Abstract
Objectives
To evaluate whether the quality of orthodontic finishing influences long-term stability of anterior tooth alignment.
Materials and Methods
This retrospective study evaluated 38 patients. Data were obtained at the beginning of treatment (T0), at the end (T1), and at least 5 years after T1 (T2). At this point, the individuals were no longer wearing retainers. Anterior tooth alignment was measured using Little's index (LI). Effect on alignment stability was tested with multiple linear regression using LI–T0, LI–T1, intercanine width difference T1–T0, overbite (T1), overjet (T1), age, gender, time without retention, and presence of third molars as predictor variables. Well-aligned (LI < 1.5 mm) and misaligned (LI > 1.5 mm) cases were compared at T2.
Results
At T2, the alignment stability in the upper arch was inversely associated with the alignment quality (R2 = 0.378, P < .001) and directly associated with overbite (R2 = 0.113, P = .008) at T1. Posttreatment changes caused cases finished with poor alignment to become similar to those finished with excellent alignment (P = .917). In the mandible, posttreatment changes were directly associated only with overjet (R2 = 0.152, P = .015) and well-finished cases displayed better alignment than poorly finished cases (P = .011). Other variables showed no significant association.
Conclusions
In arches without retention, better quality of orthodontic finishing does not guarantee the stability of anterior alignment. In the maxilla, long-term changes were more significant the greater the overbite and the better the quality of alignment at end of treatment. In the mandible, changes were not dependent on the quality of finishing but were associated with greater overbite at T2.
Keywords: Orthodontics, Orthodontic finishing, Anterior tooth alignment
INTRODUCTION
Several factors might be associated with the stability of anterior alignment after orthodontic treatment.1,2 Maintenance of the arch form has been related to better posttreatment stability. Intercanine and intermolar widths tend to decrease in the postretention period, especially if dental arches were expanded during treatment.3 The presence of third molars is routinely blamed for posttreatment tooth alignment changes, although there is no scientific evidence to support a causal relationship.4
There is some evidence that retention is the only approach capable of maintaining long-term stability.2 Nevertheless, some experts argue that quality of finishing could contribute to alignment stability and advocate that prolonged use of a retainer may be unnecessary in cases with excellent alignment. The influence of the quality of finishing on stability has been poorly investigated. Some studies reported that the excellent quality of orthodontics does not seem to prevent relapse,5–7 and even the better the quality of occlusion at the end of treatment, the greater the relapse.7 However, occlusion in the postretention phase still has better quality in well-finished cases compared to cases finished with deficiencies.5,7 In turn, one study demonstrated that the quality of finishing may reduce the risk of relapse in patients with Class III malocclusions.8 Nonetheless, these studies evaluated occlusion using the Peer Assessment Rating (PAR) Index.9 The PAR index is not specific and sensitive enough to evaluate the alignment of anterior teeth, which is an occlusal component with a high incidence of relapse.
Anterior esthetics is of great importance for patients,10 and tooth alignment produced by orthodontic treatment has a significant effect on quality of life.11 Hence, predicting alignment stability based on the quality of anterior alignment is relevant to the decision to maintain orthodontic retainers. Therefore, this study aimed to evaluate whether the quality of orthodontic finishing influenced the long-term stability of anterior tooth alignment.
MATERIAL AND METHODS
Ethical Considerations
This study was approved by the Research Ethics Committee of the Federal University of Pará under protocol no. 45537321.4.0000.0018.
Study Design, Participants, and Eligibility Criteria
This was a retrospective study written according to the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) guidelines.12 The individuals evaluated were selected from a convenience sample consisting of 58 patients treated orthodontically in a private clinic located in Natal, Brazil. The analysis of the models and clinical records was performed between February and March 2021.
Plaster models of all patients included in the sample were obtained at the beginning of treatment (T0), at the end (T1), and after a minimum period of 5 years after removal of the orthodontic appliances (T2). The retention protocol was a Hawley plate and a 3 × 3 retainer made with 0.7-mm steel wire bonded to all teeth in the upper and lower arch. At T2, all patients had discontinued use of retainers by choice. This happened from 1 month to 1 year after the debonding of orthodontic appliances, and at least 4 years before the T2 evaluation.
