Abstract
ITGCs (intratendinous ganglion cysts) involving the flexor compartment of the wrist are uncommon, and reports are scarce in the literature. The differential diagnosis is wide and can mimic sinister lesions. We report a case of a 62-year-old male, that presented to our tertiary orthopaedic oncology service with an intratendinous ganglion cyst, extending into the muscle belly of flexor carpi radialis. We describe this rare presentation and review the literature.
Keywords: Intratendinous ganglion cysts, Wrist Joint, Flexor tendons
Background
Ganglion cysts (GCs) are the most common benign soft tissue tumours affecting the hand and wrist, accounting for approximately 50–70% of all upper limb lesions [1]. They most frequently arise between the 2nd and 4th decades of life, with a predilection for females [1]. GCs has classically been classified according to their site of origin arising from bone, joint, adjacent soft tissues or tendon sheaths [2, 3]. Intratendinous ganglion cysts (ITGC) are rare lesions, and in the wrist most often develop on the dorsal aspect of the wrist joint involving the extensor tendons [4–14]. Volar ITGC involving flexor tendons are less common with a limited number of case reports in the literature [14, 15].
We present the first case of an ITGC involving the flexor carpi radialis tendon (FCR) extending into its muscle belly.
Case report
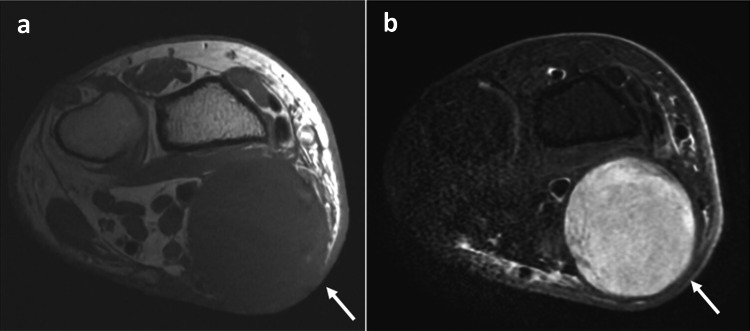
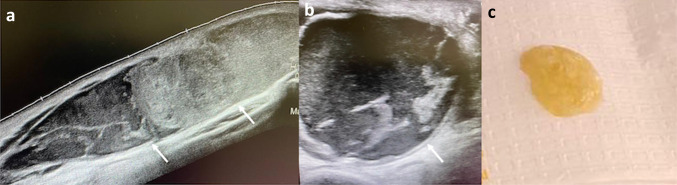
A 62-year-old, right hand dominant male, was referred to our tertiary orthopaedic oncology service with a 6-month history of a volar painless, progressively enlarging firm palpable mass, overlying the volar aspect of the wrist across the FCR tendon. There was no history of trauma or recent surgery. On clinical examination, there was a large painless volar lump with redness of the overlying skin. The lump was intimately related to the flexor tendons. Tinel’s test was negative. MRI was organised to evaluate this further. This revealed a large (8 cm × 2.5 cm × 2.6 cm) lobulated lesion within the tendon and muscle bulk of FCR. This was low signal on T1 and high on fluid sensitive sequences. (Figs. 1, 2) There was no communication of the cyst with the radiocarpal joint. The rest of the tendons and muscles were normal. The median nerve and superficial branch of the radial nerve were normal. A differential diagnosis of ganglion and neurogenic tumour was considered. Ultrasound was performed to evaluate this further. This revealed a mixed echoic 8 cm × 2.5 cm × 2.5 cm lesion within the FCR tendon and muscle belly. There was no increased signal on Doppler. An ultrasound guided aspiration was performed which revealed thick viscous fluid compatible with a ganglion. (Fig. 3) He was managed with surgical debridement/excision of ganglion.
Fig. 1.
Sagittal T1 (a) and STIR (b) showing large lobulated ganglion within the tendon and muscle belly of FCR (arrow)
Fig. 2.
Axial T1 (a) and STIR (b) showing large lobulated ganglion within the tendon and muscle belly of FCR (arrow)
Fig. 3.
Longitudinal (a) and short axis (b) ultrasound images showing large ganglion within the FCR. Image c showing thick viscous fluid aspirated from the ganglion consistent with a ganglion
Discussion
ITGCs involving the flexor compartment of the hand are uncommon, and scarce in the literature [14, 15]. As far as the authors are aware, this is the first reported case of an FCR ITGC, with extension into its muscle belly. GCs are histologically characterised by the formation of a cystic wall enveloping loose fibrous connective tissue, mucopolysaccharides and hyaluronic acid [2]. Their pathogenesis is poorly understood [15], with several underlying theories reported in the literature. These include synovial tissue invasion of tendon, mucoid degeneration, forming fluid filled cavities within tendons [8–10, 15]. Although the aetiology of ITGC is unclear, a history of trauma or overuse is considered a contributing cause, elicited in up to 10% of all cases [16]. This may be secondary to cystic degeneration or tenosynovitis, which are often found seen around GCs. Our patient had no reported history of trauma or any clinical evidence of tenosynovitis.
