Abstract
This report presents a case of malignant melanoma in a 40-year-old male who underwent resection of the tumor in his right ankle. Eleven months after the resection, a subcutaneous mass was observed on his right femur. Ultrasound examination revealed a hypoechoic tubular structure in the right thigh, with a small amount of blood flow in the lesion. Using ultrasound and fine-needle aspiration, the patient was diagnosed with metastasis and lymphovascular invasion of malignant melanoma. Treatment with an immune checkpoint inhibitor was originally scheduled, but the lesion disappeared spontaneously after the fine-needle aspiration.
Keywords: Lymphovascular invasion of malignant melanoma, Metastasis, Ultrasound, Fine-needle aspiration, Tumor regression
Introduction
Malignant melanoma is derived from melanocytes and is prone to lymph node metastasis [1]. In approximately 20% of cases, lymph node metastasis is reported with tumor diagnosis [2]. However, the frequency of lymphovascular lesions is not known. In malignant melanoma cases, ultrasound findings of lymph node metastasis are common but not lymphovascular invasion. We report a patient with lymphovascular invasion of malignant melanoma diagnosed using ultrasonographic findings and fine-needle aspiration (FNA) cytology, wherein the lesion regressed spontaneously.
Case report
A 40-year-old man with malignant melanoma underwent resection of the tumor on his right ankle. Eleven months later, a subcutaneous mass was revealed in the middle of his right femur. Ultrasound examination showed a hypoechoic tubular structure in the subcutaneous layer of the right thigh (Fig. 1). There was a small amount of blood flow in the lesion (Fig. 2), and this tubular component did not collapse on compression with the ultrasound probe. This lesion did not connect to other vessels, and a hyperechoic banded area was observed around this tubular lesion. Based on the clinical history and location of the lesion, we suspected that this lesion was the lymphovascular invasion of malignant melanoma. The FNA cytology from this lesion showed atypical spindle-shaped and/or round cells with fine brown granules, indicating the presence of melanin (Fig. 3), resulting in the diagnosis of malignant melanoma. Finally, the patient was diagnosed with metastasis and lymphovascular invasion of malignant melanoma.
Fig. 1.
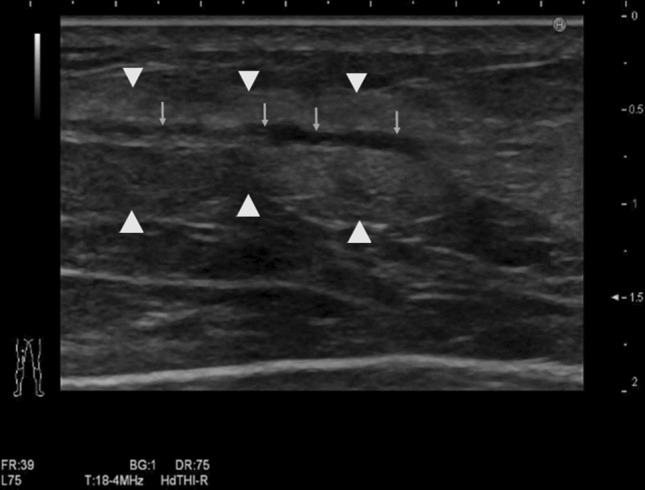
Ultrasound images of subcutaneous B-mode. The tubular structure is present in a subcutaneous layer in the right thigh (arrow). A hyperechoic banded area is observed around this tubular lesion (arrowhead)
Fig. 2.
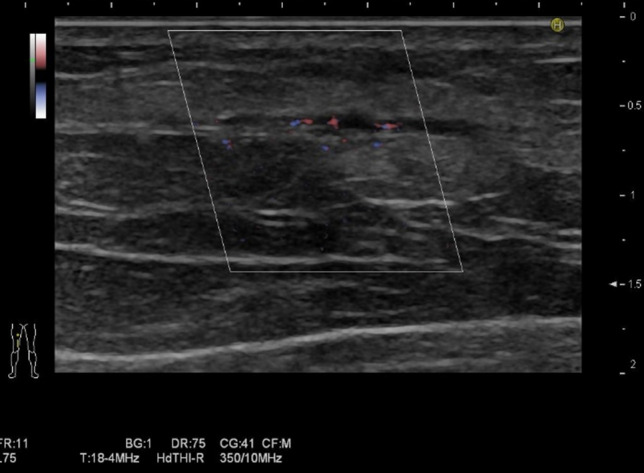
Color Doppler ultrasound images. A small amount of blood flow can be seen in the lesion
Fig. 3.
