Abstract
Background
Although several studies have shown that the Coronavirus Disease 2019 (COVID-19) lockdown has had negative impacts on mental health and eating behaviors among the general population and athletes, few studies have examined the long-term effects on elite and sub-elite athletes. The present study aimed to investigate the long-term impact of COVID-19 lockdown on mental health and eating behaviors in elite versus sub-elite athletes two years into the pandemic. A cross-sectional comparative study was conducted between March and April 2022, involving athletes from 14 countries, using a convenient non-probabilistic and snowball sampling method. A total of 1420 athletes (24.5 ± 7.9 years old, 569 elites, 35% women, and 851 sub-elites, 45% women) completed an online survey-based questionnaire. The questionnaire included a sociodemographic survey, information about the COVID-19 pandemic, the Depression, Anxiety and Stress Scale—21 Items (DASS-21) for mental health assessment, and the Rapid Eating Assessment for Participants (REAP-S) for assessing eating behavior.
Results
The results showed that compared to sub-elite athletes, elite athletes had lower scores on the DASS-21 (p = .001) and its subscales of depression (p = .003), anxiety (p = .007), and stress (p < .001), as well as a lower REAP-S score indicating lower diet quality (p = .013).
Conclusion
In conclusion, two years into the pandemic, elite athletes were likelier to have better mental health profiles than sub-elite athletes but surprisingly had lower diet quality.
Keywords: Performance, Athlete, Nutrition, Infectious disease, Health
Key Points
Elite athletes had better mental health profiles compared to sub-elite athletes, with lower levels of depression, anxiety, and stress.
Elite athletes reported greater psychological support and perceived themselves as more financially secure during the pandemic than sub-elite athletes do.
Elite athletes were more likely to have poor eating habits compared to sub-elite athletes.
Background
The first case of Coronavirus Disease 2019 (COVID-19) was reported in Wuhan, Hubei province, mainland China, on December 12, 2019 [1]. COVID-19 is a highly contagious infectious disease caused by the novel Severe Acute Respiratory Syndrome Coronavirus type 2. Since the population was virtually immunologically naïve to the virus and vaccines were not initially available, preventive public health measures consisted primarily of non-pharmaceutical interventions such as "stay-at-home" directives and lockdowns, which were implemented to halt the spread of the disease [2–4]. The COVID-19 outbreak was considered a global health and social crisis, causing high levels of psychological and social distress among various populations around the world [5–8]. Decisions on the lockdown implementation variated in both duration and severity among countries during the pandemic, making it difficult to conduct comprehensive analyses of the long-term effects of COVID-19 confinement; however, there is a clear understanding that more strict or prolonged measures result in more severe problems in different population spheres, such as mental health [9, 10].
The COVID-19 pandemic and the resulting lockdowns have had a significant impact on the sports community worldwide, with athletes unable to train, travel, or participate in competitions [11, 12]. The closure of training facilities has made it difficult for athletes to adhere to their training plans, and many have had to alter their training practices alone, without the guidance of coaching and support staff [13, 14]. This has had a detrimental impact on the physical and mental well-being of athletes, who have also faced financial difficulties due to the loss of income from canceled events.
The limitations on opportunities for sports and physical activity due to the COVID-19 pandemic have led to an increase in sedentary behavior, such as prolonged sitting and increased screen time. These changes in daily routines have significantly disrupted athletes' athletic routines [15], resulting in reduced motivation to train [12, 16] and affected their ability to perform training exercises appropriately [17]. Furthermore, some athletes may have faced financial difficulties, such as contract loss or sponsorship, which may have worsened their mental health challenges during lockdown periods [18]. The COVID-19-induced lockdown has had a detrimental effect on people's mental health [13]. Mental health is a state of well-being in which an individual can recognize their own abilities, manage everyday stressors, work productively and fruitfully, and contribute to their community [19]. During lockdown, athletes have experienced emotional distress and psychological disorders due to the lack of physical activity, isolation from sports teams, separation from the athletic community, ineffective interactions with coaches, and reduced fans/media support [20].
The uncertainty surrounding the return to sports activities, concerns about contracting COVID-19, worries about recovery if infected, financial difficulties, family conflicts, lack of access to workout facilities, and concerns about future performance can all contribute to mental health problems such as stress, depression, anxiety, and sleep disorders [21, 22]. This is particularly true for individuals who lack adequate coping strategies [23–25]. The decrease in opportunities to participate in sport-related social support networks due to the COVID-19 pandemic may result in feelings of loneliness, as reported by Lippke et al. [26]. This can be particularly challenging for elite athletes, who may experience social isolation and anxiety [25]. The elevated levels of anxiety and stress caused by the pandemic can lead to changes in sleeping habits, such as altered bedtimes, increased screen time, and an increased likelihood of sleep disturbances and disorders [17, 27]. Research has shown that disorders such as stress, anxiety, and sleep disturbances have been linked to a lack of physical activity and workouts [28–30]. Athletes who experience depression may have altered sleeping patterns, lack motivation to stay active, and prefer sedentary behavior during leisure time [16, 20]. Interestingly, athletes have been found to have better mental health compared to non-athletes [31]. Among athletic groups, elite athletes have been reported to have higher levels of self-esteem, mental health, and quality of life relative to sub-elite athletes [32–34]. Furthermore, elite athletes have been found to have better psychological and/or spiritual domains, report higher self-satisfaction and peace of mind, and experience less stress and better biopsychosocial functioning [28, 34, 35]. The COVID-19 lockdown has led to an increase in unhealthy eating behaviors, which can lead to weight gain [27] and cardiometabolic disorders. Elite athletes may be better equipped to maintain healthier dietary practices during the pandemic [36]. In addition, in those who were allowed to return to training activities earlier, faster recovery of fitness and body composition was demonstrated [37]. Factors such as economic and social status, social support, and pre-pandemic mental health and physical fitness levels also play a role in determining health-related behaviors during the pandemic [36]. Although several studies have examined the impact of COVID-19 lockdowns on the mental health and eating habits of elite and sub-elite athletes, few studies have looked at the long-term effects of these lockdowns, two years into the pandemic, on these specific populations. Comparing the experiences of elite and sub-elite athletes may help identify specific risk factors that contribute to the resulting mental health status and eating habits. As many countries have started to ease restrictions and reduce safety procedures, it is important to understand the long-term effects of the pandemic on athletes, and to develop evidence-based strategies for monitoring psychological issues and eating disorders during future lockdowns or similar scenarios.
