TABLE OF CONTENTS
ABBREVIATIONS AND ACRONYMS 163
1. METHODS SUMMARY 163
2. INTRODUCTION 164
3. TRAINING, EDUCATION AND SERVICE DELIVERY 164
3.1 Description of the evidence 164
4. HEART–LUNG MACHINE HARDWARE 166
4.1 Console with pumps and holders 166
4.1.1 Description of the evidence 166
4.2 Monitoring 166
4.2.1 Description of the evidence 166
4.3 Safety features 167
4.3.1 Description of the evidence 167
4.4 Oxygen and air, carbon dioxide and volatile anaesthetics supply 167
4.4.1 Description of the evidence 167
4.5 Heater-cooler unit 168
4.5.1 Description of the evidence 168
4.6 Patient data management systems and quality improvement 168
4.6.1 Description of the evidence 168
5. CARDIOPULMONARY BYPASS—THE DISPOSABLES 169
5.1 Cannulas 169
5.1.1 Arterial cannulation 169
5.1.2 Venous cannulation 170
5.2 Venting and suction devices 170
5.2.1 Description of the evidence 170
5.3 Reservoirs 170
5.3.1 Description of the evidence 170
5.4 Oxygenators 171
5.4.1 Description of the evidence 171
5.5 Pumps 171
5.5.1 Description of the evidence 172
5.6 Filters 172
5.6.1 Description of the evidence 172
5.7 Material and surface treatments 172
5.7.1 Description of the evidence 173
6. PREPARATION FOR CARDIOPULMONARY BYPASS 173
6.1 Checklist 173
6.1.1 Description of the evidence 173
6.2 Preoperative assessment 174
6.2.1 Description of the evidence 174
7. PROCEDURES DURING CARDIOPULMONARY BYPASS 174
7.1 Type of circuit 174
7.1.1 Description of the evidence 174
7.2 Carbon dioxide flush 175
7.2.1 Description of the evidence 175
7.3 Priming volume and autologous priming 175
7.3.1 Description of the evidence 176
7.4 Anticoagulation management 176
7.4.1 Interventions 176
7.4.2 Description of the evidence 176
7.4.2.1 Heparin dosage 176
7.4.2.2 Individualized heparin management 177
7.4.2.3 Measures to prevent heparin rebound 177
7.4.2.4 Protamine management 177
7.4.2.5 Interventions 177
7.4.2.6 Prevention of protamine overdosing 177
7.4.2.7 Alternative anticoagulation 177
7.5 Acid-base homeostasis and electrolyte management 178
7.5.1 Description of the evidence 178
7.5.2 Magnesium 179
7.6 Control of mean arterial blood pressure 179
7.6.1 Description of the evidence 179
7.7 Pump flow management 180
7.7.1 Description of the evidence 180
7.8 Pulsatile and continuous flow 181
7.8.1 Description of the evidence 181
7.9 Goal-directed haemodynamic therapy 181
7.9.1 Description of the evidence 181
7.10 Assisted drainage 182
7.10.1 Description of the evidence 182
7.11 Strategies for transfusion of blood products 182
7.11.1 Description of the evidence 182
7.11.1.1 Packed red blood cell transfusions 182
7.11.1.2 Fresh frozen plasma transfusions 183
7.12 Anaesthesia and pharmacological treatment during cardiopulmonary bypass 183
7.12.1 Volatile anaesthetics 183
7.12.2 Intravenous anaesthetics and opioids during cardiopulmonary bypass 184
7.12.3 Neuromuscular blocking agents 184
7.12.4 Corticosteroids 184
7.12.5 Glycaemic control 184
7.13 Cardioplegia 185
7.13.1 Description of the evidence 185
7.14 Lung protection 186
7.14.1 Description of the evidence 186
7.14.1.1 Cardiopulmonary modifications 186
7.14.1.2 Leucocyte filtration 186
7.14.1.3 Modified ultrafiltration 187
7.14.1.4 Pulmonary artery perfusion 187
7.14.1.5 Minimally invasive extracorporeal circulation 187
7.14.1.6 Continuous positive airway pressure and ventilation during cardiopulmonary bypass 187
7.14.2 Pharmacological interventions 187
7.14.2.1 Hyperoxia 187
7.14.2.2 High-dose dexamethasone 187
7.15 Non-invasive cerebral monitoring 188
7.15.1 Description of the evidence 188
7.15.1.1 Near-infrared spectroscopy 188
7.15.1.2 Monitoring of depth of anaesthesia 188
7.15.1.3 Transcranial Doppler 188
7.16 Management of shed blood 188
7.16.1 Description of the evidence 188
7.17 Minimally invasive surgery 189
7.17.1 Description of the evidence 189
7.18 Emergency institution and reinstitution of cardiopulmonary bypass 189
7.18.1 Description of the evidence 189
8. SEPARATION FROM CARDIOPULMONARY BYPASS 190
8.1 Reperfusion time 190
8.2 Weaning checklist 190
8.2.1 Description of the evidence 190
8.3 Haemodynamic monitoring 191
8.3.1 Description of the evidence 191
8.3.1.1 Pulmonary artery balloon catheter 191
8.3.1.2 Minimally invasive haemodynamic monitors using pulse contour analysis 191
8.3.1.3 Transoesophageal echocardiography 191
8.4 Positive inotropes 191
8.4.1 Description of the evidence 192
8.5 Haemostasis management 192
8.6 Mechanical circulatory support 192
8.7 Residual blood management 192
8.7.1 Description of the evidence 192
9. FINAL REMARKS 193
REFERENCES 194
ABBREVIATIONS AND ACRONYMS
- AAGA
Accidental awareness during general anaesthesia
- ACT
Activated clotting time
- AF
Atrial fibrillation
- AKI
Acute kidney injury
- ALF
Arterial line filter
- BIS
Bispectral index
- BSA
Body surface area
- CABG
Coronary artery bypass grafting
- CI
Confidence interval
- CO2
Carbon dioxide
- CPB
Cardiopulmonary bypass
- DO2
Oxygen delivery
- EACTA
European Association of Cardiothoracic Anaesthesiology
- EACTS
European Association for Cardio-Thoracic Surgery
- EAS
Epiaortic scanning
- EBCP
European Board of Cardiovascular Perfusion
- ECLS
Extracorporeal life support
- EEG
Electroencephalography
- FFP
Fresh frozen plasma
- GDT
Goal-directed haemodynamic therapy
- GME
Gaseous microemboli
- Hb
Haemoglobin
- HCT
Haematocrit
- HCU
Heater-cooler unit
- HES
Hydroxyethyl starch
- ICU
Intensive care unit
- LCOS
Low cardiac output syndrome
- LD
Leucodepletion
- MAP
Mean arterial pressure
- MI
Myocardial infarction
- MiECC
Minimally invasive extracorporeal circulation
- MUF
Modified ultrafiltration
- NIRS
Near-infrared spectroscopy
- OR
Odds ratio
- O2ER
Oxygen extraction ratio
- PAC
Pulmonary artery catheter
- PRBCs
Packed red blood cells
- QI
Quality improvement
- RCT
Randomized controlled trial
- RD
Risk difference
- RR
Risk ratio
- SMB
Shed mediastinal blood
- SvO2
Mixed venous oxygen saturation
- TOE
Transoesophageal echocardiography
- VAVD
Vacuum-assisted venous drainage
- VO2
Oxygen consumption
- WMD
Weighted mean difference
1. METHODS SUMMARY
To improve the outcome of adult patients undergoing heart surgery, a task force whose members were selected for their respective expertise in the area by the European Association for Cardio-Thoracic Surgery (EACTS) Council, the Board of Directors of the European Association of Cardiothoracic Anaesthesiology (EACTA) and the Quality and Outcomes Committee of the European Board of Cardiovascular Perfusion (EBCP) was given the remit of jointly developing evidence-based guidelines for the practice of cardiopulmonary bypass (CPB) (complete methodological aspects are provided in Supplementary Material, Appendix A). After the scope of the guidelines had been agreed upon by the task force members, a preliminary review of the literature was performed. The task force members established the scope and the table of contents, and topics were allocated to the writing group during a face-to-face meeting. A systematic review of the published evidence was performed based on the standardized Population, Intervention, Comparison, Outcome and Time questions. The systematic literature search was restricted to the years 2000–2019 to focus on contemporary evidence. However, essential references from publications prior to 2000 were included in some instances. The guidelines focused only on adult-acquired cardiac surgery and did not include studies in languages other than English. After methodological quality was assessed across randomized control trials (RCTs), meta-analyses and observational studies, the guidelines were developed based on the synthesis of the best available scientific evidence and medical knowledge, following the methodology manual for EACTS clinical guidelines [1].
All chapters were written through a close collaboration between the EACTS, the EACTA and the EBCP task force members. The experts on the writing panels were asked to complete declarations of interest, notify the EACTS, EACTA and EBCP chairpersons if there were any changes and write chapters only if they did not have any disclosures related to the specific topic. The agreement on the finalized document was reached through conference calls and face-to-face meetings, without excluding members with a conflict of interest. Each specific recommendation was developed after careful consideration of the scientific and medical knowledge and the evidence available at the time of their writing, according to the standardized rules of the EACTS [1]. The scientific evidence was critically appraised for quality with the assistance of a clinical epidemiologist. Furthermore, the hierarchy of evidence according to the study design and the internal hierarchy based on the study quality were used to formulate levels and grades of recommendations. In the absence of published evidence, expert consensus recommendations were made to cover specific issues that are essential to daily practice. The level of evidence and the strength of the recommendations of particular management strategies were weighted and graded according to predefined scales, as outlined in Tables 1 and 2.
Table 1:
Levels of evidence

|
Table 2:
Classes of recommendations
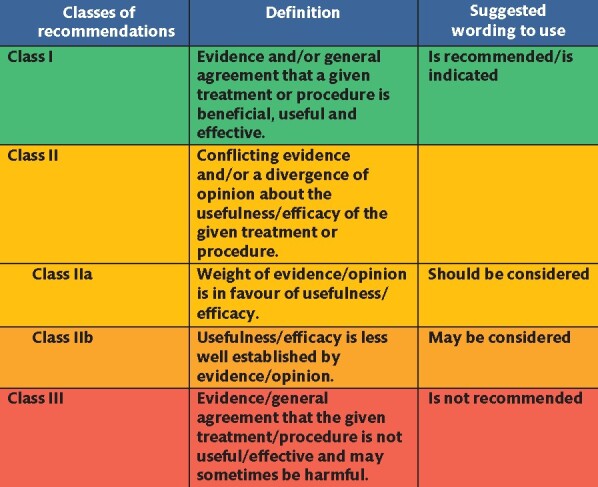
|
In summary, this is the first European publication presenting guidelines for the conduct of CPB during adult cardiac surgery. Due to the lack of scientific evidence for some topics in this field, many recommendations were based on expert consensus, and it is therefore inevitable to call for more thorough, well-thought-out and well-conducted scientific research in many aspects of CPB.
2. INTRODUCTION
The invention of CPB revolutionized cardiac surgery. This vital tool has been continuously refined over the years. Today, achieving excellent results depends on a team approach and the expertise of dedicated perfusionists. Apart from learning the skills necessary to conduct CPB, perfusionists also learn about the science behind modern CPB. Therefore, the present document particularly aims at summarizing the scientific basis for the various aspects of the CPB technique. In addition to previous guidelines and statements, which have given excellent advice on how modern CPB should be performed, these guidelines contain specific recommendations reflecting a European expert consensus. Furthermore, the document contains a chapter dedicated to the training, education and service delivery from the European perspective.
Good quality research has been conducted in several areas of perfusion, such as the use of minimized circuits. However, we found a lack of scientific investigations and clinical trials in many other fields. These CPB guidelines point out the areas where further research is required, with the hope of stimulating future investigations. These guidelines are the result of a collaborative effort by the EBCP, the EACTA and the EACTS, aiming to document a broad consensus of all parties involved in CPB. At the same time, these CPB guidelines are the first evidence-based European document that offers a comprehensive overview of all the issues that are related to modern CPB practice.
Some specific topics, such as patient blood management, have been covered by recent international guidelines. Therefore, the evidence is in part summarized in these guidelines and readers are referred to the respective guidelines [2] because the task force has not identified a need for any major update related to CPB. This approach is also true for hypothermia and temperature management during CPB [3]. The topic of deep hypothermic circulatory arrest is multifactorial and complex and will be covered in a separate document. Paediatric aspects of CPB could not be included in this document due to the given restrictions in its length. When covering broad topics, such as cardioplegia and minimally invasive surgery, the recommendations in these guidelines are focused on perfusion aspects.
3. TRAINING, EDUCATION AND SERVICE DELIVERY
The operational management of CPB is the responsibility of the clinical perfusionist. To ensure safe and effective practice, perfusionists need to be adequately trained with appropriate knowledge, skills and expertise.
Clinical perfusionists are members of the multidisciplinary operative team working in collaboration with surgeons, anaesthetists and operating room personnel. Perfusion departments need to be adequately staffed and resourced to deliver elective and emergency patient care. The effectiveness of care should be established by monitoring patient outcomes in addition to regular reporting, performing analyses and learning from adverse incidents.
3.1 Description of the evidence
Minimum standards for perfusion education, training, accreditation and service delivery have been established for many individual countries by their respective national perfusion organization, board or college. There are notable variations between countries with regard to the organization and oversight of perfusion. International organizations, such as the EBCP, recommend standardizing the quality of education and training [4], which has been implemented in a number of European countries.
It is widely accepted that clinical perfusionists should undergo a period of formal applied education and training to gain the necessary knowledge, skills and techniques [4–9]. The length of this training varies from 1 to 4 years depending on the entry requirements for the programme, and training should occur in recognized and accredited perfusion training centres. Accreditation of an educational programme is based on satisfying the minimum standards for entry requirements, facilities, syllabus, training and supervision as detailed either by national or international guidelines [5, 8, 10, 11].
The educational programme should be curriculum-based, covering applied anatomy, physiology, biochemistry, pharmacology and pathology in addition to equipment, monitoring, clinical management and service delivery. The educational programme should be delivered in conjunction with clinical training in an accredited clinical perfusion department [4, 5, 8, 11].
Increasingly, the educational benefit of simulation in perfusion is being established for the acquisition and maintenance of skills, for practising emergency procedures and for human factors training, including team and communication training [5, 8].
Following the completion of an educational programme, the trainee’s knowledge and skills should be assessed by formal written and practical examinations, leading to accreditation as a clinical perfusionist [5, 8]. After that, maintenance of an individual’s accreditation requires demonstration of a predetermined minimum annual caseload and regular participation in continuing professional development while maintaining professional standards [5–8, 10, 12]. Accreditation or recertification should be administered by the relevant national perfusion board as well as at an international level when appropriate. The framework and requirements for individual recertification vary between individual countries, and they are based on demonstration of continuing participation in professional development and education as well as the annual performance of a minimum number of clinical activities [5, 6, 8, 10].
Trained and accredited clinical perfusionists should work within an appropriate quality management framework based on documented standard operating procedures; risk assessment; regular checking and recording; leadership, teamwork and communication; and peer reviews and audits of practice and outcomes [8, 9, 13, 14].
Each department, institution or service provider should maintain a set of standard operating procedures or protocols detailing all procedures with proper equipment, the estimated frequency of occurrence, safety measures, required competencies and training, record-keeping and responsibility for adherence. These procedures or protocols should be reviewed and updated annually and approved by the institution [6, 8, 13].
Effective leadership improves quality of care and patient safety. Excellent teamwork and communication reduce errors in the operating room [8, 14]. Closed loop communication, where the sender gives a message and the recipient repeats it, reduces misunderstanding between team members [6, 7]. Regular briefings, debriefings, team meetings and self-assessments regarding team culture and performance can improve team performance [14], as can human factor training using simulation [13].
Departments should be adequately staffed in personnel and experience [8]. The daily level of accredited perfusion staff in a department should be n + 1, where n is the number of consecutive operating rooms running. For example, on a day with 3 operating rooms scheduled for CPB, there should be 4 perfusionists present in the department [6, 9]. If this is not possible—for example, outside of regular working hours—then the situation should be risk assessed with mitigating actions such as immediate availability of additional emergency equipment and support personnel.
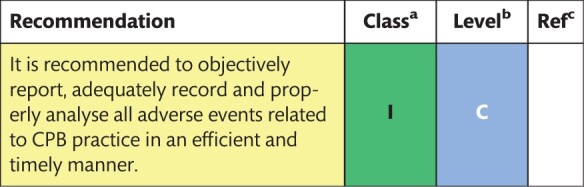
Quality assurance and improvement are fundamental to patient outcomes and safety within departments and institutions [6–8, 13, 15–17]. The health care environment must be safe; errors and untoward incidents should be reported and systematically analysed to identify system failures [12, 13]. Departments and national perfusion bodies should ensure that such outcomes are shared locally and nationally to promote shared learning.
The accurate reporting of data and outcomes with submission to a database or clinical registry enables the success and efficacy of interventions or treatments to be established. Clinical perfusionists should collect and submit such data and use it for quality assurance and improvement [6, 7, 13]. Further details relating to data management systems as an opportunity for quality improvement (QI) in perfusion practice are described in Section 4.6.
Recommendations for training, education and service delivery
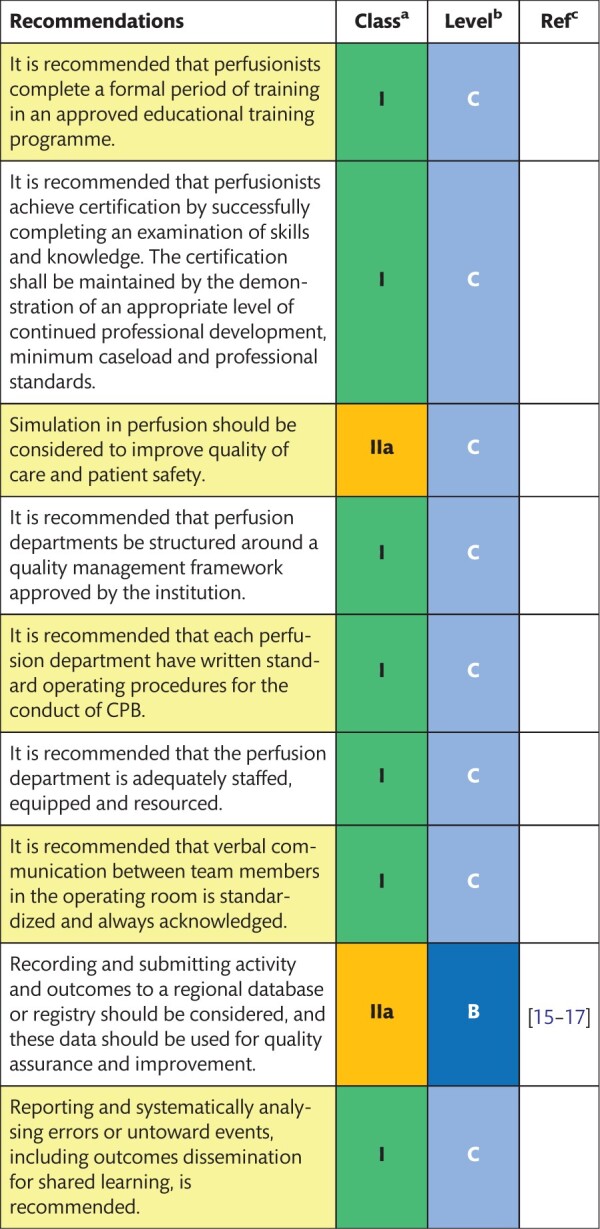
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
4. HEART–LUNG MACHINE HARDWARE
The many technological developments concerning heart–lung machine hardware and related components have made it possible to reduce the incidence of complications and problems during CPB. Clinical perfusionists can now proactively monitor the metabolic demands of the body and guide interventions to maintain adequate organ perfusion, oxygen supply and anticoagulation, with good evidence of improved outcomes.
4.1 Console with pumps and holders
The console of the heart–lung machine, with its pumps and holders, is the backbone on which disposable CPB sets are mounted. Two basic design philosophies prevail in modern heart–lung machines: the comprehensive stationary design with extensive monitoring and ergonomics versus the compact ambulatory systems, often used for extracorporeal membrane oxygenation and other indications.
4.1.1 Description of the evidence
Very few publications focus on the hardware aspect of heart–lung machines. In most centres, large stationary designs are mainly used in routine cases and complicated operations. Stationary systems may be integrated systems, modular systems or a combination. There is general agreement on which safety features should be included, as acknowledged in previous guidelines such as those of the American Society of Extracorporeal Technology and the Australian and New Zealand College of Perfusionists [6, 18]. These include pressure controllers, air detectors, low-level alarms, electrical safety specifications, pump reversal of flow or ‘runaway’ protection. Moreover, there is the possibility for the manual operation of these pumps with crank handles. Most systems include an integrated light source and batteries for operation in the event of a power failure. Although stationary systems still have wheels and can be moved around, new ambulatory systems became more popular with the increased interest in extracorporeal membrane oxygenation and minibypass systems.
It is noteworthy to mention the lack of scientific research on console designs. The few publications that can be found are focused mainly on minor aspects of the topic, such as developing universal oxygenator holders [19], improving roller pump control [20] or researching battery performance [21]. Important aspects, such as the safety of portable devices or the ergonomics of the design and safety aspects, are not among features explored by available scientific publications. Thus, recommendations are based on expert consensus and are mainly in line with the current recommendations from other societies [6, 18].
4.2 Monitoring
Monitoring of physiological patient parameters and of CPB performance parameters is the mainstay of the perfusionists’ care of patients. Whereas it is obvious and common sense to monitor basic parameters such as arterial blood pressure, pump flow and blood gas analysis, there are technologies that provide a more in-depth insight into how we treat our patients. Measurement of oxygen saturation in the venous line (SvO2) [22] and continuous blood gas monitoring [23] have gained major importance. Regional cerebral tissue oxygenation may be assessed by near-infrared spectroscopy (NIRS), whereas the measurement of oxygen delivery (DO2) has been suggested by some investigators as a worldwide standard of care for assessing arterial flow rate. Still, the cost and the weakness of the evidence make the dissemination of health care technologies and implementation in daily practice difficult. Non-invasive cerebral monitoring, such as regional cerebral tissue oxygenation and electroencephalography (EEG)-based depth of anaesthesia monitoring, is discussed in more detail in Section 7.16.
