Abstract
Fusions and mutations of anaplastic lymphoma kinase (ALK), a tyrosine kinase receptor, have been identified in several neoplastic diseases. Rearranged ALK is a driver of tumorigenesis, which activates various signaling pathway associated with proliferation and survival. To date, several agents that target and inhibit ALK have been developed. The most studied ALK-positive disease is non-small cell lung cancer, and three generations of ALK tyrosine kinase inhibitors (TKIs) have been approved for the treatment of metastatic disease. Nevertheless, the use of ALK-TKIs is associated with acquired resistance (resistance mutations, bypass signaling), which leads to disease progression and may require a substitution or introduction of other treatment agents. Understanding of the complex nature and network of resistance mutations may allow to introduce sequential and targeted therapies. In this review, we aim to summarize the efficacy and safety profile of ALK inhibitors, describe off-target anticancer effects, and discuss resistance mechanisms in the context of personalized oncology.
Keywords: anaplastic lymphoma kinase, ALK inhibitor, tyrosine kinase inhibitor, resistance mechanisms, personalized oncology
1 Introduction
Oncogenesis is a complex process associated with activation of oncogenes and inhibition of tumor suppressors. This leads to a constant cell proliferation and inhibition of apoptosis. Anaplastic lymphoma kinase (ALK) is a membrane tyrosine kinase receptor, which was identified for the first time in 1994 (Morris et al., 1994). The broad family of tyrosine kinase receptors plays a crucial role in cellular signaling and its abnormal activation due to receptor mutations is a long-known process of tumorigenesis (Lemmon and Schlessinger, 2010). In the case of ALK, it stimulates multiple signaling pathways associated with cell growth, including janus kinase-signal transducer and activator of transcription (JAK-STAT), mitogen activated protein kinases (MAPK), and phosphatidylinositol-3-kinase/protein kinase B (PI3K/AKT) pathways, among others (Figure 1). Numerous fusion partners of ALK have been identified (e.g., nucleophosmin (NPM)-ALK in anaplastic large cell lymphoma (ALCL) and echinoderm microtubule-associated protein-like 4 (EML4)-ALK in non-small cell lung cancer (NSCLC)). Furthermore, point mutations in the ALK receptor have been found in neuroblastoma and anaplastic thyroid cancer as well (Hallberg and Palmer, 2016). The aim of this review is to summarize generations of ALK tyrosine kinase inhibitors (TKI), present their efficacy and anti-cancer properties, and to discuss various mechanisms of resistance.
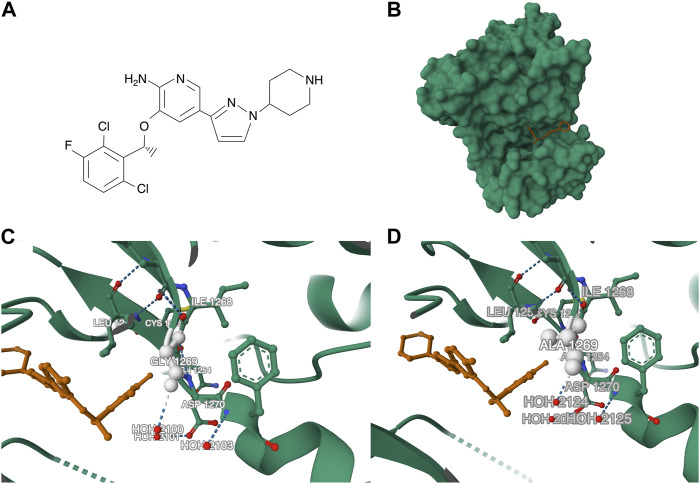
FIGURE 1.
A schematic illustration of ligand dependent ALK tyrosine kinase receptor and ALK fusions, which stimulate signaling pathways associated with proliferation and survival.
2 Anaplastic lymphoma kinase–structure and expression
The structure of ALK includes an extracellular domain (with two MAM and LDL-A domains), glycine-rich, transmembrane, and protein tyrosine kinase domains (Lee et al., 2010). Normal ALK protein is expressed at relatively low levels in most of the tissues, except for nervous system (Wu et al., 2017). While normal protein has extracellular and transmembrane domains, the majority of rearranged ALK proteins are considered to localize intracellularly (Chiarle et al., 2008; Sabir et al., 2017). Rearrangements of ALK have been broadly studied in the case of NSCLC. However, studies showed conflicting results regarding ALK expression rates, as populations with various baseline characteristics were examined. According to Shaw et al. (2009), out of 141 tumors, 19 (13%) were EML4-ALK positive. In separate studies by Zhang et al. (2016); Aguado de la Rosa et al. (2022), ALK rearrangements were observed in 5% and 5.5% of patients, respectively. Clinically, ALK rearrangement is associated with younger age, no history of smoking, advanced stage, and occurs more often in females (Fan et al., 2014; Aguado de la Rosa et al., 2022). Interestingly, these aberrations are associated with higher survival in surgically treated lung adenocarcinomas (Matsuura et al., 2023). EML4-ALK is the most-studied fusion in NSCLC. Based on the fusion breakpoints, several structurally different EML4-ALK variants have been identified. In NSCLC, variants 1 and 3a/b are the most common and presence v1 has been previously associated with improved clinical outcomes (Zhang et al., 2021). Importantly, as more advanced genetic testing methods are becoming more popular (e.g., next-generation sequencing (NGS)), multiple novel ALK-fusions have been identified. In 2020, approximately 90 ALK fusion partners in NSCLC have been described (Ou and Nagasaka, 2020). Moreover, ALK rearrangements have been identified in ALCL (translocation, 60%) (Falini et al., 1998), thyroid cancer (translocation, 2.2%) (Chou et al., 2015), and neuroblastoma (point mutation, 10.5%) (Rosswog et al., 2023), among others.
3 Anaplastic lymphoma kinase inhibitors
3.1 Anaplastic lymphoma kinase–I generation inhibitors
Crizotinib represents the first generation of ALK inhibitors, which was approved by the FDA for the treatment of NSCLC, as well as ALCL in children and young adults. It is a multitarget TKI, which inhibits ALK, mesenchymal epithelial transition growth factor (c‐MET) and ROS proto-oncogene 1 receptor kinase (ROS1) (Sahu et al., 2013). It prevents ATP from binding to ALK and its subsequent autophosphorylation (Bang, 2011). The drug showed antitumor activity in preclinical studies, as well as promising results in phase I clinical trials (Forde and Rudin, 2012). Crizotinib showed better outcomes (progression-free survival (PFS), partial response (PR)) in ALK-positive NSCLC compared to chemotherapy in phase 3 clinical trials (as a second- and first-line treatment agent). (Shaw et al., 2013; Solomon et al., 2014). In the study by Solomon et al. (2014) 13 reactions occurred more frequently in the crizotinib group than in chemotherapy. In contrast, 7 events were more common in chemotherapy cohort, while frequency of five reactions was similar between groups. Overall, the two most common adverse events (AEs) in the crizotinib group included vision disorder (71%), and diarrhea (61%). Importantly, these AEs rarely developed in grade 3–4 (1% and 2%, respectively). The most frequent grade 3–4 AEs in the study group included elevated aminotransferases (14%) and neutropenia (11%) (Solomon et al., 2014). Less is known about the efficacy of crizotinib in tumors other than NSCLC. Nevertheless, good response was presented in reports of patients with thyroid cancers (Godbert et al., 2015; de Salins et al., 2020) and inflammatory myofibroblastic tumors (IMT) (Kimbara et al., 2014; Ogata et al., 2019). According to the phase 2 study by Schöffski et al. (2021), objective response rate (ORR) was 66.7% in patients with ALK-positive IMT and 14.3% in ALK-negative tumors. Furthermore, in ALK-positive cohort, improved median PFS was observed (18 vs. 14.3 months).
Interestingly, ALK inhibitors may induce a process known as immunogenic cell death (ICD). Dying tumor cells release signals engaging the immune system, such as damage-associated molecular patterns (DAMPs), including ATP or high-mobility group box-1 (HMGB1). Furthermore, expression of certain proteins, such as calreticulin, promotes the activity of dendritic cells, and subsequently T cells (Ahmed and Tait, 2020). Liu et al. (2019) showed that crizotinib added to a human NSCLC line expressing EML4-ALK, resulted in a significant increase of calreticulin exposure, together with HMGB1 and ATP release. However, high concentrations of crizotinib induced hallmarks of ICD in EML4-ALK negative NSCLC cell lines (Figure 2). Moreover, a combination of standard chemotherapeutics with crizotinib induced immunogenicity in cancer model in vivo. Furthermore, crizotinib combined with cisplatin induced the expression of immune checkpoints in vivo and in vitro, which resulted in improved results of combination of crizotinib and immune checkpoint inhibitors (Liu et al., 2019). Furthermore, it has been demonstrated that EML4-ALK fusion induces the expression of PD-L1 through the PI3K and MEK/ERK pathways (Ota et al., 2015). Zhou and others investigated OS and PFS of 128 NSCLC patients treated with first-line crizotinib and divided them into two cohorts based on the PD-L1. Higher expression was associated with significantly worse PFS and OS (median 6 vs. 11 months, 17 vs. 53 months, respectively) (Zhou et al., 2022). In addition, an evaluation of 1001 NSCLC patients revealed that ALK and ROS1 rearrangement was associated with higher expression of PD-L1 (Chu et al., 2022). These results suggest that combination of ALK-TKIs with ICIs might provide good efficacy. Only a few studies examined this combination, but they showed significant AEs in included patients. Lin et al. described eleven patients treated sequentially with ICI and crizotinib. Five patients (45.5%) experienced grade 3/4 elevation of ALT, compared to 34 (8.1%) patients treated with crizotinib alone. Similarly, high AST concentrations (grade 3/4) were observed in the group with sequential treatment (36.4% vs. 3.4%) (Lin et al., 2019). Significant hepatotoxicity was also reported in studies evaluating crizotinib combined with nivolumab or pembrolizumab as a first-line treatment for advanced NSCLC (Spigel et al., 2018; Patel et al., 2020). Interestingly, crizotinib has been recently associated with another anti-cancer mechanism. Burikhanov et al. showed that crizotinib increased the expression of GRP78 (csGRP78), a cancer-related receptor, which triggers survival-related signaling pathways in KRAS-, NRAS, and EGFR-mutant NSCLC cells. Furthermore, the authors showed that crizotinib promoted a secretion of prostate apoptosis response-4 (Par-4) in normal cells, which binds to csGRP78 and triggers apoptosis. In mice models with ALK-negative tumor, crizotinib showed antitumor efficacy in PAR-4 +/+ animals, while it did not inhibit the growth of tumor in PAR-4 −/− mice. Therefore, crizotinib might have antitumor efficacy in both ALK-positive and negative cancers (Burikhanov et al., 2023).
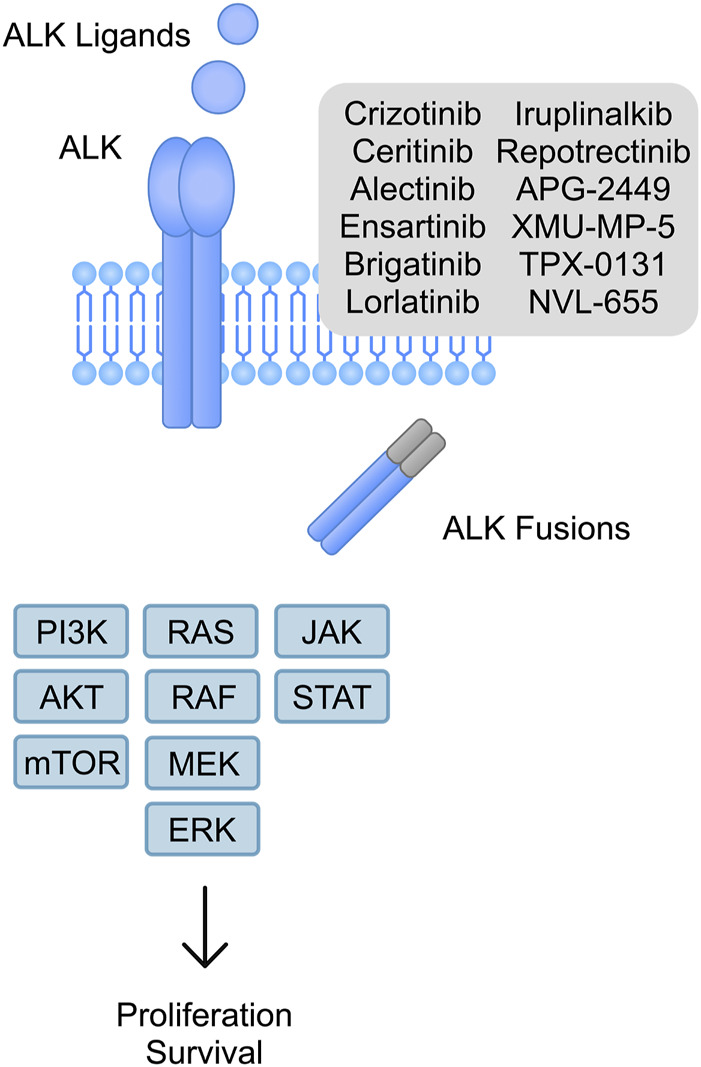
FIGURE 2.