Although benign, ITGCs can be locally aggressive and present with features similar to that of typical GCs, with a myriad of non-specific symptoms, depending on their size and location they arise from [14]. Smaller lesions can be indolent and difficult to diagnose. Only when the lesion is large enough to be noticed, a clinical diagnosis can be made [14, 15]. Physical examination is therefore critical to further distinguish the location of such lesions; by contracting the specific tendon affected, where movement of the lesion can often be noted [15]. Despite this, the differential diagnosis can be wide, and one should consider other sinister lesions. Differential diagnosis includes soft tissue sarcomas, neurogenic tumours, giant cell tumours of tendon sheath, myxomas and tenosynovitis [17–20].
Imaging plays an important role in characterising ITGCs. In general, features may mimic that of other typical GCs, and can be easily identified on USS. These features represent a lesion with anechoic to hypoechoic signals with well-defined margins and partial internal septations [21]. Given that ITGCs are rare, often MRI is warranted to further delineate these lesions and rule out other sinister lesions. Typically, on T1 MRI sequence, a well-defined lobulated mass is displayed, with either hypointense, isointense or hyperintense signal. On T2W sequence, these demonstrate high signal intensity. ITGC demonstrate peripheral wall (septal) enhancement with a thin surrounding rim on post contrast imaging [22].
The management of ITGCs is dependent on the severity of the symptoms. Most typical GC can be managed conservatively in contrast to ITGCs often requiring surgical resection [23, 24]. In contrast to typical GCs, ITGC surgical resection can be challenging, and is almost always associated with a partial tear of the affected tendon [25]. Therefore, it is essential surgeons undertake careful dissection and repair of the involved tendon, with close long-term monitoring, to reduce the risk of post-operative tenosynovitis, adhesions and recurrence [25].
Conclusion
ITGCs affecting the volar aspect of the upper limb are rare. Differential diagnosis is wide and can mimic that of more sinister lesions. Radiologists need to be aware of such lesions to initiate appropriate diagnosis and aid management. From a surgical point of view, given the location of these lesions, it is imperative to adequately prepare and consent these patients for reconstructive surgery.
Funding
No funding to declare.
Data availability
The data that support the findings of this study are available from the corresponding author, [RB], upon reasonable request.
Declarations
Conflict of interest
No conflict of interest to declare.
Informed consent
Consent was obtained from the patient.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Thornburg L. Ganglions of the hand and wrist. J Am Acad Orthop Surg. 1999;7(4):231–238. doi: 10.5435/00124635-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Head L, Gencarelli JR, Allen M, et al. Wrist ganglion treatment: systematic review and meta-analysis. J Hand Surg Am. 2015;40(3):546–553. doi: 10.1016/j.jhsa.2014.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Kim SK, Park JM, Choi JE, Rhee SK, Shim SI. Intratendinous ganglion cyst of the semimembranosus tendon. Br J Radiol. 2010;83(988):e79–82. doi: 10.1259/bjr/23178227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calandruccio JH, Jobe MT. Tumors and tumorous conditions of the hand. In: Azar FM, Beaty JH, Canale ST, editors. Campbell's operative orthopaedics. 13. Philadelphia: Elsevier; 2016. pp. 3661–3692. [Google Scholar]
- 5.Mavrogenis AF, Panagopoulos GN, Angelini A, et al. Tumors of the hand. Eur J Orthop Surg Traumatol. 2017;27(6):747–762. doi: 10.1007/s00590-017-1984-y. [DOI] [PubMed] [Google Scholar]
- 6.Rayan GM. Intratendinous ganglion. A case report. Orthop Rev. 1989;18:449–451. [PubMed] [Google Scholar]
