Abstract
OBJECTIVE:
To investigate whether early developmental intervention (EDI) can positively affect the trajectories of cognitive development among children from low-resource families.
METHODS:
Longitudinal analyses were conducted of data from 293 children in the Brain Research to Ameliorate Impaired Neurodevelopment Home-based Intervention Trial, a randomized controlled trial of a home-based EDI program, to examine trajectories of Bayley Scales of Infant Development—Second Edition Mental Development Index (MDI) scores from 12 to 36 months of age among young children from high- and low-resource families in 3 low- to middle-resource countries.
RESULTS:
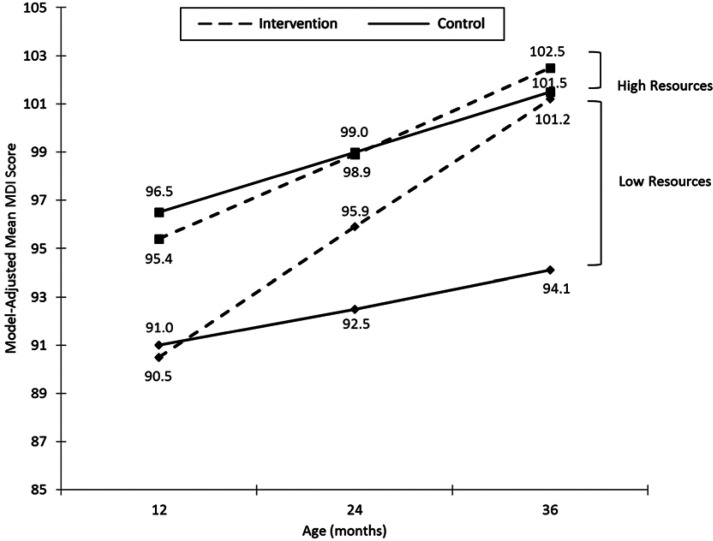
A 3-way interaction among family resources, intervention group, and age was statistically significant after controlling for maternal, child, and birth characteristics (Wald χ2(1) = 9.41, P = .002). Among children of families with high resources, both the intervention and control groups had significant increases in MDI scores over time (P < .001 and P = .002, respectively), and 36-month MDI scores for these 2 groups did not differ significantly (P = .602). However, in families with low resources, the EDI group displayed greater improvement, resulting in significantly higher 36-month MDI scores than the control group (P < .001). In addition, the 36-month MDI scores for children in families with low resources receiving EDI did not differ significantly from children from high-resource families in either the EDI (P = .509) or control (P = .882) groups.
CONCLUSIONS:
A home-based EDI during the first 3 years of life can substantially decrease the developmental gap between children from families with lower versus higher resources, even among children in low- to middle-resource countries.
What’s Known on This Subject:
Studies have found a link between socioeconomic status and cognitive development. Research suggests that early interventions can improve cognitive development. However, studies have not examined whether early intervention can ameliorate the impact of low socioeconomic status on cognitive development.
What This Study Adds:
This study demonstrates that early intervention can alter trajectories of cognitive development among children from disadvantaged backgrounds. Children from low-resource families receiving the study intervention had 36-month Mental Development Index scores statistically indistinguishable from those of children from high-resource families.
