Abstract
A sizable portion of the United States’ population lives in a rural setting. Coupled with a limited number of infectious diseases providers, this has created a need for innovative practice models to deliver outpatient antimicrobial therapy and clinical monitoring in rural settings. This article reviews existing literature regarding outpatient parenteral antimicrobial therapy in rural settings and explores existing barriers and potential solutions that may be of assistance to providers looking to provide these services.
Keywords: infectious diseases, OPAT, rural health
Introduction
Outpatient parenteral antimicrobial therapy (OPAT) involves the administration of intravenous (IV) antimicrobials to patients outside of the hospital setting. 1 OPAT patients can receive IV antibiotics in several settings, including at home with home infusion, skilled nursing facilities (SNFs), rehab facilities, infusion centers, and acute long-term care facilities. OPAT programs are instrumental in ensuring patients discharged on IV antimicrobials complete therapy safely and effectively. Several advantages of OPAT programs have been described in the literature, including increased patient satisfaction, reduced hospital length of stay, reduced risk of nosocomial infections, and increased institutional cost savings. 2 Establishing OPAT programs that serve populations in rural areas, however, poses several challenges. Patients living in rural areas often have limited resources and are often far away from the tertiary center where their infections were first diagnosed. Literature related to the practice of OPAT in rural populations has been limited. This article aims to add to the literature by exploring two OPAT programs serving largely rural populations of the United States (U.S.). The purpose of this article is to describe challenges and mitigation strategies of facilitating OPAT services in rural areas.
The need for providing quality care to patients in rural areas
Approximately 14–19% of the U.S. population resides in rural areas. 3 Rural Americans are at a greater risk of poor health outcomes compared to individuals living in urban areas for several reasons. Rural communities have a larger proportion of older patients, with one-half of all hospital admissions in rural areas being composed of patients aged 65 years or older. 4 The presence of chronic comorbidities such as heart disease, diabetes, and obesity are also higher in rural populations. Higher poverty rates, lower income, and limited access to health insurance can cause significant challenges in obtaining care. Lower health literacy and level of education in rural areas can also negatively impact a patient’s ability to understand disease processes and take medication appropriately. Furthermore, lack of transportation, fewer physicians, and limited available healthcare resources are barriers for patient access to services.3,4 Despite these barriers, there has been an increasing push to discharge patients requiring long-term antibiotic therapy home as a means to decrease healthcare exposure.5,6
Description of practice sites
West Virginia University Hospitals
The influence of rurality is important when studying the health of the U.S. A total of 60-million people live in non-metropolitan areas with 47.6% of those in the Southern region. Of the southern states, West Virginia has the highest percent of its population living in rural areas at 50.9%, ranking third nationally behind Vermont and Maine. 7 West Virginia is also the only state entirely a part of Appalachia. 8 West Virginia demonstrates the effects of Appalachian rurality by having some of the highest rates of obesity, diabetes, cardiovascular disease, and chronic obstructive pulmonary disease.9,10 West Virginia also has one of the oldest populations with over a third of its residents living with multiple chronic conditions. 11 All of these are factors that increase a person’s risk of developing significant infections. Multidisciplinary care from both surgical and medical specialists is often required in the diagnosis and treatment of complex infections. In rural areas, few facilities with this capacity exist and are often separated by large distances. This includes West Virginia University Medicine Ruby Memorial Hospital in Morgantown, WV, which is over 150 miles away from the other tertiary care centers in the state. Because of this, large percentages of our inpatient population have been transferred for specialized care.
On review of 100 patients discharged from West Virginia University Hospitals with OPAT, 93% were from outside of Morgantown, WV. Only 7% were from Morgantown, WV. The average distance traveled by these was 89.3 miles with the longest distance being over 240 miles. This presents unique challenges when arranging OPAT as the majority of patients discharged return to homes and facilities in rural areas far away from where their care was initiated.
University of New Mexico Hospitals
The state of New Mexico has a unique confluence of factors that add barriers to patients accessing care. While only 33.2% of the population lives in non-metropolitan counties, 30 of the 33 counties are medically underserved. Compounding these access issues are the state’s relative size (fifth largest) and income (third poorest), meaning patients have to travel farther with less resources to access care (Creamer, 2022).12,13 For example, the University of New Mexico Hospital is the state’s only level-I trauma center, and only academic medical center, while also functioning as the county hospital. While treating patients in their home community is important, some small-town communities struggle with getting access to running water, electricity, and internet. Studies have shown that patients prefer receiving OPAT at home. 6 This is likely influenced by the additional support provided by the patient’s family and community. In New Mexico, this can create unique challenges for patients where access to running water, electricity, and internet can be limited (e.g. portions of native American reservations).
