT patients only underwent revision surgery after completion of adjuvant radiotherapy. All revisions are completed within 6 months post-radiotherapy. PMRT: post-mastectomy radiotherapy, IMF: inframammary fold
Surgeon-reported aesthetic outcome (SrAO)
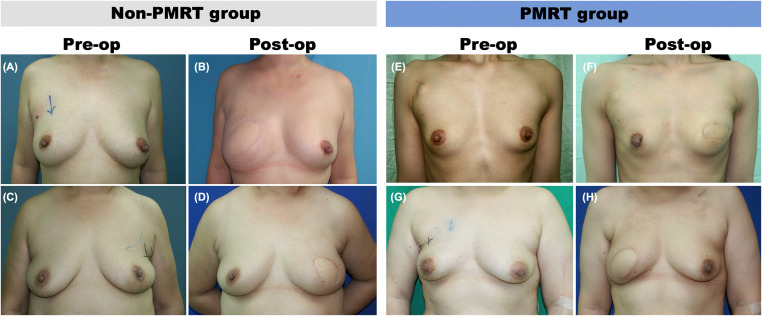
Complete postoperative photos were available for 91 patients, including 12/15 in the PMRT group and 79/86 in the non-PMRT group (Figure 1). The postoperative aesthetic outcomes rated by plastic surgeons are listed in Table 6. All patients had completed their revisional surgeries at this point of the assessment. The outcomes were comparable between the PMRT and the non-PMRT groups. The mean score of breast shape, volume, and overall outcome tends to be higher in the non-PMRT group, but the PMRT has a slightly narrow SD with the ratings between 3.1 to 4 (Table 6).
Figure 1.
(Left) Preoperative and postoperative results of two patients without PMRT. (A,B) A stage II breast cancer patient aged 45 who received right breast skin-sparing mastectomy (SSM) and free DIEP flap breast reconstruction. (A) Her preoperative appearance. (B) The result at the follow-up of 11 months with aesthetic overall outcome score 4.5. (C,D) A 64-year-old female patient with left breast cancer, staged DCIS (Ductal carcinoma in situ), who received left breast SSM and immediate free DIEP flap breast reconstruction. (C) Preoperative appearance. (D) Result at the follow-up of 13 months with aesthetic overall outcome score 4.83. (Right) Preoperative and postoperative results of two patients received PMRT. (E,F) A 34-year-old female patient with left breast cancer staged III. She received SSM and immediate breast reconstruction with free DIEP flap, following with radiotherapy 4 months after the surgery. (E) Preoperative appearance. (F) Postoperative (39 months) and postradiotherapy result (33 months) with aesthetic overall outcome score 3.83. (G,H) A 37-year-old female patient with right breast cancer, staged III. Right breast SSM following with free DIEP flap reconstruction was performed. Radiotherapy was delivered 8 months after surgery. (G) Her preoperative appearance. (H) Postoperative result at follow-up of 18 months (10 months after radiotherapy) with aesthetic overall outcome score 4.67. Mild pigmentation of the spared skin was noted. Her breasts were otherwise symmetric.
PMRT: post-mastectomy radiotherapy; DIEP: deep inferior epigastric perforator.
Table 6.
Surgeon-reported aesthetic outcome questionnaire.
| Non-PMRT (n = 79) | PMRT (n = 12) | p | |
|---|---|---|---|
| Breast shape of reconstructive site | 4.1 ± 0.5 (2.50–4.83) | 4.0 ± 0.3 (3.50–4.50) | 0.424 |
| Symmetry of inframammary fold | 4.1 ± 0.6 (2.50–4.83) | 4.3 ± 0.5 (3.50–4.83) | 0.438 |
| Symmetry of volume | 4.0 ± 0.5 (2.33–4.83) | 4.0 ± 0.5 (3.33–4.67) | 0.987 |
| Symmetry of shape | 3.9 ± 0.6 (2.33–4.83) | 3.7 ± 0.5 (3.17–4.50) | 0.291 |
| Overall outcomes | 4.1 ± 0.5 (2.67–5.0) | 3.9 ± 0.4 (3.50–4.67) | 0.342 |
Values are presented as mean ± SD (range).