Patients with damaged models, missing or partially erupted anterior teeth, anterior diastemas after treatment (T1), craniofacial syndromes, or surgical patients were excluded.
Variables Analyzed, Data Source, Measurements
To evaluate the quality of anterior finishing, Little's index (LI) was measured on plaster models at T0, T1, and T2.13 The difference between LI at T1 and T2 represented treatment stability after at least 5 years. The intercanine width (ICW) at T0 and T1 was measured using the cusp of the canine as the reference. Overjet and overbite were also assessed. Measurements were performed by a single operator using a digital caliper with a precision of 0.01 mm (Digimess, São Paulo, Brazil).
To investigate whether cases with excellent anterior alignment remained better than cases with some alignment deficiency, subjects were divided into well-finished cases in which the LI at T1 was less than or equal to 1.5 mm (maxilla: n = 20; mandible: n = 17), and cases finished with deficiencies when the LI–T1 was >1.5 mm (maxilla: n = 21; mandible: n = 21). The 1.5-mm limit was used assuming an average of 0.3 mm of displacement per contact point between the anterior teeth since lower values would be close to the resolution limit of the human eye. The subgroups were compared at T1 and T2.
All patients had both models, and they were used for the proposed interarch analyses. However, in some specific situations, such as a broken lateral incisor or a lower arch with retention at T2, it was not possible to measure the LI of that arch, but this did not prevent it from being used to measure the other variables. Data related to gender, age, presence of a third molar, and time without retainers were collected from clinical records, dental casts, and panoramic radiographs.
Statistical Analysis
Twenty models were randomly chosen and reevaluated after 30 days to analyze the method error. The random and systematic errors were analyzed using the Bland-Altman method.
The Shapiro-Wilk test was used to check data distribution. The effect of the finishing quality on anterior stability was investigated using multiple linear regression. The dependent variable analyzed was the posttreatment change obtained by the LI difference between T2 and T1. The independent variables were: LI in the upper and lower arches at T0 and T1; ICW T1–T0; overbite; overjet; age at T1; time without the use of a Hawley plate and a lower fixed retainer; and the presence of the third molar. Initially, the association of each independent variable with the dependent variable was tested through simple regression analysis. Then, the independent variables that presented with a P value < .10 were included in multiple regression analysis complemented with stepwise regression.
The independent t-test was used to compare cases finished with excellent alignment (LI < 1.5) with those finished with some deficiency (LI > 1.5). All statistical tests were performed using jamovi software (version 1.6.16, Sydney, Australia) with a significance level of 5%.
RESULTS
Participants
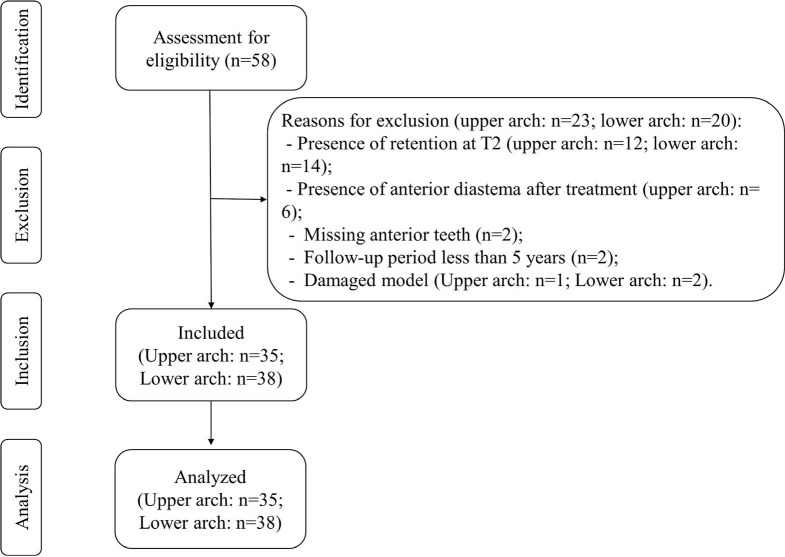
Of the 58 patients initially evaluated, 23 were excluded for the upper arch analysis and 20 for the lower arch analysis after evaluation of the models and clinical records. The reasons for exclusion included the presence of a retainer at T2 (maxilla: n = 12; mandible: n = 14); presence of an anterior diastema at T1 (maxilla: n = 6); missing anterior teeth (n = 2); follow-up time at T2 less than 5 years (n = 2); and a damaged model (maxilla: n = 1; mandible: n = 2) (Figure 1).
