Abstract
Introduction
Adverse drug events (ADEs) are a leading cause of unplanned hospital visits. We designed ActionADE, an online ADE reporting platform, and integrated it with PharmaNet, British Columbia’s (BC's) provincial medication dispensing system, to overcome identified barriers in ADE reporting and communicate ADEs to community pharmacies. Our objectives were to characterise ADEs reported in ActionADE, explore associations between patients’ age, sex and ADE characteristics, and estimate the re-dispensation rate of culprit medications in community pharmacies.
Methods
We conducted a prospective observational study of ADE reporting in four BC hospitals between April 1, 2020 and October 31, 2022. We described the characteristics of ADEs reported into ActionADE, used logistic regression modelling to examine associations between age and sex and ADE characteristics, and calculated rates of avoided culprit drug re-dispensations using community pharmacists’ responses to ActionADE alerts.
Results
In total, 3591 ADE reports were initiated by hospital clinicians, 3174 of which were included in this analysis. Serious or life-threatening ADEs resulting in permanent disability, hospitalisation, extended hospitalisation, and/or death accounted for 56.7% (1800/3174; 95% CI 55.0%–58.4%) of reports. Males were more likely to have non-adherence reported compared to females and experienced life threatening ADEs at a younger age than females. Of 591 patients who had ≥ 1 adverse drug reaction or allergy report (a subset of ADEs) transmitted to community pharmacies, 200 subsequently attempted to re-fill the culprit or a same class drug. Community pharmacists responded to preventative alerts by avoiding re-dispensation in 33.0% (66/200; 95% CI 26.5–39.5%).
Interpretation
ActionADE is the first interoperable system that communicates ADEs via a central medication database to community pharmacies. Every 10th ADE reported in ActionADE and shared to PharmaNet resulted in community pharmacists’ avoiding one culprit or same class drug re-exposure. Further research is needed to understand ActionADE’s impact on patient and health system outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40264-023-01348-7.
Key Points
| ActionADE is a novel adverse drug event reporting platform that is integrated with a central provincial drug dispensing database to enable communication with community pharmacists. |
| Reporting of known ADEs to older medications (e.g., hydrochlorothiazide) was common in ActionADE. |
| Among patients experiencing prescription drug-related harm, every tenth adverse drug event reported in ActionADE and shared with community pharmacies resulted in one avoided drug re-exposure. |
Introduction
Adverse drug events (ADEs) are unintended and harmful events associated with medications, and represent a major burden on patients and the health care system [1, 2]. They are a leading cause of unplanned emergency department (ED) visits and hospital admissions [3–5]. Between 8.2 and 12.0% of ED visits to Canadian acute care hospitals are ADE-related, 11.9 to 36.9% of which require admission; 32% of ADE-related ED visits are repeat events, of which 75% are preventable [3–7].
Preventable repeat ADEs occur because ADE information is rarely shared effectively within a patient’s circle of care [8]. Electronic medical record systems generally do not transmit ADE information between systems due to lack of uniform data standards and interoperability [9, 10]. As a result, serious ADEs leading to ED visits and hospital admissions are not automatically communicated to the medication’s prescriber or the dispensing community pharmacy. In a previous study, only 22% of ADE notifications were integrated into patient charts with re-exposures to culprit medications occurring in 27% of patients within six months of an ADE-related admission [8].
Voluntary reporting systems or websites such as Health Canada’s adverse drug reaction reporting form [11] were designed to enable documentation of ADEs for post-marketing surveillance. These systems are poorly suited to capture the complex nature of ADEs and are not integrated into electronic medical records or medication dispensing databases [12]. Adverse drug event reporting into stand-alone electronic systems or websites is time consuming for clinicians and does not result in a perceived benefit to the patient [12]. Despite ADE reporting being mandated in Canada through the Protecting Canadians from Unsafe Drugs Act (i.e., Vanessa’s Law) [13], clinicians often only document ADEs in hospital charts [14, 15]. As a result, existing systems like British Columbia Patient Safety and Learning System (BCPSLS), a web-based, free-text entry ADE reporting form that communicates events directly to Health Canada [16], are not protecting patients from re-exposures due to lack of interoperability or clinical utility.
We designed, piloted, and refined a web-based software application called ActionADE to address this gap in reporting. ActionADE allows health care providers to document ADEs in a rapid, user-friendly, and standardised manner at the bedside, and subsequently communicates the most relevant information to other systems [17–19]. ActionADE interoperates with PharmaNet, British Columbia’s (BC’s) central medication dispensation database, where ADE data are stored and automatically pushed to community pharmacy systems. When community pharmacists attempt to re-fill a prescription for a patient with an existing ADE record for the same or a same-class medication (subsequently called a culprit drug), a preventative alert appears. Pharmacists must respond to the alert in order to continue dispensing the medication.
Objectives
Our primary objective was to quantify the time needed to report and describe ADEs reported in ActionADE during the first two and a half years of its implementation. Secondary objectives were to explore patient sex- and age-based associations among reported ADEs, and to assess the rate of re-dispensations of culprit medication after sharing standardised ADE information via PharmaNet with community pharmacies.
We hypothesised that ADE reporting in ActionADE would require little time commitment, adverse drug reactions would comprise a large proportion of reports in ActionADE, patient sex and age would be associated with ADE types and outcomes, and that ADE reports would be used to inform community pharmacists’ re-dispensation decisions.
Methods
Design
This was a prospective observational cohort study in four hospitals in the Lower Mainland of BC, Canada between April 1, 2020 and October 31, 2022.
Setting
ActionADE is a web-based clinical ADE reporting application that was pilot-tested as a paper form at Vancouver General Hospital (VGH) in 2018, prior to its beta release in 2019 [17, 18]. We achieved integration of ActionADE with PharmaNet on December 7, 2020, after which completed ADE reports could be transmitted to PharmaNet [9, 20, 21]. We expanded ActionADE’s implementation to four hospitals (Vancouver General, Saint Paul’s, Lions Gate, and Richmond Hospitals), with implementation support focused on pharmacists working primarily in EDs and on medical wards, as they would be the most likely to see incoming patients with ADEs to outpatient medications. Our in-hospital implementation methods are described in detail elsewhere [22]. Community pharmacists received email communications about the intervention from their pharmacy software vendor, were able to access information on a website designed by the BC Ministry of Health, and had access to a continuing education webinar hosted by the BC Pharmacy Association [23, 24]. On May 3, 2021, we began a randomised controlled trial in which we transmitted adverse drug reaction and allergy reports (a subset of ADEs) to PharmaNet in the intervention group. At this time, we were able to determine the number of ActionADE alerts and rates of culprit medication re-dispensation in community pharmacies only for patients enrolled in the intervention group for this trial [20].
