Abstract
Introduction:
Young adulthood is a transitional period between adolescence and adulthood. Due to the unique pressures of taking on a new social role and associated uncertainties, young adults are at heightened risk for drug and alcohol use. Furthermore, adverse childhood experiences (ACEs) increases the likelihood of using maladaptive coping strategies such as using substances to avoid or soothe negative emotions. The current review aimed to summarize the associations between exposure to ACEs before the age of 18 years and subsequent drug or alcohol use between the ages of 18 and 25 years.
Methods:
The review was performed in accordance with the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The literature search of the Web of Science, PubMed, and PsycINFO databases was conducted in February 2022.
Results:
The initial search yielded 7178 articles, with 777 duplicates. Consequently, 6401 titles were inspected for relevance. After reading the full text, 88 articles were included in the review.
Conclusion:
This review provides clear evidence that exposure to multiple ACEs is a robust risk factor for the use of alcohol, cannabis and other drugs by young adults. Poor self-regulation and maladaptive coping strategies were identified as mechanisms explaining this link; however, further detailed research is needed.
Keywords: Adverse childhood experiences, young adulthood, substance use, neglect, parental abuse
Introduction
Early adulthood is a transitional period between adolescence and adulthood that encompasses the age of 18 to 25 years. 1 Due to the unique pressures of taking on a new social role and associated uncertainties, young adults are at increased risk for drug and alcohol use.2,3 According to the Substance Abuse and Mental Health Services Administration (2021), the highest rates of alcohol and illicit drug (specifically cannabis) use occur in individuals aged 18 to 25 years.
Substance use during early adulthood has been linked to environmental factors such as stress, 4 and one specific stressor is exposure to adverse childhood experiences (ACEs).5,6 Since the original study by Felitti et al,7 ACEs have been conceptualized as potentially traumatic events that a person experiences before the age of 18 years. There are 2 broad categories of ACEs: childhood maltreatment and household dysfunction. In addition, exposure to ACEs has been consistently associated with engaging in health risk behaviors, 8 worse mental health, 9 and lower quality of life 10 ; drug and alcohol abuse are the most frequently reported consequences. 11 The World Health Organization has deemed drug and alcohol abuse a global health problem and recommended the creation of a framework to prevent their negative health impacts. 12
Exposure to traumatic experiences during childhood, similar to exposure to chronic stress, has been shown to predict cortisol dysregulation, leading to heightened threat sensitivity. 13 ACEs also impact brain structures, including the prefrontal cortex and amygdala. 14 These structures are involved in behavioral inhibition, self-control, and impulsivity. Consequently, the impairment in executive functioning resulting from exposure to ACEs leads to increased substance use or dependence starting in adolescence and continuing into adulthood. 15
The diathesis-stress model is the main theoretical framework regarding the long-lasting effect of ACEs on physical and mental health. Initially developed to explain schizophrenia, this model posits that stress can induce vulnerability to specific psychopathology (the diathesis), thus explaining the differences in outcomes between vulnerable and resilient individuals who experience similar environmental pressures.16,17 By definition, ACEs are stressors; they have been shown to amplify personal predispositions in the form of traits or genes for drug and alcohol use.18,19 In addition, exposure to ACEs facilitates the development of maladaptive coping strategies, including using substances to avoid or soothe negative emotions.20,21 Furthermore, exposure to ACEs is associated with mental health issues, including depressive and anxiety symptoms as well as suicidal behavior 22 ; substance use can transform into self-medication and represent an indirect effect of ACEs.
Current study
The present review aimed to summarize the association between exposure to ACEs before the age of 18 years and the effect of ACEs on (or associations with) subsequent drug or alcohol use before the age of 25 years. Although early adulthood is sometimes expanded to the age of 29 years, the current study limited this period to the age of 18 to 25 years. This allowed us to match the age ranges used in national drug use and health surveys. Furthermore, this mirrors the upper age of transitional-aged youth (TAY), who are suggested to experience the highest risk for health risk behaviors due to unique developmental challenges most commonly encountered by young adults.23,24 Despite apparent agreement in the literature regarding the association between exposure to ACEs and drug use, the current review contributes provides 2 important contributions. First, it focuses exclusively on TAY, a distinct population that should be investigated separately from adults or adolescents.
The review included studies reporting associations in TAY who were employed and who were students. A recent literature review by Rogers et al 25 investigated a similar topic. Unfortunately, their search did not include the Web of Science database; consequently, it included few relevant papers. The current study aimed to address this omission. Second, to obtain better understanding of the association between ACEs and substance use, the present review also paid special attention to mediators and moderators of this association.
Methods
This review was conducted in accordance with the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 26
The literature review was conducted in February 2022, and the Web of Science, PubMed, and PsycINFO databases were searched. The search strategy is presented in Table 1.
Table 1.
Literature search strategy.
| Childhood Trauma | AND | Drug Use* | AND | Adult* | |
|---|---|---|---|---|---|
| OR | early life traum* | OR | drug abuse* | OR | young adult |
| OR | adverse experienc* | OR | drug misuse* | OR | early adult |
| OR | adverse childhood experience | OR | drug* | ||
| OR | childhood traum* experience | OR | substance use* | ||
| OR | substance abuse* | ||||
| OR | substance misuse* | ||||
| OR | susbstance* | ||||
| OR | alcohol use* | ||||
| OR | alcohol abuse* | ||||
| OR | alcohol* |
The accepted wildcard for the search strings.
Studies were eligible for inclusion if they met the following criteria: were published in English; had a quantitative design; were published in a peer-reviewed journal; assessed ACEs between birth and the age of 18 years; and measured alcohol or drug use, abuse, or dependence, specifically between ages 18 and 25 years.
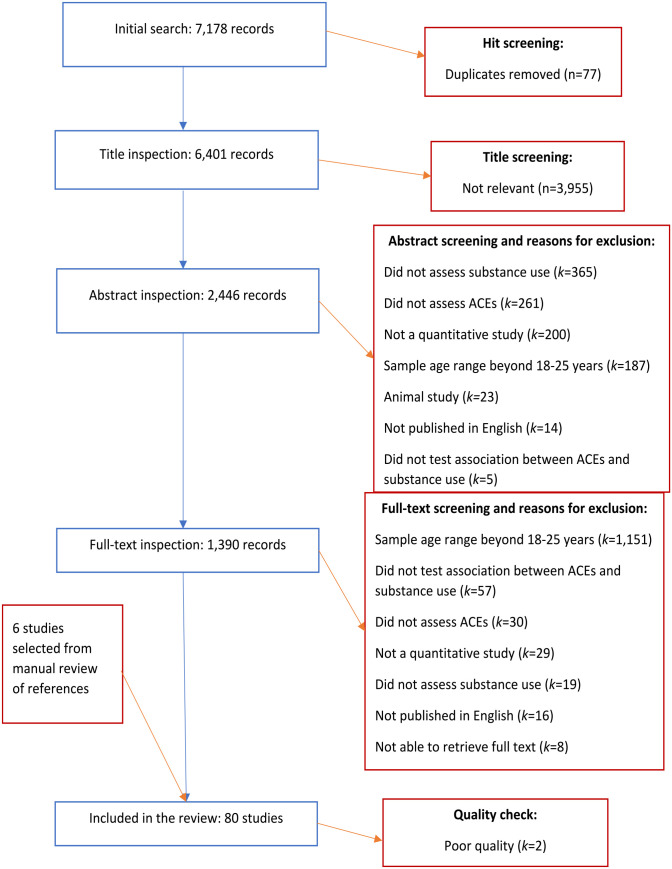
The initial search yielded 7178 articles, with 777 duplicates. The remaining 6401 titles were inspected for relevance. Removal of 3955 articles with nonrelevant titles resulted in 2446 remaining articles. Of these, 1390 were found to be relevant upon inspection of the abstract. The high number of removed articles in the previous step was mainly due to the need to verify the age of the sample and measures used to evaluate ACEs and substance use. After review of the full texts, 80 articles were deemed suitable for inclusion in the review.
Furthermore, 6 articles were added after manual inspection of references. One researcher reviewed the titles, abstracts, and full texts. Following a quality check, 2 poor-quality studies were removed, for a total of 80 studies. The details of the excluded studies are presented in Figure 1.
Figure 1.
Flowchart of study inclusion.
Study characteristics
The majority of the studies were conducted in the United States of America (n = 56), followed by Australia (n = 6) and Canada (n = 6), Spain (n = 2), and the United Kingdom (n = 2). Other countries with one study each included Sweden, Denmark, New Zealand, India, Honduras, Greece, Bosnia and Herzegovina, Columbia, Switzerland, and Turkey. In addition, there were 2 multinational studies. One study included participants from Albania, Latvia, Lithuania, Montenegro, Romania, Russia, the former Yugoslav Republic of Macedonia, and Turkey. 5 The other study incorporated data from the Czech Republic, Lithuania, the Republic of Moldova, Montenegro, Poland, Romania, Russia, Serbia, Ukraine, and the former Yugoslav Republic of Macedonia. 6 The majority of the studies were cross-sectional (n = 53). Other studies were cohort studies (n = 29) or quasiexperimental studies (n = 2). Given the clear benefits of cohort studies over cross-sectional studies for establishing causality and the aim of the study (to identify influential third variables explaining the relationship between ACEs and substance use), cohort studies investigating mediators and moderators are separately highlighted in the Results section.
The quality of the included studies was assessed using Checklists for Analytical Cross-Sectional Studies, Cohort Studies, and Quasi-Experimental Designs from the Joanna Briggs Institute (JBI) at the University of Adelaide. 27 Most studies (n = 64) were of excellent quality, defined as having a score ⩽1, or good quality (n = 20), defined as having a score >1 and ⩽1.5. Two studies were of poor quality and were excluded. Notably, although the “gold standard” of ACE exposure or substance use is governmental or medical records, studies were not penalized for using self-report questionnaires or scales because these methods are accepted as valid measures of individual behaviors by most studies. Further information about the included studies is provided in Table 2.
Table 2.
Characteristics of the included studies.
