Stromal pancreatic neoplasms are extremely rare, perhaps due to the poor representation of this tissue in the normal parenchyma.[1] Although leiomyosarcoma is the most common primary malignant mesenchymal pancreatic tumor, it represents only 0.1% of malignant pancreatic tumors and 0.5% of all adult soft tissue sarcomas.[2] This neoplasm mainly affects females (70%–80%), occurs predominantly between the fifth and sixth decades of life, and has significant metastatic potential with poor prognosis.[3,4]
We present a case of an 83-year-old woman referred to our center for dysgeusia and weight loss. In the diagnostic workup, an abdominal computed tomographic scan was performed in December 2021; a 28-mm-diameter mass in the pancreatic body, with sharp margin and bulging on the splenic vein, was found. Successively an abdominal magnetic resonance imaging described a nodular lesion at the passage between body and tail hyperintense in diffusion-weighted imaging (DWI), hypointense in T1, and isointense in T2 sequences. Contrast enhancement was slight and progressive, and all the features were not typical for adenocarcinoma. Biochemical analysis and oncological markers were all within the reference range, except chromogranin A (402 ng/mL, upper normal value <98 ng/mL). Because of this positivity, a PET-Ga-68-DOTATOC positron emission tomography (PET)/ computerized tomography (CT) was prescribed in February 2022, which demonstrates an abnormal tracer uptake in the pancreatic tail. To characterize the mass, EUS with fine needle aspiration was performed in April 2022. At the passage body-tail, we confirmed a solid mass, of 31.5 mm × 25.7 mm in diameter, inhomogeneous, hypoechoic, with hyperechoic strand, and a high stiffness at the sonoelastography. The lesion had an exophytic profile along the posterior pancreatic margin, in straight contact with splenic vessels, without infiltration signs. Fine needle aspiration tissue acquisition was performed with Echo-3 22G needle; we performed 3 passes with aspiration technique [Video 1]. Cytological samples [Figure 1] and immunohistochemical tests [Figure 2] suggested a malignant mesenchymal neoplasm with muscle differentiation. The patient underwent a distal pancreatectomy. A macroscopic examination revealed the presence of a retropancreatic grayish white mass with a whorled appearance with a maximum diameter of 4 cm in close relationship with a large blood vessel and with well-circumscribed borders. Histological examination [Figures 3 and 4] and the immunophenotypic profile agree with the diagnosis of leiomyosarcoma (grade 2 sec. Fédération Nationale des Centres de Lutte Contre le Cancer [FNCLCC] grading system). No residual disease on oncological follow-up after 9 months was observed.
Figure 1.
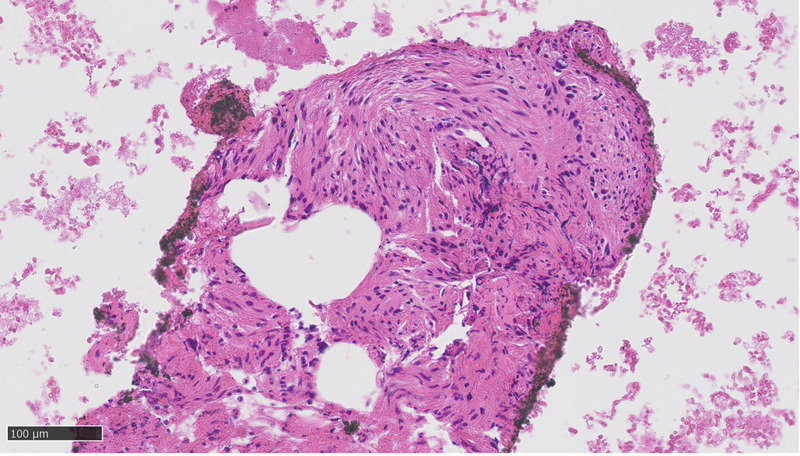
Cytological sample showed spindle cells proliferation with elongated, cigar-shaped and blunt-ended nuclei with severe atypia, variable pleomorphism, and fascicular grown pattern.
Figure 2.
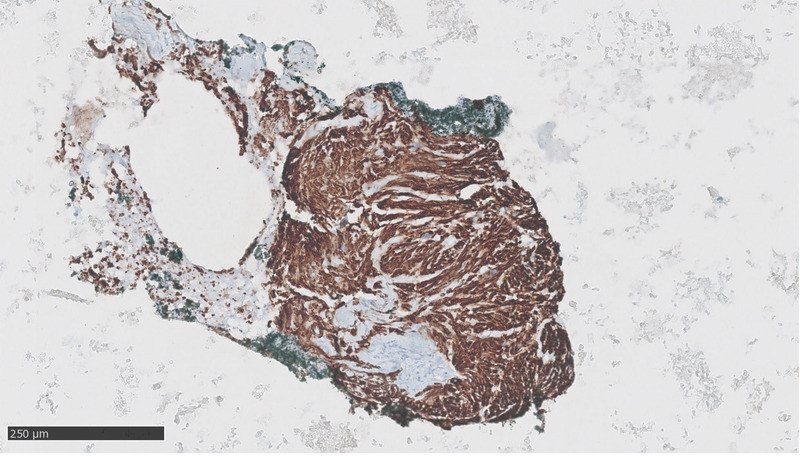
Immunohistochemical tests revealed these cells to be diffusely positive for desmin, focally positive for smooth muscle actin, and negative for CD117, DOG1, cytokeratin AE1–3, and S100. MIB1 antibody for Ki67 highlighted a proliferation rate of 10%.