Participants
We included consecutive patients for whom practicing clinicians (i.e., hospital-based clinical pharmacists, physicians, or nurse practitioners) documented an ADE in ActionADE. There were no patient-level exclusions. We considered an ADE report complete if the clinician entered information on the culprit drug, ADE type, symptom/diagnosis, certainty, and outcome into ActionADE. We excluded duplicate or incomplete ADE reports and those marked as erroneous or where a clinician changed the ADE certainty to “Refute” after the initial report was made (e.g., after test results became available).
Data Collection and Variables
Clinical pharmacists, nurse practitioners and physicians reported ADEs into ActionADE during the process of clinical care provision. ActionADE automatically imported the patient’s name, age, biological sex at birth, and their 14-month PharmaNet medication dispensation history. Clinicians used these data to obtain a best possible medication history [25]. Clinicians then selected the suspected culprit drug(s) and entered ADE type, symptoms/diagnosis, certainty, and outcome using dropdown menus and/or predictive entry from standardised pick lists [9]. Clinicians were able to visualise definitions for the dropdown options when hovering over the term in the entry form (Appendix Table 1). Clinician diagnosed and entered ADE types including adverse drug reactions (ADRs), allergies, incorrect drugs, subtherapeutic dose, supratherapeutic dose, treatment failure, drug withdrawal, drug interaction, drug misuse, non-adherence, and other (e.g., drug-disease interactions, drug-food interactions, treatment without indication). Clinicians entered up to three symptoms and diagnoses relevant to the event from the MedDRA®1 Preferred Terms list, indicated their certainty as to whether the event was caused by the drug (Certain, Probable, Possible, Unlikely, Refute) and the most serious outcome of the event (listed here from least to most severe: Unknown, Other, Worsen Pre-existing Condition, Emergency Visit, Hospitalisation Extended, Hospitalisation, Permanent Disability, Life Threatening, Fetal Defect, Death). We defined serious events as those associated with fetal defect, permanent disability, hospitalisation or extended hospitalisation, life-threatening events, and/or those resulting in death.
When patients with ADE reports in ActionADE and PharmaNet went to a community pharmacy, the community pharmacist received an alert if the patient tried to fill a prescription for a culprit or same-class drug to which an ADE had been recorded. Community pharmacists could only continue with the dispensation by responding to the alert using pre-specified response codes. We accessed the community pharmacists’ response codes through Population Data BC, which provides researchers access to publicly funded community pharmacist interventions and medication dispensations [20, 26]. We considered all alerts that were overridden, as dispensed medications, and non-overridden alerts as non-dispensations.
Statistical Analyses
Where available, we used datetime stamps from the system from the beginning and end of data entry to assess the time it took clinicians to complete a report. We presented summary statistics on the top culprit drugs, ADE type, symptoms/diagnoses, certainty, and outcome by ADE seriousness. We highlighted common ADE types and symptoms/diagnoses for the most commonly reported culprit drugs by ADE seriousness. We calculated descriptive statistics for age and sex characteristics of patients in the cohort (e.g., means/standard deviations, median/interquartile range, or frequency & percentages) and examined associations between age and/or sex and ADE characteristics using regression models adjusted for clustering at the patient and hospital level. We entered age as a continuous variable into regression models, and multiplied effect sizes by 10 to create effect sizes per 10-year groupings. We calculated rates of attempted re-dispensations and avoided re-dispensations among patients with ADRs or allergies enrolled in the intervention group of a randomised control trial [20]. We considered a p value less than 0.05 as statistically significant. We suppressed cells with fewer than five patients or reports to ensure privacy and confidentiality.
Results
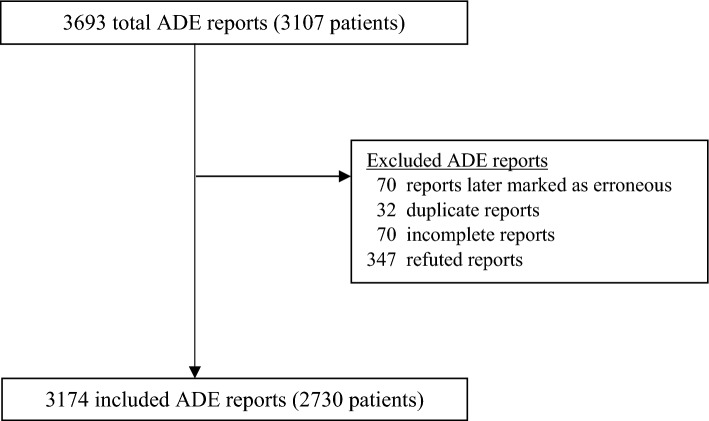
During the study period, 3591 ADE reports were initiated by clinicians, 347 of which were subsequently refuted, 70 marked as erroneous, 70 incomplete, and 32 duplicates, and were thus excluded (Fig. 1). The median time required for clinicians to complete an ADE report was 119 seconds (IQR 61–235 s) (data not shown).
Fig. 1.
Flow diagram of adverse drug event (ADE) patients and their events through the study
We included 3174 ADE reports which occurred in 2730 patients (Fig. 1). The average age of patients was 67 years and half were male. Most patients had only one report (87%), with a maximum of six reports (Table 1). Serious ADEs occurred in 58.2% of patients (1590/2730). Older patients were more likely to experience a serious ADE than younger patients (per 10 years; AOR = 1.13, 95% CI 1.09–1.18). Among the 3174 included ADE reports, the most common ADEs were ADRs (73.7%), non-adherence (11.3%), and allergies (7.8%; Table 2). The most commonly implicated culprit drugs included hydrochlorothiazide (3.8%), ramipril (3.6%), and furosemide (3.1%). The most commonly reported ADE manifestations were hyponatremia (7.0%), acute kidney injury (5.5%), and rashes (4.2%). Clinicians assigned a certainty level of probable or certain in almost three-quarters of the reported ADEs (72.2%; Table 2).
Table 1.