Recommendations for use of heart–lung machine hardware
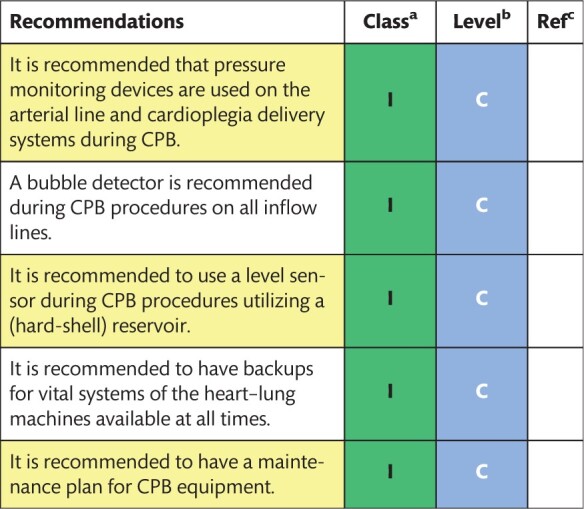
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
4.2.1 Description of the evidence
We propose a list of monitoring parameters (Supplementary Material, Appendix B) derived from other standards and guideline documents that should be followed by the cardiac surgery team [6, 24]. The list is exhaustive but not limited. Most parameters are undeniably equivalent to good practice and will probably be used by the majority of perfusionists. For other parameters, there is not always evidence that their use leads to better patient outcomes. If a parameter is monitored, then the equipment with which the parameter is measured should be calibrated and maintained regularly and checked before use.
Recommendations for standards of monitoring during cardiopulmonary bypass
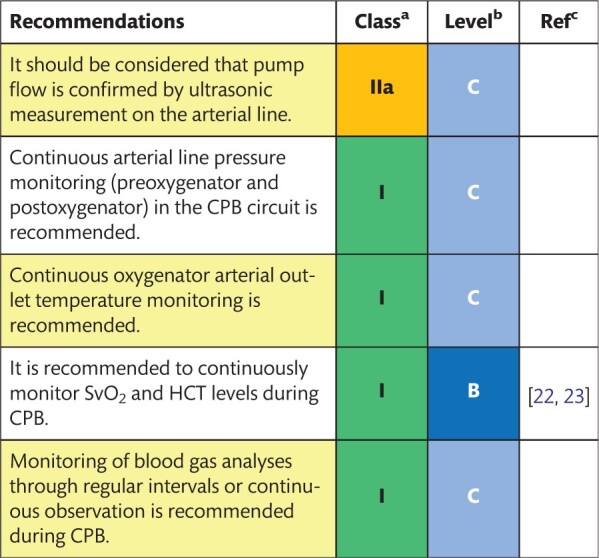
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass; HCT: haematocrit; SvO2: mixed venous oxygen saturation.
4.3 Safety features
The likelihood of death from CPB-related incidents has been declining over the last few decades to 1 in 4446–4864 patients, whereas severe injury or death was 1 in 1453–3220 patients [25, 26] in the 2000s. Studies on safety and human factors have identified numerous potential risks.
4.3.1 Description of the evidence
A Failure Mode and Effects Analysis has identified mechanisms during CPB whereby failing safety equipment or mechanical issues can compromise patient safety. Six different CPB configurations were evaluated [27]. The highest risks across all circuit types were attributed to the embolization of defoamer material, air embolism, spallation, the activation of systemic inflammatory response syndrome and overpressurization [27]. Human factor studies have highlighted several areas for improvement in addition to the mechanical safety of the device, including the organizational culture of safety [28, 29]. Collecting information on adverse events in registries will help prevent such incidents in the future [30]. An excellent tool that perfusionists can use for this purpose is the online Perfusion Improvement Reporting System of the Australian and New Zealand College of Perfusionists (https://anzcp.org/pirs-ii/). Perfusion safety can be enhanced by a multitude of measures, such as the use of dedicated safety equipment [e.g. level detectors, bubble detectors, an arterial line filter (ALF), pressure transducer, one-way vent valve, backup systems] [7]. In a survey published in 2000, 27 safety devices were identified [25]. The authors recommended improvements in coagulation monitoring and incident reporting [25]. The question remains whether new developments, such as minimally invasive extracorporeal circulation (MiECC) or surgery without CPB, increase or reduce the safety of perfusion. In a recent meta-analysis including 134 RCTs, perioperative outcomes were improved by using MiECC or the off-pump technique compared to conventional CPB (for the purpose of these guidelines, ‘conventional CPB’ is defined as CPB not fulfilling the definition of MiECC given in the text and the position paper of the Minimal invasive Extra-Corporeal Technologies international Society [31]) [32]. However, these findings are challenged by large-scale multicentric RCTs [33, 34].
Recommendation for the safety of cardiopulmonary bypass programmes
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
4.4 Oxygen and air, carbon dioxide and volatile anaesthetics supply
It is evident that continuous gas supply is required for the conduct of CPB. Oxygen, air and carbon dioxide (CO2) should be available (as well as a backup supply) in the operating room where CPB or extracorporeal life support (ECLS) is used. Monitoring gas supply and exchange is paramount to the safe conduct of CPB. The use of volatile anaesthetics during CPB is common. When using volatile anaesthetics during CPB, monitors for incoming and outgoing anaesthetic gases and a scavenging system for waste anaesthetic gases should be installed and maintained.
4.4.1 Description of the evidence
Existing standards and guidelines recommend a piped supply of oxygen and air for the gas supply to the oxygenator and of CO2 for flushing the extracorporeal circulation before priming and to maintain pH-stat acid-base management when needed. In addition, a backup supply (gas cylinders) for gases is recommended in case of technical malfunction [7, 13, 24]. Volatile anaesthetics have been frequently used during CPB. A critical review of clinical studies in this field is performed in Section 7.12. CPB entails the risk of occupational exposure to volatile anaesthetic agents. To avoid unwarranted exposure, the use of a scavenging system at the outlet of the oxygenator is recommended [7, 13, 24]. Excessive negative pressures need to be avoided with the scavenging system because they can cause a negative pressure gradient across membrane oxygenators resulting potentially in disruption of the oxygenator membrane and oxygenator failure [35]. Adequate knowledge of the effects of volatile anaesthetics is paramount for perfusionists [35].
Recommendations for security and control of gas supply
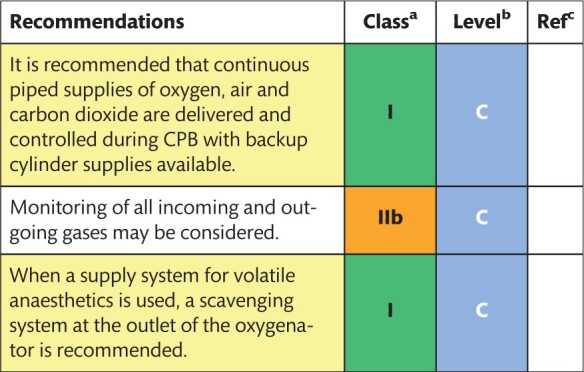
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
4.5 Heater-cooler unit
The heater-cooler unit (HCU) is an integrated hardware component of the CPB system and is a part of modern heart–lung machines. During normothermic CPB, HCUs are used to maintain the patient’s body temperature and for efficient cooling and warming in deep hypothermic circulatory arrest. This is usually achieved by running water at a precise temperature around the fibres of the oxygenator or the coils of the cardioplegia system. Previous guidelines recommendations regarding HCUs were limited to mentioning temperature and pressure safety devices and advising that the manufacturers’ instructions for maintenance be followed [18]. Very little scientific evidence regarding HCUs has been published until recently, when the deleterious effects of microbial contamination of HCUs came into focus.
4.5.1 Description of the evidence
The risks of using tap water were the focus of a publication as early as 2002 [36]. In this seminal report, an outbreak of Mycobacterium chimaera infections following open-heart surgery was identified in 6 patients at a single centre between 2008 and 2012 [37]. The evidence collected in these cases suggested an airborne transmission of the agent from the HCUs to the patients [37]. Experimental evidence confirmed how the M. chimaera contamination of the HCUs could reach the operating field and cause infection [38]. M. chimaera is a non-tuberculous mycobacterium that is commonly found in the environment and rarely causes disease [39]. Many reports from other centres confirmed that the observed phenomenon represented a global outbreak. The incidence of M. chimaera infections ranges between 156 and 282 newly diagnosed cases/year in the 10 major valve markets worldwide, with an annual rate of new diagnoses of 50–80 patients in the USA [40]. Furthermore, microbiological investigations revealed that in more than 100 cases of prosthetic valve endocarditis, vascular graft or disseminated disease, the most likely cause of infection was contamination with M. chimaera at the production site of the factory where the HCUs were assembled [39]. A recent study from Denmark showed that several brands of HCUs have been affected by contamination [41]. Recommended preventive measures include the placement of HCUs outside of operating rooms, adherence to manufacturers’ decontamination procedures, local monitoring and international cooperation [42].
Recommendations for disinfection and storage of heater-cooler unit
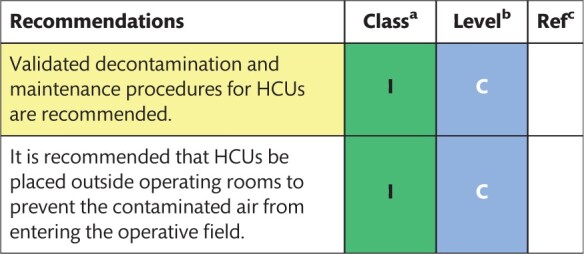
|
Class of recommendation.
Level of evidence.
References.
HCUs: heater-cooler units.
4.6 Patient data management systems and quality improvement
Technological advances allow electronic and automated recording of perfusion parameters. Electronic document management systems have several advantages compared with handwritten records [15, 43], allowing perfusionists to pay direct attention to patient and pump, especially during emergencies. Electronic charting should lead to participation in QI initiatives and national and/or international registries [7, 17, 44]. Ultimately, response feedback systems can lead to improved care [44, 45]. Limitations are that not all parameters are registered automatically; privacy, security and quality of the data should be assured; and QI initiatives should accompany electronic recording in order to ensure better health care [7, 46]. Importantly, it is advised that national law or rules established by national competent bodies be strictly followed.
4.6.1 Description of the evidence
In a comparison of electronic versus written recordings in 17 procedures, it was found that manual recording failed to capture critical events, such as maximum and minimum mean arterial pressures (MAPs) and temperatures (P < 0.05) [43].
In a study from 2008, 3 groups in an observational cohort were compared [17]. Group 1 received no QI feedback; group 2 received automated QI feedback in the form of a report generated after electronic recording; and group 3 received automated QI feedback, and a continuous QI programme was installed. The study demonstrated that the implementation of a QI process for CPB significantly reduced the cumulative time of the cardiac index below 1.6 l/min/m2 and the time of MAPs below 40 mmHg and produced a significant decrease in the cumulative time of mixed venous saturations of <60% and arterial outlet temperature >37.5°C in groups 2 and 3. The use of this technique is optimized when included as part of a QI programme, utilizing the Define, Measure, Analyse, Improve and Control method and statistical control charts [17].
The introduction of a QI programme was described in 2 phases [46]: the introduction of a database for inter-perfusionist comparison (phase I) and the implementation of electronic data recording (phase II). Although the description of the results is vague, the authors concluded that the introduction of a QI programme, together with electronic data recording, led to reduced variability among perfusionists and assured compliance with policies and standards of care.
Only a few clinical registries collect data regarding the practice of CPB. The PERForm Registry, which is an integral part of the Michigan Society of Thoracic and Cardiovascular Surgeon Quality Collaborative’s programme, has been able to successfully and accurately collect data concerning cardiovascular perfusion to improve outcome and decrease costs associated with cardiac surgery in Michigan since 2011 [15]. By examining PERForm data for CPB and related outcomes, the Michigan Society has been able to define and decrease numerous risk factors associated with adverse outcomes [47, 48]. Similar databases were developed in Australia, New Zealand [17] and Sweden [49], and the Northern New England Cardiovascular Disease Study Group has established a perfusion registry [16] to facilitate and provide perfusionists and the cardiac surgical team with valuable information to improve the practice of CPB in adults [50].
Recommendations for data collection and quality improvement
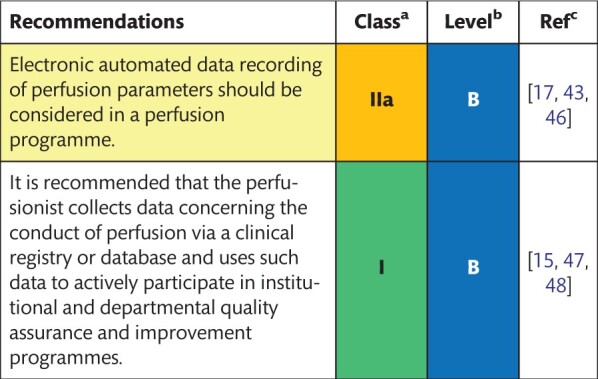
|
Class of recommendation.
Level of evidence.
References.
5. CARDIOPULMONARY BYPASS—THE DISPOSABLES
The CPB service requires adequate dedicated space—with convenient, easy access for clinical perfusionists to the operating room—for the storage of supplies of disposable equipment and hardware items. Storage areas should be designed or adapted to ensure excellent storage conditions. In particular, they should be dark, clean and dry, protected from moisture and maintained within acceptable temperature limits and humidity limits as given in label descriptions.
5.1 Cannulas
5.1.1 Arterial cannulation
The distal ascending aorta is the most common arterial cannulation site. To reduce the risk of aortic dissection, which is observed in 0.06–0.23% of aortic cannulations [51, 52], the systolic arterial blood pressure is usually lowered below 100 mmHg before cannulation. The femoral and axillary arteries are the most common alternatives to ascending aortic cannulation. The femoral artery may be the primary choice for rapid cannulation in an emergency where CPB is needed, such as cardiac arrest, aortic dissection or severe bleeding, or in reoperative or minimally invasive cardiac surgery [53, 54]. The axillary-subclavian artery is increasingly used for cannulation, especially in aortic dissection, because these vessels permit antegrade flow in the arch vessels and are usually free from atherosclerosis with rich, collateral vessels to the distal arm [53]. Other arterial cannulation sites, such as the innominate artery, the iliac artery and the apex of the left ventricle, are rarely used.
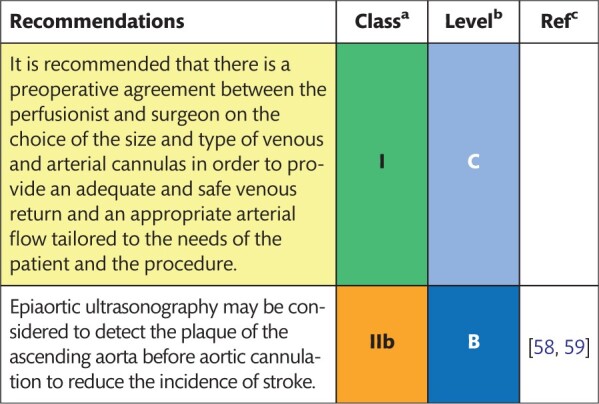
During arterial cannulation, dislodgement of atheromatous debris from the aortic wall can occur from manipulation, cross-clamping or the sand-blast effect of the cannula jet. Dislodgement is a significant cause of perioperative stroke but is also a risk for intraoperative aortic dissection [52, 55]. Therefore, special cannulas have been designed that minimize jet effects and the ‘sand-blasting’ effects of the end-hole stream [56]. To detect major atherosclerosis, simple palpation can be used, as well as transoesophageal echocardiography (TOE); however, both techniques provide inadequate views of the ascending aorta. Therefore, epiaortic scanning (EAS) is the preferred method of screening [57, 58]. Although most studies have been inadequately powered, which limits the interpretation of their results, a large retrospective study from Germany showed that the use of perioperative EAS significantly improved neurological outcomes because the cannulas were relocated and the operative course was changed in 4% of the patients due to the finding of aortic disease [58]. This situation is specifically related to patients older than 50–60 years and those with a history of transient ischaemic attacks, strokes, peripheral arterial diseases and calcifications observed on preoperative imaging or with intraoperative palpation. An RCT of 113 patients who had coronary artery bypass grafting (CABG) compared EAS with manual aortic palpation without EAS [59]; the results indicated that the use of EAS led to modifications in the intraoperative surgical approach in 29% of patients undergoing CABG. Importantly, in 0.7–2.3% of cases, with up to 4.3% of rates reported, a calcified aorta (‘porcelain aorta’) was noted in patients requiring cardiac surgery. However, there were no differences in the incidence of neurological complications between the groups [59]. Nevertheless, EAS may lead to relocation of the aortic cannula to the distal arch, axillary-subclavian or femoral arteries or to the performance of off-pump surgery in selected patients [60].
5.1.2 Venous cannulation
Central venous cannulation can be performed with bicaval, single atrial or cavoatrial (‘2-stage’) approaches with entrance into the right atrial appendage and the end of the cannula in the upper part of the inferior vena cava. Venous cannulas are usually made of flexible plastic, which may be reinforced to prevent kinking. The size of the cannula, which can have a bent or straight end, is selected based on patient size and weight, anticipated flow rate and an index of catheter flow characteristics and resistance and the vessel that is to be cannulated. Negative pressure can be applied to the venous line to provide assisted venous drainage using either a roller or a centrifugal pump system or by applying a regulated vacuum to a closed hard-shell venous reservoir. This technique permits the use of a small-diameter cannula and may be helpful when a long cannula is used. However, it can increase the risk of aspiration or of microscopic air that could cause cerebral injury or haemolysis. Optimized venous return with a self-expanding cannula is a promising concept, especially in minimally invasive surgery, but needs further investigation [61].
Recommendations for configuration and cannulation strategies
|
Class of recommendation.
Level of evidence.
References.
5.2 Venting and suction devices
During cardiac surgery, it is essential to aspirate blood from the operative field to the CPB circulation, either through cardiotomy suction or by venting the heart and great vessels. Negative pressures on the suction line and on the blood–air interface contribute to activation of blood and damage of blood cells.
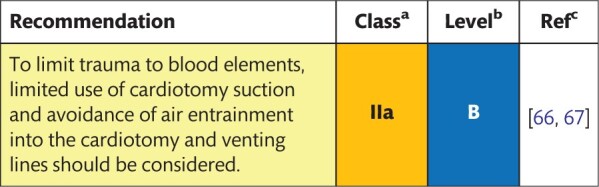
5.2.1 Description of the evidence
In vitro studies suggest that negative forces can cause haemolysis, which is augmented when there is an air interface with the blood [62–64]; granulocyte activation has also been reported in this situation [64]. One in vitro study showed more gaseous microemboli (GME) in the arterial line when the air was introduced into the venting line [65]. Two clinical studies suggested that a more gentle way of aspirating blood with passive venting [66] or the use of a smart suction device for cardiotomy suction (which only aspirates when in contact with blood) [67] can diminish the occurrence of haemolysis. However, no clinical outcomes were reported.
Recommendation for use of venting and suction devices
|
Class of recommendation.
Level of evidence.
References.
5.3 Reservoirs
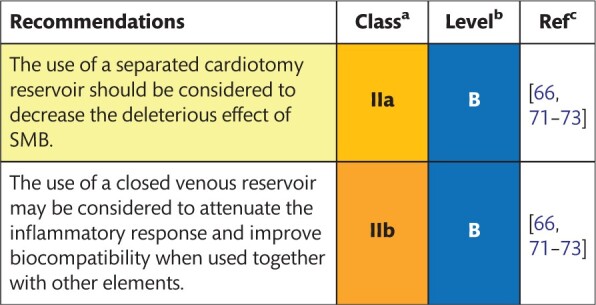
A venous reservoir to intercept the venous drainage coming from the patient and a cardiotomy reservoir to catch and process shed mediastinal blood (SMB) and blood from the venting lines are both used during standard CPB. There is a debate between advocates of closed versus open venous reservoirs. Although both types have advantages and disadvantages, no evidence points to a definite benefit for either. Whereas open reservoirs have the reputation of being safer and easier to use, closed reservoirs would be advantageous in terms of biocompatibility and saving blood. It is clear from Section 7.17 that the use of the separated cardiotomy reservoir for SMB is recommended. First experiences with a device that can eliminate fat particles and leucocytes from SMB offer conflicting results and warrant more investigation.
5.3.1 Description of the evidence
There is no difference concerning biocompatibility between open or closed reservoirs in valvular surgery or CABG [68, 69]. In a systematic review, no evidence was found for the superiority of either device [70], but the main advantage of the open system was related to ease of use. Several studies have compared closed versus open reservoirs in combination with other measures that are deemed more biocompatible (coating, a centrifugal pump, avoidance of cardiotomy suction, passive venting); they found that the combination of these measures was better in terms of biocompatibility and blood handling, but it was not possible to determine which component was responsible for which benefit [66, 71, 72]. In particular, any benefit from either open or closed reservoirs might be masked by the reinfusion of unprocessed SMB with regard to the activation of coagulofibrinolysis [73]. It was, however, shown that closed reservoirs required fewer transfusions in a low haematocrit (HCT) (∼35%) group of patients [74]. This difference was probably attributable to the significant difference in priming volume (1180 vs 760 ml).
All studies on open versus closed reservoirs published so far suffer from severe methodological limitations, including (i) small sample size, (ii) end points that are not consistent and well defined and cannot be measured objectively and finally (iii) a combination of interventions, such as the use of cardiotomy suction, that makes interpretation and the use of these findings difficult.
Three publications reported the results of investigations of a cardiotomy reservoir that was designed to remove fat particles and leucocytes from SMB [75–77]. All available studies showed a decrease in circulating leucocytes. However, some studies found a decrease in fat removal [75, 77], whereas others failed to replicate previous findings [76]. This difference is probably due to a different measurement method. More studies with clinical end points are needed to establish a benefit from this device.
Recommendations for selection and use of reservoirs
|
Class of recommendation.
Level of evidence.
References.
SMB: shed mediastinal blood.
5.4 Oxygenators
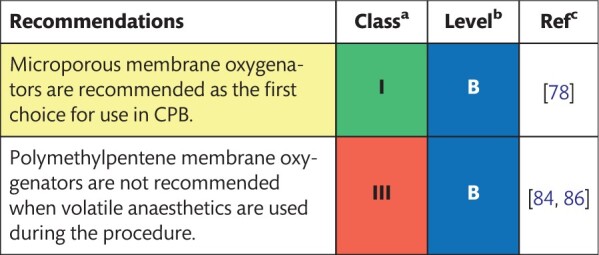
Worldwide, membrane oxygenators are the first choice for gas exchange during CPB. Many studies have shown their superiority over bubble oxygenators concerning GME generation, complement activation and neuropsychological outcome. However, not much effort has been made to evaluate the impact of membrane oxygenator design on outcome parameters.