Methods
Participants
The research employed a convenient non-probabilistic and snowball sampling method to conduct a cross-sectional study on athletes who were in or had been in lockdown due to the COVID-19 pandemic. The final sample included 1,420 athletes (41% women) from 1702 athletes who were invited to participate in our study (response rate = 83.43%). As inclusion criteria, at the time when the study was conducted, participants must be at least 18 years of age (mean ± standard deviation [SD]: 24.5 ± 7.9 years), have been under confinement for more than one week, and not to have stopped training for more than 1 week due to injury or illness; while failure to complete the survey was considered as a criterion for elimination. The study includes data from 14 different countries of four continents; Asia: (1) Iran, (2) Turkey, (3) United Arab Emirates; Africa: (4) Egypt, (5) Tunisia, and (6) Algeria; America: (7) Mexico, (8) Brazil, and (9) United States of America; and Europe: (10) Spain, (11) Portugal, (12) England, (13) Germany, and (14) France. The study included athletes who participate at national and international levels, as well as those who practice sports on a recreational basis. Athletes were classified as elite (i.e., semi-professional, high-competitive and professional level) and sub-elite (i.e., amateur and recreational level) athletes. The characteristics of the sample are presented in Table 1.
Table 1.
Athlete’s level distribution by country (n = 1420)
| Country | Sub-elite | Elite | Total |
|---|---|---|---|
| Turkey | 69 | 31 | 100 |
| United Arab Emirates | 40 | 26 | 66 |
| Iran | 102 | 84 | 186 |
| Tunisia | 72 | 59 | 131 |
| Algeria | 53 | 28 | 81 |
| Egypt | 72 | 35 | 107 |
| United States of America | 53 | 29 | 82 |
| Mexico | 69 | 59 | 128 |
| Brazil | 55 | 36 | 91 |
| Portugal | 69 | 56 | 125 |
| England | 58 | 42 | 100 |
| Spain | 65 | 29 | 94 |
| Germany | 48 | 35 | 83 |
| France | 26 | 20 | 46 |
| Total | 851 | 569 | 1420 |
Procedures
The data for the study were collected between March and April 2022, two years after the World Health Organization declared the COVID-19 pandemic. The questionnaires were transcribed into an online Google form. The researchers in each of the countries involved in the study distributed the instrument through their contacts in sports organizations and clubs who facilitated access to the athletes. Participants were invited to participate via WhatsApp or email through the link to enter the survey. For every country, a researcher was named as the main contact for response questions from the participants of the study. All participants were required to read the instructions, as well as the informed consent, and indicate their agreement to participate in the research by checking a specific box of the online survey. Athletes took an average of 10 to 15 min to answer the entire survey. Those who skipped sections or did not complete the survey were discarded from the sample. The study was approved by the Ethics Committee of Qazvin University of Medical Sciences (IR.QUMS.REC.1401.311), and athletes completed the survey in their native language or the one they were most familiar with. Sociodemographic and COVID-19-related information was collected, and the questionnaire was translated from English into several languages (e.g., Persian, Arabic, Spanish, Turkish, Portuguese, German, and French) using a back-translation method as suggested by the literature [38]. The study used existing translated versions of the Rapid Eating and Activity Assessment for Patients (REAP-S) and Depression, Anxiety and Stress Scale-21 (DASS-21) questionnaires.
Instruments
Sociodemographic and COVID-19 Information
The study used an ad hoc survey to obtain information about three main dimensions of the participants: individual characteristics (e.g., gender, age, body composition, sports history, and education level), social characteristics (e.g., marital status, family, and household), and COVID-19-related information (e.g., history, vaccine, and mental health support). This information was used to analyze and compare the mental health and eating behaviors among the athletes, as presented in Table 1.
Eating Behaviors
The REAP-S survey was used to measure the eating behaviors and nutritional status of the athletes [39]. This self-reported tool consists of one item with a Likert scale of five points to evaluate the willingness to make changes in one's eating habits to be healthier and 15 items with a four-point Likert scale to assess food intake from all food groups and diet-related habits. Scores range from 0 to 39 points, with higher scores indicating healthier dietary behavior characterized by optimal intake of fruits, vegetables, and whole grains and decreased intake of sugary foods, processed meats, and fried foods. The REAP-S is known as a useful cross-cultural questionnaire for assessing eating behavior [40–46]. It has also been applied to athletes and is a reliable tool for evaluating the dietary behaviors of this population [42, 47].
Mental Health
To assess the impact of the COVID-19 lockdown on athletes, the DASS-21 [48] was used, which is a scale consisting of 21 items that measure symptoms of depression, anxiety, and stress experienced during the past week. Athletes rated each item on a four-point scale, and the final score of each scale was calculated by multiplying the mean score of the scale by two. The DASS-21 has been validated and translated into multiple languages, and the internal consistency of the subscales has been reported to be high [49]. The scale has also been used with athletes during the beginning of the COVID-19 lockdown. In this study, the internal consistency of the DASS subscales was high, with Cronbach's alphas of 0.94, 0.88, and 0.93 for depression, anxiety, and stress, respectively. Overall, the DASS-21 is a reliable tool for assessing the mental health of athletes during the COVID-19 pandemic and has been validated in various languages and contexts.
Statistical Analysis
Before conducting statistical analyses, the homogeneity and equality of variances of the data were confirmed through the Kolmogorov–Smirnov and Levene's tests, respectively. The data in tables and text were presented as frequency, percentage, mean, and SD. To compare quantitative data of the elite and sub-elite athletes, an independent t test was used, while a Chi-square independence test was used to compare categorical data. The effect size was also calculated. The level of significance was set at alpha p < 0.05. All statistical analyses were performed using SPSS v. 23 (IBM Corporation; Armonk, NY, USA) and Excel spreadsheet (Microsoft Corporation; Redmond, WA).
