Abstract
One non-pharmacological method that can be used to safely and without negative side effects is aromatherapy. This meta-analysis study was carried out to assess the effectiveness of aromatherapy in the treatment of labor pain. The analysis included 14 randomized controlled trials of aromatherapy interventions for labor pain. In the studies, it was observed that aromatherapy was applied through massage and inhalation using oils such as lavender, jasmine, rose, chamomile, bitter orange, and boswellia. In the meta-analysis, it was discovered that aromatherapy had a beneficial effect on the management of labor pain and reduced labor pain in the intervention group in 11 studies; it was found that there was no effect in 3 studies. According to analysis findings, aromatherapy significantly lessened the intensity of labor pain. The study's findings support the notion that aromatherapy can lessen labor pain.
Keywords: Aromatherapy, Labor pain, Pain management, Non-pharmacological method
Introduction
One of the worst pains a person can experience is during childbirth. Labor pain is regarded as a complex physiological phenomenon with psychological, emotional, spiritual, and physical dimensions [1], [2]. Despite being a normal component of labor, prolonged labor pain can be harmful to both the mother and the unborn child [3]. Each woman who gives birth experiences labor pain differently [4]. Preparation for birth and the caliber of standard care protocols also play a significant role in the perception of labor pain, in addition to physiological, psycho-social, and environmental factors [5]. While some women successfully manage their pain and require less assistance, others are unable to. To treat labor pain, a variety of pharmaceutical and non-pharmacological interventions are used [6]. Because they are less expensive and less invasive than pharmaceutical treatments, non-pharmacological therapies are typically preferred [1], [6]. Non-pharmacological interventions are those used to lessen labor pain; they are straightforward, affordable solutions with little to no negative effects on the mother, fetus, or delivery process [7]. Increased mobility, walking, massage, hot and cold applications, aromatherapy, dermal stimulation, music therapy, and breath control are just a few examples of non-pharmacological methods of pain relief [1].
Aromatherapy is a non-pharmacological treatment method that is simple to apply and use. It is a method in which essential oils obtained from the flower, bark, stem, leaf, root, fruit, and other parts of the plant by various methods are used to treat diseases or reduce symptoms by inhalation, local application, or bathing [8], [9]. Due to its ease of use, aromatherapy is a complementary alternative therapy that can be used on its own. Aromatherapy has a long history of use in healthcare and treatment. Numerous nations, including India, China, France, Egypt, Greece, Iraq, Syria, Switzerland, Tibet, England, and the United States, use aromatic plants for therapeutic purposes [10]. In recent years, one of the non-pharmacological treatments for labor pain has been aromatherapy [11]. Women can use aromatherapy, a non-pharmacological treatment, to reduce prenatal symptoms and have a pleasant and comfortable birth experience [1]. It is seen that aromatherapy studies, especially on the psychological effects of labor pain and birth, started between 1996 and 2002 and accelerated until today [12], [13]. A meta-analysis study found that aromatherapy was effective in reducing labor pain and stress during the first stage of labor [14]. A meta-analysis study by Chen et al. shows that aromatherapy reduces labor time and pain felt in all three stages of labor [15]. Evidence from a systematic review also suggests that aromatherapy may help relieve maternal anxiety and pain during labor [16]. Aromatherapy is used as a simple, cost-effective and side-effectless method to control labor pain [1], [13]. Studies on the anxiety-relieving and mouth-reducing effects of aromatherapy applications using different herbs have been conducted [16]. Numerous studies on aromatherapy show that it has a very strong pain-relieving effect during labor. Though there are very few studies on this topic, it is still unclear which substance is more efficient at lessening labor pain. This is why the study has been designed with the idea that it will close the gap in the field. The effectiveness of aromatherapy with different herbs on labor pain was investigated in our study through a meta-analysis of randomized controlled trials.
Methods
The design of the study used to assess the efficacy of applications of aromatherapy used in the management of labor pain is a meta-analysis method, which is a statistical procedure application used for the purpose of combining and interpreting individual studies. The meta-analysis protocol was developed and the article was written utilizing the PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols) notification checklist [17]. In order to assess the effectiveness of massage and inhalation, as well as the effects of lavender, jasmine, rose, chamomile, bitter orange, and boswellia oil on the management of labor pain in pregnant women, a descriptive analysis of the studies was performed. The results were then statistically combined. First, a homogeneity test was run in the study to choose the appropriate model.
Search strategy and selection criteria
Between November 1 and December 1, 2021, searches in the electronic databases PubMed, Cochrane, Web of Science, and Google Scholar were done in English. In Table 1, the search terms and comprehensive search methodology are displayed.