5.4.1 Description of the evidence
No meta-analyses have been published evaluating the impact of oxygenator design on outcome parameters. One RCT investigating 9 commercial microporous membrane oxygenators, under controlled clinical conditions, documented significant differences in pressure drop, diffusion capacity, oxygen gradient and heat exchanger performance among the devices. However, no differences were observed for platelet loss or free plasma haemoglobin (Hb) concentration [78]. In addition, 2 studies looking at the relationship between shear stress, pressure drop and cell activation were unable to demonstrate differences in cell damage between the different hollow fibre membrane oxygenator designs, although white blood cell activation was more pronounced with a flat sheet design [79, 80]. An RCT studying the differences between 2 membrane oxygenators with an integrated arterial filter but different surface coatings showed a significant difference between devices with respect to postoperative bleeding, transfusion and inflammatory response as witnessed by C-reactive protein concentration [81]. However, the results could not be used to determine whether those differences were due to design variables or to the different types of coatings used. An extensive retrospective analysis looked at the impact of the use of a haemocompatible coating versus no coating on the incidence of oxygenator failure caused by the pathological absorption of fibrinogen, platelets and other blood components. The analysis showed an apparent protective effect of coating in preventing oxygenator failure (0.03% vs 4.3%) [82].
Two small RCTs show that it is not advisable to use polymethylpentene membrane oxygenators in combination with volatile anaesthetics during cardiac surgery because the membrane has a low permeability for volatile anaesthetics. As a consequence, volatile anaesthetics administered through the native lungs accumulate in the plasma, leading to an undesired greater depth of anaesthesia [83]; alternately, when added to the sweep gas of the oxygenator, they present the risk of intraoperative awareness [84, 85]. Microporous polypropylene membrane oxygenators do not have increased membrane resistance for volatile anaesthetics. The use of volatile anaesthetics does not interact with the chemical structure of the membrane and does not influence oxygenator performance over time [86].
Recommendations for selection of an oxygenator
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
5.5 Pumps
Most heart–lung machines use roller pumps for aspirating wound blood, venting cardiac chambers and delivering cardioplegia. Both, roller pumps and centrifugal pumps are used to support systemic circulation. With roller pumps, occlusion needs to be adjusted manually. Depending on the setting, they can generate haemolysis and spallation of the tubing inside the pump housing. Centrifugal pumps are non-occlusive but sensitive to sudden changes in afterload and preload. As such, they need to be used in combination with a flow probe. Because no tubing wear takes place with centrifugal pumps, they are considered more haemocompatible for prolonged usage. Despite the theoretical advantages of centrifugal blood pumps over roller pumps, it has been challenging to demonstrate that the use of centrifugal pumps improves clinical outcomes.
5.5.1 Description of the evidence
One systematic review and a meta-analysis of the existing literature investigated the effect of different blood pumps in cardiac surgery on postoperative clinical outcomes [70, 87]. Based on high-quality RCTs, no differences were seen between roller pumps and centrifugal pumps with respect to the number of patients transfused [odds ratio (OR) 1.11; 95% confidence interval (CI) 0.64–1.92], packed red blood cell (PRBC) transfusions [weighted mean difference (WMD) −0.10 units; CI −0.35 to 0.15], postoperative blood loss (WMD −10.26 ml; 95% CI −54.3 to 33.7), intensive care unit (ICU) length of stay (WMD −0.10 days; 95% CI −0.29 to 0.09), hospital length of stay (WMD −0.12 days; 95% CI −0.37 to 0.12) and death (OR 1.05; 95% CI 0.58–1.88) [87]. In contrast, a large single-centre RCT showed that the use of centrifugal pumps versus roller pumps with the same extracorporeal circuits was an independent predictor of significantly less chest tube drainage and massive blood transfusions (>5 units) [88].
The impact of the pump on blood elements remains unclear. One single-centre RCT showed significantly lower platelet activation with centrifugal pumps [89], whereas another showed a more than 50% reduction in tissue factor release with centrifugal pumps versus roller pumps but no difference in thrombin–antithrombin III, F1 + 2 or thrombin formation [90]. A recent RCT was not able to demonstrate significant differences in preoperative, perioperative and postoperative laboratory values in patients having CABG surgery using 3 different centrifugal pumps, a roller pump or a peristaltic pump [91]. When studying differences in haemolysis in vivo among centrifugal pumps, roller pumps and roller pumps with a dynamic occlusion setting, no differences between pumps were noted [92].
With respect to outcome measures, 1 single-centre RCT of 103 patients using neuropsychological testing before and after elective CABG could not find significant differences in the incidence of neuropsychological deficits for patients with a deficit in at least 1 test (centrifugal, 33% vs roller, 51%; OR 0.48; 95% CI 0.22–1.06) or patients with a deficit in >2 tests (centrifugal, 6% vs roller, 18%; OR 0.26; 95% CI 0.07–1.03), although more individual test deficits were noted in the roller pump group [93].
Recommendation for selection of a blood pump
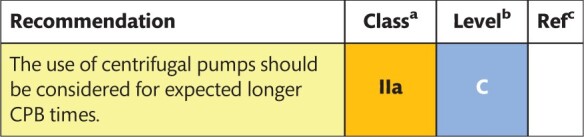
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
5.6 Filters
Since the start of cardiac surgery with CPB, solid microemboli, deformable (fat) microemboli and GME have been a concern. To minimize embolization, filters were introduced at several levels in the CPB circuit. Different filter technologies were introduced: depth filtration, screen filtration or a combination of both. A combination of both filters is used for removing particles and (activated) leucocytes to attenuate the inflammatory response. Although most cardiac centres use ALF, minimal information is available on the clinical benefits, especially when combined with extraluminal hollow fibre membrane oxygenators that act as a depth filter.
5.6.1 Description of the evidence
No recent meta-analysis comparing the impact of (integrated) ALF in combination with extraluminal hollow fibre membrane oxygenators is available. One small non-controlled trial showed a significantly lower number of GME compared with bubble oxygenators [94]. The use of ALF reduces microemboli significantly when used in combination with bubble oxygenators [95, 96]. This efficiency is inversely related to the pore size of the filter screen [97].
Interestingly, a membrane oxygenator without ALF had a lower microemboli count than a bubble oxygenator with ALF and elicited better scores in patients given neuropsychological tests 1 month postoperatively [98]. When comparing the efficiency of integrated versus standalone ALF in reducing microemboli, no differences were found for a 40-µm screen ALF, but a higher efficiency was found for a 20-µm screen ALF [99]. When using MiECC that uses no reservoir, the use of an ALF [100] and a venous bubble trap is beneficial in reducing GME [101].
A small RCT comparing leucodepletion (LD) filtration versus no filter was unable to demonstrate outcome differences but did not look for neuropsychological outcomes [102, 103]. An attempt was made to perform a meta-analysis comparing the benefit of LD filtration versus standard filtration after cardiac surgery, but the authors concluded that insufficient data were available in the literature to perform a meta-analysis or a sensitivity analysis [104]. The authors were not able to define any benefit for the length of hospital or ICU stay. An RCT comparing an LD filter with 2 standard filters showed a significantly lower microemboli count in the right middle cerebral artery in the LD group (median = 15) compared to 2 conventional screen filters (median = 67 and median = 55) (P < 0.001). However, the authors were unable to demonstrate a statistically better neuropsychological outcome [105]. Among the 2 RCTs studying the impact of LD filtration on postoperative morbidity, one was unable to show a significant impact on postoperative morbidity with an LD filter [106], whereas the other demonstrated lower pulmonary inflammation as witnessed by a significantly improved oxygenation index [107].
5.7 Material and surface treatments
The contact of blood with the CPB circuit induces a systemic inflammatory response with involvement of leucocytes; platelets; and complement, inflammatory and coagulation systems. This response can be reduced by coating the circuit and oxygenator with a biocompatible ionic or covalent heparin substance, phosphorylcholine, poly(2-methoxyethyl acrylate) or other artificial surface material. Biocompatible coatings may contribute to a reduction in the systemic inflammatory response and in the activation of the coagulation system during CPB.
Recommendations for use of blood filters
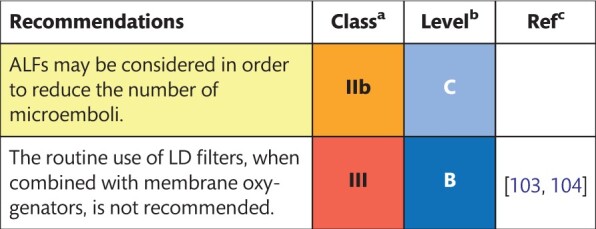
|
Class of recommendation.
Level of evidence.
References.
ALFs: arterial line filters; LD: leucodepletion.
5.7.1 Description of the evidence
Three systematic reviews and a meta-analysis investigated the effect of different biocompatible coatings in cardiac surgery on postoperative clinical outcomes [108–111]. When high-quality RCTs were taken into account, biocompatible coatings were associated with a reduction in PRBC transfusions (OR 0.88; 95% CI 1.08–1.26), atrial fibrillation (AF) (OR 0.66; 95% CI 0.49–0.88) and reduced ICU stay by 5 ± 2 h, but not with the number of deaths (OR 0.78; 95% CI 0.39–1.55) [108]. Others showed the beneficial effects of heparin-bonded circuits on blood loss and transfusion rates, reoperation for bleeding (OR 0.6; 95% CI 0.4–0.8), reduced ICU stay (WMD −9.3 h; 95% CI −14.7 to −3.9) and hospital stay (WMD −0.5 days; 95% CI −0.9 to −0.1) [109, 111]. Finally, in a systematic review of 14 RCTs, the beneficial effect of heparin or phosphorylcholine coating was shown on postoperative neurological and pulmonary functions [110].
The number of comparative studies of biocompatible coatings that focus on major end points, including neurological outcomes, kidney function or death, is limited. A relatively large RCT showed a lower incidence of postoperative neurological deviations in the heparin-coated group compared to the non-coated group (3.9% vs 9.4%; P = 0.021) after CABG surgery [112]. The use of a phosphorylcholine coating in isolated coronary surgery was associated with lower peak serum creatinine levels (1.19 ± 0.48 mg/dl vs 1.41 ± 0.94 mg/dl; P = 0.048) compared to controls [113].
Head-to-head comparisons of different surface materials for circuit coating with the clinical outcome as a primary end point are, however, lacking.
Recommendation for coating material of cardiopulmonary bypass circuits
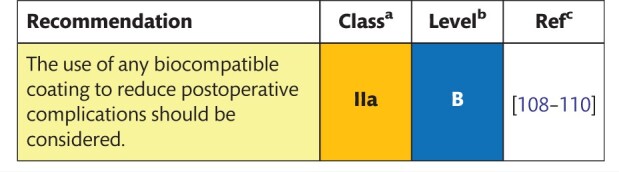
|
Class of recommendation.
Level of evidence.
References.
6. PREPARATION FOR CARDIOPULMONARY BYPASS
Prior to the initiation of CPB, several vital steps must be completed to ensure patient safety. Patient safety was defined by the Institute of Medicine [114] as ‘the prevention of harm to patients’. Emphasis is placed on the system of care that (i) prevents errors; (ii) learns from the errors that do occur; and (iii) is built on a culture of safety that involves health care professionals, organizations and patients. Adequate preparation for CPB is one of the crucial steps to successful cardiovascular operations.
6.1 Checklist
The use of checklists has been well established in medicine, specifically surgery, as well as other industries. It has been proven that their use can save lives, time and money as well as reduce the rate of complications [115]. It therefore appears logical to assume that the use of pre-CPB checklists will have similar effects, particularly with regard to complications during CPB. Checklists should be used in an appropriate, diligent and professional manner. They should be adapted to the specific working environment; they should consider emerging technologies; and they should be revised at time intervals consistent with institutional protocol.
The efficient use of checklists needs to be supported by additional safety features, such as multidisciplinarity, teamwork, professional communication, managerial support and an open safety and adverse incident reporting culture [116].
6.1.1 Description of the evidence
Although pre-CPB checklists have been increasingly used since the early days of CPB [117], there is a lack of evidence demonstrating a beneficial effect, because the topic has not been investigated in much detail. A few case reports [118, 119] and 1 study of a simulation scenario [120] suggest that adverse incidents can be avoided by the use of checklists; however, the studies fail to show that the introduction of a new checklist enhances safety in a clinical setting. One study, based on a survey from the Netherlands, suggests that there was no correlation between the reported rate of adverse incidents and the use of a written pre-CPB checklist [121]. Nevertheless, the authors recommend including a pre-CPB checklist in perfusion practice.
Recommendations for use of precardiopulmonary bypass safety checklists
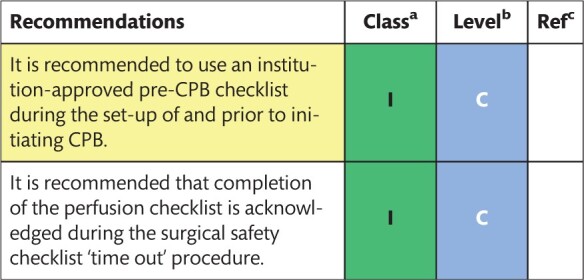
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
To conclude, it is recommended that a pre-CPB checklist be used during CPB set-up and the initiation of CPB as well as throughout the entire perioperative period (weaning from CPB, post-CPB, emergent reinstitution of CPB) and during any other procedure or technique performed by perfusionists. The EBCP has provided a checklist on its website that can be adapted to fit centres’ preferences (Supplementary Material, Appendix C) [122].
6.2 Preoperative assessment
To be fully prepared to put a patient on CPB, the perfusionist must have a situational awareness about the patient’s condition, concomitant diseases and the type of surgical procedure. Ideally, planning should be worked out together with every stakeholder involved in the pathway of care for the patient. The use of specialized preanaesthesia clinics has a beneficial impact on hospital outcomes [123, 124], whereas inadequate or incorrect preoperative assessment can lead to harm to the patient [125].
6.2.1 Description of the evidence
The institutional preoperative assessment forms should be fully employed before any initiation of CPB. A written or electronic form should be kept in the patient’s medical record. Because the quality of information is improved when using a standardized form [126], we propose such a form (Supplementary Material, Appendix D). It is an essential document where items can be added or left out.
An adequate preoperative assessment of the patient allows the perfusionist to plan the procedure and anticipate possible complications. A preoperative assessment should be a vital part of an institute-wide planning and clinical pathway for patients.
Recommendation for preoperative patient assessment
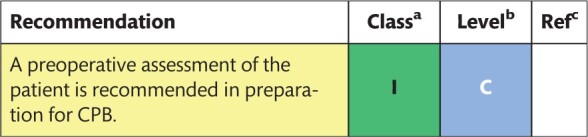
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
7. PROCEDURES DURING CARDIOPULMONARY BYPASS
Goals during CPB include the maintenance and stabilization of parameters that approximate normal physiology for optimal end-organ function, general anaesthesia and pain management and anticoagulation. Therefore, numerous specific management strategies are employed during CPB in order to modify variables that are closely related to both short-term and long-term outcomes after cardiac surgical procedures.
7.1 Type of circuit
Until a few years ago, the traditional set-up of CPB was uniformly focused on safety and maximum versatility. Following the initial success of off-pump surgery, several perfusionists tried to improve the CPB set-up. A combination of several techniques emerged that were aimed at improving biocompatibility and reducing haemodilution. The resulting minimized circuits are generally characterized by the term MiECC. The Minimally invasive Extracorporeal Technologies international Society recently published a consensus paper on terminology and definitions [31].
Features of MiECC include a small priming volume, tip-to-tip coating of the circuit, a closed system and the use of a centrifugal pump. In addition, mechanical salvage of red blood cells is used instead of cardiotomy suction. Vents are avoided whenever possible. According to the Minimally invasive Extra-Corporeal Technologies international Society, the following components are required to fulfil the definition of MiECC: a closed CPB circuit, coated contact surfaces, reduced priming volume, a centrifugal blood pump, a membrane oxygenator, a heat exchanger, a cardioplegia system, a venous bubble trap/venous air-removing device and a shed blood management system. Initially, MiECC systems were developed for coronary bypass surgery. However, all types of cardiac operations have been performed using MiECC systems today. It is important to underscore that the use of the MiECC concept relates not only to the hardware of a minimized circuit but also to a team effort to ensure successful use.
7.1.1 Description of the evidence
Three RCTs have been conducted to compare MiECC to conventional CPB [127–129]. However, none of these studies was sufficiently statistically powered to examine the primary end points. During the quality assessment, these 3 studies were classified as studies at moderate risk of bias. Therefore, systematic reviews and meta-analyses have played a central role in informing the scientific community about the effects of both interventions. Compared to the group of patients who underwent cardiac surgery with the use of conventional CPB circuits, the MiECC group of patients had a significant reduction in mean postoperative chest tube drainage and rates of transfusions of concentrated red blood cells [130, 131]. This finding may, in part, be ascribed to a reduction in haemodilution. However, chest tube drainage over the first 24 h was similar in both groups as was the rate of reoperation [131], making it difficult to judge the usefulness of MiECC. Thus, there is an ongoing scientific discussion of results indicating a reduction in blood loss, blood activation, myocardial infarction (MI), postoperative arrhythmias, cerebrovascular events and deaths [131, 132]. From a scientific point of view, interpretation of the evidence is difficult due to the inadequate statistical power of the available studies [132, 133]. As a consequence, results from meta-analyses on hard end points, such as death, are not confirmed in individual clinical trials [132].
Recommendations for the cardiopulmonary bypass circuit
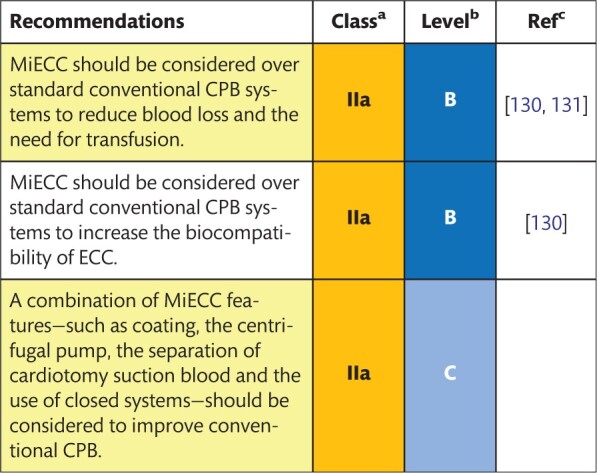
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass; ECC: extracorporeal circulation; MiECC: minimally invasive extracorporeal circulation.
7.2 Carbon dioxide flush
Neurocognitive impairment following cardiac surgery remains a significant concern. Its origin is multifactorial but particle emboli and especially GME, representing almost 80% of all emboli, are considered significant culprits because they occlude small cerebral capillaries [134]. Complete de-airing of the CPB circuit before surgery and of the cardiac chambers during open-heart procedures remains a challenge. Many techniques to optimize de-airing have been proposed over the years. A technique that regained renewed popularity is the use of CO2. The theory for using CO2 is that its higher solubility and higher density increase the buoyancy of a bubble compared to its buoyancy in air. As such, it is advocated to flush the CPB circuit with CO2 before priming and to flood the operative field with CO2 perioperatively. Many different flooding techniques have been proposed over the years. Nevertheless, there are not many studies that address the impact of the techniques on neuropsychological outcomes.
7.2.1 Description of the evidence
No meta-analysis or RCT is available that evaluates the impact of a CO2 flush before priming on the remaining amount of air in the CPB circuit. Two small studies showed a statistically significant reduction of GME [135, 136]. In order to obtain the CO2 content at 97–98% in the oxygenator, a single-centre study suggested that ∼5 min of flushing is necessary, whereas a more extended duration did not increase the value significantly [135]. Another important finding was that a CO2 flush reduced GME in the prime and not in the arterial filtration [136]. One meta-analysis has been performed regarding the impact of CO2 flooding on the neuropsychological outcome [137]. Risk difference (RD) was used as a summary statistic to account for double zero studies. Although the amount of GME was significantly lower in the CO2 flooding group (RD −0.94, 95% CI −1.63 to −0.25; P = 0.008), no differences in postoperative neurocognitive decline were noted (RD −7%, 95% CI −0.22–8; P = 0.35). Potential biases of the analysis were the non-uniform administration technique for CO2 flooding and the fact that only 1 study quantified cerebral embolization.
A single-institution RCT showed superior neurocognitive outcome when CO2 flooding was used [risk ratio (RR) 0.30, 95% CI 0.14–0.63; P = 0.001], with an RD of 13% [138]. However, no correlation could be found between the remaining air in the heart chambers, as validated by the TOE and the neurocognitive outcome. The timing of neuropsychological testing at 1 and 4 weeks postoperatively, as used in this RCT, causes an additional debate, because these tests might be influenced by anaesthetic techniques, including haemodynamic management and cerebral perfusion pressures as well as by the use of postoperative opioids [139–141]. To avoid bias, it is recommended that neuropsychological testing not be performed during the first 3 months postoperatively [142]. The only RCT that performed psychological testing at 6 weeks was not able to show the beneficial effects of CO2 flooding, although a significantly lower amount of intracardiac gas was noted on the intraoperative TOE in all cardiac chambers at any measured time point in the CO2 group compared to the control group. Furthermore, the de-airing time was significantly shorter in the CO2 group (median 9 vs 12 min, respectively; P = 0.02) [143].
The technique used for administering CO2 flooding is an important issue, because inefficient administration can result in up to 50% of the air remaining inside the thoracic cavity [144]. Ineffective de-airing may lead to conclusions that underestimate the potential benefits of CO2 flooding. Points of concern with CO2 flooding are associated hypercapnic acidosis [145], which leads to increased cerebral blood flow with its inherent risk for cerebral embolization [146], red blood cell damage [145] and a higher risk for thrombus formation in stagnant blood [147].
Recommendations for use of a carbon dioxide flush
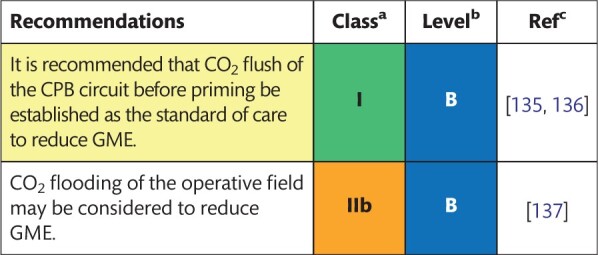
|
Class of recommendation.
Level of evidence.
References.
CO2: carbon dioxide; CPB: cardiopulmonary bypass; GME: gaseous microemboli.
7.3 Priming volume and autologous priming
The use of priming solutions in CPB induces haemodilution, may affect coagulation and may lead to fluid extravazation into the tissues. Different types and combinations of crystalloid and colloid solutions have been used, often influenced by local tradition. More recently, methods to reduce the amount of priming volume, such as autologous priming, have become popular. This reduction is achieved by allowing blood to displace the fluid in the circuit into an external reservoir in an antegrade or retrograde manner. This external reservoir is then excluded from the circuit. Unbalanced and balanced colloid solutions as priming volume or infusion fluids during CPB are discussed in Section 7.5.
