Abstract
Background
The aim of this study was to assess and compare the vertical/horizontal dimensions and occlusal accuracy of non-working/opposing casts obtained from three different impression materials and 3D print cast.
Material/Methods
Dentulous Master models simulating a case of a fixed dental prosthesis were mounted on an articulator (control group). Opposing mandibular casts obtained from three different impression materials [Hydrogum Alginate (Conventional), Hydrocolor 5 (Extended-Pour Alginate), FreeAlgin (Alginate Alternative)] and 3-dimensional print constituted test groups [Gp AL(C)], [Gp AL(E)], [Gp AL(F)] and [Gp 3D-C], respectively. Three points, anterior vertical (AV), posterior vertical (PV), and anteroposterior (AP) were compared for dimensional accuracy among casts. Occlusal accuracy was analyzed on Medit Link software at 3 teeth (#13, #17, and #27). After calculating means for each group, the differences were calculated at probability value of P≤0.05 using the single-sample t test, ANOVA, and Tukey test.
Results
The dimensions were significantly different from those of the mounted master models except in Gp AL(E) and Gp AL(F) at AV dimension and Gp AL(E) at AP dimension (P>0.05). A statistically significant difference of the error of means among the 4 tested groups [Gp AL(C), Gp AL(E), Gp AL(F), and Gp 3D-C] were detected only at 2 dimensions (AV and PV) between the Gp AL(E) and Gp 3D-C and between Gp AL(F) and Gp 3D-C groups. Other groups showed no significant differences.
Conclusions
The opposing casts obtained from the extended-pour alginate and alginate alternative impression materials showed higher occlusal accuracy compared to conventional alginate and 3D printed casts.
Keywords: Alginates; Dental Casting Technique; Dental Occlusion, Centric; Digital Technology
Background
A competent and efficient occlusal scheme is essential for the health of a biologically functioning temporomandibular joint. The joint is overly sensitive to changes in occlusal load, which can assimilate during a routine fixed prosthodontic treatment (single-crown, fixed partial denture, implant-supported fixed prosthesis). It is unanimously accepted that fixed dental prosthesis (FDP) in occlusal harmony is a key objective of clinical practice [1]. Biological tolerance of an individual to occlusal changes like a premature, uneven, or high contact is extremely low, which is one of the primary reasons why chairside adjustment of FDP is invariably required despite using highly sophisticated instruments and technology. Chairside FDP occlusal adjustment can be difficult and tiring for both patient and clinician and has been reported to be one of the most frequent sources of frustration for a clinician [2], wasting valuable clinical time and risking loss of patient trust [3,4]. In extreme but common cases, it is mandatory for the clinician to remake the FDP, the financial burden of which becomes the clinician’s sole obligation. The remake rate of single-unit crowns at the scheduled delivery appointment has been reported to be 42% even after efforts at chairside adjustment [5]. Traditionally, FDPs are indirect restorations fabricated in dental laboratories by specialized dental technicians who rely heavily on the accuracy of impressions provided by the clinician. Accurate arch impressions are significantly affected by a clinician ‘s skill and techniques and are considered essential for FDP’s overall fit [6,7]. FDP misfit has been attributed to multiple factors that include poor communication (dentist and technician) [8], inadequate clinical procedures (gingival retraction) [9], and inherent inaccuracies of materials used in the laboratory (eg, dental stone, die materials, dental waxes, dental alloy, and porcelain) [8]. Irrespective of all due care and precautions exercised and despite the prior examination of prosthesis for occlusal contacts on articulated casts verifying them as correct, FDPs continued to be occlusally inaccurate upon final testing [10]. Introduction of computer-aided diagnosis and computer-aided machining (CADCAM) in dentistry with subsequent demand [11], has led to refinement of early heavy dental CADCAM systems, large scanners (3-dimensional) and multi-axis machines, to present-day automated scanners, lightweight milling machines (tabletop), and a plethora of customized software. Present-day digital dental technology using fully digital workflow have overcome many laboratory-related inaccuracies and have bettered or equaled traditional laboratory methods in terms of accuracy [12], efficiency, and methods preferred by both consumers (patients) and providers (clinicians) [13]. Highly sensitive intra-oral scanners eliminate impression material-related variations and collect analyzable data from a patient’s mouth; data are processed in the laboratory to make the restoration without use of a working model [14]. This direct method of obtaining required data from the patient is more accurate than the indirect method (from impression or a cast), but is limited by oral conditions (eg, salivary influence, space restriction, access to intricate areas) [15]. The indirect method (scanning of the cast) has also been shown to demonstrate better prosthesis adaptation than the direct method [15]. Laboratory fabrication of restorations has also been digitalized, from traditional manufacturing (casting using the lost wax technique) to sophisticated subtractive (milling) or additive manufacturing (3D printing) [16]. Additive manufacturing like 3D printing has an added advantage over milling, which allows it to fabricate anatomical structures that cannot be milled due to milling tool size limitations [17]. Other merits of 3D printing include reduced material loss, multiple/simultaneous production at a given time and replication of minute occlusal features [18]. However, the problem of clinical adjustment persists with several types of restorations manufactured digitally, some of which are harder to adjust, while others cannot be compensated, attributed chiefly to the materials used in fabrication of digitally fabricated restorations [19]. It is important to realize that all clinical adjustments are subjective (depending on the patient and clinician) and there is no accurate method that clinically determines the exact amount of adjustment that the clinician must make [20]. While the location of areas for adjustment can be identified, subjective removal can lead to loss of functional contact in occlusion (tripod cusp contact) [21], which renders the restoration functionally ineffective in terms of cusp-to-fossa contact with opposing tooth/teeth.
For achieving a technically, functionally, and esthetically acceptable indirect restoration involving occlusion, the focus has mostly centered on accurate reproduction of involved teeth (working cast), which are critically important for locating occlusal contacts and their intensity [22]. There has been little focus on the quality of opposing casts, which could be a potential source of inaccuracy in the completed restoration of the working cast. Despite having accurate definitive impression materials like addition of silicones, there are no studies that recommend the opposing or working cast to made using such impression materials. Alginate (irreversible hydrocolloid) continues to be the most common impression material used for making diagnosis, study, and opposing casts in both fixed/removable prosthesis and orthodontic related treatment procedures [23]. Despite having well established disadvantages like syneresis and imbibition, newer alginates have been formulated and marketed, with manufacturer’s claiming to have 5 days of dimensional stability (extended-pour alginates) and are scannable, which allows them access to digital workflow. Economic alternatives to alginates are called alginate alternatives (FreeAlgin), which are low-cost vinyl polysiloxane impression materials [24]. In FDP-related clinical practice, various alginates are used to make opposing arch impressions despite evidence that it contributes to occlusal discrepancies (high restorations) in final restorations [25]. All completed indirect restorations need to be evaluated on the working cast against the opposing non-working casts, which are mounted on an articulator using an inter-occlusal record with a vinyl polysiloxane bite registration material. The exquisitely detailed occlusal anatomy recorded by VPS bite registration paste is not replicated by alginate-made opposing casts, which in turn hampers accurate seating of the registration record [26]. Based on their comparative findings, authors have recommended the use of alginate alternatives for making an opposing arch impression [26]. Digitally manufactured restorations that involve locating precise occlusal contacts can be designed, and fabricated digitally (digital cast, and digital articulation) [27], but without a physical model, the complex treatment planning and appliance fabrication are challenging [28]. 3D-printed models for orthodontic purposes have been reported to have greater accuracy than milling methods [29]. The 3D printer uses four different techniques: stereolithography apparatus (SLA), triple jetting technology (PolyJet), digital light processing (DLP), and continuous liquid interface production (CLIP). SLA technology uses a laser (ultraviolet) to polymerize the drops of resin into the desired shape. The PolyJet technique is like an inkjet printer in that it applies drops of polymerizable polymer onto a building platform. The DLP technology uses a digital projector as the light source to polymerize the liquid resin layer-by-layer across the entire platform [30]. A study has compared the accuracy in terms of trueness and precision between SLA and PolyJet techniques, with better trueness in SLA models, while PolyJet models had better precision [31]. Another study has reported that the volumetric changes in casts obtained by conventional methods were significantly higher than 3D-printed models (assessed using three different printers) [32]. Another study comparing the accuracy of SLA 3D printing, digital models, and conventional dental stone casts (polyvinylsiloxane impression and dental stone), found the accuracy of SLA 3D printing was slightly inferior to that of stone casting [33]. Tooth arch measurement comparisons between digital models, 3D printing (DLP and PolyJet), and stone models (alginate impression poured with dental stone) showed high degrees of consensus for all studied parameters except crown height, with linear dimensions on printed models being less accurate than in stone models, with an error range of 0.20 to 0.30 mm [34]. Most studies on accuracy relate to the physical dimensions, which are significant for all purposes, but in relation to FDP, the most relevant is the digital occlusal contact recording, which is performed clinically using articulating foils and papers, silicone impressions, and bite waxes [35]. Digital articulation utilizing buccal scans for digital casts has been found to be at least equivalent to the conventional method in one study [36], and more accurate than conventional methods in another study [27,37]. Interpretation of digital occlusions was well defined in a study based on T-scan analysis in terms of identifying artifacts, pressure areas, occlusal threshold, and high points [35].