A schematic illustration of additional anti-cancer mechanisms mediated by ALK inhibitors based on research performed by Liu et al. (2019); Petrazzuolo et al. (2021); Schäkel et al. (2022). (A) 1) Crizotinib and ceritinib in cells induce immunogenic cell death through 2) the release of DAMPs and 3) expression of calreticulin, 4) which stimulates dendritic cells and 5) T cells, inducing cytotoxic responses. (B) Ceritinib inhibits ectonuclease CD39, which prevents adenosine development and immunosuppressive actions.
Importantly, crizotinib has been investigated in combination with an anti-angiogenic agent. Angiogenesis is a significant mechanism in the process of tumorigenesis. Intratumoral blood vessels provide nutrients and oxygen supply to rapidly proliferating malignant cells. Vascular endothelial growth factor (VEGF) is a major pro-angiogenic mediator. Consequently, anti-angiogenic agents target VEGF or its receptors to inhibit the formation of new intratumoral vessels. Huang et al., described the safety and efficacy of crizotinib combined with bevacizumab, a monoclonal antibody targeting VEGF, in 14 patients with NSCLC, among whom ALK rearrangements were detected in 12 patients. The median PFS in a group of ALK-positive patients was 13.9 months, while the median OS was not reached. Therefore, this combination showed improved PFS than crizotinib monotherapy described in the PROFILE 1014 trial. The most common AEs in this combination were fatigue and rash, which occurred in 28.6% and 21.4%, respectively (Huang et al., 2021).
3.2 Anaplastic lymphoma kinase–II generation inhibitors
Several second-generation ALK TKIs have been developed to increase efficacy and overcome resistance to crizotinib. Ceritinib was approved by the FDA for the treatment of ALK-positive metastatic NSCLC. The drug inhibits ALK, insulin receptor, insulin growth factor receptor, and ROS1 (Khozin et al., 2015). In the ASCEND-5 trial, comparing ceritinib with chemotherapy in NSCLC, the former was associated with prolonged median PFS and better overall response (5.4 vs. 1.6 months; 39.1% vs. 6.9%, respectively) (Shaw et al., 2017). Furthermore, ceritinib showed improved outcomes in NSCLC as a first-line agent, compared to chemotherapy (Soria et al., 2017). In the first line setting, ceritinib was associated with higher frequency of diarrhoea, nausea, and vomiting, when compared to chemotherapy (85% vs. 11%; 69% vs. 55%; 66% vs. 36%, respectively). Furthermore, elevated enzymes related to hepatotoxicity were approximately three times more common in the ceritinib cohort (Soria et al., 2017). The role of cieritinib in a neoadjuvant setting still needs more investigation, but recent case report by Mai et al. (2022) demonstrated significant shrinkage of EML4-ALK positive adenosquamous carcinoma after two cycles of the TKI.
Ceritinib also shows important anti-cancer immunological effects. Adenosine signaling represents one of the mechanisms of immune escape performed by cancer cells. Schäkel et al. (2022) demonstrated that ceritinib inhibits ectonuclease CD39 in melanoma and triple negative breast cancer cells, which can contribute to the anti-cancer effects. In addition, in an in vitro experiment, Du and others showed that ceritinib decreases expression of PD-L1 in H2228 cells (NSCLC) through the inhibition of ERK (Du et al., 2020). Moreover, ceritinib was found to induce ICD in NPM1-ALK cells (Petrazzuolo et al., 2021) (Figure 2).
Other second-generation agents include alectinib, brigatinib, and ensartinib. Alectinib was approved by the FDA in 2015. The drug was developed for the treatment of patients with ALK receptor-positive NSCLC who are intolerant to crizotinib and whose disease has progressed (Larkins et al., 2016). Alectinib is a highly selective ALK inhibitor compared to crizotinib and is active against crizotinib resistance mutants (Sakamoto et al., 2011). The efficacy is related to its active metabolite M4, which suppresses cancer growth (Sato-Nakai et al., 2017). Inhibition of ALK autophosphorylation and phosphorylation of STAT3 and ALK (without ERK1/2) is the primary target of alectinib effective in NSCLC expressing EML4-ALK (Sakamoto et al., 2011). Alectinib penetrates the central nervous system (CNS), which is crucial for patients with brain metastases of NSCLC (Kodama et al., 2014; Ou et al., 2016). A recent retrospective study demonstrated superior real-world PFS in patients with advanced NSCLC treated with alectinib compared to crizotinib (Wang et al., 2023). Importantly, phase 3 trials (ALEX, J-ALEX, ALESIA) showed improved PFS in the alectinib cohort compared to crizotinib (Hida et al., 2017; Camidge et al., 2019; Zhou et al., 2019; Nakagawa et al., 2020). Moreover, the efficacy of chemotherapy versus alectinib in ALK-positive NSCLC patients previously treated with crizotinib was also compared. Alectinib has been proven to provide higher efficacy and longer PFS (Novello et al., 2018; Wolf et al., 2022). Additionally, alectinib may be used in a neoadjuvant setting. Loc et al. (2023) described 10 treatment-naïve patients treated with alectinib prior to surgery for advanced lung adenocarcinoma (stages III and IV). Fifty percent of patients showed a complete pathological response while major pathological response was detected in 90% of patients. As previously mentioned, in ALK positive patients treated with crizotinib, high expression of PD-L1 was associated with worse outcomes (Zhou et al., 2022). In contrast, PFS and OS of PD-L1 positive patients receiving alectinib did not significantly differ. Moreover, in the cohort of patients with PD-L1 tumor proportion score ≥50%, a positive trend regarding PFS was observed, but the result did not reach a statistical significance. ORR for PD-L1 negative and PD-L1 positive cohorts were 90% and 80.8%, respectively (Pan et al., 2023). As previously mentioned, alectinib shows a good penetration through blood-brain barrier. Thus, some studies evaluated its intracranial efficacy. For instance, Zou et al. (2022) described their experience with alectinib in patients with ALK-positive NSCLC and CNS metastases. These patients were divided into three cohorts, depending on their history of treatment. The first two groups involved patients, who were ALK-naïve or experienced an intracranial progression after treatment with crizotinib, respectively. The third cohort was composed of patients with CNS progression after treatment with other second generation ALK TKIs. In these groups, intracranial ORR was reported in 52.6%, 56.7%, and 33.3%, respectively (Zou et al., 2022).
Similarly to crizotinib, alectinib has also been evaluated in combination with agents targeting angiogenesis. Firstly, the protein expression of VEGF-A is elevated in NSCLC cells harboring ALK-rearrangement compared to control cell line. A preclinical study showed improved activity of combined alectinib with DC101, a VEGFR2 antibody in xenograft mouse models. Watanabe et al., demonstrated that above-mentioned combination was associated with a more significant tumor volume reduction in ALK-rearranged models, as compared to alectinib alone (Watanabe et al., 2021). In clinical settings, the combination of alectinib with bevacizumab has been investigated in an early phase trial. Eleven patients with ALK-rearranged advanced NSCLC have been evaluated. Importantly, 9 patients (81.8%) achieved an objective response and the median PFS was 19.8 months. Moreover, the ORR in 9 patients with CNS lesions was 77.8% (Lin et al., 2022). Another study investigated the use of alectinib with bevacizumab in 12 ALK-positive advanced (stages IIIB-IV) nonsquamous NSCLC patients who progressed on alectinib treatment. In contrast to the previous study, ORR was 8% and the median PFS was 3.1 months. However, a disease control rate was 67% and the median OS was 24.1 months. (Watanabe et al., 2022). These trials differed in case of efficacy. Nevertheless, the observed differences could result from baseline characteristics of included patients. In the former study, patients were ALK naive or received ALK TKIs other than alectinib. In contrast, the latter trial included patients previously treated with alectinib. Interestingly, a report by Nakasuka and others demonstrated that treatment with a combination of bevacizumab, pemetrexed and platinum promoted sensitivity to alectinib in primarily resistant patient with advanced ALK-positive NSCLC. However, the authors discovered that the tumor cells were alectinib sensitive prior to the initial treatment. Therefore, it was suggested that bevacizumab could stimulate the delivery of ALK TKI to the tumor (Nakasuka et al., 2019).
Ensartinib is another 2nd generation inhibitor which is not currently approved by the FDA. A phase 2 trial investigated the efficacy of ensartinib in a cohort of patients who progressed during the treatment with crizotinib. An objective response was observed in 52% of patients and the median PFS was 9.6 months. Importantly, an objective intracranial response and intracranial disease control were 70% and 98%, respectively (Yang et al., 2020). In addition, it showed an improved PFS compared to crizotinib as a first line ALK inhibitor in advanced, metastatic, or recurrent NSCLC cohort (Horn et al., 2021).
Brigatinib is an oral TKI approved by the FDA in 2020, which targets ALK and ROS1. Furthermore, in vitro studies showed a modest activity against FLT3, EGFR, insulin-like growth factor-1 receptor and INSR. Brigatinib inhibits ALK autophosphorylation and downstream phosphorylation of proteins such as AKT, STAT3, S6, and ERK1/2 (Hoy, 2021). Phase 3 ALTA-1L compared brigatinib to crizotinib in patients with advanced NSCLC, who did not previously receive an ALK inhibitor, and demonstrated a higher median PFS and ORR for brigatinib. Compared to crizotinib, brigatinib was associated with higher incidence (at least 5 percentage points) of increased blood creatinine kinase, cough, hypertension, and elevated lipase concentration. The percentage of patints who developed grade ≥3 AEs was slightly higher in the brigatinib group (61% vs. 55%), and the three most common serious AEs in this cohort included elevated blood creatinine kinase (16%), increased lipase level (13%), and hypertension (10%) (Camidge et al., 2018; Camidge et al., 2021). However, according to the ALTA-2 study, limited efficacy has been observed in case of NSCLC patients, who progressed on ceritinib and alectinib and were treated with brigatinib (ORR 26.2%, median PFS 3.8 months) (Ou et al., 2022). ALTA-3 trial compared the efficacy of brigatinib versus alectinib in NSCLC patients. The trial showed comparable efficacy between both TKIs (median PFS 19.3 months vs. 19.2 months for brigatinib and alectinib, respectively) (Chih-Hsin Yang et al., 2023). Furthermore, another study showed similar efficacy between both drugs in the first line setting in patients with ALK-positive advanced NSCLC in another study (Jeon et al., 2023). Second generation of ALK inhibitors are approved for the treatment of metastatic ALK positive NSCLC. Nonetheless, their efficacy has been detected in other diseases as well. For instance, brigatinib was effective in combination with chemotherapy and followed by stem cell transplantation in a pediatric patient with refractory ALCL (Caddeo et al., 2023).
3.3 Anaplastic lymphoma kinase–III generation inhibitor
Lorlatinib is a third generation ALK-TKI, which targets ALK and ROS1 and penetrates through blood-brain barrier. It was approved by the FDA in 2018 for patients with ALK-positive metastatic NSCLC, who progressed on first-line ALK inhibitors (crizotinib, alectinib, ceritinib) (Syed, 2019). Furthermore, recent study identified that lorlatinib induced tumor shrinkage in NSCLC patient with CLIP1-LTK fusion, indicating that it might also inhibit LTK kinase (Izumi et al., 2021). CROWN, a phase 3 clinical trial evaluating ALK-positive NSCLC patients, showed improved 12-month PFS and ORR with lorlatinib compared to crizotinib (80% vs. 35%; 76% vs. 58%, respectively). Furthermore, the study showed that the use of lorlatinib is significantly associated with hypercholesterolemia and hypertriglyceridemia, which respectively occurred in 70% and 64% of patients, as compared to 4% and 6% in the crizotinib cohort. The grade 3–4 severity of these AEs were 16% and 20%, respectively (Shaw et al., 2020). Recently, updated results from the CROWN study were published, which showed superior 3-year PFS in lorlatinib subgroup (64% vs. 19%) (Solomon et al., 2023). Moreover, the study also demonstrated significantly improved outcomes in patients with brain metastases (12-month PFS 78% vs. 22%) (Solomon et al., 2022). Different generations of ALK-TKIs can be used sequentially due to acquired resistance. Interestingly, patients who experienced resistance to lorlatinib may once again become sensitive for crizotinib and such therapy has been demonstrated in several reports (Shaw et al., 2016; Sakakibara-Konishi et al., 2019). Clinical efficacy of ALK-inhibitors in phase 3 trials has been summarized in Table 1.