Patient-reported outcome (BREAST-Q)
All questionnaires were completed at least 1 year after the reconstruction (Table 7). Forty-five patients completed the postoperative BREAST-Q reconstruction module, 36 out of 86 (respond rate = 41.9%) in the non-PMRT group and nine out of 15 (respond rate = 60%) in the PMRT group (Table 7). Patients reported no statistically significant differences in scores in all but one of the assessed BREAST-Q domains between these two groups. Patients in the PMRT group has a significantly lower score in the physical well-being (chest) domain comparison to the non-PMRT group (60.1 ± 20.3 versus 73.9 ± 17.3; p = 0.05) (Table 7). Several other categories were also lower in the PMRT group but did not reach statistical significance. The breast satisfaction scored 60.1 (range 48–78) in the PMRT group as opposed to 65.1 (range 34–100) in the non-PMRT group. The psychosocial well-being was 66.2 (range 43–93) in the PMRT group and 75.1 (range 43–100) in the non-PMRT group. The sexual well-being was 44.1 (range 0–62) as opposed to 50.8 (range 0–100). Twenty-five percent of the responders in the non-PMRT group and 11% of the PMRT group patients left questions specific to sexual activities blank under the sexual well-being domain.
Table 7.
Patient-reported outcomes (Breast-Q).
| Non-PMRT (n = 36) | PMRT (n = 9) | p | |
|---|---|---|---|
| BREAST-Q domains | |||
| Psychosocial well-being | 75.1 ± 17.3 (43–100) | 66.2 ± 20.1 (43–93) | 0.192 |
| Physical well-being (chest) | 73.9 ± 17.3 (36–100) | 60.1 ± 20.3 (24–85) | 0.045* |
| Physical well-being (donor site) | 78.3 ± 18.4 (39–100) | 73.2 ± 28.6 (9–100) | 0.515 |
| Sexual well-being | 50.8 ± 22.4 (0–100) | 44.1 ± 18.3 (0–62) | 0.644 |
| Satisfaction with breasts | 65.1 ± 14.8 (34–100) | 60.1 ± 10.4 (48–78) | 0.350 |
| Satisfaction with surgeon | 92.8 ± 13.5 (46–100) | 95.2 ± 9.6 (75–100) | 0.621 |
| Satisfaction of information from surgeon | 74.8 ± 18.3 (48–100) | 74.0 ± 15.1 (56–100) | 0.904 |
| Satisfaction with medical team | 93.1 ± 14.5 (53–100) | 97.3 ± 5.5 (85–100) | 0.396 |
| Satisfaction with other staff | 89.7 ± 17.1 (53–100) | 93.9 ± 13.0 (63–100) | 0.499 |
| OP time to BREAST-Q (years) | 3.23 ± 2.66 (1.04–10.63) | 3.29 ± 2.12 (1.50–7.19) | 0.939 |
Values are presented as mean ± SD (range). PMRT: post-mastectomy radiotherapy; OP: operation
Discussion
In this retrospective analysis, the data showed that there were no unexpected oncological outcomes, no significant differences in postoperative complications and revision rates in comparison to the non-PMRT cohort. Moreover, the final aesthetic outcome as assessed by surgeons indicates that while there may be a marginally lower rating, it is within acceptable range. This current study also reported one of the largest cohorts of Asian patients PRO using BREAST-Q reconstruction module in perforator-based free flap reconstruction.
The recurrence rate in the PMRT group was within acceptable range. In three cases with recurrence, it manifested as distant metastases. All three cases were stage 3 using TNM (tumor-node-metastasis) staging. Furthermore, none of the cases had delayed adjuvant treatment secondary to flap complications. Recurrence rate reported is comparable to similar groups reported in South Korea,14 as well as the United States15 at approximately 30% and 20% respectively within 2 years follow-up. In this study, the distant metastasis rate is 20% with a mean follow-up of 5 years with all patients alive. The interval between surgery and radiotherapy can be up to 8 months if adjuvant chemotherapy is required. At the author's institution, radiotherapy tends to commence after completion of chemotherapy.