| Author(s) and year | Sample | ACE measure | Drug use measure | Results | Quality rating |
|---|---|---|---|---|---|
| (Abajobir, Kisely, et al, 2017) | 3750 young adults (53% female), completed the drug questionnaire at 21 yearsCohort study, Australia | Record inspection to identify physical, sexual, and emotional abuse and neglect | Yes/no question about injected drug use during interview | ACEs were associated with drug use primarily among females. | 2 |
| Abajobir, Najman, et al (2017) | 2526 young adults (51.6% female)Cohort study, Australia | Record inspection to identify physical, sexual, and emotional abuse and neglect | Cannabis abuse and dependence assessed using the Composite International Diagnostic Interview (CIDI-Auto) version 2.1 | ACEs were primarily associated with cannabis dependence rather than cannabis abuse. | 1 |
| Allem et al (2015) | 1417 young adults (59% female)Cross-sectional study, USA | Adverse Childhood Experiences (ACE) scale 7 | Yes/no questions were used to assess the following behaviors in the past month: marijuana use, binge drinking, and hard drug use | ACEs were associated with binge drinking, cannabis and hard drug use. | 2 |
| Anderson et al (2010) | 153 young adults (65% female)Cross-sectional study, USA | Semistructured 100-item Trauma Antecedents Interview 28 ; Verbal Abuse Scale 29 ; Childhood Trauma Questionnaire (CTQ) 30 ; Straus Conflict Tactics Scale (CTS) 31 | Online survey assessing history of alcohol and recreational drug use | Interaction of ACEs with lingular thickness was associated with drug and alcohol use. | 2 |
| Baranger et al (2016) | 665 young adults (66% female)Cross-sectional study, USA | CTQ 30 | Alcohol Use Disorders Identification Test (AUDIT) 32 | Interaction between period gene (PER1) expression and ACEs was associated with alcohol use. | 2 |
| Barton et al (2015) | 505 young menCross-sectional study, USA | ACE scale 7 ; custom-made scale to assess involvement of biological and social fathers | Substance use frequency was assessed with a single item. Problematic use was assessed using 10 items from Harrison et al 33 | ACEs had direct effect on substance use. Involvement of the biological father had an indirect effect on substance use. | 2 |
| Bellis et al (2014) | 10 696 young adults (60% female)Cross-sectional study, multinational: Albania, Latvia, Lithuania, Montenegro, Romania, Russia, the former Yugoslav Republic of Macedonia, and Turkey | Adverse Childhood Experiences–International Questionnaire (ACE-IQ) 34 | Drug use and problematic alcohol use were each assessed with a yes/no question | ACEs were associated with problematic use of alcohol and drug use. | 2 |
| Bender et al (2015) | 601 young adults (35.9% female)Cross-sectional study, USA | CTQ, 30 Traumatic Life Events Questionnaire 35 | Substance use disorder assessed using the Mini International Neuropsychiatry Interview (MINI) 36 | Street victimization (rather than ACEs) was associated with substance use. | 2 |
| Cater et al (2014) | 2500 young adults (62.6% female)Cross-sectional study, Sweden | 24 items from the Juvenile Victimization Questionnaire (JVQ) , 37 12 items from Janson et al 38 and May-Chahal and Cawson 39 | AUDIT 32 | ACEs were associated with problematic alcohol use. | 1 |
| Cho and Kogan (2016) | 505 young menCohort study, USA | ACE scale, 7 Measure of Parenting Style (MOPS) 40 | Substance use frequency was assessed with 1 item. Problematic use was assessed using 10 items from Harrison et al 33 | Harsh and unresponsive parenting was indirectly associated with substance abuse. | 2 |
| Crandall et al (2020) | 438 young adults from wave 10 (51% female)Cohort study, USA | ACEs were assessed using questions adapted from the ACE scale 7 and from other studies: Barber, 41 Busby et al, 42 Grych et al, 43 Radloff, 44 Robinson et al , 45 and Umberson et al. 46 Counter-ACEs were based on the Beneficial Childhood Experiences Scale 47 | Substance use was assessed using 5 items from the Adolescent Alcohol and Drug Involvement Scale (AADIS) 48 | ACEs were associated with substance abuse. When counter-ACEs were added they had an inverse effect on only substance abuse. | 2 |
| Cronin et al (2016) | 2980 young adults (52.2% female)Cross-sectional study, Denmark | 20 questions were used to assess 4 domains of childhood maltreatment: physical, psychological, sexual, and neglect. The 4 latent classes of abuse were labeled no abuse, emotional abuse, sexual abuse, and multiple abuse | A yes/no question was used to assess alcohol misuse | ACEs were associated with alcohol misuse even after controlling for PTSD. | 2 |
| Davis et al (2021) | 2526 young adults (53.7% female), Outcomes of interest occurred at T2, T3, and T4Cohort study, USA | Items derived from the ACE scale 7 were used to create a single dichotomous variable | Separate questions were used to assess drug and alcohol use | More individuals with ACEs transitioned to more severe substance use than those without ACEs. | 1 |
| Dawson-Rose et al (2020) | 100 homeless young adults (33% female)Cross-sectional study, USA | ACE scale 7 | Substance use was assessed with the National Institute on Drug Abuse (NIDA) Quick Screen V1.0. 49 Further information was obtained using the NIDA-Modified Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) V2.049 | ACEs were correlated with opioid and stimulant use but not alcohol or cannabis use. | 1 |
| DeBeck et al (2013) | 405 street-involved young adults (32% female)Cohort study, Canada | CTQ 50 | A single question was used to assess the time from first injection of a drug to regular injection drug use | ACEs were associated with progression to injection drug use. | 2 |
| Dube et al (2006) | 8417 young adults (54% female)Cross-sectional study, USA | Questions adapted from the CTS 31 and CTQ 50 | Single questions were used to assess ever drinking alcohol and age at first drink. | ACEs were associated with ever drinking alcohol. | 2 |
| Exner-Cortens et al (2013) | 5861 young adults (52.3% female)Cohort study, USA | Custom-made questionnaire assessing neglect, physical abuse, and sexual abuse, similar to the Parent‒Child CTS 31 | Self-reported alcohol, cannabis, and illicit drug use | ACEs were associated with alcohol use among female participants only. | 2 |
| Ferguson et al (2016) | 601 homeless young adults (21% female)Cross-sectional study, USA | CTQ 30 ; street victimization was measured using a modified version of theTraumatic Life Events Questionnaire. 35 | Self-reported substance use | Street victimization mediated the relationship between ACEs and substance use. | 2 |
| Fergusson et al (2008) | 1011 young adults assessed at the ages of 18-21, 1001 young adults assessed at the ages of 21-25.Sex composition was not reportedCohort study, New Zealand | At all assessment stages, participants were asked about physical and sexual abuse | Substance dependence was assessed using items from the CIDI 51 | After adjusting for covariates, only CSA was associated with substance dependence. | 1 |
| Fernandes et al (2021) | 2751 young adults (52% female)Cross-sectional study, India | ACE-IQ 52 | Alcohol and substance use was assessed using the ASSIST 53 | Family and collective ACEs were associated with substance use, but child and community ACEs were not. | 2 |
| Filipkowski et al (2016) | 216 young adults (55% female)Cross-sectional study, USA | Adverse life experiences questionnaire was adapted for this study 54 | Participants were asked to report the frequency of substance useAlcohol use was assessed using Michigan Alcohol Screening Test (MAST). 55 | ACEs were associated with alcohol but not drug use at entry. Stress did not mediate the relationship between ACEs and drug or alcohol use. | 2 |
| Forster et al (2020) | 1065 young adults (60% female)Cohort study, USA | ACE scale 7 | Six items were used to assessalcohol, cannabis, and drug use. | ACEs were associated with alcohol and illicit drug use. ACEs moderated the relationship between dimensions of emerging adulthood and substance use. | 1 |
| Friedman et al (2022) | 9310 female young adults Cross-sectional study, USA | ACE questionnaire from the Behavioral Risk Factor Surveillance System (BRFSS) 56 | Self-reported cannabis use and binge drinking | Clusters with higher ACEs were associated with higher cannabis use and binge drinking. | 2 |
| Fusco (2021) | 185 young adults (49% female)Cross-sectional study, USA | CTQ–Short Form (CTQ-SF) 50 | Single yes/no questions were used to assess alcohol and cannabis use | ACEs were associated with alcohol and cannabis use. | 2 |
| Giovanelli et al (2016) | 1142 young adults (54% female)Quasi-experimental study, USA | Custom-designed questionnaire assessing ACEs and administrative record inspection | Single yes/no question assessing alcohol and substance use | ACEs were associated with substance use. Sociodemographic and individual characteristics mediated the effect of ACEs on substance use. | 1 |
| Goings et al (2022) | 406 young adults (59.4% female)Cohort study, USA | CTQ-SF, 50 adaptation of the Ineffective Arguing Inventory 57 | Alcohol, cannabis, and substance use was assessed using the instrument from the Monitoring the Future study. 58 | Participants with more ACEs reported more alcohol and cannabis use than those with fewer ACEs. | 2 |
| Goldstein, Faulkner, et al (2013) | 93 young adults (76.3% female)Cross-sectional study, Canada | CTQ-SF 50 | Alcohol use was assessed using items from the Ontario Student Drug Use and Health Survey 59 and the AUDIT 32 | ACEs were not correlated with alcohol use. | 2 |
| Goldstein, Henriksen, et al (2013) | 4468 young adults (female 49.9%)Cross-sectional study, USA | Questions adapted from the CTQ 30 and CTS 31 | Alcohol abuse was measured using the Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV version (AUDADIS-IV) 60 | ACEs were associated with alcohol use disorder only before controlling for Axis I disorders. The interaction of age and ACEs was associated with alcohol use disorder. | 2 |
| Gomis-Pomares et al (2021) | 420 young adults (63.3% female)Cross-sectional study, Spain | Spanish version of the ACE scale 7 | Alcohol and drug use was assessed via the Brief COPE substance use subscale 61 | ACEs were associated with drug use but not alcohol use. | 2 |
| Grigsby et al (2020) | 1389 young adults (59% female)Cohort study, USA | Spanish version of the ACE scale 7 | Substance use frequency was assessed using self-report questions. Negative consequences of substance use were measured using items from the Rutgers Alcohol Problem Index (RAPI) 63 | ACEs were associated with binge drinking, cannabis use, and negative consequences but not with alcohol use. | 262 |
| Grummitt et al (2022) | 569 young adults (70% female)Cross-sectional study, Australia | Items from the Family Health History Questionnaire. 64 | Alcohol use and related problems were measured using the AUDIT. 32 Drug use and related problems were measured using the Drug Use Disorders Identification Test (DUDIT). | ACEs were associated with alcohol and drug use. | 2 |
| Hahn et al (2016) | 425 young adults (71% female)Cross-sectional study, USA | Child Abuse and Trauma Scale (CATS) 65 | Alcohol use was assessed using the Modified Daily Drinking Questionnaire (DDQ-M) 66 | Alexithymia and negative urgency mediated the relationship between ACEs and alcohol use. | 1 |
| Hayatbakhsh et al (2009) | 3285 young adults (52% female)Cohort study, Australia | Three questions about sexual abuse were derived from the Los Angeles Epidemiologic Catchment Area project 67 | Self-reported cannabis use | Sexual abuse was associated with cannabis use. | 2 |
| Hughes et al (2019) | 14 661 young adults (60.4% female)Cross-sectional study, multinational: the Czech Republic, Lithuania, the Republic of Moldova, Montenegro, Poland, Romania, Russia, Serbia, Ukraine and the former Yugoslav Republic of Macedonia | ACE scale 7 | Single yes/no questions were used to assess alcohol and drug use | ACEs were associated with alcohol and drug use. | 2 |
| Jester et al (2015) | 1064 young adults (31% female)Cohort study, USA | Exposure to parental violence was measured via the CTS 31 | Alcohol use was measured with the Drinking and Drug History questionnaire. 68 | Exposure to parental violence had indirect effects on alcohol use via distress and coping expectancy. | 2 |
| Kalpidou et al (2021) | 194 young adults (80.4% female)Cross-sectional study, USA | ACE scale 7 | Alcohol use was assessed using the Short Michigan Alcohol Screening Test (SMAST). 55 Drug use was assessed using the Drug Abuse Screening Test-10 (DAST-10). 69 | Negative coping mediated the relationship between ACEs and drug and alcohol use. | 2 |
| Kameg and Mitchell (2021) | 616 young adults (88.8% female)Cross-sectional study, USA | ACE scale 7 | Alcohol use was assessed using the AUDIT. 32 Drug use was assessed using the DAST-10. 69 | ACEs correlated with alcohol and drug use. | 0 |
| Kappel et al (2021) | 2701, young adults (53% female)Cross-sectional study, Honduras | Items derived from the ISPCAN Child Abuse Screening Tool-Retrospective (ICAST-R) 70 and the JVQ 37 | Single yes/no items were used to assess binge drinking and drug use | ACEs were associated with drug and alcohol use. | 2 |
| Keeshin and Campbell (2011) | 64 homeless young adults, (72.7% female)Cross-sectional study, USA | Modified version of the ACE scale 7 | Interview questions about substance use | Participants with ACEs did not significantly differ in current drug use from participants without ACEs. | 0 |
| Kerr et al (2009) | 560 street-involved young adults (34% female)Cross-sectional study, Canada | Childhood trauma interview 71 | Interview questions about injection drug use | ACEs were associated with injection drug use. | 2 |
| Klein et al (2009) | 283 young adult ecstasy users Cross-sectional study, USA | CTQ 50 | Ecstasy use and related problems were assessed using a questionnaire created for this study | ACEs were associated with high ecstasy use. | 2 |
| Kogan et al (2021) | 409 young menCohort study, USA | ACE scale 7 | Substance abuse was assessed using a 9-item scale from Harrison et al 33 | The relationship between ACEs and substance abuse was mediated by stress, defensive/hostile schemas, social and developmental risk factors. | 1 |
| Konings et al (2012) | 1636 young adults (55% female)Cohort study, Greece and the Netherlands (nonrelevant) | Self-report question about parental physical punishment | Self-report question about frequency of cannabis use | Physical punishment was not associated with cannabis use. | 1 |
| Lagdon et al (2021) | 640 young adults (75% female)Cross-sectional study, UK | Items were adopted from Christoffersen et al 72 | Problematic alcohol use was assessed using the AUDIT 32 | ACEs were not associated with alcohol use. | 2 |
| Liu et al (2020) | 225 young adults (52.9% female)Cross-sectional study, USA | CTQ 50 | Alcohol use was assessed using the AUDIT 32 | The relationship between ACE and alcohol use was moderated by heart rate variability. | 2 |
| Lo and Cheng (2007) | 762 young adults (51% female)Cohort study, USA | Self-report during interviews | Self-report questions were used to measure alcohol, cannabis, and other drug abuse | ACEs were associated with alcohol, cannabis and other drug use. When depression was added to the model, most associations became nonsignificant. | 1 |
| Loxton et al (2021) | 8961 young womenCohort study, Australia | ACE scale 7 | Self-report questions were used to assess alcohol and illicit drug use | After adjusting for demographic variables, ACEs were associated with drug use but not binge drinking. | 1 |
| (Marks et al, 2021) | 245 young adults (57.3% female)Cross-sectional study, USA | ACE scale 7 | Alcohol use was assessed using the Daily Drinking Questionnaire (DDQ) 73 and Young Adult Alcohol Consequences Questionnaire (YAACQ) 74 | ACEs were associated with alcohol use. College attendance and age interacted with ACEs in predicting alcohol use. | 2 |
| Mersky et al (2013) | 1142 young adults (sex ratio unknown)Quasi-experimental study, USA | Record inspection, Life Events Checklist 75 | Measures were created for this study to assess frequency of alcohol and cannabis use | ACEs were associated with frequent alcohol and drug use. | 1 |
| Meshesha et al (2019) | 558 young adults (49.9% female)Cross-sectional study, USA | Childhood physical and sexual abuse were assessed using items from the Trauma History Questionnaire 76 | Frequency of cannabis use was assessed using Timeline Follow-Back (TLFB) method .77,78 Problems with cannabis use were assessed using the Marijuana Problems Scale (MPS)78 | The effect of physical abuse on cannabis use was mediated by coping motive. The effect of sexual abuse was not significant. | 2 |
