Abstract
Rotator cuff calcific tendinopathy is a common non-traumatic shoulder pain condition that occurs predominantly in the supraspinatus tendon. Ultrasound-guided percutaneous irrigation of calcific tendinopathy (US-PICT) is a valid treatment in the resorptive phase. A complication of calcific tendinopathy is migration of calcium deposits outside the tendon. The most common site of migration is the subacromialsubdeltoid bursa (SASD). Another, but not frequent, type of migration is the intramuscular migration which mostly affects the supraspinatus, the infraspinatus and the biceps brachii muscles. This paper reports two cases of migration of calcification from the supraspinatus tendon to the deltoid muscle. The aforementioned site of migration has so far never been described in literature. Both patients presented calcification in the resorptive phase and therefore were treated by US-PICT.
Keywords: Shoulder pain, Calcific tendinopathy, Ultrasound-guided percutaneous treatment, Intramuscular migration
Introduction
Rotator cuff tendinopathy is a pathological condition characterized by hydroxyapatite crystals on the area of fibrocartilaginous metaplasia of the tenocytes [1, 2]. About 80% of shoulder calcifications involve the supraspinatus tendon [1] and only slightly more than a third of shoulder tendon calcifications become symptomatic [3, 4]. The most accredited pathogenetic theory seems to correlate a reduction in oxygen levels to the appearance of areas of fibrocartilaginous metaplasia and intratendinous necrotic areas in which calcium crystals are deposited. Uhthoff et al. [5] described three stages of shoulder calcific tendinopathy. The pre-calcific phase in which the fibrocartilaginous metaplasia occurs in tendon tissue. The calcific phase is divided into two phases: the formative phase characterized by formation of calcium deposits, and the resorptive phase in which macrophagic phagocytosis of calcium deposits occurs. Finally the post-calcific phase includes the remodeling of the tendon. The ultrasound-guided percutaneous irrigation of calcific tendinopathy (US-PICT) is a mini-invasive treatment which is suitable for the resorptive phase [6–8]. A complication of calcific tendinopathy is migration of deposits of calcium into the adjacent structures [9]. A literature review suggests the subacromial-subdeltoid bursa (SASD) as the most common site of migration. However, albeit less common, cases of intramuscular migration have been described [10]; in particular in the supraspinatus, infraspinatus [11, 12],subscapularis, in the third proximal of biceps brachii [13] and in the humeral insertion of the pectoralis major [14]. Another atypical site is intraosseous migration [15, 16] which involves three stages: the bone erosion, the subcortical migration and the intramedullary diffusion [17]. Imaging, and in particular RX, MRI and US, allows us to evaluate positioning of calcification after migration. In particular, ultrasound (US) represents the gold standard method for the identification of intrabursal and intramuscular migration [18]. The aim of this work is to describe two cases of a rare and unusual site of migration of calcium deposits from the supraspinatus tendon to the deltoid muscle in a context of calcific tendinopathy. To our knowledge analogous cases of migration have not yet been described in literature.
Case reports
The first case refers to a 60-year-old male, amateur swimmer, non-smoker, with no cardiovascular, endocrinological or metabolic comorbidities. The patient reported a history of calcific tendinopathy affecting the supraspinatus tendon as evidenced by a muscle–tendon ultrasound examination performed 40 days earlier than our observation by another physician (Fig. 1).Upon our observation, the patient complained of right shoulder pain which irradiated to the anterior brachial and deltoid regions; despite having undergone NSAID therapy (Diclofenac 150 mg/day for 5 days) the pain was evaluated 8/10 by visual analogical scale (VAS). Clinical evaluation revealed severe functional limitation of range of motion (ROM) in passive and active mobilization.
