Abstract
The objective of this study was to evaluate the intra- and inter-rater reliability and agreement between conditions with and without a special device (SD) in the evaluation of the patellar tendon (PT) cross-sectional area (CSA). Forty trained adult volunteers participated in the study. With the knee positioned at 90°, the ultrasound probe was placed in the transverse plane at 25, 50, and 75% of the PT length. Two raters and one analyzer obtained the images. We use a two-way ANOVA with a significance level of α = 0.05. No significant differences were found between raters or conditions. Intra-rater reliability ranged from moderate to good. Inter-rater reliability without the SD ranged from low to good, improving from moderate to good when the SD was used. Evaluation of the PT ends showed a lower coefficient of variation with the SD. We observed a moderate correlation at the ends and a strong correlation in the middle between conditions. The mean difference in the three positions is small (~ 0.013 cm2/ ~ 1.7%) with an upper limit of 43.2% and a lower limit of 32.5%. Therefore, we conclude that the use of the SD can be employed for evaluating the PT ends, while for the central region, it becomes optional.
Supplementary Information
The online version supplementary material available at 10.1007/s40477-023-00829-w.
Keywords: Tendon morphology, Reproducibility, Tendon, Knee, Intra-rater, Inter-rater
Introduction
The patellar tendon transmits the force produced by the quadriceps muscle during contraction to the tibia, generating a moment around the knee joint [1]. Due to its crucial role in human locomotion, high and continuous loads are imposed on the patellar tendon during daily activities as well as during sports activities [1]. Therefore, the evaluation and analysis of the patellar tendon’s cross-sectional area (CSA) are frequently used in studies to identify changes resulting from exercises or injuries.
The hypertrophy of the patellar tendon (observed through CSA) after increased load requires highly precise measures to be detected [1]. Intervention studies have shown an increase in CSA of the patellar tendon by 4–7% following strength training [2, 3]. However, there is also evidence indicating that the CSA of the tendon remained unchanged after training [4]. These observed differences in CSA of the patellar tendon between groups varied from 4 to 13% across different age ranges [5], 22–36% between genders [5, 6], and approximately 7% between trained and untrained subjects [6]. In other words, the differences in CSA of the patellar tendon among these groups are smaller than the variation caused by ultrasound analysis (37–55%), and therefore may not be detected.
Ultrasound is an economically accessible and easy-to-use device that has been frequently used to measure the patellar tendon CSA. Ultrasound has advantages that include high axial resolution, short testing time, real-time image capture, absence of ionizing radiation, wide availability, and relatively low cost [7, 8]. However, the main technical limitation of ultrasound is related to the dependence on the perception of raters and analyzers, which can lead to measurement errors and inadequate interpretation of results [7, 9, 10]. Small changes or displacements resulting from probe placement, as well as different pressures or orientations of the transducer, can significantly influence image acquisition [11]. Additionally, there are inevitably some artifacts and blurred areas in the images. During patellar tendon assessment, it is crucial to avoid excessive pressure application on the transducer to prevent subcutaneous fluid displacement, a significant issue with the technique's application by the rater [12]. The low clarity of ultrasound images results in ambiguous accuracy of the measured CSA.
To assess the reliability of the conditions, several approaches have been described in the literature. Intra-rater reliability compares the data collected by the same rater at different time points [13, 14]. Inter-rater reliability compares the data collected by different raters (up to three distinct raters) on the same day [15]. Inter-analyst reliability compares the analysis performed by different analysts, using images regardless of who collected them [16]. A previous study evaluated the overall reliability of the assessment of the patellar tendon's CSA and obtained combined values of intraclass correlation coefficient (ICC) between raters and analysts. The results showed that the ICC ranged from 0.58 to 0.92, with a standard error of measurement ranging from 3.33 to 7.39% [17].
Regarding the raters, Gellhorn and Carlson found high levels of inter- and intra-rater reliability (ICC > 0.87) [7]. However, regarding the analyzers, Ekizos et al. identified low reliability of the method for assessing CSA (ICC = 0.59), regardless of the position (proximal, central, or distal), affected by technical limitations of ultrasound (unclear image of the bilateral and deep boundaries of the patellar tendon) [1]. On the other hand, Mc Auliffe et al. through a systematic literature review, identified that overall intra-analyzer ICC values (0.59–0.99) were slightly higher than inter-analyzer values (0.45–0.99) [17]. There seems to be lower reliability for the analyzers than the raters. This is justified due to the difficulty in observing and identifying the edges of the patellar tendon, which increases measurement error and consequently makes it more challenging to observe the effects of an intervention program.