Studies evaluating use of alginate alternatives and extended-pour alginate as opposing cast to the digitally fabricated restoration (working cast) in terms of occlusal accuracy are lacking; therefore, the present study aimed to compare the occlusal accuracy of opposing casts generated through conventional alginate, extended-pour alginate, alginate alternative impression material, and 3D print cast. Our main objective was to determine which material is most suitable as an opposing cast so that the smallest possible errors in occlusion are incorporated during indirect restoration fabrication. We hypothesized that there would be significant differences between diverse materials based on different chemical ingredients. Alternately, the null hypothesis was that there would be no significant differences between opposing casts generated using these four varied materials/techniques in terms of occlusal accuracy.
Material and Methods
Ethics
This in vitro study was proposed to and approved by the Scientific Research Unit, College of Dentistry, Jazan University on 24th March 2022 (Reference No. CODJU-2203F).
Study Design
This in vitro study utilized a comparative study approach with strict adherence to standardization of materials/techniques/instruments/procedures used during fabrication of the test samples. The measurement of data was done by a calibrated examiner who was blinded to the groups/study outcome and test sample identity.
Operational Definition
The working cast was defined as any cast that replicated the prepared tooth and ridge area in a quadrant/arch. The opposing or non-working cast was defined as any cast that replicated the opposite arch of the working cast and was used to determine the occlusion of the restoration after completion. 3D printing was defined as a procedure which prepared a physical object from a previously scanned object by laying down multiple layers and subsequently polymerizing them in succession.
Estimation of Sample Size
Assuming the study power (85%) with an alpha error of 5%, the minimum sample size estimated for the study (5 groups) through power analysis [38] was kept as ten specimens per group. One extra specimen was added to replace any faulty specimen.
Material Selection, Sample Preparation, and Grouping
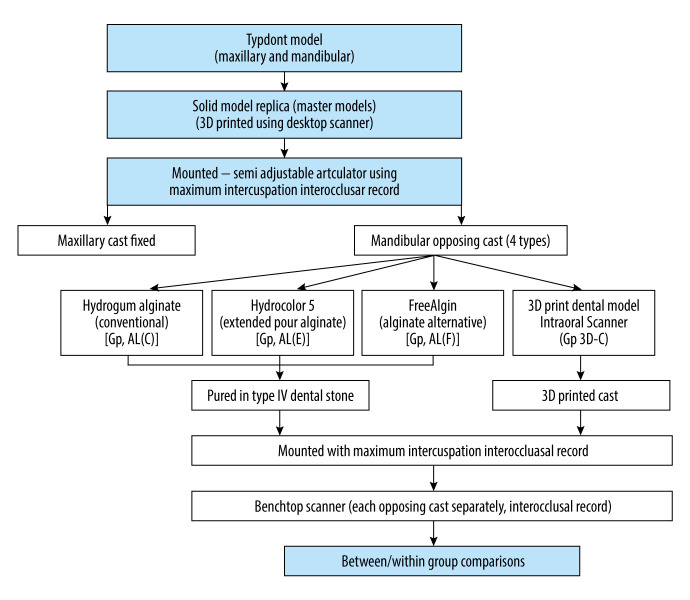
All materials and instrumentation with their specification are presented in Table 1. An organized layout of the study is presented in a flowchart (Figure 1). To simulate a clinical case scenario, a maxillary/mandibular typodont model (Frasaco GmbH, Tettnang, Germany) containing a full set of typodont teeth (teeth – acrylic, soft tissues – silicone rubber) were used to represent the master model (Control) against which comparisons were made. Maxillary tooth number 15 (right second premolar) was removed to represent a missing tooth, with adjacent teeth (#14 and #16) serving as abutments for the FDP. Standard all-ceramic tooth preparation was done for adjacent teeth (#14 and #16) using a flat-end diamond bur (6856 314 016, Komet, Germany) on a high-speed hand piece (KaVo do Brazil Ind. Com. Ltd., Joinville, SC, Brazil) mounted to a dental cast surveyor (A3005 Surveyor Type A; Dentalfarm). Tooth preparation was done according to the standard principles of tooth preparation [39] (Table 1 shows tooth preparation specifications), which was verified through a multi-sectional putty index (addition of silicone) and a graduated (in millimeters) periodontal probe. An opposing mandibular typodont model that contained a full set of teeth was used to represent the opposing cast for the master model. The maxillary and mandibular Typodont models were then scanned with a benchtop scanner (Medit, Model MD-ID0300, Medit Corp., Seoul, South Korea), following which the data was transferred to a 3D printer (ST-1600, Satori Ltd., London, UK) to print 1 maxillary and 1 mandibular solid model using photopolymerized liquid resin (NextDent, Vertex-Dental B.V., Soesterberg, The Netherlands). The fabrication of solid models not only overcame the problem of loose typodont teeth affecting the scan process, but also represented the routine clinical and laboratory procedures when digital data of the impression of the patient are transferred to the dental laboratory. These 3D maxillary and mandibular models represented the master models, which were mounted on predetermined vertical dimension of occlusion on a semi-adjustable articulator (BioArt A7 plus, São Carlos, São Paulo, Brazil) (Figure 2). The maxillary master model was mounted using a compatible facebow (BioArt A7 plus, São Carlos, São Paulo, Brazil), while the mandibular master model was mounted in the maximum intercuspation position using hand articulation, with the incisal pin of the articulator touching the incisal guide table at zero inclination on the anterior guidance table. Three reproducible and repeatable indentations were made on the maxillary master model (A1 – anterior between the maxillary central incisors; P1 – posterior at maxillary right first molar, and P2 – posterior between maxillary right 1st and 2nd premolars) (Figure 3). Similarly, three indentations were made on the mandibular master model (A2 – anteriorly between mandibular central incisors parallel to the anterior indentation made in the maxillary master model; P3 – posterior at mandibular right first molar, and P4 – posterior between mandibular right 1st and 2nd premolars). All indentations were prepared just 2 mm below the gingival margin to enable registering the indentation in the mandibular master model with the impression.
Table 1.
Armamentarium, materials used and group distribution in the study.
| Material | Group | Manufacturer/specifications/features |
|---|---|---|
| Maxillary Typodont (Master Model) | (Control Gp) |
|
| Hydrogum Alginate (Conventional) | Gp AL(C) |
|
| Hydrocolor 5 (Extended Pour Alginate) | Gp AL(E) |
|
| FreeAlgin (Alginate Alternative) | Gp AL(F) |
|
| 3D Print Dental Model Resin (Yellow) | Gp 3D-C |
|
| 3D Printer |
|
|
| Advance (#387314), Full Arch Bite Trays |
|
|
| A-Silicone bite registration (Air) |
|
|
| Benchtop 3D Scanner |
|
|
| Intraoral scanner |
|
|
| LCD 3D Printer (Photopolymer Resin) |
|
|
| Imaging powder |
|
|
| Semi-Adjustable Articulator |
|
|
| Type IV Die Stone |
|
|
| Mounting Stone |
|
|
| Vacuum Mixer |
|
|
| Vibrator |
|
|
| Zeta 7 solution/spray |
|
|
| Tooth Preparation Specifications |
|
|
Gp – Group; AL(C) – conventional alginate; AL(E) – extended pour alginate; AL(F) – alginate free (Alginate alternative); 3D-C – three-dimensional printed cast.