7.3.1 Description of the evidence
There is no consensus regarding an optimal priming solution. According to a recent survey, crystalloids are the preferred priming solution in European centres [148]. Some colloids have been used, such as albumin, gelatin-based solutions and hydroxyethyl starch (HES). The goal of adding colloids to the priming solution is to reduce fluid extravazation and oedema formation. Recent studies have shown that this goal is feasible [149]. However, there is no evidence to support the use of a more defined priming volume, particularly because the priming volume depends on patient- and circuit-related variables. In addition, priming volume is one of several constituents of fluid management before, during and after CPB.
Many studies have been performed to evaluate the effects of adding HES regarding coagulation and acute kidney injury (AKI). Most studies on priming solutions using postoperative blood loss and/or transfusion requirements as the primary end point reported no difference in postoperative blood loss [150]. A recent Cochrane review found clear evidence of an increased risk of AKI when using a solution of HES, and its use is discouraged [151]. Recently, the use of a dextran 40-based priming solution has been advocated. However, possible advantages, such as a reduced fluid balance, and disadvantages, such as allergic reactions, have not been investigated in larger trials.
In many centres, mannitol is added to the priming solution in an attempt to reduce the risk of AKI [152]. A recent Cochrane review found no evidence to support this notion [153]. However, the quality of the evidence was not high.
Autologous priming is often combined with other methods when minimized CPB systems are used. Only smaller RCTs focused on autologous priming. A total of 6 RCTs that were explicitly conducted to investigate autologous priming were summarized in a meta-analysis published in 2009 [154]. These studies showed that autologous priming preserved HCT and reduced homologous blood transfusion, particularly in patients with a small body surface area (BSA). A more recent meta-analysis of 10 RCTs confirmed that the use of autologous priming was associated with a significant reduction in both intraoperative (RR 0.39, 95% CI 0.29–0.53; P < 0.001) and perioperative transfusion of PRBCs (RR 0.53, 95% CI 0.43–0.66; P < 0.001) [155]. These findings were confirmed in an RCT with 120 patients with a small BSA (<1.5 m2) [156]. The largest retrospective study, which included 753 patients [157], suggested that retrograde priming is associated with reduced transfusion requirements. In contrast, another study showed no benefits of retrograde priming for transfusion end points [158]. This difference was attributed to the lower transfusion threshold and the infusion of large amounts of fluids intraoperatively in the latter study [157].
Recommendations for priming volume in the cardiopulmonary bypass circuit
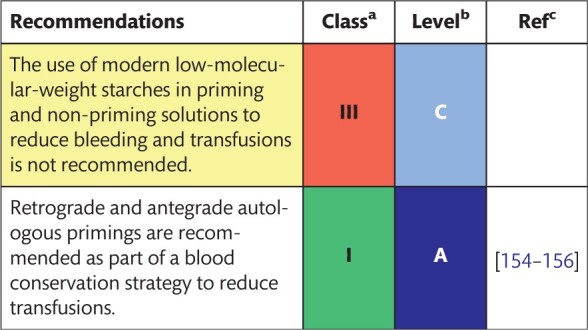
|
Class of recommendation.
Level of evidence.
References.
7.4 Anticoagulation management
Unfractionated heparin serves as an anticoagulant during cardiac procedures with CPB. Heparin binds to antithrombin, thereby potentiating the inactivation of thrombin and factor Xa by antithrombin up to 1000-fold. The sensitivity to heparin is determined by patient-specific characteristics [159]. The perioperative effect of heparin on the coagulation system is assessed by the activated clotting time (ACT). The ACT is a whole-blood coagulation test for the intrinsic coagulation system that is influenced by patient and surgical factors, including temperature, haemodilution and platelet counts. Target ACT values that are commonly used during CPB range from 300 to 600 s. Both heparin and protamine prolong the ACT [160].
Although the use of heparin is part of daily clinical care, challenges exist regarding heparin dosing, because this might influence haemostasis and the risk of postoperative bleeding. Moreover, the global variation in heparin potency may result in a different anticoagulation effect of heparin purchased from different suppliers.
7.4.1 Interventions
Heparin is usually dosed based on patient dimensions, starting with a heparin dose that ranges from 300 to 500 U/kg. During CPB, ACT tests are regularly performed and additional heparin doses are given in case of a decrease in the ACT. Heparin resistance and postoperative heparin rebound are 2 significant limitations of this strategy. Heparin resistance may lead to insufficient anticoagulation during the procedure, whereas heparin rebound may contribute to postsurgical bleeding. Interventions that contribute to tailored heparin dosing include the use of heparin measurements, anti-Xa measurements or computer-based dosing models.
7.4.2 Description of the evidence
7.4.2.1 Heparin dosage
Although most units aim for an ACT of >480 s during CPB, this threshold has been challenged in numerous clinical studies. Patients who underwent CABG with heparin-coated circuits and an ACT of 250 s during CPB did not show a significantly increased risk of thromboembolic events or signs of clotting or other technical incidents [161]. Another large cohort study from 2 centres also reported that the use of heparin-coated circuits with target ACT between 250 and 300 s was safe and effective [162]. Additionally, a small RCT of CABG procedures using MiECC has shown the clinical safety of an ACT below 300 s [163]. Taken together, it appears that the required safe ACT depends on the specifics of the circuits used. However, further research in this field is warranted.
7.4.2.2 Individualized heparin management
Individualized heparin management or titration is based on the use of the Hepcon Haemostasis Management System (Medtronic, Minneapolis, MN, USA), anti-Xa measurements or blood heparin measurements in addition to the ACT. The majority of publications on this topic considered postoperative bleeding and transfusions as the secondary end point.
Using a point-of-care–based haemostasis protocol in CABG did not reveal a difference in postoperative blood loss between patients with individual heparin titration and patients without, as shown in an RCT of 102 patients [164]. However, these findings are difficult to translate to daily practice, because a mean 24-h blood loss of more than 750 ml is considered unusually high in CABG surgery [164]. A more recent study investigated how Hepcon-based heparin and protamine management influenced heparin and protamine doses compared to a conservative anticoagulation strategy in patients having CABG surgery [165]. The study showed no differences in total heparin doses between groups, but protamine dosing was significantly reduced in the Hepcon group. This reduction was associated with an increase of 75 ml in the 12-h blood loss but not with differences in transfusion requirements [165]. In contrast, the use of a Hepcon-based strategy increased heparin dosing and reduced protamine dosing in valve surgery compared to an ACT-based strategy [166]. In the Hepcon group, fewer patients showed more than 450 ml blood loss 24 h following surgery. A small study showed that the increase in heparin dosing during a Hepcon-based strategy did not result in less haemostatic activation or postoperative bleeding compared to ACT-based management [167]. A Hepcon-based anticoagulation strategy did not influence heparin and protamine dosing or postoperative haemostasis or bleeding compared to ACT-based dosing [168]. Contrarily, the use of the Hepcon/HMS device resulted in a highly significant difference for the total protamine dose compared to ACT-based dosing (mean protamine dose: 14.190 IU vs 24.777 IU; P < 0.001) and total blood volume (mean blood loss: 804 ml vs 1416 ml; P < 0.001), whereas there was no difference in the total heparin dose [169]. Due to the lack of perioperative bleeding and transfusion rates as primary end points in these studies, larger multicentre studies are required to determine the added value of individual heparin management in the modern cardiosurgical setting.
7.4.2.3 Measures to prevent heparin rebound
Heparin rebound is the result of residual concentrations of heparin in the blood in the postoperative phase. Although most literature on this topic originates from the 1980s and 1990s, the recent literature can be divided into studies focusing on the presence of residual heparin in the blood following weaning from CPB and studies on the occurrence of postoperative bleeding associated with residual heparin. Unfortunately, most available studies focus on surrogate haemostatic end points and are not powered to show differences in postoperative bleeding and transfusions. The only comparative study that is currently available investigated whether continuous protamine infusion (25 mg/h for 6 h) to neutralize residual heparin resulted in reduced mediastinal blood loss compared to control subjects [170]. Whereas protamine infusion resulted in a reduction in a 24-h blood loss of ∼100 ml, there were no differences in transfusion rates between the groups. Blood heparin levels in the control group were highest at 3 h following surgery and normalized within 9 h postoperatively. The study was, however, limited by the possibility of administering additional protamine to normalize ACT values to preheparin values, which occurred more frequently in the control group and might have enhanced postoperative bleeding [170].
7.4.2.4 Protamine management
After weaning from CPB, protamine is used to neutralize heparin. The heparin–protamine complex that is formed leads to dissociation of heparin from antithrombin and restores the procoagulant properties of blood. Apart from systemic hypotension and pulmonary hypertension, protamine sulphate can cause anaphylactic reactions (<1%), which can result in cardiovascular collapse and are associated with an increased risk of death. Inadequate protamine dosing may influence patient haemostasis and the risk of postoperative bleeding.
7.4.2.5 Interventions
The dosage of protamine is regularly based on the initial or total administered dosage of heparin throughout the procedure. Interventions that may contribute to tailored protamine dosing include the use of heparin measurements, anti-Xa measurements or computer-based dosing models.
7.4.2.6 Prevention of protamine overdosing
A small RCT showed that protamine dosing based on the initial heparin dose resulted in prolonged clotting times and microvascular bleeding compared to protamine dosing based on the measured heparin concentration following CPB [171]. Others found that a protamine-to-heparin dosing ratio of 1.3 is associated with coagulation abnormalities, impaired restoration of post-protamine thrombin levels and postoperative bleeding compared to a protamine-to-heparin dosing ratio of 0.8 [172]. Post-protamine ACT levels were comparable among groups, and none of the patients showed signs of heparin rebound. This study was limited by the calculation of the protamine dose over the total heparin dosage administered throughout the procedure.
In addition, several studies have shown that individualized heparin and protamine dosing strategies based on Hepcon result in higher heparin and lower protamine dosages compared to ACT-based strategies in valve surgery [166] or CABG procedures [173]. This individualized strategy was associated with the preservation of platelet function [173] and with a reduction in coagulation disturbances [166]. In contrast, a recent trial of patients having CABG surgery showed that a protamine-to-heparin ratio below 0.6 was associated with enhanced blood loss and increased transfusion requirements compared to patients with a ratio exceeding 0.8 [165]. In summary, protamine should be given in a ratio of 0.8–1.0 of the initial doses of heparin. Excessive administration of protamine in the absence of a sufficient concentration of heparin is associated with perioperative bleeding and enhanced transfusion requirements.
7.4.2.7 Alternative anticoagulation
In some patients, heparin and/or protamine is contraindicated (for example, in those with severe protamine allergy or heparin-induced thrombocytopaenia). In these patients, direct thrombin inhibitors are indicated, such as the recombinant hirudin analogue bivalirudin or argatroban, a synthetic L-arginine derivative [174]. The therapeutic level of bivalirudin is measured using the ecarin clotting time, although the ACT can also be used. A baseline ACT value is measured before the administration of bivalirudin, aiming for a target of an ACT of 2.5 times baseline during CPB. Bivalirudin has a relatively short half-life of 25–36 min. Clearance of bivalirudin is mainly driven by proteolytic cleavage, and the rest of the ∼20% of the unchanged agent is cleared by the kidney [175]. Although the use of bivalirudin in comparison with heparin was associated with similar postoperative chest tube output in the literature [176], its pharmacological properties require avoidance of blood stagnation in the CPB circuit to minimize the risk of thrombosis. These characteristics ultimately affect the set-up of the perfusion system and the conduct of CPB. Thus, the routine use of bivalirudin is restricted to a skilled perfusionist/surgeon/anaesthesiologist team. On the other hand, argatroban undergoes hepatic clearance with a half-life of 40–50 min; it can therefore be used in patients with renal failure. No specific reversal agents are available for either of these direct thrombin inhibitors. Although renal replacement therapy can be used to reduce the plasma concentrations of bivalirudin, it has only modest effects on the pharmacokinetics of argatroban.
Recommendations for periprocedural anticoagulation management
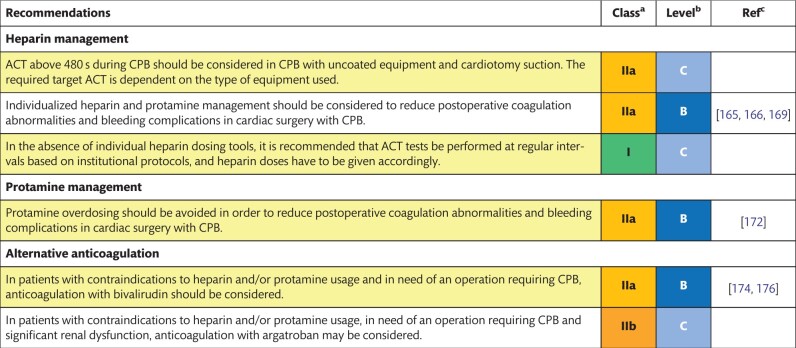
|
Class of recommendation.
Level of evidence.
References.
ACT: activated clotting time; CPB: cardiopulmonary bypass.
7.5 Acid-base homeostasis and electrolyte management
Tissue hypoxia or an electrolyte imbalance may lead to metabolic acidosis, which increases the risk of tissue injury and organ dysfunction during CPB. The excessive use of normal saline or unbalanced colloid solutions may further lead to an electrolyte imbalance and acidosis due to supraphysiological concentrations of chloride (>154 mmol/l). The management of acid-base blood gases during CPB with mild to moderate hypothermia (excluding procedures associated with deep hypothermic circulatory arrest), is normally temperature uncorrected (alpha-stat) in adult patients undergoing cardiac surgery, i.e. the blood gas measurement takes place at 37°C and it is interpreted uncorrected for body temperature.
7.5.1 Description of the evidence
In a retrospective study, moderate perioperative acidosis (pH < 7.35) and hyperlactataemia (lactate > 4.0 mmol/l) were associated with a higher 12 h chest drainage volume compared to no acidosis/hyperlactataemia (mean blood loss: 576 vs 406 ml; P = 0.001), but no other outcomes were reported [177]. In a subgroup analysis of the Transfusion Requirements After Cardiac Surgery (TRACS) trial, it was shown that lactate levels >3 mmol/l at 6 h following surgery increased the odds for major complications (OR 3.28; 95% CI 1.61–6.69) [178].
The use of alpha-stat acid-base management in adult cardiac surgery with moderate to mild hypothermia was supported by 3 RCTs from the 1990s, where it was demonstrated that alpha-stat acid-base management is associated with improved postoperative neurological and neuropsychological outcome compared with pH-stat, i.e. temperature corrected [179–181].
Normal saline or unbalanced colloid solutions that are used as priming volume or infusion fluids during CPB may result in hyperchloraemic acidosis. In 81 patients receiving either an unbalanced or balanced 6% HES 130/0.4 solution, the results showed higher plasma chloride levels, lower pH levels and a more significant decrease in base excess in the unbalanced HES group [182]. This study was, however, underpowered to show differences in clinically relevant end points.
There is a lack of large, prospective studies exploring the impact of the prevention of acidosis or hyperchloraemia during cardiac surgery on patient outcome. However, there is general agreement that normal physiological circumstances should be maintained, including an optimal pH and the avoidance of hyperchloraemic acidosis.
Increased potassium levels are commonly associated with CPB as a result of the use of cardioplegia. This is usually self-limiting and only rarely needs to be treated. However, if potassium concentrations increase to levels above 6.5–7 mmol/l, treatment should be considered with the use of modified ultrafiltration (MUF), calcium or insulin/dextrose. In addition, hypocalcaemia can occur during CPB as a result of haemodilution and particularly after transfusion of citrated blood products. Due to the important physiological role of calcium, particularly regarding cardiac surgery, relevant parameters such as coagulation, cardiac rhythm, positive inotropy and vascular tone, hypocalcaemia should be promptly treated.
7.5.2 Magnesium
Whether intravenous magnesium can prevent postoperative arrhythmias after cardiac surgery has been investigated in several small RCTs. A recent meta-analysis including 20 RCTs and 3696 patients indicated that magnesium might reduce the incidence of supraventricular arrhythmias compared with the placebo. However, this effect was lost when studies of higher quality were considered [183]. Magnesium had no effect on any other postoperative outcome variable, such as death or major morbidity and length of stay. A more recent RCT of 389 patients undergoing cardiac surgery demonstrated that intraoperative magnesium did not reduce the postoperative incidence of AF [184]. Recent comprehensive Scottish recommendations about cardiac arrhythmias in coronary artery disease suggest that magnesium may be used when prophylaxis for AF and ventricular arrhythmias is indicated following CABG surgery [185].
7.6 Control of mean arterial blood pressure
Targeting sufficient mean arterial blood pressure during CPB is of importance in order to maintain appropriate perfusion pressures in all end-organs, particularly the kidneys, the brain and the gastrointestinal tract. Vasoplegic syndrome during CPB may derive from the release of proinflammatory cytokines, anaesthetic drugs, active endocarditis and the preoperative use of angiotensin-converting enzyme inhibitors and calcium channel blockers. Hypertension during CPB may derive from an inadequate level of anaesthesia/analgesia, a release of catecholamines, vasoconstriction due to hypothermia and others.
7.6.1 Description of the evidence
A recent RCT compared high-target (70–80 mmHg) to low-target (40–50 mmHg) mean arterial blood pressure during CPB in 197 patients who had cardiac surgery, finding no differences in terms of cerebral injury [186]. In this study, the pump flow was the same in the 2 groups, and the achievement of the target perfusion pressure was based on the significantly higher amount of norepinephrine used in the high-target group. Of note, there was a trend towards a higher rate of stroke (7.0% vs 1.1%; P = 0.06; respectively) and death (4.1% vs 0%; P = 0.06; respectively) in the high-target group. Previous RCTs found conflicting results. No differences in the mortality rate, major neurological or cardiac complications, cognitive complications or deterioration in functional status were found between patients treated at a target MAP of 80 mmHg and a ‘custom’ MAP (based on the pre-CPB MAP) [187]. The Cornell Coronary Artery Bypass Outcomes Trial (CCABOT) Group Gold [188] randomized patients into a high-MAP (80–100 mmHg) group or a low-MAP (50–60 mmHg) group, finding a significantly higher rate of major cardiac and neurological outcomes in the low-MAP (12.9%) versus the high-MAP (4.8%) group. However, the high-MAP group reached a mean MAP lower than the target (69 ± 7 mmHg). In another RCT, less cognitive dysfunction and delirium were found in patients treated at an MAP of 80–90 mmHg versus 60–70 mmHg [189]. In the retrospective series, no differences in MAP during CPB were observed in patients who developed postoperative AKI versus patients with a normal renal outcome [190, 191]. It was suggested that the optimal MAP during CPB should reflect the preoperative MAP [190]; more recently, the optimal MAP (during CPB and during the early postoperative period) was assessed using ultrasound-tagged NIRS based on cerebral blood flow autoregulation [192, 193]. The extent of the MAP excursions below the optimal MAP was superior in patients with postoperative AKI and delirium [193]. Finally, the MAP during CPB is usually accepted in a range of 50–80 mmHg; however, novel approaches to settle the optimal blood pressure have been recently proposed [192].
Recommendations for acid-base balance and electrolyte management
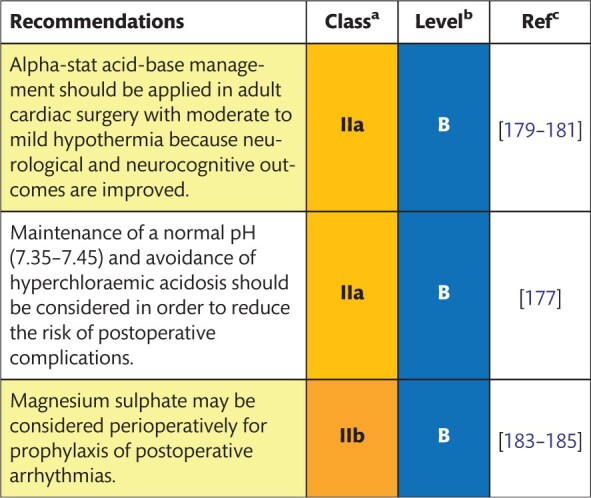
|
Class of recommendation.
Level of evidence.
References.
Vasopressors (epinephrine, norepinephrine, vasopressin, terlipressin, phenylephrine, metaraminol, methylene blue, hydroxocobalamin and combinations) are required to treat vasoplegic syndrome during CPB [194, 195]. In an RCT enrolling patients under angiotensin-converting enzyme inhibitors, methylene blue was effective for the prevention/treatment of vasoplegic syndrome (compared to saline), resulting in lower lactate levels during and after CPB [196]. In a similar patient population, vasopressin was effective in preventing/treating vasoplegic syndrome compared to saline [197]. The use of hydroxocobalamin has been reported as a rescue treatment for methylene blue-refractory cardioplegic syndrome during CPB [198]. The depth of anaesthesia should be checked and adequately adjusted before using vasodilators. Different intravenous vasodilating agents are available once the level of anaesthesia is guaranteed as adequate (sodium nitroprusside, nitroglycerin, milrinone, enoximone, phentolamine, urapidil). At present, the existing literature does not contain adequate information to provide recommendations on the choice of vasodilating agents.
7.7 Pump flow management
The target blood flow during CPB is traditionally determined according to BSA and temperature. Under moderate hypothermia-to-normothermic conditions, the pump flow rate is set between 2.2 and 2.8 l/min/m2 by the majority of perfusionists. However, this range may suffer from a number of limitations that recently emerged, including the use of BSA to determine pump flow rate. For example, the BSA may not be an adequate measure of the metabolic needs in obese patients [200], and lean body mass has been suggested as a more sensitive estimate of systemic metabolism [201]. In turn, the purpose of the pump flow is to fulfil the oxygen needs of the different organs [oxygen consumption (VO2)] through an adequate DO2; however, the DO2 is obtained from the product of the pump flow multiplied by the oxygen content, which derives from the Hb content (g/dl) and the Hb oxygen saturation (SaO2). Therefore, recent studies suggest determining the adequate pump flow based not only on BSA and temperature but also on the DO2 [199, 202–204].
7.7.1 Description of the evidence
Retrospective and propensity-matched studies highlighted that patients suffering from postoperative AKI were treated at lower pump flows than patients without AKI [190, 199]. Older studies (anterior to 1990) did not find any association between pump flow and adverse cerebral, neurocognitive or renal outcomes [205–207].
At present, no RCTs have investigated the association between pump flow and outcomes. A retrospective study on conventional CPB (for the purpose of these guidelines, ‘conventional CPB’ is defined as CPB not fulfilling the definition of MiECC given in the text and the position paper of the Minimal invasive Extra-Corporeal Technologies international Society [31]) versus miniaturized CPB (MiECC) showed that patients treated with miniaturized CPB experienced a significantly lower pump flow rate but had significantly less haemodilution [208]. As a result, the DO2 was equivalent and the renal outcome was equivalent. However, the risk of developing stage 1 AKI was significantly and inversely associated with the DO2 in the pooled groups [208].