Fewer family resources and lower socioeconomic status (SES) have been consistently linked with poorer child developmental outcomes,1 particularly for cognitive development. Research in the United States and other higher-resource countries has shown that young children from lower SES families, for example, receive lower scores on measures of cognitive and language skills,2–4 perform more poorly on intelligence tests,5 exhibit diminished executive functioning,6–8 are less likely to be ready for school,9–11 and have poorer performance once they enter school.12
This same socioeconomic differential in development has been found in low- to middle-resource countries as well.13 For example, a study in Madagascar found significant variation in cognitive and language scores based on the mother’s education and the family’s wealth.14 Similar socioeconomic gaps were found in Extended Ages and Stages Questionnaire scores for children in 4 low- to middle-resource countries (India, Indonesia, Peru, and Senegal), and these gaps increase during the first 2 years of life.15
Children from lower SES backgrounds are also at greater risk for poorer birth outcomes that can adversely affect their developmental trajectories. Lower SES, as measured by either individual- or community-level indicators, has been linked with greater risk of low birth weight (eg, Parker et al16; Zeka et al17), which in turn has been linked to diminished cognitive ability.18 Children in low- to middle-resource countries are particularly at increased risk for poor birth outcomes. Of an estimated 2.9 million neonatal deaths occurring each year,19 the vast majority (∼99%) occur in low-resource countries.20
Early developmental intervention (EDI) can improve cognitive outcomes among socially or medically disadvantaged children (eg, Nahar et al21; Nordhov et al22; Wallander et al23). It is estimated that >200 million children under age 5 years do not reach their developmental potential because of poverty, malnutrition, poor health, and unstimulating home environments; the majority of these children reside in South Asia and sub-Saharan Africa.24,25 Walker and colleagues26 identified inadequate cognitive stimulation as 1 of 4 key risk factors for which there is an urgent need for intervention. In a literature review of EDI in developing countries, Baker-Henningham and Boo27 found that 9 of 10 intervention studies with disadvantaged children reported significant improvements in mental development scores. These interventions generally included home visits in which the mother was shown activities to foster child development and improve mother–child interactions. The 1 study not finding a significant effect consisted primarily of group meetings with mothers.27,28
The Brain Research to Ameliorate Impaired Neurodevelopment Home-based Intervention Trial (BRAIN-HIT) used a randomized controlled trial (RCT) design and found that a home-based EDI program that initiated training shortly after birth to parents on age-appropriate child stimulation activities was successful at improving child cognitive and psychomotor development at 3 years of age, as measured by Bayley Scales of Infant Development—Second Edition (BSID-II),29 among infants who survived birth asphyxia or had healthy births in 3 low- to middle-resource countries (India, Pakistan, and Zambia).30,31 The aim of the current study was to examine whether this early intervention could also ameliorate the developmental gap expected between children of low- versus high-resource families.
Methods
Study Design
The BRAIN-HIT (registered at ClinicalTrials.gov: NCT00639184) was an RCT involving an EDI program among young children in rural communities marked by poverty in India, Pakistan, and Zambia. As detailed elsewhere,23 this parallel design RCT was implemented in 2 populations: (1) infants with birth asphyxia unresponsive to stimulation who received bag and mask ventilation and (2) infants without asphyxia who did not require any resuscitation (discussed subsequently). Infants in each cohort were randomized individually, using 1:1 concealed parallel allocation, matched for country and chronological time using variable block sizes to ensure allocation concealment to either EDI plus health education or a control intervention consisting of health education only (see the flow diagram in Carlo et al30). The allocation sequence was generated centrally and distributed using sealed envelopes to the local investigators, who obtained consent for the trial. Written informed consent was obtained before randomization. The trial was approved by institutional review boards at the University of Alabama, Birmingham, RTI International, and each participating clinical site.30,31
Study Populations
Infants with birth asphyxia unresponsive to stimulation, who received bag and mask ventilation for resuscitation at birth, were screened for enrollment. Birth asphyxia was defined as the inability to initiate or sustain spontaneous breathing at birth using the World Health Organization32 definition. Exclusion criteria were (1) the infant’s birth weight was <1500 g, (2) the infant’s neurologic examination at 7 days was severely abnormal (grade III by criteria from Ellis et al33), (3) the mother was under 15 years of age, (4) the mother was unable/unwilling to participate, or (5) the mother was not planning to stay in the study communities for the following 3 years. In addition, infants who did not require any resuscitation and had normal neurologic exams at 7 days of age but otherwise met the same criteria as infants with birth asphyxia were randomly identified from the next 1 or 2 births after the infant with asphyxia, matched for country and chronological time, and enrolled into this trial
Participants
Among the 540 infants who were screened, 438 (81%) were eligible for participation in the study, and 407 (93%) of the eligible infants had families who consented to participate in the study.30 Among infants whose families consented, 293 (72%) had scores for the BSID-II Mental Developmental Index (MDI) at 12 and 36 months (discussed subsequently) and were included in the current analyses.
Intervention Conditions
Participants and parent trainers in both conditions were masked to the objectives and hypotheses of the study. Both interventions were delivered using a biweekly schedule of home visits, starting before age 1 month and ending at 36 months of age.