Table 1.
Example Scanning Strategy.
| Key words | (Labor pain (Aromatherapy OR Aroma OR Essential oils OR Lavender OR Rosa OR Geranium OR Jasmin OR Chamomile OR Peppermint) OR Delivery pain) |
|---|---|
| Scan 1. | ((Aromatherapy [Title]) OR (Aroma [Title]) OR (Essential oils [Title]) OR (Lavender [Title]) OR (Rosa [Title]) OR (Geranium [Title]) OR (Jasmin [Title]) OR (Chamomile [Title]) OR (Peppermint [Title]) AND (Labor pain [Title])) |
| Scan 2. | ((Aromatherapy [Title]) OR (Aroma [Title]) OR (Essential oils [Title]) OR (Lavender [Title]) OR (Rosa [Title]) OR (Geranium [Title]) OR (Jasmin [Title]) OR (Chamomile [Title]) OR (Peppermint [Title]) AND (Delivery pain [Title])) |
| Scan 3. | ((Aromatherapy [Title]) OR (Aroma [Title]) OR (Essential oils [Title]) OR (Lavender [Title]) OR (Rosa [Title]) OR (Geranium [Title]) OR (Jasmin [Title]) OR (Chamomile [Title]) OR (Peppermint [Title]) AND (Labor pain [Title]) OR (Delivery pain [Title])) |
Inclusion and exclusion criteria
Studies published in international peer-reviewed journals between 2011 and 2021 that had full texts available were included in the study. The inclusion and exclusion criteria were established in accordance with PICOS. In this situation, the requirements for study inclusion are;.
P (Patient/Participant): Pregnant women (single, at term, aged 18–35, without a risky pregnancy, presenting with a cephalic pattern, in the active phase).
I (Intervention): Uses for aromatherapy.
C (Comparison/Comparative group): Expectant mothers receiving standard care.
O (Outcome/Conclusion): A change in the way that labor pain is perceived.
S (Study design): Randomized controlled studies.
The following studies were excluded from the study because they did not meet the inclusion criteria: observational studies, study designs, study protocols, qualitative studies, and repeated studies.
Selection of studies
The articles (n = 80) that were found through the search were added to the Endnote library so that they could be separated later and the best ones for the study could be chosen. After duplications were eliminated, the remaining articles (n = 74) were first screened based on their titles and abstracts (n = 5), with 74 articles considered potentially relevant being subjected to a full-text review. Following a thorough analysis of the full texts (n = 69) that were evaluated for suitability, 36 studies were chosen for the synthesis after excluding studies whose full texts could not be accessed, which were discovered to be protocols, whose language was not English, and whose methods were different. By eliminating studies that lacked pain evaluation results or had inconsistent timing for evaluations, a total of 14 studies were left from these studies to complete the meta-analysis. In Fig. 1, the PRISMA flowchart, the research selection procedure for the study is shown.
Fig. 1.
Prisma Flow Chart.
Extraction of study data
Utilizing a prepared checklist, data were manually gathered from each study that was part of the meta-analysis. This checklist's components are as follows: study design, study information, and publication, time period, sample size, intervention, intervention group, control group, sample size, and pain measurement tool, In case and control groups, pre- and post-intervention labor pain was measured. Measured variables include mean, SD, delivery time, delivery method, and result. Data extracted using the data extraction tool were tabulated and grouped. The results were presented using a narrative synthesis. The total sample size was 902 in the control group and 1155 in the intervention group. The earliest study was completed in 2013 and the most recent in 2021. As a measurement tool for birth pain, the numerical rating scale (NRS) was used in 5 studies and the visual analog scale (VAS) in 9.
Evaluation of methodological quality of studies and risk of bias
Using the Joanna Briggs Institute's Checklists for Randomized Controlled Studies, two researchers independently assessed the quality of each study that was included in the meta-analysis. A total of 13 points can be earned by scoring each item on the checklist as "Yes = 1, No = 0, Uncertain = 0, or Not applicable = 0." Studies that are evaluated as "no/uncertain/not applicable" out of 1–2 items are considered to have a "low risk weakness," 3–4 items are considered to have a "medium risk weakness," and 5–8 items are "no/uncertain/not applicable." has been classified as a "high-risk weakness."[18] Using the updated Cochrane risk of bias tool (RoB 2) for randomized studies, the studies' bias was evaluated [19].
Based on the CONSORT checklist criteria, all of the studies that were included in the meta-analysis had moderate to high methodological quality. Table 2 displays the characteristics of the studies that were a part of the meta-analysis.