Figure 1.
Flow chart showing sample preparation and group distribution. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft corporation).
Figure 2.

Master models mounted on a semi-adjustable articulator (BioArt A7 plus). Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft corporation).
Figure 3.
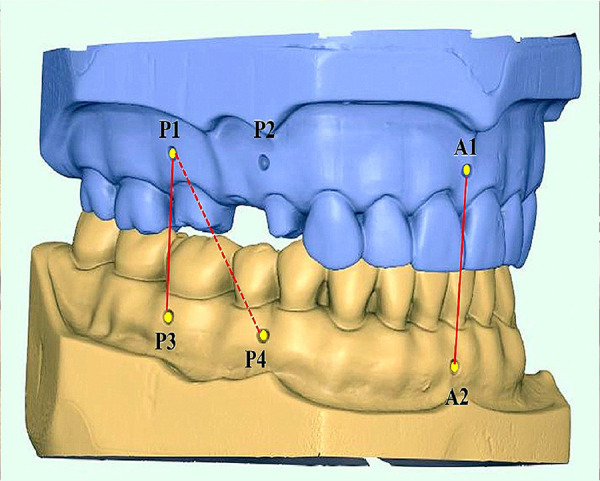
Three repeatable and reproducible indentations made on the maxillary and mandibular master models with A1 between maxillary central incisors, A2 between mandibular central incisors, P1 at right maxillary first molar, P2 between maxillary right first and second premolar, P3 at mandibular first molar and P4 between mandibular right first and second premolar. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft corporation).
Fabrication and Mounting of Opposing (Non-Working) and 3D-Printed Casts
A metallic rim lock perforated (mandibular) stock tray was selected to fit on the mandibular typodont model with at least a gap of 4 mm between the border of the tray and the surfaces of the teeth on either side. A total of ten perforated impression trays were used (size 6) to make ten conventional impressions for each group: Hydrogum Alginate (Conventional) [Gp AL(C)], Hydrocolor 5 (Extended-Pour Alginate) [Gp AL(E)], and FreeAlgin (Alginate Alternative) [Gp AL(F)]. All impressions were poured with vacuum (Mix-R, Dentalfarm, Torino, Italy)-mixed stone (type IV) (Elite Rock, Zhermack, Italy), and poured on the vibrator (Dentalfarm, Italy) according to the manufacturer’s recommendations. The mandibular master model was then scanned ten times with a Medit intra-oral scanner (Medit i700, Medit, Seoul, South Korea) and sent to the production laboratory for printing [three-dimensional (3D)] using a 3D printing machine (ST-1600, Satori, Ltd., London, UK). The stereolithography (SLA) machine printed ten models (3DCAST) using the photopolymerized liquid resin (JAMG HE, LOT No. WX353N02, Shenzhen, Guangdong, China), which represented the fourth test group for the study [Gp 3D-C]. In total, forty mandibular models obtained under four diverse groups (10 each) represented four different types of opposing casts: two from the alginate-related impression, 1 alginate alternative, and 1 3D-printed cast.
Mounting of mandibular models for each group against previously mounted maxillary master model was done using silicone bite registration paste (Maxill, Cortland, OH, USA), which was injected on a bite tray to make a bite registration record at the maximum intercuspation position. The bite registration record was used for mounting the mandibular stone casts made from the 3 impression materials, Hydrogum alginate (conventional), Hydrocolor 5 (Extended-Pour Alginate), FreeAlgin (Alginate Alternative), and the 3D-printed models (3DCAST) – with the upper maxillary master model being fixed standard (for all) on the semi-adjustable articulator (Figure 4). A 2-sided bite registration tray ensured standardization of interocclusal records.
Figure 4.
Four different mandibular casts mounted to the same maxillary master model cast on the semi-adjustable articulator using a maximum intercuspation bite registration record. Clockwise right - Hydrogum Alginate (Conventional) [Gp AL(C)], Hydrocolor 5 (Extended-Pour Alginate) [Gp AL(E)], 3D Print Dental Model (Gp 3D-C), FreeAlgin (Alginate Alternative) [Gp AL(F)]. Photographs taken using Digital Single-Lens Reflex (DSLR) (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft corporation)
Measurements and Data Evaluation, Collection, and Analysis
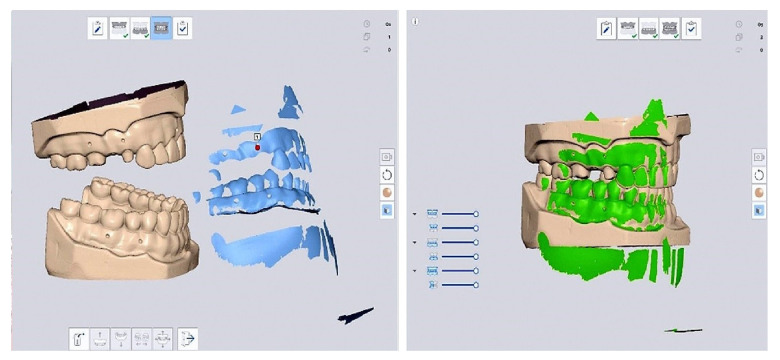
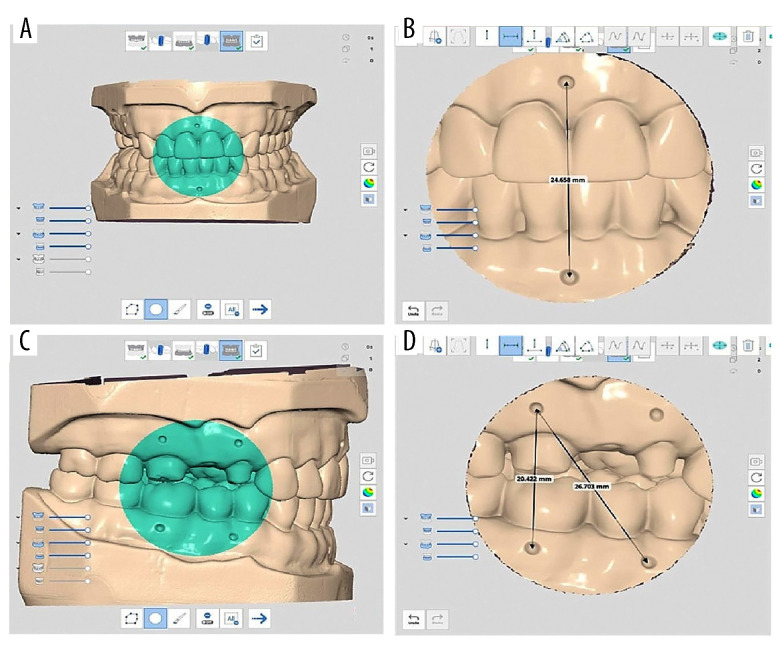
The distances between the pre-marked master models mounted on the articulator were measured for 3 different dimensions – A1–A2: Anterior Vertical (midline) for measurement of vertical changes anteriorly; P1–P3: Posterior Vertical for measurement of vertical changes posteriorly; and P1–P4: Diagonal posterior for measurement of anterior-posterior (horizontal) changes. The mounted maxillary and mandibular master models on the semi-adjustable articulator were further scanned with a benchtop 3D scanner (MD-ID0300, SN 1V19045DE406, Medit Corp., Seoul, South Korea). Three scan files were obtained for each mounted model (upper jaw, lower jaw, and bite for occlusion) at 1 time for one sample in each group. For scanning the bite, a customized compatible attachment was used for mounting the articulator on the benchtop scanner for repeatable and accurate positioning of all samples. Each cast was oriented to a level where the occlusal plane would lie in the same plane for each sample. For each case, the three files were imported into the Medit Link software (Medit Link v 2.4.4; Medit, Seoul, Republic of Korea) for measurement. The manual alignment tool in the software was used aligning of the maxillary and mandibular jaws using the bite (Figure 5). Once the digital models showed the desired occlusal contacts, the measurement tool was selected and used to measure the anterior vertical (A1–A2), posterior vertical (P1–P3), and anterior-posterior (P1–P4) distances between the digital master models and digital opposing casts of each group (Figure 6). Each distance on the articulated master models was measured ten times. Average values were calculated and used as the control to compare it with the four groups of the mounted maxillary master model and the mandibular casts in each group: Gp AL(C), Gp AL(E), Gp AL(F), and Gp 3D (C).