EDI
A home-based, parent-implemented EDI model was the active intervention (detailed in Wallander et al23). Following the Partners for Learning34 curriculum, parent trainers introduced playful interactive learning activities and modeled them for the parents during home visits. This curriculum covers (1) cognitive and fine motor, (2) social and self-help, (3) gross motor, and (4) language skills. During each home visit, the trainer presented 1 or 2 learning activities, and each activity targeted a developmentally appropriate skill. The parent practiced the activity in the presence of the trainer, who provided feedback. Cards depicting the activities were then left with the parent, who was encouraged to apply the activities in daily life with the child until the next home visit. The trainer introduced new activities in subsequent visits to enhance the child’s developmental competencies. The trainers were supervised during weekly group meetings and observations during home visits. Of all possible home visits during the study, home visit completion rates for the intervention group by site were as follows: India (92.2%), Pakistan (80.9%), and Zambia (82.8%). Further information on the intervention dose (eg, home visits, intervention adherence) for BRAIN is available in Wallander and colleagues.35
Control Intervention
Parents in both trial conditions received health education during every home visit, but this was the sole content of the control intervention. Implemented separately by EDI and control trainers, health education was based on a World Health Organization36 curriculum that addressed, for example, breastfeeding, nutrition, hygiene, and vaccinations.
Measures
Data were collected on demographic characteristics of the mother (age, education, marital status, education, parity, prenatal care) and child (gender), birth-related factors (vaginal vertex delivery, location, birth attendant, birth weight, gestational age, 1- and 5-minute Apgar scores), and whether the child had to be resuscitated in the delivery room.
Family Resources
A Family Resources Index was calculated on the basis of family assets and living standards, as shown in Table 1. Possible scores range from 0 to 20, and higher values indicate greater resources; for descriptive purposes, scores were classified into low versus high resources based on a median split (<8 vs ≥8). Cronbach’s α for the measure was high with a value of 0.79, indicating good internal consistency. Table 1 depicts the difference in assets and living standards between families with high and low family resources.
TABLE 1.
Scoring and Distribution of Family Resources
| Resources | Item Scoringa | % With Resource | |
|---|---|---|---|
| Low (n = 160) | High (n = 133) | ||
| Assets | |||
| Radio | 1 | 35 | 80 |
| Television | 1 | 6 | 74 |
| Refrigerator | 1 | 1 | 23 |
| Bicycle | 1 | 19 | 52 |
| Motorcycle or car | 1 | 4 | 19 |
| Sewing machine | 1 | 4 | 27 |
| Watch/clock | 1 | 23 | 80 |
| Sofa | 1 | 2 | 30 |
| Fan | 1 | 6 | 51 |
| Videocassette player/recorder | 1 | 1 | 23 |
| Living standards | |||
| Source of water | |||
| Private pipe/pump | 2 | 18 | 50 |
| Public pipe/pump | 1 | 56 | 38 |
| Other | 0 | 26 | 11 |
| Source of toilet | |||
| Any flush/latrine | 2 | 25 | 75 |
| Bus/field | 0 | 75 | 25 |
| Source of light | |||
| Electricity | 2 | 46 | 74 |
| Kerosene/gas/oil | 1 | 49 | 22 |
| Other | 0 | 5 | 4 |
| House materials | |||
| High-quality materials only | 2 | 2 | 47 |
| High- and low-quality materials | 1 | 21 | 32 |
| Low-quality materials only | 0 | 78 | 20 |
| Number of sleepers per room | |||
| 1–2 sleepers per room | 2 | 25 | 67 |
| 3–4 sleepers per room | 1 | 41 | 22 |
| 5+ sleepers per room | 0 | 34 | 11 |
The overall Family Resources Index score is computed by summing the scores across all items. Families not owning an asset are assigned a value of 0 for that item. Overall scores are classified into low (<8) versus high (8+).
Cognitive Development
The primary outcome for the EDI was cognitive development, measured by the BSID-II MDI. The MDI is a standardized score with a mean of 100 and SD of 15. The BSID-II was used in this study because of its well-established reliability and validity and its previous extensive use in low- to middle-resource countries.37 As outlined in Biasini and colleagues,38 the BSID-II was pretested in each of the sites participating in BRAIN (India, Pakistan, and Zambia), and minor modifications were made to a few items to make them more culturally appropriate. For example, a picture of a sandal rather than shoe was used. Assessments were completed at 12, 24, and 36 months of corrected age in the local language. Evaluators from the 3 sites jointly received training on the BSID-II in 4-day workshops during which they practiced administering the instrument until adequate reliability was achieved. Each workshop was held before commencing the yearly assessments. Evaluators were fluent in the local language, familiar with the culture, and masked to the participant’s resuscitation history or treatment assignment. If an evaluation could not be completed because of acute illness or uncharacteristic behavioral problems, the assessment was rescheduled when possible.