Patient perspective
While it is possible to review the medical literature and epidemiology regarding infectious diseases (ID) and rural healthcare to quantify the needs and barriers of providing OPAT services in rural settings, it potentially over-simplifies the existing challenges. Contextualizing the problem through the patient’s perspective can provide meaningful emphasis to the ramification of the decisions providers make when coordinating care for these patients. Below is one such example.
The patient was a 42-year-old-male living in Grants, New Mexico. There are currently no ID physicians practicing in his rural county. As such, when he was admitted to a local hospital with concern for new lumbar spine osteomyelitis, he had to be transferred to the closest hospital with ID providers 80 miles away. The patient was diagnosed with candida osteomyelitis and started on micafungin. Multiple trials of oral azole antifungal therapy were attempted but ultimately were unsuccessful, leading to readmission in one case. Requiring 6 months of therapy, the patient first was discharged to a SNF in Albuquerque to facilitate easier outpatient ID follow-up. As he improved, the patient was transferred to a SNF in Grants for several weeks and was eventually discharged home to receive daily micafungin infusions at an infusion center.
While the patient’s care was clinically complicated, the impact on his home life was profound. His wife would drive multiple times per week to see him as was feasible while working and taking care of their school-aged child. Unfortunately, given the patient’s prolonged stay in Albuquerque, his wife quickly utilized all of her occupational leave and eventually lost her job. This resulted in added financial burden on an already stressful situation. Appointments needed to be scheduled around their child’s school schedule and transportation to any follow-up appointment in Albuquerque became difficult.
While some of this hardship is tragically unavoidable, the patient’s case illustrates the additional challenges patients in rural settings have to bear to receive care in the current healthcare landscape. To facilitate efficient transportation and clinical follow-up, having the patient remain geographically close to available services, and may be encouraged, or even required, by either the discharging institution or accepting facility. It is important to realize the detrimental emotional and financial consequences the patient may experience from being separated from their family and community for extended periods of time to receive OPAT services.
Challenges of providing OPAT services in rural areas
While OPAT can be provided in a variety of settings (home-based, infusion center-based, or SNF-based model) the majority of OPAT occurs via self-administration at home. 1 Several challenges exist when trying to provide OPAT services to patients living in rural areas. There is a significant shortage of ID-trained healthcare professionals with roughly 80% of U.S. counties (or 208 million people) living without an ID physician. 14 This limits the number of providers available to provide OPAT oversight and clinical management of patients. Additionally, patients may lack transportation and reside in remote locations far away from healthcare facilities. This poses a challenge for close monitoring as patients may need to travel long distances to a hospital or clinic for follow-up appointments or to receive first doses of IV antimicrobials in a monitored environment. Traveling to healthcare settings for routine lab draws and IV infusions may also be necessary if patients do not qualify for home health care or home infusion services. The number of home infusion and home health care agencies available for a patient may also be limited due to geographic location. In a study conducted to describe practices and limitations of the use of OPAT in French rural areas, patient’s geographic isolation was identified as one of the main factors limiting the use of OPAT prescriptions by practitioners. 15 In the U.S., studies have shown that the majority of Medicare beneficiaries live in counties with at least one home health agency but did identify those without these services were in mostly rural settings. 16 Rural areas are more vulnerable to national shortages of healthcare workers and facilities. The COVID-19 pandemic has led to the closures of healthcare facilities utilized previously by OPAT patients.17,18 These issues both demonstrate the importance of OPAT programs serving rural populations in staying up-to-date on the available resources unique to each patient’s geographic location.
Patients with low income may also be uninsured or underinsured, leading to affordability barriers for outpatient IV antibiotics and the associated cost of devices and supplies. Factors such as a lack of running water, refrigeration, or working telephone may render a patient ineligible for home infusion services. Furthermore, individuals with limited health literacy may have lower confidence associated with self-administration of IV antibiotics and communication with healthcare professionals.