Results
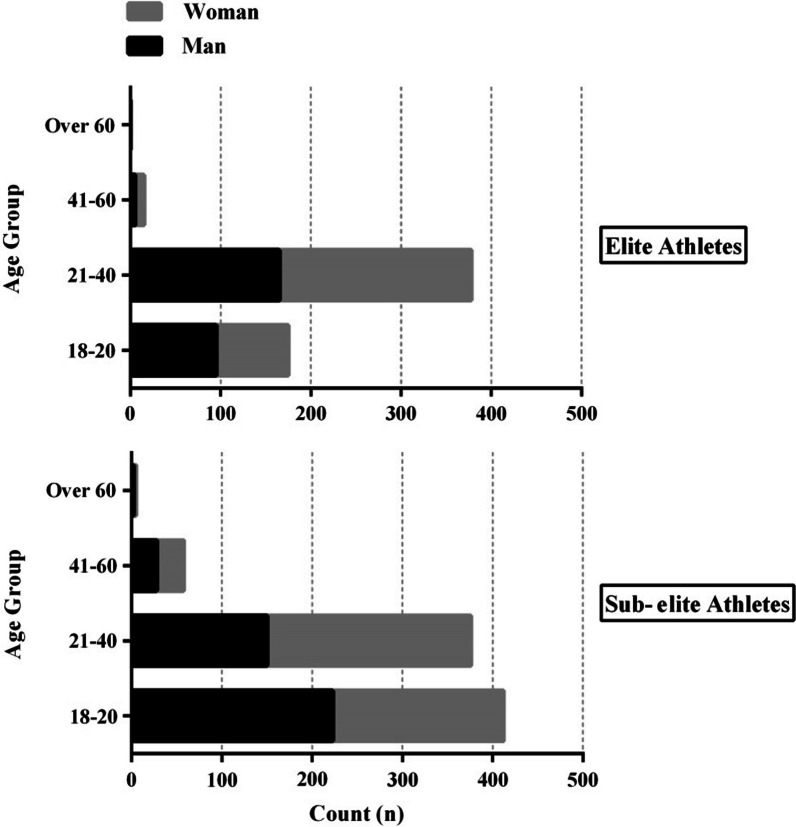
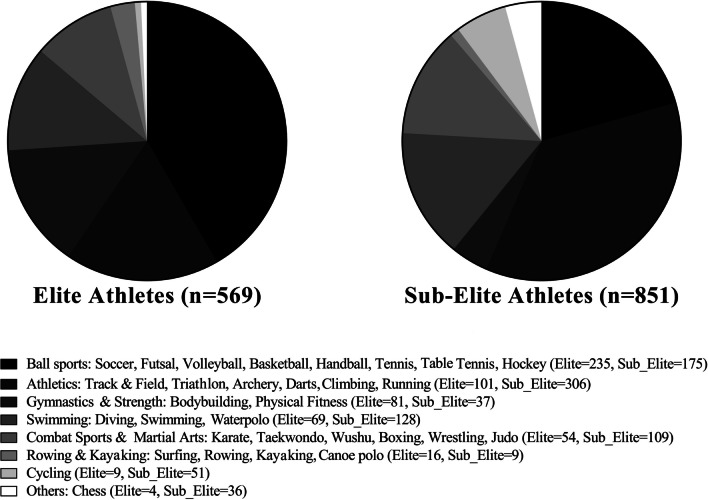
The distribution of age groups among elite and sub-elite athletes and the type of sport they participated in are shown in Figs. 1 and 2, respectively. Table 1 exposes the athlete’s level distribution by country.
Fig. 1.
Histogram detailing the gender split and age groups for elite (n = 569) and sub-elite (n = 851) athletes groups
Fig. 2.
Pie chart of sports played by the elite (n = 569) and sub-elite (n = 851) athletes’ sample
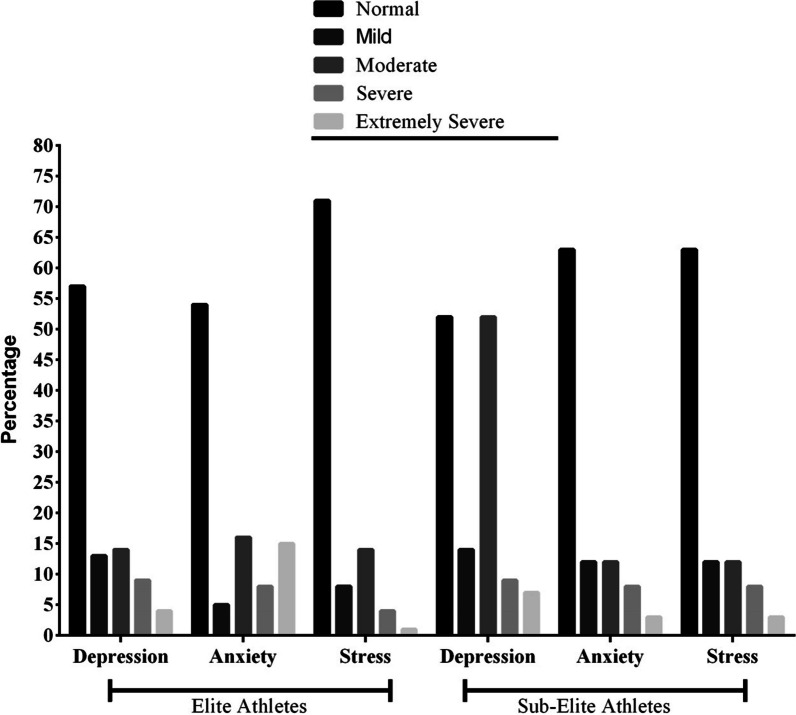
Athlete demographics were compared between groups and can be found in Table 2. More than half of the athletes experienced 1 to 4 weeks of social distancing, with sub-elite athletes reporting significantly more social distancing than elite athletes do. The levels of depression, anxiety, and stress were compared between elite and sub-elite athletes, and the results are displayed in Fig. 3. The data suggest that elite athletes had lower levels of depression compared to sub-elite athletes, with 52.1% of elite athletes reporting moderate depression (p < 0.001).
Table 2.