Figure 5.
Digital articulation between the maxillary and mandibular digital casts showing the casts separated and in articulation position after using the manual alignment tool in the software (Medit Link). Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft corporation).
Figure 6.
Digital measurement of reference points (A) Identifying the measuring landmarks (B) cropping the image and measuring the distance between anterior points (A1–A2) (C) identifying the posterior landmark area (D) cropped image to measure the posterior distances (P1–P3) and (P1–P4). Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft corporation).
Occlusal Accuracy
The occlusal contacts for each opposing cast in each group against the working cast (master model) were analyzed using Occlusal Analysis tools in Medit Link software (Medit Link v 2.4.4; Medit, Seoul, Republic of Korea) (Figure 7). The software system analyzes occlusion while displaying the results in a color map that has various intensities of blue and red with an intervening single color of green. The occlusal areas that are within the acceptable range of tolerance are shown in green [40,41]. The occlusal contacts in the green zone showing a deviation value of −0.100 to + 0.100 were considered the acceptable occlusal contacts. Areas that are high (occlusal interferences) are depicted as higher positive values on the screen with a change in color intensity (intensity signifies the amount). Non-interferences are colored with grades of blue color and have negative values.
Figure 7.
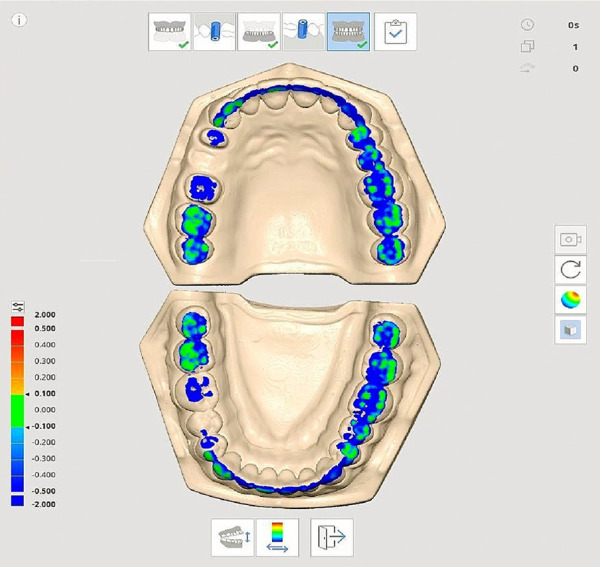
Digital occlusal analysis of articulated exemplary master model using Occlusal Analysis tool (Medit Link software) [Color green indicates occlusal contacts and the degree of occlusal contact (pressure) while blue indicates no contact. Compiled Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), windows 11 Pro, Microsoft corporation).
All digital measurements were done by a single calibrated investigator who was blinded (file names and codes and the outcome of the study). Intra-rater reliability was achieved prior to measuring the final samples, during which ten samples from different groups were randomly selected and analyzed by the investigator. Occlusal measurements were done on three separate days for samples in the reliability test. Intra-rater reliability for measurement of the scanned images and occlusal accuracy was 0.911 and 0.897, respectively (good) [95% confidence interval, 4 levels of precision] [42]. The reproducibility of the measurements was analyzed using SPSS version 24.0 (SPSS 24.0; SPSS, Inc., Chicago, Illinois, USA), thereby calculating the intra-class correlation coefficient (ICC), which was also high (0.901).
Statistical Analysis
All data were coded, corrected, and refined within Microsoft excel sheets, then data were entered into SPSS version 24.0 (SPSS 24.0; SPSS, Inc., Chicago, Illinois, USA) for statistical analysis and testing. The test for distribution of the data was performed using the Shapiro-Wilk test. Descriptive statistics calculations produced mean and standard deviations. A one-sample t test analyzed measurement dispersion (around fixed values of the master models). One-way analysis of variance (ANOVA) assessed the differences between the casts generated in four different groups. Pairwise comparison using Tukey’s HSD test determined the differences between the tested subgroups. For all statistically significant differences, the probability level (P) was considered significant at the predetermined value of less than or equal to 0.05 (P≤0.05).
Results
The mean and standard deviation of anterior vertical, posterior vertical, and anterior-posterior measurements (in millimeters) on the articulated master model and the four tested groups – Gp AL(C), Gp AL(E), Gp AL(F), and Gp 3D (C) – are presented in Table 2. Gp AL(C) and Gp 3D-C showed statistically significant differences in anterior vertical, while all groups showed significant differences in means for posterior vertical. For anterior-posterior dimensions, only Gp AL(E) did not show any significant differences in means from the master model. Both Gp AL(C) and Gp 3D-C showed significant differences in means for all measured dimensions. Pairwise comparison using the t test (Table 3) showed that the anterior vertical dimensions of Gp AL(C) and Gp 3D-C were significantly higher than those for the master model (baseline) (P<0.05). However, no significant differences were detected in the anterior vertical dimension between the articulated master model and Gp AL(E) and Gp AL(F) (P<0.05). For posterior vertical dimensions, all groups showed significant differences from the master model. For anterior-posterior dimensions, all groups except Gp AL(E) showed differences in means that were significantly higher than the master model. Mean measurement error (average errors in group) values of each group for each measured dimension against the master model are presented in Table 4. The highest errors were found for posterior vertical dimension in Gp 3D-C (0.56±0.26), while the lowest were found for anterior vertical in Gp AL(F) (0.13±0.09). One-way ANOVA was performed to test the differences in accuracy of the articulated casts made by the 3 impression materials and the printed models (Table 5) for 3 measured dimensions. The one-way ANOVA revealed that a significant difference of error of means at anterior and posterior vertical dimension location (P<0.005), with no significant difference of error of the means at anterior-posterior dimension location (P>0.05). Further analysis for 2 significant dimensions (anterior vertical and posterior vertical) using Tukey’s HSD post hoc test shows that the differences existed only between Gp AL(E)/Gp 3D-C (P<0.001) and Gp AL(F)4p 3D-C (Table 6). No differences for both dimensions were observed between the other groups.
Table 2.
Comparative differences in the mean value measurements (millimeters) between the articulated master model and the 4 tested groups.
| Parameter (Dimensions) | Master model | AL(C) | AL(E) | AL(F) | 3D-C |
|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | |
| Anterior vertical (A1–A2) | 24.660±0.001 | 24.830±0.19* | 24.624±0.19 | 24.721±0.15 | 25.045±0.33* |
| Posterior vertical (P1–P3) | 20.416±0.001 | 20.836±0.15* | 20.648±0.12* | 20.616±0.22* | 20.977±0.26* |
| Anterior-posterior (P1–P4) | 26.711±0.001 | 27.054±0.24* | 26.791±0.24 | 26.976±0.23* | 26.982±0.23* |
SD – standard deviation; AL(C) – conventional alginate; AL(E) – extended pour alginate; AL(F) – alginate free; 3D-C – three-dimensional printed cast. Significant differences when compared to Master Model at P≤.05 (one sample t-test used).
Table 3.
One-sample t test showing the dispersion of the measurements and relative differences of each group measurement against the test values of the Articulated Master model.
| t(df) | Mean diff. (95% CI) | P value# | |
|---|---|---|---|
| 1. Anterior Vertical Test Value (Master model)=24.660 | |||
| AL(C) | 2.89(9) | 0.17 (0.04, 0.30) | 0.018* |
| AL(E) | −0.62(9) | −0.04 (−0.17, 0.10) | 0.551 (NS) |
| AL(F) | 1.28(9) | 0.06 (−0.05, 0.17) | 0.233 (NS) |
| 3D-C | 3.72(9) | 0.38 (0.15, 0.62) | 0.005** |
| 2. Posterior Vertical Test Value (Master model)=20.416 | |||
| AL(C) | 9.00(9) | 0.42 (0.31, 0.53) | 0.001** |
| AL(E) | 5.96(9) | 0.23 (0.14, 032) | 0.001** |
| AL(F) | 2.90(9) | 0.20 (0.04, 0.35) | 0.018* |
| 3D-C | 6.89(9) | 0.56 (0.38, 0.75) | 0.001** |
| 3. Anterior-Posterior Test Value (Master model)=26.711 | |||
| AL(C) | 4.53(9) | 0.34 (0.17, 0.51) | 0.001** |
| AL(E) | 1.07(9) | 0.08 (−0.09, 0.25) | 0.313 (NS) |
| AL(F) | 3.65(9) | 0.27 (0.10, 0.43) | 0.005** |
| 3D-C | 3.70(9) | 0.27 (0.11, 0.44) | 0.005** |
AL(C) – conventional alginate; AL(E) – extended pour alginate; AL(F) – alginate free; 3D-C – three-dimensional printed cast; df – degree of freedom; CI – confidence interval.