There were no significant differences in the complication rate between the two groups. The most significant complication with impact on the aesthetic outcomes would be the radiation related permanent pigmentation change, which is rare. Fat necrosis or wound issues requiring surgical treatment were extremely low in this study. In the literature, the fat necrosis rate historically was cited as high as 43.8%16 using free TRAM flap for reconstruction. However, in a recent systematic review in 2021,3 the fat necrosis rate is around 15% in immediate autologous breast reconstruction with adjuvant radiotherapy. Several studies also reported no difference in complications rates in general between autologous reconstruction with or without PMRT.17,18 O'Connell et al speculate improved microsurgical technicalities in perforator flaps and more sophisticated radiation delivery explains this trend.19 Several studies reporting on immediate DIEP flap reconstruction with adjuvant radiotherapy seemed to mirror complication rate of the current study.4,20
The final aesthetic outcome by SrAO scores of the PMRT group aesthetic outcomes were above 3, with the mean score of the overall outcome being 3.9. When compared to the patients in the non-PMRT group, the differences were not obvious. While the larger sample size of the non-PMRT group may have shown slight numerical superiority, the PMRT group's scores are quite concentrated around the mean score, suggesting an acceptable overall aesthetic outcome.21 Besides, there was no significant increase of revision rate in the PMRT group. A detailed looked at the data revealed one patient with four revisional surgeries who was not available for final outcome assessments and five patients with one revisional surgery. Thus, other than an outlier with four revisions, the revisional surgery rate was minimal.
PRO using BREAST-Q was overall lower in the PMRT group with a mean score of 60.1 (range 52–78) as opposed to the non-PMRT group (mean of 65.1, range 34–100). While this did not achieve statistical significance, most likely due to the small number of patients, it should be noted that six of the nine responded patient rated their breast satisfaction below the mean in other reported studies in Asian women.11,22 One could attribute this to the effect of PMRT, although Jagsi et al17 has shown that breast satisfaction was not affected by radiation in their study.
Finally, using a validated condition specific PRO BREAST-Q,12 the current study appears to show differences in PRO between two groups. While the patients were satisfied with the medical team and the care provided, the PMRT group has lower psychosocial well-being, sexual well-being and chest physical well-being. Differences are apparent when compared to normative data reported in the West,23 with our study cohort scoring lower than their counterparts in the West. It is difficult to speculate the differences due to the limitations of this study. However, these are topics worth exploring in future studies. As aforementioned, BREAST-Q in assessing PRO in perforator flap-based reconstruction is not common in the Asian population.6,9,11,22 Data derived from this study will be helpful in further longitudinal studies for the counselling and support of the local patient population.
The current study is limited by its retrospective nature and small patient numbers in the PMRT group to have meaningful statistical analysis. The data collected is cross-sectional, and some of the data can be more meaningful when examined in a longitudinal fashion.24 Obtaining PRO using BREAST-Q in this study will help with future data collection and hopefully allow researchers to understand differences in the perceived experience of Asian women from different regions. Although this is a small cohort without a control group from a Western country and thus cannot fully represent the situation in Asia, it provided additional information from Asian women as a reference. Well-designed prospective multicenter trial utilizing BREAST-Q is underway in Japan (SAQLA, Satisfaction and Quality of Life After Immediate Breast Reconstruction, study)25 and China26 which will provide more information in this important topic.
Conclusion
Immediate perforator flap-based breast reconstruction with adjuvant radiotherapy is oncologically safe, with acceptable complication rate and frequency of revisional surgery in this study population. A rare but worst-expected complication is permanent pigmentation change, and patients should be warned about this possibility. The final aesthetics may be affected, but is within acceptable range. In general, however, patient's own reported breast satisfactory rate and psychological outcomes may be slightly inferior to patients without PMRT. Further study will need to examine if it is confounded by the experience of adjuvant therapy or related to other factors such as anxiety regarding poorer tumour prognosis.