TABLE 1.
A list of selected phase 3 clinical trials evaluating the efficacy of ALK inhibitors in non-small cell lung cancer.
| ALK-TKI | Name of the clinical trial/NCT registration number | ALK-naive | Arms | Number of patients | PFS (median months) | Response a |
|---|---|---|---|---|---|---|
| Crizotinib Shaw et al. (2013) | NCT00932893 | Yes | Crizotinib | 173 | 7.7 | 65% |
| Chemotherapy | 174 | 3 | 20% | |||
| Crizotinib Solomon et al. (2014) | PROFILE-1014 | Yes | Crizotinib | 172 | 10.9 | 74% |
| Chemotherapy | 171 | 7 | 45% | |||
| Ceritinib Shaw et al. (2017) | ASCEND-5 | Patients after crizotinib | Ceritinib | 115 | 5.4 | 39.1% |
| Chemotherapy | 116 | 1.6 | 6.9% | |||
| Ceritinib Soria et al. (2017) | ASCEND-4 | Yes | Ceritinib | 189 | 16.6 | 72.5% |
| Chemotherapy | 187 | 8.1 | 26.7% | |||
| Alectinib Camidge et al. (2019) | ALEX | Yes | Alectinib | 152 | 34.8 | 82,9% |
| Crizotinib | 151 | 10.9 | 75,5% | |||
| Alectinib Hida et al. (2017); Nakagawa et al. (2020) | J-ALEX | Yes | Alectinib | 103 | 34.1 | 92% |
| Crizotinib | 104 | 10.2 | 79% | |||
| Alectinib Wolf et al. (2022) | ALUR | Patients after crizotinib | Alectinib | 79 | 10.9 | 50.6% |
| Chemotherapy | 40 | 1.4 | 2.5% | |||
| Ensartinib Horn et al. (2021) | NCT02767804 | Yes | Ensartinib | 143 | 25.8 | 74% |
| Crizotinib | 147 | 12.7 | 67% | |||
| Brigatinib Camidge et al. (2018); Camidge et al. (2021) | ALTA-1L | Yes | Brigatinib | 137 | 24 | 71% |
| Crizotinib | 138 | 11.1 | 60% | |||
| Brigatinib Chih-Hsin Yang et al. (2023) | ALTA-3 | Patients after crizotinib | Brigatinib | 125 | 19.3 | 52% |
| Alectinib | 123 | 19.2 | 61% | |||
| Lorlatinib Shaw et al. (2020) | CROWN | Yes | Lorlatinib | 149 | - | 76% |
| Crizotinib | 147 | 9.3 | 58% |
the response includes an objective response rate or overall response, PFS, progression-free survival.
3.4 Novel anaplastic lymphoma kinase inhibitors
Iruplinalkib is a novel TKI, which suppresses ROS1 and ALK. The drug was found to inhibit phosphorylation of ALK, together with ERK and AKT (without STAT3) in vitro (NCI-H3122 cells). However, in an in vivo experiment (mouse NCI-H3122 xenograft model) iruplinalkib decreased phosphorylation of STAT3 and STAT5 (Yang et al., 2023). According to the phase 1 study by Shi et al., the use of iruplinalkib in ALK-rearranged patients resulted in objective response achieved in 58.2%. The ORR of 76% was observed in ALK-TKI naive patients. Among all patients, who received iruplinaklib, 97% of cases experienced AEs. The most common AEs (occurring in than 30% patients) were vomiting, nausea, hypercholesterolemia, and elevated hepatic enzymes (Shi et al., 2022). In a phase 2 study, advanced NSCLC patients with ALK-positive and crizotinib-resistant tumors were treated with iruplinalkib and ORR was 63% (Shi et al., 2023).
Lu and others developed XMU-MP-5, a new-generation ALK-TKI, which showed activity against EML4-ALK Ba/F3 cells. Moreover, in EML4-ALK Ba/F3, XMU-MP-5 inhibited ALK phosphorylation, together with downstream molecules (pSTAT3, pERK and pAKT). In addition, the novel drug inhibited proliferation of lung cancer cells (H3122), while reduced activity was observed in ALK negative lung cancer cells (A549, H1299, PC9) (L et al., 2022). Fang et al. described the development of APG-2449, which inhibits ALK, ROS1, and focal adhesion kinase (FAK). The authors observed that APG-2449 demonstrated antitumor properties in mice tumor models bearing different mutations (H3122 - EML4-ALK; KARPAS-299 - NPM-ALK; Ba/F3 - CD74-ROS1) (Fang et al., 2022).
Repotrectinib is another TKI, which targets ALK, ROS1, and TRK. In preclinical studies, it showed higher potency in EML4-ALK Ba/F3 cells, when compared to crizotinib. Furthermore, it presented similar activity to ceritinib, alectinib, and brigatinib, while it showed decreased potency compared to lorlatinib (Drilon et al., 2018). Moroever, repotrectinib showed antitumor efficacy in ALK-dependent neuroblastoma cells (Cervantes-Madrid et al., 2019). TPX-0131 and NVL-655 are two other drugs, which showed activity against wild type and mutant ALK, and are considered as a fourth generation ALK inhibitors (Murray et al., 2021; Pelish et al., 2021). Phase 1/2 clinical trial (NCT05384626) will evaluate dose-limiting toxicities, dosage, and ORR in ALK-positive advanced/metastatic NSCLC or other solid tumors (Inc, 2022). Furthermore, recent studies report several novel compounds/agents capable of inhibiting ALK (Wang et al., 2022; Cao et al., 2023; Fan et al., 2023).
4 Anaplastic lymphoma kinase inhibitors–resistance mechanisms
The use of ALK-TKIs is associated with acquired resistance, which may require the use of other treatment agent [median duration of response with crizotinib was 11.3 months according to the study by Solomon et al. (2014)]. Resistance may develop due to several mechanisms, such as secondary ALK mutation or amplification (Figure 3). Shaw et al. (2014) described 19 ALK-positive NSCLC patients with disease progression on crizotinib, who were later treated with ceritinib. In this subgroup, seven patients were identified with acquired ALK mutations or amplification. Interestingly, 12 patients did not have any additional genetic ALK aberrations. Katayama and others described 18 crizotinib-resistant ALK-positive NSCLC patients. High-level amplification was detected in only one patients while resistance mutations was identified in 4 patients (Katayama et al., 2012). These findings suggest that crizotinib might insufficiently inhibit ALK or that other mechanisms unrelated to ALK rearrangements might confer resistance. For instance, cancer cells might become stimulated through other tyrosine kinases, which is known as a bypass signal-induced resistance. In the case of ALK, activation of signaling pathways through EGFR, HER2, and HER3 with concomitant absence of ALK secondary mutations has been observed (Tanizaki et al., 2012). Tani et al. demonstrated that a knockdown of TGFα (a ligand of EGFR), restores the sensitivity to alectinib in resistant NSCLC cell line (H3122-AR) (Tani et al., 2016). EGFR signaling has been also found in lorlatinib-resistant cell lines (Katayama et al., 2023). Clinically, case reports showed detection of EGFR mutation in patients treated with various generations of ALK inhibitors. Michaux et al. demonstrated NSCLC patients, who were respectively sequentially treated with crizotinib + alectinib and alectinib + lorlatinib, and who developed EGFR mutations. Strategies used to overcome resistance included an introduction of brigatinib (shows activity against EGFR), a combination of ALK and EGFR inhibitors, and chemotherapy (Michaux et al., 2023). Thus, EGFR bypass is an important resistance mechanism which could develop after treatment with various generations of ALK-TKIs. Overcoming bypass resistance represents a significant clinical challenge. Introduction of dual inhibitors, which showed promising efficacy in in vitro experiments, could become a novel opportunity for these patients in the future (An et al., 2023). Interestingly, Talwelkar et al. demonstrated that combining ALK inhibitors with agents targeting its downstream molecule (PI3Kβ) is associated with an improved anticancer efficacy in ALK-rearranged NSCLC cell lines (Talwelkar et al., 2023). Similarly, a combination of crizotinib with duvelisib (PI3Kδ/γ inhibitor) increased anticancer efficacy in ALCL cell lines partially resistant to ALK inhibitors, as well as in an in vivo experiment (Mastini et al., 2023). In the case of enhanced HER3 phosphorylation as a resistance mechanism, a combination of pan-HER inhibitors, such as afatinib and dacomitinib, with lorlatinib might resensitize cells to the third generation ALK inhibitor, which has been recently demonstrated in an in vitro experiment (Taniguchi et al., 2023).
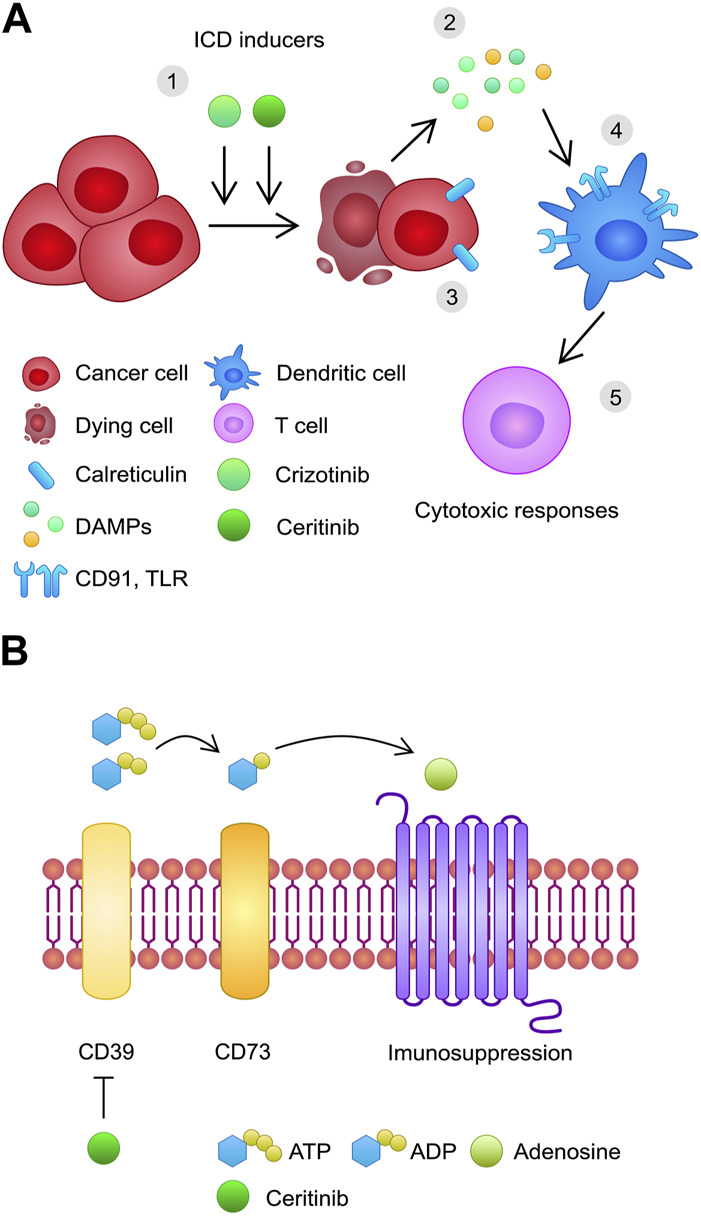
FIGURE 3.
A schematic illustration of acquired resistance mechanisms to ALK inhibitors, including (A) resistance mutations; (B) amplification; (C) bypass signaling; (D) epithelial to mesenchymal transition. (E) A potential course of sequential treatment of ALK-positive cancer with a development of subsequent resistance mutations.