| Messman-Moore et al (2009) | 339 young womenCohort study, USA | CTQ 50 and Sexual Experiences Survey (SES) 79 | Alcohol use was assessed using the Drinking Habits Questionnaire (DHQ) 80 | When the path from ACEs to alcohol use was removed from the SEM, the fit improved. | 1 |
| Messman-Moore et al (2013) | 229 young womenCross-sectional study, USA | CTQ, 50 revised SES 79 | Alcohol use was assessed using the AUDIT. 32 Drug use was measured using the Frequency of Involvement subscale of the Cognitive Appraisal of Risky Events Questionnaire—Revised (CARE–R) 81 | Women with a history of sexual assault during childhood reported higher levels of alcohol use and related problems than those who had no such history. | 2 |
| Mills et al (2017) | 3778 young adults (53% female)Cohort study, Australia | Record inspection | Cannabis abuse and dependence were assessed using custom-designed questions and the CIDI 82 | ACEs were associated with early cannabis use but not cannabis dependency. | 2 |
| Murase et al (2021) | 508 young adults (73% female)Cross-sectional study, USA | CATS 65 | Alcohol use was assessed using the DDQ-M 66 | The effect of sexual abuse and neglect on alcohol use was mediated by anxious attachment and selfless interpersonal problems. | 2 |
| Musa et al (2018) | 400 young adults (58.5% female)Cross-sectional study, Bosnia and Herzegovina | ACE scale 7 | Alcohol and drug use was assessed using self-report questions | ACEs were associated with alcohol and drug use. | 2 |
| Narendorf et al (2018) | 374 homeless young adults (54.0% female)Cross-sectional study, USA | ACE scale 7 | Substance use was assessed using items from Monitoring the Future.75 | Groups with more ACEs were more likely to engage in substance use. | 2 |
| Narendorf and McMillen (2010) | 325 young adults (61% female)Cohort study, USA | CTQ, 50 3 items from Russell (1986) were used to measure sexual abuse | Use of alcohol, cannabis and other drugs was assessed using modified items from the Diagnostic Interview Schedule, version IV (DIS-IV). 83 Substance abuse and dependence were assessed using items from the Comprehensive Addiction Severity Index for Adolescents 84 | ACEs were associated with substance dependence, cannabis and alcohol use at the age of 19 y. | 1 |
| Newbury et al (2018) | 2066 young adults (51% female)Cohort study, UK | Prospective ACEs were assessed via interviews with caregivers, home inspections, and report inspections. Retrospective ACEs were assessed using the CTQ 50 | Alcohol and cannabis dependence was assessed using the DIS-IV 83 | ACEs were associated with alcohol or substance dependence. | 1 |
| Oshri et al (2017) | 1265 young adults (59.3% female)Cohort study, USA | Items adapted from Malamuth et al 85 | Alcohol and cannabis use were assessed using single questions | ACEs were associated with alcohol and cannabis use. | 1 |
| Oshri, Kogan, et al (2018) | 9421 young adults (55.6% female)Cohort study, USA | Four items from the National Longitudinal Study of Adolescent to Adult Health (Add Health) 86 | Cannabis use was assessed using self-report questions | ACEs were associated with cannabis use. | 1 |
| Oshri, Liu, et al (2018) | 225 young adults (52.9% female)Cross-sectional study, Canada | CTQ-SF 50 | Alcohol use was assessed using the AUDIT 32 Drug use was assessed using the DUDIT | ACEs had an indirect effect on alcohol use via delayed reward discounting that was moderated by heart rate variability. | 2 |
| Pereira-Morales et al (2017) | 274 young adults (75.1% female)Cross-sectional study, Columbia | Spanish version of the CTQ-SF 50 and Family APGAR 86 | Alcohol and substance use was assessed using the ASSIST 53 and the AUDIT 32 | The best fit model for predicting polysubstance use included the interaction of family functioning with alcohol use and anxiety but not ACEs. | 2 |
| Richardson et al (2019) | 225 young adults (52% female) Cohort study, USA | CTQ 30 | Urine samples were used to assess cannabis use. | ACEs were correlated with cannabis use. | 2 |
| Rollins and Crandall (2021) | 489 young adults (51% female)Cohort study, USA | Items from the ACE scale 7 | Substance abuse was assessed using the AADIS 48 | Self-regulation partially mediated the relationship between ACEs and substance abuse. | 2 |
| Rougemont-Bücking et al (2018) | 5308 young adult male military conscriptsCross-sectional study, Switzerland | Parental relationship quality and parenting quality were assessed using 2 items from the European School Survey Project on Alcohol and Drugs (ESPAD)88,89. The presence of a family member with a mental health disorder was determined using the family history section of the Addiction Severity Index 89 . Physical or sexual assault by a family member was assessed using items from the PDS 90 | A self-report questionnaire was used to assess alcohol and substance use | ACEs were associated with alcohol and substance use. | 2 |
| Russotti et al (2021) | 391 young adults (51.3% female)Cohort study, USA | Records were coded using the Maltreatment Classification System (MCS) 91 | Substance use disorder was assessed using the DIS-IV 83 | Externalizing behavior mediated the relationship between ACEs and substance use disorder. | 2 |
| Saadatmand et al (2020) | 440 young adults (52.3% female)Cross-sectional study, USA | Childhood Exposure to Violence Scale 92 | Substance use assessment was based on items from the CDCYouth Risk Behavior Surveillance System (YRBSS) | ACEs were associated with substance use. | 2 |
| Shin et al (2018b) | 336 young adults (51.5% female)Cross-sectional study, USA | CTQ, 30 Verbal Aggression Scale (VAS) 93 | Alcohol use was assessed using the RAPI. 63 Drug dependence was assessed using the substance use section of the CIDI 94 | ACEs were associated with alcohol use. | 2 |
| Shin et al (2016) | 300 young adults (51.5% female)Cross-sectional study, USA | CTQ, 30 the Maltreatment and Abuse Chronology of Exposure (MACE) scale 29 | Alcohol use and alcohol use disorder were assessed using self-report questions, the RAPI 63 and the CIDI 94 | ACEs were associated with alcohol use. | 2 |
| Shin, Hassamal, et al (2015) | 337 young adults (52.5% female)Cross-sectional study, USA | Computer-assisted self-interviewing (CASI) method of the CTQ 30 | Alcohol use and alcohol use disorder were assessed using self-report questions, the RAPI 63 and the CIDI 94 | Psychological distress mediated the effect of ACEs on alcohol use and dependence. | 2 |
| Shin, Jiskrova, et al (2019) | 335 young adults (52% female)Cross-sectional study, USA | CASI method of the CTQ 30 | Alcohol use and alcohol use disorder were assessed using self-report questions, the RAPI 63 and the CIDI 94 | Dysregulation and peer alcohol use mediated the effect of ACEs on alcohol use. Dysregulation and psychological symptoms mediated the effect of ACEs on alcohol dependence. | 2 |
| Shin et al (2020) | 208 young adults (78% female)Cross-sectional study, USA | CTQ 30 | Alcohol use problems were assessed using self-report questions and the RAPI 63 | Coping motives mediated the effect of ACEs on alcohol-related problems. | 2 |
| Shin, Lee, et al (2015) | 286 young adults (51.9% female)Cross-sectional study, USA | CASI method of the CTQ 30 | Alcohol use and alcohol use disorder were assessed using self-report questions, the RAPI 63 and the CIDI 94 | The urgency aspect of impulsivity mediated the effect of ACEs on alcohol use and dependence. | 2 |
| Shin et al (2018a) | 335 young adults (51.5% female)Cross-sectional study, USA | CTQ , 30 VAS 93 | Alcohol use was assessed using the AUDIT. 32 | Alcohol use was higher among classes with more ACEs. | 2 |
| Shin, Wang, et al (2019) | 339 young adults (52.5% female)Cross-sectional study, USA | CTQ 30 | Alcohol use-related problems were assessed using self-report questions and the RAPI 63 | Parental warmth moderated the effect of ACEs of alcohol use problems. | 2 |
| Smith et al (2010) | 508 young adults (23% female)Cohort study, USA | Exposure to intimate partner violence (IPV) was assessed using the CTS 31 | Self-report questions were used to assess problems with alcohol and drug use | Exposure to IPV was associated with alcohol use among female but not male participants. The effect of ACEs on drug use was not significant. | 2 |
| Smith et al (2005) | 637 young adults (27.1% female)Cohort study, USA | Record inspection based on Cicchetti and Barnett’s 95 system | Drug use was assessed during interviews | ACEs were associated with drug use. | 2 |
| Taşören (2017) | 43 incarcerated young menCross-sectional study, Turkey | CTQ 30 | Drug use was assessed with a single self-report question. | ACEs were associated with drug use. | 1 |
| Turner and Lloyd (2003) | 1803 young adults (23% female)Cross-sectional study, USA | The Life History Calendar (LHC) derived from Freedman et al 96 was used to assess exposure to adversity | Drug use and dependence was assessed using an updated version of the Michigan CIDI 97 | ACEs were associated with drug use. | 2 |
| Vilhena-Churchill and Goldstein (2014) | 125 young adults (66.9% female)Cross-sectional study, Canada | CTQ-SF 50 | Cannabis use and related problems were assessed using self-reported questions and the MPS 98 | Emotion dysregulation and coping motive mediated the effect of ACEs on cannabis use. | 2 |
| Villamil Grest et al (2021) | 1179 young adults (58.95% female)Cohort study, USA | ACE scale 7 | Alcohol and cannabis use were assessed using self-report questions | ACEs were associated with alcohol and cannabis use. | 2 |
| Villanueva and Gomis-Pomares (2021) | 490 young adults (62.4% female)Cross-sectional study, Spain | Spanish version of the ACE scale 7 | Alcohol and drug use was assessed using self-report questions | ACEs were associated with alcohol and drug use. However, having a family member with mental illness was inversely associated with alcohol and drug use. | 2 |
| Wardell et al (2016) | 232 young adults (53% female)Cross-sectional study, Canada | CTQ-SF 50 | Alcohol and cannabis use was estimated using the TLFB method 76 ; self-report questions, the RAPI63,98 and the MPS | Negative urgency mediated the effect of ACEs on alcohol and cannabis use. | 2 |
| Windle et al (2018) | 2969 young adults (63% female)Cross-sectional study, USA | ACE scale 7 | Alcohol and cannabis use were assessed via a self-report questionnaire | ACEs were associated with alcohol and cannabis use. | 2 |
| Wymbs et al (2017) | 433 young adults (62.8% female)Cross-sectional study, USA | CTQ-SF 50 | Alcohol use was assessed with the AUDIT. 32 Drug use was assessed using a self-report questionnaire | ACEs were associated with drug use but not with alcohol use. | 1 |
| Young et al (2006) | 41 482 young adult male US Navy recruitsCross-sectional study, USA | ACE scale, 7 CTQ , 30 CTS 31 | Alcohol use was assessed using the AUDIT 32 | ACEs were associated with alcohol use. However, emotional neglect had an inverse association. | 2 |
Substance use measurements
Most studies included assessments of alcohol (n = 55) or illicit drug use (n = 48). Approximately one-fourth of the studies (n = 22) incorporated specific measurements of cannabis use. Self-report questions created by the authors were the most common approach (n = 36) for assessing alcohol, cannabis, or drug use; in most cases, it was the only measure used (n = 34). The instruments most frequently used to assess substance use were the Alcohol Use Disorders Identification Test (AUDIT) 32 (n = 12); the Rutgers Alcohol Problem Index (RAPI) 63 (n = 9); and the Composite International Diagnostic Interview (CIDI) 51 (n = 8). Six studies also used questions from other published studies. Other measures used in 3 or fewer studies are noted in Table 2.
ACE measurements
The most widely used ACE measure was the Childhood Trauma Questionnaire (CTQ) (n = 33), in long or short form (Bernstein et al30,50), closely followed by the questionnaire from the original ACE study (n = 20). 7 Only 7 studies used record inspection; a similar number used items that the researchers created or those published in other studies. The Conflict Tactics Scale 31 was the questionnaire most often used (n = 5) to measure parental conflict and estimate family dysfunction. Information on the other instruments used in 1 or 2 studies is presented in Table 2.
Results
Unspecified ACEs
More than half of the studies (n = 56) reported an association between unspecified childhood maltreatment or family dysfunction and substance or alcohol use. Most of these studies (n = 51) reported a positive association between these 2 variables. Individuals with ACEs were more likely to use or abuse alcohol or other substances during early adulthood; this association was pronounced for multiple ACEs.5,6,99-147 Interestingly, Crandall et al 99 showed that when counter-ACEs were included in the model, they weakened the significant association of ACEs with substance use. This suggests that positive and encouraging childhood experiences can not only “cancel out” the effect of adverse experiences but also serve as a protective factor against substance use in early adulthood. However, only one study explored this association; therefore, these findings are only preliminary.
Nevertheless, 4 studies found no association between unspecified childhood ACEs and substance use in young adults. Although Goldstein et al 149 reported no significant correlation between ACEs and past-year drinking among adults in the welfare system, this was a correlational analysis that did not control for covariates. Other studies within the same population have demonstrated the importance of considering covariates. For instance, Ferguson et al 103 showed that childhood abuse was indirectly related to substance use through street victimization among young homeless adults.
Despite removing the paths from different forms of ACEs to posttraumatic stress disorder (PTSD) symptoms in the final SEM, Messman-Moore et al 150 found that PTSD symptomatology was associated with higher use of various substances. It is possible that removal of the pathways between ACEs and PTSD did not entirely erase their relationship because they were the only variables assessed retrospectively. In addition, Langdon et al 151 showed that among students, ACEs were not associated with alcohol use either individually or in a model controlling for age, sex, and relationship status and including social support as a mediator. The authors suggested that the lack of an expected positive association between ACEs and alcohol use was due to the large proportion of female participants (approximately 75% of the sample). However, Exner-Cortens et al 152 found no association of physical and psychological victimization in childhood with heavy drinking or cannabis or other drug use among male or female participants. The lack of association may be due to the use of only 3 items to assess abuse.
Some studies (n = 13) that found increasing substance use among those with ACEs investigated this association in greater detail and identified significant mediators and moderators. Anderson et al 142 reported that exposure to childhood maltreatment positively interacted with the thickness of the lingula of the anterior cerebellar vermis and that they jointly predicted alcohol and drug use. This brain structure is also known as lobule I of the anterior cerebellar vermis, which is the first small lobe of the median part of the cerebellum connecting the 2 hemispheres. Anderson et al 142 hypothesized that people with thicker lingula are more likely to consume stronger alcohol as their vestibular sensitivity is blunted; thus, they require more or stronger alcohol to achieve the sense of vestibular inebriation or being “spaced out”. Giovanelli et al 110 attributed the positive association between multiple ACEs and drug or alcohol use to 9 mediators, including cognitive skills, socioemotional adjustment, school commitment, and juvenile arrest. Likewise, Cho and Kogan 148 demonstrated that exposure to harsh and unresponsive parenting was associated with precocious transitions, which increased economic instability and led to a weaker future orientation; this inversely predicted the use of any substances. Although their study had a cohort design and assessed substance use over time, the assessment of ACEs was performed retrospectively, thereby limiting causal inferences.