In this way, devices that aim to improve the image quality obtained by ultrasound and facilitate assessment are essential in both clinical and scientific environments. However, the lack of studies on device reliability hinders results comparison and highlights the need for a common reproducible methodology for applied research. Although Ekizos et al. used a gel pad for patellar tendon evaluation, there was no comparison between conditions (with and without the gel pad) with many details [1]. Based on this, we present a proposed device to enhance the image quality of the Achilles tendon obtained by ultrasound. The device makes it possible to enlarge the obtained image, allowing for a quick and easy marking of the patellar tendon edges during the analysis of the Achilles tendon. However, it is unknown whether this will affect the reliability of the patellar tendon's Achilles tendon thickness measurement.
The determination of reliability and measurement error in the assessment and analysis of the morphological properties of the patellar tendon, as well as tissue adaptations under increased or decreased use conditions, is of fundamental importance. Therefore, the present study aims to evaluate intra- and inter-rater reliability and agreement between conditions with and without a special device for assessing the patellar tendon's CSA. We hypothesize that there will be high reliability in both intra- and inter-rater.
Material and methods
Forty physically active volunteers, both men and women, aged between 18 and 50 years (30.35 ± 8.62 years), participated in the study. The selection of study volunteers was non-probabilistic (non-random) and intentional. The inclusion and exclusion criteria for the study were as follows: no musculoskeletal injuries in the lower limbs in the past 12 months, no previous knee pain, and no training in the past 24 h. Prior to data collection, all volunteers were informed about the procedures and signed the informed consent form. The study was approved by the local Research Ethics Committee for Human Subjects (Approval: 2.695.031).
The evaluation protocols were conducted at the biomechanics laboratory of the institution where the project was approved. All ultrasound evaluations were performed by two independent raters (2 years of experience = more experienced; 6 months = beginner). Standard operating procedures were developed to systematize the data collection procedures among the assessors [18]. All data collection was carried out over 40 days. The assessors underwent a two-month training in measurement techniques before the study. The images were analyzed by a researcher with expertise in the analysis procedure (3 years).
The participants were positioned sitting on a stretcher with the hip and knee joints fixed at 90° (considered full extension as 180°). The patellar tendon was visualized using a 50 mm linear probe (6–15 MHz linear array) connected to an ultrasound system (LOGIC S7 Expert model, General Electric, USA). A conductive gel (colorless conductive gel, RMC Gel Clínico Ltda) was used for the acoustic coupling of the transducer.
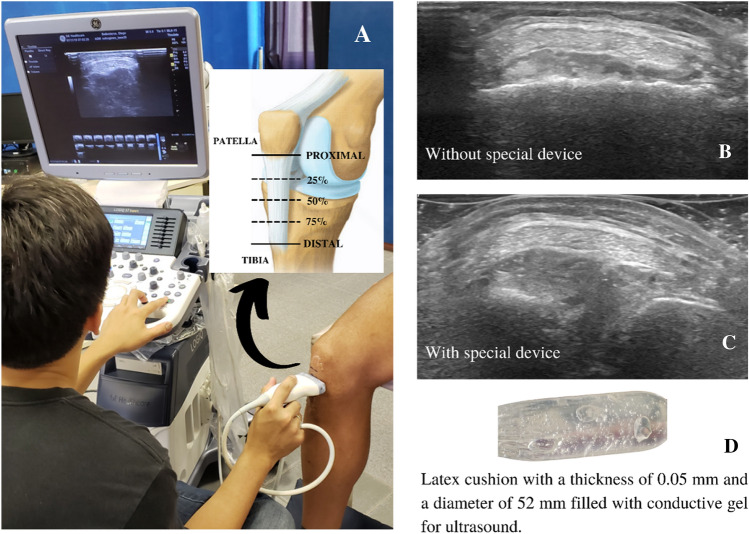
In the present study, three anatomical points (proximal, medial, and distal) were selected and identified to provide representative information about the Patellar Tendon's Achilles Tendon (Fig. 1). Internal structures (patella and tibia) were used to standardize and control the experimental procedure. The proximal and distal edges of the patellar tendon were identified using palpation methods and marked with a skin pen. The proximal edge is considered the lower region of the patella, and the distal edge is located above the tibia bone (Fig. 1). The measurement of the total length was taken, and then measurements were calculated for 25% (proximal), 50% (medial), and 75% (distal) of the location where the tests will be performed. Three attempts were made in each of the positions, totaling nine attempts for each rater. The evaluation was done randomly, removing and repositioning the probe for each test. The order of the raters was also randomized.