Additionally, an in vitro study showed that alectinib resistance is associated with increased phosphorylation of MET and elevated expression of hepatocyte growth factor (HGF). Inhibition of MET restored alectinib sensitivity. Moreover, a combination of metformin with alectinib lead to an interesting discovery of restoring alectinib sensitivity through the suppression of Gab1, an element of the HGF/MET signaling pathway (Chen et al., 2020). In clinical settings, Shiraishi and others have recently reported an ALK-positive NSCLC patient, who was treated with alectinib, lorlatinib, chemotherapy with carboplatin and nanoparticle albumin-bound paclitaxel, and bevacizumab, but the disease progressed. NGS analysis confirmed an amplification of the MET and HER2 genes. An introduction of crizotinib showed improvement for 4 months, until the disease progressed again (Shiraishi et al., 2023). Importantly, MAPK mutations also have been found to confer resistance to ALK inhibitor in neuroblastoma (Berko et al., 2023).
Moreover, a study conducted by Gainor et al. (2016) investigated resistance mutations after treatment with various ALK-TKIs. L1196M and G1269A mutations were the most common among resistance mutations identified in crizotinib-treated patients (7% and 4%, respectively) (Figure 4). Other mutations included I1171T, E1210K, G1202R, S1206Y, and C1156Y. In addition, the authors evaluated mutation profiles after treatment with second-generation TKIs. After treatment with ceritinib (24 patients, 21 after previous crizotinib treatment), 54% and 17% presented single and several ALK resistance mutations, respectively. G1202R and F1174C/L were the most frequent (21% and 16.7%, respectively). Two cases with C1156Y mutations also harbored other ALK aberrations (I1171N; V1180L and G1202del). Among 17 patients treated with crizotinib and alectinib, 9 patients with ALK mutations were identified: G1202R (29%), I1171T/S (12%), V1180L (6%), and L1196M (6%). In the brigatinib cohort (5 out of 6 previously treated with crizotinib), G1202R mutation was the most common. Furthermore, the study showed that treatment with second generation of ALK TKIs is associated with more common ALK resistance mutations compared to crizotinib (Gainor et al., 2016). Shaw and others performed a similar study, additionally evaluating molecular analysis (tumor tissue, cell-free DNA) and its relationship with response to lorlatinib. The authors found that treatment with the third generation TKI was associated with ORR 73% of NSCLC patients previously treated with crizotinib. Response rate did not differ between cohorts with or without ALK mutation. In contrast, lorlatinib treatment in patients with ≥1 prior second generation ALK-TKI was correlated with better response in mutation-positive cohort (62% vs. 32%, respectively). Importantly, lorlatinib showed antitumor efficacy in the five most common resistance mutations (G1202R/del, F1174X, L1196M, G1269A, I1171X) (Shaw et al., 2019).
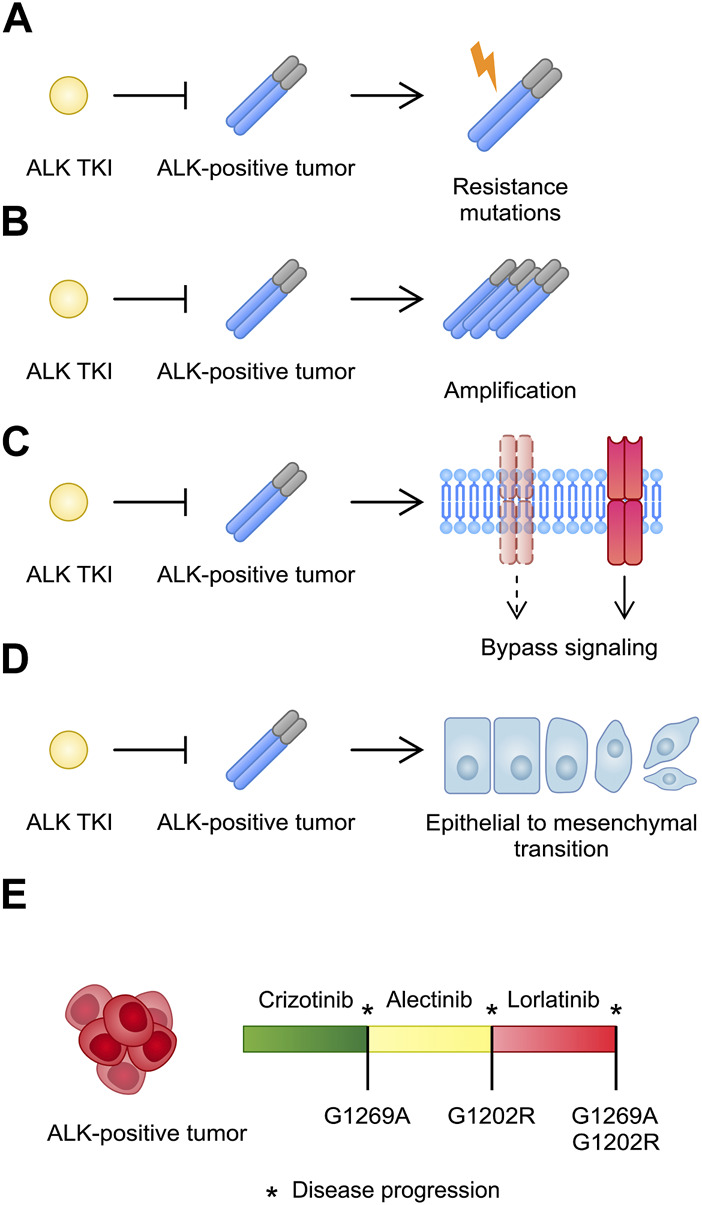
FIGURE 4.
(A) Chemical structure of crizotinib. (B) Structure of the ALK in complex with crizotinib [PDB ID: 2XP2 (Berman et al., 2000; Cui et al., 2011; Sehnal et al., 2021)]. (C) Structure of the ALK in complex with crizotinib with focus on the G1269 region (PDB ID: 2XP2). (D) Structure of the G1269A mutant ALK [PDB ID: 4ANQ (Huang et al., 2014)].
Therefore, acquired mutations are associated with various sensitivity profiles towards other ALK-TKIs. For instance, alectinib shows antitumor activity in cells with ALK G1269A mutation (Yoshimura et al., 2016). Moreover, ceritinib demonstrates efficacy against G1269A, I1171T, S1206Y, and L1196M mutations, among others (Friboulet et al., 2014). Importantly, novel ALK-TKIs demonstrate efficacy against resistance mutations as well. For instance, in ALK mutant Ba-F3 cell lines, XMU-MP-5 showed efficacy against G1269A and 1196M mutations, together with I1171T, C1156Y, and S1206Y. The half-maximal inhibitory concentration (IC50) of XMU-MP-5 in G1202R mutation was 49.4 nM. In contrast, in the same mutation, IC50 of crizotinib, alectinib and brigatinib was 206, 479 and 433 nM, respectively. XMU-MP-5 was inactive against cells harboring F1174L mutation (L et al., 2022). APG-2449 showed efficacy in mice with ALK L1196M mutation. Furthermore, it achieved better antitumor activity in G1202R mutations than crizotinib, ceritinib, ensartinib, and alectinib (Fang et al., 2022). Furthermore, in a study by Drilon et al., repotrectinib showed comparable activity to lorlatinib against EML4-ALK Ba/F3 cells harboring G1202R resistance mutation (Drilon et al., 2018). In another study, G1202R and I1171N mutants (alectinib-resistant) showed sensitivity to repotrectinib and ensartinib in Ba/F3 cells, respectively. The authors also predicted repotrectinib resistance mutations (G1202R + L1196M, F1174C/L/I, E1129V/K, C1156Y) (Doi et al., 2022).
Importantly, the majority of cells harboring single ALK mutations seem to be sensitive to lorlatinib (Gainor et al., 2016). However, L1256F represents a lorlatinib-resistant single mutation (Okada et al., 2019). Additionally, the development of resistance mutations seems dynamic, as they might become indetectable in plasma after introduction of higher generation TKI (Hua et al., 2022). Recent studies started to reveal multiple mutations, which drive resistance to the third generation TKI. For instance, G1269A + G1202R, I1171N + L1198F, and G1202R + S1206F + G1269A represent mutations identified in lorlatinib-treated patients. Importantly, Shiba-Ishii demonstrated that lorlatinib analogs might poses higher sensitivity towards these mutations (Shiba-Ishii et al., 2022). These mutations seem to develop more often in patients treated sequentially with first, second, and third lines of ALK-TKIs (Hua et al., 2022). Importantly, after occurrence of a compound mutation the patient may still respond to a previous-line ALK inhibitors. For instance, Takahashi et al. showed that Ba/F3 cells harboring I1171S + G1269A double mutation were resistant to crizotinib, alectinib and lorlatinib. In contrast, sensitivity was detected when cells were treated with brigatinib and ceritinib (Takahashi et al., 2020). Furthermore, lorlatinib-resistant patients may also benefit from re-administration of crizotinib. Sakakibara-Konishi et al. described a patient, who was treated with crizotinib, alectinib, and lorlatinib (as well as with standard chemotherapeutics), but subsequently progressed. In post-lorlatinib sample, the authors identified G1269A mutation, low ALK copy number gain, and MET amplification. Since crizotinib is a MET inhibitor, this alteration could have contributed to the resensitization (Sakakibara-Konishi et al., 2019). Moreover, Shaw et al. (2016) reported a patient who developed resistance to crizotinib (C1156Y mutation), but subsequently responded to lorlatinib. Nevertheless, resistance to the third generation TKI developed approximately 8 months later (L1198F mutation). Interestingly, the amount of tumor cells with C1156Y mutation substantially increased (50% after crizotinib treatment and nearly 100% after the development of lorlatinib resistance). A subsequent in vitro experiment revealed that Ba/F3 cells expressing ALK L1198F-C1156Y were resistant to second and third generation of ALK-TKI, but treatment with crizotinib showed good efficacy. Structural analysis revealed that L1198 is located close to ATP-binding site, which decreased lorlatinib binding affinity (Shaw et al., 2016). Interestingly, Mizuta and others demonstrated that some TKIs may demonstrate off target effects and present antitumor efficacy in cells with ALK resistance mutations. The authors found that gilteritinib, a TKI used to treat FLT3 (+) refractory acute myeloid leukemia, inhibited viabillity of Ba/F3 cells harboring EML4-ALK I1171N + F1174I mutations. Importantly, these cells were resistant to first, second, and third generation of ALK-TKI. Furthermore, gliteritinib inhibited I1171N + L1198H mutant, which partialy responded only to crizotinib and brigatinib. Moreover, among gliteritinib, alectinib and lorlatinib, low concentrations the former inhibited phosphorylation of ALK in I1171N + F1174I mutant overexpressed H3122 cells. Gliteritinib also showed good efficacy against number of single mutations resistant to second- or third-generation ALK inhibitors, such as I1171N or L1256F, as well as compound mutations resistant to lorlatinib (I1171N + L1256F) (Mizuta et al., 2021). Novel ALK TKIs represent a promising perspective regarding the compound mutations. For instance, Doi et al. showed that TPX-0131 inhibits mutations composed of G1202R with L1196M, E1129V, and C1156Y (Doi et al., 2022).
Nonetheless, ALK-rearranged tumors may still show resistance to all three generations of ALK-TKIs due to primary resistance mechanisms. For instance, simultanous mutations in other genes might confer such resistance. Kunimasa and others reported a patient with lung adenocarcinoma, who rapidly progressed on crizotinib (4 months), lorlatinib (1 month) and alectinib (1 month). NGS analysis revealed co-occurrence of PIK3CA E542K and RB1 L303V mutations in all sites (Kunimasa et al., 2021).
In addtion, resistance to ALK inhibitors may involve histological transformation. Fujita et al. reported a patient with metastatic lung adenocarcinoma, who was treated with crizotinib for 7 months, until the disease progressed. After standard chemotherapy, the patient was given alectinib. Surprisingly, metastatic lesions responded to treatment, but primary tumor progressed. Subsequent biopsy confirmed small cell lung cancer (Fujita et al., 2016). Transformation of metastatic lesion was recently reported by Xia and others (Xia et al., 2023). Importantly, both tumors remained ALK-positive after transformation. Recently, another report described a patient with small cell lung cancer transformation, which was followed by a NSCLC metastasis with I1171T mutation. To control both NSCLC and small cell lung cancer, the patient received temozolamide in combination with lorlatinib (Majeed et al., 2023). Moreover, a process of epithelial to mesenchymal transition (EMT) can play a role in ALK TKI resistance. EMT is an important mechanism taking part in embryogenesis. In tumorigenesis, EMT has been associated with the ivasiveness of cancer cells (Huang et al., 2022). Lung cancer resistant to crizotinib also showed a mesenchymal features. Importantly, silencing vimentin, a marker of a mesenchymal phenotype, improved the anti-cancer effects of ALK inhibitors (Kim et al., 2013). Furthermore, hypoxic condition could also contribute to the ALK TKI resistance through the induction of EMT (Kogita et al., 2014). Therefore, the disease can develop several resistance mechanisms to resist ALK inhibitors.