Hahn et al 113 showed that exposure to maltreatment was associated with an increased likelihood of alexithymia, which increased the inclination for impulsive behavior following negative affect, increasing alcohol use. Supporting the role of impulsivity, Wardell et al 141 reported that the association between ACEs and problematic alcohol or cannabis use was positively mediated by negative urgency. Oshri et al 128 also demonstrated that the association between exposure to early life adversity and alcohol use was positively mediated by impulsive decision-making, exemplified by delayed reward discounting, among those with low heart rate variability (HRV) in response to mild stressors but negatively mediated among those with high HRV responses to mild stressors.
Rollins and Crandall, 130 using a cohort study with prospective measurement, showed that ACEs decreased self-regulation during early childhood, negatively predicting alcohol and drug use. Kalpidou et al 114 also suggested that childhood maltreatment facilitated maladaptive coping, which was associated with the use of alcohol and illicit drugs. Kogan et al’s 117 structural equation model provided a more straightforward path from early life adversity to the consumption of drugs or alcohol. They found that substance use developed from exposure to ACEs through stressors and defensive relational schemas, which heightened the risk of social maladjustment and increased substance use. However, although mediators and substance use were assessed at various time points, ACEs were assessed retrospectively. While this raises a question regarding the causality between exposure to ACEs and contextual stressors, the pathway from heightened stress to social maladjustment through hostile schemas was strongly supported and further confirmed by Rollins and Crandall. 130 On a larger scale, also using a prospective design, Russotti et al 132 showed that early and late (before and after the age of 5 years, respectively) experience of adversities, or chronic ACEs, led to the development of externalizing behaviors, creating an association with substance use disorders in early adulthood.
Shin et al 153 examined problematic drinking reported that it could be driven by the motive to cope, which was evoked by past maltreatment. Vilhena-Churchill and Goldstein 139 further investigated this association with a different substance. They found that poor coping mediated the association between emotional dysregulation and the use of cannabis. Given that emotional dysregulation was associated with exposure to ACEs, their results suggested a stepwise process whereby exposure to traumatic experiences contributed to emotional dysregulation, inducing poor coping that facilitated substance use. However, as this was a cross-sectional study, the inferred causality needs to be tested and verified with a longitudinal design. In addition, Marks et al 121 reported a positive association between ACEs and weekly alcohol use in college students and women but not in nonstudents and men.
Interestingly, Baranger et al 145 showed that childhood adversity could moderate the effect of the PER1 gene on alcohol use. They found that male and female carriers of the C allele were more likely to report higher alcohol abuse only when they experienced high levels of childhood maltreatment (not low or medium levels). Similarly, Forster et al 107 found that exposure to multiple childhood adversities positively moderated the influences of self-focus, identity exploration, and experimentation in emerging adulthood on binge drinking and drug use. Unfortunately, despite utilizing participants from a longitudinal study, Forster et al 107 assessed ACEs retrospectively. This prevents determination of whether the moderating effect of ACEs was due to causal influences or simple correlations.
The results of studies examining the association between unspecified ACEs and substance use in young adults revealed a robust association between these 2 variables. Furthermore, some studies suggested that this association could be explained via impulsive decision-making and maladaptive coping. These 2 mediators clearly explained how the inability to cope with stressors in early adulthood could lead to substance use as a means of maladaptive coping.
Childhood maltreatment
Almost all included studies assessed childhood maltreatment (n = 81). Of these studies, more than half (n = 51) reviewed a specific form of childhood maltreatment in the analysis, mainly physical (n = 39) and sexual abuse (n = 35), followed by emotional abuse (n = 29), physical neglect (n = 27), emotional neglect (n = 24), and street victimization (n = 8).
Physical abuse
Approximately half of the studies investigating physical abuse found that it was associated with substance use in early adulthood. Physical maltreatment during childhood was related to injection drug use.109,154,155 Although DeBeck et al 156 employed a cohort design, their retrospective assessment of ACEs precluded causal inferences. Only one study found a significant sex difference; specifically, there was an association between physical abuse and substance use in only female but not male participants. 109 Physical abuse also predicted cannabis and other drug use and abuse in some studies, including prospective cohort studies.5,115,120,123,126,130,142,153,157 -160 However, as some of these studies reported, this association was not always direct. Anderson et al 142 reported that physical maltreatment was strongly associated with drug use among subjects with the greatest lingular thickness, while Meshesha et al 160 showed that physical abuse increased daily cannabis use through coping motives rather than enhancement or social motives.
Similar to the association with drug use, experiencing physical abuse in childhood was associated with increased alcohol use.5,115,126,142,157,161 -168 Given that Newbury et al 126 confirmed this association in a prospective cohort study, it is likely that this relationship is causal. Nevertheless, this association is not always present. Dube et al 103 reported that experiencing physical abuse was not significantly associated with ever drinking alcohol. Lo and Cheng 158 demonstrated that after including depression in the model, physical abuse was no longer a significant predictor of alcohol use but not drug use. Extending this finding, Goldstein et al 149 showed that physical abuse was associated with alcohol use only before controlling for Axis I and personality disorders. Their results also indicated a significant interaction with age, with a more pronounced link between physical abuse and alcohol use disorder in younger participants.
Three studies reported an inverse association between childhood physical abuse and substance use. First, Narendorf and McMillen 169 demonstrated that physical abuse was associated with a lower likelihood of substance dependence at the age of 19. Nevertheless, at the age of 18, the association was not significant. Likewise, Saadatmand et al 170 found that being a victim of adult or peer violence was inversely related to alcohol and drug use in males and inversely related to polydrug use in both sexes. Finally, Shin et al 135 reported that although physical abuse was positively correlated with problematic drinking, it was negatively associated with drinking frequency.
Furthermore, some studies did not find a significant association between physical abuse and substance use.114,135,136,153,169-174 There is no single obvious reason that explains the absence of this association. In some cases, the lack was attributed to the presence of a mediator or covariate. Murase et al 173 found that physical abuse (in the form of physical punishment) was associated with increased avoidant attachment and inappropriate attention seeking, which in turn was associated with increased problems related to alcohol consumption but not alcohol consumption itself. In other cases, the lack was attributed to the overall effect of another type of maltreatment, such as sexual abuse. 171
Thus, despite overwhelming evidence that childhood physical abuse is associated with substance use problems, these studies suggest that this association needs to be considered cautiously. There appears to be an association between physical abuse and substance abuse, but it is highly influenced by covariates such as ACEs, mental health, and sociodemographic characteristics as well as by mediators such as sensitivity to inebriation.
Sexual abuse
Most studies have reported that experiencing sexual abuse in childhood is associated with increased substance use among young adults. In particular, the association of childhood sexual abuse with cannabis use was pronounced. Hayatbakhsh et al 175 reported that forced sexual contact and rape were associated with both frequent and occasional cannabis use in women but only with frequent cannabis use in men. In addition, Rougemont-Bücking et al 157 showed that sexual assault by a stranger was associated with increased psychostimulant and hallucinogen use. In contrast, sexual abuse by a family member was associated with lower use of cannabis only. Mills et al 123 conducted a prospective cohort study and reported that sexual abuse was positively associated with daily cannabis use after adjusting for sex. Likewise, childhood sexual abuse has been shown to increase the use of other drugs in numerous studies, including a cohort study with retrospective ACE assessment.5,109,115,131,136,154,166,170,171 Interestingly, in a prospective cohort study, Smith et al 136 found that sexual abuse specifically during adolescence predicted drug use in early adulthood. However, these results were not universal. In a prospective cohort study, Abajobir et al 109 reported that sexual abuse was associated with injection drug use among only female participants and that after adjusting for sociodemographic characteristics, this relationship was no longer significant.
In addition to a consistent association between childhood sexual abuse and increased alcohol use, some studies identified influential mediators and moderators.5,99,102,130,153,158,161 -163,165,166,168,173,176 Although this association is supported by the findings of a cohort study, causality cannot be inferred because this cohort study utilized a retrospective assessment of ACEs. 169 Cronin et al 100 reported that after controlling for PTSD and other disorders, sexual abuse was associated with alcohol misuse only among women, while Goldstein et al 111 showed that sexual abuse was associated with alcohol use disorder (AUD) only before controlling for Axis I and personality disorders. Murase et al 173 found that sexual abuse was associated with increased anxious attachment, which led to heightened eagerness to accommodate others and was associated with alcohol consumption in early adulthood. Finally, many studies, including prospect cohort studies, did not find an independent direct association between childhood sexual abuse and substance use problems120,124,135,155,156,160,161,168,177; thus, this association appears heavily dependent on mediators and moderators.
Emotional abuse
Similar to physical and sexual abuse, emotional abuse has been shown to affect substance use. Several studies, including prospective cohort studies, found that emotional abuse predicted increased cannabis use.120,123,131,152,158 Importantly, Exner-Cortens et al 152 specified that emotional abuse was associated with cannabis use among only male participants. Moreover, in a prospective cohort study, Mills et al 123 showed that emotional abuse was predictive of an early start (before the age of 17) of cannabis use rather than daily use or cannabis dependence. Emotional abuse was also associated with increased use of other drugs according to various studies, including prospective cohort studies.5,108,114,123,125,130
Additionally, childhood emotion abuse was associated with increased use of alcohol in early adulthood.5,39,102,130,134,135,152,153,158 ,161 -163,165,103,170,174,178 However, most studies used mixed samples, and the cohort study of Exner-Cortens et al 152 used retrospective ACE assessment. Furthermore, unlike cannabis use, alcohol use followed childhood emotional abuse in men but not women. Furthermore, Goldstein et al 112 suggested that, similar to physical abuse, emotional abuse was associated with AUD only before adjusting for Axis I and personality disorders. Nevertheless, more complex models have shown that the influence of emotional abuse could be indirect. Shin et al 161 reported that emotional abuse was associated with behavioral dysregulation, which in turn was associated with binge drinking, problematic alcohol consumption, and AUD. Behavioral dysregulation was also partially associated with other psychological symptoms that also led to AUD.
Moreover, behavioral dysregulation led to increases in perceived use of alcohol by peers, which was associated with binge drinking. Another mediator was impulsivity (operationalized as negative urgency), which was fueled by emotional abuse and led to binge drinking and AUD. 162 Distress was an additional mediator through which emotional maltreatment could lead to problematic drinking. 168 However, protective factors were also identified. The interaction between emotional abuse and parental warmth predicted inappropriate alcohol use; specifically, the association between emotional abuse and inappropriate alcohol use was weaker when parental warmth was high. 135
Although 4 studies reported no significant association between emotional abuse and substance use,142,154,156,166 most studies suggested that childhood emotional abuse is a risk factor for substance use, especially alcohol use, in early adulthood. Although DeBeck 156 used a cohort design, the retrospective assessment of ACEs precludes exclusion of emotional abuse as a risk factor for substance use. Similar to the results for unspecified ACEs, the association of emotional abuse with alcohol use was mediated by impulsive decision-making. In addition, associations of emotional abuse with substance use, specifically cannabis use, were reported in some studies, but further research is needed.
Neglect
The association between physical or emotional neglect in childhood and substance use during early adulthood is less clear than the association of abuse with substance use. In a prospective cohort study, Abajobir et al 120 showed that a combined variable consisting of physical and emotional neglect was associated with cannabis use and dependence. In addition, Oshri et al 155 assessed only emotional neglect and reported that it was associated with cannabis use. However, Fusco, 158 Narendorf and McMillen, 169 and Saadatmand et al 170 did not find any significant associations of physical and emotional neglect (as combined or separate variables) with cannabis use.
Similar inconsistencies were observed regarding the use of other drugs or multiple substances. Bellis et al 5 and Musa et al 124 demonstrated that emotional neglect was associated with increased drug use. A similar association of combined physical and emotional neglect with increased drug use was found in males and females. 136 However, Abajobir et al 120 employed a prospective cohort design and demonstrated that this association was present in women but not men for injection drug use. Furthermore, Newbury et al 126 found that physical neglect was associated with substance dependence when evaluated prospectively and retrospectively, while emotional neglect was associated with substance dependence only when assessed retrospectively. Nevertheless, DeBeck et al 156 and Kerr et al 154 did not find a significant association between physical and emotional neglect (assessed separately) and injection drug use. Likewise, Grummitt et al, 166 Villanueva and Gomis-Pomares, 174 Narendorf and McMillen, 169 and Pereira-Morales et al 178 found no influence of physical or emotional neglect on substance use. Furthermore, Saadatmand et al 170 reported no association of combined physical and emotional neglect (operationalized as feeling unsafe during childhood) with polydrug use. Thus, prospective cohort studies did not validate the results of cross-sectional studies or studies that retrospectively assessed ACEs, highlighting the need for further investigation.
In addition, there was no clear association between childhood neglect and alcohol use. Shin et al161,168 reported a correlation between combined neglect and alcohol dependency. Murase et al 173 specified that combined neglect was associated with alcohol consumption through anxious attachment and the desire to accommodate others; however, Fusco 158 , Shin et al135,162 did not find that these mediators were significant. Moreover, Saadatmand et al 170 showed that combined neglect (feeling unsafe) was negatively related to alcohol use. Similarly, Young et al 163 reported an inverse association between emotional neglect and alcohol use. However, some reports have shown increased alcohol use in individuals exposed to physical or emotional neglect.5,102,153 Other studies have found that this association is not significant.166,169,174,178 While Goldstein et al 112 showed that physical neglect was associated with AUD only before controlling for Axis I and personality disorders, this is unlikely to be the sole explanation for inconsistent results, as not all of the studies reporting a lack of association controlled for psychopathologies.