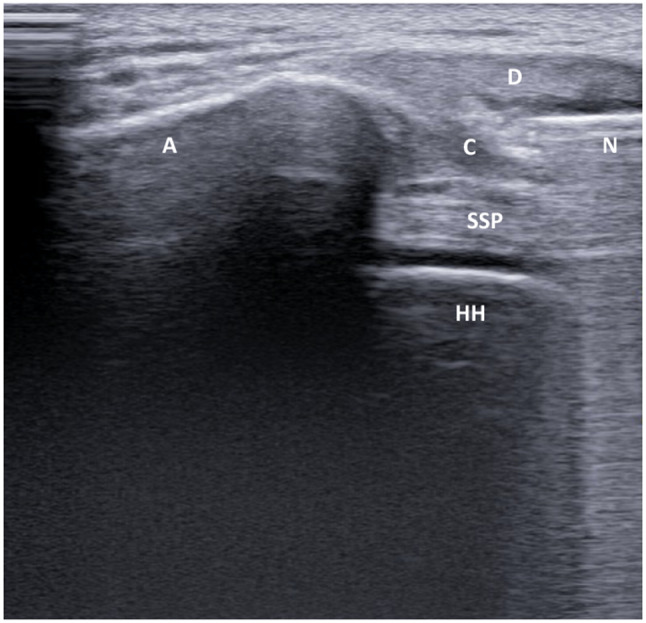
Fig. 1.
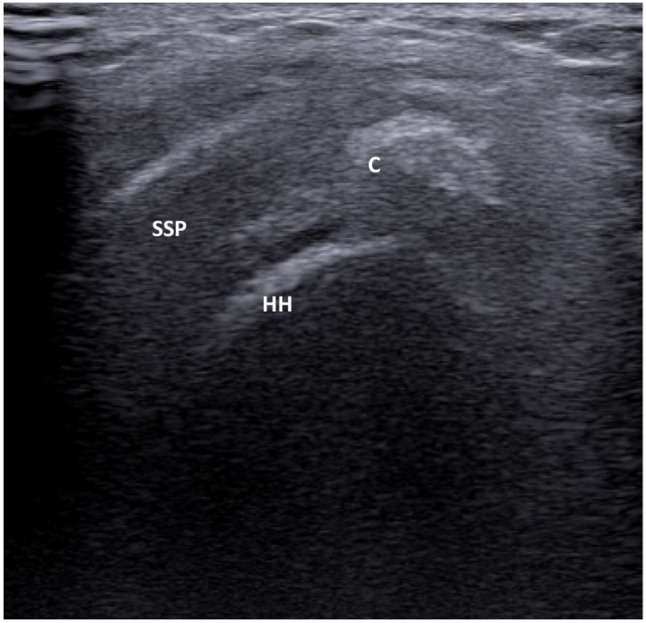
The ultrasound examination performed 40 days before than our observation shows the presence of calcium deposits inside the supraspinatus tendon. C calcification; HH humeral head; SSP = supraspinatus tendon
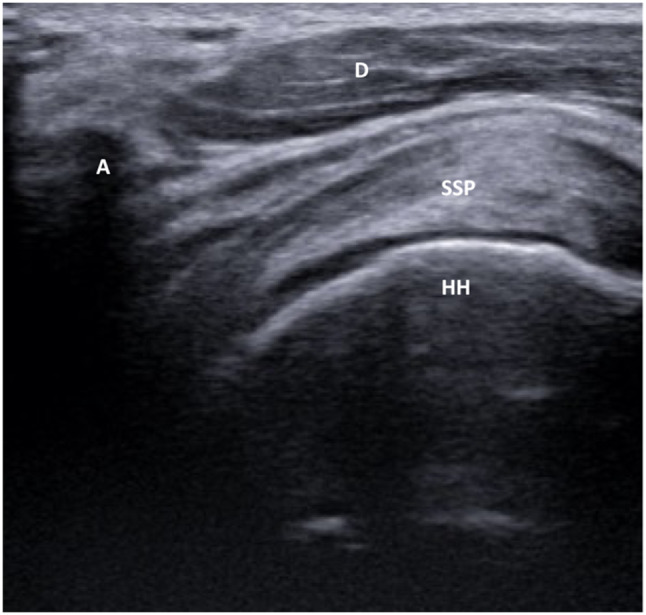
The ultrasound examination, performed with a MyLab40 system (Esaote Biomedica, Genoa, Italy) and a 5–12 MHz linear probe, showed the absence of calcification in the previous intratendinous localization which appeared to have migrated to the deltoid muscle near the proximal acromial insertion (Fig. 2). Color Power Doppler showed an area of peri-calcific hyperemia related to phenomena of neoangiogenesis and capillary proliferation typical of the resorptive phase [19].
Fig. 2.