As demonstrated above, multiple studies have investigated resistance mechanisms in ALK-positive NSCLC. Nevertheless, the efficacy of ALK-TKI may differ in patients with less frequent ALK fusion partners. Kang eat al. described 11 NSCLC patients with huntingtin-interacting protein 1 (HIP1)-ALK rearrangements, among whom one patient with adenosquamous cell cancer harbored three fusions (EML4-ALK, HIP1-ALK, and ALK-PLEKHH20). Crizotinib was given to ten patients and in 9 cases an objective response was observed. Median OS and PFS were 58.8 and 17.9 months, respectively. First-line Lorlatinib was given to one patient, who achieved PR for over 26.5 months. Six variants of HIP1-ALK could be identified from these 11 patients: H21:A20, H28:A20, H30:A20, H19:A20, H19:A19, and H1:A16 (Kang et al., 2022). What’s more, it is unclear whether abundance of mutation contributes to the treatment sensitivity. In EGFR-mutated lung cancer, higher adjusted variant allele frequency (aVAF) has been associated with better efficacy of EGFR-TKI (Gieszer et al., 2021). According to Rao et al. (2023), aVAF was not correlated with PFS in first line crizotinib treatment. Furthermore, the authors did not find any correlations between PFS and ALK subclonality thresholds. Nevertheless, technical limitations of NGS might contribute to the negative results (Rao et al., 2023). In contrast, a recent study by Hizal et al. demonstrated that patients stratified by the expression of ALK-positive cells (NSCLC) respond differently to the first line alectinib treatment. Higher expression was associated with elevated ORR and PFS (Hizal et al., 2023). ALK VAF was found to correlate with clinical course in some patients with neuroblastoma. Berko and others showed that disease progression was associated with an elevation of VAF, while decrease or stable VAF level were observed in patients responding to lorlatinib. Nevertheless, a group of patients with small VAF and disease progression was observed as well, which might result from tumor heterogeneity or mutaitons of other genes (Berko et al., 2023). Furthermore, monitoring of interleukins may also help identify disease progression. Angeles and others investigated serum from ALK positive NSCLC patients treated with ALK inhibitors and found that elevation of IL-8, IL-6 and IL-10 were associated with disease progression (Angeles et al., 2023).
5 Conclusions and future perspectives
To conclude, targeted and individualized oncology represents a novel and hopeful trend in treating patients with neoplastic diseases. A recent study performed by Scott and others illustrates this sentence very well. The authors showed that inferior survival outcomes were achieved in NSCLC patients treated before the detection of actionable oncogenic drivers, and who were not subsequently switched to according TKIs, as compared to patients whose treatment began after the mutation report (Scott et al., 2023). To date, NSCLC remains the most studied ALK-positive cancer and good efficacy of ALK inhibitors resulted in approval of these agents for the treatment of metastatic NSCLC. Recently, crizotinib was also approved for the treatment of ALCL and IMT, which shows that ALK inhibitors can be beneficial in patients with various ALK-positive neoplastic diseases. However, it is worth mentioning that despite good and promising efficacy, these drugs may induce serious adverse reactions. Therefore, application of ALK inhibitors requires monitoring for drug-specific AEs. Furthermore, the treatment with ALK inhibitors is associated with acquired resistance. With the use of NGS and circulating tumor DNA (ctDNA), we can monitor genetic aberrations and detect resistance mutations. CtDNA molecules harbor genetic profiles of the primary tumor and can be identified in the blood. Therefore, monitoring ctDNA is an interesting and non-invasive method of molecular profiling (Cheng et al., 2016). For instance, ctDNA monitoring may be used to detect molecular residual disease after curative-intent first line treatment and to evaluate the risk of recurrence (Chaudhuri et al., 2017). Qiu et al. demonstrated that a positive ctDNA detection could precede the radiological recurrence of NSCLC by 88 days (Qiu et al., 2021). In patients treated with ALK inhibitors, the detection of ctDNA could identify a resistance mechanism and thus, discontinue the current treatment or apply another targeted agent (Guo et al., 2018).
Recent studies allowed us to understand the sensitivity profiles of these mutations to other treatment agents. Consequently, patients who progress on ALK inhibitors may still benefit from other mutation-sensitive agents. In addition, a detection of bypass signaling may require an introduction of other targeted therapies, which could prolong the response. Importantly, as sequential use of ALK inhibitors is correlated with occurrence of multiple mutations, further research should evaluate the sensitivity profiles of these genetic aberrations. Novel ALK-TKIs may be required to overcome the development of several mutations. Moreover, future studies should focus on investigating novel ALK-rearrangements and co-occurrence of mutations, which may drive a primary resistance to ALK inhibitors.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The publication fee was financed by the Pomeranian Medical University in Szczecin, Poland.
Author contributions
KK: Writing–original draft, Writing–review and editing. JŻ: Writing–original draft, Writing–review and editing. RB: Conceptualization, Supervision, Writing–original draft, Writing–review and editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Aguado de la Rosa C., Cruz Castellanos P., Lázaro-Quintela M., Dómine M., Vázquez Estévez S., López-Vivanco G., et al. (2022). Identification of ALK-positive patients with advanced NSCLC and real-world clinical experience with crizotinib in Spain (IDEALK study). Lung Cancer 173, 83–93. 10.1016/j.lungcan.2022.09.010 [DOI] [PubMed] [Google Scholar]
- Ahmed A., Tait S. W. G. (2020). Targeting immunogenic cell death in cancer. Mol. Oncol. 14 (12), 2994–3006. 10.1002/1878-0261.12851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- An B., Fan Y., Li W., Nie W., Nie H., Wang M., et al. (2023). Discovery of potent and effective inhibitors containing sulfoxide structures targeting EML4-ALK rearrangement and EGFR mutant non-small cell lung cancer. Bioorg Chem. 138, 106653. 10.1016/j.bioorg.2023.106653 [DOI] [PubMed] [Google Scholar]
- Angeles A. K., Janke F., Daum A. K., Reck M., Schneider M. A., Thomas M., et al. (2023). Integrated circulating tumour DNA and cytokine analysis for therapy monitoring of ALK-rearranged lung adenocarcinoma. Br. J. Cancer 129, 112–121. 10.1038/s41416-023-02284-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bang Y. J. (2011). The potential for crizotinib in non-small cell lung cancer: a perspective review. Ther. Adv. Med. Oncol. 3 (6), 279–291. 10.1177/1758834011419002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berko E. R., Witek G. M., Matkar S., Petrova Z. O., Wu M. A., Smith C. M., et al. (2023). Circulating tumor DNA reveals mechanisms of lorlatinib resistance in patients with relapsed/refractory ALK-driven neuroblastoma. Nat. Commun. 14 (1), 2601. 10.1038/s41467-023-38195-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman H. M., Westbrook J., Feng Z., Gilliland G., Bhat T. N., Weissig H., et al. (2000). The protein data bank. Nucleic Acids Res. 28 (1), 235–242. 10.1093/nar/28.1.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burikhanov R., Ganguly S., Ellingson S., Sviripa V. M., Araujo N., Li S., et al. (2023). Crizotinib induces Par-4 secretion from normal cells and GRP78 expression on the cancer cell surface for selective tumor growth inhibition. Am. J. Cancer Res. 13 (3), 976–991. [PMC free article] [PubMed] [Google Scholar]
- Caddeo G., Tecchio C., Chinello M., Balter R., Zaccaron A., Vitale V., et al. (2023). Refractory anaplastic large cell lymphoma rescued by the combination of the second-generation ALK inhibitor brigatinib, high-dose chemotherapy and allogeneic stem cell transplantation: a case report and review of the literature. Clin. Hematol. Int. 5, 130–138. 10.1007/s44228-023-00038-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camidge D. R., Dziadziuszko R., Peters S., Mok T., Noe J., Nowicka M., et al. (2019). Updated efficacy and safety data and impact of the EML4-ALK fusion variant on the efficacy of alectinib in untreated ALK-positive advanced non-small cell lung cancer in the global phase III ALEX study. J. Thorac. Oncol. 14 (7), 1233–1243. 10.1016/j.jtho.2019.03.007 [DOI] [PubMed] [Google Scholar]
- Camidge D. R., Kim H. R., Ahn M. J., Yang J. C., Han J. Y., Lee J. S., et al. (2018). Brigatinib versus crizotinib in ALK-positive non-small-cell lung cancer. N. Engl. J. Med. 379 (21), 2027–2039. 10.1056/NEJMoa1810171 [DOI] [PubMed] [Google Scholar]
- Camidge D. R., Kim H. R., Ahn M. J., Yang J. C. H., Han J. Y., Hochmair M. J., et al. (2021). Brigatinib versus crizotinib in ALK inhibitor-naive advanced ALK-positive NSCLC: final results of phase 3 ALTA-1L trial. J. Thorac. Oncol. 16 (12), 2091–2108. 10.1016/j.jtho.2021.07.035 [DOI] [PubMed] [Google Scholar]
- Cao Z., Zhang J., Guo M., Shao B., Wei X., Li S., et al. (2023). Discovery of novel phenyl triazole analogs as TRK/ALK dual inhibitors with prospective antitumor effects. Bioorg Chem. 136, 106563. 10.1016/j.bioorg.2023.106563 [DOI] [PubMed] [Google Scholar]
- Cervantes-Madrid D., Szydzik J., Lind D. E., Borenäs M., Bemark M., Cui J., et al. (2019). Repotrectinib (TPX-0005), effectively reduces growth of ALK driven neuroblastoma cells. Sci. Rep. 9 (1), 19353. 10.1038/s41598-019-55060-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri A. A., Chabon J. J., Lovejoy A. F., Newman A. M., Stehr H., Azad T. D., et al. (2017). Early detection of molecular residual disease in localized lung cancer by circulating tumor DNA profiling. Cancer Discov. 7 (12), 1394–1403. 10.1158/2159-8290.CD-17-0716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Lin C., Peng T., Hu C., Lu C., Li L., et al. (2020). Metformin reduces HGF-induced resistance to alectinib via the inhibition of Gab1. Cell. Death Dis. 11 (2), 111. 10.1038/s41419-020-2307-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng F., Su L., Qian C. (2016). Circulating tumor DNA: a promising biomarker in the liquid biopsy of cancer. Oncotarget 7 (30), 48832–48841. 10.18632/oncotarget.9453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiarle R., Voena C., Ambrogio C., Piva R., Inghirami G. (2008). The anaplastic lymphoma kinase in the pathogenesis of cancer. Nat. Rev. Cancer 8 (1), 11–23. 10.1038/nrc2291 [DOI] [PubMed] [Google Scholar]
- Chih-Hsin Yang J., Liu G., Lu S., He J., Burotto M., Ahn M. J., et al. (2023). Brigatinib versus alectinib in ALK-positive non-small cell lung cancer after disease progression on crizotinib: results of phase 3 ALTA-3 trial. J. Thorac. Oncol. 10.1016/j.jtho.2023.08.010 [DOI] [PubMed] [Google Scholar]