Taken together, the findings regarding the association between childhood neglect and substance abuse in early adulthood did not indicate a clear conclusion. This lack of consistency can largely be attributed to differences in the operationalization of neglect, as some studies examined combined physical and emotional neglect, others examined physical neglect alone, and others examined emotional neglect alone. Unfortunately, few studies used the same operationalization of neglect. Consequently, further research into specific domains of neglect is needed to discern the association between these 2 variables.
Street victimization
Street victimization is another type of ACE, but only a few of the included studies assessed this variable (n = 5). As the content of street victimization can vary, corresponding associations with substance use also differed. Cater et al 165 found that being a victim of property crime was associated with problematic alcohol use only among males, but witnessing any violence was associated with alcohol use in both sexes. However, Saadatmand et al 170 reported that witnessing gunfire or physical assault was inversely related to alcohol use but positively associated with cannabis use among young adults (and specifically young male adults). In addition, witnessing murder was associated with less problematic substance use among females than among males. However, seeing or being a victim of an assault with a weapon was associated with polydrug use only among women.
Furthermore, although Kappel et al 114 showed that witnessing violence in the community was associated with increased binge drinking and drug use in both men and women, Fernandes et al 105 did not find an association between community or collective violence and any substance use after adjusting for sociodemographic characteristics.
Family dysfunction
Approximately 1 in 4 studies assessed the family environment during childhood (n = 24). Most studies evaluated household substance use (n = 13), followed by parental conflict (n = 11). Having an incarcerated family member, having a family member with mental health problems, and living with parents who were separated or divorced were less frequently assessed (n = 9). One unique study assessed family functioning in general. Pereira-Morales et al 178 found that the model that explained the most variance in polydrug use included family functioning, alcohol use, and anxiety rather than physical and emotional abuse, neglect, and sexual abuse.
Parental substance use
Almost all studies (n = 12) assessing household substance use found that it increased the likelihood of substance abuse in early adulthood. Allem et al 131 showed that household substance use was directly associated with cannabis use. Additional studies reported that living in a household with a person who used drugs or alcohol facilitated the use of other substances.5,166,174,179 Likewise, household substance use was associated with alcohol use in early adulthood.5,103,131,162,163,166,168,174 Given that parental substance use is associated with subsequent substance use by their offspring through multiple pathways, such as genetics 168 or parental behavior, 131 the precise effect of growing up with household substance abuse needs further investigation. Interestingly, Kerr et al 154 found that parental drug use was inversely associated with subsequent injection drug use during early adulthood, suggesting that observing the adverse effects of drug use might prevent drug use through vicarious reinforcement. Shin et al 168 showed that parental alcoholism was associated with AUD through increased distress. However, some studies reported no association between parental use of substances and children’s drug or alcohol use in adulthood.124,135
Parental conflict
More than half of the studies reported that witnessing parental conflict was associated with increased substance use during early adulthood. In cross-sectional and prospective cohort studies, witnessing parental conflict significantly contributed to increased drug and alcohol use.5,115,163,180,181 In a prospective study, Jester et al 180 reported that violence directed at either parent increased distress during early adolescence, which led to the expectation that alcohol can create a positive mood and help individuals cope with distress; these beliefs culminated in heavy drinking during early adulthood. However, in another prospective study, Smith et al 181 showed that exposure to domestic violence was associated with alcohol use only in females. Moreover, Grummitt et al 166 did not find a significant association between domestic violence and alcohol use in either sex, and Villanueva and Gomis-Pomares 174 reported that witnessing parents’ violence toward each other decreased alcohol use. However, the study by Jester et al 180 was the only cohort study to prospectively measure ACEs in early childhood (aged 3-5 years), while Smith et al 81 assessed ACEs in adolescence only. This not only supports a direct relationship between exposure to violence at home and alcohol use but also suggests that the identified mediators (increased distress and the expectation that alcohol can alleviate distress) represent a causal pathway from a specific ACE to substance use.
Incarceration
The included studies reported inconsistent findings regarding the association between having an incarcerated family member and substance use during early adulthood. Some reported that this experience was associated with increased cannabis and drug use and alcohol consumption.5,103,131,182 Importantly, although Grigsby et al 182 relied on retrospective assessments of ACEs, the factual nature of this specific experience renders common retrospective report biases less applicable. Nevertheless, Gomis-Pomares et al 179 demonstrated that models predicting alcohol consumption and drug use included not having an incarcerated family member. Furthermore, Grummitt et al 163 showed that having an incarcerated family member was inversely related to alcohol use.
In contrast, Musa et al 124 and Villanueva and Gomis-Pomares 174 did not a significant association between having an incarcerated family member and substance use. Although the inconsistent results cast doubts on the ability of having an incarcerated family member to robustly predict substance use during early adulthood, the presence of this relationship in a cohort study, albeit retrospective, suggests the need for further research.
Mental health issues in the family
Most studies found that having a family member with a mental health issue was associated with increased alcohol use.5,103,131 However, some studies found that this association was not significant,124,157,166 and Villanueva and Gomis-Pomares 174 reported an inverse association. Moreover, Gomis-Pomares et al 179 found that not having relatives with mental health issues predicted alcohol use. Concerning cannabis use, the results were more consistent. Allem et al 131 and Rougemont-Bücking et al 157 found an association between having a family member with mental health issues and cannabis use. Nevertheless, the results were less consistent regarding drug use in early adulthood. Bellis et al 5 and Rougemont-Bücking et al 157 found that having a mental illness in the family was associated with increased drug use in early adulthood. However, Allen et al, 131 Grummitt et al, 166 and Musa et al 124 did not find a significant association, and Villanueva and Gomis-Pomares 174 found an inverse association.
Family separation
Family environment was another factor affecting substance use in early adulthood. One study assessed paternal involvement. Barton et al 146 showed that when biological fathers were involved with their children, they had expectations of future positive events; these expectations were inversely associated with substance use. Other studies investigated the effect of parental separation, which was mainly associated with increased alcohol use.5,103,124 However, some studies found that this association was not significant.115,166,174
Young et al 163 reported that being raised by 2 parents was associated with risky drinking, suggesting an inverse association with parental separation. Regarding drug use, most studies did not find a significant association with parental separation.124,166,174 Only Bellis et al 5 and Kappel et al 115 reported that parental separation during childhood was associated with increased drug use in early adulthood.
Discussion
This literature review aimed to investigate the effects and associations of different types of ACEs on alcohol and drug use by young adults. Specifically, it focused on the associations of different ACEs with use of different types of substances. Despite differences in measurement tools, most of the included studies were of good or excellent quality. Overall, the results demonstrated a robust association between exposure to ACEs before the age of 18 years and subsequent use of alcohol, cannabis, or other illicit drugs between the ages of 18 and 25 years. This association was most pronounced among high-quality studies. Prospective cohort studies repeatedly demonstrated that physical and sexual abuse, physical neglect, and parental conflict predicted substance abuse. Interestingly, the results pertaining to the impact of childhood sexual abuse were mixed. Nevertheless, the results of prospective cohort studies aligned with results from the majority of cross-sectional studies showing a long-lasting impact of multiple ACEs; polyvictimization in childhood is likely to lead to increased use of various substances during adulthood. However, several studies showed that the likelihood of substance abuse in childhood was significant only in individuals with multiple ACEs and that it increased exponentially with every additional ACE.6,107,122,134 This is consistent with the dose‒response association between ACEs and adverse mental health outcomes in adulthood.11,22
In line with the diathesis-stress framework, 18 Baranger et al 145 showed that exposure to ACEs was associated with risky alcohol use among individuals sensitive to stressors due to carrying the minor C allele at rs3027172. In addition to vulnerabilities induced by substance use, risk factors for substance use due to associations of these factors with ACEs were identified. Weak self-regulation, specifically impulsivity, and poor socioeconomic status mediated the association between exposure to ACEs and alcohol or drug use in early adulthood.110,113,130,141,148,155 Furthermore, as expected, exposure to ACEs was strongly associated with substance use, a form of maladaptive coping.117,153 Numerous prospective studies have shown that ACEs are strong predictors of externalizing behaviors and poor self-regulation,130,132 which can increase strain that individuals may attempt to alleviate via the use of substances, regardless of the (in)effectiveness of this strategy in the long term. Taken together, these findings indicate that although exposure to ACEs dramatically increases the risk of alcohol or drug use by young adults, other mechanisms amplify or fully explain this association; these variables can be targeted by relevant interventions. Exposure to ACEs does not inevitably lead to substance use in early adulthood. Crandall et al 98 compared the effect of ACEs with favorable childhood experiences. The results, which are preliminary but promising, showed that such counter-ACEs could negate the impact of ACEs and decrease substance use in early adulthood.
Inspection of individual ACEs revealed slightly different patterns, as not all adverse experiences had an equally strong association with substance use. Most studies reported that physical and emotional abuse was associated with increased substance use in young adults. Emotional abuse was more consistently associated with substance use, possibly due to its stronger association with subsequent psychological distress; substances such as alcohol are impulsively chosen to soothe such distress.161,162,168 In addition, the influence of sexual abuse on drug and alcohol use was not consistent across studies. While some cohort studies supported this relationship,136,169 they either prospectively assessed ACEs during adolescence only or retrospectively assessed sexual abuse. Given that other prospective 119 and retrospective cohort studies 156 did not find a significant association between sexual abuse and substance use, caution is merited when considering this ACE as a predictor of substance use, and further investigation is needed. Currently, the impact of sexual abuse appears contingent on other variables, such as female sex.100,109 The authors suggest that this sex difference might be due to a higher likelihood of females experiencing this maltreatment and the tendency to respond with internalizing rather than externalizing behavior. Although there is no obvious factor that accounts for disparities in the influence of physical abuse, its association may be overshadowed by other ACEs, such as sexual and emotional abuse.171,174
Furthermore, it is essential to note that in 3 studies, experience of physical violence in childhood predicted less drug and alcohol use in early adulthood.161,169,170 These findings suggest that emotional aspects of childhood maltreatment have a more robust association with substance use than physical harm. A prospective cohort study by Newbury et al 126 showed that when analyzed independently, the association between emotional abuse (retrospectively assessed) and substance dependence was more robust than that between physical abuse and substance abuse. This suggests that individuals with ACEs might have more vivid memories of the emotional aspects of abuse. However, the same study showed that when assessed prospectively, emotional abuse, in contrast to physical abuse, was not associated with substance dependence. Consequently, the inconsistency in reports regarding the influence of physical abuse may be due to the reliance on primarily retrospective assessments of ACEs.
Compared to directed maltreatment, such as physical, emotional, and sexual abuse, indirect maltreatment, such as physical or emotional neglect, had more inconsistent associations with substance use. Although some studies found that childhood neglect was associated with substance use in young adults, this association was not always significant. Directed maltreatment, where the behavior is aimed at a child, may have a greater influence on substance use in early adulthood than indirect abuse in the form of neglect.
Similar to experiencing childhood maltreatment, exposure to family dysfunction had varying associations with substance use in young adults. Having a family member with substance use was most consistently associated with substance use in offspring. While some researchers suggested that this can be due to children recreating the behavioral patterns of their parents, 179 others pointed out that the resulting psychological distress mediates risky alcohol use. 168 Interestingly, while most studies reported that witnessing parental violence was associated with substance use due to induced distress and use of maladaptive coping mechanisms, 180 Villanueva and Gomis-Pomares 174 reported an inverse association, possibly due to the development of a stronger bond with the victimized parent. However, given that their study was the only study to report such an inverse relationship and that their study was cross-sectional (while Jester et al’s 180 was a cohort study), further investigation is needed. In addition, the consequences of having an incarcerated or mentally ill family member and having separated parents were generally inconsistent. Given the lack of studies on family dysfunction (regardless of maltreatment) that incorporated mediators, consensus on the impact of family dysfunction on substance abuse in early adulthood is lacking. This inconsistency may be because of individual traits of children lead to variation in stress experienced by witnessing family dysfunction. However, further research is needed to test this assumption.
Implications for future research
Although the literature indicates a robust association between exposure to ACEs and substance use in early adulthood, further research addressing the specifics of this association is needed. First, studies should specify the age at which ACEs were experienced, as such stratification would establish whether the slope of the dose‒response association between the ACEs and substance use in early adulthood differs depending on the time of first ACE. Moreover, as indicated by the inconsistent results regarding the associations of individual ACEs, future studies need to evaluate and compare the effects of different ACEs. As seen in the Results section, few studies investigated the associations of family dysfunction domains (eg, substance use in the family) with substance use in early adulthood, while several studies examined associations of maltreatment (eg, sexual abuse) with substance use in early adulthood. This highlights the importance of exploring all forms of ACEs.
One approach to address this is to focus on personal factors that can determine the extent of stress induced by ACEs. For instance, Oshri et al 128 reported that HRV reactivity moderated relationships of any ACE with delayed reward discounting and subsequent alcohol use. However, psychological factors such as perceived self-efficacy in dealing with stressors or the quality of parental relationships can also play a role. Additionally, given that early adulthood presents unique pressures, these pressures should be incorporated into models predicting substance use. Following the identification of relevant moderators, future studies should also focus on identifying mediators that explain the mechanisms through which exposure to ACEs increases the risk of using alcohol and drugs in early adulthood. Importantly, future investigation of mediators and moderators should not be restricted to risk factors. Identifying protective factors can provide a more holistic and accurate explanation of substance use in young adults.