Fig. 1.
Schematic drawing of data collection (A) and images without (B) and with (C) the special device (D)
For each attempt, the probe was placed perpendicular to the tendon (transverse plane) to examine the patellar tendon CSA. The evaluations were performed with and without the 0.05 mm thick latex pad with a diameter of 52 mm filled with ultrasound conductive gel. All captured videos were converted into images (frame by frame), and in each video, the image with the best tendon visibility was selected for further scanning. The ultrasound videos captured from all 36 examined trials—three trials in each of the three positions for rater 1 and rater 2, and under both conditions with and without the special device—from each participant were analyzed by an analyzer. During the analysis, the analyzer was blinded to the raters and the condition (with or without the special device). The scanning of CSA was manually performed using image processing software (ImageJ 1.52v, Wayne Rasband National Institutes of Health, USA). The analyzer performed a 4-month training.
The statistical analysis was conducted using SPSS 22.0 software. All data were presented as mean and standard deviation (SD). Data normality was assessed using the Shapiro–Wilk test. A two-way ANOVA (rater vs. condition) was performed to examine differences between raters and between conditions (with and without a special device) for each patellar tendon CSA length (25%, 50%, and 75%). Additionally, to assess intra-rater reliability (same rater in two conditions), the ICC was calculated. Furthermore, to determine inter-rater reliability with and without the special device (different raters in the same condition) for each patellar tendon CSA length (25%, 50%, and 75%), the ICC, confidence interval (CI), standard error of measurement (SEM), minimal detectable change (MDC), and coefficient of variation (CV) were calculated.
The ICC values were classified according to the literature [19] as very low (< 0.20), low (0.21–0.40), moderate (0.41–0.60), good (0.61–0.80), and excellent (0.81–1.00). The SEM was estimated using the following equation: SEM = SD∙√1 − ICC, where SD is the standard deviation of the measurements. The MDC was estimated based on a 95% confidence interval, where MDC = 1.96∙SEM. The coefficient of variation was calculated using the equation: CV = SD/X∙100, where X is the mean value. To assess the agreement between the conditions, Bland–Altman plots were used to illustrate the correlation between the measurements of the conditions at different lengths of the patellar tendon. A significance level of 5% was adopted for all analyses.
Results
Our results showed that there was no significant difference in the measurement of the patellar tendon between the raters and between the conditions (with and without the special device) (Table 1) for the three assessment sites (25%, 50%, and 75%). Despite the lack of significant differences, rater 1 presented “low” reliability for CSA at 25% (CSA25%) and “good” reliability for CSA at 50% (CSA50%) and CSA at 75% (CSA75%), while rater 2 presented “moderate” reliability for CSA25% and “good” reliability for CSA50% and CSA75%.
Table 1.
Mean and standard deviation (SD) values of the cross-sectional area (CSA) measurements of the patellar tendon acquired under different conditions (with and without the special device) and by two different assessors
| Rater 1 | Rater 2 | |||||
|---|---|---|---|---|---|---|
| Without device (Mean ± SD) | With device (Mean ± SD) | ICC | Without device (Mean ± SD) | With device (Mean ± SD) | ICC | |
| CSA25% (cm2) | 0.787 ± 0.166 | 0.794 ± 0.210 | –0.35 | 0.799 ± 0.195 | 0.841 ± 0.216 | 0.41 |
| CSA50% (cm2) | 0.790 ± 0.156 | 0.778 ± 0.191 | 0.70 | 0.794 ± 0.163 | 0.837 ± 0.169 | 0.79 |
| CSA75% (cm2) | 0.776 ± 0.159 | 0.775 ± 0.175 | 0.63 | 0.783 ± 0.197 | 0.786 ± 0.163 | 0.62 |
ICC intraclass correlation coefficient
In Table 2, it is possible to observe that the inter-rater evaluation without the special device shows “low” reliability for CSA25% (ICC = 0.36), “good” for CSA50% (ICC = 0.65), and “moderate” for CSA75% (ICC = 0.47). However, in the evaluations with the special device, an improvement in reliability is observed with “moderate” and “good” ICC values. The inter-rater evaluation with the special device showed “moderate” reliability for CSA25% (ICC = 0.46) and “good” for CSA50% (ICC = 0.65) and CSA75% (ICC = 0.73). It is also worth noting that for the evaluation of the extremities (CSA25% and CSA75%), the results showed a lower coefficient of variation when the special device was used.