- Chou A., Fraser S., Toon C. W., Clarkson A., Sioson L., Farzin M., et al. (2015). A detailed clinicopathologic study of ALK-translocated papillary thyroid carcinoma. Am. J. Surg. Pathol. 39 (5), 652–659. 10.1097/PAS.0000000000000368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C. H., Huang Y. H., Lee P. H., Hsu K. H., Chen K. C., Su K. Y., et al. (2022). Various impacts of driver mutations on the PD-L1 expression of NSCLC. PLoS One 17 (8), e0273207. 10.1371/journal.pone.0273207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui J. J., Tran-Dubé M., Shen H., Nambu M., Kung P. P., Pairish M., et al. (2011). Structure based drug design of crizotinib (PF-02341066), a potent and selective dual inhibitor of mesenchymal-epithelial transition factor (c-MET) kinase and anaplastic lymphoma kinase (ALK). J. Med. Chem. 54 (18), 6342–6363. 10.1021/jm2007613 [DOI] [PubMed] [Google Scholar]
- de Salins V., Loganadane G., Joly C., Abulizi M., Nourieh M., Boussion H., et al. (2020). Complete response in anaplastic lymphoma kinase-rearranged oncocytic thyroid cancer: a case report and review of literature. World J. Clin. Oncol. 11 (7), 495–503. 10.5306/wjco.v11.i7.495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doi Y., Tagaya H., Noge A., Semba K. (2022). Prediction of resistance mutations against upcoming anaplastic lymphoma kinase inhibitors. Target Oncol. 17 (6), 695–707. 10.1007/s11523-022-00919-5 [DOI] [PubMed] [Google Scholar]
- Drilon A., Ou S. I., Cho B. C., Kim D. W., Lee J., Lin J. J., et al. (2018). Repotrectinib (TPX-0005) is a next-generation ROS1/TRK/ALK inhibitor that potently inhibits ROS1/TRK/ALK solvent- front mutations. Cancer Discov. 8 (10), 1227–1236. 10.1158/2159-8290.CD-18-0484 [DOI] [PubMed] [Google Scholar]
- Du P., Hu T., An Z., Li P., Liu L. (2020). In vitro and in vivo synergistic efficacy of ceritinib combined with programmed cell death ligand-1 inhibitor in anaplastic lymphoma kinase-rearranged non-small-cell lung cancer. Cancer Sci. 111 (6), 1887–1898. 10.1111/cas.14397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falini B., Bigerna B., Fizzotti M., Pulford K., Pileri S. A., Delsol G., et al. (1998). ALK expression defines a distinct group of T/null lymphomas ("ALK lymphomas") with a wide morphological spectrum. Am. J. Pathol. 153 (3), 875–886. 10.1016/S0002-9440(10)65629-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan L., Feng Y., Wan H., Shi G., Niu W. (2014). Clinicopathological and demographical characteristics of non-small cell lung cancer patients with ALK rearrangements: a systematic review and meta-analysis. PLoS One 9 (6), e100866. 10.1371/journal.pone.0100866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan Y., Li W., Nie W., Yao H., Ren Y., Wang M., et al. (2023). Novel dual-target kinase inhibitors of EGFR and ALK were designed, synthesized, and induced cell apoptosis in non-small cell lung cancer. Molecules 28 (5), 2006. 10.3390/molecules28052006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang D. D., Tao R., Wang G., Li Y., Zhang K., Xu C., et al. (2022). Discovery of a novel ALK/ROS1/FAK inhibitor, APG-2449, in preclinical non-small cell lung cancer and ovarian cancer models. BMC Cancer 22 (1), 752. 10.1186/s12885-022-09799-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forde P. M., Rudin C. M. (2012). Crizotinib in the treatment of non-small-cell lung cancer. Expert Opin. Pharmacother. 13 (8), 1195–1201. 10.1517/14656566.2012.688029 [DOI] [PubMed] [Google Scholar]
- Friboulet L., Li N., Katayama R., Lee C. C., Gainor J. F., Crystal A. S., et al. (2014). The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small cell lung cancer. Cancer Discov. 4 (6), 662–673. 10.1158/2159-8290.CD-13-0846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita S., Masago K., Katakami N., Yatabe Y. (2016). Transformation to SCLC after treatment with the ALK inhibitor alectinib. J. Thorac. Oncol. 11 (6), e67–e72. 10.1016/j.jtho.2015.12.105 [DOI] [PubMed] [Google Scholar]
- Gainor J. F., Dardaei L., Yoda S., Friboulet L., Leshchiner I., Katayama R., et al. (2016). Molecular mechanisms of resistance to first- and second-generation ALK inhibitors in ALK-rearranged lung cancer. Cancer Discov. 6 (10), 1118–1133. 10.1158/2159-8290.CD-16-0596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gieszer B., Megyesfalvi Z., Dulai V., Papay J., Kovalszky I., Timar J., et al. (2021). EGFR variant allele frequency predicts EGFR-TKI efficacy in lung adenocarcinoma: a multicenter study. Transl. Lung Cancer Res. 10 (2), 662–674. 10.21037/tlcr-20-814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godbert Y., Henriques de Figueiredo B., Bonichon F., Chibon F., Hostein I., Pérot G., et al. (2015). Remarkable response to crizotinib in woman with anaplastic lymphoma kinase-rearranged anaplastic thyroid carcinoma. J. Clin. Oncol. 33 (20), e84–e87. 10.1200/JCO.2013.49.6596 [DOI] [PubMed] [Google Scholar]
- Guo J., Guo L., Sun L., Wu Z., Ye J., Liu J., et al. (2018). Capture-based ultra-deep sequencing in plasma ctDNA reveals the resistance mechanism of ALK inhibitors in a patient with advanced ALK-positive NSCLC. Cancer Biol. Ther. 19 (5), 359–363. 10.1080/15384047.2018.1433496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallberg B., Palmer R. H. (2016). The role of the ALK receptor in cancer biology. Ann. Oncol. 27, iii4–iii15. iii4-iii15. 10.1093/annonc/mdw301 [DOI] [PubMed] [Google Scholar]
- Hida T., Nokihara H., Kondo M., Kim Y. H., Azuma K., Seto T., et al. (2017). Alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer (J-ALEX): an open-label, randomised phase 3 trial. Lancet 390 (10089), 29–39. 10.1016/S0140-6736(17)30565-2 [DOI] [PubMed] [Google Scholar]
- Hizal M., Bilgin B., Paksoy N., Atcı M. M., Kahraman S., Kılıçkap S., et al. (2023). The percentage of ALK-positive cells and the efficacy of first-line alectinib in advanced non-small cell lung cancer: is it a novel factor for stratification? (Turkish Oncology Group Study). J. Cancer Res. Clin. Oncol. 149 (8), 4141–4148. 10.1007/s00432-022-04252-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn L., Wang Z., Wu G., Poddubskaya E., Mok T., Reck M., et al. (2021). Ensartinib vs crizotinib for patients with anaplastic lymphoma kinase-positive non-small cell lung cancer: a randomized clinical trial. JAMA Oncol. 7 (11), 1617–1625. 10.1001/jamaoncol.2021.3523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoy S. M. (2021). Brigatinib: a review in ALK-inhibitor naïve advanced ALK-positive NSCLC. Drugs 81 (2), 267–275. 10.1007/s40265-020-01449-y [DOI] [PubMed] [Google Scholar]
- Hua G., Zhang X., Zhang M., Wang Q., Chen X., Yu R., et al. (2022). Real-world circulating tumor DNA analysis depicts resistance mechanism and clonal evolution in ALK inhibitor-treated lung adenocarcinoma patients. ESMO Open 7 (1), 100337. 10.1016/j.esmoop.2021.100337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Q., Johnson T. W., Bailey S., Brooun A., Bunker K. D., Burke B. J., et al. (2014). Design of potent and selective inhibitors to overcome clinical anaplastic lymphoma kinase mutations resistant to crizotinib. J. Med. Chem. 57 (4), 1170–1187. 10.1021/jm401805h [DOI] [PubMed] [Google Scholar]
- Huang Y., Hong W., Wei X. (2022). The molecular mechanisms and therapeutic strategies of EMT in tumor progression and metastasis. J. Hematol. Oncol. 15 (1), 129. 10.1186/s13045-022-01347-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z., Xiong Q., Cui Z., Tao H., Zhang S., Wang L., et al. (2021). Efficacy and safety of crizotinib plus bevacizumab in ALK/ROS-1/c-MET positive non-small cell lung cancer: an open-label, single-arm, prospective observational study. Am. J. Transl. Res. 13 (3), 1526–1534. [PMC free article] [PubMed] [Google Scholar]
- Inc N. A. (2022). Study of NVL-655 in patients with advanced NSCLC and other solid tumors harboring ALK rearrangement or activating ALK mutation (ALKOVE-1). Available at: https://classic.clinicaltrials.gov/show/NCT05384626.
- Izumi H., Matsumoto S., Liu J., Tanaka K., Mori S., Hayashi K., et al. (2021). The CLIP1-LTK fusion is an oncogenic driver in non-small-cell lung cancer. Nature 600 (7888), 319–323. 10.1038/s41586-021-04135-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon Y., Park S., Jung H. A., Sun J. M., Lee S. H., Ahn J. S., et al. (2023). First-line alectinib vs. Brigatinib in advanced NSCLC with ALK rearrangement: real-world data. China, Cancer Res Treat. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang J., Deng Q. M., Peng K. C., Li P., Zhu B. T., Wang P., et al. (2022). Clinicopathological features and resistance mechanisms in HIP1-ALK-rearranged lung cancer: a multicenter study. Genes. Chromosom. Cancer 61 (4), 177–186. 10.1002/gcc.23005 [DOI] [PubMed] [Google Scholar]
- Katayama R., Shaw A. T., Khan T. M., Mino-Kenudson M., Solomon B. J., Halmos B., et al. (2012). Mechanisms of acquired crizotinib resistance in ALK-rearranged lung Cancers. Sci. Transl. Med. 4 (120), 120ra17. 10.1126/scitranslmed.3003316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katayama Y., Yamada T., Tanimura K., Tokuda S., Morimoto K., Hirai S., et al. (2023). Adaptive resistance to lorlatinib via EGFR signaling in ALK-rearranged lung cancer. NPJ Precis. Oncol. 7 (1), 12. 10.1038/s41698-023-00350-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khozin S., Blumenthal G. M., Zhang L., Tang S., Brower M., Fox E., et al. (2015). FDA approval: ceritinib for the treatment of metastatic anaplastic lymphoma kinase-positive non-small cell lung cancer. Clin. Cancer Res. 21 (11), 2436–2439. 10.1158/1078-0432.CCR-14-3157 [DOI] [PubMed] [Google Scholar]
- Kim H. R., Kim W. S., Choi Y. J., Choi C. M., Rho J. K., Lee J. C. (2013). Epithelial-mesenchymal transition leads to crizotinib resistance in H2228 lung cancer cells with EML4-ALK translocation. Mol. Oncol. 7 (6), 1093–1102. 10.1016/j.molonc.2013.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbara S., Takeda K., Fukushima H., Inoue T., Okada H., Shibata Y., et al. (2014). A case report of epithelioid inflammatory myofibroblastic sarcoma with RANBP2-ALK fusion gene treated with the ALK inhibitor, crizotinib. Jpn. J. Clin. Oncol. 44 (9), 868–871. 10.1093/jjco/hyu069 [DOI] [PubMed] [Google Scholar]
- Kodama T., Hasegawa M., Takanashi K., Sakurai Y., Kondoh O., Sakamoto H. (2014). Antitumor activity of the selective ALK inhibitor alectinib in models of intracranial metastases. Cancer Chemother. Pharmacol. 74 (5), 1023–1028. 10.1007/s00280-014-2578-6 [DOI] [PubMed] [Google Scholar]
- Kogita A., Togashi Y., Hayashi H., Sogabe S., Terashima M., De Velasco M. A., et al. (2014). Hypoxia induces resistance to ALK inhibitors in the H3122 non-small cell lung cancer cell line with an ALK rearrangement via epithelial-mesenchymal transition. Int. J. Oncol. 45 (4), 1430–1436. 10.3892/ijo.2014.2574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunimasa K., Hirotsu Y., Kukita Y., Ueda Y., Sato Y., Kimura M., et al. (2021). EML4-ALK fusion variant.3 and co-occurrent PIK3CA E542K mutation exhibiting primary resistance to three generations of ALK inhibitors. Cancer Genet. 256-257, 131–135. 10.1016/j.cancergen.2021.05.010 [DOI] [PubMed] [Google Scholar]
- Lu Y., Fan Z., Zhu S. J., Huang X., Zhuang Z., Li Y., et al. (2022). A new ALK inhibitor overcomes resistance to first- and second-generation inhibitors in NSCLC. EMBO Mol. Med. 14 (1), e14296. 10.15252/emmm.202114296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkins E., Blumenthal G. M., Chen H., He K., Agarwal R., Gieser G., et al. (2016). FDA approval: alectinib for the treatment of metastatic, ALK-positive non-small cell lung cancer following crizotinib. Clin. Cancer Res. 22 (21), 5171–5176. 10.1158/1078-0432.CCR-16-1293 [DOI] [PubMed] [Google Scholar]