Figure 3.
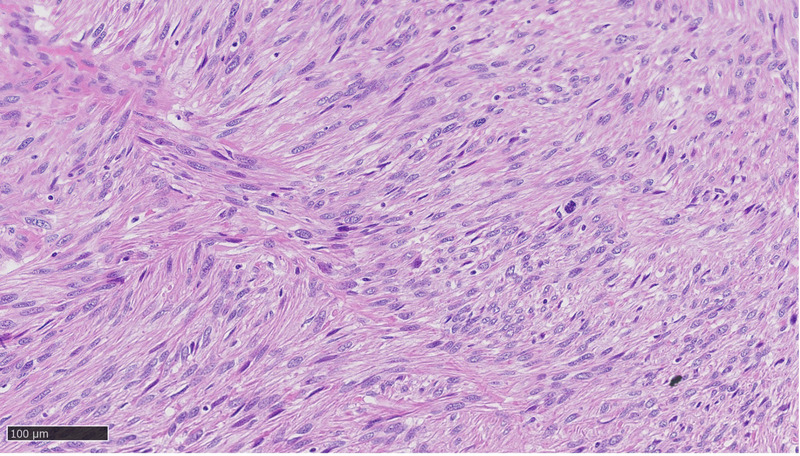
Histological examination of the neoplasm showed spindle-shaped cells with plump, blunt-ended nuclei, fields of nuclear pleomorphism, and distinctly eosinophilic fibrillary cytoplasm. Mitotic figures were common, including atypical ones. The cells merged with blood vessel's wall and were set in long intersecting fascicles. Hyalinized hypocellular areas and tumor necrosis were focally present.
Figure 4.
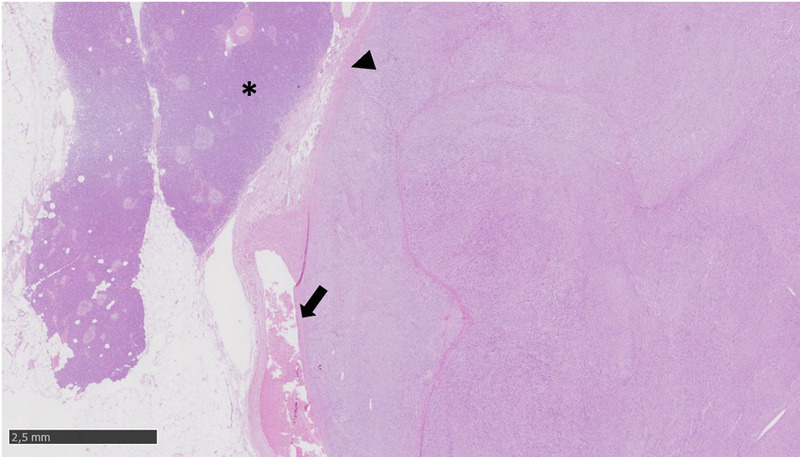
At low magnification, the tumor merges with the blood vessel's wall (arrow), and the tumor borders appear well circumscribed (arrowhead) without invasion of pancreatic parenchyma (*).
Video Legend.
Videos are only available at the official website of the journal (http://www.eusjournal.com).
Footnotes
Supplemental digital content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s Web site (www.eusjournal.com).
C.G. De Angelis and S. Gaia share the co-senior authorship.
Published online: 23 October 2023
Contributor Information
Noemi Sara Bertetti, Email: marcantonio.gesualdo@gmail.com.
Umberto Mortara, Email: marcantonio.gesualdo@gmail.com.
Francesca Maletta, Email: marcantonio.gesualdo@gmail.com.
Francesco Moro, Email: marcantonio.gesualdo@gmail.com.
Marco Sacco, Email: marcantonio.gesualdo@gmail.com.
Mauro Bruno, Email: marcantonio.gesualdo@gmail.com.
Claudio Giovanni De Angelis, Email: marcantonio.gesualdo@gmail.com.
Silvia Gaia, Email: marcantonio.gesualdo@gmail.com.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent. In the form, the patient's guardians have given their consent for his images and other clinical information to be reported in the journal. The patient's guardians understand that his names and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
The authors declare no conflict of interest.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Marcantonio Gesualdo and Noemi Sara Bertetti. The first draft of the manuscript was written by Marcantonio Gesualdo, Silvia Gaia and Claudio Giovanni De Angelis and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- 1.Hébert-Magee S, Varadarajulu S, Frost AR, Ramesh J. Primary pancreatic leiomyosarcoma: a rare diagnosis obtained by EUS-FNA cytology. Gastrointest Endosc 2014;80(2):361–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fadaee N, Sefa T, Das A, Rajkomar K. Pancreatic leiomyosarcoma: a diagnostic challenge and literature review. BMJ Case Rep 2019;12(11):e231529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sweeney JT, Crabtree DK, Yassin R, Somogyi L. Metastatic uterine leiomyosarcoma involving the pancreas diagnosed by EUS with fine-needle aspiration. Gastrointest Endosc 2002;56(4):596–597. [DOI] [PubMed] [Google Scholar]
- 4.Miyajima S Takeda S Goda K, et al. Metastatic primary pulmonary leiomyosarcoma to the pancreas diagnosed by endoscopic ultrasound-guided fine-needle aspiration. Clin J Gastroenterol 2021;14(6):1779–1784. [DOI] [PubMed] [Google Scholar]