Table 2.
Methodological Quality Evaluations of the Studies.
| Tag of the article | criteria |
Total (%) | Weakness Risk | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |||
| Alavi vd.,2017 | B | B | E | B | B | B | E | E | E | E | E | E | H | 6/13 (%46) | High |
| Cenkçi, 2017 | E | E | E | B | B | B | E | E | E | E | E | E | H | 9/13 (%69) | Average |
| Hamdamian vd.,2018 | E | E | E | B | B | B | E | E | E | E | E | E | H | 9/13 (%69) | Average |
| Tanvisut vd.,2018 | E | E | E | E | B | B | E | E | E | E | E | E | H | 10/13 (%88) | Average |
| Yazdkhasti & Pirak, 2016 | E | E | E | E | B | B | E | E | E | E | E | E | H | 10/13 (%88) | Average |
| Esmaelzadeh vd., 2018 | E | E | E | H | B | E | E | E | E | E | E | E | H | 10/13 (%88) | Average |
| Vakilian vd., 2018 | E | E | E | B | B | B | E | E | E | E | E | E | H | 9/13 (%69) | Average |
| Janula ve Singh, 2014 | B | B | E | B | B | B | E | E | E | E | E | E | H | 7/13 (%54) | High |
| Janula ve Singh, 2015 | B | B | E | B | B | B | E | E | E | E | E | E | H | 6/13 (%46) | High |
| Joseph ve Fernandes, 2013 | B | B | E | B | B | B | E | E | E | E | E | E | H | 6/13 (%46) | High |
| Kaviani vd.,2014(a) | B | E | E | B | B | B | E | E | E | E | E | E | H | 8/13 (%61) | High |
| Kaviani vd.,2014(b) | B | E | E | B | B | B | E | E | E | E | E | E | H | 8/13 (%61) | High |
| Lamadah ve Nomani, 2016 | B | E | E | B | B | B | E | E | E | E | E | E | H | 8/13 (%61) | High |
| Namazi vd.,2014 | B | B | E | B | B | B | E | E | E | E | E | E | H | 7/13 (%54) | High |
*Note: Y = Yes; N = No; U = Uncertain; G = Not applicable; 1–13: Items from the checklist for randomized controlled trials created by the Joanna Briggs Institute
The risk of bias assessment of the studies included in the study is shown in Table 3.
Table 3.
Evaluation of the Risk of Bias of Studies.
| Criteria | Alavi vd.,2017 | Cenkçi, 2017 | Hamdamian vd.,2018 | Tanvisut vd.,2018 | Yazdkhasti & Pirak, 2016 | Esmaelzadeh vd., 2018 | Vakilian vd., 2018 | Janula ve Singh, 2014 | Janula ve Singh, 2015 | Joseph ve Fernandes, 2013 | Kaviani vd.,2014 (a) | Kaviani vd.,2014 (b) | Lamadah ve Nomani, 2016 | Namazi vd.,2014 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias arising from the randomization process | ? | + | + | + | + | + | + | ? | ? | ? | ? | ? | ? | ? |
| Risk of bias due to deviations from intended interventions (impact of assignment on intervention) | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Risk of bias due to deviations from intended interventions (effect of adherence to the intervention) | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Risk of bias due to missing outcome data | ? | ? | + | ? | ? | + | + | + | ? | + | + | + | + | + |
| Risk of bias in measuring outcome | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? |
| Risk of bias in selection of the reported outcome | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
+ Low risk of bias ? Suspicious bias risk -High risk of bias
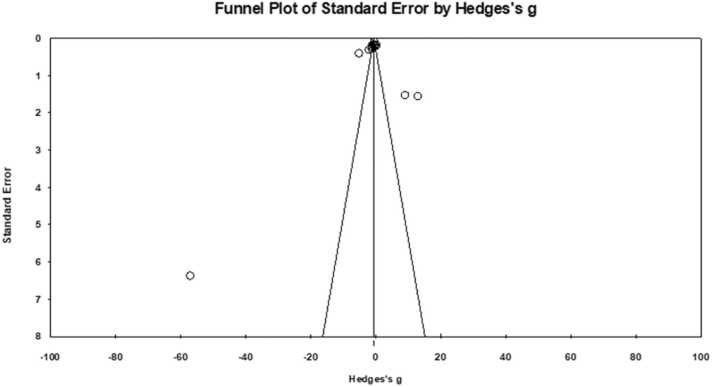
The funnel plot, which was created to examine the publication bias of the study, is displayed in Fig. 2.
Fig. 2.