It is not possible to produce recommendations on the optimal pump flow rate when this index is considered alone. However, low values of mixed venous oxygen saturation (SvO2), DO2, NIRS and high values of the oxygen extraction ratio (O2ER) and lactates during CPB are markers of inadequate perfusion associated with adverse outcomes [209–211]. A large retrospective study showed that a strategy focused on maintenance of an SvO2 >75% resulted in a lower rate of stage 1 AKI in patients reaching the goal [212].
Pump flow rate adjustment based on the Hb content in order to maintain an adequate DO2 (‘goal-directed perfusion’) was effective in reducing the AKI rate in a propensity-matched prospective study [199]. A recent RCT confirmed the efficacy of goal-directed perfusion over conventional perfusion in reducing the rate of stage 1 AKI (RR 0.45, 95% CI 0.25–0.83; P = 0.01) [213].
Recommendations for control of mean arterial blood pressure during cardiopulmonary bypass
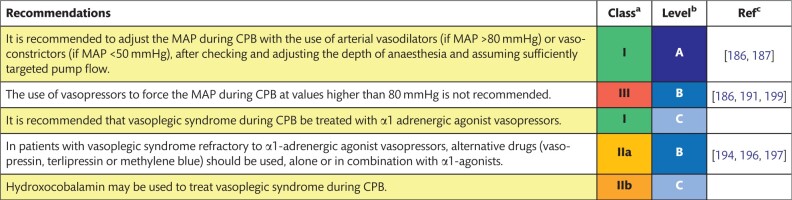
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass; MAP: mean arterial pressure.
Recommendations for pump flow management during CPB
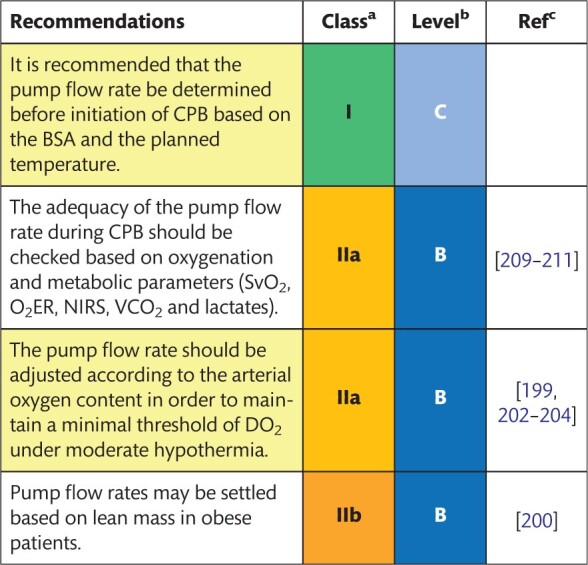
|
Class of recommendation.
Level of evidence.
References.
BSA: body surface area; CPB: cardiopulmonary bypass; DO2: oxygen delivery; NIRS: near-infrared spectroscopy; O2ER: oxygen extraction ratio; SVO2: mixed venous oxygen saturation; VCO2: carbon dioxide production.
7.8 Pulsatile and continuous flow
All over the world, the majority of CPB procedures are run with a continuous flow (with roller or centrifugal pumps). A pulsatile flow during CPB may be generated by modified conventional pumps or by specifically designed pulsatile pumps. However, there is no universal definition of pulsatile perfusion and its quantification. A correct quantification should be based on an energy gradient rather than on a pressure gradient [70, 214, 215]. The inhomogeneity of definitions and the quantification of pulsatile flow make it challenging to compare different studies and, moreover, to pool different studies on pulsatile versus continuous flow. A limited number of RCTs are available, which have been pooled in different (but similar) meta-analyses [216–218].
7.8.1 Description of the evidence
Meta-analyses of RCTs have found that patients treated with pulsatile flow had a better renal outcome, as characterized by a lower rate of acute renal insufficiency (RR 0.52, 95% CI 0.39–0.68), a better-preserved creatinine clearance rate and lower values of arterial blood lactates postoperatively [216, 217].
Another meta-analysis that included 9 RCTs investigated pulmonary function and general outcome in patients receiving pulsatile versus non-pulsatile perfusion [218]. Only 2 studies contained respiratory indices [pulmonary compliance, ratio of arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FiO2), chest radiography score], and the findings favoured pulsatile perfusion for all the indices. The same article addressed clinical outcomes that were presented in 3–4 RCTs and found that pulsatile flow was associated with shorter intubation time and shorter stays in the ICU and hospital. The need for non-invasive ventilation was lower in patients treated with the pulsatile flow (RR 0.48, 95% CI 0.36–0.63). Additionally, other RCTs found beneficial effects of the pulsatile flow in terms of micro or macro haemodynamics [219–221].
Several RCTs showed beneficial effects on splanchnic perfusion and the inflammatory reaction by adding an intra-aortic balloon pump to the CPB circuit, which creates pulsation directly inside the body of the patient [222, 223]. In the evaluation of pulsatile perfusion, the main problem when pooling studies on pulsatile perfusion is the vast heterogeneity in definitions, which results in relatively large publication bias. However, data from the RCTs converge in identifying beneficial pulmonary and renal effects.
Recommendation for the type of cardiopulmonary bypass pump flow
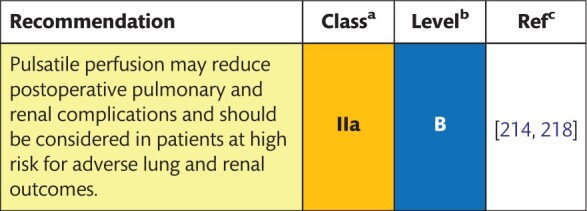
|
Class of recommendation.
Level of evidence.
References.
7.9 Goal-directed haemodynamic therapy
Perioperative optimization of the balance between DO2 and VO2 is a cornerstone of the management of patients undergoing cardiac surgery. DO2 in patients being operated on CPB may be decreased due to numerous factors, including myocardial depression, rhythm disturbances and impaired vascular tone [224]. Goal-directed haemodynamic therapy (GDT) is a strategy based on increasing cardiac output by using fluids and/or inotropes to improve DO2 to the tissues [225].
7.9.1 Description of the evidence
Numerous RCTs have been conducted to assess the influence of a goal-directed protocol on clinical outcomes, including death [226–230]. In a prospective, controlled, parallel-arm and open-label trial, 100 patients who were to undergo CABG and/or aortic valve replacement were randomized to receive GDT (study group) or standard care (control group) [226]. It was shown that early (after induction of anaesthesia) GDT—based on cardiac index, stroke volume variation and an optimized global end-diastolic volume index—resulted in a reduced incidence of postoperative complications (study group vs control group: 40 vs 63; P = 0.004) and shortened the length of stay in the ICU (study group vs control group: 42 ± 19 h vs 62 ± 58 h; P = 0.018).
An RCT combined with a systematic review was designed to investigate the effect of GDT on outcomes in high-risk cardiac surgical patients [EuroSCORE >6, left ventricular ejection fraction <50%, recent acute MI or high-risk unstable angina (<14 days) or combined cardiac surgical procedure] [228]. Patients were randomized into a GDT group (n = 62) or a standard care group (n = 64). In the GDT group, intravenous fluids, inotropes and PRBC transfusions were used to maintain a cardiac index of >3.0 l/min/m2. The primary outcomes comprised the 30-day mortality rate and the number of major postoperative complications, which were reduced in the GDT group (27.4% vs 45.3%; P = 0.037). A meta-analysis of 6 trials showed that, when compared with standard treatment, GDT significantly reduced the overall rate of postoperative complications and the length of hospital stay. However, no significant difference in the postoperative mortality rate was observed for GDT (9 of 410, 2.2%) compared with standard care (15 of 415, 3.6%; OR 0.61, 95% CI 0.26–1.47; P = 0.27). A more recent meta-analysis of 9 trials (1148 patients) showed that GDT significantly reduced the length of hospital stay [231].
Recommendation for perioperative haemodynamic management

|
Class of recommendation.
Level of evidence.
References.
GDT: goal-directed haemodynamic therapy.
7.10 Assisted drainage
The use of vacuum-assisted venous drainage (VAVD) has been developed in paediatric cardiac surgery and during minimally invasive cardiac procedures. VAVD is now often used in standard CPB. A dedicated vacuum controller is connected to the lid of the hard-shell venous reservoir to enhance the venous return from the patient. Alternatively, negative pressure may be generated by using a centrifugal pump between the venous cannula and the reservoir [232].
7.10.1 Description of the evidence
The main advantage of VAVD is the increased venous return compared to gravitational drainage, allowing the use of a smaller cannula that increases visibility in a narrow operative field [233]. Moreover, the reservoir can be positioned closer to the patient, allowing for a marked reduction in priming volume [234]. On the other hand, several risks have been associated with the use of VAVD. In a recent survey on the use of VAVD, the risks identified consisted of pressurized venous reservoirs, air introduction through the membrane oxygenator and non-functional VAVD devices [235], emphasizing the need for initial safety checks and monitoring. The increase in the combined negative pressureon the venous reservoir by combining VAVD with gravity drainage may increase the risk of haemolysis [232]. A trial for adult cardiac patients comparing gravity drainage to different vacuum levels showed that haemolysis was increased at −80 mmHg compared to −40 mmHg or gravity drainage [236]. Furthermore, GME formation is associated with increased negative pressure in VAVD [237]. Although VAVD seems to be safe under the circumstances with controlled negative pressures, clinical air embolism has been described [232].
Recommendations for use of assisted venous drainage
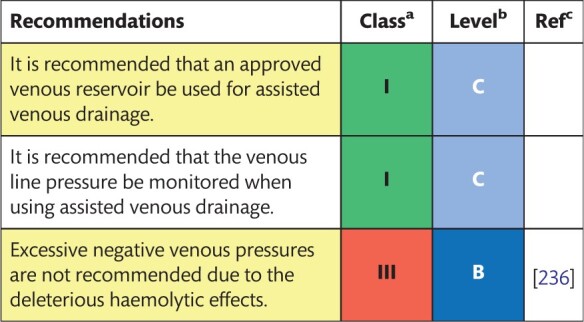
|
Class of recommendation.
Level of evidence.
References.
7.11 Strategies for transfusion of blood products
PRBCs and fresh frozen plasma (FFP) transfusions may be required during CPB, whereas usually no role exists for platelet or cryoprecipitate transfusions during CPB. PRBCs are typically transfused when the Hb values fall below a threshold considered critical for adequate DO2. When considering PRBC transfusions in other scenarios, this threshold is difficult to identify based on absolute values, and it should be individualized based on the measured DO2 and on indices of oxygen extraction (SvO2 and O2ER). Low values of Hb during CPB have been associated with adverse outcomes in many studies [238–240], and this concept raised the hypothesis of a more liberal transfusion trigger during CPB; however, in the presence of a low Hb value, the DO2 is preserved by increasing the pump flow [203]. FFP has been used during CPB as a source of antithrombin for patients with poor heparin responsiveness. However, the use of antithrombin concentrates is an effective way to treat this condition, avoiding the use of FFP.
7.11.1 Description of the evidence
7.11.1.1 Packed red blood cell transfusions
Few RCTs have compared different Hb or HCT trigger values for RBC transfusions during CPB. In a small RCT [241], patients with an HCT during CPB between 21% and 25% were randomized for receiving or not receiving RBC transfusions. The results suggest that non-transfused patients had similar renal outcomes. An RCT of liberal versus restrictive transfusion protocols, inclusive of RBC transfusions for an Hb <7.0 g/dl during CPB in the restrictive group and <9.5 g/dl in the liberal group, resulted in more substantial transfusions for the liberal group but more adverse events in the restrictive group [242]. However, this study included transfusion strategies after CPB. A retrospective study showed that, during CPB, PRBC transfusions are effective if the SvO2 is <68% and/or the O2ER is >39% [243].
Existing guidelines suggest transfusing PRBCs if the Hb is <6.0 g/dl [244] and an acceptable HCT value between 21% and 24% if the DO2 is maintained above 273 ml/min/m2 [2].
7.11.1.2 Fresh frozen plasma transfusions
FFP during CPB has the sole indication of supplementing antithrombin in patients with poor heparin responsiveness. However, RCTs and existing guidelines demonstrated that antithrombin concentrate is more effective than FFP in restoring heparin responsiveness and allows a reduction in FFP transfusions and volume overload [2, 244–247]. Prophylactic use of FFP to decrease perioperative bleeding is ineffective and should be abandoned [248, 249].
Recommendations for transfusion management during cardiopulmonary bypass
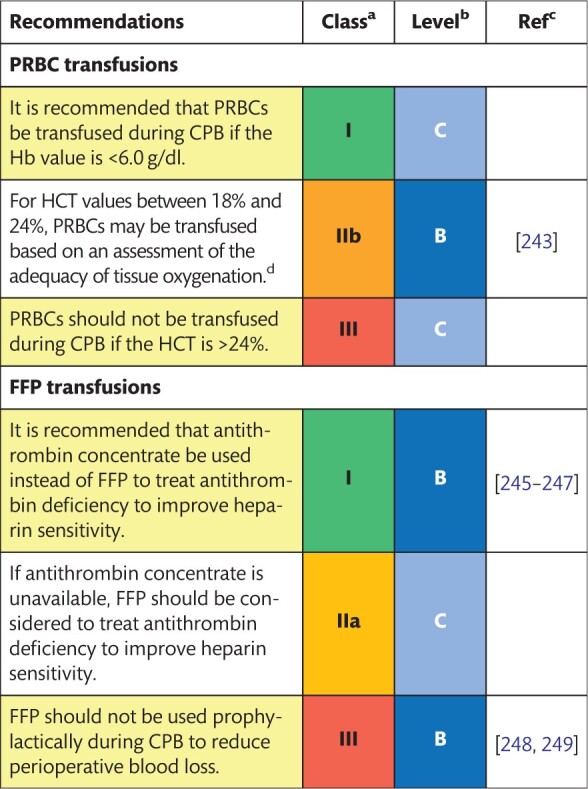
|
Class of recommendation.
Level of evidence.
References.
The DO2 is maintained at >273 ml/min/m2 and cerebral oximetry is satisfied.
CPB: cardiopulmonary bypass; FFP: fresh frozen plasma; Hb: haemoglobin; HCT: haematocrit; PRBCs: packed red blood cells.
7.12 Anaesthesia and pharmacological treatment during cardiopulmonary bypass
CPB is associated with significant changes in the pharmacokinetics and pharmacodynamics of anaesthetic drugs. Causes include priming-induced haemodilution and reduced plasma protein concentrations, hypothermia-induced altered drug clearance and drug sequestration during lung isolation [250]. These alterations demand particular expertise by cardiac anaesthesiologists regarding sedation and anaesthetic depth, analgesia and neuromuscular blockade. Other aspects that should be considered during anaesthesia include corticosteroids and glycaemic control, which are discussed at the end of this chapter. Haemodynamic drugs, coagulation-related drugs and serum electrolytes are discussed in other sections.
7.12.1 Volatile anaesthetics
RCTs have shown that volatile anaesthetics used to maintain general anaesthesia during cardiac surgery and also during CPB have the potential to improve postoperative morbidity and mortality rates [251, 252]. However, a recent large international multicentre RCT in 36 centres, including 5400 patients undergoing elective CABG surgery, showed that the use of a volatile agent did not reduce the rate of all-cause death at 1 year compared to total intravenous anaesthesia (2.8% vs 3.0%; P = 0.71). The discussion of this lack of protection included the fact that patients in this trial had a relatively low risk for ischaemia reperfusion injury and that propofol was co-administered in the volatile anaesthetic group [253].
Haemodilution and hypothermia counterbalance each other during most phases of CPB, with hypothermia increasing the blood/gas partition coefficient and haemodilution decreasing it. During rewarming, however, the increase in temperature is faster than the increase in HCT, resulting in a lower blood/gas partition coefficient and thus in increased wash-in and more rapid increase in depth of anaesthesia [254, 255]. The effect during rewarming, i.e. reduced blood/gas partition coefficient and faster wash-in, is subsequently reversed towards the end of CPB.
It is of note that the effects of temperature and HCT described previously were assessed with prime volumes of 2 l or more and a drop in temperature to about 30°C [255]. Therefore, these effects will be less pronounced with the CPB techniques used today, which include lower prime volumes and the use of milder degrees of systemic hypothermia or even normothermia.
Using EEG-based bispectral index (BIS) monitors and auditory-evoked responses as a measure for depth of anaesthesia indicates that the requirements of volatile anaesthetics are temperature dependent, with a lower requirement during systemic hypothermia and a higher requirement during rewarming [256, 257].
However, the use of EEG-based BIS monitors as a surrogate for depth of anaesthesia during CPB may have limitations, because a burst-and-suppression EEG pattern in anaesthetized and hypothermic patients might correlate with high (awake) BIS values, and there is a high variability of BIS values below 32°C. It has been shown that the BIS value is reduced by about 1.2 units per 1°C reduction [258, 259].
Volatile anaesthetics cross the conventional and commonly used microporous polypropylene hollow fibre membrane oxygenator. During CPB, the concentration of the volatile anaesthetic in the oxygenator exhaust line should be monitored [256]. It has been demonstrated that this concentration correlates well with the arterial concentration [250, 260], although others dispute this [250]. During CPB, isoflurane and sevoflurane can cause hypotension by vasodilation. This effect may add to the vasodilatation during prolonged CPB.
Nitrous oxide is highly insoluble in blood and can therefore enlarge air bubbles [261]. Therefore, its use immediately before and after CPB may result in potential adverse effects on neurological outcome through the expansion of gaseous emboli. Apart from the reduction of MAP, heart rate, stroke volume and cardiac output, the cardiovascular effects of nitrous oxide after CPB include the induction of regional wall motion abnormalities and possibly diastolic dysfunction [262].
7.12.2 Intravenous anaesthetics and opioids during cardiopulmonary bypass
There is widespread use of total intravenous anaesthesia for the maintenance of general anaesthesia in cardiac patients, particularly in Europe [250]. During CPB, there will be a reduction of the total concentration of intravenous anaesthetic drugs due to haemodilution. However, propofol and opioids are highly protein bound and, therefore, with haemodilution-induced lower blood concentrations of proteins (such as albumin), their unbound and pharmacodynamically active free fractions will increase, offsetting the haemodilution-induced reduced drug concentrations [263–266].
In addition, hypothermia, decreased microcirculatory flows and reduced organ perfusion during CPB affect hepatic metabolism and renal clearance, resulting in prolonged elimination half-lives of anaesthetics and leading to small increases in blood levels of propofol and opioids.
Based on the temperature-dependent Hofmann elimination of remifentanil, a remifentanil infusion can be reduced after initiation of CPB by about 30% for each 5°C drop in temperature. The dose reduction can start immediately after initiation of CPB if the patient is cooled to 27°C and after 20 min if he/she is cooled to 32°C, because it takes about 20–30 min for the reduced temperature-induced reduction in metabolism by Hofmann elimination to offset the haemodilution-induced reduction in plasma levels [265].
During lung isolation, opioids such as fentanyl and sufentanil have been shown to sequester in the lungs, resulting in increased plasma levels of these drugs during separation from CPB [263, 264]. Similar to volatile anaesthetics, during CPB, propofol may cause hypotension by vasodilation.
7.12.3 Neuromuscular blocking agents
Historically, pancuronium was used as a neuromuscular blocker in cardiac anaesthesia due to its vagolytic actions, reducing the incidence of bradycardia during induction.
The recent 5th National Audit Project in the UK, which assessed accidental awareness during general anaesthesia (AAGA), confirmed a high risk for AAGA in cardiac anaesthesia. It also confirmed that AAGA is associated with the use of neuromuscular blocking agents, particularly in cardiac anaesthesia; this finding would support the use of short-acting neuromuscular blockers [267]. In addition, fast-tracking patients and enhanced recovery protocols after cardiac surgery would also support the use of short-acting neuromuscular blockade during induction only.
Atracurium and rocuronium were used in 90% of cases in the 6th National Audit Project in the UK, which reported the incidence of life-threatening allergic reactions during anaesthesia and surgery. The incidence of anaphylactic reactions was 4.2/100 000 administrations with atracurium [268]. The risk of an anaphylactic reaction, if the risk of atracurium is equal to 1, is 1.42 for rocuronium and 0.78 for mivacurium.
7.12.4 Corticosteroids
Two multicentre RCTs assessed whether the outcome could be improved with high doses of intraoperative corticosteroids [269, 270]. The Dexamethasone for Cardiac Surgery (DECS) trial randomized 4494 patients with 1 single intraoperative dose of dexamethasone 1 mg/kg given to patients in the treatment group. The incidence of the primary outcome, which was a composite of postoperative death, cardiac, renal, respiratory or cerebral adverse events, was lower in the study group (7% compared to 8.5% in control patients) but without statistical significance (P = 0.07) [269].
The more recent Steroids in Cardiac Surgery (SIRS) trial randomized 7507 patients to receive 500 mg of methylprednisolone intraoperatively. The results were also neutral, with no reduction in the postoperative mortality rate at 30 days (with 4% in the treatment group vs 5% in the control group) and no change in the risk of death or major morbidity (with an incidence of 24% in both groups) [270].
Based on these 2 large neutral RCTs, one can, therefore, conclude that routine intraoperative corticosteroids do not affect postoperative mortality or morbidity rates. A recent systematic review and meta-analysis including 56 RCTs and 16 013 patients confirmed an unclear effect on the mortality rate. In addition, it demonstrated an increased risk of myocardial injury with perioperative corticosteroids but also a lower risk of new onset AF [271]. The hypothesis that patients younger than 75 years might benefit from corticosteroids in cardiac surgery is currently being investigated in a large RCT [272]. The potentially beneficial pulmonary effects of perioperative dexamethasone are discussed in Section 7.15.
7.12.5 Glycaemic control
There is a high incidence of hyperglycaemia in patients during CPB due to (i) a high prevalence of diabetes mellitus in patients presenting for heart surgery, (ii) surgery- and CPB-associated inflammation and stress and (iii) the use of positive inotropes. The degree of intraoperative glycaemic control is controversial. Tight control of blood glucose levels may be associated with a lower mortality rate and fewer adverse outcomes including AF, the requirement of epicardial pacing and shorter durations of mechanical ventilation and ICU stay [273]. However, tight control of glucose levels may induce hypoglycaemia, which is associated with an increase in morbidity and mortality rates. Whether the benefit of tight glucose control outweighs the risks of hypoglycaemia remains unclear. Recently, it was suggested that patients with diabetes can be managed with a more liberal glycaemic control strategy, with blood glucose levels up to 10 mmol/l, whereas management of patients who do not have diabetes may be beneficial if the blood glucose level is kept at <7.8 mmol/l [274].