Descriptive statistics of athletes (n = 1420)
| Demographics | Unit/Category | Sub-elite (n = 851) | Elite (n = 569) | Total (n = 1420) | p value |
|---|---|---|---|---|---|
| Agea | Years | 24.2 (8.8) | 24.9 (6.6) | 24.5 (7.9) | = .756 |
| Heighta | Cm | 171.2 (9.7) | 175.6 (10.2) | 172.9 (10.2) | = .002* |
| Weighta | kg | 69.2 (14.8) | 73.3 (17.5) | 70.9 (16.1) | < .001* |
| Sports historya | Years | 5.8 (7.01) | 9.6 (6.3) | 7.3 (6.9) | = .022* |
| Marital statusb | Solid partnership / Married | 166 (19.2) | 116 (20.4) | 282 (19.9) | < .001* |
| Living without a partner / single | 685 (80.8) | 453 (79.6) | 1138 (80.1) | < .001* | |
| Education levelb | No schooling completed | 76 (8.9) | 33 (5.8) | 109 (7.7) | = .008 |
| High school graduate | 208 (24.4) | 132 (23.2) | 340 (23.9) | < .001* | |
| Bachelor’s degree | 494 (58.1) | 329 (57.8) | 823 (57.9) | < .001* | |
| Master’s degree | 52 (6.1) | 62 (10.9) | 114 (8.1) | < .001* | |
| Doctoral’s degree | 21 (2.5) | 13 (2.3) | 34 (2.4) | < .001* | |
| Count of householdsb | Live alone | 295 (34.7) | 193 (33.9) | 488 (34.4) | < .001* |
| 2 | 88 (10.3) | 71 (12.5) | 159 (11.2) | < .001* | |
| More than 2 | 468 (55.0) | 305 (53.6) | 773 (54.4) | < .001* | |
| History of COVID-19b | Yes | 257 (30.2) | 219 (38.5) | 476 (33.5) | < .001* |
| Doses of vaccineb | 0 | 39 (4.6) | 42 (7.4) | 81 (5.7) | = .025* |
| 1 | 35 (4.1) | 35 (6.1) | 70 (4.9) | < .001* | |
| 2 | 403 (47.3) | 258 (45.3) | 661 (46.5) | < .001* | |
| 3 & more | 367 (43.1) | 241 (42.3) | 608 (42.9) | < .001* | |
| Type of sportb | Individual Sport Athlete | 398 (46.8) | 249 (43.8) | 647 (45.6) | < .001* |
| Team Sport Athlete | 453 (53.2) | 320 (56.2) | 773 (54.4) | < .001* | |
| Financially secureb | Yes | 270 (31.7) | 203 (35.7) | 473 (33.3) | < .001* |
| Weeks spent social distancingb | 1–4 Weeks | 462 (54.3) | 366 (64.3) | 828 (58.3) | < .001* |
| 1–2 Months | 179 (21.0) | 101 (17.7) | 280 (19.7) | < .001* | |
| 2–4 Months | 121 (14.2) | 73 (12.8) | 194 (13.7) | < .001* | |
| More than 4 Months | 89 (10.5) | 29 (5.1) | 118 (8.3) | < .001* | |
| Sought psychological or mental support: Yesb | Before COVID-19 | 24 (2.8) | 9 (1.6) | 33 (2.3) | < .001* |
| During COVID-19 | 102 (12.0) | 72 (12.7) | 174 (12.3) | < .001* |
COVID-19 Coronavirus disease 2019. Data were aMean (standard deviation), bNumber (%). *p value < .05 (Chi-square independence test or independent t test)
Fig. 3.
Bar chart of Depression, Anxiety and Stress Scale-21 in elite (n = 569) and sub-elite (n = 851) athlete groups
Summary statistics for the DASS-21 and REAP-S in elite and sub-elite athletes are reported in Table 3. There were significant differences in the means of depression (t(1418) = 2.99, p = 0.003, η2 = 0.16), anxiety (t(1418) = 2.72, p = 0.007, η2 = 0.15), stress (t(1418) = 4, p < 0.001, η2 = 0.22), total scale of DASS-21 (t(1418) = 3.47, p = 0.001, η2 = 0.19), and REAP-s (t(1418) = 2.48, p = 0.013, η2 = 0.13).
Table 3.
Summary statistics for the DASS-21 and REAP-S in athletes (n = 1420)
| Elite (n = 569) | Sub-elite (n = 851) | Total athletes (n = 1420) | t (p value) | effect size | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scale | Subscales | Mean | SD | Range | Mean | SD | Range | Mean | SD | Range | ||
| DASS-21 | Depression | 8.78 | 9.37 | 0–36 | 10.35 | 9.88 | 0–36 | 9.72 | 9.71 | 0–36 | 2.99* | − 0.48 |
| Anxiety | 8.86 | 9.31 | 0–42 | 10.27 | 9.75 | 0–42 | 9.71 | 9.60 | 0–42 | 2.72* | − 0.43 | |
| Stress | 9.89 | 9.34 | 0–36 | 11.99 | 10.01 | 0–36 | 11.15 | 9.79 | 0–36 | 4.0* | − 0.53 | |
| Total scale | 27.53 | 26.15 | 0–114 | 32.62 | 27.61 | 0–114 | 30.58 | 27.2 | 0–114 | 3.47* | − 0.54 | |
| REAP-S | 23.69 | 7.44 | 0–28 | 24.69 | 7.48 | 0–39 | 24.29 | 7.48 | 0–39 | 2.48* | − 0.51 | |
DASS-21 Depression, Anxiety and Stress Scale-21. REAP-S Rapid Eating and Activity Assessment for Patients. SD Standard deviation. Scores on the DASS-21 are multiplied by 2 to calculate the final scores. *p value < .05 (independent t tests between Elite and Sub-elite athletes)
Discussion
This study aimed to explore and compare the impact of the COVID-19 pandemic on the mental health and dietary habits of elite and sub-elite athletes worldwide; two years after the pandemic began. The results showed that elite athletes had better mental health profiles than sub-elite athletes, with lower levels of depression, anxiety, and stress. Elite athletes reported greater psychological support and perceived themselves as more financially secure than sub-elite athletes did during the pandemic. Both groups had good adherence to healthy dietary habits, but elite athletes exhibited less positive eating behaviors than sub-elite athletes did. The results of the study indicate that elite athletes were better equipped to handle the psychological challenges posed by the pandemic but may have been less attentive to their nutritional habits compared to sub-elite athletes. These findings suggest that the better mental health profiles of elite athletes may be attributed to factors such as coping ability, income inequalities, and support.
Elite athletes are often equipped with superior coping abilities, allowing them to navigate the challenges and pressures of competitive sports with greater ease. Research studies support this notion, suggesting that experienced or higher-level athletes tend to have better coping skills, which may enable them to cope more effectively with the uncertainties of the COVID-19 pandemic [25, 50]. Additionally, research has shown that elite athletes generally exhibit better mental health outcomes, with lower levels of stress and depressive symptoms, compared to lower-level athletes [34].
Our study findings align with prior research, suggesting that elite athletes may be more accepting of the negative impacts of the pandemic on their sporting careers, such as the cancelation or postponement of important competitions, including the Olympic Games [13, 51]. Moreover, we found that elite athletes perceived themselves as more financially secure than sub-elite athletes, consistent with research among football players worldwide [52]. Perceptions of financial security have been identified as a significant risk factor for mental health [53–55], which may be particularly relevant for sub-elite athletes who may experience income loss due to sport-related job disruptions [52, 54]. However, this factor may not be as crucial for some elite athletes.