Conflicts of interest
The authors declare that they have no conflict of interest.
Declarations
Ethics approval and consent to participate: This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the institutional review board of Chang Gung Medical Foundation (IRB number: 201900634B0).
Consent for publication: Informed consent was obtained from the patient included in this study.
Availability of data and materials: The raw datasets generated within this study are available from the corresponding author on reasonable request.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements: None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jpra.2023.09.001.
Appendix. Supplementary materials
References
- 1.Heimes AS, Stewen K, Hasenburg A. Psychosocial aspects of immediate versus delayed breast reconstruction. Breast Care (Basel) 2017;12:374–377. doi: 10.1159/000485234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schaverien MV, Macmillan RD, McCulley SJ. Is immediate autologous breast reconstruction with postoperative radiotherapy good practice?: A systematic review of the literature. J Plast Reconstr Aesthet Surg. 2013;66:1637–1651. doi: 10.1016/j.bjps.2013.06.059. [DOI] [PubMed] [Google Scholar]
- 3.Hershenhouse KS, Bick K, Shauly O, et al. Systematic review and meta-analysis of immediate versus delayed autologous breast reconstruction in the setting of post-mastectomy adjuvant radiation therapy. J Plast Reconstr Aesthet Surg. 2021;74:931–944. doi: 10.1016/j.bjps.2020.11.027. [DOI] [PubMed] [Google Scholar]
- 4.Clarke-Pearson EM, Chadha M, Dayan E, et al. Comparison of irradiated versus nonirradiated DIEP flaps in patients undergoing immediate bilateral DIEP reconstruction with unilateral postmastectomy radiation therapy (PMRT) Ann Plast Surg. 2013;71:250–254. doi: 10.1097/SAP.0b013e31828986ec. [DOI] [PubMed] [Google Scholar]
- 5.Sebastin SJ, Chung KC. A systematic review of the outcomes of replantation of distal digital amputation. Plast Reconstr Surg. 2011;128:723–737. doi: 10.1097/PRS.0b013e318221dc83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang B, Li L, Yan W, et al. The type of breast reconstruction may not influence patient satisfaction in the Chinese population: A single institutional experience. PLoS One. 2015;10 doi: 10.1371/journal.pone.0142900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levine SM, Levine A, Raghubir J, Levine JP. A 10-year review of breast reconstruction in a university-based public hospital. Ann Plast Surg. 2012;69:376–379. doi: 10.1097/SAP.0b013e31824b26d2. [DOI] [PubMed] [Google Scholar]
- 8.Lee KC, Kim TH, Park SS, et al. Reliability of reconstructed breast flap after chemotherapy and radiotherapy in immediate breast reconstruction. Arch Plast Surg. 2012;39:497–503. doi: 10.5999/aps.2012.39.5.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim EK, Eom JS, Ahn SH, Son BH, Lee TJ. Evolution of the pedicled TRAM flap: A prospective study of 500 consecutive cases by a single surgeon in Asian patients. Ann Plast Surg. 2009;63:378–382. doi: 10.1097/SAP.0b013e3181951708. [DOI] [PubMed] [Google Scholar]
- 10.Chao LF, Patel KM, Chen SC, et al. Monitoring patient-centered outcomes through the progression of breast reconstruction: A multicentered prospective longitudinal evaluation. Breast Cancer Res Treat. 2014;146:299–308. doi: 10.1007/s10549-014-3022-7. [DOI] [PubMed] [Google Scholar]
- 11.He S, Yin J, Robb GL, et al. Considering the optimal timing of breast reconstruction with abdominal flaps with adjuvant irradiation in 370 consecutive pedicled transverse rectus abdominis myocutaneous flap and free deep inferior epigastric perforator flap performed in a Chinese oncology center: Is there a significant difference between immediate and delayed? Ann Plast Surg. 2017;78:633–640. doi: 10.1097/SAP.0000000000000927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q. Plast Reconstr Surg. 2009;124:345–353. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 13.Cano SJ, Klassen AF, Scott AM, Cordeiro PG, Pusic AL. The BREAST-Q: Further validation in independent clinical samples. Plast Reconstr Surg. 2012;129:293–302. doi: 10.1097/PRS.0b013e31823aec6b. [DOI] [PubMed] [Google Scholar]