Recommendations for anaesthesia and pharmacological management
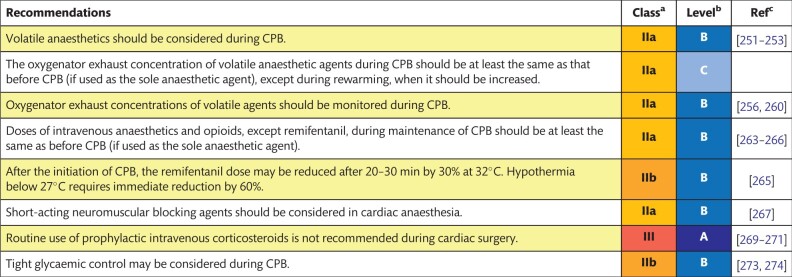
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
7.13 Cardioplegia
Protection of myocardial function from ischaemic damage during CPB and the ability to provide a quiet and bloodless operative field are the main goals of cardioplegia techniques. The standard technique for the induction of cardiac arrest includes the delivery of a high concentration of potassium of 8–20 mEq/l by either crystalloid or blood carrier solutions to the myocardium, leading to fast inactivation in the sodium channels and thereby inducing depolarized arrest. The composition of cardioplegia solutions varies considerably, but they are generally divided into 2 distinct categories: pure crystalloids or blood-to-crystalloid mixtures. Pure crystalloid solutions may be of either the intracellular or extracellular type, whereas conventional blood cardioplegia is a mix of both crystalloid solution and blood, typically in a ratio (4:1) of 4 parts of blood to 1 part of crystalloid [275]. Moreover, the blood mixtures include del Nido cardioplegia [which contains 1 part of blood to 4 parts of crystalloids (1:4) with the addition of lidocaine to prolong the hyperpolarization lifetime] together with microplegia [which delivers cardioplegia with a minimal crystalloid solution in a ratio of at least 66 parts of blood to 1 part of crystalloid (66:1) or no crystalloid at all].
7.13.1 Description of the evidence
Several experimental studies favour the use of blood cardioplegia over crystalloid solutions when comparing the release of cardiac enzymes and metabolic response. Nevertheless, the 2 largest clinical trials in the field showed no statistical differences in terms of major or minor postoperative clinical outcomes between crystalloid or blood cardioplegia among 1140 randomized patients who underwent CABG [276] and 345 patients after aortic valve replacement [277]. Furthermore, a systematic review and meta-analysis of 34 RCTs that compared crystalloid with blood cardioplegia in 5044 patients found no difference between the groups regarding the rates of perioperative MI and death; however, a significantly lower incidence of low cardiac output syndrome (LCOS) was observed immediately upon reperfusion with blood cardioplegia [278]. A more recent meta-analysis of 36 RCTs showed similar results in terms of in-hospital death (RR 0.96, 95% CI 0.60–1.51; P = 0.83) or perioperative MI (RR 0.79, 95% CI 0.55–1.12; P = 0.12), but the difference in LCOS disappeared after the inclusion of more recent studies (RR 0.69, 95% CI 0.48–1.04; P = 0.072) [279].
Although the difference in outcomes between crystalloid and blood cardioplegia has been studied extensively, most of the studies did not report the risk of bleeding complications and transfusion rates. In an RCT including 100 patients, crystalloid cardioplegia was compared to blood cardioplegia and was associated with significantly higher intraoperative haemodilution, greater blood loss and more PRBC transfusions [280]. Moreover, in the recently published 2017 EACTS/EACTA guidelines on patient blood management [2], the limitation of haemodilution has been recognized as a vital part of a blood conservation strategy to reduce bleeding and perioperative transfusion requirements (class IB recommendation). Thus, due to limited crystalloid fluid content, the use of blood cardioplegia solutions should be considered as the preferred strategy in patients with anaemia, low BSA and chronic kidney disease or patients undergoing complex procedures to reduce haemodilution and the risk of subsequent complications including AKI, bleeding and the need for transfusions perioperatively.
The most commonly used mode of application for cardioplegia is antegrade, applied directly into the aortic root proximal to the aortic cross-clamp at a pressure of 60–100 mmHg or infused directly into the coronary ostia with pressure monitoring. Retrograde cardioplegia is administered via direct insertion of a catheter into the coronary sinus, using a flow of 200–400 ml/min to a coronary sinus pressure of between 30 and 50 mmHg [281]. Higher pressures should be avoided to prevent coronary venous system injury [281]. Induction of cardiac arrest is usually slower with retrograde than with antegrade cardioplegia, often 2–4 min instead of 30–60 s, but it should be noted that experimental results indicate that the flow to the microvasculature of the right ventricle is inadequate during retrograde cardioplegia and, therefore, the protection of the right ventricle might be incomplete [282]. In more complex cases, where the cross-clamp time is extended or severe coronary disease with poorly developed collaterals or aortic valvular insufficiency is present, antegrade plus retrograde cardioplegia can be used to ensure adequate distribution of the cardioplegia [283, 284].
Usually, cardioplegia is administered cold and intermittently every 20–30 min to maintain cardiac arrest and hypothermia; however, a single-shot cardioplegia may also be applied in low-risk cases with short aortic clamp times. A single-shot approach, often using intracellular crystalloid solutions or the del Nido solution, minimizes interruptions during the surgery for repeated administration of cardioplegia and also facilitates less invasive procedures. Although the interest in these methods has been continuously growing, the evidence to support their use in daily practice in high-risk operations is insufficient due to a lack of adequately powered RCTs to prove their superiority over conventional approaches [285]. The most recent systematic review and meta-analysis, which compared the del Nido solution with conventional approaches in adult patients undergoing cardiac surgery, included 9 observational studies and small RCTs (n = 1501). This meta-analysis showed that the use of the del Nido solution did not result in the reduction of the mortality rate (RD 0, 95% CI −0.01 to 0.01; P = 0.53), a lower release of postoperative myocardial enzymes (standardized mean difference −0.16, 95% CI −0.41 to 0.08; P = 0.18) or reduced length of hospital stay (standardized mean difference −0.10, 95% CI −0.26 to 0.05; P = 0.18) [286].
The warm or tepid blood cardioplegic approach was developed for use in patients with acute MI and to enhance the recovery of contractile function after hours of ischaemia [287]. The less commonly used method is an infusion of continuous warm or tepid cardioplegia through the coronary sinus. In the meta-analysis of 41 RCTs with 5879 patients, in-hospital deaths, length of stay, incidence of stroke and AF and the use of an intra-aortic balloon pump were compared and did not differ between warm versus cold cardioplegia groups [288]. However, warm cardioplegia was associated with a significantly better postoperative cardiac index and lower cardiac enzyme release. In a large prospective study comparing early and late outcomes of patients receiving tepid/warm or cold cardioplegia during isolated CABG, adjusted perioperative mortality rates were not different (OR 1.45, 95% CI 0.95–2.22; P = 0.09) but patients in the cold blood cardioplegia group had 1.86 times higher adjusted odds for having MI compared with the patients in the warm cardioplegia group (OR 1.86, 95% CI 1.36–2.53; P < 0.001) [289]. A drawback of warm or tepid cardioplegia is that the poor distribution or interruption of normothermic cardioplegia may induce anaerobic metabolism and warm ischaemic injury. Therefore, normothermic cardioplegia must be delivered continuously and homogeneously, which explains its relatively limited popularity [275]. Small RCTs have indicated some benefits regarding myocardial metabolic derangements with the use of warm blood-controlled reperfusion (‘hot-shot’), often administered retrogradely at the end of a complex procedure, but this strategy requires further validation [290].
Recommendations for control of ischaemic cardiac arrest
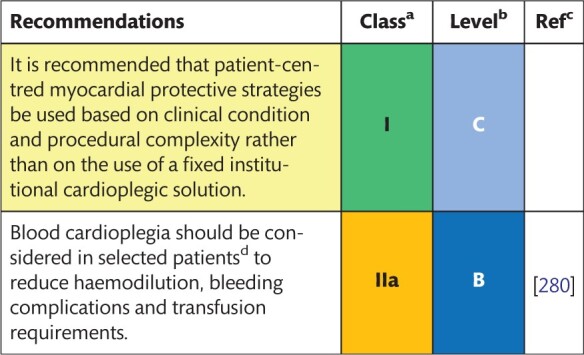
|
Class of recommendation.
Level of evidence.
References.
Patients with anaemia, low body surface area, chronic kidney disease or undergoing complex procedures.
7.14 Lung protection
Respiratory failure is a common complication after cardiac surgery, with an incidence of 9% and a 6-fold increase in the mortality rate compared to patients without respiratory failure [291]. CPB activates inflammatory and oxidative stress pathways, resulting in pulmonary ischaemia reperfusion injury. Apart from CPB, causes of respiratory failure include median sternotomy, dissection of the internal mammary artery, local cooling for myocardial protection and transfusion of blood products. Intraoperative strategies to reduce cardiac surgery-associated lung injury include CPB modifications, continuous positive airway pressure and/or ventilation during CPB and pharmacological interventions.
7.14.1 Description of the evidence
7.14.1.1 Cardiopulmonary modifications
Biocompatible modifications of circuits are designed to mimic endothelial surfaces by coatings, including heparin, poly(2-methoxyethyl acrylate), synthetic protein and phosphorylcholine. A single-centre RCT of 78 patients undergoing CABG compared biocompatible coated circuits with an uncoated control group and demonstrated that biocompatible coatings resulted in fewer inflammatory responses and less oxidative stress [292]. A systematic review and meta-analysis assessing 4360 patients in 36 trials and clinical outcomes found no differences in postoperative lung dysfunction and mechanical ventilation times when biocompatible bypass circuits were compared with uncoated circuits. There was, however, a significantly shorter duration of stay in the ICU when biocompatible bypass circuits were used. However, heterogeneity of different biocompatible modifications was noted, with 78% of trials using heparin-bonded surfaces only [108].
7.14.1.2 Leucocyte filtration
Activated leucocytes play a crucial role in inflammatory lung damage. The effect of systemic leucofiltration on the pulmonary injury after CPB has been assessed in a meta-analysis that included 995 patients in 21 studies. Results revealed that short-term pulmonary outcomes, such as oxygenation at 12 h after CPB, were improved but not at 24 h. Postoperative ventilation times were also reduced. However, lengths of stay in critical care and the hospital were unchanged. There was high heterogeneity among RCTs [293]. A more recent, small single-centre RCT compared inflammation and lung function in 30 patients with leucocyte filtration in the cardiotomy suction, showing no evidence of improved pulmonary function when leucocyte filters were used [294]. Another RCT in 60 patients with mild-to-moderate lung dysfunction assessed systemic and cardioplegic leucocyte filtration. Whereas the postoperative ventilation time was shorter in the intervention group, there were no differences in pulmonary complications such as pneumonia and acute lung injury [295]. A potentially unwanted effect of leucocyte filtration is that it results in increased neutrophil elastase levels in patients. Elastase hydrolyses proteins and plays a crucial role in inflammatory lung tissue injury [296].
7.14.1.3 Modified ultrafiltration
MUF includes the removal of fluids and low-molecular-weight substances at the end of CPB. This technique was assessed in an RCT of 573 patients, and it was associated with significantly decreased numbers of patients with postoperative respiratory failure [297]. A more recent small RCT of 37 patients suggested that the MUF decreased airway resistance postoperatively [298]. However, a large prospective RCT is necessary to find out whether MUF has an impact on meaningful long-term clinical pulmonary outcomes.
7.14.1.4 Pulmonary artery perfusion
Two single-centre RCTs assessed selective pulsatile pulmonary perfusion with oxygenated blood during CPB in 64 and 30 patients, respectively. On the one hand, this technique demonstrated a reduction of lung tissue inflammation with lower neutrophilic/lymphocytic alveolar infiltration in the bronchoalveolar lavage and improved oxygenation and lung compliance immediately after the operation. However, circulating cytokine levels were unaffected, and the effect on meaningful long-term clinical pulmonary outcomes remains open [299, 300]. Another more recent small RCT assessed selective pulmonary perfusion with cold (2°C) venous blood during CPB in 59 patients with chronic obstructive pulmonary disease; the study demonstrated a non-significant trend towards a shorter ventilation time and stay in the ICU in the treatment group [301].
7.14.1.5 Minimally invasive extracorporeal circulation
Features of MiECC are described in Section 7.1. MiECC includes a small priming volume, a closed system, a centrifugal pump and a biocompatible coated system. No venous reservoir is used. A recent systematic review and meta-analysis of RCTs including 2770 patients in 24 studies showed that MiECC was associated with shorter durations of postoperative mechanical ventilation and shorter ICU stays. However, different minibypasses were assessed, and outcome results did not include meaningful longer-term outcomes beyond the discharge of patients [130].
7.14.1.6 Continuous positive airway pressure and ventilation during cardiopulmonary bypass
Whether continuous positive airway pressure or ventilation during CPB can protect the lungs has been assessed in a meta-analysis and semi-quantitative review of 16 RCTs and 814 patients. Results demonstrated that continuous positive airway pressure or vital capacity manoeuvres during CPB improve oxygenation variables directly after CPB. However, improved oxygenation was not sustained, and clinical outcomes were unchanged. Besides, the methodological quality of the RCTs in this meta-analysis was graded as low [302]. A multicentre RCT of 870 patients is planned to address this question, with patients randomized to receive no mechanical ventilation, continuous positive end-expiratory pressure or low minute volume ventilation with a continuous positive end-expiratory pressure during CPB. The primary end point will be the incidence of respiratory failure until discharge from the critical care unit [303].
7.14.2 Pharmacological interventions
7.14.2.1 Hyperoxia
Exposure of the alveolus to 100% oxygen leads to alveolar collapse and the generation of oxygen radicals, which might exacerbate ischaemia-reperfusion injury after CPB. Small RCTs assessed the effect of hyperoxia on postoperative ventilation times, with conflicting results, demonstrating prolonged ventilation times with intraoperative hyperoxia in 1 RCT but not in others [304]. The lengths of the stays in the critical care unit and in the hospital were not affected [304].
7.14.2.2 High-dose dexamethasone
A large multicentre RCT, where 4494 patients were randomized to receive high-dose dexamethasone (1 mg/kg), demonstrated a significant improvement in lung protection relevant secondary outcome variables: incidence of prolonged ventilation (>24 h), with 3.4% in the dexamethasone group compared to 4.9% in the placebo group; and postoperative pneumonia in the treatment group, with a reduction from 10.6% to 6%. However, the primary outcome, which was the 30-day incidence of major adverse events, was similar in both groups [269].
Recommendations for lung protection during cardiopulmonary bypass
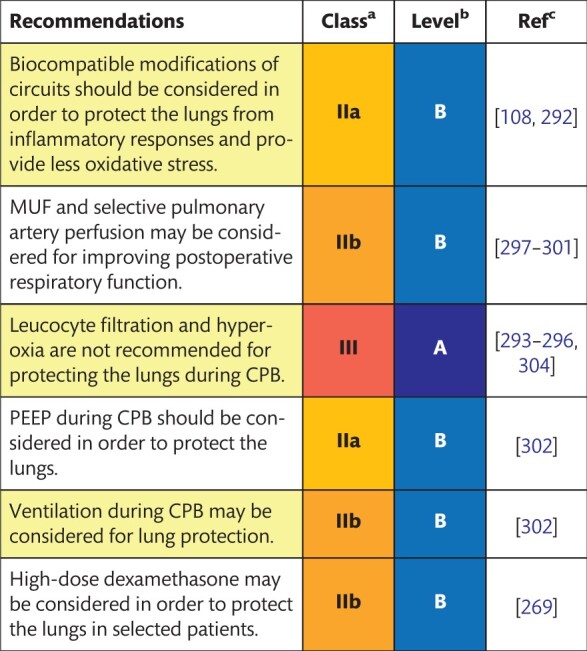
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass; MUF: modified ultrafiltration; PEEP: positive end-expiratory pressure.
7.15 Non-invasive cerebral monitoring
Despite significant improvements in CPB technology and anaesthetic techniques, neurological complications remain a concern. Adverse cerebral outcomes after cardiac surgery are associated with increased mortality rates, prolonged ICU and hospital stays and the use of additional hospital resources. Hence, the choice of an optimal monitoring tool for the early diagnosis of deteriorating neurological function is required to improve surgical outcomes.
7.15.1 Description of the evidence
7.15.1.1 Near-infrared spectroscopy
Several studies claim that the magnitude and duration of cerebral oxygen desaturation are associated with early postoperative neuropsychological dysfunction and a prolonged hospital stay after cardiac surgery [211, 305]. The use of NIRS-based algorithms intended to improve the cerebral oxygen supply/demand ratio to improve clinical outcomes is currently undergoing extensive research. In a landmark study, 200 patients undergoing on-pump CABG were randomized to receive either the NIRS-based algorithm or standard care intraoperatively [211]. Although there were no differences in the overall incidence of complications, the rates of major organ morbidity and mortality were significantly lower in patients treated using the NIRS-based algorithm. An improvement in neurocognitive function was also observed in the interventional group according to the results of several studies [306, 307].
However, 2 recent high-quality trials that included patients with a high risk of complications [308, 309] and a recently published meta-analysis and systematic review of 1466 patients from 10 randomized controlled studies showed no clinical benefit of the use of NIRS-based algorithms [310]. These results clearly contradict previously published evidence.
7.15.1.2 Monitoring of depth of anaesthesia
Intraoperative awareness, although rare, negatively influences the neuropsychological status of patients after surgery. Processed EEG monitors are widely used to reduce the incidence of recall during surgery. No studies have specifically focused on patients undergoing surgical procedures requiring CPB. In a prospective study, 2000 patients (26.5% had planned open-heart surgery) were randomly assigned to EEG-derived BIS-guided anaesthesia (target BIS range, 40–60) or end-tidal anaesthetic gas concentration-guided anaesthesia (target end-tidal anaesthetic gas range, 0.7–1.3 minimum alveolar concentration) [311]. The authors found no differences in intraoperative awareness or in the need for volatile anaesthetics between the 2 groups. It is of note that only 2 cases of intraoperative awareness in each group were reported. The results of a later randomized study that analysed 5713 patients confirmed these results [312]. According to the results of a meta-analysis and systematic review, BIS-guided anaesthesia can reduce the risk of intraoperative awareness in surgical patients at high risk for awareness compared to the use of clinical signs as a guide for anaesthetic depth [313]. BIS-guided and end-tidal anaesthetic gas-guided anaesthesia may provide equivalent protection against intraoperative awareness.
7.15.1.3 Transcranial Doppler
Transcranial Doppler monitoring is used in patients undergoing cardiac surgery under CPB to detect the velocity and the direction of cerebral blood flow. Due to several disadvantages that limit the wide application of this technique, including the requirement for special equipment, the need for technical expertise and the challenges of identifying an acoustic window, transcranial Doppler is not discussed here in detail.
Recommendations for use of non-invasive cerebral monitoring
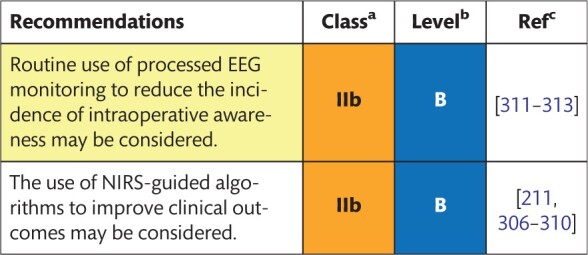
|
Class of recommendation.
Level of evidence.
References.
EEG: electroencephalography; NIRS: near-infrared spectroscopy.
7.16 Management of shed blood
Traditionally, shed blood—also known as cardiotomy suction blood, pleural and pericardial blood or wound blood—was aspirated back into the heart–lung machine via cardiotomy suckers. Over time, however, it was discovered that shed blood is highly activated and might be associated with thrombin generation, the activation of coagulation and fibrinolytic and inflammatory pathways and could contribute to higher transfusion requirements [2]. Moreover, reinfusion of shed blood is associated with neurological injury, cognitive decline and lung injury attributed in part to increased levels of haemolysis and fat in the scavenged blood and lung injury [314–316]. By collecting shed blood apart from the systemic blood that flows through the heart–lung machine, it becomes possible to handle this blood separately, e.g. with a cell saver, before returning it to the patient. In this way, it may be possible to reduce the pathological activation caused by shed blood.
7.16.1 Description of the evidence
During CPB, intraoperative autotransfusion, either with blood directly from the cardiotomy suction or processed using centrifugation to concentrate red cells, may be considered as part of a blood conservation programme [244]. Clinical studies comparing retransfusion of unprocessed versus discarded or processed shed blood report conflicting results regarding bleeding and transfusion requirements and neurological injury. It has been shown that processed or discarded shed blood is associated with decreased expression of markers for thrombin generation, platelet activation, inflammation, neuronal injury and decreased blood loss [314, 317–319]. However, contradictory findings showed more postoperative bleeding and transfusion requirements and no clinical evidence of any neurological benefit when shed blood was discarded or processed before transfusion [320–322].
In vitro laboratory assays for haemolysis, coagulation, inflammation and neurological injury in retransfusing shed blood show that this blood is severely contaminated. The extent to which this contamination has consequences for the clinical outcome is difficult to estimate. Based on current knowledge, it is justified to avoid retransfusion of unprocessed shed blood as much as possible. It is preferable, if reinfusion is necessary, to first process the shed blood with a cell saver and, thereafter, to filter it [2, 244, 314].
Shed blood can be collected separately in a suitable cardiotomy reservoir (dual chamber), a blood transfusion bag or in the reservoir of a cell saver. The best way to deal with shed blood depends on the volume of shed blood and the characteristics (e.g. BSA, preoperative HCT, Hb, platelet count) of the patient. For example, smaller volumes of shed blood may be discarded and medium volumes may be processed before returning it [317, 318]. With larger quantities, in most cases, the choice must be made to return shed blood to the patient because large volumes of cell-salvaged red blood cells may lead to an excessive loss of plasma and may result in impaired coagulation [2, 321].
It remains crucial that, during the operation, blood loss should be kept to a minimum. Preferably, the blood that is lost should be aspirated away as soon as possible. The longer the blood stays in the chest cavity, outside the bloodstream, the more activated it becomes [315, 322].
Research results in the area of shed blood management are difficult to interpret. On the one hand, the results often come from smaller, single-centre RCTs; on the other hand, the diversity in the quality of the studies is tremendous. Furthermore, it is unfortunate that no relevant review article has been published so far.
Recommendations for management of shed blood
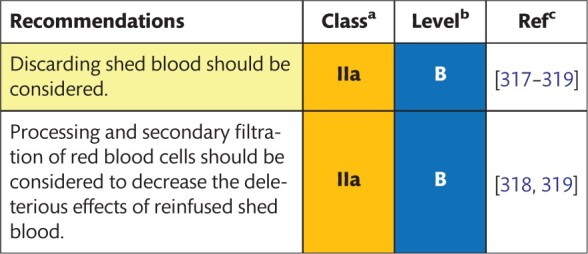
|
Class of recommendation.