Funnel Plot for Studies Included in the Meta-Analysis.
It is clear that there is publication bias when the effect sizes are distributed asymmetrically in the funnel plot, as opposed to when they are distributed symmetrically [20]. In light of Fig. 2, it can be concluded that there is no publication bias in the research because the effect sizes are close to symmetrical distributions and the standard errors of the studies included in the meta-analysis are small. Table 4.
Table 4.
Aromatherapies and Their Effects on Labor Pain.
| Tag | Measuring Tool | Plant used | Phase | Intervention Group | Control Group | Effect on labor pain |
|---|---|---|---|---|---|---|
| Alavi vd.,2017 | Visual Analog Scale (VAS) | Jasmine Oil | Stage 1 | 5.18 ± 8.07 | 6.17 ± 5.39 | Decreased |
| Stage 2 | 7.00 ± 9.89 | 8.15 ± 4.06 | ||||
| Stage 3 | 0.01 ± 6.69 | 9.07 ± 3.58 | ||||
| Cenkçi, 2017 | VAS | Lavender Oil | Stage 1 | 3.40 ± 2.10 | 6.60 ± 2.00 | Decreased |
| Stage 2 | 6.10 ± 1.70 | 8.70 ± 1.00 | ||||
| Stage 3 | 8.30 ± 0.90 | 9.80 ± 0.50 | ||||
| Esmaelzadeh vd., 2018 | NPRS (Numaric Pain Rating Scale) | Boswellia Oil |
Stage 1 | 4.98 ± 0.93 | 6.68 ± 1.28 | Decreased |
| Stage 2 | 5.79 ± 1.13 | 7.23 ± 1.54 | ||||
| Stage 3 | 6.35 ± 1.63 | 7.71 ± 1.38 | ||||
| Hamdamian vd.,2018 | NPRS | Rose Oil | Stage 1 | 3.25 ± 1.02 | 6.36 ± 1.02 | Decreased |
| Stage 2 | 5.11 ± 0.71 | 8.42 ± 0.50 | ||||
| Stage 3 | 6.69 ± 0.47 | 9.78 ± 0.42 | ||||
| Janula & Singh, 2014 | VAS | Lavender Oil | Stage 1 | 6.20 ± 0.13 | 8.60 ± 0.50 | Decreased |
| Stage 2 | 7.50 ± 0.21 | 9.00 ± 0.34 | ||||
| Stage 3 | 8.30 ± 0.47 | 9.60 ± 0.21 | ||||
| Janula & Singh, 2015 | VAS | Lavender Oil | Stage 1 | 6.20 ± 0.13 | 8.60 ± 0.50 | Decreased |
| Stage 2 | 7.50 ± 021 | 9.00 ± 0.34 | ||||
| Stage 3 | 8.30 ± 047 | 9.60 ± 0.21 | ||||
| Joseph & Fernandes, 2013 | VAS | Jasmine Oil | Stage 1 | 3.10 ± 1.10 | 7.95 ± 1.50 | Decreased |
| Kaviani vd.,2014 (a) | VAS | Jasmine Oil | Stage 1 | 6.60 ± 2.20 | 7.80 ± 1.90 | No Effect |
| Stage 2 | 6.90 ± 2.30 | 8.50 ± 1.60 | ||||
| Kaviani vd.,2014 (b) | VAS | Lavender Oil | Stage 1 | 3.19 ± 1.10 | 3.17 ± 1.20 | Decreased |
| Stage 2 | 4.31 ± 0.90 | 3.98 ± 1.27 | ||||
| Lamadah ve Nomani, 2016 | VAS | Lavender Oil | Stage 1 | 7.00 ± 0.11 | 8.10 ± 0.14 | No Effect |
| Stage 2 | 6.54 ± 0.20 | 8.90 ± 0.19 | ||||
| Stage 3 | 7.70 ± 0.17 | 9.60 ± 0.50 | ||||
| Namazi vd.,2014 | NPRS | Bitter Orange Oil | Stage 1 | 4.97 ± 0.74 | 8.08 ± 0.67 | Decreased |
| Stage 2 | 6.65 ± 0.48 | 8.67 ± 0.56 | ||||
| Stage 3 | 7.57 ± 0.56 | 9.46 ± 0.53 | ||||
| Tanvisut vd.,2018 | NPRS | Lavender Oil | Stage 1 | 1.88 ± 2.24 | 2.60 ± 2.21 | Decreased |
| Stage 2 | 3.82 ± 2.45 | 4.39 ± 2.10 | ||||
| Stage 3 | 5.45 ± 2.28 | 5.62 ± 2.10 | ||||
| Vakilian vd., 2018 | VAS | Lavender Oil | Stage 1 | 6.53 ± 2.04 | 7.07 ± 1.95 | Decreased |
| Stage 2 | 6.77 ± 2.10 | 7.41 ± 1.71 | ||||
| Stage 3 | 7.01 ± 2.04 | 7.82 ± 1.96 | ||||
| Yazdkhasti & Pirak, 2016 | NPRS | Lavender Oil | Stage 1 | 6.10 ± 2.30 | 7.70 ± 2.10 | No Effect |
| Stage 2 | 6.70 ± 2.00 | 8.60 ± 1.60 | ||||
| Stage 3 | 7.93 ± 2.10 | 9.40 ± 1.10 |
Data analysis