Statistical Analyses
Analyses were conducted using an intent-to-treat approach. Descriptive statistics were computed for maternal and infant characteristics. Frequencies and percentages were reported for categorical variables and means and standard deviations for continuous variables.
Generalized estimating equation models were conducted to compare trajectories of MDI scores from the 12-, 24-, and 36-month assessments by high versus low family resources and intervention group, while accounting for repeated measurements and clustering of children by site. We began by fitting a model testing a 2-way interaction between age and intervention group to determine whether children in the EDI group had different trajectories of MDI scores over time than those in the control group. We then tested a 3-way interaction (age × intervention × family resources) to determine whether the impact of the intervention on the trajectories of MDI scores varied depending on family resources. Both models included site; intervention group; family resources; resuscitation status; and the maternal, child, and birth characteristic listed in Table 2. The analyses included children with 36-month MDI scores. However, as a sensitivity check, the regression models were rerun adding in children with missing 36-month scores to determine whether results are consistent. All analyses were conducted in SAS version 9.4.
TABLE 2.
Maternal, Child, and Birth Characteristics and Outcomes by Family Resources
| Variable | Total (n = 293) | Family Resources | ||
|---|---|---|---|---|
| Low (n = 160) | High (n = 133) | P | ||
| Intervention group, n (%) | ||||
| Early developmental intervention | 146 (50) | 79 (49) | 67 (50) | .865 |
| Control | 147 (50) | 81 (51) | 66 (50) | |
| Site, n (%) | ||||
| India | 81 (28) | 36 (23) | 56 (41) | .002 |
| Pakistan | 120 (41) | 49 (31) | 32 (24) | |
| Zambia | 92 (31) | 75 (47) | 45 (34) | |
| Maternal characteristics | ||||
| Age (y), mean ± SD | 25.4 ± 5.6 | 25.5 ± 5.5 | 25.4 ± 5.7 | .894 |
| Age (y), n (%) | ||||
| <20 | 36 (12) | 19 (12) | 17 (13) | .751 |
| 20–24 | 102 (35) | 53 (33) | 49 (37) | |
| 25–34 | 129 (44) | 75 (47) | 54 (41) | |
| ≥35 | 26 (9) | 13 (8) | 13 (10) | |
| Highest level of maternal education, n (%) | ||||
| No formal education | 143 (51) | 99 (63) | 44 (36) | <.001 |
| Literate/primary education | 80 (29) | 42 (27) | 38 (31) | |
| Secondary/university | 55 (20) | 15 (10) | 40 (33) | |
| Married, n (%) | 278 (95) | 159 (99) | 119 (89) | <.001 |
| Primiparous, n (%) | 94 (32) | 48 (30) | 46 (35) | .418 |
| Prenatal care, n (%) | 231 (79) | 113 (71) | 118 (89) | <.001 |
| Child characteristics | ||||
| Gender (male), n (%) | 166 (58) | 92 (58) | 74 (58) | .944 |
| Birth wt (g), n (%) | ||||
| 1500–2499 | 68 (24) | 41 (26) | 27 (22) | .649 |
| 2500–2999 | 109 (39) | 58 (37) | 51 (41) | |
| >3000 | 105 (37) | 58 (37) | 47 (38) | |
| Apgar scores, mean ± SD | ||||
| 1 min | 7.2 ± 2.6 | 7.3 ± 2.5 | 7.1 ± 2.6 | .671 |
| 5 min | 9.2 ± 1.4 | 9.3 ± 1.3 | 9.0 ± 1.5 | .106 |
| Preterm, n (%) | 91 (32) | 57 (36) | 34 (26) | .060 |
| Resuscitated, n (%) | 123 (42) | 73 (46) | 50 (38) | .166 |
| Birth characteristics | ||||
| Vaginal vertex delivery, n (%) | 277 (99) | 155 (99) | 122 (98) | .433 |
| Location of birth, n (%) | ||||
| Home | 155 (55) | 99 (63) | 56 (44) | .005 |
| Clinic | 66 (23) | 28 (18) | 38 (30) | |
| Hospital | 63 (22) | 30 (19) | 33 (26) | |
| Birth attendant, n (%) | ||||
| Physician | 23 (8) | 12 (8) | 11 (9) | .004 |
| Nurse/midwife/health worker | 120 (42) | 52 (33) | 68 (54) | |
| Traditional birth attendant | 132 (46) | 87 (55) | 45 (35) | |
| Family/unattended | 9 (3) | 6 (4) | 3 (2) | |
Results
Average maternal age among study participants was 25.4 years with a little over half having no formal education (Table 2). The majority of mothers were married, had received prenatal care, and had a vaginal vertex delivery. Mean (95% confidence interval) overall family resource index scores were 4.94 (4.70–5.18) for low-resource families and 11.98 (11.48–12.53) for high-resource families (P < .001). Families with low resources were more likely to be from Zambia, have no formal education, be married, have not received prenatal care, have delivered at home, and have had a traditional birth attendant (Table 2).