Descriptive statistics of included patients
| Patients with ≥ 1 complete ADE reports (N = 2730) | Patients with ≥ 1 serious ADE reportsa (N = 1590) | |
|---|---|---|
| Reports/patient, n (%) | ||
| 1 report | 2379 (87.1) | 1417 (89.1) |
| 2 reports | 285 (10.4) | 148 (9.3) |
| 3 reports | 46 (1.7) | 15 (0.9) |
| 4 reports | 14 (0.5) | Suppressed |
| ≥ 5 reports | 6 (0.2) | Suppressed |
| Mean patient age (SD) | 67.0 (19.5) | 69.1 (18.5) |
| Median patient age [IQR] | 71.0 [55.0, 82.0] | 73.0 [59.0, 83.0] |
| Male sex, n (%) | 1360 (49.8) | 822 (51.7) |
Cell sizes < 5 are suppressed
ADE adverse drug event, IQR interquartile range, SD standard deviation
aSerious ADEs are those with an outcome of fetal defect, permanent disability, hospitalisation, extended hospitalisation, life threatening, or death
Table 2.
Descriptive statistics of included ADE reports, by severity
| Overall (N = 3174) | Serious ADEsa (N = 1800) | |
|---|---|---|
| ADE types, n (%) | ||
| Adverse drug reactionb | 2340 (73.7) | 1362 (75.7) |
| Non-adherence | 357 (11.3) | 257 (14.3) |
| Allergyb | 249 (7.8) | 58 (3.2) |
| Supratherapeutic dose | 90 (2.8) | 52 (2.9) |
| Drug–drug interaction | 44 (1.4) | 22 (1.2) |
| Drug misuse | 28 (0.9) | 14 (0.8) |
| Subtherapeutic dose | 24 (0.8) | 11 (0.6) |
| Other (e.g., drug-disease interaction) | 14 (0.4) | 9 (0.5) |
| Treatment failure | 14 (0.4) | 9 (0.5) |
| Drug withdrawal | 10 (0.3) | Suppressed |
| Incorrect drug | Suppressed | Suppressed |
| Most common ADE drugs, n (%) | ||
| Hydrochlorothiazide | 120 (3.8) | 77 (4.3) |
| Ramipril | 113 (3.6) | 53 (2.9) |
| Apixaban | 99 (3.1) | 65 (3.6) |
| Furosemide | 99 (3.1) | 67 (3.7) |
| Acetylsalicylic acid | 95 (3.0) | 67 (3.7) |
| Warfarin | 88 (2.8) | 56 (3.1) |
| Rivaroxaban | 83 (2.6) | 47 (2.6) |
| Empagliflozin | 68 (2.1) | 58 (3.2) |
| Spironolactone | 66 (2.1) | 37 (2.1) |
| Sulfamethoxazole/trimethoprim | 58 (1.8) | 26 (1.4) |
| Most common ADE symptoms/diagnoses, n (%) | ||
| Hyponatremia | 223 (7.0) | 157 (8.7) |
| Acute kidney injury | 174 (5.5) | 126 (7.0) |
| Rash | 169 (5.3) | 36 (2.0) |
| Gastrointestinal hemorrhage | 127 (4.0) | 103 (5.7) |
| Hyperkalemia | 88 (2.8) | 45 (2.5) |
| Hypotension | 86 (2.7) | 51 (2.8) |
| Hypoglycemia | 83 (2.6) | 49 (2.7) |
| Bradycardia | 72 (2.3) | 43 (2.4) |
| Confusion | 71 (2.2) | 53 (2.9) |
| Nausea | 70 (2.2) | 26 (1.4) |
| ADE certainty, n (%) | ||
| Certain | 502 (15.8) | 291 (16.2) |
| Probable | 1791 (56.4) | 1081 (60.1) |
| Possible | 862 (27.2) | 419 (23.3) |
| Unlikely | 19 (0.6) | 9 (0.5) |
| Most serious ADE outcome reported, n (%) | ||
| Unknown | 249 (7.8) | 0 |
| Other (e.g., change in medication therapy) | 347 (10.9) | 0 |
| Worsened pre-existing condition | 84 (2.7) | 0 |
| Emergency visit | 694 (21.9) | 0 |
| Hospitalisation extended | 177 (5.6) | 177 (9.8) |
| Hospitalisation | 1393 (43.9) | 1393 (77.4) |
| Permanent disability | 10 (0.3) | 10 (0.6) |
| Life threatening | 211 (6.7) | 211 (11.7) |
| Fetal defect | 0 | 0 |
| Death | 9 (0.3) | 9 (0.5) |
ADE adverse drug event, ED emergency department, GP general practitioner
aSerious ADEs are those with an outcome of fetal defect, permanent disability, hospitalisation, extended hospitalisation, life threatening, or death
bOf the 2589 adverse drug reactions (ADRs) and allergies in the final cohort, 570 were not sent to PharmaNet because they were reported before the start of the randomised control trial and 606 reports were for drugs not eligible to be listed in PharmaNet (e.g., non-prescription drugs). Patients under 19 years old or with ADE outcomes of life threatening, fetal defect, or death were also excluded from the trial. 1129 patients with 1286 ADRs/allergies were included in the trial, of whom 538 patients with 648 ADRs/allergies were randomised to the control group where the ADR/allergy record was not sent to PharmaNet leaving 591 patients with 638 ADRs/allergy reports in PharmaNet as a part of the trial
Certain ADEs (i.e., common culprit drugs, types and symptoms) were reported more frequently than others (Tables 3, 4). Adverse drug reactions to hydrochlorothiazide resulting in hyponatremia represented 50.0% of all reports for hydrochlorothiazide (60/120) and 1.9% of reports overall (60/3174; Table 3). These reports were also the most common among the 1800 serious ADEs, where they represented 49.4% of all serious ADE reports to hydrochlorothiazide (38/77) and 2.1% of serious ADEs overall (38/1800; Table 4). Adverse drug reactions to empagliflozin were commonly reported and resulted in euglycemic diabetic ketoacidosis in 50.0% of empagliflozin reports (34/68), and 1.1% of the 3174 overall reports (34/3174; Table 3). These ADEs were common among serious ADEs, with 50.0% of serious ADEs to empagliflozin resulting in euglycemic diabetic ketoacidosis (1.6% of all serious ADEs; Table 4). Adverse drug reactions to chlorthalidone were less common (N = 43), but 65.4% (17/26) of all serious reports for chlorthalidone were ADRs resulting in hyponatremia, making up 0.9% of all serious ADEs (17/1800; Table 4).
Table 3.