The data from the study were analyzed using the Comprehensive Meta-Analysis (CMA) program. The pre-test and post-test results, standard deviations, sample sizes, and types of interventions from all studies of the intervention and control groups were entered, and the effect sizes were calculated using Hedge's g analysis. Calculating the effect size requires knowledge of how homogeneous or heterogeneous the studies are. Fixed effects models are used to calculate effect sizes when studies are homogeneous, and random effects models are used when studies are heterogeneous [20]. Using the Cochran Q and Higgins I2 tests, the heterogeneity among the studies under consideration was assessed, and it was agreed that an I2 of more than 50 % indicates significant heterogeneity. The studies that make up the meta-analysis have been found to have a heterogeneous structure, and the analysis should choose a statistical model based on the random effects model. For categorical variables, the study's data were converted to 95 % confidence intervals (CI), odds ratios (OR), and standard mean differences (SMD) and mean differences (MD) for continuous variables. The relationship between the pre- and post-intervention labor pain scale scores and the publication year, sample size, and quality assessment score was also examined using meta-regression. By type of aromatherapy, study population, and application method, subgroup analysis was conducted. All tests were computed using the two-tailed method. Comprehensive meta-analysis software (version 2) was applied for the meta-analysis, and p < .050 was considered statistically significant. While calculating the effect sizes, the classification of the effect level was also handled as follows: - 0.15 ≤ Cohen d < 0.15 insignificant level, 0.15 ≤ Cohen d < 0.40 at small level, 0.40 ≤ Cohen d < 0.75 at medium level, 0.75 ≤ Cohen d < 1.10 at large level, 1.10 ≤ Cohen d < 1.45 very broad, 1.45 ≤ Cohen d excellent [21].
Results
The effects of lavender, jasmine, rose, chamomile, bitter orange, and boswellia oil on labor pain management in pregnant women were examined in the study. Following the meta-analysis, the effect sizes of the studies included in the study were calculated, and the results were provided in separate tables.
Table 5 shows that 3 studies had positive effect size values that ranged between 0.26 and 12.98, while 11 studies had negative effect size values that ranged from −0.21 to −56.93. This situation demonstrates that using aromatherapy to treat labor pain has a pain-reducing effect in favor of the intervention group in 11 studies. The study's studies' confidence intervals ranged from − 69.42–16.03. Moreover, Fig. 3 presents the forest plot illustrating the distribution of the effect size values of the studies included in the meta-analysis produced in accordance with the random effects model.
Table 5.
Effect Size, Variance and Standard Error Values of Studies.
| Study | Effect Size | Standart Error | Variance | Lower Limit | Upper Limit |
|---|---|---|---|---|---|
| Alavi vd.,2017 | -0.98 | 0.24 | 0.05 | -1.45 | -0.51 |
| Cenkçi, 2017 | -1.99 | 0.31 | 0.09 | -2.61 | -1.38 |
| Esmaelzadeh vd., 2018 | -1.09 | 0.19 | 0.03 | -1.46 | -0.71 |
| Hamdamian vd.,2018 | -5.08 | 0.40 | 0.16 | -5.88 | -4.29 |
| Janula & Singh, 2014 | -1.09 | 0.28 | 0.08 | -1.65 | -0.53 |
| Janula & Singh, 2015 | -1.10 | 0.11 | 0.01 | -1.32 | -0.88 |
| Joseph & Fernandes, 2013 | -56.93 | 6.37 | 40.61 | -69.42 | -44.44 |
| Kaviani vd.,2014(a) | -0.69 | 0.16 | 0.02 | -1.01 | -0.37 |
| Kaviani vd.,2014(b) | 0.26 | 0.19 | 0.03 | -0.11 | 0.65 |
| Lamadah & Nomani, 2016 | 9.07 | 1.52 | 2.33 | 6.07 | 12.07 |
| Namazi vd.,2014 | -0.38 | 0,18 | 0.03 | -0.74 | -0.03 |
| Tanvisut vd.,2018 | -0.21 | 0,19 | 0.03 | -0.59 | 0.16 |
| Vakilian vd., 2018 | -0.22 | 0,18 | 0.03 | -0.57 | 0.13 |
| Yazdkhasti & Pirak, 2016 | 12.98 | 1,55 | 2.43 | 9.92 | 16.03 |
Fig. 3.
