Urinothorax, is the accumulation of urine in the pleural space, and is a rare and unusual condition.[1] Several etiologies are responsible for this, with trauma being the most common,[2] along with, surgical renal procedures (percutaneous nephrolithotomy, PCNL), retroperitoneal inflammation, urinary obstruction and malignancies.[3,4] Massive collections of a urinothorax or a hydrothorax can lead to tension, mediastinal shifts and cardiac arrests. We describe a case of tension urinothorax that led to cardiac arrest and was resuscitated successfully in the emergency department (ED).
CASE
A 42-year-old patient with a past history of hypertension, was brought to the ED with a clinical picture of an acute onset of respiratory distress, progressively worsening in the past 2 h and associated with sweating. On arrival, the patient had the following vitals: blood pressure not recordable, pulse rate 68 beats/min, respiratory rate 30 breaths/min, oxygen saturation 60% on room air, blood sugar 189 mg/dL and temperature 36.8 °C. The patient had a pigtail catheter in situ in the right lumbar region.
Soon after the primary survey, the patient went into cardiac arrest. Cardiopulmonary resuscitation (CPR) was started while the team took history from the family and treating physician. The patients’ attendants gave a history of discharge from the hospital a day earlier. Of note was that the patient had undergone right-sided PCNL for an obstructive calculus one week before arrival. During that same admission, the patient had suffered from a right sided pleural effusion that had been drained. It was suspected that the patient possibly had a recurrence of pleural effusion leading to hypoxic arrest. During chest compression pause and intubation, an X-ray of the chest was quickly performed. To our surprise, the X-ray was suggestive of complete opacification of the right hemithorax with collapse of the underlying lung (Figure 1A). We suspected this to be a tension hydrothorax leading to a tamponade effect. CPR was continued while a tube thoracostomy in the right 5th intercostal space was performed. A 28F intercostal drainage tube was placed, almost 4 liters of fluid was initially drained and immediately a return of spontaneous circulation (ROSC) was achieved. Post ROSC, the X-ray showed lung expansion and partial clearance of the fluid and no evidence of midline shifts (Figure 1B). The drained straw-coloured fluid had a suspicious pungent smell of ammonia. Pleural fluid creatinine was thus sent in view of a possible urinothorax. Post ROSC, the patient’s vitals were as follows: blood pressure 90/72 mmHg (1 mmHg=0.133 kPa), heart rate 109 beats/min, respiratory rate 22 breaths/min on mechanical ventilator, oxygen saturation of 100% on ventilator support, temperature 35.8 °C, blood sugar 195 mg/dL. Post ROSC targeted temperature management was also initiated. His blood work was significant for troponin 0.05 ng/mL, international normalized ratio (INR) 1.18, serum creatinin 7.13 mg/dL, serum uric acid 11.3 mg/dL, HCO3- 10.53 mmol/L, serum urea 150.7 mg/dL. Arterial blood gas was taken which was significant for the following: pH 7.128, pCO2 40 mmHg, pO2 56.6 mmHg, Na+ 124 mmol/L, K+ 5.7 mmol/L, Cl- 103 mmol/L, strong ion difference (SID) 21 mmol/L, Lac 4.3 mmol/L, glucose 278 mg/dL, hemoglobin 9.3 g/dL. Pleural fluid creatinine was 34.6 mg/dL, compared to serum creatinine, which confirmed our diagnosis of urinothorax. Point of care ultrasound (POCUS) was performed while CPR was ongoing and showed massive pleural effusion. A pleural fluid to serum creatinine ratio greater than 1 often supports the diagnosis of urinothorax, whereas a ratio greater than 1.7 may be considered diagnostic, which in our case was 20.6:1.[1] In view of shock, inotropic support was started with noradrenaline infusion at a rate of 20 mL/h (10 μg/min in a 50 mL syringe via an infusion pump) and a sodium bicarbonate infusion at the rate of 20 mL/h (5 mEq/kg titrated in a 50 mL syringe via an infusion pump). Post intubation, sedation was started with fentanyl at the rate of 50 μg/h and maintenance balanced crystalloids at the rate of 100 mL/h. The patient was shifted to the intensive care unit under a multi-disciplinary team. He later developed massive intracerebral hemorrhage and finally succumbed to his illness after a month long stay in the hospital.