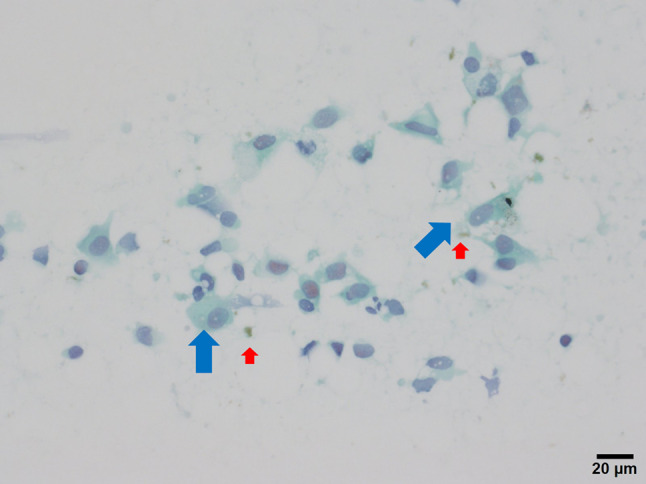
Cytological finding. Atypical melanocyte (blue arrow) with fine brown granules (red arrow), indicating the presence of melanin
The patient was treated with an immune checkpoint inhibitor as originally planned, but the lesion disappeared after FNA. Computed tomography (CT) scans performed nine days after FNA did not reveal the lesion. One month after the initial ultrasound examination, the follow-up ultrasound did not detect any tumor. The lesion was considered to have disappeared spontaneously.
Discussion
In this case, ultrasound examination revealed hypoechoic ductal structures that existed between the resected primary tumor and the associated lymph nodes. Moreover, this lesion did not collapse on compression and was not connected to other vessels. A hyperechoic banded area was observed around this tubular lesion. We diagnosed this lesion as the lymphovascular invasion of malignant melanoma based on ultrasound imaging and FNA. The hyperechoic area around this lesion was presumed to be a metastatic lesion. In the clinical course, the tumor spontaneously disappeared, as confirmed by CT and ultrasound imaging. It is estimated that 35% of spontaneous tumor regression occurs at the primary lesion of malignant melanoma [3] and 0.5% at metastatic lesions [4]. Most cases of spontaneous tumor regression occur naturally [5, 6]. However, a study reported the case of tumor regression following palliative endoscopic treatment [7]. Spontaneous regression has been proposed to be linked to tumor immunity; in particular, activated killer T cells recognize malignant melanoma-specific peptides [8]. Moreover, pathological findings reveal the replacement of tumor cells by lymphocytic inflammation [3]. In this case, inflammation could have been triggered by the puncture for FNA, leading to tumor regression. However, this cannot be confirmed, as pathological investigation was not performed.
The prognosis of malignant melanoma with tumor regression has been controversial [9]. In the present case, the patient showed no evidence of recurrence or metastasis 11 months after the initial ultrasound examination. The patient's progress should be carefully monitored in the future.
Author contributions
Ultrasound examination of the patient were performed by HK, MI, and NT. HO was responsible for the patient’s treatment. YA was responsible for pathological diagnosis. The first draft of the manuscript was written by HK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data availability statement
Data sharing is not applicable to this article as this is a case report.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Patient consent statement
Oral informed consent was obtained from the patient.
Consent to publish
The authors affirm that human research participants provided informed consent for the publication of the images in Figs. 1, 2, and 3.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dinnes J, Ferrante-di-Ruffano L, Takwoingi Y, et al. Ultrasound, CT, MRI, or PET-CT for staging and re-staging of adults with cutaneous melanoma. Cochrane Database Syst Rev. 2019;2019:CD012806. doi: 10.1002/14651858.CD012806.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakamura Y, Asai J, Igaki H, et al. Japanese Dermatological Association Guidelines: outlines of guidelines for cutaneous melanoma 2019. J Dermatol. 2020;47:89–103. doi: 10.1111/1346-8138.15151. [DOI] [PubMed] [Google Scholar]
- 3.Cartron AM, Aldana PC, Khachemoune A. Reporting regression in primary cutaneous melanoma. Part 1: history, histological criteria and pathogenesis. Clin Exp Dermatol. 2021;46:28. doi: 10.1111/ced.14328. [DOI] [PubMed] [Google Scholar]
- 4.Blessing K, McLaren KM. Histological regression in primary cutaneous melanoma: recognition, prevalence and significance. Histopathology. 1992;20:315–322. doi: 10.1111/j.1365-2559.1992.tb00988.x. [DOI] [PubMed] [Google Scholar]
- 5.Mori S, Yokota K, Ogawa A, et al. Malignant melanoma showing regression of the primary lesion. Pract Dermatol. 2016;38:515. [Google Scholar]
- 6.Horaguchi Y, Maeda F, Takahashi K, Akasaka T. (2016) A cutaneous malignant melanoma showing a partially regression tendency associated with pulmonary metastasis. Jpn J Clin Dermatol. 2006;60:1133. [Google Scholar]
- 7.Tanaka M, Ohira T, Harada Y, et al. (2019) Primary malignant melanoma of the esophagus with spontaneous erosion after palliative endoscopic treatment. Stomach Intest. 2019;54:1434. [Google Scholar]
- 8.Gualano MR, Osella-Abate S, Scaioli G, Marra E, Bert F, Faure E, Baduel ES, Balagna E, Quaglino P, Fierro MT, Siliquini R, Ribero S. Prognostic role of histological regression in primary cutaneous melanoma: a systematic review and meta-analysis. Br J Dermatol. 2018;178:357–362. doi: 10.1111/bjd.15552. [DOI] [PubMed] [Google Scholar]
- 9.Cartron AM, Aldana PC, Khachemoune A. Reporting regression in primary cutaneous melanoma. Part 2: prognosis, evaluation and management. Clin Exp Dermatol. 2020;45:818. doi: 10.1111/ced.14329. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as this is a case report.