Confirming results of a previous BRAIN-HIT evaluation,31 when controlling for site; intervention; and the other maternal, child, and birth characteristics, children in the EDI and control groups displayed significantly different trajectories of MDI scores from 12 to 36 months (Wald χ2[1] = 9.56, P = .002; Table 3, Model 1). Pursuant to the aim of the current study, in the model including family resources as a moderator of this intervention-by-age interaction effect, the 3-way interaction among age, intervention, and family resources was statistically significant (Wald χ2[1] = 9.41, P = .002; Table 3, Model 2). This finding is consistent if participants missing 36-month scores are also included (Wald χ2[1] = 10.25, P = .001).
TABLE 3.
Regression Models of Trajectories of MDI Scores (12–36 Months)
| Variable | Model 1: Intervention Effect Only | Model 2: Family Resources as Moderator of Intervention Effect | ||
|---|---|---|---|---|
| B (SE) | P | B (SE) | P | |
| Early developmental intervention | −3.67 (2.51) | .144 | −11.21 (5.41) | .038 |
| Age (mo) at assessment (adjusted) | 0.16 (0.05) | .002 | −0.08 (0.10) | .398 |
| Family resources | 0.41 (0.21) | .049 | −0.23 (0.39) | .553 |
| Age × intervention | 0.22 (0.07) | .002 | 0.60 (0.15) | <.001 |
| Age × family resources | N/A | N/A | 0.03 (0.01) | .006 |
| Intervention × family resources | N/A | N/A | 0.94 (0.58) | .102 |
| Age × intervention × family resources | N/A | N/A | −0.05 (0.02) | .002 |
N = 292. All models adjusted for site, resuscitation status, and all maternal, child, and birth characteristics noted in Table 2, none of which contributed significantly in the models.
As shown in Fig 1, trajectories of MDI scores varied by family resources. In families with high resources, as defined here (see Table 1), both the intervention and control groups had significant increases in MDI scores over time (P < .001 and P = .002, respectively), and 36-month MDI scores for these 2 groups did not differ significantly (adjusted means: 102.5 vs 101.5; P = .602). However, in families with low resources, the EDI group displayed greater improvement, resulting in significantly higher 36-month MDI scores than the control group (adjusted means: 101.2 vs 94.1; P < .001). In addition, the 36-month MDI scores for children in families with low resources receiving EDI did not differ significantly from children from high-resource families in either the EDI (adjusted means: 101.2 vs 102.5; P = .509) or control (adjusted means 101.2 vs 101.5; P = .882) groups.
FIGURE 1.
Model-adjusted mean BSID-II MDI scores by family resources and intervention. Means are adjusted for intervention, adjusted age, family resources, site, gender, maternal age, education, marital status, prenatal care, primiparous, vaginal vertex delivery, gestational age, birth weight, birth attendant, location of birth, 1- and 5-minute Apgar scores, resuscitation, and age × intervention, age × family resources, intervention × family resources, age × intervention × family resources interactions.
Resuscitation status was included along with the other control variables in both models to account for the possible impact of birth asphyxia on MDI scores. Resuscitation status did not have a significant impact on MDI scores in either model: Model 1 (P = .178) and Model 2 (P = .233). In the addition, the 3-way interaction among age, intervention, and family resources remains significant when the resuscitated group is removed (Wald χ2[1] = 12.06, P < .001).
Discussion
Results indicate that a home-based EDI during the first 3 years of life can substantially decrease the developmental gap between children from families with lower versus higher resources, even among children in low- to middle-resource countries and who experience asphyxia at birth. Whereas children of low-resource families who did not receive the EDI experienced a widening gap in cognitive development over time than those in high-resource families, children of low-resource families who received 36 months of EDI reached similar levels of cognitive development as those in high-resource families. Although already behind in development at 12 months, children in low-resource families appeared to catch up in cognitive development to become indistinguishable from those in high-resource families after 2 additional years of receiving EDI. This is a noteworthy achievement given the challenges a low-resource family environment poses for children’s development, especially in developing countries,25 which EDI appears to overcome.