- Lee C. C., Jia Y., Li N., Sun X., Ng K., Ambing E., et al. (2010). Crystal structure of the ALK (anaplastic lymphoma kinase) catalytic domain. Biochem. J. 430 (3), 425–437. 10.1042/BJ20100609 [DOI] [PubMed] [Google Scholar]
- Lemmon M. A., Schlessinger J. (2010). Cell signaling by receptor tyrosine kinases. Cell. 141 (7), 1117–1134. 10.1016/j.cell.2010.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J. J., Chin E., Yeap B. Y., Ferris L. A., Kamesan V., Lennes I. T., et al. (2019). Increased hepatotoxicity associated with sequential immune checkpoint inhibitor and crizotinib therapy in patients with non-small cell lung cancer. J. Thorac. Oncol. 14 (1), 135–140. 10.1016/j.jtho.2018.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J. J., Muzikansky A., Kennedy E., Kuberski H., Stober L. L., Wanat A. C., et al. (2022). Safety and activity of alectinib plus bevacizumab in patients with advanced ALK-rearranged non-small-cell lung cancer: a phase I/II study. ESMO Open 7 (1), 100342. 10.1016/j.esmoop.2021.100342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu P., Zhao L., Pol J., Levesque S., Petrazzuolo A., Pfirschke C., et al. (2019). Crizotinib-induced immunogenic cell death in non-small cell lung cancer. Nat. Commun. 10 (1), 1486. 10.1038/s41467-019-09415-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lococo F., Cancellieri A., Chiappetta M., Leonetti A., Cardillo G., Zanelli F., et al. (2023). Salvage surgery after first-line alectinib for locally-advanced/metastatic ALK-rearranged NSCLC: pathological response and perioperative results. Clin. Lung Cancer 24, 467–473. 10.1016/j.cllc.2023.03.008 [DOI] [PubMed] [Google Scholar]
- Mai S., Wang Y., Wang X., Yang W., Gao H., Xu Z., et al. (2022). Neoadjuvant ceritinib treatment in ALK-rearranged locally advanced adenosquamous carcinoma: a case report. Thorac. Cancer 13 (15), 2275–2278. 10.1111/1759-7714.14558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majeed U., Li S., Seegobin K., Nassar A., Manochakian R., Zhao Y., et al. (2023). First report of management of sequential small cell transformation and ALK I1171T mutation as resistance mechanisms in a patient with ALK-EML4 fused non-small cell lung adenocarcinoma with a novel combination of temozolomide and lorlatinib: a case report. JTO Clin. Res. Rep. 4 (7), 100536. 10.1016/j.jtocrr.2023.100536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastini C., Campisi M., Patrucco E., Mura G., Ferreira A., Costa C., et al. (2023). Targeting CCR7-PI3Kγ overcomes resistance to tyrosine kinase inhibitors in ALK-rearranged lymphoma. Sci. Transl. Med. 15 (702), eabo3826. 10.1126/scitranslmed.abo3826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuura Y., Mun M., Shintani Y., Okami J., Ito H., Ohtsuka T., et al. (2023). Features of anaplastic lymphoma kinase rearrangement in early-stage lung cancer: analysis of a nationwide Japanese database. J. Surg. Oncol. 128, 916–924. 10.1002/jso.27384 [DOI] [PubMed] [Google Scholar]
- Michaux L., Perrier A., Mehlman C., Alshehhi H., Dubois A., Lacave R., et al. (2023). Therapeutic strategies to overcome EGFR mutations as acquired resistance mechanism in ALK-rearranged non-small-cell lung cancer: case Reports. Front. Oncol. 13, 1182558. 10.3389/fonc.2023.1182558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuta H., Okada K., Araki M., Adachi J., Takemoto A., Kutkowska J., et al. (2021). Gilteritinib overcomes lorlatinib resistance in ALK-rearranged cancer. Nat. Commun. 12 (1), 1261. 10.1038/s41467-021-21396-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris S. W., Kirstein M. N., Valentine M. B., Dittmer K. G., Shapiro D. N., Saltman D. L., et al. (1994). Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin's lymphoma. Science 263 (5151), 1281–1284. 10.1126/science.8122112 [DOI] [PubMed] [Google Scholar]
- Murray B. W., Zhai D., Deng W., Zhang X., Ung J., Nguyen V., et al. (2021). TPX-0131, a potent CNS-penetrant, next-generation inhibitor of wild-type ALK and ALK-resistant mutations. Mol. Cancer Ther. 20 (9), 1499–1507. 10.1158/1535-7163.MCT-21-0221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa K., Hida T., Nokihara H., Morise M., Azuma K., Kim Y. H., et al. (2020). Final progression-free survival results from the J-ALEX study of alectinib versus crizotinib in ALK-positive non-small-cell lung cancer. Lung Cancer 139, 195–199. 10.1016/j.lungcan.2019.11.025 [DOI] [PubMed] [Google Scholar]
- Nakasuka T., Ichihara E., Makimoto G., Maeda Y., Kiura K. (2019). Primary resistance to alectinib was lost after bevacizumab combined chemotherapy in ALK-rearranged lung adenocarcinoma. J. Thorac. Oncol. 14 (8), e168–e169. 10.1016/j.jtho.2019.03.009 [DOI] [PubMed] [Google Scholar]
- Novello S., Mazières J., Oh I. J., de Castro J., Migliorino M. R., Helland Å., et al. (2018). Alectinib versus chemotherapy in crizotinib-pretreated anaplastic lymphoma kinase (ALK)-positive non-small-cell lung cancer: results from the phase III ALUR study. Ann. Oncol. 29 (6), 1409–1416. 10.1093/annonc/mdy121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogata M., Hatachi Y., Ogata T., Satake H., Imai Y., Yasui H. (2019). Effectiveness of crizotinib for inflammatory myofibroblastic tumor with ALK mutation. Intern Med. 58 (7), 1029–1032. 10.2169/internalmedicine.1640-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okada K., Araki M., Sakashita T., Ma B., Kanada R., Yanagitani N., et al. (2019). Prediction of ALK mutations mediating ALK-TKIs resistance and drug re-purposing to overcome the resistance. EBioMedicine 41, 105–119. 10.1016/j.ebiom.2019.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ota K., Azuma K., Kawahara A., Hattori S., Iwama E., Tanizaki J., et al. (2015). Induction of PD-L1 expression by the EML4-ALK oncoprotein and downstream signaling pathways in non-small cell lung cancer. Clin. Cancer Res. 21 (17), 4014–4021. 10.1158/1078-0432.CCR-15-0016 [DOI] [PubMed] [Google Scholar]
- Ou S. H., Ahn J. S., De Petris L., Govindan R., Yang J. C., Hughes B., et al. (2016). Alectinib in crizotinib-refractory ALK-rearranged non-small-cell lung cancer: a phase II global study. J. Clin. Oncol. 34 (7), 661–668. 10.1200/jco.2015.63.9443 [DOI] [PubMed] [Google Scholar]
- Ou S. I., Nagasaka M. (2020). A catalog of 5' fusion partners in ROS1-positive NSCLC circa 2020. JTO Clin. Res. Rep. 1 (3), 100048. 10.1016/j.jtocrr.2020.100048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ou S. I., Nishio M., Ahn M. J., Mok T., Barlesi F., Zhou C., et al. (2022). Efficacy of brigatinib in patients with advanced ALK-positive NSCLC who progressed on alectinib or ceritinib: ALK in lung cancer trial of brigAtinib-2 (ALTA-2). J. Thorac. Oncol. 17 (12), 1404–1414. 10.1016/j.jtho.2022.08.018 [DOI] [PubMed] [Google Scholar]
- Pan Y., Liu X., Zhang W., Wang W., Wang H., Luo L., et al. (2023). Association of PD-L1 expression with efficacy of alectinib in advanced NSCLC patients with ALK fusion. Lung Cancer 181, 107233. 10.1016/j.lungcan.2023.107233 [DOI] [PubMed] [Google Scholar]
- Patel S. P., Pakkala S., Pennell N. A., Reckamp K. L., Lanzalone S., Polli A., et al. (2020). Phase ib study of crizotinib plus pembrolizumab in patients with previously untreated advanced non-small cell lung cancer with ALK translocation. Oncologist 25 (7), 562–e1012. 10.1634/theoncologist.2020-0034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelish H. E., Tangpeerachaikul A., Kohl N. E., Porter J. R., Shair M. D., Horan J. C. (2021). Abstract 1468: NUV-655 (NVL-655) is a selective, brain-penetrant ALK inhibitor with antitumor activity against the lorlatinib-resistant G1202R/L1196M compound mutation. Cancer Res. 81, 1468. 10.1158/1538-7445.am2021-1468 [DOI] [Google Scholar]
- Petrazzuolo A., Perez-Lanzon M., Martins I., Liu P., Kepp O., Minard-Colin V., et al. (2021). Pharmacological inhibitors of anaplastic lymphoma kinase (ALK) induce immunogenic cell death through on-target effects. Cell. Death Dis. 12 (8), 713. 10.1038/s41419-021-03997-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu B., Guo W., Zhang F., Lv F., Ji Y., Peng Y., et al. (2021). Dynamic recurrence risk and adjuvant chemotherapy benefit prediction by ctDNA in resected NSCLC. Nat. Commun. 12 (1), 6770. 10.1038/s41467-021-27022-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao W., Liu Y., Li Y., Guo L., Qiu T., Dong L., et al. (2023). Potential unreliability of ALK variant allele frequency in the efficacy prediction of targeted therapy in NSCLC. Front. Med. 17, 493–502. 10.1007/s11684-022-0946-x [DOI] [PubMed] [Google Scholar]
- Rosswog C., Fassunke J., Ernst A., Schömig-Markiefka B., Merkelbach-Bruse S., Bartenhagen C., et al. (2023). Genomic ALK alterations in primary and relapsed neuroblastoma. Br. J. Cancer 128 (8), 1559–1571. 10.1038/s41416-023-02208-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabir S. R., Yeoh S., Jackson G., Bayliss R. (2017). EML4-ALK variants: biological and molecular properties, and the implications for patients. Cancers (Basel) 9 (9), 118. 10.3390/cancers9090118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu A., Prabhash K., Noronha V., Joshi A., Desai S. (2013). Crizotinib: a comprehensive review. South Asian J. Cancer 2 (2), 91–97. 10.4103/2278-330X.110506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakakibara-Konishi J., Kitai H., Ikezawa Y., Hatanaka Y., Sasaki T., Yoshida R., et al. (2019). Response to crizotinib Re-administration after progression on lorlatinib in a patient with ALK-rearranged non-small-cell lung cancer. Clin. Lung Cancer 20 (5), e555–e559. 10.1016/j.cllc.2019.06.021 [DOI] [PubMed] [Google Scholar]
- Sakamoto H., Tsukaguchi T., Hiroshima S., Kodama T., Kobayashi T., Fukami T. A., et al. (2011). CH5424802, a selective ALK inhibitor capable of blocking the resistant gatekeeper mutant. Cancer Cell. 19 (5), 679–690. 10.1016/j.ccr.2011.04.004 [DOI] [PubMed] [Google Scholar]
- Sato-Nakai M., Kawashima K., Nakagawa T., Tachibana Y., Yoshida M., Takanashi K., et al. (2017). Metabolites of alectinib in human: their identification and pharmacological activity. Heliyon 3 (7), e00354. 10.1016/j.heliyon.2017.e00354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäkel L., Mirza S., Winzer R., Lopez V., Idris R., Al-Hroub H., et al. (2022). Protein kinase inhibitor ceritinib blocks ectonucleotidase CD39 - a promising target for cancer immunotherapy. J. Immunother. Cancer 10 (8), e004660. 10.1136/jitc-2022-004660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schöffski P., Kubickova M., Wozniak A., Blay J. Y., Strauss S. J., Stacchiotti S., et al. (2021). Long-term efficacy update of crizotinib in patients with advanced, inoperable inflammatory myofibroblastic tumour from EORTC trial 90101 CREATE. Eur. J. Cancer 156, 12–23. 10.1016/j.ejca.2021.07.016 [DOI] [PubMed] [Google Scholar]
- Scott J. A., Lennerz J., Johnson M. L., Gordan L. N., Dumanois R. H., Quagliata L., et al. (2023). Compromised outcomes in stage IV non-small-cell lung cancer with actionable mutations initially treated without tyrosine kinase inhibitors: a retrospective analysis of real-world data. JCO Oncol. Pract., OP2200611. 10.1200/OP.22.00611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sehnal D., Bittrich S., Deshpande M., Svobodová R., Berka K., Bazgier V., et al. (2021). Mol* Viewer: modern web app for 3D visualization and analysis of large biomolecular structures. Nucleic Acids Res. 49 (W1), W431–W437. 10.1093/nar/gkab314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw A. T., Bauer T. M., de Marinis F., Felip E., Goto Y., Liu G., et al. (2020). First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N. Engl. J. Med. 383 (21), 2018–2029. 10.1056/NEJMoa2027187 [DOI] [PubMed] [Google Scholar]