The opioid crisis poses an additional challenge for providing OPAT services in rural areas. West Virginia has the highest opioid overdose death rate in the U.S. with 81.4 overdose deaths per 100,000 persons. 19 Both states, however, have experienced significant increases in the number of fatal drug overdoses since the start of the COVID-19 pandemic in March 2020. 19 Persons who inject drugs have often been excluded from OPAT services due to concern of peripherally inserted central catheter (PICC) line misuse, although data has shown OPAT may be feasible with appropriate addiction therapy and follow-up. 20
Strategies to provide OPAT services successfully in rural areas
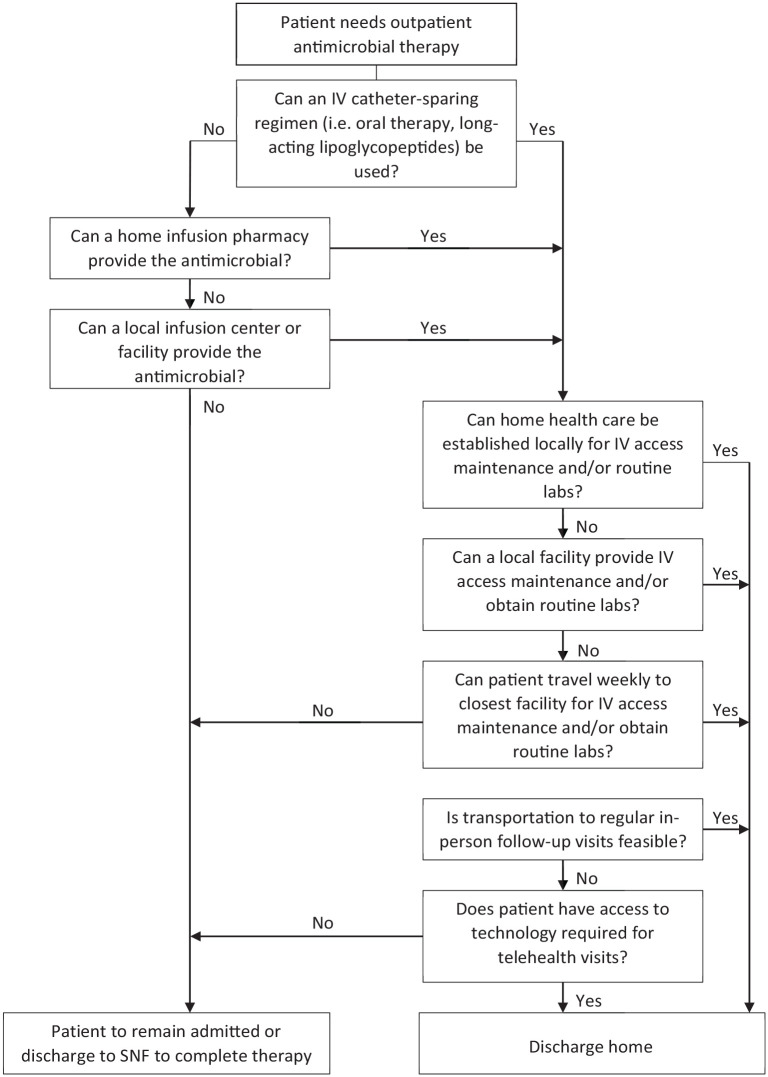
When evaluating the capability of patients to receive antimicrobials in a rural setting, providers should first review all components typically assessed in establishing a patient for outpatient IV antimicrobial therapy. All patients receiving OPAT should have access to reliable and regular IV access care, laboratory monitoring, and physician follow-up. Additionally, patients receiving OPAT at home must have the ability to receive antimicrobial therapy from a home infusion company and have running water, adequate heat, and refrigeration that is required to safely store IV medications. 21 For patients living in rural areas who must present in-person for services, attempting to align the patient’s appointments with other medical appointments they may have in the same area will reduce transportation needs of the patient. Collaborating with other local health care facilities close to the patient’s home for certain in-person services also allows convenience for the patient. Additionally, non-emergency medical transportation may be a covered medical benefit for these patients. Working with care management and social work can help providers identify what services and benefits are available to the patient to ensure access to appropriate follow-up. If patients do not have access to reliable transportation for in-person follow-up visits, telemedicine could be used by providers to provide the necessary clinical follow-up. If all components can reliably be provided, patients living in rural areas can safely receive OPAT (Figure 1).