Figure 1.
Flow chart illustrating the selection of participants throughout the study.
Descriptive Data
For the upper arch analysis, models from 25 females (71.4%) and 10 males (28.6%) were included. The lower arches of 26 females (68.4%) and 12 males (32.6%) were analyzed. The mean age was 13.63 (±6.74) years at T0, 16.30 at T1 (±6.63), and 23.64 (±6.65) at T2. The mean posttreatment follow-up time was 7.68 (±1.89) years.
The period without a retainer for the upper arch was 7.22 years (±1.66). For the lower arch, the time without retention was 7.24 (±1.77) years. Fourteen subjects (40%) had at least one upper third molar at T2, while at least one mandibular third molar was present in 12 patients (31.6%).
At T1, the mean overbite was 1.79 mm (±0.82), while the mean overjet was 0.92 (±0.86). The mean difference of the ICW T1–T0 was 1.84 (±2.17) in the maxilla and 0.19 (±1.90) in the mandible. The LI in the upper arch was 5.85 (±2.78) mm at T0, 1.55 (±1.01) mm at T1, and 2.54 (±1.17) mm at T2. In the lower arch, the mean was 4.25 (±2.26) at T0, 1.86 (±1.08) mm at T1, and 3.19 (±1.94) mm at T2. The difference of LI T2–T1 (stability) was 0.98 mm (±1.48) in the upper arch and 1.28 (±1.89) in the lower arch (Table 1).
Table 1. .
Descriptive Statistics. Evaluated Arches (n), Sex and the Presence of Third Molars. Mean and Standard Deviation (SD) for Age, Follow-Up Time, Years Without Retention, Overbite, Overjet, Intercanine Width (ICW), Little's Index (LI), and Posttreatment Changes (LI T2–T1)a
|
Sample (F/M) |
Mean Age in Years (±SD) |
Follow-Up Period in Years (±SD) |
Years Without Upper Hawley Retainer (±SD) |
Years Without Lower 3X3 Retainer (±SD) |
| Upper arch: 35 (25/10); Lower arch: 38 (26/12). | T0: 13.63 (±6.74) | 7.68 (±1.89) | 7.39 (±1.96) | 7.19 (±1.66) |
| T1: 15.97 (±6.63) | ||||
| T2: 23.64 (±6.65) |
F indicates female; m, male.
Table 1. .
Extended
|
Presence of Third Molars |
Overbite/Overjet at T1 |
ICW T1–T0 (±SD) |
Upper LI in Millimeters (±SD) |
Lower LI in Millimeters (±SD) |
LI T2–T1 (±SD) |
| Upper: present in 14 (40%), absent in 21 (60%); Lower: present in 12 (31.6%), absent in 26 (68.4%) | 1.79 (±0.82); 0.92 (±0.82) | Upper arch: 1.88 (±2.22); Lower arch: 0.11 (±1.87) | T0: 5.83 (±2.86) | T0: 4.22 (±2.38) | Upper arch: 0.98 (±1.48); Lower arch: 1.25 (±1.86) |
| T1: 1.55 (±1.01) | T1: 1.94 (±1.15) | ||||
| T2: 2.54 (±1.17) | T2: 3.19 (±1.94) |
Main Results
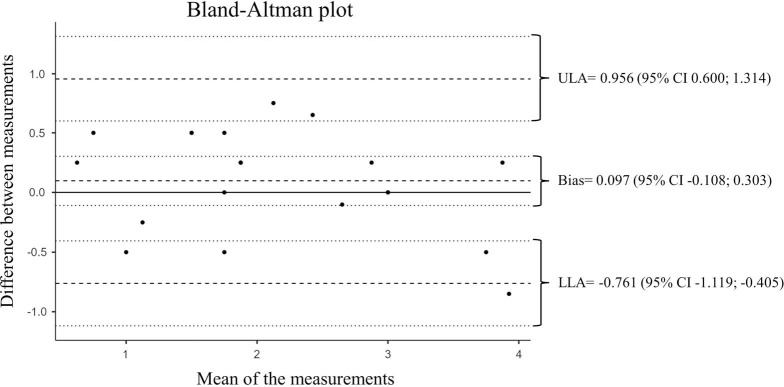
The systematic error (bias) of the mean difference was 0.097 (95% CI: –0.108 to 0.303). The random error had an upper limit of agreement (ULA) of 0.956 (95% CI: 0.600 to 1.314) and a lower limit of agreement (LLA) of –0.761 (95% CI: –1.119 to –0.405). The results remained within the confidence interval, with no outliers, and showed good agreement between the measurements and variation without clinical significance between the measurements (Figure 2).