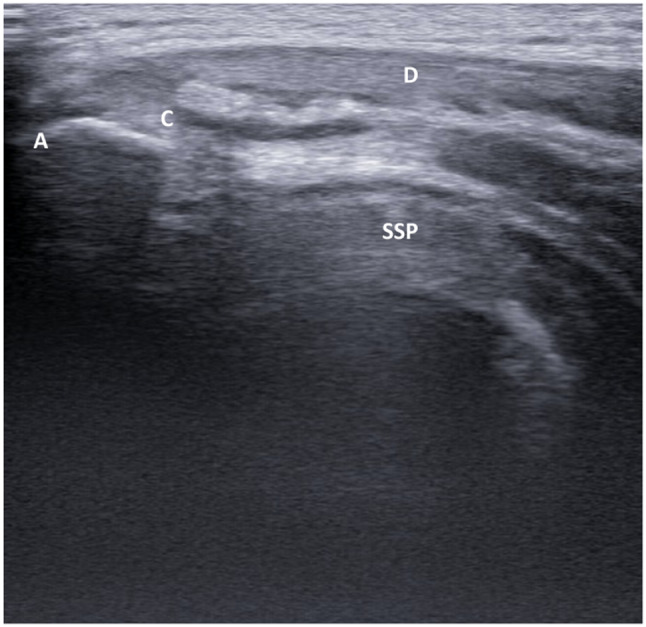
The ultrasound examination shows the presence of calcium deposits in the deltoid muscle. A acromion; C calcification; D deltoid; SSP supraspinatus tendon
The second case refers to a 42-year-old female amateur tennis player, smoker with absence of endocrinological and metabolic comorbidities. The patient brought an ultrasound exam of the left shoulder performed 2 months earlier than our observation which showed the presence of a calcification in the tendon of the supraspinatus muscle. During medical examination the patient reported an increase of symptoms, despite taking Ibuprofen 600 mg/day for 4 days. The symptoms were associated to reduction of free ROM in abduction and external rotation and pain intensity 7/10 by VAS. The ultrasound examination showed the calcific deposits in between the SASD bursa and the deltoid muscle (Fig. 3).
Fig. 3.
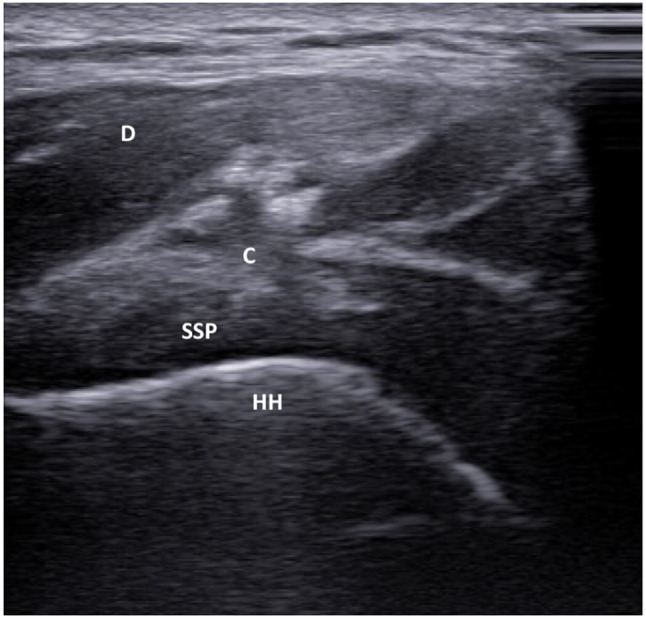
The ultrasound examination shows the presence of calcium deposits between the deltoid muscle and the supraspinatus tendon. C calcification; D deltoid; HH = humeral head; SVSP = supraspinatus tendon
Despite absence of guidelines regarding the treatment of intramuscular migration of calcification, based on the experience gained in the treatment of tendon calcifications and the ultrasound staging of the pathology, both patients were treated whit US-PICT [20]. The patient described in the second case returned after 7 days for treatment. The ultrasound re-evaluation illustrated the complete migration of the calcification to the deltoid muscle (Fig. 4).
Fig. 4.