Consistent with expectations, children from low-resource families not receiving EDI maintained a relatively flat developmental trajectory from 12 to 36 months, obtaining an MDI ∼0.5 SD below that of children in high-resource families who also did not receive EDI. In contrast, for children in high-resource families, EDI did not make a difference on cognitive development. Children from high-resource families in the control condition still reached a cognitive development at 36 months of age that was not different from children from the same background receiving EDI. It is possible that parents in these families are already engaging their children in stimulating interactions and providing a rich environment, so additional training and prompts do not have an additional impact on their children’s development. For example, more highly educated mothers in the United States talk more, ask more questions, and use fewer directives than less educated mothers,3,39 and at least 1 study indicates that a similar pattern exists in low-resource countries.40
We are not aware of studies that examined the differential impact of EDI for children in low- versus high-resource families. Numerous studies in low-resource countries have reported beneficial effects from EDI on the cognitive development of children in low socioeconomic families as well as those with biological risks (see reviews by Aboud and Yousafzai24; Walker et al26), but none have examined the moderating effect of family resources on developmental outcomes when children are exposed to EDI. If replicated, the present findings suggest that EDI should target primarily children from low-resource families, which may result in a decrease in the developmental gap otherwise expected between children in low- versus high-resource families.
Limitations include that the independent variable of interest, family resources, was not experimentally manipulated. Thus, the primary findings here are from an observational study. In addition, children were evaluated across the first 3 years when neurodevelopmental assessments may be less predictive of long-term outcomes than at later ages. It is conceivable that larger benefits will be observed at school age. Finally, the findings may not generalize to high-resource countries, such as the United States, where family resources can differ greatly from those in the low-middle income countries included in the current study.
Conclusions
EDI may be beneficial in reducing the intergenerational transmission of poverty in low- and middle-resource countries. Early cognitive development predicts later school outcomes. Nationally representative studies from many countries show associations between family resources and children’s school enrollment and dropout, grades attained, and educational achievement.25 Children who achieve poorly in school are more likely to have low incomes in adulthood and difficulty providing for their own children,41 resulting in reduced developmental outcomes in the next generation. Much evidence accumulated to date suggests that EDI should be one of the approaches used to improve early development in low- and middle-income countries.
Glossary
- BRAIN-HIT
Brain Research to Ameliorate Impaired Neurodevelopment Home-based Intervention Trial
- BSID-II
Bayley Scales of Infant Development, Second Edition
- EDI
early developmental intervention
- MDI
Mental Developmental Index
- RCT
randomized controlled trial
- SES
socioeconomic status
Footnotes
Dr Bann conceptualized and conducted statistical analyses and wrote the initial draft of the manuscript; Dr Wallander participated in the design of the study, research aims and hypothesis, and data collection instruments and wrote the initial draft of the manuscript; Ms Do and Ms Thorsten conducted statistical analyses and critically reviewed the manuscript; Drs Pasha and Goudar participated in the design of the study and data collection instruments, monitored data collection at 1 site, and reviewed the manuscript; Dr Biasini participated in the design of the study, research aims and hypothesis, and data collection instruments and reviewed the manuscript; Dr Bellad contributed to the aims and hypotheses for the manuscript, participated in the design of the study, and reviewed the manuscript; Dr Chomba conceptualized and designed the study and critically reviewed the manuscript; Dr McClure participated in the design of the study and data collection instruments, managed data collection, and reviewed the manuscript; Dr Carlo, as principal investigator, conceptualized and designed the overall study and provided critical review and revisions of the manuscript; and all authors approved the final manuscript as submitted.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH); NIH staff contributed to the design of the original study and collection of the data, but not to the analysis, preparation, review, or approval of the manuscript or the decision to submit the manuscript.
This trial has been registered at www.clinicaltrials.gov (identifier NCT NCT00639184).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development Global Network for Women’s and Children’s Health Research and the National Institute of Neurologic Disorders and Stroke (grants HD43464, HD42372, HD40607, and HD40636), the Fogarty International Center (TW006703), the Perinatal Health and Human Development Research Program, and the Children’s of Alabama Centennial Scholar Fund of the University of Alabama at Birmingham.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2016-0137.