The graph of the effect sizes of the studies according to the random effects model.
The squares in Fig. 3's forest graph represent the effect sizes of the research's included studies, and the lines on either side of the squares represent the lower and upper bounds of those effect sizes at the 95 % confidence level. The rhombus displays the overall effect size of the studies, while the width of the squares indicates the weight of the individual works. The highest effect size value is − 56.93, and the smallest effect size value is 12.98 when the effect sizes of the studies are examined. In 11 studies, aromatherapy was effective in managing labor pain and reducing labor pain for the intervention group; however, in 3 studies, there was no effect. As a result, it was determined that studies looking at the impact of aromatherapy on labor pain management had an effect in favor of the intervention group. The lower and upper limits of the 95 % confidence interval were found to be within the limits of − 0.88 and − 0.65, taking into account the total effect size (−0.77) in the Random Effects Model.
The weighted sum of squares (Q statistic) of the effect sizes, the p value, and the I2 value, which displays the ratio of the excess variance to the total variance, were calculated in order to determine whether or not the studies examining the effectiveness of aromatherapy applications used in the management of labor pain included in the meta-analysis are homogeneous. These values are displayed in Table 6.
Table 6.
Heterogeneity Test Analysis Results of Effect Sizes of 14 Studies Examining the Efficacy of Aromatherapy Applications Used in the Management of Labor Pain.
| Heterogeneity | |||
|---|---|---|---|
| Q-value | Sd (Q) | p- value | I2 |
| 389.20 | 13 | .000 | 96.66 |
It can be seen from Table 6 that the Q statistic (Q=389.20; p = .000; significant at the 0.05 level) indicates that the studies' actual effect sizes are not uniform and homogeneous. Along with the Q statistic, the I2 statistic (96.66 %) value demonstrates that 95 % of the observed variance is caused by variations in the effect sizes of the studies included in the meta-analysis. I2 values of 25 %, 50 %, and 75 % were described as low, medium, and high heterogeneity by Higgins et al. in 2003 [20]. A significant degree of heterogeneity between the studies was discovered, and the effect size value calculated in accordance with the random effects model was taken into account when interpreting the results, according to the results of the heterogeneity test (Q and I2) carried out to determine which model will be used in the meta-analysis.
Discussion
It is frequently used during labor and delivery because it is non-pharmacological, safe, and economical [22]. By combining 14 studies that met specific criteria, this meta-analysis study, which aims to assess the level of effect of aromatherapy used in pain reduction on labor pain, was carried out. The studies included 2057 participants in total, 20 in each of the intervention and control groups. Jasmine oil was used in both the first and second stages of labor in both studies [23]; it was given to pregnant women in one of the studies that made up this meta-analysis during the first stage of labor [24], [25]. In the other 11 studies, aromatherapy was used in the first, second, and third stages of labor using one of the following oils: jasmine, lavender, rose, bitter orange, and boswellia. In 11 of the 14 studies included in the study, aromatherapy of jasmine, lavender, rose, bitter orange and boswellia oil [12], [23], [24], [26], [27], [28], [29], [30], [31], as well as mixed aromatherapy [13] perceived by pregnant women. It is seen that it has a reducing effect on labor pain. When the remaining studies are examined, it is seen that aromatherapy has no effect on labor pain in pregnant women in two studies in which lavender oil is applied [32], [33]; and in one study in which jasmine oil is applied [25].
In this study, it was found that eleven of the 14 studies that were included in the meta-analysis, in which aromatherapy with inhalation or massage method was applied individually or in combination, found that aromatherapy to be effective in the management of labor pain, and that it was ineffective in only three of them. In this regard, it has been determined that lavender oil is used the most in studies involving aromatherapy and that it significantly lessens labor pain. The meta-analysis's included studies' total effect size value was determined to be − 0.77 using the random effects model. According to Thalheimer and Cook's (2002) classification of effect levels, this effect size value shows that the results have a large effect size and are statistically significant (p < .050). The application of aromatherapy reduces the perception of pain in pregnant women, and the procedure has a positive impact on the intervention group, as indicated by the negative mean effect size value (−0.77). This makes it possible to say that the effects of aromatherapy, a non-pharmacological method, on the management of labor pain are better and more effective than those of other methods (methods used in control groups; distilled water, massage, saline, routine care).