Figure 1.
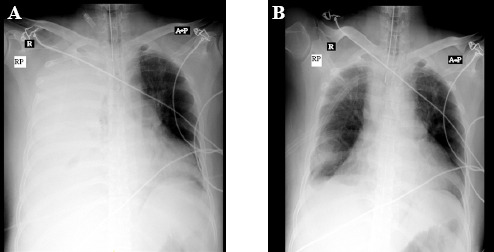
The X-rays of the patient. A: pre-tube thoracostomy (patient still in cardiac arrest); B: post-tube thoracostomy draining the urine (ROSC achieved).
DISCUSSION
It is believed that the first case of urinothorax in the medical literature, was described by France and Back in 1954,[5] but for most, the first case was described by Corriere et al in 1968.[6] A systematic review found 88 case reports and series of urinothorax over the past 62 years[7] which shows how rare this occurrence is. It was found that the effusion was mostly unilateral (87%), covering over two-thirds of the hemithorax in most cases (64%), and was straw-coloured mostly (72%) but in all of the occurrences, the fluid smelled like urine.[7] Urinothorax is a highly misdiagnosed and undiagnosed condition[1] that occurs due to retroperitoneal leakage and accumulation of urine within the pleural cavity. A high degree of suspicion is required to diagnose this condition, as the patient may present with mild, moderate or severe respiratory complaints. Multiple radiographic modalities are currently available to help diagnose this condition, starting from chest radiographs, which tend to show extensive pleural effusions and possible lung collapse. Intravenous pyelography (IVP), can show the leakage of contrast from the retroperitoneal space to the pleural cavity, but with the advent of computed tomography (CT), it has become indispensable in diagnosis and treatment.[8] Studies have suggested two theories for the phenomena of transdiaphragmatic evasion of urine: (i) lymphatic drainage of urine[9,10] and (ii) direct collection of urine through a tract for drainage into the pleural cavity.[11] Since there are few incidences of urinothorax throughout the literature, it is difficult to diagnose, treat and distinguish this condition. Often, a patient presents with complaints of dyspnea, flank pain, fever and tachypnea.[12,13] For the detection of urinothorax, multiple radiographic and laboratory investigative modalities are available. The most common and initial modality is chest radiography, which is capable of showing massive pleural effusions, along with IVP to look for leakage of the contrast from the kidney or ureter, but is seldom brought into use.[3,4] Abdominal and thoracic CT scans and technetium-99m-labeled diethylenetriaminepentaacetate (99mTc-DTPA) scans are also now being used in certain cases.[3,8,10] The diagnoses of urinoma are made by thoracocentesis to examine the pleural fluid biochemically.[14] The fluid is usually straw-coloured with the distinctive smell of urine.[12] In the majority of cases, it is proven to be transudative, with low glucose, low pH, the possibility of high lactate dehydrogenase (LDH) and low protein concentration.[12,15] Despite all this, the most critical parameter to diagnose urinothorax, is the pleural fluid creatinine to serum creatinine ratio, which is higher than 1 and, in most cases, greater than 10.[12,14] Our patient had a ratio of 20.6:1, which confirmed our diagnosis. The treatment for urinothorax is straightforward, and corrects the underlying cause, which is thoracocentesis. [16] The majority of cases are unilateral, but bilateral and contralateral cases of urinothorax have also been reported.[10,14] In our case, the patient had an ipsilateral urinothorax that presented post PCNL surgery in the right kidney.