Figure 2.
Bland-Altman scatter plot comparing the measurements for the two time periods.
For the maxilla, simple regression revealed a significant association between posttreatment changes in the anterior alignment (LI T2–T1) and the variables LI–T1 (P < .001) and overbite (P = .043). The other variables did not reach a P value of <.10. In the multiple regression, LI–T1 (β = –0.910, P = <.001) showed an inverse association with LI T2–T1, while overbite showed a direct relationship (β = 0.064, P = .008). The two variables together determined 47.2% (R2 = 0.472) of the posttreatment changes in the anterior tooth alignment in the upper arch. Stepwise regression revealed a 37.8% determination for LI–T1 (R2 = 0.378), 11.3% for overbite at T1 (R2 = 0.113) (Table 2).
Table 2. .
Analysis Using Simple Linear Regression and Multiple Linear Regression Model of Variables Associated With Posttreatment Changes in Maxillary Anterior Tooth Alignment (Dependent Variable)a
|
Dependent Variables |
Simple Regression |
Multiple Regression Model |
|||||||||
|
Multiple |
Stepwise |
||||||||||
|
P Value |
Adjusted P Value |
95% CI |
B Value |
R2 |
Adjusted R2 |
F Test |
P Value |
R2 |
Adjusted R2 |
||
|
Lower |
Upper |
||||||||||
| LI at T1 | <.001* | <.001* | –1.280 | –0.536 | –0.910 | 0.503 | 0.472 | 16.2 | <.001* | 0.378 | 0.359 |
| Overbite | .043* | .008* | 0.008 | 0.120 | 0.064 | <.001* | 0.503 | 0.472 | |||
| Overjet | .463 | ||||||||||
| Age at T1 | .175 | ||||||||||
| ICW T1–T0 | .930 | ||||||||||
| LI at T0 | .375 | ||||||||||
| Years without upper Hawley retainer | .387 | ||||||||||
| Sex | .406 | ||||||||||
| Presence of third molar | .497 | ||||||||||
CI indicates confidence interval; *, statistical significance.
In the mandible, simple regression detected an association between posttreatment changes in the anterior alignment (LI T2–T1) and the variables LI–T1 (P = .046), ICW T1–T0 (P = .031), and overjet (P = .015). The other variables did not reach a P value of <.10. Analyzing the multiple regression, the only variable that showed a significant association was overjet (β = –0.826, P = .015). However, the model that showed the best prediction was the one that included overjet and ICW T1–T0 (β = 0.303, P = .057). These variables determined posttreatment changes in alignment of 29.2% (R2 = 0.292) (Table 3). If the variable LI–T1 (P = .452) was included in the multiple regression, the model lost predictive ability, so this variable was excluded in the final model.
Table 3. .