Characteristics of the most commonly reported adverse drug events (n ≥ 5) among the top 10 most commonly reported culprit drugs
| Top 10 culprit drugs | ADE type(s) | Symptoms/diagnoses | Reports/drug, n (%) |
|---|---|---|---|
| Hydrochlorothiazide (n = 120) | Adverse Drug Reaction | Hyponatraemia | 60 (50.0) |
| Hypokalaemia | 10 (8.3) | ||
| Hypokalaemia and hyponatraemia | 8 (6.7) | ||
| Dizziness and hyponatraemia | 5 (4.2) | ||
| Ramipril (n = 113) | Adverse Drug Reaction | Angioedema | 20 (17.7) |
| Cough | 15 (13.3) | ||
| Acute kidney injury | 12 (10.6) | ||
| Hyperkalaemia | 9 (8.0) | ||
| Acute kidney injury and hyperkalaemia | 6 (5.3) | ||
| Hypotension | 6 (5.3) | ||
| Apixaban (n = 99) | Adverse Drug Reaction | Gastrointestinal haemorrhage | 14 (14.1) |
| Haematuria | 10 (10.1) | ||
| Epistaxis | 7 (7.1) | ||
| Chronic gastrointestinal bleeding | 5 (5.1) | ||
| Furosemide (n = 99) | Adverse Drug Reaction | Acute kidney injury | 11 (11.1) |
| Hyponatraemia | 6 (6.1) | ||
| Hypokalaemia | 5 (5.1) | ||
| Non-adherence | Cardiac failure congestive | 7 (7.1) | |
| Acetylsalicylic acid (n = 95) | Adverse Drug Reaction | Gastrointestinal haemorrhage | 28 (29.5) |
| Chronic gastrointestinal bleeding | 7 (7.4) | ||
| Haematuria | 5 (5.3) | ||
| Warfarin (n = 88) | Adverse Drug Reaction | Laboratory test abnormal | 8 (9.1) |
| Gastrointestinal haemorrhage | 7 (8.0) | ||
| Supratherapeutic Dose | International normalised ratio increased | 5 (5.7) | |
| Rivaroxaban (n = 83) | Adverse Drug Reaction | Gastrointestinal haemorrhage | 11 (13.3) |
| Epistaxis | 9 (10.8) | ||
| Haematuria | 7 (8.4) | ||
| Hemoptysis | 6 (7.2) | ||
| Lower gastrointestinal haemorrhage | 5 (6.0) | ||
| Empagliflozin (n = 68) | Adverse Drug Reaction | Euglycemic diabetic ketoacidosis | 34 (50.0) |
| Diabetic ketoacidosis | 12 (17.6) | ||
| Spironolactone (n = 66) | Adverse Drug Reaction | Hyperkalaemia | 15 (22.7) |
| Acute kidney injury and hyperkalaemia | 7 (10.6) | ||
| Sulfamethoxazole/trimethoprim (n = 58) | Adverse Drug Reaction | Hyperkalemia | 8 (13.8) |
| Rash | 6 (10.3) |
ADE adverse drug event
Table 4.
The most commonly reported ADEs (n ≥ 5) among 1590 patients with 1800 serious adverse drug events
| ADE culprit drugs | ADE type | Symptom/diagnosis | Report frequency, n | Proportion of reports/drug | Proportion of all reports (N = 1800) |
|---|---|---|---|---|---|
| Hydrochlorothiazide (n = 77) | Adverse Drug Reaction | Hyponatraemia | 38 | 49.4 | 2.1 |
| Hypokalemia & hyponatremia | 7 | 9.1 | 0.4 | ||
| Acetylsalicylic acid (n = 67) | Adverse Drug Reaction | Gastrointestinal hemorrhage | 25 | 37.3 | 1.4 |
| Chronic gastrointestinal bleeding | 6 | 9.0 | 0.3 | ||
| Furosemide (n = 67) | Adverse Drug Reaction | Acute kidney injury | 8 | 11.9 | 0.4 |
| Non-adherence | Cardiac failure congestive | 6 | 9.0 | 0.3 | |
| Apixaban (n = 65) | Adverse Drug Reaction | Gastrointestinal hemorrhage | 12 | 18.5 | 0.7 |
| Hematuria | 6 | 9.2 | 0.3 | ||
| Empagliflozin (n = 58) | Adverse Drug Reaction | Euglycemic diabetic ketoacidosis | 29 | 50.0 | 1.6 |
| Diabetic ketoacidosis | 12 | 20.7 | 0.7 | ||
| Warfarin (n = 56) | Adverse Drug Reaction | Gastrointestinal hemorrhage | 6 | 10.7 | 0.3 |
| Laboratory test abnormal | 5 | 8.9 | 0.3 | ||
| Ramipril (n = 53) | Adverse Drug Reaction | Acute kidney injury | 8 | 15.1 | 0.4 |
| Angioedema | 8 | 15.1 | 0.4 | ||
| Rivaroxaban (n = 47) | Adverse Drug Reaction | Gastrointestinal hemorrhage | 6 | 12.8 | 0.3 |
| Insulin glargine (n = 37) | Adverse Drug Reaction | Hypoglycemia | 7 | 18.9 | 0.4 |
| Non-adherence | Diabetic ketoacidosis | 8 | 21.6 | 0.4 | |
| Hyperglycemia | 5 | 13.5 | 0.3 | ||
| Spironolactone (n = 37) | Adverse Drug Reaction | Acute kidney injury & hyperkalemia | 6 | 16.2 | 0.3 |
| Metformin (n = 35) | Adverse Drug Reaction | Lactic acidosis | 11 | 31.4 | 0.6 |
| Candesartan cilexetil (n = 33) | Adverse Drug Reaction | Acute kidney injury | 7 | 21.2 | 0.4 |
| Hyperkalemia | 6 | 18.2 | 0.3 | ||
| Acute kidney injury & hyperkalemia | 5 | 15.2 | 0.3 | ||
| Ibuprofen (n = 32) | Adverse Drug Reaction | Gastrointestinal hemorrhage | 6 | 18.8 | 0.3 |