- Shaw A. T., Friboulet L., Leshchiner I., Gainor J. F., Bergqvist S., Brooun A., et al. (2016). Resensitization to crizotinib by the lorlatinib ALK resistance mutation L1198F. N. Engl. J. Med. 374 (1), 54–61. 10.1056/NEJMoa1508887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw A. T., Kim D. W., Mehra R., Tan D. S., Felip E., Chow L. Q., et al. (2014). Ceritinib in ALK-rearranged non-small-cell lung cancer. N. Engl. J. Med. 370 (13), 1189–1197. 10.1056/NEJMoa1311107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw A. T., Kim D. W., Nakagawa K., Seto T., Crinó L., Ahn M. J., et al. (2013). Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N. Engl. J. Med. 368 (25), 2385–2394. 10.1056/NEJMoa1214886 [DOI] [PubMed] [Google Scholar]
- Shaw A. T., Kim T. M., Crinò L., Gridelli C., Kiura K., Liu G., et al. (2017). Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 18 (7), 874–886. 10.1016/S1470-2045(17)30339-X [DOI] [PubMed] [Google Scholar]
- Shaw A. T., Solomon B. J., Besse B., Bauer T. M., Lin C. C., Soo R. A., et al. (2019). ALK resistance mutations and efficacy of lorlatinib in advanced anaplastic lymphoma kinase-positive non-small-cell lung cancer. J. Clin. Oncol. 37 (16), 1370–1379. 10.1200/JCO.18.02236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw A. T., Yeap B. Y., Mino-Kenudson M., Digumarthy S. R., Costa D. B., Heist R. S., et al. (2009). Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J. Clin. Oncol. 27 (26), 4247–4253. 10.1200/JCO.2009.22.6993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y., Chen J., Zhang H., Zhang Z., Zhang Y., Wang Z., et al. (2023). Efficacy and safety of iruplinalkib (WX-0593) in ALK-positive crizotinib-resistant advanced non-small cell lung cancer patients: a single-arm, multicenter phase II study (INTELLECT). BMC Med. 21 (1), 72. 10.1186/s12916-023-02738-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y., Fang J., Hao X., Zhang S., Liu Y., Wang L., et al. (2022). Safety and activity of WX-0593 (Iruplinalkib) in patients with ALK- or ROS1-rearranged advanced non-small cell lung cancer: a phase 1 dose-escalation and dose-expansion trial. Signal Transduct. Target Ther. 7 (1), 25. 10.1038/s41392-021-00841-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiba-Ishii A., Johnson T. W., Dagogo-Jack I., Mino-Kenudson M., Johnson T. R., Wei P., et al. (2022). Analysis of lorlatinib analogs reveals a roadmap for targeting diverse compound resistance mutations in ALK-positive lung cancer. Nat. Cancer 3 (6), 710–722. 10.1038/s43018-022-00399-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiraishi T., Yamasaki K., Kidogawa M., Shingu T., Ujimiya F., Jotatsu T., et al. (2023). Successful treatment with crizotinib to overcome drug resistance possibly due to <i>Mesenchymal-epithelial transition</i> amplification in a lung cancer patient with the <i>Echinoderm microtubule-associated protein-like 4-anaplastic lymphoma kinase</i> fusion gene. Intern Med., 1164-22. 10.2169/internalmedicine.1164-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon B. J., Bauer T. M., Ignatius Ou S. H., Liu G., Hayashi H., Bearz A., et al. (2022). Post hoc analysis of lorlatinib intracranial efficacy and safety in patients with ALK-positive advanced non-small-cell lung cancer from the phase III CROWN study. J. Clin. Oncol. 40 (31), 3593–3602. 10.1200/JCO.21.02278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon B. J., Bauer T. M., Mok T. S. K., Liu G., Mazieres J., de Marinis F., et al. (2023). Efficacy and safety of first-line lorlatinib versus crizotinib in patients with advanced, ALK-positive non-small-cell lung cancer: updated analysis of data from the phase 3, randomised, open-label CROWN study. Lancet Respir. Med. 11 (4), 354–366. 10.1016/S2213-2600(22)00437-4 [DOI] [PubMed] [Google Scholar]
- Solomon B. J., Mok T., Kim D. W., Wu Y. L., Nakagawa K., Mekhail T., et al. (2014). First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N. Engl. J. Med. 371 (23), 2167–2177. 10.1056/NEJMoa1408440 [DOI] [PubMed] [Google Scholar]
- Soria J. C., Tan D. S. W., Chiari R., Wu Y. L., Paz-Ares L., Wolf J., et al. (2017). First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet 389 (10072), 917–929. 10.1016/S0140-6736(17)30123-X [DOI] [PubMed] [Google Scholar]
- Spigel D. R., Reynolds C., Waterhouse D., Garon E. B., Chandler J., Babu S., et al. (2018). Phase 1/2 study of the safety and tolerability of nivolumab plus crizotinib for the first-line treatment of anaplastic lymphoma kinase translocation - positive advanced non-small cell lung cancer (CheckMate 370). J. Thorac. Oncol. 13 (5), 682–688. 10.1016/j.jtho.2018.02.022 [DOI] [PubMed] [Google Scholar]
- Syed Y. Y. (2019). Lorlatinib: first global approval. Drugs 79 (1), 93–98. 10.1007/s40265-018-1041-0 [DOI] [PubMed] [Google Scholar]
- Takahashi K., Seto Y., Okada K., Uematsu S., Uchibori K., Tsukahara M., et al. (2020). Overcoming resistance by ALK compound mutation (I1171S + G1269A) after sequential treatment of multiple ALK inhibitors in non-small cell lung cancer. Thorac. Cancer 11 (3), 581–587. 10.1111/1759-7714.13299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talwelkar S. S., Mäyränpää M. I., Schüler J., Linnavirta N., Hemmes A., Adinolfi S., et al. (2023). PI3Kβ inhibition enhances ALK-inhibitor sensitivity in ALK-rearranged lung cancer. Mol. Oncol. 17 (5), 747–764. 10.1002/1878-0261.13342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tani T., Yasuda H., Hamamoto J., Kuroda A., Arai D., Ishioka K., et al. (2016). Activation of EGFR bypass signaling by TGFα overexpression induces acquired resistance to alectinib in ALK-translocated lung cancer cells. Mol. Cancer Ther. 15 (1), 162–171. 10.1158/1535-7163.MCT-15-0084 [DOI] [PubMed] [Google Scholar]
- Taniguchi H., Akagi K., Dotsu Y., Yamada T., Ono S., Imamura E., et al. (2023). Pan-HER inhibitors overcome lorlatinib resistance caused by NRG1/HER3 activation in ALK-rearranged lung cancer. Cancer Sci. 114 (1), 164–173. 10.1111/cas.15579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanizaki J., Okamoto I., Okabe T., Sakai K., Tanaka K., Hayashi H., et al. (2012). Activation of HER family signaling as a mechanism of acquired resistance to ALK inhibitors in EML4-ALK-positive non-small cell lung cancer. Clin. Cancer Res. 18 (22), 6219–6226. 10.1158/1078-0432.CCR-12-0392 [DOI] [PubMed] [Google Scholar]
- Wang M., Slatter S., Sussell J., Lin C. W., Ogale S., Datta D., et al. (2023). ALK inhibitor treatment patterns and outcomes in real-world patients with ALK-positive non-small-cell lung cancer: a retrospective cohort study. Target Oncol. 18 (4), 571–583. 10.1007/s11523-023-00973-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Hu Y., Zou X., Wang P., Yue H., Guo M., et al. (2022). Discovery of 2,4-diarylaminopyrimidine derivatives bearing dithiocarbamate moiety as novel ALK inhibitors. Bioorg Med. Chem. 66, 116794. 10.1016/j.bmc.2022.116794 [DOI] [PubMed] [Google Scholar]
- Watanabe H., Ichihara E., Kayatani H., Makimoto G., Ninomiya K., Nishii K., et al. (2021). VEGFR2 blockade augments the effects of tyrosine kinase inhibitors by inhibiting angiogenesis and oncogenic signaling in oncogene-driven non-small-cell lung cancers. Cancer Sci. 112 (5), 1853–1864. 10.1111/cas.14801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe S., Sakai K., Matsumoto N., Koshio J., Ishida A., Abe T., et al. (2022). Phase II trial of the combination of alectinib with bevacizumab in alectinib refractory ALK-positive nonsquamous non-small-cell lung cancer (NLCTG1501). Cancers (Basel). 15 (1), 204. 10.3390/cancers15010204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf J., Helland Å., Oh I. J., Migliorino M. R., Dziadziuszko R., Wrona A., et al. (2022). Final efficacy and safety data, and exploratory molecular profiling from the phase III ALUR study of alectinib versus chemotherapy in crizotinib-pretreated ALK-positive non-small-cell lung cancer. ESMO Open 7 (1), 100333. 10.1016/j.esmoop.2021.100333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu W., Haderk F., Bivona T. G. (2017). Non-canonical thinking for targeting ALK-fusion onco-proteins in lung cancer. Cancers (Basel) 9 (12), 164. 10.3390/cancers9120164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia G., Huang J., Ni J., Song M., Zhang J., Hofman P., et al. (2023). Transformation of ALK-positive NSCLC to SCLC after alectinib resistance and response to combined atezolizumab: a case report. Transl. Lung Cancer Res. 12 (3), 637–646. 10.21037/tlcr-23-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Zheng Q., Wang X., Zhao S., Huang W., Jia L., et al. (2023). Iruplinalkib (WX-0593), a novel ALK/ROS1 inhibitor, overcomes crizotinib resistance in preclinical models for non-small cell lung cancer. Investig. New Drugs 41 (2), 254–266. 10.1007/s10637-023-01350-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Zhou J., Feng J., Zhuang W., Chen J., Zhao J., et al. (2020). Efficacy, safety, and biomarker analysis of ensartinib in crizotinib-resistant, ALK-positive non-small-cell lung cancer: a multicentre, phase 2 trial. Lancet Respir. Med. 8 (1), 45–53. 10.1016/S2213-2600(19)30252-8 [DOI] [PubMed] [Google Scholar]
- Yoshimura Y., Kurasawa M., Yorozu K., Puig O., Bordogna W., Harada N. (2016). Antitumor activity of alectinib, a selective ALK inhibitor, in an ALK-positive NSCLC cell line harboring G1269A mutation: efficacy of alectinib against ALK G1269A mutated cells. Cancer Chemother. Pharmacol. 77 (3), 623–628. 10.1007/s00280-016-2977-y [DOI] [PubMed] [Google Scholar]
- Zhang Q., Sun T., Kang P., Qian K., Deng B., Zhou J., et al. (2016). Combined analysis of rearrangement of ALK, ROS1, somatic mutation of EGFR, KRAS, BRAF, PIK3CA, and mRNA expression of ERCC1, TYMS, RRM1, TUBB3, EGFR in patients with non-small cell lung cancer and their clinical significance. Cancer Chemother. Pharmacol. 77 (3), 583–593. 10.1007/s00280-016-2969-y [DOI] [PubMed] [Google Scholar]
- Zhang S. S., Nagasaka M., Zhu V. W., Ou S. I. (2021). Going beneath the tip of the iceberg. Identifying and understanding EML4-ALK variants and TP53 mutations to optimize treatment of ALK fusion positive (ALK+) NSCLC. Lung Cancer 158, 126–136. 10.1016/j.lungcan.2021.06.012 [DOI] [PubMed] [Google Scholar]
- Zhou C., Kim S. W., Reungwetwattana T., Zhou J., Zhang Y., He J., et al. (2019). Alectinib versus crizotinib in untreated Asian patients with anaplastic lymphoma kinase-positive non-small-cell lung cancer (ALESIA): a randomised phase 3 study. Lancet Respir. Med. 7 (5), 437–446. 10.1016/S2213-2600(19)30053-0 [DOI] [PubMed] [Google Scholar]
- Zhou Y., Song L., Xu Q., Zeng L., Jiang W., Yang N., et al. (2022). Investigation on the survival implications of PD-L1 expression status in ALK- rearranged advanced non-small cell lung cancer treated with first-line crizotinib. Lung Cancer 167, 58–64. 10.1016/j.lungcan.2022.04.002 [DOI] [PubMed] [Google Scholar]
- Zou Z., Xing P., Hao X., Wang Y., Song X., Shan L., et al. (2022). Intracranial efficacy of alectinib in ALK-positive NSCLC patients with CNS metastases-a multicenter retrospective study. BMC Med. 20 (1), 12. 10.1186/s12916-021-02207-x [DOI] [PMC free article] [PubMed] [Google Scholar]