It is worth noting that both elite and sub-elite athletes reported an increase in seeking psychological support during the pandemic, with a higher percentage of elite athletes seeking support than sub-elite athletes. Seeking support was more prevalent among elite athletes than among lower-level athletes during the pandemic or lockdown [12, 14], which is consistent with findings reported by Jaenes Sánchez et al. [51]. Despite the onset of emotional distress as a result of COVID-19, the normalization of seeking support from mental health professionals may have helped elite athletes cope better with the mental health challenges associated with confinement and could prove vital in promoting better coping strategies in the face of future stressful situations.
Studies investigating the impact of COVID-19 on the mental health of athletes have yielded inconclusive results, with some suggesting that athletes are experiencing mental health issues. This underscores the importance of individual-level psychological interventions [34, 52, 54–56] to support athletes in managing their mental health during times of stress and uncertainty. To gain a more comprehensive understanding of these issues, it is crucial to continue researching this phenomenon even after it has been declared a solved or controlled problem.
Based on the DASS-21 results, our study participants exhibited normal to moderate levels of depression, anxiety, and stress. This differs from what has been reported in other studies that found high rates of depression [57] and stress [58] among the general population in Italy. However, some studies conducted at the beginning of the COVID-19 pandemic among athletes found an increase in psychobiological stress response [35], and high levels of dysfunctional psychological responses [35, 50]. Similar findings have been reported in studies carried out more than a year after the pandemic began [55, 56]. This disparity in findings could be attributed to differences in the investigations' timing and the extent of social distancing measures in place at the time of data collection. It is possible that our study participants had less restricted measures of social distancing, which may have enabled them to return to their sports activities more easily than participants in other studies. Our findings are consistent with previous research indicating that increased physical activity has a protective effect on mental health, such as reducing anxiety symptoms associated with the COVID-19 pandemic [51, 59]. It is also possible that our participants underwent a learning process and familiarized themselves with the conditions of the new pandemic world, which may have contributed to their improved mental health outcomes [34, 56].
Contrary to the existing literature, our study found that sub-elite athletes have better dietary habits than elite athletes. A systematic review by Heaney et al. [60] concluded that elite athletes generally have better eating habits than sub-elite or non-athletes. However, a study conducted with Turkish taekwondo athletes [61], as well as research carried out with elite Iranian athletes [62] during the COVID-19 pandemic, reported similar results to our study, where lower-level athletes exhibited more positive nutritional habits. This behavior could be explained by the fact that elite athletes typically have more restricted diets and better nutritional habits during normal circumstances, the COVID-19 pandemic disrupted their routines and made it more challenging for them to adapt to changes in their eating habits. Additionally, the cancelation or modification of competition schedules may have led to increased relaxation and altered eating behavior, such as consuming more food or snacks while spending more time at home.
It is important to provide nutritional support to athletes to minimize the negative impact of COVID-19 on their eating habits through online education or interaction with athletes [20, 63]. Previous research reported how important it is for elite athletes to maintain good eating habits to help their sleep quality during the COVID-19 pandemic [64]. However, there is limited research on the eating behavior of athletes during the pandemic, and it appears that maintaining optimal weight may be an additional stressor for elite athletes. Therefore, further research is needed, especially comparisons between elite and sub-elite athletes, to gain a better understanding of these issues.
Additionally, the REAP-S data collected in our study indicated positive nutritional practices in both groups [41]. Some studies have reported positive changes in eating behaviors during the pandemic [7, 65]. This may be attributed to individuals having more time to prepare their own food, coupled with restrictions on getting food outside the home and a greater awareness of the importance of maintaining a healthy diet [7, 66]. Therefore, our study contributes to understanding how the COVID-19 pandemic has affected the overall food consumption and dietary habits of both elite and sub-elite athletes.
The present study has several strengths, including the availability of a survey in multiple languages that has been widely distributed across various continents. This cross-cultural design involved scientists and researchers from diverse sports science disciplines and countries, who worked together to facilitate the study process. Moreover, this study focused on elite and sub-elite athletes from different continents and countries, and only a few comprehensive studies have been conducted in this field. However, our study does have some limitations. One of the limitations was the failure to consider the influence of sports type (individual vs. team). As participating in a team sport could have a protective effect on mental health, this difference may be a confounding factor. Future studies should take this factor into account and compare the effectiveness of each sport type on athletes' mental health. Additionally, the cross-sectional design of the study was the other limitation. It should also be noted that online surveys commonly suffer from two serious methodological limitations. First, the population to which they are distributed cannot be described, and respondents with biases may select themselves for the sample. We are also aware that some factors, such as coping abilities, psychological support, economic security, and the period of the study, could have influenced the observed results. Differences in the severity of lockdowns experienced in different countries may influence the responses of participants. Furthermore, because lockdown was a “surprise” measure in many countries, we were unable to develop and disseminate the survey "before" lockdown for baseline measures. In this study, one additional limitation could be the reliance on self-reporting by the athletes regarding their experiences during the pandemic. Since a significant amount of time has passed, there may be a possibility of recall bias or inaccuracies in their responses. Furthermore, future research could consider using more objective measures or cross-referencing with other sources of information to validate the athletes' responses.
Conclusions
This global study investigated the long-term effects of the COVID-19 pandemic on the mental health and nutritional practices of elite and sub-elite athletes. According to the study’s findings, despite the changes in everyday life caused by the COVID-19 pandemic, elite athletes appeared to have better mental health outcomes than sub-elite athletes, as indicated by lower levels of emotional distress as reflected in their DASS-21 score. Furthermore, the data revealed that elite athletes were more likely to have poor eating habits compared to sub-elite athletes, which is an important finding that may be explained by a lack of guidance/education (or even willingness) to maintain their nutritional regimen (e.g., preparing their own food), among others.
Acknowledgements
The authors thank the colleagues in our consortium who collaborated greatly in the research and who contributed their knowledge and experience. We thank all colleagues and athletes who believed in this initiative and helped distribute the anonymous survey worldwide.
Abbreviations
- COVID
Corona Virus Disease
- DASS
Depression, Anxiety and Stress Scale
- REAP-S
Rapid Eating Assessment for Participants
Author Contributions
MT, JAW were involved in conceptualization; MT, HBS, JAW, LFR-S, MM, KT, MM, HM-H, LJM-D-S, AS, FT, YS, RLV, SD, ST, ÖE, HC, ID, JS, AFG-M, TL, ESE, AA, HZ, AT, CC, NB, MA, MSR, AA, HN, KI were involved in data curation; MM, CK, MS contributed to formal analysis; MT, HBS, JAW, LFR-S, MM, LY, KT, MM, HM-H, LJM-D-S, AS, FT, YS, CK, RLV, SD, MA, ST, MS, HC, ID, JS, AFG-M, TL, ESE, AA, HZ, AT, CC, NB, AA, HN, KI were involved in investigation; MT, LFR-S, MM, KT, HM-H, LJM-D-S, AA, KI methodology; MT contributed to project administration; AA were involved in validation; MT, ST contributed to writing—original draft; HBS, JAW, LFR-S, MM, TL, AA, KBA, NLB, MT, KW, BK, KI were involved in writing—review & editing. All authors have read and agreed to the published version of the manuscript.