| Clopidogrel (n = 29) | Adverse Drug Reaction | Gastrointestinal hemorrhage | 6 | 20.7 | 0.3 |
| Naproxen (n = 29) | Adverse Drug Reaction | Gastrointestinal hemorrhage | 8 | 27.6 | 0.4 |
| Chlorthalidone (n = 26) | Adverse Drug Reaction | Hyponatraemia | 17 | 65.4 | 0.9 |
| Escitalopram (n = 23) | Adverse Drug Reaction | Hyponatraemia | 8 | 34.8 | 0.4 |
| Perindopril (n = 19) | Adverse Drug Reaction | Hyponatraemia | 7 | 36.8 | 0.4 |
| Pantoprazole (n = 17) | Adverse Drug Reaction | Gastrointestinal hemorrhage | 5 | 29.4 | 0.3 |
| Glyburide (n = 15) | Adverse Drug Reaction | Hypoglycemia | 10 | 66.7 | 0.6 |
| Gliclazide (n = 14) | Adverse Drug Reaction | Hypoglycemia | 8 | 57.1 | 0.4 |
| Aripiprazole (n = 13) | Non-adherence | Acute psychosis | 5 | 38.5 | 0.3 |
| Indapamide (n = 13) | Adverse Drug Reaction | Hyponatraemia | 6 | 46.2 | 0.3 |
| Cyclophosphamide (n = 8) | Adverse Drug Reaction | Febrile neutropenia | 5 | 62.5 | 0.3 |
| Empagliflozin/metformin (n = 6) | Adverse Drug Reaction | Euglycemic diabetic ketoacidosis | 6 | 100.0 | 0.3 |
| Doxorubicin (n = 5) | Adverse Drug Reaction | Febrile neutropenia | 5 | 100.0 | 0.3 |
ADE adverse drug event
Serious ADEs are those with an outcome of fetal defect, permanent disability, hospitalisation, extended hospitalisation, life threatening, or death
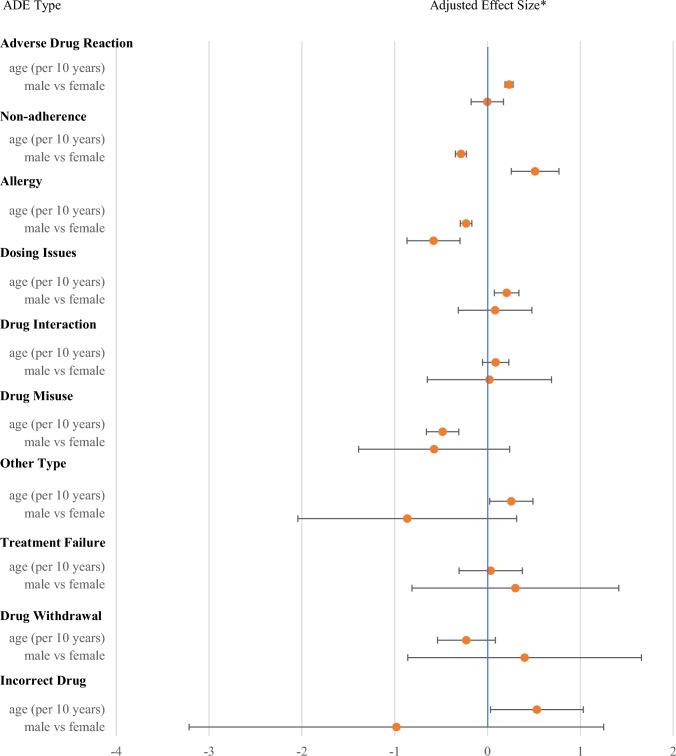
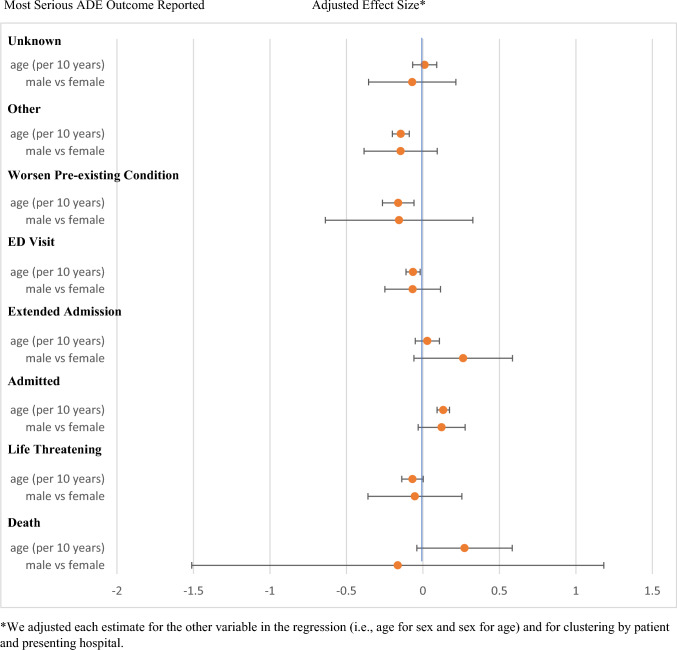
The types of ADEs reported varied by patient age, with drug misuse, allergies, and non-adherence being more commonly reported among younger patients, whereas dose-related ADEs, use of incorrect drugs, and ADRs were more common among older patients (Fig. 2). Younger patients were more likely to experience a worsening of a pre-existing condition, an emergency department visit, or a change in medication (i.e., “other”), whereas older patients were more likely to be hospitalised due to their ADE (Fig. 3). Males were more likely to report ADEs related to non-adherence, whereas females were more likely to have an allergy reported (Fig. 2).
Fig. 2.
Adjusted effects of patient age and sex on type of adverse drug event (ADE) reported (N =3174). *We adjusted each estimate for the other variable in the regression (i.e., age for sex and sex for age) and for clustering by patient and presenting hospital
Fig. 3.
Adjusted effects of patient age and sex on the outcome of adverse drug events (ADEs) reported (N = 3174). *We adjusted each estimate for the other variable in the regression (i.e., age for sex and sex for age) and for clustering by patient and presenting hospital
During the study period, data from 638 adverse drug reactions and allergies that occurred in 591 patients were transmitted to PharmaNet. Of 591 patients with transmitted reports, 200 (33.8%, 95% CI 30.0–37.8%) attempted to have the culprit drug re-dispensed. Of these, 44.5% (89/200; 95% CI 37.6–51.4%) occurred within two weeks of the ADE report. Community pharmacists did not re-dispense the culprit drug in 33.0% (66/200; 95% CI 26.5–39.5%) of cases when presented with information about the prior ADE. In 33 attempted re-dispensations (33/200; 16.5%, 95%CI 11.4–21.6%), community pharmacists contacted prescribers for advice resulting in 15 (15/200; 7.5%, 95% CI 3.9–11.2%) re-dispensations and 18 (18/200; 9.0%, 95% CI 5.0–13.0%) dispensation reversals.
Discussion
ActionADE is one of the first interoperable electronic ADE reporting platforms integrated into the clinical workflow of hospital clinicians and community pharmacists that transmits relevant ADE information across health sectors to inform clinical care. ActionADE captured a high volume of reports in 18 months from four participating hospitals. We attribute the high volume of reporting to the user-friendliness of ActionADE and the short amount of time required to generate reports (<2 min/report). Adverse drug event reporting requirements through Vanessa’s Law were met as a by-product of data generated for clinical care provision [27]. We believe these features and others described below motivated clinicians to report ADEs [12].