One way ‘t’ test. Levels of significance: NS (not-significant) =P≥0.05;
Significant=P≤0.05;
Very significant=P≤0.01;
Highly significant=P≤0.001.
Table 4.
Comparative mean error at 3 observed measurements for each group relative to the reference master model (mm).
| Parameter (Dimensions) | AL(C) | AL(E) | AL(F) | 3D-C |
|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | |
| Anterior vertical | 0.22±0.12 | 0.14±0.12 | 0.13±0.09 | 0.38±0.33 |
| Posterior vertical | 0.38±0.25 | 0.23±0.12 | 0.22±0.20 | 0.56±0.26 |
| Anterior-posterior | 0.36±0.22 | 0.22±0.11 | 0.26±0.23 | 0.29±0.20 |
mm – millimetres; AL(C) – conventional alginate; AL(E) – extended pour alginate; AL(F) – alginate free; 3D-C – three-dimensional printed cast.
Table 5.
Comparative differences of mean errors for various measurements among studied groups in relation to the reference master model.
| Parameter (Dimensions) | Material | n | Mean±SD | F Statistics (df) | P value# |
|---|---|---|---|---|---|
| Anterior vertical | AL(C) | 10 | 0.22±0.12 | 3.92(3,36) | 0.016* |
| AL(E) | 10 | 0.14±0.12 | |||
| AL(F) | 10 | 0.13±0.09 | |||
| 3D-C | 10 | 0.38±0.33 | |||
| Posterior vertical | AL(C) | 10 | 0.38±0.25 | 5.64(3,36) | 0.003** |
| AL(E) | 10 | 0.23±0.12 | |||
| AL(F) | 10 | 0.22±0.20 | |||
| 3D-C | 10 | 0.56±0.26 | |||
| Anterior-posterior | AL(C) | 10 | 0.36±0.22 | 0.93(3,36) | 0.438 (NS) |
| AL(E) | 10 | 0.22±0.11 | |||
| AL(F) | 10 | 0.26±0.23 | |||
| 3D-C | 10 | 0.29±0.20 |
AL(C) – conventional alginate; AL(E) – extended pour alginate; AL(F) – alginate free; 3D-C – three-dimensional printed cast; df – degree of freedom; CI – confidence interval.
One-Way ANOVA tests. Levels of significance: NS (not-significant)=P≥0.05;
Significant=P≤0.05;
Very significant=P≤0.01;
Highly significant=P≤0.001.
Table 6.
Multiple pairwise comparisons of the accuracy of the articulated casts by the 3 impression materials and 3D printed system using Tukey’s HSD test.
| Pairwise comparison | Mean (SD) | Mean difference | P value# | |
|---|---|---|---|---|
| Anterior vertical | AL(C) | 0.22 (0.12) | 0.08 | 0.181 |
| AL(E) | 0.14 (0.12) | |||
| AL(C) | 0.22 (0.12) | 0.09 | 0.693 | |
| AL(F) | 0.13 (0.09) | |||
| AL(C) | 0.22 (0.12) | −0.16 | 0.157 | |
| 3DC | 0.38 (0.33) | |||
| AL(E) | 0.14 (0.12) | −0.01 | 0.765 | |
| AL(F) | 0.13 (0.09) | |||
| AL(E) | 0.14 (0.12) | −0.24 | 0.001** | |
| 3DC | 0.38 (0.33) | |||
| AL(F) | 0.13 (0.09) | −.25 | 0.013* | |
| 3DC | 0.38 (0.33) | |||
| Posterior vertical | AL(C) | 0.38 (0.25) | 0.15 | 0.152 |
| AL(E) | 0.23 (0.12) | |||
| AL(C) | 0.38 (0.25) | 0.16 | 0.071 | |
| AL(F) | 0.22 (0.20) | |||
| AL(C) | 0.38 (0.25) | −0.18 | 0.377 | |
| 3DC | 0.56 (0.26) | |||
| AL(E) | 0.23 (0.12) | 0.01 | 0.983 | |
| AL(F) | 0.22 (0.20) | |||
| AL(E) | 0.23 (0.12) | −0.33 | 0.003** | |
| 3DC | 0.56 (0.26) | |||
| AL(F) | 0.22 (0.20) | −0.34 | 0.001** | |
| 3DC | 0.56 (0.26) |
AL(C) – conventional alginate; AL(E) – extended pour alginate; AL(F) – alginate free; 3D-C – three-dimensional printed cast; df – degree of freedom; CI – confidence interval.
Tukey’s HSD Test. Levels of significance: NS (not-significant)=P≥0.05;
Significant=P≤0.05;
Very significant=P≤0.01;
Highly significant=P≤0.001.
Occlusal accuracy was determined by observing the relative occlusal contacts between teeth number 13, 17, and 27 between articulated master models and 4 different opposing casts/groups. Occlusal contacts falling in the green zone (−0.100 to + 0.100) were ideal and clinically acceptable. For master models, all 3 teeth (13, 17, and 27) showed contacts in the green zone. When opposed by conventional alginate [Gp AL(C)], all occlusal contacts were ideal (green zone) except for 1 sample at tooth number 27, where it was in the blue zone (−0.200 to −2.00). When opposed by a cast made from extended-pour alginate Gp AL(E), 3 samples showed occlusal contacts in the blue zone at tooth number 27 (−0.200 to −2.00). When the master model was opposed by cast obtained from alternative alginate or alginate-free AL(F), 4 samples out of 10 were in the blue zone (−0.200 to −2.00) at tooth number 27. When the master model was opposed by the same opposing cast Gp 3D-C, 4 samples showed blue zone contacts (−0.200 to −2.00) at tooth number 3. To summarize, the opposing casts obtained in Gp AL(C) showed better occlusal distribution since most contacts at the 3 investigated locations (13, 17, and 27) were in the green zone, followed by Gp AL(E), Gp AL(F), and Gp 3D-C.