- 7.Ikeda K, Tomita K, Matsumoto H. Intratendinous ganglion in the extensor tendon of a finger: a case report. J Orthop Surg (Hong Kong) 2001;9:63–65. doi: 10.1177/230949900100900213. [DOI] [PubMed] [Google Scholar]
- 8.Young SC, Freiberg A. A case of an intratendinous ganglion. J Hand Surg Am. 1985;10:723–724. doi: 10.1016/S0363-5023(85)80218-5. [DOI] [PubMed] [Google Scholar]
- 9.Seidman GD, Margles SW. Intratendinous ganglia of the hand. J Hand Surg Am. 1993;18:707–710. doi: 10.1016/0363-5023(93)90323-U. [DOI] [PubMed] [Google Scholar]
- 10.Botchu R, Bharath A, Uhiara O, Davies M, James S. Iatrogenic intratendinous ganglion cyst of the extensor digitorum tendon following intravenous cannulation. J Ultrasound. 2018;21(4):329–331. doi: 10.1007/s40477-017-0275-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chew EM, Yam AKT, Tay SC. Simultaneous intratendinous ganglion and synovial cyst of the wrist. J Hand Surg Eur Vol. 2010;35(1):80–81. doi: 10.1177/1753193409348878. [DOI] [PubMed] [Google Scholar]
- 12.Lee HJ, Kim PT, Chang HW. Intratendinous ganglion of the extensor tendon of the hand. Hand Surg. 2015;20(2):316–318. doi: 10.1142/S0218810415720132. [DOI] [PubMed] [Google Scholar]
- 13.Satonaka H, Tsujii M, Sudo A. Tenosynovitis of the extensor pollicis longus tendon caused by an intratendinous ganglion: a case report. J Hand Surg (Eur Vol) 2014;39(6):669–671. doi: 10.1177/1753193412453428. [DOI] [PubMed] [Google Scholar]
- 14.Senda H, Mizutani J, Okamoto H. Intratendinous ganglion of the hand: two case reports occurring in the extensor digitorum communis and the flexor digitorum superficialis tendon. Case Rep Plast Surg Hand Surg. 2017;4(1):9–12. doi: 10.1080/23320885.2016.1278170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chia DS, Kong JC, Teoh LC. An atypical presentation of a flexor intratendinous ganglion of the hand. Ann Plast Surg. 2015;74:306–307. doi: 10.1097/SAP.0b013e31829ba9c5. [DOI] [PubMed] [Google Scholar]
- 16.Meena S, Gupta A. Dorsal wrist ganglion: current review of literature. J Clin Orthop Trauma. 2014;5(2):59. doi: 10.1016/j.jcot.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Young SC, Freiberg A. A case of an intratendinous ganglion. J Hand Surg. 1985;10(5):723–724. doi: 10.1016/S0363-5023(85)80218-5. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy CL, McNally EG. The MRI appearance of cystic lesions around the knee. Skeletal Radiol. 2004;33:187–209. doi: 10.1007/s00256-003-0741-y. [DOI] [PubMed] [Google Scholar]
- 19.Costa CR, Morrison WB, Carrino JA, Raiken SM. MRI of an intratendinous ganglion cyst of the peroneus brevis tendon. AJR Am J Roentgenol. 2003;181:890–891. doi: 10.2214/ajr.181.3.1810890. [DOI] [PubMed] [Google Scholar]
- 20.Kishimoto K, Akisue T, Fujimoto T, Kawamoto T, Hara H, Hitora T, et al. Intra-tendinous ganglion in the long head of the biceps humeri. Skeletal Radiol. 2008;37:263–265. doi: 10.1007/s00256-007-0418-z. [DOI] [PubMed] [Google Scholar]
- 21.Teefey S, Dahiya N, Middleton W, Gelberman R, Boyer M. Ganglia of the hand and wrist: a sonographic analysis. AJR Am J Roentgenol. 2008;191(3):716–720. doi: 10.2214/AJR.07.3438. [DOI] [PubMed] [Google Scholar]
- 22.Bermejo A, De Bustamante T, Martinez A, Carrera R, Zabía E, Manjón P. MR imaging in the evaluation of cystic-appearing soft-tissue masses of the extremities. Radiographics. 2013;33(3):833–855. doi: 10.1148/rg.333115062. [DOI] [PubMed] [Google Scholar]
- 23.Langford K, Rahmi H. Surgical management of an intratendinous ganglion cyst of the long head of the biceps brachii: a case report. JESES. 2022;16(8):550–553. doi: 10.1016/j.xrrt.2022.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Athanasian EA. Green’s operative hand surgery. 6. New York: Churchill Livingstone; 2010. Bone and soft tissue tumors; pp. 2150–2166. [Google Scholar]
- 25.Chalidis B, Kitridis D, Dimitriou C, Givissis P. Intratendinous ganglion cyst of the hand: a case report and review of the literature. Case Rep Orthop. 2020;14(2020):8847563. doi: 10.1155/2020/8847563. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, [RB], upon reasonable request.