Numerous EDs todays are also equipped with their own ultrasound machines. In our case also, since an ultrasound machine was available, it was utilized during the CPR session, before obtaining a chest X-ray to try and find the cause for reduced chest rise on one side. Ultrasounds allow for the detection of fluids amounting from as small as 3–5 mL in the thorax, in contrast to radiography, which can detect fluid beyond 50 mL. Ultrasounds also help establish a distinction between loculated fluid pockets and thickened pleura and can also assist in guiding thoracocentesis. The defining features for fluid in pleural spaces are the Quad sign and Sinusoid sign. The Quad sign helps establish the boundaries of the pleural effusion seen between two ribs, whereas the Sinusoid sign shows a decrease in the depth of the effusion during inspiration in the M-mode. In the B-mode, when the lung is fully submerged in fluid, it depicts jellyfish-like behavior and hence is called the jellyfish sign, which is a subset of the Sinusoid sign.[17]
American Heart Association guidelines for cardiopulmonary resuscitation advise about the effectiveness of ruling out the 5H’s and 5T’s for achieving ROSC, which gives a higher chance of survival of patients in cardiac arrest.[18] It is of note that tension hydrothorax should also be taken into account by emergency physicians, with the provision of an adequate history, as a reversible cause of cardiac arrest. Of all the indexes searched, none of the cases of urinothorax went into cardiac arrest. Few studies cited had patients who were in the pre-arrest clinical picture, but our patient went into cardiac arrest on arrival and was resuscitated after draining the hydrothorax thus emphasizing the clinical situation. In 2016, Casallas et al[19] comprehensively described all the cases of urinothorax published with their consequent causes. Of the 34 case reports and 44 patients described, the majority were men, with ages ranging from 3 months to 82 years old. The most common underlying conditions were neoplasms, nephrolithiasis, gynaecological diseases, car accidents, renal failure, vesicoureteral reflux and renal dysplasia (VURD), benign prostatic hyperplasia (BPH), hydroureteronephrosis and urinary tract infections.
It is essential to note that the ACLS protocol mentions different reversible causes for cardiac arrest that should be taken into account while resuscitating a patient. One unmentioned cause, with appropriate history as discussed in the case, is the presence of a tension pleural effusion, which once relieved immediately may lead to the ROSC. It is vital that good history taking and prompt actions are needed in all cases of cardiac arrest, and in the case presented, placing a tube thoracostomy stat while CPR was going on, led to the revival of the patient. We understand that since the case is rare, the chance of receiving many patients in such a manner is a scarcity, but each life matters and this could help save one of them.
CONCLUSION
It would be prudent for emergency physicians to remember that any hydrothorax especially urinothorax, can quickly escalate to tension, causing a tamponade effect leading to cardiac arrest.
Footnotes
Funding: The authors have not received any funding for this manuscript.
Ethical approval: Not needed.
Conflicts of interest: The authors have no competing interests.
Author contribution: AW and AV are the primary authors and contributed towards report conceptualization, writing and literature review. All other co-authors contributed to the literature review, editing and proofreading.