Discussion
This in vitro study investigated the occlusal accuracy and its related parameters, which are the linear measurements (anterior vertical, posterior vertical, and anterior-posterior) of an articulated maxillary master model against the opposing casts fabricated using 4 different types of commonly used materials (conventional alginate, extended-pour alginate, alginate alternative or FreeAlgin, and 3D printing). The main findings of the study reveal that the linear measurements for 3D-printed, and conventional alginate group derived opposing casts were significantly higher (P<0.05) than those for articulated master model (Typodont 3D-printed). The occlusal accuracy of extended-pour alginate and alginate alternative groups in comparison to the articulated master models was not significantly different except at posterior vertical dimension for extended-pour alginate and at the anterior-posterior dimension for alginate alternative groups. This nullifies the null hypothesis that stated that there would be no differences between the groups. In the current scenario of digital dentistry, the results of our study have some important clinical relevance that can help clinicians in selecting the best possible impression material/technique to be used as an opposing cast against the digitally fabricated fixed dental prosthesis (FDP). Despite implant-supported prosthesis being the first treatment of choice in most cases, conventional FPDs remain popular patients’ treatment choice due to immediate restoration of functions [43]. Yearly, on average the 3D manufactured product sales have been reported to expand at the rate of 33%, which includes major growths in medical/dental related products [44]. The accuracy of models derived from a digital 3D printer has been previously investigated, but the results of those studies need to be interpreted according to their respective context. An orthodontic model that is used specifically for diagnosis cannot fulfill the requirement of a cast that is used for fabrication of the occlusal surface of an FDP. A diagnostic cast has different purposes for different dental applications. For occlusal surfaces, the diagnostic casts need to reproduce both convex and concave surfaces (occlusal anatomy), while maintaining the surfaces smoothly. With 3D printing, intricate geometrical concave surfaces have been reported to be reproduced better than with milling [18,45]. Our study utilized fabrication of 3D models with stereo lithographic apparatus (SLA), which has been reported to have good accuracy [46] when compared to the commonly used PolyJet (photopolymer jetting). Our study utilized a print layer height of 16 μm, which is less than the recommended 25 μm that has been reported to have high accuracy in 3D printing [47]. This could be one of the reasons why 3D-printed models showed less accuracy in our study. Studies that measured crown heights have associated accuracy and surface finish to the print layer height and thickness of the layer and concluded that the printer must print thicker layers in the z axis, which contributes to greater accuracy [17,48]. PolyJet printers, despite printing thinner layers in the z axis, still are accurate since they do not need post curing, which removes changes associated with shrinkage [17]. Our results are in partial agreement with the results obtained by Park and Shin [32], who concluded that conventional methods of cast fabrication were more dependable than that of 3D printers. However, they measured smaller specimens that were related to tooth preparation rather than opposing cast and used vinyl polysiloxane in a customized impression tray as their method. In their study no physical casts were made as they scanned the impressions and evaluated discrepancies by overlapping scanned images. On the other hand, both alginate and type IV dental stone material have high accuracy of reproduction in terms of surface landmarks on the occlusal surface [49]. In a recent study by Abduo, the whole-arch accuracy obtained from alginate impression was not greater than that of polyvinylsiloxane and intra-oral scanned casts [49], which is contrary to other previous study [50]. Abduo attributed these findings to immediate pouring of alginate impressions and the nature of the model used (dentate) with natural undercuts, which strain the polyvinylsiloxane, while having no effect on the alginate impression. His study also found that alginate impressions were more accurate on the occlusal cusps, incisal edges, and proximal and axial surfaces, which are least affected by removal of impressions. Both extended alginate and alginate alternative impression materials used in this study have formulations that provide greater dimensional stability, high elasticity, and high tear resistance, which overall contributes to their accuracy in producing a reliable opposing cast. The differences in shrinkage between the type IV dental stone (0.00% to 0.01%) and the photopolymer resin (up to 3%) used for different groups in this study also contributes to inaccuracies in the 3D-printed casts. The individual minimal shrinkage in the photopolymer layer during polymerization is compounded by the accumulated error of sequential layers that has been observed previously [49]. Contraction of layers while curing introduces stresses resulting in dimensional distortion of the whole cast, which has been shown to affect the posterior region of the cast. The vertical layering of the photopolymer resin causes a staircase effect, which affects the inclined/corrugated surfaces present on the occlusal surfaces of the 3D-printed cast [49]. Another source of error is that SLA printing reuses leftover non-polymerized resin when compared to PolyJet printing, which uses the polymer from new cartridges [31]. Scanning errors that are known to contribute to inaccuracies in the production of a 3D-printed cast have also been studied. These have been attributed to small scanning field, missed shadow surfaces, multiple imaging to generate continuous arch, stitching errors (more pronounced effect on posterior aspect), surface mismatch, and image inaccuracies [36,49,50]. Studies done on intra-oral scanners have concluded that their accuracy was limited to short-span scanning (crowns), and whole-arch scanning should be limited to diagnostic purposes only since it does not have sufficient accuracy for prosthesis fabrication that involves a whole-arch scan [29,51,52].
The results of our study show that the mean error relative to the reference master model was higher than the clinically accepted range (≤200 microns) in all groups except for opposing casts of extended alginate and alginate alternative groups at the anterior vertical dimension. Although 3D-printed casts may have inaccuracies, they have certain clinical advantages. In a consensus of assorted studies, the acceptable range of extra-orally scanned 3D-printed casts was 0.20–0.50 mm [17,53]. An error of such magnitude may be of little relevance if the purpose of the cast is diagnostic or wax-up, but the same error can magnify occlusal discrepancies if they are present on critical areas like functional cusps. In both anterior vertical and posterior vertical dimensions of the articulated casts, significant differences were found (Table 5), which when further analyzed were between extended-pour alginate with 3D-printed opposing casts and alginate alternative with 3D-printed casts. Changes in anterior vertical dimensions of the cast may have little significance for the outcome of the restorations unless the anterior teeth are being replaced, which involves correction or the establishment of anterior guidance, as in full-mouth rehabilitation cases [54]. Changes in posterior vertical dimensions are significant for every posterior restoration since they form a vertical stop. Lee et al [55] evaluated the articulation accuracy of milled models and found no differences in occlusion in the posterior areas, while finding a significantly higher percentage force distribution in the canine region. The differences in results are based on the method of evaluation used in his study. He used quadrant model digital evaluation, in which each quadrant was evaluated independently, while our study used complete arch casts in digital evaluation. He also attributed his finding (more force distribution anteriorly) to quadrant model digital evaluation and reasoned that the higher forces were due to the absence of contralateral articulating stops in quadrant models, which results in higher contact areas in digital-mounted quadrant models.
In our study the opposing casts of Gp Al (E) – extended-pour alginate – demonstrated a better occlusal distribution since most contacts at the three predetermined locations (13, 17, and 27) were in the green zone, which was followed by conventional alginate, alginate alternative, and 3D-printed opposing casts. The less accurate occlusal distribution of the 3D-printed opposite cast could be explained by the findings of Jin et al, who found more deviation of the posterior region with uneven contraction of occlusal surface of 3D-printed models [31]. This significant deviation has been found to occur due to a higher density of photopolymers in the posterior region, which introduces more deviation because of high polymerization reaction [56]. Uneven shrinkage patterns on the occlusal surfaces of the posterior regions in 3D-printed models have been attributed to the occlusal grooves, which are influenced by the pattern of printing as well as the scan path of the scanner used [57]. A 3D-printing error that occurs during 3D printing of photopolymers in the posterior deep pits and fissure occlusal surface is related to the printer’s inability to self-clean the sticky resin and the inability of the liquid adhesive to flow into these areas. This results in the material being cured on its own and resulting in printing error, which can be prevented by filling the deep grooves in the models (digital or stone models) [58].
Occlusal inaccuracy in digital articulation has also been attributed to the unequal distribution of occlusal contacts between interocclusal registration material and the digital casts. Edher et al [59] analyzed virtual interocclusal registrations scanning and concluded that the occlusal contacts obtained from the scanning of interocclusal records were highly and significantly variable according to different arch segments. He also concluded that the differences were greater in complete arch scans, which resulted in the tilting of the digital record towards the side of the registration scan. In another study that evaluated virtual interocclusal records, the authors reported the accuracy to be clinically acceptable, but during their study they reported that these records tend to miss interocclusal contacts more frequently than introducing a false one [60].
Contrary to our findings, numerous studies on 3D-printed casts have reported them to be more accurate than conventional stone casts or had comparable trueness to stone casts [31,33,34]. All three studies, however, used an intra-oral scanner and two of the studies analyzed digital casts rather than physical casts, while the third one used conventional alginate as the reference (baseline/control group), which our study also found to be inaccurate. Moreover, these studies did not involve measuring arch accuracy, and were limited to measurements specifically related to the teeth. Finally, it must be considered that dental materials could present differences when measuring mechanical properties like micro-hardness [61], flexural strength [62], and fatigue resistance [63]. These factors could affect occlusal accuracy. All these aspects should be considered in future studies.
Strengths and Limitations of the Study
Very few studies have assessed the occlusal accuracy of digitally derived whole casts and ours is first to study the effect of the opposing cast on the occlusion. Limitations of the present study include the in vitro design and using ideal models rather than the patient’s occlusion, which varies individually. Another limitation is that only one brand of scanner was used with a single brand of 3D printer, while there are many commercially available. The study lacks simulation of oral conditions that have been shown to influence the scanning procedure (eg, saliva, tongue, light, access). This necessitates further studies which evaluate the accuracy of other scanners and printers in conditions such as those inside the oral cavity.