Table 2.
Mean values and standard deviation (SD), intraclass correlation coefficient (ICC), 95% confidence interval (95% CI), standard error of measurement (SEM), minimal detectable change (MDC), and coefficient of variation (CV) for inter-rater measurements of the cross-sectional area (CSA) of the Patellar Tendon
| Mean ± SD (cm2) | ICC | 95% CI | p value | SEM (cm2) | MDC (cm2) | CV (%) | |
|---|---|---|---|---|---|---|---|
| Inter-rater–without device | |||||||
| CSA25% | 0.793 ± 0.181 | 0.36 | 0.11–0.58 | 0.02 | 0.14 | 0.40 | 22.65 |
| CSA50% | 0.792 ± 0.160 | 0.65 | 0.47–0.78 | < 0.001 | 0.09 | 0.26 | 13.10 |
| CSA75% | 0.780 ± 0.179 | 0.47 | 0.25–0.66 | < 0.001 | 0.13 | 0.36 | 20.96 |
| Inter-rater–with device | |||||||
| CSA25% | 0.817 ± 0.213 | 0.46 | 0.21–0.64 | < 0.001 | 0.15 | 0.43 | 12.64 |
| CSA50% | 0.807 ± 0.180 | 0.65 | 0.47–0.78 | < 0.001 | 0.10 | 0.29 | 14.44 |
| CSA75% | 0.780 ± 0.169 | 0.73 | 0.58–0.83 | < 0.001 | 0.08 | 0.34 | 12.64 |
The SEM between raters ranged from 10.3% to 18.4% in each condition (respectively without and with the special device) for the three locations (CSA25% = 17.7%; 18.4%; CSA50% = 11.4%; 12.4%; CSA75% = 16.7%; 10.3%). The ICC between raters ranged from 32.8% to 52.6% in each condition (respectively without and with the special device) for the three locations (CSA25% = 50.4% and 54.2%; CSA50% = 32.8% and 36.6%; CSA75% = 45.4% and 42.9%).
In Fig. 2, we observe a moderate correlation at the edges (CSA25% and CSA75%) and a strong correlation in the middle (CSA50%) between the conditions with and without the special device. It is worth noting that the average difference in the three positions is small (~ 0.013 cm2 / ~ 1.7%).
Fig. 2.
Scatter plots (1) and Bland–Altman plots (2) compare cross-sectional area (CSA) at 25% (A), 50% (B), and 75% (C) of Patellar Tendon length with and without the special device. UL upper limit; LL lower limit
Discussion
Implementations aimed at improving image quality are important for both clinical and scientific environments. With that in mind, we propose a special device that aims to enhance the image of the patellar tendon during CSA (Articular Surface Tension) analysis using ultrasound, allowing for an enlarged image that facilitates marking the tendon's edges. Therefore, the main objective of this study was to evaluate the intra- and inter-rater reliability and agreement between conditions, with and without the special device, for evaluating the patellar tendon's CSA.
Ultrasound has many advantages, however, its main technical limitation is related to the dependence on the perception and experience of the raters and analysts [7, 9, 10]. Ultrasound analysis is rater-dependent, so operators who follow the same protocol but have different levels of experience can lead to significant variations in the obtained image [20]. Small changes in the probe placement, as well as different pressures or orientations of the transducer, can significantly influence image acquisition [11]. When comparing an experienced rater and a novice one, our results show satisfactory reliability (Table 1), but with values below those reported in the literature (ICC > 0.87) [7]. Our values may have been influenced by the analyzer, which in the literature presents lower ICC values, representing a limitation of our study in terms of the lack of verification of inter- and intra-examiner reliability.