References
- 1.Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371–399 [DOI] [PubMed] [Google Scholar]
- 2.Christensen DL, Schieve LA, Devine O, Drews-Botsch C. Socioeconomic status, child enrichment factors, and cognitive performance among preschool-age children: results from the Follow-Up of Growth and Development Experiences study. Res Dev Disabil. 2014;35(7):1789–1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoff E. The specificity of environmental influence: socioeconomic status affects early vocabulary development via maternal speech. Child Dev. 2003;74(5):1368–1378 [DOI] [PubMed] [Google Scholar]
- 4.Raviv T, Kessenich M, Morrison FJ. A mediational model of the association between socioeconomic status and three-year-old language abilities: the role of parenting factors. Early Child Res Q. 2004;19(4):528–547 [Google Scholar]
- 5.Turkheimer E, Haley A, Waldron M, D’Onofrio B, Gottesman II. Socioeconomic status modifies heritability of IQ in young children. Psychol Sci. 2003;14(6):623–628 [DOI] [PubMed] [Google Scholar]
- 6.Sarsour K, Sheridan M, Jutte D, Nuru-Jeter A, Hinshaw S, Boyce WT. Family socioeconomic status and child executive functions: the roles of language, home environment, and single parenthood. J Int Neuropsychol Soc. 2011;17(1):120–132 [DOI] [PubMed] [Google Scholar]
- 7.Farah MJ, Shera DM, Savage JH, et al. Childhood poverty: specific associations with neurocognitive development. Brain Res. 2006;1110(1):166–174 [DOI] [PubMed] [Google Scholar]
- 8.Mezzacappa E. Alerting, orienting, and executive attention: developmental properties and sociodemographic correlates in an epidemiological sample of young, urban children. Child Dev. 2004;75(5):1373–1386 [DOI] [PubMed] [Google Scholar]
- 9.Currie J. Health disparities and gaps in school readiness. Future Child. 2005;15(1):117–138 [DOI] [PubMed] [Google Scholar]
- 10.Garcia E. Inequalities at the Starting Gate: Cognitive and Noncognitive Skills Gaps Between 2010–2011 Kindergarten Classmates. Washington, DC: Economic Policy Institute; 2015 [Google Scholar]
- 11.Larson K, Russ SA, Nelson BB, Olson LM, Halfon N. Cognitive ability at kindergarten entry and socioeconomic status. Pediatrics. 2015;135(2). Available at: www.pediatrics.org/cgi/content/full/135/2/e440 [DOI] [PubMed] [Google Scholar]
- 12.Malecki CK, Demaray MK. Social support as a buffer in the relationship between socioeconomic status and academic performance. Sch Psychol Q. 2006;21(4):375–395 [Google Scholar]
- 13.World Bank . Early childhood development (chapter 5). World Development Report 2015: Mind, Society, and Behavior. 2015. Available at: http://www.worldbank.org/content/dam/Worldbank/Publications/WDR/WDR%202015/WDR-2015-Full-Report.pdf. Accessed September 29, 2015
- 14.Fernald LC, Weber A, Galasso E, Ratsifandrihamanana L. Socioeconomic gradients and child development in a very low income population: evidence from Madagascar. Dev Sci. 2011;14(4):832–847 [DOI] [PubMed] [Google Scholar]
- 15.Fernald LC, Kariger P, Hidrobo M, Gertler PJ. Socioeconomic gradients in child development in very young children: evidence from India, Indonesia, Peru, and Senegal. Proc Natl Acad Sci USA. 2012;109(suppl 2):17273–17280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parker JD, Schoendorf KC, Kiely JL. Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States. Ann Epidemiol. 1994;4(4):271–278 [DOI] [PubMed] [Google Scholar]
- 17.Zeka A, Melly SJ, Schwartz J. The effects of socioeconomic status and indices of physical environment on reduced birth weight and preterm births in Eastern Massachusetts. Environ Health. 2008;7:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richards M, Hardy R, Kuh D, Wadsworth ME. Birth weight and cognitive function in the British 1946 birth cohort: longitudinal population based study. BMJ. 2001;322(7280):199–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lawn JE, Blencowe H, Oza S, et al. ; Lancet Every Newborn Study Group . Every Newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189–205 [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization . Trends in maternal mortality: 1990 to 2013. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. Geneva, Switzerland: World Health Organization; 2014 [Google Scholar]
- 21.Nahar B, Hamadani JD, Ahmed T, et al. Effects of psychosocial stimulation on growth and development of severely malnourished children in a nutrition unit in Bangladesh. Eur J Clin Nutr. 2009;63(6):725–731 [DOI] [PubMed] [Google Scholar]