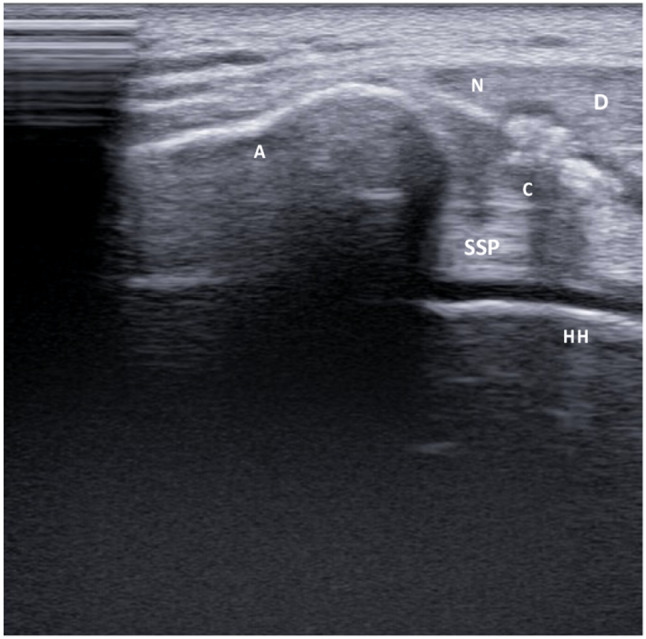
The image illustrates the ultrasound-guided percutaneous irrigation of migrated calcification inside the deltoid muscle. The ultrasound examination shows the needle inside the calcification during the treatment. A acromion; C calcification; D deltoid
The following procedure was adopted to treat the calcic formation: the first phase was an accurate two-step skin disinfection with povidone-iodine and chlorhexidine. The double color disinfection allows us to "center" the area of treatment; secondly through ultrasound guide and a 21G needle, 5 ml of lidocaine 2% was injected into the SASD bursa. Two minutes later the needle was introduced into the calcification using ultrasound guide to aspire calcium deposits by means of compression and release of the syringe plunger (Fig. 4). The procedure was performed by the same needle but changing syringes, until all the amorphous material of the calcification aspirated. Without removing the needle, 1 mL of triamcinolone acetonide 40 mg/ml was injected into the SASD bursa to avoid reactive bursitis. In the second patient the introduction of a separate needle from the other side of the calcification to complete the irrigation of the calcific deposits was necessary (Fig. 5). The last phase was a post-procedural ultrasound check to exclude periprocedural complications. After the procedure the needle entry site was covered with sterile gauze and dry ice was applied for 15 min.
Fig. 5.
The image shows the treatment of the calcification of the second patient where the introduction of a separate needle from the other side of the calcification to complete the procedure was necessary. A acromion; C calcification; N needle; HH humeral
The patients were instructed to rest for 3 days from treatment and subsequently for 15 days avoiding elevation and abduction movements. The clinical and ultrasound evaluations were performed after 3 weeks from procedure after which physiotherapy was initiated. At the first check at 3 weeks from the procedure the patient of the first case reported a complete remission of the symptoms while the second patient reported the persistence of minimal pain (VAS 2/10). Ultrasound examination showed in both patients the disappearance of hyperechoic area in the deltoid muscle referable to the migrated calcification and the absence of the previously described inflammatory phenomena. The final clinical and ultrasound evaluation was performed at 60 days from the procedure; both patients reported the remission of the pain symptoms with complete recovery of the joint ROM in all movement; the ultrasound examination showed the absence of calcific deposits in the deltoid muscle and the supraspinatus tendon, and the absence of inflammatory reactions affecting the SASD bursa (Fig. 6). Both patients resumed regular sport activity.
Fig. 6.
The ultrasound examination performed 60 days after the procedure shows the absence of calcific deposits inside the deltoid muscle. A acromion; D deltoid; HH humeral head; SSP supraspinatus tendon
Discussion
Migration of intratendinous hydroxyapatite crystal deposits into adjacent structures is a rare complication which mainly concerns the SASD bursa. Cases of intramuscular migration, mainly in the supraspinatus and infraspinatus muscles, are reported, as evidenced by Pereira et al. [21] in a multicenter retrospective study. Other cases of intramuscular migration in the subscapularis muscle and proximal third of the biceps brachii have also been described. Another atypical migration is intraosseous, in which MRI becomes fundamental in addition to the ultrasound examination that allows to highlight the erosion of the humeral head related to the passage of calcification. In fact, as demonstrated by the literature, MRI is fundamental to identify the correct phase of intraosseous migration of calcification (the bone erosion phase, the subcortical migration or the intramedullary diffusion) and to make the differential diagnosis with other bone pathologies [22]. From our analysis of literature, cases of migration of rotator cuff calcifications in the deltoid have not been described.