Figure 1.
Assessing appropriateness of OPAT for patients living in rural areas.
OPAT, Outpatient parenteral antimicrobial therapy.
Patient and caregiver education
Patient and caregiver education is important to provide quality OPAT services and has previously been described as a vital component of OPAT bundles created to improve patient outcomes.22,23 Patient and caregiver education is especially important in rural settings where there is a prevalence of lower health literacy. A study assessing patient perspectives on the quality of OPAT found that patients perceived antibiotic side effects, instructions for use, IV access device information and complications and information about treatment progress were important topics to be discussed. Patients felt that both written and oral information should be provided to them. 24 Educating parents and caregivers at the bedside about OPAT services allows them to be familiar with the OPAT team, the treatment and monitoring plan, and who to contact with questions, concerns, or information about adverse effects prior to being discharged. OPAT education packets can be a useful tool to provide to patients and caregivers. Education materials should be written in a patient-friendly, easy to understand manner. Information to consider including in education packets are discussed in Table 1. Additionally, patients being discharged with home infusion require teachings on infusion devices, administration techniques, antibiotic storage and line maintenance. Open communication and questions about OPAT should be encouraged by healthcare professionals. Patients and caregivers should be assessed to ensure that they understand the information given to them. The teach back method can be employed to check patient and caregiver understanding.
Table 1.
OPAT patient education information.
| Description of “what is OPAT?” |
| What to expect during treatment |
| IV antibiotic regimen description with common side effects |
| Type of labs monitored and frequency |
| Length of treatment |
| OPAT treatment setting (home health/home infusion, skilled nursing facility, or infusion center) |
| Follow-up appointment information |
| OPAT team contact information |
IV, intravenous; OPAT, outpatient parenteral antimicrobial therapy.
Complex outpatient oral antimicrobial therapy
An ever-growing body of evidence continues to demonstrate that oral antibiotics regimens are non-inferior to IV regimens for the management of many of the infections currently managed in OPAT. 25 This is of significant value for patients living in rural settings as it eliminates potential logistical barriers for rural OPAT (i.e. home-health, infusions pharmacy, etc.). However, this should not be construed as a means to discharge patients without appropriate follow-up. Real-world implementation of an oral antibiotic treatment protocol in an orthopedic hospital demonstrated a higher rate of adverse drug reactions in the patients receiving oral antibiotics, largely related to gastrointestinal symptoms. 26 Additionally, Vollmer et al. demonstrated a high rate (36%) of unplanned discontinuation of oral antibiotic regimens for prosthetic joint infections (PJI) when using the Infectious Diseases Society of America (IDSA) PJI guideline preferred agent of a fluoroquinolone.27,28 While there is currently no guideline-based recommendation for minimum monitoring frequency for patients on oral therapy, formalized monitoring by an ID provider or potentially local provider is likely warranted.
Transitioning to oral antimicrobials can also be associated with barriers. Some oral antimicrobials may require prior authorization (e.g. linezolid) or may have quantity restrictions (e.g. fluoroquinolones) that can potentially limit access. Additionally, it should be noted that transitioning a patient to oral antimicrobials may change the patient’s ability to access certain resources (e.g. home health nursing services) despite the underlying infectious process remaining the same. Prior to transition to oral antimicrobials, either pre- or post-discharge, these barriers should be evaluated and addressed with the patient.
Long-acting lipoglycopeptides
Long-acting lipoglycopeptides (LaLGPs) such as IV dalbavancin and oritavancin can be used as a treatment strategy for patients living in rural areas with socioeconomic barriers to receiving OPAT who may not be appropriate candidates for oral therapy. Reasons for why a patient may not be a candidate for step-down to oral therapy include lack of adherence, impaired absorption, low bioavailability, drug-interactions, non-susceptible pathogens, and potential inability for an oral agent to penetrate the site of infection. 29 Dalbavancin and oritavancin are FDA approved for the treatment of complicated gram-positive skin and soft tissue infections; however, due to their long half-lives, they have been used off-label for deep-seated infections such as bloodstream infections, bone and joint infections and endocarditis. 30 The half-lives of dalbavancin and oritavancin have been described to range from 10–14 days. 29 Dosing strategies for off-label indications have varied; however, one to two doses have been commonly used for the treatment duration.29–31 There are several advantages to using LaLGPs. These agents can be used to facilitate patient discharge, allowing for a reduced patient length of stay. PICC line placement and potential associated complications can be avoided. The long half-life of dalbavancin and oritavancin provides a solution for patients who may not be adherent to IV or oral therapy. The low number of infusions required also allows patients to resume their daily activities and return back to work. 29 The need for home infusion and home health services can also be avoided with this method, although patients may still need to attend follow-up appointments or travel to a local clinic for lab work.