Previous studies have shown that patellar tendon assessment has moderate reliability (ICC = 0.59), even with a gel pad, with a significant difference between assessments conducted on different days and with a significant effect of the analyzer [1]. The authors also found low reliability in the three examined positions. On the other hand, our results (Table 2) demonstrate that it is possible to observe that inter-rater assessment without the special device shows “low” reliability for CSA25%, “good” reliability for CSA50%, and “moderate” reliability for CSA75%. However, in assessments with the special device, an improvement in reliability is observed with “moderate” and “good” ICC. The inter-rater assessment with the special device showed “moderate” reliability for CSA25% and “good” reliability for CSA50% and CSA75%. We also highlight that for the assessment of the extremes (CSA25% and CSA75%), the results demonstrated a lower coefficient of variation when the special device was used.
The SEM between raters ranged from 10.3 to 18.4% for each condition (without and with the special device) across the three locations, demonstrating a relatively high error regardless of the condition used. The ICC between raters ranged from 32.8 to 52.6% for each condition (without and with the special device) across the three locations. Similar values were observed between the conditions, leading us to believe that the use of the device does not have a negative influence, and its utilization is recommended as it facilitates the visualization of tendon edges. However, further studies are needed to evaluate the influence of the special device on the examiner.
Our findings highlight that the assessment of Patellar Tendon CSA (Arch and Strain Threshold) requires careful interpretation of its results due to the high variability in the reliability of the obtained outcomes. To facilitate data analysis and reduce measurement errors, we propose the use of a special device, a latex pad, with a thickness of 0.05 mm and a diameter of 52 mm, filled with ultrasound-conductive gel. A moderate correlation was observed at the ends (CSA25% and CSA75%), and a strong correlation in the middle (CSA50%), between the conditions with and without the special device. Additionally, the average difference in the three positions is small (~ 0.013 cm2 / ~ 1.7%). Given the similar results between the conditions, we recommend using the special device to evaluate the tendon's ends, while its use in the central region may be optional.
Clinicians and training professionals should pay attention to the MDC values when interpreting the results of a clinical trial that employs CSA with a special device for the patellar tendon. Although excellent reliability was not observed, ultrasound remains a cost-effective evaluation method for both clinical practice and scientific research. Therefore, it is important to develop methods to minimize measurement errors associated with this equipment. It would have been ideal to scan each subject's tendon on two different occasions to limit bias, but we were unable to do this given the time constraints of our subjects. Another point is interesting to add another analyzer. This could lead to greater reliability.
We concluded that the low reliability of the method was not influenced by the position (25%, 50%, or 75%), but it is affected by the technical limitations of ultrasound. Specifically, the low visibility caused using ultrasound affects the identification of the boundaries of the patellar tendon. In this sense, the use of the special device evaluated in this study is recommended both in clinical practice and in scientific research, as it demonstrated a higher reliability of CSA measurement at the ends of the patellar tendon (25% and 75%). In addition, the Patellar tendon might need a longer training period by different raters and analyzers to increase reliability.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES)-Finance Code 001 and the National Council of Scientific Research (CNPq) Brazil.
Author contrbutions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ML, RLS, FEF, FCS and LTS. The first draft of the manuscript was written by ML and FEF and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Declarations
Conflict of interest
The authors have not disclosed any competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ekizos A, Papatzika F, Charcharis G, Bohm S, Mersmann F, Arampatzis A. Ultrasound does not provide reliable results for the measurement of the patellar tendon cross sectional area. J Electromyogr Kinesiol. 2013;23(6):1278–1282. doi: 10.1016/j.jelekin.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Kongsgaard M, Reitelseder S, Pedersen TG, Holm L, Aagaard P, Kjaer M, et al. Region specific patellar tendon hypertrophy in humans following resistance training. Acta Physiol. 2007;191(2):111–121. doi: 10.1111/j.1748-1716.2007.01714.x. [DOI] [PubMed] [Google Scholar]