Level of evidence.
References.
7.17 Minimally invasive surgery
A significant number of cardiac surgical units offer minimally invasive cardiac surgical procedures, mainly valve surgery, to selected patients. Specialized perfusion techniques are required to achieve the goal of minimal invasiveness. Peripheral cannulation, most often in the groin, is used instead of central access. This procedure necessitates the use of a special cannula, and, usually, vacuum-assisted drainage is applied. Moreover, the type of cardioplegia used has to be adjusted. Minimized perfusion circuits may be used instead of conventional circuits. Readers are referred to the dedicated chapters in this document on cannulas (Section 5.1) and the type of circuit (Section 7.1).
7.17.1 Description of the evidence
Clinical results of minimally invasive surgery have been evaluated in several modest clinical trials, and the results of individual studies are combined in meta-analyses. Most publications focus on a specific procedure, i.e. mitral valve surgery or aortic valve surgery. The most recent meta-analysis and systematic review on mitral valve surgery, based on a few RCTs and a more significant number of non-randomized evidence, suggests that minimally invasive surgery has some benefits, such as decreased bleeding, AF, sternal wound infection and length of stay in the ICU [323]. However, an increased risk for stroke, vessel injury including aortic dissection and increased procedure time were found [323].
There are a larger number of RCTs concerning aortic valve replacement. A meta-analysis on aortic valve replacement using a Bayesian network method revealed comparable clinical results between conventional and minimally invasive methods but confirmed longer procedure times for minimally invasive surgery [324]. However, groin or vascular access complications were not addressed in this meta-analysis. Few studies have been conducted to examine different perfusion strategies in minimally invasive cardiac surgery, but none of them are supported by the evidence from prospectively randomized settings. In a comparison between the use of the endoaortic balloon occlusion and transthoracic aortic clamping, neither of the techniques was found to be superior [325].
Recommendations for minimally invasive surgery
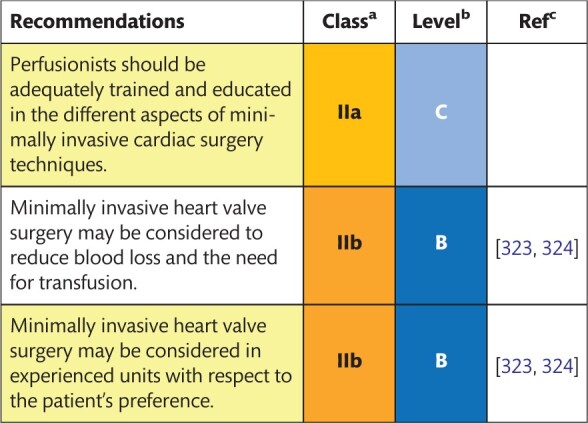
|
Class of recommendation.
Level of evidence.
References.
7.18 Emergency institution and reinstitution of cardiopulmonary bypass
Perfusionists regularly work in an urgent/emergent situation. They should always be prepared to institute and reinstitute CPB in life-saving settings, which can be either for an urgent or emergent procedure or reinstitution on CPB after weaning. Perfusionists can be best trained periodically for these emergencies through protocols and/or team simulation sessions.
7.18.1 Description of the evidence
There is no scientific evidence available with regard to the reinstitution of CPB in emergent situations, but common sense must prevail. For emergent procedures, always have a sterile set-up ready, be it primed or dry. For reinstitution on CPB after weaning, keep the extracorporeal circulation operable, with sterile tubing on the operating table, until the patient’s sternum has been closed. In case of urgent institution or reinstitution on CPB, it is of vital importance to make sure that the patient is adequately anticoagulated such that sufficient heparin has been administered and that it has circulated. National guidelines mention a few recommendations for emergency procedures [6, 9]. Every hospital must consider how these recommendations can best be implemented with regard to sterility and local regulations. After reviewing the available literature and the documents of the national societies, the task force is in consensus that a 72-h storage time for primed circuits and a 30-day storage time for dry circuits should be considered as an institutional policy.
Recommendations for emergent institution and reinstitution of cardiopulmonary bypass
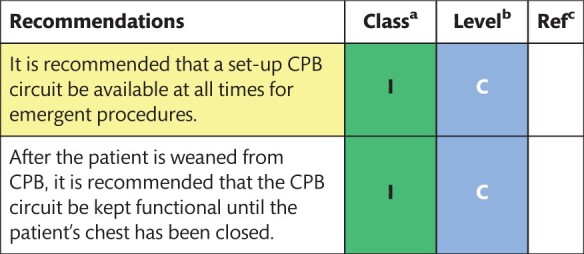
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
8. SEPARATION FROM CARDIOPULMONARY BYPASS
Weaning from CPB refers to the transition from mechanical circulatory and respiratory support to the unassisted functioning of the patient’s heart and lungs. Successful weaning from CPB is defined as adequate circulation, oxygenation and organ perfusion without the aid of ongoing CPB. It is a complex, multistep and interdisciplinary team effort. Therefore, appropriate planning and close communication between the surgeon(s), anaesthesiologist(s), perfusionist(s) and operating room staff are imperative during the weaning period in order to be able to prompt, react and adequately solve any medical or technical problems.
8.1 Reperfusion time
It seems evident that a sufficient reperfusion time following aortic cross-clamping is an essential prerequisite for successful separation from CPB. However, there are many parameters that influence myocardial recovery and, indeed, the recovery of other organs following ischaemia. Moreover, there is a massive variation in routine practice without apparent differences in results. Clear and practical advice on what is the optimal reperfusion time after cardiac ischaemic arrest is currently not available from the scientific literature.
8.2 Weaning checklist
Weaning from CPB is a multidisciplinary effort in which communication between all team members is of crucial importance. The use of a checklist can structure this process and optimize safety. Weaning scenarios, together with the use of a checklist, can be trained and validated through interactive training sessions and simulations.
8.2.1 Description of the evidence
It is difficult to prove that a cognitive aid, such as a checklist before weaning, might improve patient outcomes. In general, recent research suggests that the use of a checklist reduces errors of omission and enhances patient safety. No research has been performed concerning the use of a weaning checklist by perfusionists, but research in anaesthesia may be extrapolated. One study compared simulation-based weaning scenarios for anaesthesiologists, performed with and without a checklist [120]. The use of a checklist resulted in significantly better performance in completing 5 of the 9 designated tasks (P < 0.01). Several authors have proposed checklists, developed using different methods, and have obtained divergent results. It is noteworthy to mention the 4-item checklist [326] and the 7-item checklist [327]. The use of these checklists was suggested in combination with team education and simulation-based training to help develop crucial skills that allow operating room staff to reach their full potential. Others proposed several structural measures before weaning from CPB and pointed out that a failed weaning attempt might invoke haemodynamic instability, causing organ injury or dysfunction [328]. A structured approach was used by different physicians [120, 329]. The items on the checklist were generated using a Delphi method. The checklists were created by 7 centre-specific anaesthesiologists [120] or by 90 nation-wide anaesthesiologists [329]. Simulation-based training was compared to interactive seminar-based training. The authors concluded that high-fidelity simulation-based training leads to better performance and checklist adherence during CPB weaning [330].
Derived from these different checklists, we propose a weaning checklist (Supplementary Material, Appendix E) for cardiac surgery. The checklist may be adjusted to individual unit needs. The use of a checklist is recommended before the actual weaning process so that teams can restore focus and no critical steps are omitted.
Recommendation for use of weaning checklist
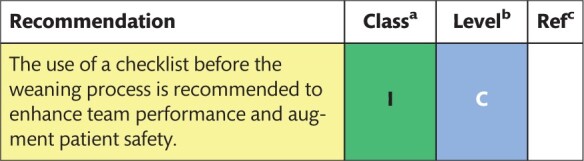
|
Class of recommendation.
Level of evidence.
References.
8.3 Haemodynamic monitoring
Apart from the electrocardiogram for the assessment of heart rate, rhythm and myocardial ischaemia, haemodynamic monitoring devices for weaning from CPB include the pulmonary artery catheter (PAC), newer haemodynamic minimally invasive monitors (pulse contour analysis) and TOE. They help to assess cardiac performance, including preload, afterload and contractility of left and right ventricles, as well as the quality of the surgical intervention including retained intracardiac air.
8.3.1 Description of the evidence
8.3.1.1 Pulmonary artery balloon catheter
Despite the introduction of the PAC into clinical use in the 1970s, there is a lack of evidence about the balance of benefits and complications during cardiac surgery. Whereas advantages include the possible assessments of cardiac output, pulmonary artery pressures and SvO2, disadvantages are technical errors such as unreliable data or false interpretation and iatrogenic complications such as arrhythmias, pulmonary embolism or haemorrhage.
A recent retrospective observational study of cardiac surgical patients in the USA, including 76 297 patients without and 40 036 patients with a PAC during a 4-year period, showed no increased risk of intraoperative cardiac arrest and no significant decrease in mortality associated with the PAC [331]. The PAC was also assessed in 2 063 337 patients during 10 years in the USA. A propensity-matched subgroup analysis revealed that the mortality rate was higher when the PAC was used in octogenarian patients (OR 1.24, 95% CI 1.03–1.50; P = 0.024) and high-risk patients (OR 1.30, 95% CI 1.14–1.48; P < 0.001). In addition, a higher incidence of prolonged mechanical ventilation and length of stay beyond 30 days was seen in patients receiving the PAC [332]. A smaller single-centre retrospective analysis in 2414 low-risk patients undergoing off-pump CABG revealed that the use of a PAC did not affect the conversion to an on-pump procedure, intraoperative intra-aortic balloon pump use, LCOS or in-hospital death [333].
Meaningful results of RCTs are needed to further assess the potential usefulness of the PAC. Overall, one can conclude that there is no indication to use the PAC as a routine monitor.
8.3.1.2 Minimally invasive haemodynamic monitors using pulse contour analysis
There are several devices that use an algorithm based on pulse contour analysis in order to calculate cardiac output. Agreement of cardiac output assessments between these minimally invasive pulse contour analysis monitors in comparison to the ‘practical’ gold standard PAC has been poor in a meta-analysis of accuracy and precision with a mean percentage error of 41%, which is beyond the accepted agreement of a reference standard of 30% or less [334]. In addition, particularly during the clinical situation of weaning the patient off CPB with possible haemodynamic instability and changes in temperature, vascular tone, afterload and intravascular volume, these devices are not particularly accurate, which leads to questions about their usefulness during these situations [335]. There are no clinical studies assessing clinical outcomes and the use of minimally invasive haemodynamic monitors using pulse contour analysis.
8.3.1.3 Transoesophageal echocardiography
The usefulness of intraoperative TOE has been evaluated in a retrospective study in 12 566 consecutive patients in 1 institution, demonstrating that before and also after CPB, TOE influenced surgical decisions in 7.0% and 2.2% of patients, respectively. After CABG surgery, post-CPB TOE influenced 1.5% of decisions and after isolated valve procedures, it influenced 3.3% of surgical decisions [336]. Routine TOE has been shown to reduce costs in a prospective study in 300 patients undergoing elective valve replacement [337] and also in a retrospective study in 430 patients undergoing cardiac procedures under CPB [338]. However, one also has to consider complications related to perioperative TOE, particularly in view of recent results from a 1-year prospective audit. This national audit in the UK reported an incidence of major TOE-associated complications of 0.08% and a mortality rate of 0.03% [339]. Based on this unexpectedly high incidence of TOE-associated morbidity and mortality rates, the routine use of TOE in cardiac surgery needs to be rethought.
Recent guidelines by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists confirm that, in the absence of contraindications, intraoperative TOE should be performed in all open-heart (i.e. valvular) and thoracic aortic procedures and also in some CABG operations [340]. Apart from confirming and refining the preoperative diagnosis, detecting new or unsuspected disease and adjusting the anaesthetic and surgical plan accordingly, TOE during and after weaning off CPB is also indicated to assess the results of the surgical intervention [341].
Recommendations for haemodynamic monitoring
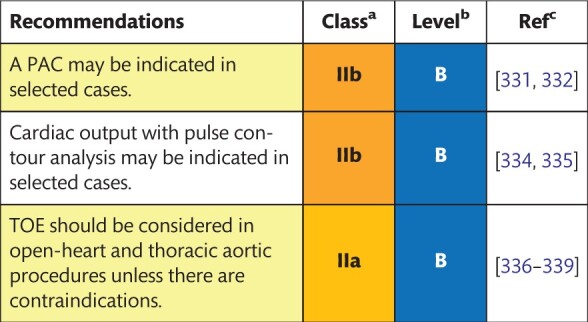
|
Class of recommendation.
Level of evidence.
References.
PAC: pulmonary artery catheter; TOE: transoesophageal echocardiography.
8.4 Positive inotropes
LCOS in cardiac surgery is a life-threatening complication, particularly during weaning off CPB. It is associated with increased morbidity and short-term and long-term mortality rates and places a burden on hospital resources. Reduced cardiac output decreases DO2 to the tissues, causing subsequent tissue hypoxia. Inotropes are usually the first-line therapy to manage this complication and should only be started after correction of potential causes of LCOS, such as graft dysfunction or hypovolaemia. Inotropes such as dobutamine, adrenaline, noradrenaline, phosphodiesterase III inhibitors and calcium sensitizers are the most commonly used drugs in this setting.
8.4.1 Description of the evidence
Although the use of inotropes/vasopressors in patients undergoing cardiac surgery is widely accepted, there are no randomized studies that have compared the effects of these drugs to no treatment at all. The majority of evidence as to the beneficial effects of inotropes/vasopressors in cardiac surgery comes from small RCTs. Several RCTs showed that prophylactic infusion of phosphodiesterase III inhibitors before weaning off CPB was associated with significant improvements in haemodynamics and reduced demand for other inotropes [342–345] and also with improved weaning success [343]. Results of a meta-analysis found that the use of inotropes/vasopressor therapy was not associated with differences in mortality rates among 28 280 patients from 177 RCTs in critical care and the perioperative setting [346]. However, in the cardiac surgical subgroup (40% of all patients in this meta-analysis, including 70 studies), the authors demonstrated a reduction in the mortality rates associated with inotrope/vasopressor use [51/1899 (2.7%) vs 77/1884 (4.1%), RR 0.70, 95% CI 0.50–0.96; P = 0.03]. Three recently published, large multicentre trials were devoted to the study of the perioperative use of levosimendan, either prophylactically in patients with low left ventricular ejection fraction [347, 348], or for the treatment of LCOS [349]. None of the trials showed any benefit regarding the use of the drug in terms of survival. An updated meta-analysis of levosimendan use in cardiac surgery showed that survival benefits related to the drug were not observed in either multicentre or in high-quality trials [350]. However, in high-quality subgroup trials, levosimendan therapy was associated with reduced mortality rates in patients with low preoperative ejection fractions (RR 0.58, 95% CI 0.38–0.88; P = 0.01).
Recommendations for use of positive inotropes
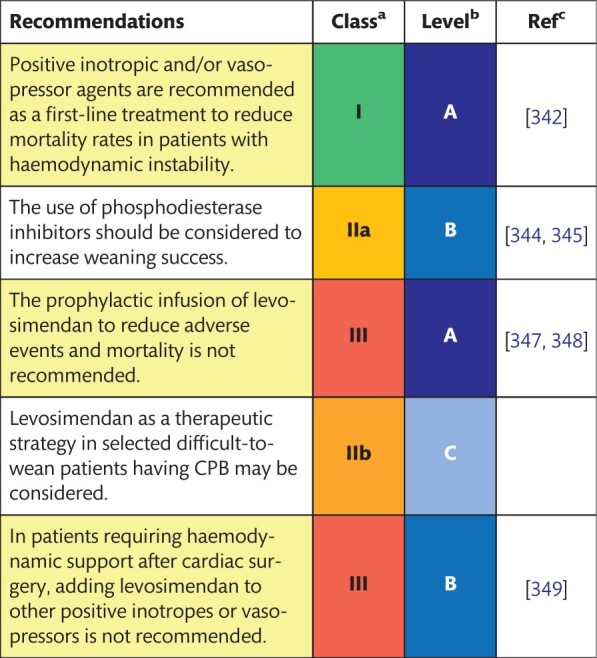
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
8.5 Haemostasis management
Haemostasis management following CPB includes monitoring and treatment of coagulation abnormalities in patients who are bleeding. With the introduction of point-of-care tests, including thromboelastography, thromboelastometry and platelet function analyses, haemostatic monitoring shifted to the setting of the operating room. Nowadays, most centres use haemostatic monitoring algorithms to reduce the risk of transfusion. Moreover, antifibrinolytic agents are routinely used as an additive to the prime or given prior to CPB to reduce fibrinolysis.
For a full review of evidence-based haemostatic management and treatment strategies following CPB, we refer readers to the 2017 EACTS/EACTA guidelines on patient blood management for adult cardiac surgery [2].
8.6 Mechanical circulatory support
Mechanical circulatory support during the perioperative period for cardiac surgery is comprehensively addressed in the upcoming joint document of the EACTS, the Society of Thoracic Surgeons (STS), the American Association for Thoracic Surgery (AATS) and the Extracorporeal Life Support Organization (ELSO) on post-cardiotomy ECLS. Taking into account the complexity of this topic and the word limit, we refer readers to the upcoming position statement of the 4 societies.
8.7 Residual blood management
Retransfusion of the residual volume of the CPB circuit at the end of CPB is part of a blood conservation strategy. It can be accomplished in 2 different ways: first, direct retransfusion without processing; and, second, after processing by centrifugation, cell salvage or ultrafiltration (MUF). When processing by centrifugation or cell salvage, only the red blood cells are returned; and most of the plasma components are discarded. With ultrafiltration, however, whole blood is concentrated and water-soluble components are removed.
8.7.1 Description of the evidence
Direct retransfusion without processing can be done by collecting the residual volume of the CPB circuit into an infusion bag and returning it to the patient. An alternative is to chase the residual blood into the circulation through the arterial cannula with Ringer’s acetate solution. In a randomized study of 40 patients [351], retransfusion of residual blood of the CPB circuit with the Ringer’s chase technique was compared to the commonly used ‘infusion bag’ technique. In this study, the Ringer’s chase technique was associated with better-preserved platelet function, reduced haemolysis, fewer signs of coagulation and fibrinolysis. There were no significant differences in blood loss during the operation and during the 4 h after surgery.
A prospective RCT compared the clinical effects of direct retransfusion, cell salvage and ultrafiltration [352]. Among the 3 groups (20 patients in each group), there were no significant differences in postoperative Hb levels, platelet counts, ACTs, partial thromboplastin times and postoperative chest tube drainage on arrival in the ICU and 12 h after CPB. A more recent study of 51 patients compared the effects of centrifugation, cell salvage and ultrafiltration [353]. Their results showed that cell salvage was superior with respect to postoperative Hb gain and washout of free Hb compared to centrifugation or ultrafiltration. Unfortunately, for ethical reasons, they were unable to include a retransfusion group without blood processing. A prospective RCT comparing retransfusion of blood unprocessed versus blood processed by cell salvage showed reduced blood loss (859 ± 382 vs 605 ± 265 ml, respectively; P = 0.019) and a decreased number of units of allogeneic erythrocyte concentrate suspension transfused during the first 24 h postoperatively (2.5 ± 0.7 vs 1.6 ± 1.4 units, respectively; P = 0.023) in the cell salvage group. Both groups showed impaired haemostasis, no significant differences in measured coagulation parameters and no significant differences in complement activation [354]. A pilot study comparing the same techniques showed similar blood volumes in the chest drains 4 h after surgery but reduced platelet numbers, prolonged clot formation time and less maximum clot firmness in the cell salvage group [355]. Comparing no retransfusion of the residual volume of the CPB circuit to retransfusion of the residual blood salvaged through a cell saver showed increased chest tube drainage (749 ± 320 vs 592 ± 264; P > 0.05) and FFP transfusion rate [5 (29%) patients vs 0 patients (0%); P < 0.04] in the cell salvage group. Cell salvage of the residual volume of the CPB circuit improved postoperative Hb levels (differences intraoperatively and 2 h after the end of CPB; P = 0.003) but induced strong thrombin generation, fibrinolysis activation and lower fibrinolysis inhibition. These conditions could generate a consumption coagulopathy [356]. In an RCT involving 200 patients, ultrafiltration of residual pump blood was compared to retransfusion of unprocessed blood. This study demonstrated no effect of ultrafiltration on the transfusion of homologous blood, postoperative haemorrhage or discharge Hb [357]. In contrast to this study, another prospective RCT in 573 patients receiving ultrafiltration at the end of CPB (treatment) or no ultrafiltration (control) showed a lower prevalence of early morbidity [66 of 284 (23.2%) vs 117 of 289 (40.5%); P = 0.0001] and lower blood transfusion requirements (1.66 ± 2.6 vs 2.25 ± 3.8 U/patient; P = 0.039) in the ultrafiltration group [297]. In a similar, smaller RCT (60 patients), also comparing ultrafiltration to no ultrafiltration at the end of CPB, ultrafiltration was associated with increased inflammatory response, reduced chest tube drainage (598 ± 123 ml vs 848 ± 455 ml; P = 0.04) and fewer blood transfusions (0.6 ± 0.6 U/patient vs 1.6 ± 1.1 U/patient; P = 0.03) [358].
Due to the publication of contradictory results, indicating the best way to deal with the residual volume of the CPB circuit is complicated. However, processed or not, there is agreement that retransfusion of the residual volume of the CPB circuit at the end of the procedure is part of blood-saving strategies.
Recommendations for residual blood management
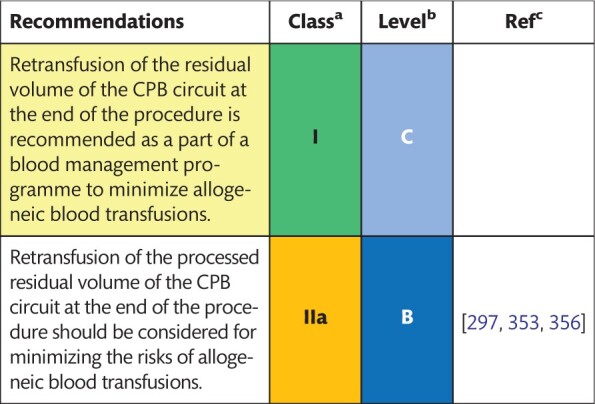
|
Class of recommendation.
Level of evidence.
References.
CPB: cardiopulmonary bypass.
9. FINAL REMARKS
These guidelines list over 100 practical recommendations about CPB procedures in adult cardiac surgery, the majority of which contain a significant body of scientific evidence to support a given recommendation (classes I and III are summarized in Supplementary Material, Appendices F and G). These are the first ever EACTS/EACTA/EBCP cardiopulmonary bypass guidelines.