REFERENCES
- 1.Laskaridis L, Kampantais S, Toutziaris C, Chachopoulos B, Perdikis I, Tahmatzopoulos A, et al. Urinothorax-an underdiagnosed cause of acute dyspnea:report of a bilateral and of an ipsilateral urinothorax case. Case Rep Emerg Med. 2012;2012:395653. doi: 10.1155/2012/395653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leung FW, Williams AJ, Oill PA. Pleural effusion associated with urinary tract obstruction:support for a hypothesis. Thorax. 1981;36(8):632–3. doi: 10.1136/thx.36.8.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhattacharya A, Venkataramarao SH, Kumar S, Mittal BR. Urinothorax demonstrated on 99m Tc ethylene dicysteine renal scintigraphy. Nephrol Dial Transplant. 2007;22(6):1782–3. doi: 10.1093/ndt/gfm105. [DOI] [PubMed] [Google Scholar]
- 4.Salcedo JR. Urinothorax:report of 4 cases and review of the literature. J Urol. 1986;135(4):805–8. doi: 10.1016/s0022-5347(17)45862-9. [DOI] [PubMed] [Google Scholar]
- 5.France NE, Back EH. Neonatal ascites associated with urethral obstruction. Arch Dis Child. 1954;29(148):565–8. doi: 10.1136/adc.29.148.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corriere JN, Miller WT, Murphy JJ. Hydronephrosis as a cause of pleural effusion. Radiology. 1968;90(1):79–84. doi: 10.1148/90.1.79. [DOI] [PubMed] [Google Scholar]
- 7.Toubes ME, Lama A, Ferreiro L, Golpe A, Álvarez-Dobaño JM, González-Barcala FJ, et al. Urinothorax:a systematic review. J Thorac Dis. 2017;9(5):1209–18. doi: 10.21037/jtd.2017.04.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jelic S, Sampogna RV. Detection of unrecognized urinothorax with renal scintigraphy. Kidney Int. 2009;76(3):353. doi: 10.1038/ki.2009.149. [DOI] [PubMed] [Google Scholar]
- 9.Nusser RA, Culhane RH. Recurrent transudative effusion with an abdominal mass Urinothorax. Chest. 1986;90(2):263–4. doi: 10.1378/chest.90.2.263. [DOI] [PubMed] [Google Scholar]
- 10.Ralston MD, Wilkinson RH., Jr Bilateral urinothorax identified by technetium-99m DPTA renal imaging. J Nucl Med. 1986;27(1):56–9. [PubMed] [Google Scholar]
- 11.Ferreira PG, Furriel F, Ferreira AJ. Urinothorax as an unusual type of pleural effusion - clinical report and review. Rev Port Pneumol. 2013;19(2):80–3. doi: 10.1016/j.rppneu.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Pachon E, Padilla-Navas I. Urinothorax:case report and review of the literature with emphasis on biochemical diagnosis. Respiration. 2004;71(5):533–6. doi: 10.1159/000080642. [DOI] [PubMed] [Google Scholar]
- 13.Tortora A, Casciani E, Kharrub Z, Gualdi G. Urinothorax:an unexpected cause of severe dyspnea. Emerg Radiol. 2006;12(4):189–91. doi: 10.1007/s10140-006-0468-x. [DOI] [PubMed] [Google Scholar]
- 14.Handa A, Agarwal R, Aggarwal AN. Urinothorax:an unusual cause of pleural effusion. Singapore Med J. 2007;48(11):e289–e292. [PubMed] [Google Scholar]
- 15.Light RW. Pleural effusions:the diagnostic separation of transudates and exudates. Ann Intern Med. 1972;77(4):507. doi: 10.7326/0003-4819-77-4-507. [DOI] [PubMed] [Google Scholar]
- 16.Vinck EE, Garzón JC, Peterson T, Villarreal R, Cabrera L, Van den Eijnden L. Tension hydrothorax:emergency decompression of a pleural cause of cardiac tamponade. Am J Emerg Med. 2018;36(8):1524.e1–1524.e4. doi: 10.1016/j.ajem.2018.04.041. [DOI] [PubMed] [Google Scholar]
- 17.Esmadi M, Lone N, Ahmad DS, Onofrio J, Brush RG. Multiloculated pleural effusion detected by ultrasound only in a critically-ill patient. Am J Case Rep. 2013;14:63–6. doi: 10.12659/AJCR.883816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3:adult basic and advanced life support:2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142(16_suppl_2):S366–S468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 19.Casallas A, Castañeda-Cardona C, Rosselli D. Urinothorax:Case report and systematic review of the literature. Urol Ann. 2016;8(1):91–4. doi: 10.4103/0974-7796.164851. [DOI] [PMC free article] [PubMed] [Google Scholar]