Analysis Using Simple Linear Regression and Multiple Linear Regression Model of Variables Associated With Posttreatment Changes in Lower Arch Anterior Tooth Alignment (Dependent Variable)a
|
Dependent Variables |
Simple Regression Model |
Multiple Regression Model |
|||||||||
|
Multiple |
Stepwise |
||||||||||
|
P Value |
Adjusted P Value |
95% CI |
B Value |
R2 |
Adjusted R2 |
F Test |
P Value |
R2 |
Adjusted R2 |
||
|
Lower |
Upper |
||||||||||
| Overjet | .015* | .015* | –1.510 | –0.183 | –0.826 | 0.345 | 0.292 | 6.58 | .031* | 0.152 | 0.129 |
| ICW T1–T0 | .031* | .063 | –0.018 | 0.614 | 0.303 | .057 | 0.345 | 0.292 | |||
| LI at T1 | .046* | .452 | |||||||||
| Overbite | .651 | ||||||||||
| LI at T0 | .481 | ||||||||||
| Age at T1 | .979 | ||||||||||
| Years without upper Hawley retainer | .804 | ||||||||||
| Sex | .791 | ||||||||||
| Presence of third molar | .991 | ||||||||||
CI indicates confidence interval; *, statistical significance.
Post hoc sample size calculation for the multiple linear regression using G*Power software (version 3.1.9.6, Kiel University, Germany) showed a power of 96.56% for the upper arch (two-tail, effect size: f2 ≈ 0. 8939; α = 0.001, sample size = 35, number of predictor variables = 2) and 87.52% for the lower arch (two=tail, effect size: f2 ≈ 0.3888; α = 0.012, sample size = 38, number of predictor variables = 3).
At T1, the mean LI among the best-finished cases was 0.72 ± 0.48 mm in the upper arch and 0.98 ± 0.53 mm in the lower arch. The cases finished with some deficiency had LI of 2.43 ± 0.58 mm in the maxilla and LI of 2.71 ± 0.91 mm in the mandible. At T2, only for the lower arch (P = .011) the best finished cases showed better alignment (2.32 ± 1.34 mm) than those finished with some deficiency (3.89 ± 2.09 mm). For the upper arch, no statistical difference was found between the groups (P = .917) (Table 4).
Table 4. .
Comparison of LI Between Better Finished and Worst Finished Cases at T1 and T2 by Independent t-Test
|
|
Group |
n |
Mean (SD) |
Mean Difference (mm) |
95% CI |
P Value |
|
|
Lower |
Upper |
||||||
| Upper LI at T1 | Better finished cases | 18 | 0.72 (±0.48) | –1.71 | –2.070 | –1.350 | <.001* |
| Cases finished with deficiency | 17 | 2.43 (±0.58) | |||||
| Lower LI at T1 | Better finished cases | 17 | 0.98 (±0.53) | –1.73 | –2.230 | –1.220 | <.001* |
| Cases finished with deficiency | 21 | 2.71 (±0.91) | |||||
| Upper LI at T2 | Better finished cases | 18 | 2.52 (±1.48) | –0.04 | –0.861 | 0.777 | .917 |
| Cases finished with deficiency | 17 | 2.56 (±0.76) | |||||
| Lower LI at T2 | Better finished cases | 17 | 2.32 (±1.34) | –1.57 | –2.760 | –0.386 | .011* |
| Cases finished with deficiency | 21 | 3.89 (±2.09) | |||||
Statistical significance.
DISCUSSION
This study focused on the effect of the quality of anterior tooth alignment with treatment stability. In the mandible, the quality of alignment at the end of orthodontic treatment did not affect posttreatment anterior tooth alignment changes. However, in the upper arch, the better the treatment finishing, the greater the posttreatment tooth alignment changes. In well-treated cases with a LI close to zero at T1, tooth alignment worsened after retainer removal, characterizing a regression to the mean. Well-finished cases tend to end treatment without diastemas, especially anterior diastemas. In this study, patients with anterior diastemas were excluded from the final sample, and only cases finished with tight anterior contact points were used, making the sample more homogeneous.
A study evaluating patients after 10 years without retention concluded that the greater the change in alignment during treatment, the greater the posttreatment changes.14 In this way, the amount of movement of the anterior teeth during treatment is being evaluated to determine its effect on the stability of their alignment. Perhaps, it is not the difference between the initial and posttreatment alignment that affects stability, but rather this variable at T0 or T1. In the present study, initial anterior tooth alignment showed no association with posttreatment changes. This was in contrast to alignment in the upper arch at T1 in which, the better the initial alignment, the greater the posttreatment changes. In the lower arch, LI–T1 showed no association with LI T2–T1.