Most institutions restrict the inpatient use of LaLGPs to select patients in part due to higher acquisition costs compared to standard-of-care antibiotic therapies. While acquisition costs will vary per institution, the average wholesale price of a single-dose of dalbavancin 1500 mg or oritavancin 1200 mg typically ranges from $4057.20 to $6,037.20.32,33 Outpatient administration of LaLGPs can also be challenging as these medications often are non-formulary on most insurance plans and will require a prior authorization. Infusion centers may have difficulties obtaining these medications again due to cost. For patients who receive multiple doses of these medications, the first dose may be given inpatient on day 1 with the second dose being administered outpatient on day 8. 34 Additional consideration needs to be given to coordination of care to ensure patients can attend their follow-up appointment at the appropriate time interval to prevent incomplete or suboptimal antibiotic treatment.
Telemedicine in OPAT
The use of telemedicine is a practical approach to providing OPAT services to patients who reside in remote geographic locations. Telemedicine allows OPAT teams to communicate with patients through video calls or over the telephone without the patient having to attend an appointment in person. This is useful in situations where a patient lacks transportation and lives a long distance away. The 2018 Infectious Diseases Society of America clinical practice guideline for the management of OPAT also identifies telemedicine as a possible solution for patients in rural settings.1,21 Tan et al. reviewed the impact of a virtual OPAT clinic established in Australia. 35 During the roughly 4 year time period, 88 patients were managed remotely, with 37 patients living in remote or very remote settings. Unplanned readmission relating to OPAT and the infection were low (7%) and the clinic was able to avert over 100,000 km of travel. 35 A systematic review assessed the current available evidence for the clinical efficacy, safety, acceptability and cost-effectiveness of tele-OPAT. The meta-analysis included a total of 2572 OPAT patients, of which over 1245 received telemedicine. 36 The review found a significantly lower readmission risk in patients who received tele-OPAT compared to those that received conventional OPAT methods. Clinical cure rates were found to be comparable and similar rates of adverse events occurred between groups. Additionally, tele-OPAT was found to be more cost-effective than conventional OPAT methods. 36
With the on-going COVID pandemic, the capability of implementing telemedicine has increased drastically. It is important to note that areas of the U.S. that lack access to high-speed internet are largely rural which could inhibit teleconferencing applications. 37 Evaluation of the technological infrastructure should be included in the evaluation for OPAT. Telemedicine has the potential to help increase equitable access to care for patients; however, long term sustainability of clinics and financial compensation by payers will impact continued utilization moving forward.
Conclusion
The facilitation of OPAT services in rural areas is faced with several challenges, but can be effectively accomplished. Once a patient has been identified as living in a rural area and needing long-term antibiotic therapy, early coordination with ID providers, Care Management, and the OPAT team can help identify barriers to receiving safe and effective OPAT services. Further innovation and evaluation of healthcare delivery in the rural setting is warranted.
Acknowledgments
None.
Footnotes
ORCID iD: Keenan L. Ryan  https://orcid.org/0000-0002-5384-0711
https://orcid.org/0000-0002-5384-0711
Contributor Information
Meera Mehta, West Virginia University Hospitals, Morgantown, WV, USA.
Molly Benning, Inpatient Pharmacy Department, University of New Mexico Hospital, Albuquerque, NM, USA.
Jessica E. Johnson, Department of Medicine, Section of Infectious Diseases, West Virginia University, Morgantown, WV, USA
Keenan L. Ryan, Inpatient Pharmacy Department, University of New Mexico Hospital, 2211 Lomas Blvd, Albuquerque, NM 87106, USA.
Declarations
Ethics approval and consent to participate: Our study did not require ethical approval because this is a review article.
Consent for publication: There is a description of a patient scenario that was included with written consent from the patient.
Author contributions: Meera Mehta: Conceptualization; Writing – original draft; Writing – review & editing.