To characterise ADEs resulting in hospitalisation, prior studies regularly collected data retrospectively (i.e., from administrative data or through medical record review) [28–32]. In our prospective cohort, we reported fewer allergic reactions (8 % vs 13–23%) and more ADRs (74% vs 0.7–29%) than these retrospective studies. Rates of reported ADRs vary significantly between studies using retrospective versus prospective case identification [28, 33–36]. Administrative data are poorly sensitive for ADEs, often capturing fewer than 10% of events depending on the algorithms used [35, 37, 38]. As a result, retrospective data collection will systematically underestimate ADRs like hyponatraemia and acute kidney injury, which are difficult to diagnose with certainty. ActionADE allowed clinicians to document ADEs even when they may not have been certain about their diagnosis by allowing them to rate the certainty of the ADE diagnosis (e.g., suspected vs probable), and providing the option to subsequently edit or even refute events. We excluded refuted events in our analyses, 95% of which were allergy reports. Had they been included the proportion of ActionADE allergy reports would be equal to those previously been reported (17% vs 13–23%) [28, 30]. ActionADE’s design may increase reporting of select events by addressing some of the limitations encountered with other methods commonly used to generate ADE data for surveillance, quality improvement and research, and may help redirect prevention efforts to more prevalent and serious ADEs for greater patient and system-level impact.
The most commonly reported ADEs in ActionADE were ADRs to diuretics, ACE inhibitors, and anticoagulants. These findings align with those of prior studies in which the most commonly reported ADRs were from the cardiovascular medication class [28, 29]. Thiazide diuretics, including hydrochlorothiazide and chlorthalidone, were responsible for over one-fifth of reported events, most manifesting as hyponatremia, and commonly requiring hospitalisation. Other antihypertensive agents (e.g., ramipril, amlodipine) rarely caused ADEs that clinicians reported. While thiazide diuretics do not feature among the top ten drugs prescribed in BC, ramipril and amlodipine do [39]. This indicates that thiazide diuretics may cause a disproportionate number of serious ADEs in comparison to alternative blood pressure-lowering agents. Spontaneous reporting into stand-alone systems remains the basis of many international post-marketing drug surveillance systems. Thiazide diuretics have been on the market for some time, and hyponatraemia is a known side effect [40]. It is likely that these reactions are not being spontaneously reported to post-market surveillance systems, where reporting is driven by drug novelty, reaction severity, and the ease with which the ADE can be diagnosed [15]. Thus, they have not generated safety signals to trigger further investigation, even though they are among the most common events seen in clinical care. While ActionADE was designed primarily as a clinical communication tool, not a surveillance system, its data provide an opportunity to better understand which ADEs are causing the greatest burden to both patients and the health care system while supporting more patient-centred and individualised care.
We found that younger ED patients were more likely to be diagnosed with allergies, non-adherence and drug misuse whereas older patients were more likely to experience ADRs and dosing issues. These findings are in line with studies of similar phenomena in other settings [41–45]. Male patients were more likely to be diagnosed with non-adherence compared to females who were diagnosed more frequently with allergies. It is unclear whether these differences were due to biological sex- or gender-related factors [46]. We also saw differences in reported rates of ADE outcomes by age, but were unable to draw conclusions about why those differences occurred without further understanding of the patient pharmacokinetics, behaviour and access, as well as prescriber and clinician reporting behaviour.
ActionADE has the potential to improve patient safety. One in three patients diagnosed with an ADE to an outpatient medication that was reported in ActionADE and shared via PharmaNet with community pharmacies sought a re-dispensation of the culprit drug. Provision of patient-specific medication-class level information about prior ADEs was associated with avoided re-dispensations of same or same class medications. This potentially prevented repeat ADEs in one in ten patients with an ADE report shared with PharmaNet.
This study is not without limitations. First, while we aimed to address the limitations of many other ADE reporting systems through ActionADE’s user-friendly design and integration [10], reporting remained an additional task for care providers. Thus, underreporting remains, the degree of which we were unable to estimate. Providers may have been less likely to report ADEs when ongoing medication use was indicated (e.g., hypoglycaemia from insulin in diabetic patients). This could have accounted for the lower proportion of events to warfarin or insulin reported in ActionADE compared to other studies, as both drugs are deemed essential medications that would have needed to be continued in almost all cases [30]. Second, reports in ActionADE are not representative of all ADEs to outpatient medications, as reports were generated in acute care hospitals where ActionADE is implemented. Our results are thus not representative of events treated in other health care locations (e.g., walk-in clinics, general practitioners’ offices, long-term care). Third, the community pharmacists responded to ADE alerts in various ways including overriding them, consulting with a physician, changing the drug, or changing the dose. We did not have access to dispensing data, or any instructions provided to the patient outside of PharmaNet (e.g., to decrease the dose) and thus were unable to ascertain dosing or drug changes. The outcome of avoided re-dispensation is therefore a conservative measure that does not encompass all the actions a pharmacist may have taken in response to the ADE information presented. These data could be generalisable to other regions if they were to implement ActionADE or a similar system. ActionADE is web-based and could be used as a stand-alone system or integrated with existing legacy systems in other regions with development of workflows and systems architecture. Finally, we cannot infer causality between the display of ActionADE information and avoided re-dispensations, as data from the control group were unavailable for analysis. We will report these results once enrolment into the trial has been completed.
Conclusions
ActionADE is a novel ADE reporting platform that addresses many limitations of stand-alone systems. Reporting of known ADEs to older medications was common and may reflect their burden on patients and the health system. Reporting and communicating ADEs to community pharmacies using ActionADE was associated with avoided re-exposures to culprit or same-class medications.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Funding
Funding for this work was provided by the Canadian Institutes of Health Research, with support from the Ministry of Health British Columbia, Vancouver Coastal Health, the Lower Mainland Consolidated Pharmacies, and the BC SUPPORT Unit. CMH is a Michael Smith Foundation for Health Research Health Professional-Investigator award holder. EL is supported by the Michael Smith Health Research BC Research Trainee Award. The funders have no role in the design, conduct, analysis, interpretation of data, or the drafting of scientific manuscripts.
Conflicts of interest
ActionADE’s intellectual property is jointly shared between the University of British Columbia and Simon Fraser University. None of the authors have any competing interests to declare.
Ethics approval
The University of British Columbia clinical research ethics board approved of this research (H18-01332 & H21-02973) and provided a waiver for obtaining informed consent as this study meets the Tri-Council Policy Statement (TCPS) minimal risk criteria.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability
Access to data can be requested through the Population Data BC Data Steward(s) or their designated service providers. All inferences, opinions, and conclusions drawn in this publication are those of the author(s), and do not reflect the opinions or policies of the Data Steward(s).