Over the years, arch dimensions tend to gradually decrease15,16 and the lower arch seems to be more susceptible to transverse reduction than the upper arch. A previous study reported that a decrease of 4 mm was observed in the mandible while no change in arch perimeter was found in the maxilla of patients between the ages of 5 and 31 years.16 A study evaluating subjects with normal occlusion over a period of 40 years reported a decrease in ICW only in the mandible.15 In the present study, regression analysis showed that changes in ICW during treatment did not predict posttreatment changes in the anterior alignment of cases when adjusted to other variables.
Regarding overbite, there was a direct association with LI T2–T1 in the upper arch but not for the lower arch. In turn, overjet only showed a direct association with LI T2–T1 in the mandible. Another retrospective study found no association between these variables and posttreatment changes in anterior alignment.17 Nonetheless, the sample in that study used retainers for a longer period (3.3 years, 95% CI: 2.85–3.69) and spent less time without retainers (2.6 years, 95% CI: 2.0–3.1), which may have influenced the results. In the current study, the greater the overbite and overjet at the end of treatment, the more changes were observed in the upper and lower tooth alignment, respectively. Therefore, orthodontists should seek to finish their cases with adequate overjet and overbite to provide better stability of anterior tooth alignment after orthodontic treatment.
In older patients, especially those with periodontal involvement, there could be a tendency for greater instability in the anterior alignment due to the loss of alveolar bone in this region.18 In the present study, age had no effect on the LI T2–T1. The mean age was 16.30 years at T1 and 23.64 at T2, with only one individual older than 30 years at both time points. Therefore, changes in anterior posttreatment alignment due to alveolar bone loss may not have been observed because of the relatively short observation time and/or age range examined.
The presence of third molars was not associated with posttreatment changes in any dental arch, demonstrating that the removal of these teeth to avoid tertiary crowding is not justified. This finding reinforces previous observations reported in several studies that found no association between the presence of third molars and posttreatment anterior crowding.5
Regarding use of retainers, the number of years without the use of the upper retainer and the lower retainer showed no association with posttreatment changes in anterior alignment. In the current study, the subjects in the sample spent almost the entire posttreatment period without a retainer, 7.22 (±1.66) years without the lower fixed retainer and 7.24 (±1.77) years without the upper Hawley. However, even after a long period of time using a fixed retainer, relapse can be expected, especially in the lower arch.2 Thus, it seems that regardless of how long the retainer is used, when removed, tooth alignment tends to worsen. The cases that had better alignment in the upper arch worsened to the point that, after the follow-up period, there was no difference between them and the worst-finished cases. In the lower arch, alignment also worsened. Nevertheless, the better finished cases presented better alignment at T2 than the poorly finished ones. This may indicate that, even in cases with excellent anterior tooth alignment, use of a retainer for long periods of time seems to be a way to preserve the alignment after orthodontic treatment.
Limitations
Due to its retrospective nature, this study may be subject to selection bias and lack of control of variables. Attempts were made to control these risks through the eligibility criteria and a regression model to control confounding factors. However, variables such as residual growth and loss of oversight after orthodontic treatment were not possible to control. Hence, there is a need for better conducted prospective studies that can control these factors and improve the level of evidence.
CONCLUSIONS
Quality of anterior alignment obtained during treatment does not ensure posttreatment alignment stability in cases without retention. Therefore, retention seems necessary even in well-finished cases.
In the maxilla, the better the dental alignment at the end of treatment the greater the posttreatment changes. Furthermore, the greater the overbite, the more susceptible the alignment becomes to posttreatment changes.
In the mandible, the quality of orthodontic finishing does not improve the long-term stability of alignment. Additionally, the greater the overjet, the more susceptible the alignment becomes to posttreatment changes.