Funding
The research has been financially supported by Iran National Science Foundation (INSF) (Grant No. 4005118).
Availability of Data and Materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of Qazvin University of Medical Sciences (IR.QUMS.REC.1401.311) and followed the guidelines and ethical recommendations for the treatment of subjects and the data obtained as stated in the 1964 Declaration of Helsinki. All participants gave an electronic informed consent prior to the study.
Consent for Publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Morteza Taheri, Email: taheri.mortza@ut.ac.ir.
Beat Knechtle, Email: beat.knechtle@hispeed.ch.
References
- 1.Wu F, Zhao S, Yu B, Chen Y-M, Wang W, Song Z-G, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodge A. Implications of COVID-19 for nutrition. Public Health Nutr. 2020;23:3057–3058. doi: 10.1017/S136898002000436X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koh D. COVID-19 lockdowns throughout the world. Occup Med. 2020;70:322–322. doi: 10.1093/occmed/kqaa036. [DOI] [Google Scholar]
- 4.Marroquín B, Vine V, Morgan R. Mental health during the COVID-19 pandemic: effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Res. 2020;293:113419. doi: 10.1016/j.psychres.2020.113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dergaa I, Abdelrahman H, Varma A, Yousfi N, Souissi A, Ghram A, et al. COVID-19 vaccination, herd immunity and the transition toward normalcy: challenges with the upcoming sports events. Ann Appl Sport Sci. 2021;9:e1032. doi: 10.52547/aassjournal.1032. [DOI] [Google Scholar]
- 6.Moshtagh M, Mirlashari J, Amiri R. Global collaboration and social practices to mitigate impacts of COVID-19 in the world: a lived experience of infecting. Qual Soc Work. 2021;20:366–374. doi: 10.1177/1473325020981088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salman A, Sigodo KO, Al-Ghadban F, Al-Lahou B, Alnashmi M, Hermassi S, et al. Effects of COVID-19 lockdown on physical activity and dietary behaviors in Kuwait: a cross-sectional study. Nutrients. 2021;13:2252. doi: 10.3390/nu13072252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vancini RL, Borges Viana R, dos Santos Andrade M, Andre Barbosa de Lira C, Theodoros Nikolaidis P, Aparecido de Almeida A, et al. YouTube as a source of information about physical exercise during COVID-19 outbreak. Int J Sport Stud Health 2022;4: e123312. 10.5812/intjssh.123312
- 9.Fountoulakis KN, Karakatsoulis GN, Abraham S, Adorjan K, Ahmed HU, Alarcón RD, et al. The effect of different degrees of lockdown and self-identified gender on anxiety, depression and suicidality during the COVID-19 pandemic: data from the international COMET-G study. Psychiatry Res. 2022;315:114702. doi: 10.1016/j.psychres.2022.114702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: a review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104(2):3685042110198. doi: 10.1177/00368504211019854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samuel RD, Tenenbaum G, Galily Y. The 2020 coronavirus pandemic as a change-event in sport performers’ careers: conceptual and applied practice considerations. Front Psychol. 2020;11:567966. doi: 10.3389/fpsyg.2020.567966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Washif JA, Farooq A, Krug I, Pyne DB, Verhagen E, Taylor L, et al. Training during the COVID-19 lockdown: knowledge, beliefs, and practices of 12,526 athletes from 142 countries and six continents. Sports Med. 2022;52:933–948. doi: 10.1007/s40279-021-01573-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carnevale Pellino V, Lovecchio N, Puci MV, Marin L, Gatti A, Pirazzi A, et al. Effects of the lockdown period on the mental health of elite athletes during the COVID-19 pandemic: a narrative review. Sport Sci Health. 2022 doi: 10.1007/s11332-022-00964-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Washif JA, Sandbakk Ø, Seiler S, Haugen T, Farooq A, Quarrie K, et al. COVID-19 lockdown: a global study investigating the effect of athletes’ sport classification and sex on training practices. Int J Sports Physiol Perform. 2022;17:1242–1256. doi: 10.1123/ijspp.2021-0543. [DOI] [PubMed] [Google Scholar]
- 15.Vitali F, Bisagno E, Coco M, Cadamuro A, Maldonato NM, Di Corrado D. A moderated mediation analysis of the effects of the COVID-19 pandemic on well-being and sport readiness of italian team sports players: the role of perceived safety of the training environment. Int J Environ Res Public Health. 2022;19:2764. doi: 10.3390/ijerph19052764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pillay L, Janse van Rensburg DCC, Jansen van Rensburg A, Ramagole DA, Holtzhausen L, Dijkstra HP, Nowhere to hide: The significant impact of coronavirus disease,, et al. (COVID-19) measures on elite and semi-elite South African athletes. J Sci Med Sport. 2019;2020(23):670–679. doi: 10.1016/j.jsams.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Washif JA, Ammar A, Trabelsi K, Chamari K, Chong CSM, Mohd Kassim SFA, et al. Regression analysis of perceived stress among elite athletes from changes in diet, routine and well-being: effects of the COVID-19 lockdown and “bubble” training camps. Int J Environ Res Public Health. 2021;19:402. doi: 10.3390/ijerph19010402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haan R, Ali Alblooshi ME, Syed DH, Dougman KK, Al Tunaiji H, Campos LA, et al. Health and well-being of athletes during the coronavirus pandemic: a scoping review. Front Public Health. 2021;9:641392. doi: 10.3389/fpubh.2021.641392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reardon CL, Hainline B, Miller-Aron C, Baron D, Baum AL, Bindra A, et al. Mental health in elite athletes: international olympic committee consensus statement (2019) Br J Sports Med. 2019;53:667–699. doi: 10.1136/bjsports-2019-100715. [DOI] [PubMed] [Google Scholar]