- 14.Lee TJ, Hur WJ, Kim EK, Ahn SH. Outcome of management of local recurrence after immediate transverse rectus abdominis myocutaneous flap breast reconstruction. Arch Plast Surg. 2012;39:376–383. doi: 10.5999/aps.2012.39.4.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crisera CA, Chang EI, Da Lio AL, Festekjian JH, Mehrara BJ. Immediate free flap reconstruction for advanced-stage breast cancer: Is it safe? Plast Reconstr Surg. 2011;128:32–41. doi: 10.1097/PRS.0b013e3182174119. [DOI] [PubMed] [Google Scholar]
- 16.Tran NV, Chang DW, Gupta A, Kroll SS, Robb GL. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg. 2001;108:78–82. doi: 10.1097/00006534-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Jagsi R, Momoh AO, Qi J, et al. Impact of radiotherapy on complications and patient-reported outcomes after breast reconstruction. J Natl Cancer Inst. 2018;110:157–165. doi: 10.1093/jnci/djx148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang EI, Liu TS, Festekjian JH, Da Lio AL, Crisera CA. Effects of radiation therapy for breast cancer based on type of free flap reconstruction. Plast Reconstr Surg. 2013;131:1e–8e. doi: 10.1097/PRS.0b013e3182729d33. [DOI] [PubMed] [Google Scholar]
- 19.O'Connell RL, Di Micco R, Khabra K, et al. Comparison of immediate versus delayed DIEP flap reconstruction in women who require postmastectomy radiotherapy. Plast Reconstr Surg. 2018;142:594–605. doi: 10.1097/PRS.0000000000004676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu T, Freijs C, Klein HJ, et al. Patients with abdominal-based free flap breast reconstruction a decade after surgery: A comprehensive long-term follow-up study. J Plast Reconstr Aesthet Surg. 2018;71:1301–1309. doi: 10.1016/j.bjps.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 21.El-Sabawi B, Ho AL, Sosin M, Patel KM. Patient-centered outcomes of breast reconstruction in the setting of post-mastectomy radiotherapy: A comprehensive review of the literature. J Plast Reconstr Aesthet Surg. 2017;70:768–780. doi: 10.1016/j.bjps.2017.02.015. [DOI] [PubMed] [Google Scholar]
- 22.Kim KD, Kim Z, Kuk JC, et al. Long-term results of oncoplastic breast surgery with latissimus dorsi flap reconstruction: A pilot study of the objective cosmetic results and patient reported outcome. Ann Surg Treat Res. 2016;90:117–123. doi: 10.4174/astr.2016.90.3.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mundy LR, Homa K, Klassen AF, Pusic AL, Kerrigan CL. Breast cancer and reconstruction: Normative data for interpreting the BREAST-Q. Plast Reconstr Surg. 2017;139:1046e–1055e. doi: 10.1097/PRS.0000000000003241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu LQ, Branford OA, Mehigan S. BREAST-Q measurement of the patient perspective in oncoplastic breast surgery: A systematic review. Plast Reconstr Surg Glob Open. 2018;6:e1904. doi: 10.1097/GOX.0000000000001904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saiga M, Hosoya Y, Utsunomiya H, et al. Protocol for a multicentre, prospective, cohort study to investigate patient satisfaction and quality of life after immediate breast reconstruction in Japan: The SAQLA study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-042099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li L, Yang B, Li H, et al. Chinese multicentre prospective registry of breast cancer patient-reported outcome-reconstruction and oncoplastic cohort (PRO-ROC): A study protocol. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-032945. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.