REFERENCES
- 1.Park H, Boley JC, Alexander RA, Buschang PH. Age-related long-term posttreatment occlusal and arch changes Angle Orthod 2010. 80 247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steinnes J, Johnsen G, Kerosuo H. Stability of orthodontic treatment outcome in relation to retention status: an 8-year follow-up Am J Orthod Dentofacial Orthop 2017. 151 1027–1033. [DOI] [PubMed] [Google Scholar]
- 3.Myser SA, Campbell PM, Boley J, Buschang PH. Long-term stability: postretention changes of the mandibular anterior teeth Am J Orthod Dentofacial Orthop 2013. 144 420–429. [DOI] [PubMed] [Google Scholar]
- 4.Zawawi KH, Melis M. The role of mandibular third molars on lower anterior teeth crowding and relapse after orthodontic treatment: a systematic review ScientificWorldJournal 2014. 2014 615429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Freitas KM, Janson G, de Freitas MR, Pinzan A, Henriques JF, Pinzan-Vercelino CR. Influence of the quality of the finished occlusion on postretention occlusal relapse Am J Orthod Dentofacial Orthop. 2007. 132:428 e429–414. [DOI] [PubMed] [Google Scholar]
- 6.Freitas KM, Freitas DS, Valarelli FP, Freitas MR, Janson G. PAR evaluation of treated Class I extraction patients Angle Orthod 2008. 78 270–274. [DOI] [PubMed] [Google Scholar]
- 7.Maia NG, Normando AD, Maia FA, Ferreira MA, Alves MS. Factors associated with orthodontic stability: a retrospective study of 209 patients World J Orthod 2010. 11 61–66. [PubMed] [Google Scholar]
- 8.Blagitz MN, Almeida GA, Normando D. Factors associated with the stability of compensatory orthodontic treatment of Class III malocclusion in the permanent dentition Am J Orthod Dentofacial Orthop 2020. 158 e63–e72. [DOI] [PubMed] [Google Scholar]
- 9.Richmond S, Shaw WC, O'Brien KD, et al. The development of the PAR Index (Peer Assessment Rating): reliability and validity Eur J Orthod 1992. 14 125–139. [DOI] [PubMed] [Google Scholar]
- 10.Paula DF,, Jr.,, Silva ET, Campos AC, Nunez MO, Leles CR. Effect of anterior teeth display during smiling on the self-perceived impacts of malocclusion in adolescents Angle Orthod 2011. 81 540–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Claudino D, Traebert J. Malocclusion, dental aesthetic self-perception and quality of life in a 18 to 21 year-old population: a cross section study BMC Oral Health 2013. 13 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies Int J Surg 2014. 12 1495–1499. [DOI] [PubMed] [Google Scholar]
- 13.Little RM. The irregularity index: a quantitative score of mandibular anterior alignment Am J Orthod Dentofacial Orthop 1975. 68 554–563. [DOI] [PubMed] [Google Scholar]
- 14.Bjering R, Sandvik L, Midtbo M, Vandevska-Radunovic V. Stability of anterior tooth alignment 10 years out of retention J Orofac Orthop 2017. 78 275–283. [DOI] [PubMed] [Google Scholar]
- 15.Massaro C, Miranda F, Janson G, et al. Maturational changes of the normal occlusion: A 40-year follow-up Am J Orthod Dentofacial Orthop 2018. 154 188–200. [DOI] [PubMed] [Google Scholar]
- 16.Thilander B. Dentoalveolar development in subjects with normal occlusion. A longitudinal study between the ages of 5 and 31 years Eur J Orthod 2009. 31 109–120. [DOI] [PubMed] [Google Scholar]
- 17.de Bernabe PG, Montiel-Company JM, Paredes-Gallardo V, Gandia-Franco JL, Bellot-Arcis C. Orthodontic treatment stability predictors: a retrospective longitudinal study Angle Orthod 2017. 87 223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meyer-Marcotty P, Klenke D, Knocks L, Santander P, Hrasky V, Quast A. The adult orthodontic patient over 40 years of age: association between periodontal bone loss, incisor irregularity, and increased orthodontic treatment need Clin Oral Investig 2021. 25 6357–6364. [DOI] [PMC free article] [PubMed] [Google Scholar]