- 20.Ammar A, Chtourou H, Boukhris O, Trabelsi K, Masmoudi L, Brach M, et al. COVID-19 home confinement negatively impacts social participation and life satisfaction: a worldwide multicenter study. Int J Environ Res Public Health. 2020;17:6237. doi: 10.3390/ijerph17176237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shukla A, Dogra DK, Bhattacharya D, Gulia S, Sharma R. Impact of COVID-19 outbreak on the mental health in sports: a review. Sport Sci Health. 2023 doi: 10.1007/s11332-023-01063-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jia L, Carter MV, Cusano A, Li X, Kelly JD, Bartley JD, et al. The effect of the COVID-19 pandemic on the mental and emotional health of athletes: a systematic review. Am J Sports Med. 2023;51:2207–2215. doi: 10.1177/03635465221087473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andreato LV, Coimbra DR, Andrade A. Challenges to athletes during the home confinement caused by the COVID-19 pandemic. Strength Cond J. 2020;42:1–5. doi: 10.1519/SSC.0000000000000563. [DOI] [Google Scholar]
- 24.Mehrsafar AH, Gazerani P, Moghadam Zadeh A, Jaenes Sánchez JC. Addressing potential impact of COVID-19 pandemic on physical and mental health of elite athletes. Brain Behav Immun. 2020;87:147–148. doi: 10.1016/j.bbi.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tingaz EO. The psychological impact of COVID-19 pandemic on elite athletes, management strategies and post-pandemic performance expectations: a semi structured interview study. Int J Edu Res Innov. 2020;23:73. doi: 10.46661/ijeri.4863. [DOI] [Google Scholar]
- 26.Lippke S, Fischer MA, Ratz T. Physical activity, loneliness, and meaning of friendship in young individuals – a mixed-methods investigation prior to and during the COVID-19 pandemic with three cross-sectional studies. Front Psychol. 2021;12:617267. doi: 10.3389/fpsyg.2021.617267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parekh N, Deierlein AL. Health behaviours during the coronavirus disease 2019 pandemic: implications for obesity. Public Health Nutr. 2020;23:3121–3125. doi: 10.1017/S1368980020003031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lautenbach F, Leisterer S, Walter N, Kronenberg L, Manges T, Leis O, et al. Amateur and recreational athletes’ motivation to exercise, stress, and coping during the corona crisis. Front Psychol. 2021;11:611658. doi: 10.3389/fpsyg.2020.611658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mutz M, Gerke M. Sport and exercise in times of self-quarantine: how Germans changed their behaviour at the beginning of the Covid-19 pandemic. Int Rev Sociol Sport. 2021;56:305–316. doi: 10.1177/1012690220934335. [DOI] [Google Scholar]
- 30.Saemi E, Nobari H, Badicu G, Ghazizadeh H, Pashabadi A, Imani F, et al. The impact of COVID-19 pandemic restrictions on physical activity and mental health status of Iranian people. BMC Sports Sci Med Rehabil. 2022;14:186. doi: 10.1186/s13102-022-00584-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Snyder AR, Martinez JC, Bay RC, Parsons JT, Sauers EL, McLeod TCV. Health-related quality of life differs between adolescent athletes and adolescent nonathletes. J Sport Rehabil. 2010;19:237–248. doi: 10.1123/jsr.19.3.237. [DOI] [PubMed] [Google Scholar]
- 32.Samadzadeh M, Abbasi M, Shahbazzadegan B. Comparison of sensation seeking and self-esteem with mental health in professional and amateur athletes, and non- athletes. Procedia Soc Behav Sci. 2011;15:1942–1950. doi: 10.1016/j.sbspro.2011.04.032. [DOI] [Google Scholar]
- 33.dos Santos ALP. Quality of life in professional, semiprofessional, and amateur athletes: an exploratory analysis in Brazil. SAGE Open. 2013;3:215824401349772. doi: 10.1177/2158244013497723. [DOI] [Google Scholar]
- 34.Lima Y, Denerel N, Devran S, Günver MG, Bayraktar B, Rice S. Mental health problems and risk assessment in football players infected with SARS-CoV-2: a cross-sectional study. J Sports Med Phys Fitness. 2022;62:1723–1734. doi: 10.23736/S0022-4707.22.13493-6. [DOI] [PubMed] [Google Scholar]
- 35.di Fronso S, Costa S, Montesano C, Di Gruttola F, Ciofi EG, Morgilli L, et al. The effects of COVID-19 pandemic on perceived stress and psychobiosocial states in Italian athletes. Int J Sport Exerc Psychol. 2022;20:79–91. doi: 10.1080/1612197X.2020.1802612. [DOI] [Google Scholar]
- 36.American College of Sports Medicine Academy of nutrition and dietetics, dietitians of Canada. Nutrition and athletic performance. Med Sci Sports Exerc. 2016;48:543–568. doi: 10.1249/MSS.0000000000000852. [DOI] [PubMed] [Google Scholar]
- 37.Silva IA, da Silva Santos AM, Maldonado AJ, de Moura HP, Rossi PA, Neves LM, Dos Santos MA, Machado DC, Ribeiro SL, Rossi FE. Detraining and retraining in badminton athletes following 1-year COVID-19 pandemic on psychological and physiological response. Sport Sci Health. 2022;18(4):1427–1437. doi: 10.1007/s11332-022-00939-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jeanrie C, Bertrand R. Translating tests with the international test commission’s guidelines: keeping validity in mind. Eur J Psychol Assess. 1999;15:277–283. doi: 10.1027//1015-5759.15.3.277. [DOI] [Google Scholar]
- 39.Segal-Isaacson CJ, Wylie-Rosett J, Gans KM. Validation of a short dietary assessment questionnaire: the rapid eating and activity assessment for participants short version (REAP-S) Diabetes Educ. 2004;30:774–781. doi: 10.1177/014572170403000512. [DOI] [PubMed] [Google Scholar]
- 40.Gans KM, Risica PM, Wylie-Rosett J, Ross EM, Strolla LO, McMurray J, et al. Development and evaluation of the nutrition component of the rapid eating and activity assessment for patients (REAP): a new tool for primary care providers. J Nutr Educ Behav. 2006;38:286–292. doi: 10.1016/j.jneb.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 41.Schröder H, Fitó M, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, et al. A short screener is valid for assessing mediterranean diet adherence among older Spanish men and women. J Nutr. 2011;141:1140–1145. doi: 10.3945/jn.110.135566. [DOI] [PubMed] [Google Scholar]
- 42.Kurka JM, Buman MP, Ainsworth BE. Validity of the rapid eating assessment for patients for assessing dietary patterns in NCAA athletes. J Int Soc Sports Nutr. 2014;11:42. doi: 10.1186/s12970-014-0042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaiser B, Jeannot E, Razurel C. Determinants of health behaviors after gestational diabetes mellitus: a prospective cohort study in Geneva. J Midwifery Womens Health. 2016;61:571–577. doi: 10.1111/jmwh.12486. [DOI] [PubMed] [Google Scholar]