Although aromatherapy has a wide range of uses, it does not receive enough scientific attention in the world and in our country. It is known that aromatherapy reduces medical interventions used in pain management and cesarean section rate in studies. However, for the clinical use of aromatherapy in studies, scientific studies covering a larger population and duration are needed. There is also a need for randomized controlled studies with high level of evidence to evaluate the effectiveness of the methods. It is thought that conducting studies comparing the effectiveness of the plant species preferred in aromatherapy application, the method of application, the effectiveness of single or combined use and the preferability of aromatherapy by users will contribute to this field. In addition, it is thought that the knowledge of health professionals about the use of aromatherapy and planning for the safe application of aromatherapy in care services may be effective in reducing the cost of health care services.
Conclusion
With its beneficial effects and numerous studies proving its efficacy, aromatherapy is recognized as a complementary approach that is growing in popularity. This meta-analysis showed that the use of aromatherapy with lavender oil, jasmine oil, rose oil, chamomile oil, bosweilla oil and bitter orange oil was effective in reducing pain as a non-pharmacological method in the first stage of labor. However, randomized controlled trials comparing the efficacy of various aromatherapy methods, individually or in combination with different methods of application (massage, breathing, etc.) are needed to evaluate the effectiveness of aromatherapy techniques.
Funding
There are no institutions and organizations that support and fund the study.
Author contributions
Study conception and design; AK, HYS, EK, EG.
Literature search and review; AK, HYS.
Data extraction, interpretation, and analysis; AK, HYS, EK, EG.
Manuscript preparation and revision; AK, HYS.
Critical revision of the paper; EK, EG.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Atike Kaya, Email: atike20102011@gmail.com.
Havva Yeşildere Sağlam, Email: havvayesildere@gmail.com.
Engin Karadağ, Email: engin.karadag@hotmail.com.
Elif Gürsoy, Email: elif070@gmail.com.
References
- 1.Shaterian N., et al. Labor pain in different dilatations of the cervix and apgar scores affected by aromatherapy: a systematic review and meta-analysis. Reprod Sci. 2021:1–17. doi: 10.1007/s43032-021-00666-4. [DOI] [PubMed] [Google Scholar]
- 2.Whitburn L.Y., et al. The meaning of labour pain: how the social environment and other contextual factors shape women’s experiences. BMC Pregnancy Childbirth. 2017;17(1):1–10. doi: 10.1186/s12884-017-1343-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khaskheli M., Baloch S. Subjective pain perceptions during labour and its management. J Pak Med Assoc. 2010;60(6):473–476. [PubMed] [Google Scholar]
- 4.Farnham T. Reviewing pain management options for patients in active labor. Nursing2021. 2020;50(6):24–30. doi: 10.1097/01.NURSE.0000662352.97953.cd. [DOI] [PubMed] [Google Scholar]
- 5.Shnol H., Paul N., Belfer I. Labor pain mechanisms. Int Anesthesiol Clin. 2014;52(3):1–17. doi: 10.1097/AIA.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 6.Adams J., et al. Use of pharmacological and non-pharmacological labour pain management techniques and their relationship to maternal and infant birth outcomes: examination of a nationally representative sample of 1835 pregnant women. Midwifery. 2015;31(4):458–463. doi: 10.1016/j.midw.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 7.Jones L., et al. Pain management for women in labour: an overview of systematic reviews. Cochrane Database Syst Rev. 2012;3 doi: 10.1002/14651858.CD009234.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jafari-Koulaee A., et al. A systematic review of the effects of aromatherapy with lavender essential oil on depression. Cent Asian J Glob Health. 2020;9(1) doi: 10.5195/cajgh.2020.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ali B., et al. Essential oils used in aromatherapy: a systemic review. Asian Pac J Trop Biomed. 2015;5(8):601–611. [Google Scholar]
- 10.Buckle J. Churchill Livingstone,; New York: 2015. Clinical aromatherapy, essential oil in healthcare; pp. 2–90. [Google Scholar]
- 11.Bertone A.C., Dekker R.L. Aromatherapy in obstetrics: a critical review of the literature. Clin Obstet Gynecol. 2021;64(3):572–588. doi: 10.1097/GRF.0000000000000622. [DOI] [PubMed] [Google Scholar]
- 12.Namazi M., et al. Aromatherapy with Citrus aurantium oil and anxiety during the first stage of labor. Iran Red Crescent Med J. 2014;16(6) doi: 10.5812/ircmj.18371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanvisut R., Traisrisilp K., Tongsong T. Efficacy of aromatherapy for reducing pain during labor: a randomized controlled trial. Arch Gynecol Obstet. 2018;297(5):1145–1150. doi: 10.1007/s00404-018-4700-1. [DOI] [PubMed] [Google Scholar]
- 14.Liao C.-C., et al. Aromatherapy intervention on anxiety and pain during first stage labour in nulliparous women: a systematic review and meta-analysis. J Obstet Gynaecol. 2021;41(1):21–31. doi: 10.1080/01443615.2019.1673707. [DOI] [PubMed] [Google Scholar]
- 15.Chen S.-F., et al. Labour pain control by aromatherapy: a meta-analysis of randomised controlled trials. Women Birth. 2019;32(4):327–335. doi: 10.1016/j.wombi.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 16.Tabatabaeichehr M., Mortazavi H. The effectiveness of aromatherapy in the management of labor pain and anxiety: a systematic review. Ethiop J Health Sci. 2020;30(3) doi: 10.4314/ejhs.v30i3.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joanna Briggs Institute JBI. Critical Appraisal Checklist for Randomized Controlled Trials. 2017; https://jbi.global/critical-appraisal-tools.