The ultrasound examination allows us to identify the correct phase of the calcification and the migration into the adjacent structures. Bianchi et al. [23] describe three different types of calcification visualized on ultrasound in the calcific phase: type I which appear as hyperechoic structures with a well-defined acoustic shadow; type II are hyperechoic but with a mild acoustic shadow and type III which appears as isoechoic without an acoustic shadow. Types II and III generally correspond to the resorptive phase. The passage of calcifications to adjacent tissues occurs mainly during the resorptive phase. In this phase, due to the softer consistency of the calcification, the US-PICT is indicated and in our experience it allows a rapid regression of pain symptoms [24]. Ultrasound exam allows the correct diagnosis of the position of the calcification inside the tendon, the staging of the calcification and the identification of the reactive phlogosis, detectable as edema surrounding the calcium deposits. The presence in both cases of a previous ultrasound evaluation (respectively 40 and 60 days before our observation) with relative diagnosis of calcific tendinopathy of the supraspinatus tendon, combined with the identification of calcification only in the intramuscular site allowed the correct diagnosis of migration inside the deltoid muscle.
Conclusion
This paper demonstrates that the deltoid localization can be considered a possible, although rare, site of atypical migration of rotator cuff calcifications. Moreover ultrasound-guided percutaneous treatment has proven to be a valid option for pain relief and recovery of the shoulder in cases with intramuscular migration of calcification.
Funding
The authors have not disclosed any funding.
Data availability
All data relating to the two case reports are available in the manuscript.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of Helsinki Declaration.
Informed consent
IRB approval and informed consent from the patients included in the cases report was obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Serafini G, Sconfienza M, Lacelli F, et al. Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two needle US-guided percutaneous treatment-nonrandomized controlled trial. Radiology. 2009;252(1):157–164. doi: 10.1148/radiol.2521081816. [DOI] [PubMed] [Google Scholar]
- 2.De Carli A, Pulcinelli F, Rose GD, Pitino D, Ferretti A. Calcific tendinitis of the shoulder. Joints. 2014;2:130–136. doi: 10.11138/jts/2014.2.3.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clavert P, Sirveaux F. Societe francaise, shoulder calcifying tendinitis. Rev Chir Orthop Repar Appar Mot. 2008;94:336–355. doi: 10.1016/j.rco.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Barile A, Bruno F, Mariani S, et al. Follow-up of surgical and minimally invasive treatment of Achilles tendon pathology: a brief diagnostic imaging review. Musculoskelet Surg. 2017;101:51–61. doi: 10.1007/s12306-017-0456-1. [DOI] [PubMed] [Google Scholar]
- 5.Uhthoff HK, Sarkar K. Calcifying tendinitis. Baillieres Clin Rheumatol. 1989;3:567–581. doi: 10.1016/S0950-3579(89)80009-3. [DOI] [PubMed] [Google Scholar]
- 6.Lafrance S, Doiron-Cadrin P, Saulnier M, et al. Is ultrasound-guided lavage an effective intervention for rotator cuff calcic tendinopathy? A systematic review with a meta-analysis of randomised controlled trials. BMJ Open Sport Exerc Med. 2019;5:e0005. doi: 10.1136/bmjsem-2018-000506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iovane A, Di Gesù M, Mantia F, Thomas E, Messina G. Ultrasound-guided percutaneous treatment of a calcific acromioclavicular joint: a case report. Medicine (Baltimore) 2020;99(1):e18645. doi: 10.1097/MD.0000000000018645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greis AC, Derrington SM, McAuliffe M. Evaluation and nonsurgical management of rotator cuff calcific tendinopathy. Orthop Clin N Am. 2015;46:293–302. doi: 10.1016/j.ocl.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Della Valle V, Bassi EM, Calliada F. Migration of calcium deposits into subacromial–subdeltoid bursa and into humeral head as a rare complication of calcifying tendinitis: sonography and imaging. J Ultrasound. 