Clinical Implications
These findings support the benefits of using 3D-printed models that should be limited to diagnosis, treatment planning, and fabrication of temporary restorations only, and their use as antagonist/opposing cast may result in significant occlusal errors in the definitive restoration and/or prosthesis.
Conclusions
Within the limitations of this study, the following conclusions can be drawn:
The conventional method of cast fabrication using alginate alternative and extended-pour alginate impression materials presented less changes in anterior and posterior vertical dimensions than that of the 3D printer used in this study.
The best digital occlusal accuracy was observed when opposing casts were obtained from extended-pour alginate and alginate alternative materials, with 3D-printed cast having the poorest fit.
Extended-pour alginate and alginate alternative-derived opposing casts may be comparable to each other in preparations of the opposing cast for fixed prosthodontic restorations fabrication.
Acknowledgement
We thank the staff and supporting staff of the preclinical prosthodontic laboratory for allowing us to use the laboratory facilities during sample preparation. We would also like to acknowledge the sincere efforts of technical staff at the laboratory where digital analysis was performed.
Footnotes
Conflict of interest: None declared
Department and Institution Where Work Was Done
Department of Prosthetic Dental Sciences, College of Dentistry, Jazan University, Jazan, Saudi Arabia.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Carlsson GE. Dental occlusion: Modern concepts and their application in implant prosthodontics. Odontology. 2009;97:8–17. doi: 10.1007/s10266-008-0096-x. [DOI] [PubMed] [Google Scholar]
- 2.Meng JC, Nagy WW, Wirth CG, et al. The effect of equilibrating mounted dental stone casts on the occlusal harmony of cast metal complete crowns. J Prosthet Dent. 2010;104:122–32. doi: 10.1016/S0022-3913(10)60105-9. [DOI] [PubMed] [Google Scholar]
- 3.Sharma A, Kalra T, Jain S, et al. Comparative evaluation in linear dimensions among various interocclusal recording materials at various mounting times: An in vitro study. World J Dent. 2020;11(6):462–67. [Google Scholar]
- 4.Cowie RR. The successful crown delivery. J Dent Technol. 2015:38–44. [Google Scholar]
- 5.McCracken MS, Litaker MS, Gordan VV, et al. Remake rates for single-unit crowns in clinical practice: Findings from The National Dental Practice-Based Research Network. J Prosthodont. 2019;28:122–30. doi: 10.1111/jopr.12995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christensen GJ. The state of fixed prosthodontic impressions: Room for improvement. J Am Dent Assoc. 2005;136:343–46. doi: 10.14219/jada.archive.2005.0175. [DOI] [PubMed] [Google Scholar]
- 7.Alghamdi NS, Alamoudi RA, Baba SM, et al. A scanning electron microscopy study comparing 3 obturation techniques to seal dentin to root canal bioceramic sealer in 30 freshly extracted mandibular second premolars. Med Sci Monit. 2023;29:e940599. doi: 10.12659/MSM.940599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waylen A. The importance of communication in dentistry. Dent Update. 2017;44(8):774–80. [Google Scholar]
- 9.Kumar L, Mattoo KA, Jain S, et al. A clinical study of 50 partially edentulous patients with fixed partial denture restorations to compare clinical parameters and changes in gingival sulcus width after displacement with 2 different gingival retraction cord materials (cotton and polymer) Med Sci Monit. 2023;29:e940098. doi: 10.12659/MSM.940098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loos LG, Boyarsky HP, Quiring DJ. Procedure for occlusal refinement of mounted definitive casts to reduce clinical time required for adjustment of occlusion. J Prosthet Dent. 2001;85:246–51. doi: 10.1067/mpr.2001.114271. [DOI] [PubMed] [Google Scholar]
- 11.Jain S, Mattoo K, Khalid I, et al. A study of 42 partially edentulous patients with single-crown restorations and implants to compare bone loss between crestal and subcrestal endosseous implant placement. Med Sci Monit. 2023;29:e939225. doi: 10.12659/MSM.939225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seelbach P, Brueckel C, Wöstmann B. Accuracy of digital and conventional impression techniques and workflow. Clin Oral Investig. 2013;17:1759–64. doi: 10.1007/s00784-012-0864-4. [DOI] [PubMed] [Google Scholar]
- 13.Alves de Carvalho IF, Santos Marques TM, Araújo FM, et al. Clinical performance of CAD/CAM tooth-supported ceramic restorations: A systematic review. Int J Periodontics Restor Dent. 2018;38:e68–78. doi: 10.11607/prd.3519. [DOI] [PubMed] [Google Scholar]
- 14.Fasbinder DJ. Digital dentistry: Innovation for restorative treatment. Compend Contin Educ Dent. 2010;31:2–11. [PubMed] [Google Scholar]
- 15.Luthardt RG, Bornemann G, Lemelson S, et al. An innovative method for evaluation of the 3-D internal fit of CAD/CAM crowns fabricated after direct optical versus indirect laser scan digitizing. Int J Prosthodont. 2004;17:680–85. [PubMed] [Google Scholar]
- 16.Christensen GJ. Impressions are changing: Deciding on conventional, digital or digital plus in-office milling. J Am Dent Assoc. 2009;140:1301–4. doi: 10.14219/jada.archive.2009.0054. [DOI] [PubMed] [Google Scholar]
- 17.Keating AP, Knox J, Bibb R, Zhurov A. A comparison of plaster, digital and reconstructed study model accuracy. J Orthod. 2008;35:191–201. doi: 10.1179/146531207225022626. [DOI] [PubMed] [Google Scholar]
- 18.Yau HT, Yang TJ, Lin YK. Comparison of 3-D printing and 5-axis milling for the production of dental models from intra-oral scanning. Comput Aided Des Appl. 2016;13:32–38. [Google Scholar]
- 19.Şeker E, Ozcelik TB, Rathi N, Yilmaz B. Evaluation of marginal fit of CAD/CAM restorations fabricated through cone beam computerized tomography and laboratory scanner data. J Prosthet Dent. 2016;115(1):47–51. doi: 10.1016/j.prosdent.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Indicators SO. Accuracy, reliability and clinical implications of static compared to quantifiable occlusal indicators. Eur J Prosthod Rest Dent. 2020;28:1–2. doi: 10.1922/EJPRD_2202Qadeer12. [DOI] [PubMed] [Google Scholar]
- 21.Koyano K, Tsukiyama Y, Kuwatsuru R. Rehabilitation of occlusion – science or art? J Oral Rehabil. 2012;39(7):513–21. doi: 10.1111/j.1365-2842.2012.02303.x. [DOI] [PubMed] [Google Scholar]
- 22.Filtchev AD, Kalachev YS. Phenomenon of domination of the strongest contacts in centric occlusion. Quintessence Int. 2008;39:99–106. [PubMed] [Google Scholar]
- 23.Saeed F, Muhammad N, Khan AS, et al. Prosthodontics dental materials: From conventional to unconventional. Mater Sci Eng C. 2020;106:110167. doi: 10.1016/j.msec.2019.110167. [DOI] [PubMed] [Google Scholar]
- 24.Nassar U, Hussein B, Oko A, et al. Dimensional accuracy of 2 irreversible hydrocolloid alternative impression materials with immediate and delayed pouring. J Can Dent Assoc. 2012;78(78):c2. [PubMed] [Google Scholar]
- 25.Christensen GJ. Making fixed prostheses that are not too high. J Am Dent Assoc. 2006;137:96–98. doi: 10.14219/jada.archive.2006.0027. [DOI] [PubMed] [Google Scholar]
- 26.Boksman L. Optimizing occlusal results for crown and bridge prostheses. Dent Today. 2011;30:154, 156–57. [PubMed] [Google Scholar]
- 27.Iwauchi Y, Tanaka S, Kamimura-Sugimura E, Baba K. Clinical evaluation of the precision of interocclusal registration by using digital and conventional techniques. J Prosthet Dent. 2022;128(4):611–17. doi: 10.1016/j.prosdent.2021.01.021. [DOI] [PubMed] [Google Scholar]
- 28.Hazeveld A, Slater JJ, Ren Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am J Orthod Dentofacial Orthop. 2014;145:108–15. doi: 10.1016/j.ajodo.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 29.Jeong YG, Lee WS, Lee KB. Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method. J Adv Prosthodont. 2018;10:245–51. doi: 10.4047/jap.2018.10.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dawood A, Marti Marti B, Sauret-Jackson V, et al. 3D printing in dentistry. Br Dent J. 2015;219:521–29. doi: 10.1038/sj.bdj.2015.914. [DOI] [PubMed] [Google Scholar]