Code availability
The custom code written for this study can be made available upon request.
Author’s contribution
AC and CMH designed this study. CMH, AC, and SS were involved in the work to design and integrate the ActionADE software with PharmaNet. SS, EL, AL, CMH and KB aided in the clinical implementation of the ActionADE software and CMH and KB in community pharmacy implementation efforts. SS, KB, and AC monitored and cleaned the report data and AC performed all analyses. AC drafted the manuscript, and all authors contributed to interpreting study findings and editing the manuscript. All authors approved of the manuscript in its current form.
Footnotes
“MedDRA® the Medical Dictionary for Regulatory Activities terminology is the international medical terminology developed under the auspices of the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). MedDRA® trademark is owned by the International Federation of Pharmaceutical Manufacturers and Associations (IFPMA) on behalf of ICH.
The original online version of this article was revised: In this article due to the coding error in analysis, several data to be updated under the Declarations sections. The Tables 1 to 4 and Figure 3 are updated.
Change history
8/5/2024
A Correction to this paper has been published: 10.1007/s40264-024-01452-2
References
- 1.The WHO Research Priority Setting Working Group. Global priorities for research in patient safety (first edition) [Internet]. World Health Organization; 2008 [cited 2023 Sep 28]. https://www.who.int/publications/i/item/WHO-IER-PSP-2008.13
- 2.Harris Y, Hu DJ, Lee C, Mistry M, York A, Johnson TK. Advancing medication safety: establishing a national action plan for adverse drug event prevention. Jt Commun J Qual Patient Saf. 2015;41:351–60. [DOI] [PubMed] [Google Scholar]
- 3.Hohl CM, Brubacher J, Hunte G, Wiens MO, Abu-Laban R, Singer J, et al. Clinical decision rules to improve the detection of adverse drug events in emergency department patients. Acad Emerg Med. 2012;19:640–9. 10.1111/j.1553-2712.2012.01379.x [DOI] [PubMed] [Google Scholar]
- 4.Hohl CM, Badke K, Zhao A, Wickham ME, Woo SA, Sivilotti MLA, et al. Prospective validation of clinical criteria to identify emergency department patients at high risk for adverse drug events. Griffey RT, editor. Acad Emerg Med. 2018;25:1015–26. 10.1111/acem.13407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zed PJ, Abu-Laban RB, Balen RM, Loewen PS, Hohl CM, Brubacher JR, et al. Incidence, severity and preventability of medication-related visits to the emergency department: a prospective study. Can Med Assoc J. 2008;178:1563–9. 10.1503/cmaj.071594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hohl CM, Woo SA, Cragg A, Wickham ME, Ackerley C, Scheuermeyer F, et al. Repeat adverse drug events associated with outpatient medications: a descriptive analysis of 3 observational studies in British Columbia, Canada. CMAJ Open. 2019;7:E446–53. 10.9778/cmajo.20180190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woo SA, Cragg A, Wickham ME, Villanyi D, Scheuermeyer F, Hau JP, et al. Preventable adverse drug events: descriptive epidemiology. Br J Clin Pharmacol. 2020;86:291–302. 10.1111/bcp.14139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Linden CMJ, Kerskes MCH, Bijl AMH, Maas HAAM, Egberts ACG, Jansen PAF. Represcription after adverse drug reaction in the elderly: a descriptive study. Arch Intern Med. 2006;166:1666–7. 10.1001/archinte.166.15.1666 [DOI] [PubMed] [Google Scholar]
- 9.Chan E, Small SS, Wickham ME, Cheng V, Balka E, Hohl CM. The utility of different data standards to document adverse drug event symptoms and diagnoses: mixed methods study. J Med Internet Res. 2021;23: e27188. 10.2196/27188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bailey C, Peddie D, Wickham ME, Badke K, Small SS, Doyle-Waters MM, et al. Adverse drug event reporting systems: a systematic review. Br J Clin Pharmacol. 2016;82:17–29. 10.1111/bcp.12944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Government of Canada HC. Side effect reporting—drug health product register [Internet]. 2014 [cited 2023 Mar 31]. https://hpr-rps.hres.ca/side-effects-reporting-form.php?form=hospital&lang=en.
- 12.Hohl CM, Small SS, Peddie D, Badke K, Bailey C, Balka E. Why clinicians don’t report adverse drug events: qualitative study. JMIR Public Health Surveill. 2018;4: e21. 10.2196/publichealth.9282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Health Canada. Protecting Canadians from unsafe drugs act (Vanessa’s law): questions/answers [Internet]. 2013 [cited 2022 Dec 7]. https://www.canada.ca/en/health-canada/services/drugs-health-products/legislation-guidelines/questions-answers-regarding-law-protecting-canadians-unsafe-drugs-act-vanessa-law.html.
- 14.Hazell L, Shakir S. Under reporting of adverse drug reactions: a systematic review. Drug Saf. 2006;29:385–96. 10.2165/00002018-200629050-00003 [DOI] [PubMed] [Google Scholar]
- 15.Alomar M, Tawfiq AM, Hassan N, Palaian S. Post marketing surveillance of suspected adverse drug reactions through spontaneous reporting: current status, challenges and the future. Ther Adv Drug Saf. 2020;11:204209862093859. 10.1177/2042098620938595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.About Us [Internet]. BC PSLS Blog. 2013 [cited 2023 Jun 28]. http://bcpslscentral.ca/about-us/.
- 17.Peddie D, Small SS, Badke K, Wickham ME, Bailey C, Chruscicki A, et al. Designing an adverse drug event reporting system to prevent unintentional reexposures to harmful drugs: study protocol for a multiple methods design. JMIR Res Protoc. 2016;5: e169. 10.2196/resprot.5967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chruscicki A, Badke K, Peddie D, Small S, Balka E, Hohl CM. Pilot-testing an adverse drug event reporting form prior to its implementation in an electronic health record. Springerplus. 2016;5:1764. 10.1186/s40064-016-3382-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peddie D, Small SS, Badke K, Bailey C, Balka E, Hohl CM. Adverse drug event reporting from clinical care: mixed-methods analysis for a minimum required dataset. JMIR Med Inform. 2018;6: e10248. 10.2196/10248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hau JP, Brasher PMA, Cragg A, Small S, Wickham M, Hohl CM. Using ActionADE to create information continuity to reduce re-exposures to harmful medications: study protocol for a randomized controlled trial. Trials. 2021;22:119. 10.1186/s13063-021-05061-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Small SS, Hohl CM, Balka E. Organizational implications of implementing a new adverse drug event reporting system for care providers and integrating it with provincial health information systems. Healthc Manag Forum. 2019;32:208–12. 10.1177/0840470419845384 [DOI] [PubMed] [Google Scholar]
- 22.Lau E, Small SS, Butcher K, Cragg A, Loh GW, Shalansky S, et al. An external facilitation intervention to increase uptake of an adverse drug event reporting intervention. Front Health Serv. 2023;3:1106586. [DOI] [PMC free article] [PubMed]
- 23.British Columbia Ministry of Health. Adverse drug events (ADEs) in PharmaNet [Internet]. Province of British Columbia; [cited 2023 Jun 19]. https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/pharmacare/pharmanet-bc-s-drug-information-network/ades-pharmanet.