2015;18(3):259–263. doi: 10.1007/s40477-015-0163-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Albano D, Coppola A, Gitto S, Rapisarda S, Messina C, Sconfienza LM. Imaging of calcific tendinopathy around the shoulder: usual and unusual presentations and common pitfalls. Radiol Med. 2021;126(4):608–619. doi: 10.1007/s11547-020-01300-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cocco G, Ricci V, Boccatonda A, Iannetti G, Schiavone C. Migration of calcium deposit over the biceps brachii muscle, a rare complication of calcific tendinopathy: Ultrasound image and treatment. J Ultrasound. 2021;21(4):351–354. doi: 10.1007/s40477-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Becciolini M, Bonacchi G, Galletti S. Intramuscular migration of calcific tendinopathy in the rotator cuff: ultrasound appearance and a review of the literature. J Ultrasound. 2016;19(3):175–181. doi: 10.1007/s40477-016-0202-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marinetti A, Sessa M, Falzone A, Della Sala SW. Intraosseous migration of tendinous calcifications: two case reports. Skelet Radiol. 2018;47:131–136. doi: 10.1007/s00256-017-2769-4. [DOI] [PubMed] [Google Scholar]
- 14.Dukan R, Amsallem L, Silvera J, Masmejean EH. Atypical localization of calcific shoulder tendinopathy: humeral insertion of the pectoralis major. J Orthop Case Rep. 2020;10(6):44–48. doi: 10.13107/jocr.2020.v10.i06.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalaycı CB, Kızılkaya E. Calcific tendinitis: intramuscular and intraosseous migration. Diagn Interv Radiol. 2019;25(6):80–484. doi: 10.5152/dir.2019.18593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malghem J, Omoumi P, Lecouvet F, Vande BB. Intraosseous migration of tendinous calcifications: cortical erosions, subcortical migration and extensive intramedullary diffusion: a SIMS series. Skelet Radiol. 2015;44:1403–1412. doi: 10.1007/s00256-015-2165-x. [DOI] [PubMed] [Google Scholar]
- 17.Paruthikunnan SM, Boily M, Martin MH, Assaf A, Jaffer R. Intra-osseous migration in calcific rotator cuff tendinopathy- a novel depiction of temporal evolution on multimodality imaging. BJR Case Rep. 2022;8(2):20210156. doi: 10.1259/bjrcr.202101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zampa V, Aringhieri G, Rossi P, Capanna R, Caramella D. Humeral greater tuberosity osteolysis as a complication of intraosseous calcification migration: natural history depicted by imaging. Acta Biomed. 2021;92(S1):e2021052. doi: 10.23750/abm.v9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uhthoff HK, Sarkar K. Calcific tendinopathy of the rotator cuff. J Am Acad Orthop Surg. 1997;5:183–191. doi: 10.5435/00124635-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Lanza E, Banfi G, Serafini G, Lacelli F, Orlandi D, Bandirali M, Sardanelli F, Sconfienza LM. Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: what is the evidence? A systematic review with proposals for future reporting. Eur Radiol. 2015;25(7):2176–2183. doi: 10.1007/s00330-014-3567-1. [DOI] [PubMed] [Google Scholar]
- 21.Pereira BP, Chang EY, Resnick DL, Pathria MN. Intramuscular migration of calcium hydroxyapatite crystal deposits involving the rotator cuff tendons of the shoulder: report of 11 patients. Skelet Radiol. 2016;45(1):97–103. doi: 10.1007/s00256-015-. [DOI] [PubMed] [Google Scholar]
- 22.Gwalani R, Thombare P, Verma M, Ahuja G, Patkar D. MRI findings in intraosseous extension of calcific supraspinatus tendonitis. Radiol Case Rep. 2020;15(7):975–977. doi: 10.1016/j.radcr.2020.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bianchi S, Becciolini M. Ultrasound appearance of the migration of tendon calcifications. J Ultrasound Med. 2019;38(9):2493–2506. doi: 10.1002/jum.14933. [DOI] [PubMed] [Google Scholar]
- 24.Cho NS, Lee BG, Rhee YG. Radiologic course of the calcific deposits in calcific tendinitis of the shoulder: does the initial radiologic aspect affect the final results? J Shoulder Elb Surg. 2010;19:267–272. doi: 10.1016/j.jse. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relating to the two case reports are available in the manuscript.