Moreover, such research could inform the development of proactive (rather than reactive) substance use interventions. In addition to investigating mediators and moderators, it is also important to account for covariates, as highlighted by the fact that most high-quality studies included in this review considered covariates in their models. Consequently, it is recommended that future studies follow their example. The covariates most often included were sociodemographic characteristics of the participants, namely, age, sex, socioeconomic status, and race or ethnicity. While these factors are the minimally required confounders for models, studies have also included family income or standard of living during childhood, parental education levels, and depression. Finally, given the results of the present literature review showing that various ACEs are associated with substance abuse, it is also important to include all types of ACEs in the models.
Limitations
The current review has some limitations. Unfortunately, not all included studies used the same instruments to assess ACEs, and most relied on retrospective self-report data. Although caution is merited when interpreting the results, the association between ACEs and substance use in early adulthood was also reported by studies utilizing record inspection. This strengthens the findings of self-report-based studies and lends validity to the retrospective assessment of ACEs. Another limitation related to the use of retrospective assessments is the inclusion of cross-sectional studies alongside cohort studies. However, some cohort studies also employed retrospective ACE assessments. Furthermore, cross-sectional studies are an integral part of research, as they represent preliminary exploration of associations between variables that are then tested with more rigorous longitudinal or experimental designs. Additionally, as included studies were limited to those published in English, most of the data were obtained from countries with moderate to high socioeconomic levels. Given that socioeconomic status is an essential covariate in the association of ACEs with substance use105,109,133 and was even identified as a relevant mediator of this relationship,101,148 the results might differ in countries with lower socioeconomic levels. Although the 2 multinational studies found that exposure to ACEs was associated with the use of drugs or alcohol by young adults,5,6 studies in other countries would also allow us to investigate the impact of cultural norms on substance use by young adults. Another limitation of the present literature review is the use of a qualitative systematic review rather than a quantitative approach, such as meta-analysis, which would establish more robust association patterns between ACEs and substance use in early adulthood.
Furthermore, as the majority of the included studies relied on structured retrospective self-reports for the assessment of ACE exposure and unstructured self-report questions to establish alcohol use, the presented association between these 2 variables needs to be considered with caution. Furthermore, as the included studies were limited to those with participants aged 18 to 25 years, the findings of this study cannot be immediately applied to other age groups. This feature was designed to identify the impact of factors unique to young adults or TAY—however, only Forester et al 106 accounted for stressors specific to this population. As they found that the relationship between ACEs and substance use was moderated by these stressors, future studies should also account for such factors.
Conclusion
This review provides clear evidence that exposure to ACEs, especially multiple ACEs, is a strong predictor for increased use of alcohol, cannabis, and other drugs by young adults. However, ACEs represent only one risk factor among many. As this effect was amplified by poor self-regulation and maladaptive coping strategies, these factors may represent initial targets for interventions. Likewise, these variables represent stepping stones for future research aiming to map the specific pathways by which ACEs increase the risk of substance use in early adulthood. In addition to identifying risk factors for substance use in individuals with ACEs, future research should identify protective factors that can reduce or eliminate the impacts of previous adverse experiences and buffer against future stressors.
Footnotes
Author’s Note: Ivan Sebalo is also affiliated to Department of Psychiatry, Charles University and General University Hospital, Prague, Czechia.
Author Contributions: IS did the literature search, analysis of the results and the article write-up, MSV did the article write-up, RP did the design and literature search MA did the analysis of results and secured funding of the article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The publication of this article was funded by university grant : Cooperatio 207 038, research area: health sciences and neurosciences.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Referances
- 1. Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469-480. [PubMed] [Google Scholar]
- 2. Arnett JJ. The developmental context of substance use in emerging adulthood. J Drug Issues. 2005;35(2):235-254. [Google Scholar]
- 3. Arnett JJ, Žukauskienė R, Sugimura K. The new life stage of emerging adulthood at ages 18-29 years: implications for mental health. Lancet Psychiatry. 2014;1:569-576. [DOI] [PubMed] [Google Scholar]
- 4. Temmen CD, Crockett LJ. Relations of stress and drinking motives to young adult alcohol misuse: variations by gender. J Youth Adolesc. 2020;49(4):907-920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bellis MA, Hughes K, Leckenby N, et al. Adverse childhood experiences and associations with health-harming behaviours in young adults: surveys in eight eastern European countries. Bull World Health Organ. 2014;92:641-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hughes K, Bellis MA, Sethi D, et al. Adverse childhood experiences, childhood relationships and associated substance use and mental health in young Europeans. Eur J Public Health. 2019;29(4):741-747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am J Prev Med. 1998;14(4):245-258. [DOI] [PubMed] [Google Scholar]
- 8. Wade R, Cronholm PF, Fein JA, et al. Household and community-level adverse childhood experiences and adult health outcomes in a diverse urban population. Child Abuse Negl. 2016;52:135-145. [DOI] [PubMed] [Google Scholar]
- 9. Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br J Psychiatry. 2010;197:378-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cohrdes C, Mauz E. Self-efficacy and emotional stability buffer negative effects of adverse childhood experiences on young adult health-related quality of life. J Adolesc Heal Internet. 2020;67(1):93-100. [DOI] [PubMed] [Google Scholar]
- 11. Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:E356-E366. [DOI] [PubMed] [Google Scholar]
- 12. Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am J Prev Med. 2010;39(1):93-98. [DOI] [PubMed] [Google Scholar]
- 13. Alink LR, Cicchetti D, Kim J, Rogosch FA. Longitudinal associations among child maltreatment, social functioning, and cortisol regulation. Dev Psychol. 2012;48:224-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106(1):29-39. [DOI] [PubMed] [Google Scholar]
- 15. Trossman R, Spence S-L, Mielke JG, McAuley T. How do adverse childhood experiences impact health? Exploring the mediating role of executive functions. Psychol Trauma Theory Res Pract Policy. 2021;13:206-213. [DOI] [PubMed] [Google Scholar]
- 16. Gottesman Shields J, II. A polygenic theory of schizophrenia. Proc Natl Acad Sci USA. 1967;58:199-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychol Bull. 1991;110:406-425. [DOI] [PubMed] [Google Scholar]
- 18. Pasman JA, Verweij KJH, Vink JM. Systematic review of polygenic gene–environment interaction in tobacco, alcohol, and cannabis use. Behav Genet. 2019;49(4):349-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rioux C, Castellanos-Ryan N, Parent S, Vitaro F, Séguin JR. The interactive effects of parental knowledge with impulsivity and sensation seeking in adolescent substance use. Child Psychiatry Hum Dev. 2019;50(1):95-107. [DOI] [PubMed] [Google Scholar]
- 20. Lee K, Pang YC, Lee JAL, Melby JN. A study of adverse childhood experiences, coping strategies, work stress, and self-care in the child welfare profession. Hum Serv Organ Manage Leadersh Gov. 2017;41(4):389-402. [Google Scholar]
- 21. Sheffler JL, Piazza JR, Quinn JM, Sachs-Ericsson NJ, Stanley IH. Adverse childhood experiences and coping strategies: identifying pathways to resiliency in adulthood. Anxiety Stress Coping. 2019;32:594-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and Neglect: A systematic review and meta-analysis. PLoS Med. 2012;9:e1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bukstein OG. Challenges and gaps in understanding substance use problems in transitional age youth. Child Adolesc Psychiatr Clin N Am. 2017;26(2):253-269. [DOI] [PubMed] [Google Scholar]
- 24. Dariotis JK, Chen FR. Stress coping strategies as mediators: toward a better understanding of sexual, substance, and delinquent behavior-related risk-taking among transition-aged youth. Deviant Behav. 2022;43(4):397-414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rogers CJ, Pakdaman S, Forster M, et al. Effects of multiple adverse childhood experiences on substance use in young adults: a review of the literature. Drug Alcohol Depend. 2022;234:109407. [DOI] [PubMed] [Google Scholar]
- 26. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moola S, Munn Z, Tufanaru C, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. JBI; 2020:217-269. [Google Scholar]
- 28. Roy CA, Perry JC. Instruments for the assessment of childhood trauma in adults. J Nerv Ment Dis. 2004; 192(5): 343-351. [DOI] [PubMed] [Google Scholar]
- 29. Teicher MH, Parigger A. The “Maltreatment and Abuse Chronology of Exposure” (MACE) Scale for the retrospective assessment of abuse and neglect during development. PLOS One. 2015; 10(2): e0117423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and Neglect. Am J Psychiatr. 1994;151:1132-1136. [DOI] [PubMed] [Google Scholar]
- 31. Straus MA. Measuring intrafamily conflict and violence: the conflict tactics (CT) scales. J Marriage Fam. 1979;41(1):75. [Google Scholar]
- 32. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–ii. Addiction. 1993;88:791-804. [DOI] [PubMed] [Google Scholar]
- 33. Harrison PA, Fulkerson JA, Beebe TJ. DSM-IV substance use disorder criteria for adolescents: A critical examination based on a statewide school survey. Am J Psychiatry. 1998; 155(4): 486-492. [DOI] [PubMed] [Google Scholar]
- 34. World Health Organization. Adverse Childhood Experiences International Questionnaire (ACE-IQ); 2013. www.who.int. https://www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq)
- 35. Kubany ES, Leisen MB, Kaplan AS, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychol Assess. 2000; 12(2): 210-224. [DOI] [PubMed] [Google Scholar]
- 36. Sheehan D, Lecrubier Y, Sheehan K, et al. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998; 59: 22-33. [PubMed] [Google Scholar]
- 37. Finkelhor D, Hamby SL, Ormrod R, Turner H. The juvenile victimization questionnaire: Reliability, validity, and national norms. Child Abuse Negl. 2005; 29(4): 383-412. [DOI] [PubMed] [Google Scholar]
- 38. Janson S, Långberg B, Svensson B. Våld mot barn 2006-2007 – en nationell kartläggning [Violence against children – A national survey in Sweden 2006–2007]. Stiftelsen Allmänna Barnhuset och Karlstad universitet; 2007: 4. [Google Scholar]
- 39. May-Chahal C, Cawson P. Measuring child maltreatment in the United Kingdom: A study of the prevalence of child abuse and neglect. Child Abuse Negl. 2005; 29: 969-984. [DOI] [PubMed] [Google Scholar]
- 40. Parker G, Roussos J, Hadzi-Pavlovic D, et al. The development of a refined measure of dysfunctional parenting and assessment of its relevance in patients with affective disorders. Psychol Med. 1997; 27(5): 1193-1203. [DOI] [PubMed] [Google Scholar]
- 41. Barber BK. Parental psychological control: Revisiting a neglected construct. Child Dev. 1996; 67(6): 3296. [PubMed] [Google Scholar]
- 42. Busby DM, Holman TB, Taniguchi N. RELATE: Relationship evaluation of the individual, family, cultural, and couple contexts*. Family Relations. 2001; 50(4): 308-316. [Google Scholar]
- 43. Grych JH, Seid M, Fincham FD. Assessing marital conflict from the child’s perspective: The children’s perception of interparental conflict scale. Child Dev. 1992; 63(3): 558. [DOI] [PubMed] [Google Scholar]
- 44. Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977; 1(3): 385-401. [Google Scholar]
- 45. Robinson CC, Mandleco B, Olsen SF, Hart CH. The parenting styles and dimensions questionnaire (PSQD). In: Perlmutter BF, Touliatos J, Holden GW, eds. Handbook of Family Measurement Techniques. Vol. 3. Sage; 2001:319-321. [Google Scholar]
- 46. Umberson D, Williams K, Powers DA, et al. Stress in childhood and adulthood: effects on marital quality over time. J Marriage Fam. 2005; 67: 1332-1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Narayan AJ, Rivera LM, Bernstein RE, Harris WW, Lieberman AF. Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: A pilot study of the benevolent childhood experiences (BCEs) scale. Child Abuse Negl. 2018; 78: 19-30. [DOI] [PubMed] [Google Scholar]
- 48. Moberg DP, Hahn L. The adolescent drug involvement scale. J Child Adolesc Subst Abuse. 1991; 2(1): 75-88. [Google Scholar]
- 49. National Institute on Drug Abuse. Screening for Drug Use in General Medical Settings: Resource Guide; 2018. https://www.drugabuse.gov/sites/default/files/resource_guide.pdf
- 50. Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169-190. [DOI] [PubMed] [Google Scholar]
- 51. World Health Organization. Composite International Diagnostic Interview (CIDI). WHO; 1993. [Google Scholar]
- 52. World Health Organization. Adverse Childhood Experiences International Questionnaire (ACE-IQ); 2018. www.who.int. https://www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq)