- 22.Nordhov SM, Rønning JA, Dahl LB, Ulvund SE, Tunby J, Kaaresen PI. Early intervention improves cognitive outcomes for preterm infants: randomized controlled trial. Pediatrics. 2010;126(5). Available at: www.pediatrics.org/cgi/content/full/126/5/e1088 [DOI] [PubMed] [Google Scholar]
- 23.Wallander JL, McClure E, Biasini F, et al. ; BRAIN-HIT Investigators . Brain research to ameliorate impaired neurodevelopment--home-based intervention trial (BRAIN-HIT). BMC Pediatr. 2010;10:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aboud FE, Yousafzai AK. Global health and development in early childhood. Annu Rev Psychol. 2015;66:433–457 [DOI] [PubMed] [Google Scholar]
- 25.Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B; International Child Development Steering Group . Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369(9555):60–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walker SP, Wachs TD, Gardner JM, et al. ; International Child Development Steering Group . Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007;369(9556):145–157 [DOI] [PubMed] [Google Scholar]
- 27.Baker-Henningham H, Boo FL. Early childhood stimulation interventions in developing countries: a comprehensive literature review (Discussion Paper IZA DP No. 5282). Available at: http://ftp.iza.org/dp5282.pdf. 2010. Accessed May 15, 2015
- 28.Aboud FE. Evaluation of an early childhood parenting programme in rural Bangladesh. J Health Popul Nutr. 2007;25(1):3–13 [PMC free article] [PubMed] [Google Scholar]
- 29.Bayley N. Bayley Scales of Infant Development. 2nd ed. San Antonio, TX: The Psychological Corporation; 1993 [Google Scholar]
- 30.Carlo WA, Goudar SS, Pasha O, Chomba E, Wallander JL, Biasini FJ, et al. Randomized trial of early developmental intervention on outcomes in children after birth asphyxia in developing countries. J Pediatr. 2013;162(4):705–712.e703 [DOI] [PMC free article] [PubMed]
- 31.Wallander JL, Bann CM, Biasini FJ, et al. Development of children at risk for adverse outcomes participating in early intervention in developing countries: a randomized controlled trial. J Child Psychol Psychiatry. 2014;55(11):1251–1259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization . Basic Newborn Resuscitation: A Practical Guide. Geneva, Switzerland: World Health Organization; 1997 [Google Scholar]
- 33.Ellis M, Manandhar DS, Manandhar N, Wyatt J, Bolam AJ, Costello AM. Stillbirths and neonatal encephalopathy in Kathmandu, Nepal: an estimate of the contribution of birth asphyxia to perinatal mortality in a low-income urban population. Paediatr Perinat Epidemiol. 2000;14(1):39–52 [DOI] [PubMed] [Google Scholar]
- 34.Sparling JJ, Lewis IS. Partners for Learning: Birth to 24 Months. Lewisville, NC: Kaplan Press; 1984 [Google Scholar]
- 35.Wallander JL, Biasini FJ, Thorsten V, et al. Dose of early intervention treatment during children’s first 36 months of life is associated with developmental outcomes: an observational cohort study in three low/low-middle income countries. BMC Pediatr. 2014;14:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization . Integrated Management of Childhood Illnesses (IMCI): An Illustrated Guide to Improve Family and Community Practices. Geneva, Switzerland: World Health Organization; 2009 [Google Scholar]
- 37.Fernald LCH, Kariger P, Engle P, Raikes A. Examining Early Child Development in Low Income Countries: A Toolkit for the Assessment of Children in the First Five Years of Life. Washington, DC: The World Bank; 2009
- 38.Biasini FJ, De Jong D, Ryan S, et al. Development of a 12 month screener based on items from the Bayley II Scales of Infant Development for use in Low Middle Income countries. Early Hum Dev. 2015;91(4):253–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hart B, Risley T. Meaningful Differences in the Everyday Experience of Young American Children. Baltimore, MD: Paul H. Brookes Publishing; 1995 [Google Scholar]
- 40.Paxson C, Schady N. Cognitive development among young children in Ecuador the roles of wealth, health, and parenting. J Hum Resour. 2007;42(1):49–84 [Google Scholar]
- 41.Walker SP, Chang SM, Powell CA, Grantham-McGregor SM. Effects of early childhood psychosocial stimulation and nutritional supplementation on cognition and education in growth-stunted Jamaican children: prospective cohort study. Lancet. 2005;366(9499):1804–1807 [DOI] [PubMed] [Google Scholar]