- 44.Aceijas C, Waldhäusl S, Lambert N, Cassar S, Bello-Corassa R. Determinants of health-related lifestyles among university students. Perspect Public Health. 2017;137:227–236. doi: 10.1177/1757913916666875. [DOI] [PubMed] [Google Scholar]
- 45.Johnston CS, Bliss C, Knurick JR, Scholtz C. Rapid Eating Assessment for participants [shortened version] scores are associated with healthy eating index-2010 scores and other indices of diet quality in healthy adult omnivores and vegetarians. Nutr J. 2018;17:89. doi: 10.1186/s12937-018-0399-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mohamed HG, Fattah MA, Emara R. Relations between eating and exercise behaviors and predicted risk of cardiovascular disease (CVD) and metabolic syndrome (METS) among nurses at Alexandria main university hospital. IOSR J Nurs Health Sci. 2018;7:8–22. doi: 10.9790/1959-0705040822. [DOI] [Google Scholar]
- 47.Skinner J, Vento KA, Johnston CS, Wardenaar FC. Using nutrition knowledge and diet quality questionnaires as screening tools to identify female collegiate athletes in need of dietitian referral. Can J Diet Pract Res. 2022;83:133–138. doi: 10.3148/cjdpr-2022-004. [DOI] [PubMed] [Google Scholar]
- 48.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- 49.Szabo M, Lovibond PF. Development and psychometric properties of the DASS-Youth (DASS-Y): an extension of the depression anxiety stress scales (DASS) to adolescents and children. Front Psychol. 2022;13:e766890. doi: 10.3389/fpsyg.2022.766890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.González-Hernández J, López-Mora C, Yüce A, Nogueira-López A, Tovar-Gálvez MI. “Oh, my god! my season is over!” COVID-19 and regulation of the psychological response in Spanish high-performance athletes. Front Psychol. 2021;12:622529. doi: 10.3389/fpsyg.2021.622529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jaenes Sánchez JC, Alarcón Rubio D, Trujillo M, Peñaloza Gómez R, Mehrsafar AH, Chirico A, et al. Emotional reactions and adaptation to COVID-19 lockdown (or confinement) by Spanish competitive athletes: some lesson for the future. Front Psychol. 2021;12:621606. doi: 10.3389/fpsyg.2021.621606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Washif JA, Mujika I, DeLang MD, Brito J, Dellal A, Haugen T, et al. Training practices of football players during the early COVID-19 lockdown worldwide. Int J Sports Physiol Perform. 2023;18:37–46. doi: 10.1123/ijspp.2022-0186. [DOI] [PubMed] [Google Scholar]
- 53.Killgore WDS, Cloonan SA, Taylor EC, Dailey NS. Mental health during the first weeks of the COVID-19 pandemic in the United States. Front Psychiatry. 2021;12:561898. doi: 10.3389/fpsyt.2021.561898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lima Y, Denerel N, Öz ND, Senisik S. The psychological impact of COVID-19 infection on athletes: example of professional male football players. Sci Med Football. 2021;5:53–61. doi: 10.1080/24733938.2021.1933156. [DOI] [PubMed] [Google Scholar]
- 55.Lima Y, Rice S. Mental health symptoms and correlates among amateur football players: a cross-sectional study. Int J Environ Health Res. 2022 doi: 10.1080/09603123.2022.2112659. [DOI] [PubMed] [Google Scholar]
- 56.Lima Y, Denerel N, Devran S, Rice S, Bayraktar B. Which athletes are more vulnerable to mental health symptoms during the COVID-19 crisis? A cross-sectional study. Res Sports Med. 2022 doi: 10.1080/15438627.2022.2102917. [DOI] [PubMed] [Google Scholar]
- 57.Delmastro M, Zamariola G. Depressive symptoms in response to COVID-19 and lockdown: a cross-sectional study on the Italian population. Sci Rep. 2020;10:22457. doi: 10.1038/s41598-020-79850-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Morales-Beltrán RA, Hernández-Cruz G, González-Fimbres RA, Rangel-Colmenero BR, Zazueta-Beltrán DK, Reynoso-Sánchez LF. La actividad física como moderador en la ansiedad asociada al COVID-19 en estudiantes universitarios (Physical activity as a moderator in anxiety associated to COVID-19 in university students) Retos. 2022;45:796–806. doi: 10.47197/retos.v45i0.92974. [DOI] [Google Scholar]
- 60.Heaney S, O’Connor H, Michael S, Gifford J, Naughton G. Nutrition knowledge in athletes: a systematic review. Int J Sport Nutr Exerc Metab. 2011;21:248–261. doi: 10.1123/ijsnem.21.3.248. [DOI] [PubMed] [Google Scholar]
- 61.Karagun E, Sarper Kahveci M, Selvi S. Analysis of daily habits and nutritional attitudes of taekwondo athletes during COVID-19 pandemic. Progress Nutr. 2021;23:e2021131. doi: 10.23751/pn.v23iS1.11481. [DOI] [Google Scholar]
- 62.Taheri M, Esmaeili A, Irandoust K, Mirmoezzi M, Souissi A, Laher I, et al. Mental health, eating habits and physical activity levels of elite Iranian athletes during the COVID-19 pandemic. Sci Sports. 2023 doi: 10.1016/j.scispo.2023.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Washif JA, Mohd Kassim SFA, Lew PCF, Chong CSM, James C. Athlete’s perceptions of a “quarantine” training camp during the COVID-19 lockdown. Front Sports Act Living. 2021;2:e622858. doi: 10.3389/fspor.2020.622858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Taheri M, Irandoust K, Reynoso-Sánchez LF, Muñoz-Helú H, Cruz-Morales KN, Torres-Ramírez R, et al. Effects of home confinement on physical activity, nutrition, and sleep quality during the COVID-19 outbreak in amateur and elite athletes. Front Nutr. 2023;10:114334. doi: 10.3389/fnut.2023.1143340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Deschasaux-Tanguy M, Druesne-Pecollo N, Esseddik Y, de Edelenyi FS, Allès B, Andreeva VA, et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March–May 2020): results from the French NutriNet-Santé cohort study. Am J Clin Nutr. 2021;113:924–938. doi: 10.1093/ajcn/nqaa336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Roberts C, Gill N, Sims S. The influence of COVID-19 lockdown restrictions on perceived nutrition habits in Rugby union players. Front Nutr. 2020;7:589737. doi: 10.1093/ajcn/nqaa336. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.