Molly Benning: Conceptualization; Writing – original draft; Writing – review & editing.
Jessica E. John: Conceptualization; Writing – original draft; Writing – review & editing.
Keenan L. Ryan: Conceptualization; Writing – original draft; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. Norris AH, Shrestha NK, Allison GM, et al. 2018 Infectious diseases society of America clinical practice guideline for the management of outpatient parenteral antimicrobial therapya. Clin Infect Dis 2019; 68: e1–e35. [DOI] [PubMed] [Google Scholar]
- 2. Jacobs DM, Leung W-Y, Essi D, et al. Incidence and risk factors for healthcare utilisation among patients discharged on outpatient parenteral antimicrobial therapy. Epidemiol Infect 2018; 146: 782–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Coughlin SS, Clary C, Johnson JA, et al. Continuing challenges in rural health in the United States. J Environ Health Sci 2019; 5: 90–92. [PMC free article] [PubMed] [Google Scholar]
- 4. Nielsen M, D’Agostino D, Gregory P. Addressing rural health challenges head on. Mo Med 2017; 114: 363–366. [PMC free article] [PubMed] [Google Scholar]
- 5. Rivera CG, Mahoney MV, Stevens RW, et al. Out of sight but not out of mind: caring for patients receiving OPAT during the SARS-CoV-2 pandemic. Open Forum Infect Dis 2020; 7: ofaa309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mansour O, Keller S, Katz M, et al. Outpatient parenteral antimicrobial therapy in the time of COVID-19: the urgent need for better insurance coverage. Open Forum Infect Dis 2020; 7: ofaa287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ratcliffe MBC, Holder K, Fields A. Defining rural at the U.S. census bureau American community survey and geography brief, https://www2.census.gov/geo/pdfs/reference/ua/Defining_Rural.pdf
- 8. United States Census Bureau. Quick facts west virginia, https://www.census.gov/quickfacts/WV
- 9. Centers for Disease Control and Prevention. Prevalence of self-reported obesity among U.S. adults by state and territory, https://www.cdc.gov/obesity/data/prevalence-maps.html#states
- 10. West Virginia Department of Health and Human Resources. Division of health promotion and chronic disease: data and reports, https://dhhr.wv.gov/hpcd/data_reports/
- 11. Ward BW, Black LI. State and regional prevalence of diagnosed multiple chronic conditions among adults aged ⩾18 years — United States, 2014. MMWR Morb Mortal Wkly Rep 2016; 65: 735–738. [DOI] [PubMed] [Google Scholar]
- 12. Bureau UC. State Area Measurements and Internal Point Coordinates. Census.gov, https://www.census.gov/geographies/reference-files/2010/geo/state-area.html (2021, accessed 1 May 2023).
- 13. Creamer J, Shrider EA, Burns K, et al. U.S. Census Bureau, Current Population Reports, P60-277, Poverty in the United States: 2021, U.S. Government Publishing Office, Washington, DC, September 2022. [Google Scholar]
- 14. Walensky RP, McQuillen DP, Shahbazi S, et al. Where is the ID in COVID-19? Ann Int Med 2020; 173: 587–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Triffault-Fillit C, Ferry T, Perpoint T, et al. Outpatient parenteral antibiotic therapy: evaluation of practices and limits of use in rural areas in France. Médecine et Maladies Infectieuses 2018; 48: 130–135. [DOI] [PubMed] [Google Scholar]
- 16. Medicare Payment Advisory Commission. March 2023 Report to the congress: medicare payment policy. Chapter 8 Home Health Care Services [Internet]. Washington, DC: MedPAC, https://www.medpac.gov/document/march-2023-report-to-the-congress-medicare-payment-policy/ (2023, accessed 18 March 2023). [Google Scholar]
- 17. WBOY News. Fairmont regional medical center officially closes, Marion Co. EMS prepares to adapt [Internet]. WBOY, https://www.wboy.com/top-stories/fairmont-regional-medical-center-officially-closes-marion-co-ems-prepares-to-adapt/ (2023, accessed 18 March 2023).