- 3.Seynnes OR, Erskine RM, Maganaris CN, Longo S, Simoneau EM, Grosset JF, et al. Training-induced changes in structural and mechanical properties of the patellar tendon are related to muscle hypertrophy but not to strength gains. J Appl Physiol. 2009;107(2):523–530. doi: 10.1152/japplphysiol.00213.2009. [DOI] [PubMed] [Google Scholar]
- 4.Reeves ND, Maganaris CN, Narici MV. Effect of strength training on human patella tendon mechanical properties of older individuals. J Physiol-Lond. 2003;548(3):971–981. doi: 10.1113/jphysiol.2002.035576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carroll CC, Dickinson JM, Haus JM, Lee GA, Hollon CJ, Aagaard P, et al. Influence of aging on the in vivo properties of human patellar tendon. J Appl Physiol. 2008;105(6):1907–1915. doi: 10.1152/japplphysiol.00059.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Westh E, Kongsgaard M, Bojsen-Moller J, Aagaard P, Hansen M, Kjaer M, et al. Effect of habitual exercise on the structural and mechanical properties of human tendon, in vivo, in men and women. Scand J Med Sci Sports. 2008;18(1):23–30. doi: 10.1111/j.1600-0838.2007.00638.x. [DOI] [PubMed] [Google Scholar]
- 7.Gellhorn AC, Carlson MJ. Inter-rater, intra-rater, and inter-machine reliability of quantitative ultrasound measurements of the patellar tendon. Ultrasound Med Biol. 2013;39(5):791–796. doi: 10.1016/j.ultrasmedbio.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Weinreb JH, Sheth C, Apostolakos J, Mccarthy M, Barden B, Cote MP, et al. Tendon structure, disease, and imaging. Muscles Ligaments Tendons J. 2014;4(1):66–73. doi: 10.32098/mltj.01.2014.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’connor PJ, Grainger AJ, Morgan SR, Smith KL, Smith KL, Waterton JC, Nash AFP. Ultrasound assessment of tendons in asymptomatic volunteers: a study of reproducibility. Eur Radiol. 2004;14(11):1968–1973. doi: 10.1007/s00330-004-2448-4. [DOI] [PubMed] [Google Scholar]
- 10.Skou ST, Aalkjaer JM. Ultrasonographic measurement of patellar tendon thickness—a study of intra- and interobserver reliability. Clin Imaging. 2013;37(5):934–937. doi: 10.1016/j.clinimag.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Castro J, Carvalho KL, Silva PE, Fachin-Martins E, Babault N, Marqueti RC, et al. Intra- and inter-rater reproducibility of ultrasound imaging of patellar and quadriceps tendons in critically ill patients. PLoS ONE. 2019;14(6):1–15. doi: 10.1371/journal.pone.0219057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alves TI, Girish G, Kalume Brigido M, Jacobson JA. US of the knee: scanning techniques, pitfalls, and pathologic conditions. Radiographics. 2016;36(6):1759–1775. doi: 10.1148/rg.2016160019. [DOI] [PubMed] [Google Scholar]
- 13.Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101–110. doi: 10.1002/(sici)1097-0258(19980115)17:1<101::aid-sim727>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 14.VIM . International vocabulary of metrology: basic and general concepts and associated terms. 3. Joint Committee for Guides in Metrology; 2012. [Google Scholar]
- 15.Sedrez JA, Candotti CT, Rosa MIZ, Medeiros FS, Marques MT, Los JF. Assessment of Vert-3D repeatability and reproducibility for evaluating the scoliosis of children with different nutritional profiles. Fisioter Mov. 2018;30(4):715–723. doi: 10.1590/1980-5918.030.004.AO06. [DOI] [Google Scholar]
- 16.Sarwal A, Parrt SM, Berry MJ, Hsu FC, Lewis MT, Justus NW, et al. Interobserver reliability of quantitative muscle sonographic analysis in the critically ill population. J Ultrasound Med. 2015;34(7):1191–1200. doi: 10.7863/ultra.34.7.1191. [DOI] [PubMed] [Google Scholar]
- 17.Mc Auliffe S, Mc Creesh K, Purtill H, O’sullivan K. A systematic review of the reliability of diagnostic ultrasound imaging in measuring tendon size: is the error clinically acceptable? Phys Therapy Sport. 2017;26:52–63. doi: 10.1016/j.ptsp.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Gough JMA, Hamrell M. Standard operating procedures (SOPs): how companies can determine which documents they must put in place. Drug Inf J. 2010;44:49–54. doi: 10.1177/009286151004400106. [DOI] [Google Scholar]
- 19.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometria. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 20.Del Baño ME, Martínez-Payá JJ, Ríos-Díaz J, Mejías-Suárez S, Serrano-Carmona S, Groot-Ferrando A. Ultrasound measures of tendon thickness: intra-rater, inter-rater and Inter-machine reliability. Muscles Ligaments Tendons J. 2017;7(1):192–199. doi: 10.11138/mltj/2017.7.1.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.