- 53. World Health Organization. The ASSIST-linked brief intervention for hazardous and harmful substance use: A manual for use in primary care, 2010. https://apps.who.int/iris/bitstream/handle/10665/44321/9789241599399_eng.pdf?sequence=1
- 54. Smyth JM, Hockemeyer JR, Heron KE, Wonderlich SA, Pennebaker JW. Prevalence, type, disclosure, and severity of adverse life events in college students. J Am Coll Health. 2008; 57(1): 69-76. [DOI] [PubMed] [Google Scholar]
- 55. Selzer ML. The Michigan alcoholism screening test: The quest for a new diagnostic instrument. Am J Psychiatry. 1971; 127(12): 1653-1658. [DOI] [PubMed] [Google Scholar]
- 56. Centers for Disease Control and Prevention, N. C. for C. D. P. and H. P., Division of Population Health. BRFSS Prevalence & Trends Data, 2015. https://www.cdc.gov/brfss/brfssprevalence/
- 57. Kurdek LA. Differences between heterosexual-nonparent couples and gay, lesbian, and heterosexual-parent couples. J Fam Issues. 2001; 22(6): 727-754. [Google Scholar]
- 58. Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: National Survey Results on Drug Use, 1975–2006. Volume I: Secondary School Students (NIH Publication No. 07-6205). National Institute on Drug Abuse; 2007. http://monitoringthefuture.org/pubs/monographs/vol1_2006.pdf [Google Scholar]
- 59. Adlaf EM, Paglia-Boak A. Drug Use Among Ontario Students: 1977–2007 (CAMH Research Document, Series No. 21). Centre for Addiction and Mental Health; 2007. [Google Scholar]
- 60. Grant BF, Goldstein RB, Smith SM, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): Reliability of substance use and psychiatric disorder modules in a general population sample. Drug Alcohol Depend. 2015; 148: 27-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Perczek R, Carver CS, Price AA, Pozo-Kaderman C. Coping, mood, and aspects of personality in Spanish translation and evidence of convergence with English versions. J Pers Assess. 2000; 74(1): 63-87. [DOI] [PubMed] [Google Scholar]
- 62. Berman AH, Bergman H, Palmstierna T, Schlyter F. Evaluation of the drug use disorders identification test (DUDIT) in criminal justice and detoxification settings and in a Swedish Population Sample. Eur Addict Res. 2004; 11(1): 22-31. [DOI] [PubMed] [Google Scholar]
- 63. White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989;50(1):30-37. [DOI] [PubMed] [Google Scholar]
- 64. Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics. 2003; 111(3): 564-572. [DOI] [PubMed] [Google Scholar]
- 65. Sanders B, Becker-Lausen E. The measurement of psychological maltreatment: Early data on the child abuse and trauma scale. Child Abuse Negl. 1995; 19(3): 315-323. [DOI] [PubMed] [Google Scholar]
- 66. Dimeff LA, Baer JS, Kivlahan DR, Marlatt G. Brief Alcohol Screening and Intervention for College Students (BASICS): Aharm Reduction Approach. Guilford Press; 1999. [Google Scholar]
- 67. Sorenson SB, Stein JA, Siegel JM, Golding JM, Burnam MA. The prevalence of adult sexual assault: The Los Angeles Epidemiologic Catchment Area project. Am J Epidemiol. 1987; 126: 1154-1164. [DOI] [PubMed] [Google Scholar]
- 68. Zucker RA, Fitzgerald HE, Noll RB. Drinking and Drug History (Unpublished instrument). Michigan State University; 1990. [Google Scholar]
- 69. Skinner HA. The drug abuse screening test. Addict Behav. 1982; 7: 363-371. [DOI] [PubMed] [Google Scholar]
- 70. Dunne MP, Zolotor AJ, Runyan DK, et al. ISPCAN Child Abuse Screening Tools Retrospective version (ICAST-R): Delphi study and field testing in seven countries. Child Abuse Negl. 2009; 33: 815-825. [DOI] [PubMed] [Google Scholar]
- 71. Fink LA, Bernstein D, Handelsman L, Foote J, Lovejoy M. Initial reliability and validity of the childhood trauma interview: A new multidimensional measure of childhood interpersonal trauma. Am J Psychiatry. 1995; 152(9): 1329-1335. [DOI] [PubMed] [Google Scholar]
- 72. Christoffersen MN, Armour C, Lasgaard M, Andersen TE, Elklit A. The prevalence of four types of childhood maltreatment in Denmark. Clin Pract Epidemiol Ment Health. 2013; 9: 149-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. J Consult Clin Psychol. 1985; 53(2): 189-200. [DOI] [PubMed] [Google Scholar]
- 74. Read JP, Kahler CW, Strong DR, Colder CR. Development and preliminary validation of the Young Adult Alcohol Consequences Questionnaire. J Stud Alcohol. 2006; 67(1): 169-177. [DOI] [PubMed] [Google Scholar]
- 75. Johnson JH, McCutcheon SM. Assessing life stress in older children and adolescents: Preliminary findings with the Life Events Checklist. In: Sarason IG, Spielberger CD, eds. Stress and Anxiety. Hemisphere; 1980:111-125. [Google Scholar]
- 76. Green BL. Psychometric review of Trauma History Questionnaire (self-report). In: Stamm BH, Varra EM, eds. Measurement of Stress, Trauma and Adaptation. Sidran; 1996. [Google Scholar]
- 77. Sobell LC, Sobell MB. Timeline Followback User’s Guide: A Calendar Method for Assessing Alcohol and Drug Use. Addiction Research Foundation; 1996. [Google Scholar]
- 78. Stephens R, Roffman R, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000; 68: 898-908. [PubMed] [Google Scholar]
- 79. Koss MP, Gidycz CA. Sexual experiences survey: Reliability and validity. J Consult Clin Psychol. 1985; 53: 422-423. [DOI] [PubMed] [Google Scholar]
- 80. Cahalan D, Cisin IH, Crossley HM. American Drinking Practices: A National Study of Drinking Behavior and Attitudes. Rutgers Center of Alcohol Studies; 1969. [Google Scholar]
- 81. Fromme K, Katz EC, Rivet K. Outcome expectancies and risk-taking behavior. Cogn Ther Res. 1997; 21: 421-442. [Google Scholar]
- 82. Peters L, Andrews G. Procedural validity of the computerized version of the Composite International Diagnostic Interview (CIDI-Auto) in the anxiety disorders. Psychol Med. 1995; 25(6): 1269-1280. [DOI] [PubMed] [Google Scholar]
- 83. Robins L, Cottler L, Bucholz K, Comptom W. Diagnostic Interview Schedule for DSM-IV. Washington University in St. Louis; 1995. [Google Scholar]
- 84. Myers K. Comprehensive addiction severity index for adolescents. In: McClellan T, Dembo R, eds. Screening and Assessment of Alcohol-and Other Drug-Abusing Adolescents. Substance Abuse and Mental Health Services Administration; 1994. [Google Scholar]
- 85. Malamuth NM, Sockloskie RJ, Koss MP, Tanaka JS. Characteristics of aggressors against women: Testing a model using a national sample of college students. J Consult Clin Psychol. 1991; 59(5): 670-681. [DOI] [PubMed] [Google Scholar]
- 86. Harris KM, Halpern CT, Haberstick BC, Smolen A. The national longitudinal study of adolescent health (add health) sibling pairs data. Twin Res Hum Genet. 2013; 16(1): 391-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Forero Ariza LM, Avendaño Durán MC, Duarte Cubillos ZJ, Campo-Arias A. Consistencia interna y análisis de factores de la escala APGAR para evaluar el funcionamiento familiar en estudiantes de básica secundaria. Revista Colombiana de Psiquiatría 2006; 35(1): 23-29. [Google Scholar]
- 88. Hibell B, Guttormsson U, Ahlström S, et al. The 2011 ESPAD Report. Substance Use Among Students in 36 European Countries. The Swedish Council for Information on Alcohol and other Drugs, 2013. [Google Scholar]
- 89. McLellan AT, Luborsky L, O’brien CP, Woody GE. An improved evaluation instrument for substance abuse patients: The Addiction Severity Index. J Nerv Ment Dis 1980; 168: 26-33. [DOI] [PubMed] [Google Scholar]
- 90. Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychol Assess. 1997; 9(4): 445. [Google Scholar]
- 91. Barnett D, Manly JT, Cicchetti D. Defining child maltreatment: The interface between policy and research. In: Cicchetti D, Toth SL, eds. Child Abuse, Child Development, and Social Policy. Ablex; 1993:7-73. [Google Scholar]
- 92. Hamby SL, Finkelhor D, Ormrod RK, Turner HA. The Comprehensive Juvenile Victimization Questionnaire. University of New Hampshire; 2004. [Google Scholar]
- 93. Tomoda A, Sheu YS, Rabi K, et al. Exposure to parental verbal abuse is associated with increased gray matter volume in superior temporal gyrus. NeuroImage. 2011; 54(Suppl. 1): S280-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Cottler LB, Robins LN, Grant BF, et al. The CIDI-core substance abuse and dependence questions: Cross-cultural and nosological issues. The WHO/ADAMHA Field Trial. Br J Psychiatry. 159; 1991: 653-658. [DOI] [PubMed] [Google Scholar]
- 95. Cicchetti D, Barnett D. Toward the development of a scientific nosology of child maltreatment. In: Cicchetti D, Grover W, eds. Thinking Clearly About Psychology: Essays in Honor of Paul E. Meehl: Personality and Psychopathology. Vol. 2. University of Minnesota Press; 1991:346-377. [Google Scholar]
- 96. Freedman D, Thornton A, Camburn D, Alwin D, Young-DeMarco L. The life history calendar: A technique for collecting retrospective data. In: Clogg CC, ed. Sociological Methodology. Institute for Social Research, University of Michigan; 1988:37-68. [PubMed] [Google Scholar]
- 97. Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): A critical review. J Psychiatr Res. 1994; 28(1): 57-84. [DOI] [PubMed] [Google Scholar]
- 98. Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000; 68(5): 898-908. [PubMed] [Google Scholar]
- 99. Crandall A, Broadbent E, Stanfill M, et al. The influence of adverse and advantageous childhood experiences during adolescence on young adult health. Child Abuse Negl. 2020;108: 104644. [DOI] [PubMed] [Google Scholar]
- 100. Cronin S, Murphy S, Elklit A. Investigating the relationship between childhood maltreatment and alcohol misuse in a sample of Danish young adults: exploring gender differences. Nord Stud Alcohol Drugs. 2016;33:287-298. [Google Scholar]
- 101. Davis JP, Tucker JS, Stein BD, D’Amico EJ. Longitudinal effects of adverse childhood experiences on substance use transition patterns during young adulthood. Child Abuse Negl. 2021;120:105201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Dawson-Rose C, Shehadeh D, Hao J, et al. Trauma, substance use, and mental health symptoms in transitional age youth experiencing homelessness. Public Health Nurs. 2020;37:363-370. [DOI] [PubMed] [Google Scholar]
- 103. Dube SR, Miller JW, Brown DW, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006;38(4):e1444.e1-10444.e10. [DOI] [PubMed] [Google Scholar]
- 104. Ferguson KM, Bender K, Thompson SJ. Predicting illegal income generation among homeless male and female young adults: understanding strains and responses to strains. Child Youth Serv Rev. 2016;63:101-109. [Google Scholar]
- 105. Fernandes GS, Spiers A, Vaidya N, et al. Adverse childhood experiences and substance misuse in young people in India: results from the multisite cVEDA cohort. BMC Public Health. 2021;21:1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Filipkowski KB, Heron KE, Smyth JM. Early adverse experiences and health: the transition to college. Am J Health Behav. 2016;40:717-728. [DOI] [PubMed] [Google Scholar]
- 107. Forster M, Vetrone S, Grigsby TJ, Rogers C, Unger JB. The relationships between emerging adult transition themes, adverse childhood experiences, and substance use patterns among a community cohort of Hispanics. Cult Divers Ethn Minor Psychol. 2020;26:378-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Friedman JK, Santaularia NJ, Dadi D, Erickson DJ, Lust K, Mason SM. The influence of childhood and early adult adversities on substance use behaviours in racial/ethnically diverse young adult women: a latent class analysis. Int J Inj Contr Saf Promot. 2022;29(1):3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Abajobir AA, Kisely S, Williams G, Clavarino A, Strathearn L, Najman JM. Gender-based differences in injecting drug use by young adults who experienced maltreatment in childhood: findings from an Australian birth cohort study. Drug Alcohol Depend. 2017;173(3):163-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Giovanelli A, Reynolds AJ, Mondi CF, Ou SR. Adverse childhood experiences and adult well-being in a low-income, urban cohort. Pediatrics. 2016;137(4):e20154016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Goings TC, Yu T, Brody GH. Contextual risks and psychosocial outcomes among rural African American emerging adults: a latent profile analysis. Dev Psychopathol. 2022;34:395-407. [DOI] [PubMed] [Google Scholar]
- 112. Goldstein AL, Henriksen CA, Davidov DM, Kimber M, Pitre NY, Afifi TO. Childhood maltreatment, alcohol use disorders, and treatment utilization in a national sample of emerging adults. J Stud Alcohol Drugs. 2013;74(2):185-194. [DOI] [PubMed] [Google Scholar]
- 113. Hahn AM, Simons RM, Simons JS. Childhood maltreatment and sexual risk taking: the mediating role of alexithymia. Arch Sex Behav. 2016;45(1):53-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Kalpidou MM, Volungis AM, Bates C. Mediators between adversity and well-being of college students. J Adult Dev. 2021;28(4):286-298. [Google Scholar]
- 115. Kappel RH, Livingston MD, Patel SN, Villaveces A, Massetti GM. Prevalence of Adverse Childhood Experiences (ACEs) and associated health risks and risk behaviors among young women and men in Honduras. Child Abuse Negl. 2021;115:104993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Klein H, Elifson KW, Sterk CE. Young adult ecstasy users’ enhancement of the effects of their ecstasy use. J Psychoactive Drugs. 2009;41:113-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Kogan SM, Bae D, Cho J, Smith AK, Nishitani S. Pathways linking adverse environments to emerging adults’ substance abuse and depressive symptoms: a prospective analysis of rural African American men. Dev Psychopathol. 2021;33:1496-1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Liu S, Oshri A, Duprey EB. Heart rate variability reactivity moderates the indirect link between child maltreatment and young adult alcohol use problems via depressive symptoms. Am J Addict. 2020;29:141-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Loxton D, Forder PM, Cavenagh D, et al. The impact of adverse childhood experiences on the health and health behaviors of young Australian women. Child Abuse Negl. 2021;111:104771. [DOI] [PubMed] [Google Scholar]