- 24.British Columbia Pharmacy Association. ActionADE: communicating adverse drug events through PharmaNet [Internet]. [cited 2023 Jun 19]. https://www.bcpharmacy.ca/events/actionade-communicating-adverse-drug-events-through-pharmanet.
- 25.Canadian Patient Safety Institute, Institute for Safe Medication Practices Canada. Medication Reconciliation in Acute Care: Getting Started Kit [Internet]. 2017 [cited 2023 Sep 28]. https://www.ismp-canada.org/download/MedRec/MedRec-AcuteCare-GSK-EN.pdf.
- 26.British Columbia Ministry of Health. PharmaNet. V2. Population data BC. Data Extract. Data Stewardship Committee; 2022.
- 27.Hohl C, Lexchin JR, Balka E. Can reporting of adverse drug reactions create safer systems while improving health data? CMAJ. 2015;187:789–90. 10.1503/cmaj.150057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kongkaew C, Noyce PR, Ashcroft DM. Hospital admissions associated with adverse drug reactions: a systematic review of prospective observational studies. Ann Pharmacother. 2008;42:1017–25. 10.1345/aph.1L037 [DOI] [PubMed] [Google Scholar]
- 29.Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004;329:15–9. 10.1136/bmj.329.7456.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365:2002–12. 10.1056/NEJMsa1103053 [DOI] [PubMed] [Google Scholar]
- 31.Lo Giudice I, Mocciaro E, Giardina C, Barbieri MA, Cicala G, Gioffrè-Florio M, et al. Characterization and preventability of adverse drug events as cause of emergency department visits: a prospective 1-year observational study. BMC Pharmacol Toxicol. 2019;20:21. 10.1186/s40360-019-0297-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Almeida SM, Romualdo A, de Abreu FA, Zelezoglo GR, Marra AR, Edmond MB. Use of a trigger tool to detect adverse drug reactions in an emergency department. BMC Pharmacol Toxicol. 2017;18:71. 10.1186/s40360-017-0177-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karpov A, Parcero C, Mok CPY, Panditha C, Yu E, Dempster L, et al. Performance of trigger tools in identifying adverse drug events in emergency department patients: a validation study: performance of trigger tools in identifying adverse drug events. Br J Clin Pharmacol. 2016;82:1048–57. 10.1111/bcp.13032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hohl CM, Karpov A, Reddekopp L, Stausberg J. ICD-10 codes used to identify adverse drug events in administrative data: a systematic review. J Am Med Inform Assoc. 2014;21:547–57. 10.1136/amiajnl-2013-002116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wickham ME, McGrail KM, Law MR, Cragg A, Hohl CM. Validating use of diagnostic codes in Canadian administrative data for identification of adverse drug events. Br J Clin Pharmacol. 2023 (submitted). [DOI] [PubMed]
- 36.Jhung MA, Budnitz DS, Mendelsohn AB, Weidenbach KN, Nelson TD, Pollock DA. Evaluation and overview of the National Electronic Injury Surveillance System-Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Med Care. 2007;45:S96-102. 10.1097/MLR.0b013e318041f737 [DOI] [PubMed] [Google Scholar]
- 37.Hohl CM, Kuramoto L, Yu E, Rogula B, Stausberg J, Sobolev B. Evaluating adverse drug event reporting in administrative data from emergency departments: a validation study. BMC Health Serv Res. 2013;13:473. 10.1186/1472-6963-13-473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Habib B, Tamblyn R, Girard N, Eguale T, Huang A. Detection of adverse drug events in e-prescribing and administrative health data: a validation study. BMC Health Serv Res. 2021;21:376. 10.1186/s12913-021-06346-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.British Columbia Ministry of Health. PharmaCare Trends 2019-20 [Internet]. 2021 [cited 2023 Jun 19]. https://www2.gov.bc.ca/assets/gov/health/health-drug-coverage/pharmacare/pharmacare-trends-2019-20.pdf.
- 40.Hwang KS, Kim G-H. Thiazide-induced hyponatremia. Electrolyte Blood Press. 2010;8:51–7. 10.5049/EBP.2010.8.1.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim SJ, Kwon OD, Han EB, Lee CM, Oh S-W, Joh H-K, et al. Impact of number of medications and age on adherence to antihypertensive medications: a nationwide population-based study. Medicine. 2019;98: e17825. 10.1097/MD.0000000000017825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cragg A, Hau JP, Woo SA, Kitchen SA, Liu C, Doyle-Waters MM, et al. Risk factors for misuse of prescribed opioids: a systematic review and meta-analysis. Ann Emerg Med. 2019;74:634–46. 10.1016/j.annemergmed.2019.04.019 [DOI] [PubMed] [Google Scholar]
- 43.Canadian Institute for Health Information. Anaphylaxis and allergy in the Emergency Department [Internet]. 2014 [cited 2023 Jun 29]. https://secure.cihi.ca/free_products/Anaphylaxis_Infosheet_en.pdf.
- 44.Just KS, Dormann H, Schurig M, Böhme M, Steffens M, Plank-Kiegele B, et al. The phenotype of adverse drug effects: do emergency visits due to adverse drug reactions look different in older people? Results from the ADRED study. Br J Clin Pharmacol. 2020;86:2144–54. 10.1111/bcp.14304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.U.S. Food & Drug Administration. As you age: you and your medicines [Internet]. 2019 [cited 2023 Jun 29]. https://www.fda.gov/drugs/information-consumers-and-patients-drugs/you-age-you-and-your-medicines.
- 46.Brabete AC, Greaves L, Maximos M, Huber E, Li A, Lê M-L. A sex- and gender-based analysis of adverse drug reactions: a scoping review of pharmacovigilance databases. Pharmaceuticals. 2022;15:298. 10.3390/ph15030298 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Access to data can be requested through the Population Data BC Data Steward(s) or their designated service providers. All inferences, opinions, and conclusions drawn in this publication are those of the author(s), and do not reflect the opinions or policies of the Data Steward(s).