- 19.Sterne J.A., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. 2019;366 doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 20.Dinçer S. Pegem Akademi; Ankara: 2014. Uygulamalı meta analiz. [Google Scholar]
- 21.Thalheimer W., Cook S. How to calculate effect sizes from published research: a simplified methodology. Work-Learn Res. 2002;1(9) [Google Scholar]
- 22.Ergin A., Mallı P. Aromatherapy in childbirth: a systematic review. Kocaeli Üniversitesi Sağlık Bilim Derg. 2019;5(2):72–80. [Google Scholar]
- 23.Joseph R.M., Fernandes P. Effectiveness of jasmine oil massage on reduction of labor pain among primigravida mothers. J Health Allied Sci NU. 2013;3(04):104–107. [Google Scholar]
- 24.Kaviani M., et al. Comparison of the effect of aromatherapy with Jasminum officinale and Salvia officinale on pain severity and labor outcome in nulliparous women. Iran J Nurs Midwifery Res. 2014;19(6):666. [PMC free article] [PubMed] [Google Scholar]
- 25.Kaviani M., et al. The effect of aromatherapy with Salvia officinalis on the severity of labor pain in nulliparous women. Nurs Midwifery J. 2014;12(2):79–85. [PMC free article] [PubMed] [Google Scholar]
- 26.Alavi Fili A., et al. Comparison of effect of massage therapy with jasmine oil and aroma therapy with jasmine oil in reducing delivery pain. Iran J Obstet, Gynecol Infertil. 2017;20(3):40–47. [Google Scholar]
- 27.Cenkci Z., Nazik E. The effect of aromatherapy on pain, comfort and satisfaction during childbirth. New Trends Issues Proc Humanit Soc Sci. 2017;4(2):11–19. [Google Scholar]
- 28.Janula Raju M.S. Effectiveness of aromatherapy in reducing labour pain and duration of labour among primigravidas: a pilot study. Int J Health Sci Res (IJHSR) 2014;4(2):124–128. [Google Scholar]
- 29.Vakilian K., Keramat A., Gharacheh M. Controlled breathing with or without lavender aromatherapy for labor pain at the first stage: a randomized clinical trial. Crescent J Med Biol Sci. 2018;5(3):172–175. [Google Scholar]
- 30.Esmaelzadeh-Saeieh S., et al. The effects of inhalation aromatherapy with Boswellia carterii essential oil on the intensity of labor pain among nulliparous women. Nurs Midwifery Stud. 2018;7(2):45. [Google Scholar]
- 31.Hamdamian S., et al. Effects of aromatherapy with Rosa damascena on nulliparous women’s pain and anxiety of labor during first stage of labor. J Integr Med. 2018;16(2):120–125. doi: 10.1016/j.joim.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 32.Yazdkhasti M., Pirak A. The effect of aromatherapy with lavender essence on severity of labor pain and duration of labor in primiparous women. Complement Ther Clin Pract. 2016;25:81–86. doi: 10.1016/j.ctcp.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 33.Lamadah S.M., Nomani I. The effect of aromatherapy massage using lavender oil on the level of pain and anxiety during labour among primigravida women. Am J Nurs Sci. 2016;5(2):37–44. [Google Scholar]