- 120. Abajobir AA, Najman JM, Williams G, Strathearn L, Clavarino A, Kisely S. Substantiated childhood maltreatment and young adulthood cannabis use disorders: a pre-birth cohort study. Psychiatry Res. 2017;256:21-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Marks LR, Acuff SF, Withers AJ, MacKillop J, Murphy JG. Adverse childhood experiences, racial microaggressions, and alcohol misuse in Black and White emerging adults. Psychol Addict Behav. 2021;35:274-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the US. Child Abuse Negl. 2013;37(11):917-925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Mills R, Kisely S, Alati R, Strathearn L, Najman JM. Child maltreatment and cannabis use in young adulthood: a birth cohort study. Addiction. 2017;112:494-501. [DOI] [PubMed] [Google Scholar]
- 124. Musa S, Peek-Asa C, Jovanović N, Selimović E. Association of adverse childhood experiences and health risk behaviors among young adults visiting a regional primary healthcare center, Federation of Bosnia and Herzegovina. PLoS One. 2018;13:e0194439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Narendorf SC, Bowen E, Santa Maria D, Thibaudeau E. Risk and resilience among young adults experiencing homelessness: a typology for service planning. Child Youth Serv Rev. 2018;86:157-165. [Google Scholar]
- 126. Newbury JB, Arseneault L, Moffitt TE, et al. Measuring childhood maltreatment to predict early-adult psychopathology: comparison of prospective informant-reports and retrospective self-reports. J Psychiatr Res. 2018;96:57-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Oshri A, Carlson MW, Bord S, Zeichner A. Alcohol-impaired driving: the influence of adverse rearing environments, alcohol, cannabis use, and the moderating role of anxiety. Subst Use Misuse. 2017;52(4):507-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Oshri A, Liu S, Duprey EB, MacKillop J. Child maltreatment, delayed reward discounting, and alcohol and other drug use problems: the moderating role of heart rate variability. Alcohol Clin Exp Res. 2018;42:2033-2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Richardson GA, De Genna NM, Goldschmidt L, Larkby C, Donovan JE. Prenatal cocaine exposure: direct and indirect associations with 21-year-old offspring substance use and behavior problems. Drug Alcohol Depend. 2019;195:121-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Rollins EM, Crandall A. Self-regulation and shame as mediators between childhood experiences and young adult health. Front Psychiatry. 2021;12:649911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Allem J-P, Soto DW, Baezconde-Garbanati L, Unger JB. Adverse childhood experiences and substance use among Hispanic emerging adults in Southern California. Addict Behav. 2015;50:199-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Russotti J, Warmingham JM, Duprey EB, et al. Child maltreatment and the development of psychopathology: the role of developmental timing and chronicity. Child Abuse Negl. 2021;120:105215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Shin SH, McDonald SE, Conley D. Patterns of adverse childhood experiences and substance use among young adults: a latent class analysis. Addict Behav. 2018;78:187-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Shin SH, McDonald SE, Conley D. Profiles of adverse childhood experiences and impulsivity. Child Abuse Negl. 2018;85:118-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Shin SH, Wang X, Yoon SH, Cage JL, Kobulsky JM, Montemayor BN. Childhood maltreatment and alcohol-related problems in young adulthood: the protective role of parental warmth. Child Abuse Negl. 2019;98:104238. [DOI] [PubMed] [Google Scholar]
- 136. Smith CA, Ireland TO, Thornberry TP. Adolescent maltreatment and its impact on young adult antisocial behavior. Child Abuse Negl. 2005;29(10):1099-1119. [DOI] [PubMed] [Google Scholar]
- 137. Taşören AB. Drug Use and self-harming behavior among incarcerated men: does childhood abuse, anger, and executive function make a difference? J Aggress Maltreat Trauma. 2017;26(9):1006-1023. [Google Scholar]
- 138. Turner RJ, Lloyd DA. Cumulative adversity and drug dependence in young adults: racial/ethnic contrasts. Addiction. 2003;98:305-315. [DOI] [PubMed] [Google Scholar]
- 139. Vilhena-Churchill N, Goldstein AL. Child maltreatment and marijuana problems in young adults: examining the role of motives and emotion dysregulation. Child Abuse Negl. 2014;38(5):962-972. [DOI] [PubMed] [Google Scholar]
- 140. Villamil Grest C, Cederbaum JA, Lee JO, Unger JB. Adverse childhood experiences and the substance use behaviors of Latinx youth. Drug Alcohol Depend. 2021;227:108936. [DOI] [PubMed] [Google Scholar]
- 141. Wardell JD, Strang NM, Hendershot CS. Negative urgency mediates the relationship between childhood maltreatment and problems with alcohol and cannabis in late adolescence. Addict Behav. 2016;56:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Anderson CM, Rabi K, Lukas SE, Teicher MH. Cerebellar lingula size and experiential risk factors associated with high levels of alcohol and drug use in young adults. Cerebellum. 2010;9:198-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Windle M, Haardörfer R, Getachew B, et al. A multivariate analysis of adverse childhood experiences and health behaviors and outcomes among college students. J Am Coll Health. 2018;66:246-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Wymbs BT, Dawson AE, Suhr JA, Bunford N, Gidycz CA. ADHD symptoms as risk factors for intimate partner violence perpetration and victimization. J Interpers Violence. 2017;32(5):659-681. [DOI] [PubMed] [Google Scholar]
- 145. Baranger DA, Ifrah C, Prather AA, et al. PER1 rs3027172 genotype interacts with early life stress to predict problematic alcohol use, but not reward-related ventral striatum activity. Front Psychol. 2016;7:464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Barton AW, Kogan SM, Cho J, Brown GL. Father involvement and young, rural African American men’s engagement in substance misuse and multiple sexual partnerships. Am J Community Psychol. 2015;56(3–4):241-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Bender K, Brown SM, Thompson SJ, Ferguson KM, Langenderfer L. Multiple victimizations before and after leaving home associated with PTSD, depression, and substance use disorder among homeless youth. Child Maltreat. 2015;20(2):115-124. [DOI] [PubMed] [Google Scholar]
- 148. Cho J, Kogan SM. Risk and protective processes predicting rural African American young men’s substance abuse. Am J Community Psychol. 2016;58(3–4):422-433. [DOI] [PubMed] [Google Scholar]
- 149. Goldstein AL, Faulkner B, Wekerle C. The relationship among internal resilience, smoking, alcohol use, and depression symptoms in emerging adults transitioning out of child welfare. Child Abuse Negl. 2013;37(1):22-32. [DOI] [PubMed] [Google Scholar]
- 150. Messman-Moore TL, Ward RM, Brown AL. Substance use and PTSD symptoms impact the likelihood of rape and revictimization in college women. J Interpers Violence. 2009;24(3):499-521. [DOI] [PubMed] [Google Scholar]
- 151. Lagdon S, Ross J, Robinson M, Contractor AA, Charak R, Armour C. Assessing the mediating role of social support in childhood maltreatment and psychopathology among college students in Northern Ireland. J Interpers Violence. 2021;36:n2112-n2136. [DOI] [PubMed] [Google Scholar]
- 152. Exner-Cortens D, Eckenrode J, Rothman E. Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics. 2013;131:71-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Shin SH, Jiskrova GK, Yoon SH, Kobulsky JM. Childhood maltreatment, motives to drink and alcohol-related problems in young adulthood. Child Abuse Negl. 2020;108:104657. [DOI] [PubMed] [Google Scholar]
- 154. Kerr T, Stoltz J-A, Marshall BDL, Lai C, Strathdee SA, Wood E. Childhood trauma and injection drug use among high-risk youth. J Adolesc Health. 2009;45(3):300-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Oshri A, Kogan SM, Kwon JA, et al. Impulsivity as a mechanism linking child abuse and neglect with substance use in adolescence and adulthood. Dev Psychopathol. 2018;30:417-435. [DOI] [PubMed] [Google Scholar]
- 156. DeBeck K, Kerr T, Marshall BDL, Simo A, Montaner J, Wood E. Risk factors for progression to regular injection drug use among street-involved youth in a Canadian setting. Drug Alcohol Depend. 2013;133(2):468-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Rougemont-Bücking A, Grazioli VS, Daeppen JB, Gmel G, Studer J. Family-related stress versus external stressors: differential impacts on alcohol and illicit drug use in young men. Eur Addict Res. 2017;23:284-297. [DOI] [PubMed] [Google Scholar]
- 158. Fusco RA. Frequent marijuana or alcohol use in low-income emerging adults: impact of adverse life experiences. Subst use misuse. 2021;56:711-717. [DOI] [PubMed] [Google Scholar]
- 159. Lo CC, Cheng TC. The impact of childhood maltreatment on young adults’ substance abuse. Am J Drug Alcohol Abuse. 2007;33:139-146. [DOI] [PubMed] [Google Scholar]
- 160. Meshesha LZ, Abrantes AM, Anderson BJ, Blevins CE, Caviness CM, Stein MD. Marijuana use motives mediate the association between experiences of childhood abuse and marijuana use outcomes among emerging adults. Addict Behav. 2019;93:166-172. [DOI] [PubMed] [Google Scholar]
- 161. Shin SH, Jiskrova GK, Wills TA. Childhood maltreatment and alcohol use in young adulthood: the role of self-regulation processes. Addict Behav. 2019;90:241-249. [DOI] [PubMed] [Google Scholar]
- 162. Shin SH, Lee S, Jeon S-M, Wills TA. Childhood emotional abuse, negative emotion-driven impulsivity, and alcohol use in young adulthood. Child Abuse Negl. 2015;50:94-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Young SY, Hansen CJ, Gibson RL, Ryan MA. Risky alcohol use, age at onset of drinking, and adverse childhood experiences in young men entering the US marine corps. Arch Pediatr Adolesc Med. 2006;160:1207-1214. [DOI] [PubMed] [Google Scholar]
- 164. Allen CD, Breshears DD, McDowell NG. On underestimation of global vulnerability to tree mortality and forest die-off from hotter drought in the Anthropocene. Ecosphere. 2015;6(8):art129. [Google Scholar]
- 165. Cater Å K, Andershed A-K, Andershed H. Youth victimization in Sweden: prevalence, characteristics and relation to mental health and behavioral problems in young adulthood. Child Abuse Negl. 2014;38(8):1290-1302. [DOI] [PubMed] [Google Scholar]
- 166. Grummitt LR, Kelly EV, Barrett EL, et al. Associations of childhood emotional and physical neglect with mental health and substance use in young adults. Aust N Z J Psychiatr. 2022;56(4):365-375. [DOI] [PubMed] [Google Scholar]
- 167. Shin SH, Chung Y, Rosenberg RD. Identifying sensitive periods for alcohol use: the roles of timing and chronicity of child physical abuse. Alcohol Clin Exp Res. 2016;40(5):1020-1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Shin SH, Hassamal S, Groves LP. Examining the role of psychological distress in linking childhood maltreatment and alcohol use in young adulthood. Am J Addict. 2015;24(7):628-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Narendorf SC, McMillen JC. Substance use and substance use disorders as foster youth transition to adulthood. Child Youth Serv Rev. 2010;32(1):113-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Saadatmand F, Dearfield C, Bronson J, Harrison R. Exposure to personal and community violence and associated drug use outcomes in African American young adults. J Ethn Subst Abuse. 2022;21(2):708-729. [DOI] [PubMed] [Google Scholar]
- 171. Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse Negl. 2008;32:607-619. [DOI] [PubMed] [Google Scholar]
- 172. Konings M, Stefanis N, Kuepper R, et al. Replication in two independent population-based samples that childhood maltreatment and cannabis use synergistically impact on psychosis risk. Psychol Med. 2012;42(1):149-159. [DOI] [PubMed] [Google Scholar]
- 173. Murase H, Simons RM, Simons JS. Distinct paths to alcohol problems: impacts of childhood maltreatment, attachment insecurity, and interpersonal problems. Addict Behav. 2021;115:106780. [DOI] [PubMed] [Google Scholar]
- 174. Villanueva L, Gomis-Pomares A. The cumulative and differential relation of adverse childhood experiences and substance use during emerging adulthood. Child Psychiatry Hum Dev. 2021;52:420-429. [DOI] [PubMed] [Google Scholar]
- 175. Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, O’Callaghan MJ, Williams GM. Childhood sexual abuse and cannabis use in early adulthood: findings from an Australian birth cohort study. Arch Sex Behav. 2009;38:135-142. [DOI] [PubMed] [Google Scholar]
- 176. Messman-Moore TL, Ward RM, Zerubavel N. The role of substance use and emotion dysregulation in predicting risk for incapacitated sexual revictimization in women: Results of a prospective investigation. Psychol Addict Behav. 2013;27(1):125-132. [DOI] [PubMed] [Google Scholar]
- 177. Lo LY, Cheng MY. A quick eye to anger: an investigation of a differential effect of facial features in detecting angry and happy expressions. Int J Psychol. 2017;52:171-179. [DOI] [PubMed] [Google Scholar]
- 178. Pereira-Morales AJ, Adan A, Camargo A, Forero DA. Substance use and suicide risk in a sample of young Colombian adults: an exploration of psychosocial factors. Am J Addict. 2017;26:388-394. [DOI] [PubMed] [Google Scholar]
- 179. Gomis-Pomares A, Villanueva L, Prado-Gascó V. Does it run in the family? Intergenerational transmission of household dysfunctions. Child Adolesc Social Work J. 2023;40:419-432. [Google Scholar]
- 180. Jester JM, Steinberg DB, Heitzeg MM, Zucker RA. Coping expectancies, not enhancement expectancies, mediate trauma experience effects on problem alcohol use: A prospective study from early childhood to adolescence. J Stud Alcohol Drugs. 2015;76:781-789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Smith CA, Elwyn LJ, Ireland TO, Thornberry TP. Impact of adolescent exposure to intimate partner violence on substance use in early adulthood. J Stud Alcohol Drugs. 2010;71:219-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Grigsby TJ, Forster M, Davis L, Unger JB. Substance use outcomes for Hispanic emerging adults exposed to incarceration of a household member during childhood. J Ethn Subst Abuse. 2020;19(3):358-370. [DOI] [PMC free article] [PubMed] [Google Scholar]