- 18. Current-Argus. NM rural hospitals suffer amid coronavirus pandemic [Internet]. Current-Argus, https://www.currentargus.com/story/news/local/2020/04/24/nm-rural-hospitals-suffer-amid-coronavirus-pandemic/5166957002/ (2020, accessed 18 March 2023)
- 19. Tanz LJ, Dinwiddie AT, Snodgrass S, et al. A qualitative assessment of circumstances surrounding drug overdose deaths during the early stages of the COVID-19 pandemic. SUDORS Data Brief, No 2. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, 2022. [Google Scholar]
- 20. Price CN, Solomon DA, Johnson JA, et al. Feasibility and safety of outpatient parenteral antimicrobial therapy in conjunction with addiction treatment for people who inject drugs. J Infect Dis 2020; 222: S494–S498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Paladino JA, Poretz D. Outpatient parenteral antimicrobial therapy today. Clin Infect Dis 2010; 51: S198–S208. [DOI] [PubMed] [Google Scholar]
- 22. Muldoon EG, Allison GM, Gallagher D, et al. Outpatient parenteral antimicrobial therapy (OPAT) in the republic of Ireland: results of a national survey. Eur J Clin Microbiol Infect Dis 2013; 32: 1465–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Madaline T, Nori P, Mowrey W, et al. Bundle in the Bronx: impact of a transition-of-care outpatient parenteral antibiotic therapy bundle on all-cause 30-day hospital readmissions. Open Forum Infect Dis 2017; 4: ofx097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Berrevoets MAH, Oerlemans AJM, Tromp M, et al. Quality of outpatient parenteral antimicrobial therapy (OPAT) care from the patient’s perspective: a qualitative study. BMJ Open 2018; 8: e024564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wald-Dickler N, Holtom PD, Phillips MC, et al. Oral is the new IV. Challenging decades of blood and bone infection dogma: a systematic review. Am J Med 2022; 135: 369–379.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Azamgarhi T, Shah A, Warren S. Clinical experience of implementing oral versus intravenous antibiotics (OVIVA) in a specialist orthopedic hospital. Clin Infect Dis 2021; 73: e2582–e2588. [DOI] [PubMed] [Google Scholar]
- 27. Vollmer NJ, Rivera CG, Stevens RW, et al. Safety and tolerability of fluoroquinolones in patients with staphylococcal periprosthetic joint infections. Clin Infect Dis 2021; 73: 850–856. [DOI] [PubMed] [Google Scholar]
- 28. Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the infectious diseases society of America. Clin Infect Dis 2013; 56: e1–e25. [DOI] [PubMed] [Google Scholar]
- 29. Krsak M, Morrisette T, Miller M, et al. Advantages of outpatient treatment with long-acting lipoglycopeptides for serious gram-positive infections: a review. Pharmacotherapy 2020; 40: 469–478. [DOI] [PubMed] [Google Scholar]
- 30. Tran TT, Gomez Villegas S, Aitken SL, et al. New perspectives on antimicrobial agents: long-acting lipoglycopeptides. Antimicrob Agents Chemother 2022; 66: e02614-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Morrisette T, Miller MA, Montague BT, et al. Long-acting lipoglycopeptides: “Lineless Antibiotics” for serious infections in persons who use drugs. Open Forum Infect Dis 2019; 6: ofz274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dalbavancin. Lexi-Drugs. Hudson, OH: Lexicomp. http://online.lexi.com/ (2023, accessed 29 March 2023). [Google Scholar]
- 33. Oritavancin. Lexi-Drugs. Hudson, OH: Lexiomp. http://online.lexi.com/ (2023, accessed 29 March 2023). [Google Scholar]
- 34. Allergan. Package insert: Dalvance (dalbavancin), https://www.allergan.com/assets/pdf/dalvance_pi (2021, accessed 29 March 2023).
- 35. Tan SJ, Ingram PR, Rothnie AJ, et al. Successful outpatient parenteral antibiotic therapy delivery via telemedicine. J Antimicrob Chemother 2017; 72: 2898–2901. [DOI] [PubMed] [Google Scholar]
- 36. Durojaiye OC, Jibril I, Kritsotakis EI. Effectiveness of telemedicine in outpatient parenteral antimicrobial therapy (Tele-OPAT): a systematic review. J Telemed Telecare. Epub ahead of print October 2022. DOI: 10.1177/1357633X221131842. [DOI] [PubMed] [Google Scholar]
- 37. Eight Broadband Progress Report. Federal communications commission, https://www.fcc.gov/reports-research/reports/broadband-progress-reports/eighth-broadband-progress-report (2012, accessed 21 March 2023).