- 31.Jin SJ, Kim DY, Kim JH, et al. Accuracy of dental replica models using photopolymer materials in addictive manufacturing: In vitro three-dimensional evaluation. J Prosthodont. 2018;2:e557–e62. doi: 10.1111/jopr.12928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park ME, Shin SY. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J Prosthet Dent. 2018;119(5):861e1–e7. doi: 10.1016/j.prosdent.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 33.Aly P, Mohsen C. Comparison of the accuracy of three-dimensional printed casts, digital, and conventional casts: An in vitro study. Eur J Dent. 2020;14(2):189–93. doi: 10.1055/s-0040-1705243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown GB, Currier GF, Kadioglu O, Kierl JP. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am J Orthod Dentofacial Orthop. 2018;154(5):733–39. doi: 10.1016/j.ajodo.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 35.Millstein P, Maya A. An evaluation of occlusal contact marking indicators: A descriptive quantitative method. J Am Dent Assoc. 2001;132(9):1280–86. doi: 10.14219/jada.archive.2001.0373. [DOI] [PubMed] [Google Scholar]
- 36.Zimmermann M, Ender A, Attin T, Mehl A. Accuracy of buccal scan procedures for the registration of habitual intercuspation. Oper Dent. 2018;43:573–80. doi: 10.2341/17-272-C. [DOI] [PubMed] [Google Scholar]
- 37.Tabatabaian F, Namdari M, Mahshid M, et al. Accuracy and precision of intraoral scanners for shade matching: A systematic review. J Prosthet Dent. 2022 doi: 10.1016/j.prosdent.2022.08.034. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 38.Festing MF, Altman DG. Guidelines for the design and statistical analysis of experiments using laboratory animals. ILAR J. 2002;43:244–58. doi: 10.1093/ilar.43.4.244. [DOI] [PubMed] [Google Scholar]
- 39.Rosenstiel SF, Land MF, Fujimoto J. Principles of tooth preparation. In: Duncan L, editor. Contemporary fixed prosthodontics. Vol. 2. Mosby-Year Book, Inc; St. Louis: 1995. pp. 135–67. [Google Scholar]
- 40.Revilla-León M, Kois DE, Zeitler JM, et al. An overview of the digital occlusion technologies: Intraoral scanners, jaw tracking systems, and computerized occlusal analysis devices. J Esthet Restor Dent. 2023;35(5):735–44. doi: 10.1111/jerd.13044. [DOI] [PubMed] [Google Scholar]
- 41.Medit occlusal analyzer. [Last accessed June 19, 2023]. Available at: https://support.medit.com/hc/en-us/articles/360021126151-Occlusion-analysis.
- 42.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jain S, Mattoo K, Khalid I, et al. A study of 42 partially edentulous patients with single-crown restorations and implants to compare bone loss between crestal and subcrestal endosseous implant placement. Med Sci Mon. 2023;29:e939225. doi: 10.12659/MSM.939225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stansbury JW, Idacavage MJ. 3D printing with polymers: Challenges among expanding options and opportunities. Dent Mater. 2016;32:54–64. doi: 10.1016/j.dental.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 45.Rungrojwittayakul O, Kan JY, Shiozaki K, et al. Accuracy of 3D printed models created by two technologies of printers with different designs of model base. J Prosthodont. 2020;29(2):124–28. doi: 10.1111/jopr.13107. [DOI] [PubMed] [Google Scholar]
- 46.Patzelt SB, Bishti S, Stampf S, et al. Accuracy of computer-aided design/computer-aided manufacturing-generated dental casts based on intraoral scanner data. J Am Dent Assoc. 2014;145:1133–40. doi: 10.14219/jada.2014.87. [DOI] [PubMed] [Google Scholar]
- 47.Favero CS, English JD, Cozad BE, et al. Effect of print layer height and printer type on the accuracy of 3-dimensional printed orthodontic models. Am J Orthod Dentofacial Orthop. 2017;152(4):557–65. doi: 10.1016/j.ajodo.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 48.Zyzalo JR. Masked projection stereolithography: improvement of the Limaye model for curing single layer medium sized part: [thesis] Albany, New Zealand: Massey University; 2008. [Google Scholar]
- 49.Abduo J. Accuracy of casts produced from conventional and digital workflows: A qualitative and quantitative analyses. J Adv Prosthodont. 2019;11(2):138–46. doi: 10.4047/jap.2019.11.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ender A, Attin T, Mehl A. In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J Prosthet Dent. 2016;115:313–20. doi: 10.1016/j.prosdent.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 51.Al-Imam H, Gram M, Benetti AR, Gotfredsen K. Accuracy of stereolithography additive casts used in a digital workflow. J Prosthet Dent. 2018;119:580–85. doi: 10.1016/j.prosdent.2017.05.020. [DOI] [PubMed] [Google Scholar]
- 52.Cho SH, Schaefer O, Thompson GA, Guentsch A. Comparison of accuracy and reproducibility of casts made by digital and conventional methods. J Prosthet Dent. 2015;113:310–15. doi: 10.1016/j.prosdent.2014.09.027. [DOI] [PubMed] [Google Scholar]
- 53.Labib MA, El-Beialy AR, Attia KH. Evaluation of the accuracy of digital models obtained using intraoral and extraoral scanners versus gold standard plaster model (diagnostic accuracy study) Open J Med Imaging. 2020;10(03):151. [Google Scholar]
- 54.Darraj A, Mattoo KA, Gupta I. Full mouth rehabilitation of a rheumatoid arthritis patient – the muzyanas challenge. AIMDR. 2017;3(6):10. [Google Scholar]
- 55.Lee JD, Gallucci GO, Lee SJ. An in-vitro evaluation of articulation accuracy for digitally milled models vs. conventional gypsum casts. Dent J. 2022;10(1):11. doi: 10.3390/dj10010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Al Sunbul H, Silikas N, Watts DC. Polymerization shrinkage kinetics and shrinkage-stress in dental resin-composites. Dent Mater. 2016;32:998–1006. doi: 10.1016/j.dental.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 57.Chuang SF, Huang PS, Chen TYF, et al. Shrinkage behaviors of dental composite restorations – the experimental-numerical hybrid analysis. Dent Mater. 2016;32:e362–e73. doi: 10.1016/j.dental.2016.09.022. [DOI] [PubMed] [Google Scholar]
- 58.Winder J, Bibb R. Medical rapid prototyping technologies: State of the art and current limitations for application in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2005;63(7):1006–15. doi: 10.1016/j.joms.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 59.Edher F, Hannam AG, Tobias DL, Wyatt CC. The accuracy of virtual interocclusal registration during intraoral scanning. J Prosthet Dent. 2018;120(6):904–12. doi: 10.1016/j.prosdent.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 60.Abdulateef S, Edher F, Hannam AG, et al. Clinical accuracy and reproducibility of virtual interocclusal records. J Prosthet Dent. 2020;124(6):667–73. doi: 10.1016/j.prosdent.2019.11.014. [DOI] [PubMed] [Google Scholar]
- 61.Colombo M, Gallo S, Poggio C, et al. New resin-based bulk-fill composites: In vitro evaluation of micro-hardness and depth of cure as infection risk indexes. Materials (Basel) 2020;13(6):1308. doi: 10.3390/ma13061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cacciafesta V, Sfondrini MF, Lena A, Scribante A, et al. Flexural strengths of fiber-reinforced composites polymerized with conventional light-curing and additional postcuring. Am J Orthod Dentofac Orthop. 2007;132(4):524–27. doi: 10.1016/j.ajodo.2005.09.036. [DOI] [PubMed] [Google Scholar]
- 63.Rodríguez-Ivich J, Razaghy M, Henriques B, Magne P. Accelerated fatigue resistance of bonded composite resin and lithium disilicate screw-retained incisor crowns with long and short titanium bases. Int J Perio Restor Dent. 2022;42(4):459–69. doi: 10.11607/prd.5736. [DOI] [PubMed] [Google Scholar]