During the systematic literature review of the current body of evidence, we identified several gaps in knowledge and areas in which evidence is conflicting or lacking, resulting in expert consensus statements, based on expert opinion. High-quality clinical research is necessary in the near future to fill the knowledge gaps and improve the current recommendations.
We believe that these European guidelines contribute towards optimization and standardization of CPB techniques. The next steps for CPB teams and stakeholders include dissemination and implementation of these recommendations into clinical practice, adoption into national guidelines and evaluation of the impact of these guidelines on patient outcomes after cardiac surgery.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank Korneel Vandewiele (Department of Perfusion, Heart Centre, University Hospital of Ghent, Belgium) for his assistance with data collection.
Funding
This article was produced by, and is under the sole responsibility of, the European Association for Cardio-Thoracic Surgery (EACTS), the European Association for Cardio-Thoracic Anaesthesiology (EACTA) and the European Board of Cardiovascular Perfusion (EBCP).
Conflict of interest: Filip M.J.J. De Somer: Speaker and consultancy fees paid to the University of Ghent. Speaker fee from Fresenius Kabi and Maquet Cardiopulmonary. Vladimir Lomivorotov: Speaking honoraria from Baxter, AbbVie and Orion Pharma. Frank Merkle: Speaker Bureau/Hospital contract for LivaNova. Marco Ranucci: Consultancy fees from LivaNova and Medtronic and royalties from LivaNova for the commercial application of a patent on a metabolic monitoring system; research grant from Roche Diagnostics; personal fees from Haemonetics, IL-Werfen Grifols and Vigor. All other authors declared no conflict of interest.
Contributor Information
Luc Puis, Department of Perfusion, University Hospital Brussels, Jette, Belgium.
Milan Milojevic, Department of Cardiovascular Anaesthesia and Intensive Care Unit, Dedinje Cardiovascular Institute, Belgrade, Serbia; Department of Cardiothoracic Surgery, Erasmus University Medical Center, Rotterdam, Netherlands.
Christa Boer, Department of Anaesthesiology, Amsterdam UMC, VU University, Amsterdam Cardiovascular Sciences, Amsterdam, Netherlands.
Filip M J J De Somer, Department of Cardiac Surgery, Ghent University Hospital, Ghent, Belgium.
Tomas Gudbjartsson, Department of Cardiothoracic Surgery, Faculty of Medicine, Landspitali University Hospital, University of Iceland, Reykjavik, Iceland.
Jenny van den Goor, Department of Cardiothoracic Surgery, Academic Medical Centre of the University of Amsterdam, Amsterdam, Netherlands.
Timothy J Jones, Department of Paediatric Cardiac Surgery, Birmingham Women’s and Children’s Hospital, Birmingham, UK.
Vladimir Lomivorotov, Department of Anesthesiology and Intensive Care, E. Meshalkin National Medical Research Center, Novosibirsk State University, Novosibirsk, Russia.
Frank Merkle, Academy for Perfusion, Deutsches Herzzentrum, Berlin, Germany.
Marco Ranucci, Department of Cardiovascular Anaesthesia and Intensive Care Unit, IRCCS Policlinico San Donato, Milan, Italy.
Gudrun Kunst, Department of Anaesthetics and Pain Medicine, King's College Hospital NHS Foundation Trust and School of Cardiovascular Medicine & Sciences, King's College London British Heart Foundation Centre of Excellence, London, UK.
Alexander Wahba, Department of Cardio-Thoracic Surgery, St Olav s University Hospital, Trondheim, Norway; Department of Circulation and Medical Imaging, Norwegian University of Science and Technology, Trondheim, Norway.
EACTS/EACTA/EBCP Committee Reviewers:
Peter Alston, David Fitzgerald, Aleksandar Nikolic, Francesco Onorati, Bodil Steen Rasmussen, and Staffan Svenmarker
Disclaimer 2019: The EACTS/EACTA/EBCP Guidelines represent the views of the EACTS, the EACTA and EBCP and were produced after careful consideration of the scientific and medical knowledge and the evidence available at the time of their dating. The EACTS, EACTA and EBCP are not responsible in the event of any contradiction, discrepancy and/or ambiguity between the EACTS, EACTA and EBCP Guidelines and any other official recommendations or guidelines issued by the relevant public health authorities, in particular in relation to good use of healthcare or therapeutic strategies. Health professionals are encouraged to take the EACTS, EACTA and EBCP Guidelines fully into account when exercising their clinical judgement as well as in the determination and the implementation of preventive, diagnostic or therapeutic medical strategies; however, the EACTS, EACTA and EBCP Guidelines do not, in any way whatsoever, override the individual responsibility of health professionals to make appropriate and accurate decisions in consideration of each patient’s health condition and, where appropriate and/or necessary, in consultation with that patient and the patient’s care provider. Nor do the EACTS, EACTA and EBCP Guidelines exempt health professionals from giving full and careful consideration to the relevant official, updated recommendations or guidelines issued by the competent public health authorities, in order to manage each patient’s case in light of the scientifically accepted data pursuant to their respective ethical and professional obligations. It is also the health professional’s responsibility to verify the applicable rules and regulations relating to drugs and medical devices at the time of prescription.
The article has been co-published with permission in the British Journal of Anaesthesia, the European Journal of Cardio-Thoracic Surgery and the Interactive CardioVascular and Thoracic Surgery.
REFERENCES
- 1. Sousa-Uva M, Head SJ, Thielmann M, Cardillo G, Benedetto U, Czerny M. Methodology manual for European Association for Cardio-Thoracic Surgery (EACTS) clinical guidelines. Eur J Cardiothorac Surg 2015;48:809–16. [DOI] [PubMed] [Google Scholar]
- 2. Pagano D, Milojevic M, Meesters MI, Benedetto U, Bolliger D, von Heymann C et al. 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery. Eur J Cardiothorac Surg 2018;53:79–111. [DOI] [PubMed] [Google Scholar]
- 3. Engelman R, Baker RA, Likosky DS, Grigore A, Dickinson TA, Shore-Lesserson L et al. The Society of Thoracic Surgeons, The Society of Cardiovascular Anesthesiologists, and The American Society of ExtraCorporeal Technology: Clinical Practice Guidelines for Cardiopulmonary Bypass—Temperature Management During Cardiopulmonary Bypass. J Extra Corpor Technol 2015;47:145–54. [PMC free article] [PubMed] [Google Scholar]
- 4.The European Board of Cardiovascular Perfusion: Accreditation Manual. https://www.ebcp.eu/login/files/6fdd5b091fb9dd608d26d02a8fd40e46774005df.pdf (28 April 2019, date last accessed).
- 5.The American Board of Cardiovascular Perfusion: Booklet of Information. http://abcp.org/pd/boi.pdf (28 April 2019, date last accessed).
- 6.American Society of Extracorporeal Technology: Standards and Guidelines for Perfusion Practice. http://www.amsect.org/p/cm/ld/fid=1617 (28 April 2019, date last accessed).
- 7. Baker RA, Bronson SL, Dickinson TA, Fitzgerald DC, Likosky DS, Mellas NB et al. Report from AmSECT's International Consortium for Evidence-Based Perfusion: American Society of Extracorporeal Technology Standards and Guidelines for Perfusion Practice: 2013. J Extra Corpor Technol 2013;45:156–66. [PMC free article] [PubMed] [Google Scholar]
- 8.Australian and New Zealand College of Anaesthetists: Guidelines for Major Extracorporeal Perfusion. http://www.anzca.edu.au/documents/ps27-2015-guidelines-for-major-extracorporeal-perf.pdf (28 April 2019, date last accessed).
- 9.The Society of Clinical Perfusion Scientists of Great Britain and Ireland and The College of Clinical Perfusion Scientists of Great Britain and Ireland: Code of Practice. https://www.scps.org.uk/index.php? option=com_content&task=view&id=34&Itemid=40 (28 April 2019, date last accessed).
- 10.The European Board of Cardiovascular Perfusion: Amended Requirement for Recertification. https://www.ebcp.eu/login/files/f7e5dfaf8982e4ab2fa7e81dc6a3c87b69b62a37.pdf (28 April 2019, date last accessed).
- 11.Commission on Accreditation of Allied Health Education Programs: Standards and Guidelines for the Accreditation of Education Programs in Perfusion. https://www.caahep.org/CAAHEP/media/CAAHEP-Documents/PerfusionStandards2012.pdf (28 April 2019, date last accessed).
- 12.The Society of Clinical Perfusion Scientists of Great Britain and Ireland and The College of Clinical Perfusion Scientists of Great Britain and Ireland: Standards of Practice Document. https://www.scps.org.uk/index.php? option=com_content&task=view&id=25&Itemid=40 (28 April 2019, date last accessed).
- 13.The Department of Health: A Guide to Good Practice in Clinical Perfusion. https://www.scps.org.uk/pdfs/GuidetoGoodPractice.pdf (28 April 2019, date last accessed).
- 14. Wahr JA, Prager RL, Abernathy JH 3rd, Martinez EA, Salas E, Seifert PC et al. Patient safety in the cardiac operating room: human factors and teamwork: a scientific statement from the American Heart Association. Circulation 2013;128:1139–69. [DOI] [PubMed] [Google Scholar]
- 15. Paugh TA, Dickinson TA, Theurer PF, Bell GF, Shann KG, Baker RA et al. Validation of a perfusion registry: methodological approach and initial findings. J Extra Corpor Technol 2012;44:104–15. [PMC free article] [PubMed] [Google Scholar]
- 16. DioDato CP, Likosky DS, DeFoe GR, Groom RC, Shann KG, Krumholz CF et al. Cardiopulmonary bypass recommendations in adults: the northern New England experience. J Extra Corpor Technol 2008;40:16–20. [PMC free article] [PubMed] [Google Scholar]
- 17. Baker RA, Newland RF. Continous quality improvement of perfusion practice: the role of electronic data collection and statistical control charts. Perfusion 2008;23:7–16. [DOI] [PubMed] [Google Scholar]
- 18.Australian and New Zealand College of Anaesthetists: Regulations and Guidelines for Perfusionists. http://isect.org/images/media/pdfs/anzcp-regulations-guidelines-for-perfusionist.pdf (28 April 2019, date last accessed).
- 19. Edaigbini SA, Delia IZ, Aminu MB. Zaria universal oxygenator holder phase I. Niger J Surg 2014;20:16–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Skoletsky JS, White BT, Austin JW. Innovative design to prevent reversal of roller blood pump rotation in the event of electromechanical failure: an easy solution to a devastating problem. J Extra Corpor Technol 2007;39:96–8. [PMC free article] [PubMed] [Google Scholar]
- 21. Marshall C, Hargrove M, O'Donnell A, Aherne T. Variations in battery life of a heart-lung machine using different pump speeds, pressure loads, boot material, centrifugal pump head, multiple pump usage, and battery age. J Extra Corpor Technol 2005;37:278–81. [PMC free article] [PubMed] [Google Scholar]
- 22. Svenmarker S, Haggmark S, Ostman M, Holmgren A, Naslund U. Central venous oxygen saturation during cardiopulmonary bypass predicts 3-year survival. Interact CardioVasc Thorac Surg 2013;16:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ottens J, Tuble SC, Sanderson AJ, Knight JL, Baker RA. Improving cardiopulmonary bypass: does continuous blood gas monitoring have a role to play? J Extra Corpor Technol 2010;42:191–8. [PMC free article] [PubMed] [Google Scholar]
- 24.The Society of Clinical Perfusion Scientists of Great Britain and Ireland: Recommendations for Standards of Monitoring during Cardiopulmonary Bypass. https://www.scps.org.uk/index.php? option=com_content&task=view&id=27&Itemid=42 (28 April 2019, date last accessed).
- 25. Mejak BL, Stammers A, Rauch E, Vang S, Viessman T. A retrospective study on perfusion incidents and safety devices. Perfusion 2000;15:51–61. [DOI] [PubMed] [Google Scholar]
- 26. Charriere JM, Pelissie J, Verd C, Leger P, Pouard P, de Riberolles C et al. Survey: retrospective survey of monitoring/safety devices and incidents of cardiopulmonary bypass for cardiac surgery in France. J Extra Corpor Technol 2007;39:142–57; discussion 58–9. [PMC free article] [PubMed] [Google Scholar]
- 27. Wehrli-Veit M, Riley JB, Austin JW. A failure mode effect analysis on extracorporeal circuits for cardiopulmonary bypass. J Extra Corpor Technol 2004;36:351–7. [PubMed] [Google Scholar]
- 28. Lawson C, Predella M, Rowden A, Goldstein J, Sistino JJ, Fitzgerald DC. Assessing the culture of safety in cardiovascular perfusion: attitudes and perceptions. Perfusion 2017;32:583–90. [DOI] [PubMed] [Google Scholar]
- 29. Martinez EA, Thompson DA, Errett NA, Kim GR, Bauer L, Lubomski LH et al. Review article: high stakes and high risk: a focused qualitative review of hazards during cardiac surgery. Anesth Analg 2011;112:1061–74. [DOI] [PubMed] [Google Scholar]
- 30. Kurusz M. Perfusion safety: new initiatives and enduring principles. Perfusion 2011;26(Suppl 1):6–14. [DOI] [PubMed] [Google Scholar]
- 31. Anastasiadis K, Murkin J, Antonitsis P, Bauer A, Ranucci M, Gygax E et al. Use of minimal invasive extracorporeal circulation in cardiac surgery: principles, definitions and potential benefits. A position paper from the Minimal invasive Extra-Corporeal Technologies international Society (MiECTiS). Interact CardioVasc Thorac Surg 2016;22:647–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kowalewski M, Pawliszak W, Raffa GM, Malvindi PG, Kowalkowska ME, Zaborowska K et al. Safety and efficacy of miniaturized extracorporeal circulation when compared with off-pump and conventional coronary artery bypass grafting: evidence synthesis from a comprehensive Bayesian-framework network meta-analysis of 134 randomized controlled trials involving 22 778 patients. Eur J Cardiothorac Surg 2016;49:1428–40. [DOI] [PubMed] [Google Scholar]
- 33. Shroyer AL, Hattler B, Wagner TH, Collins JF, Baltz JH, Quin JA et al. Five-year outcomes after on-pump and off-pump coronary-artery bypass. N Engl J Med 2017;377:623–32. [DOI] [PubMed] [Google Scholar]
- 34. Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Straka Z et al. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med 2016;375:2359–68. [DOI] [PubMed] [Google Scholar]
- 35. McMullan V, Alston RP, Tyrrell J. Volatile anaesthesia during cardiopulmonary bypass. Perfusion 2015;30:6–16. [DOI] [PubMed] [Google Scholar]
- 36. Weitkemper HH, Spilker A, Knobl HJ, Korfer R. The heater-cooler unit—a conceivable source of infection. J Extra Corpor Technol 2002;34:276–80. [PubMed] [Google Scholar]
- 37. Sax H, Bloemberg G, Hasse B, Sommerstein R, Kohler P, Achermann Y et al. Prolonged outbreak of Mycobacterium chimaera infection after open-chest heart surgery. Clin Infect Dis 2015;61:67–75. [DOI] [PubMed] [Google Scholar]
- 38. Sommerstein R, Ruegg C, Kohler P, Bloemberg G, Kuster SP, Sax H. Transmission of Mycobacterium chimaera from heater-cooler units during cardiac surgery despite an ultraclean air ventilation system. Emerg Infect Dis 2016;22:1008–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. van Ingen J, Kohl TA, Kranzer K, Hasse B, Keller PM, Katarzyna Szafranska A et al. Global outbreak of severe Mycobacterium chimaera disease after cardiac surgery: a molecular epidemiological study. Lancet Infect Dis 2017;17:1033–41. [DOI] [PubMed] [Google Scholar]
- 40. Sommerstein R, Hasse B, Marschall J, Sax H, Genoni M, Schlegel M et al. Global health estimate of invasive Mycobacterium chimaera infections associated with heater-cooler devices in cardiac surgery. Emerg Infect Dis 2018;24:576–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Svensson E, Jensen ET, Rasmussen EM, Folkvardsen DB, Norman A, Lillebaek T. Mycobacterium chimaera in heater-cooler units in Denmark related to isolates from the United States and United Kingdom. Emerg Infect Dis 2017;23:507–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.European Centre for Disease Prevention and Control. Rapid Risk Assessment: Invasive Cardiovascular Infection by Mycobacterium Chimaera Associated with the 3T Heater-Cooler System Used during Open-Heart Surgery. https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/RRA-mycobacterium-chimaera-November-2016.pdf (28 April 2019, date last accessed).
- 43. Ottens J, Baker RA, Newland RF, Mazzone A. The future of the perfusion record: automated data collection vs. manual recording. J Extra Corpor Technol 2005;37:355–9. [PMC free article] [PubMed] [Google Scholar]
- 44. Newland RF, Baker RA, Stanley R. Electronic data processing: the pathway to automated quality control of cardiopulmonary bypass. J Extra Corpor Technol 2006;38:139–43. [PMC free article] [PubMed] [Google Scholar]
- 45. Beck JR, Fung K, Lopez H 2nd, Mongero LB, Argenziano M. Real-time data acquisition and alerts may reduce reaction time and improve perfusionist performance during cardiopulmonary bypass. Perfusion 2015;30:41–4. [DOI] [PubMed] [Google Scholar]
- 46. Stammers AH, Trowbridge CC, Pezzuto J, Casale A. Perfusion quality improvement and the reduction of clinical variability. J Extra Corpor Technol 2009;41:P48–58. [PMC free article] [PubMed] [Google Scholar]
- 47. Likosky DS, Paugh TA, Harrington SD, Wu X, Rogers MA, Dickinson TA et al. Prediction of transfusions after isolated coronary artery bypass grafting surgical procedures. Ann Thorac Surg 2017;103:764–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Paugh TA, Dickinson TA, Martin JR, Hanson EC, Fuller J, Heung M et al. Impact of ultrafiltration on kidney injury after cardiac surgery: the Michigan experience. Ann Thorac Surg 2015;100:1683–8. [DOI] [PubMed] [Google Scholar]
- 49. Svenmarker S, Haggmark S, Jansson E, Lindholm R, Appelblad M, Aberg T. Quality assurance in clinical perfusion. Eur J Cardiothorac Surg 1998;14:409–14. [DOI] [PubMed] [Google Scholar]
- 50. Baker RA, Newland RF, Fenton C, McDonald M, Willcox TW, Merry AF. Developing a benchmarking process in perfusion: a report of the Perfusion Downunder Collaboration. J Extra Corpor Technol 2012;44:26–33. [PMC free article] [PubMed] [Google Scholar]
- 51. Leontyev S, Borger MA, Legare JF, Merk D, Hahn J, Seeburger J et al. Iatrogenic type A aortic dissection during cardiac procedures: early and late outcome in 48 patients. Eur J Cardiothorac Surg 2012;41:641–6. [DOI] [PubMed] [Google Scholar]
- 52. Williams ML, Sheng S, Gammie JS, Rankin JS, Smith PK, Hughes GC. Aortic dissection as a complication of cardiac surgery: report from the Society of Thoracic Surgeons database. Ann Thorac Surg 2010;90:1812–6. [DOI] [PubMed] [Google Scholar]
- 53. Carino D, Mori M, Pang PYK, Singh M, Elkinany S, Tranquilli M et al. Direct axillary cannulation with open Seldinger-guided technique: is it safe? Eur J Cardiothorac Surg 2018;53:1279–81. [DOI] [PubMed] [Google Scholar]
- 54. Fusco DS, Shaw RK, Tranquilli M, Kopf GS, Elefteriades JA. Femoral cannulation is safe for type A dissection repair. Ann Thorac Surg 2004;78:1285–9. [DOI] [PubMed] [Google Scholar]
- 55. Tunick PA, Kronzon I. Atheromas of the thoracic aorta: clinical and therapeutic update. J Am Coll Cardiol 2000;35:545–54. [DOI] [PubMed] [Google Scholar]
- 56. Fukuda I, Fujimori S, Daitoku K, Yanaoka H, Inamura T. Flow velocity and turbulence in the transverse aorta of a proximally directed aortic cannula: hydrodynamic study in a transparent model. Ann Thorac Surg 2009;87:1866–71. [DOI] [PubMed] [Google Scholar]
- 57. Davila-Roman VG, Phillips KJ, Daily BB, Davila RM, Kouchoukos NT, Barzilai B. Intraoperative transesophageal echocardiography and epiaortic ultrasound for assessment of atherosclerosis of the thoracic aorta. J Am Coll Cardiol 1996;28:942–7. [DOI] [PubMed] [Google Scholar]
- 58. Rosenberger P, Shernan SK, Loffler M, Shekar PS, Fox JA, Tuli JK et al. The influence of epiaortic ultrasonography on intraoperative surgical management in 6051 cardiac surgical patients. Ann Thorac Surg 2008;85:548–53. [DOI] [PubMed] [Google Scholar]
- 59. Djaiani G, Ali M, Borger MA, Woo A, Carroll J, Feindel C et al. Epiaortic scanning modifies planned intraoperative surgical management but not cerebral embolic load during coronary artery bypass surgery. Anesth Analg 2008;106:1611–8. [DOI] [PubMed] [Google Scholar]
- 60. Osaka S, Tanaka M. Strategy for porcelain ascending aorta in cardiac surgery. Ann Thorac Cardiovasc Surg 2018;24:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. von Segesser LK, Ferrari E, Delay D, Maunz O, Horisberger J, Tozzi P. Routine use of self-expanding venous cannulas for cardiopulmonary bypass: benefits and pitfalls in 100 consecutive cases. Eur J Cardiothorac Surg 2008;34:635–40. [DOI] [PubMed] [Google Scholar]
- 62. Mulholland JW, Massey W, Shelton JC. Investigation and quantification of the blood trauma caused by the combined dynamic forces experienced during cardiopulmonary bypass. Perfusion 2000;15:485–94. [DOI] [PubMed] [Google Scholar]
- 63. Pohlmann JR, Toomasian JM, Hampton CE, Cook KE, Annich GM, Bartlett RH. The relationships between air exposure, negative pressure, and hemolysis. ASAIO J 2009;55:469–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. El-Sabbagh AM, Toomasian CJ, Toomasian JM, Ulysse G, Major T, Bartlett RH. Effect of air exposure and suction on blood cell activation and hemolysis in an in vitro cardiotomy suction model. ASAIO J 2013;59:474–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Myers GJ, Voorhees C, Haynes R, Eke B. Post-arterial filter gaseous microemboli activity of five integral cardiotomy reservoirs during venting: an in vitro study. J Extra Corpor Technol 2009;41:20–7. [PMC free article] [PubMed] [Google Scholar]
- 66. Koster A, Bottcher W, Merkel F, Hetzer R, Kuppe H. The more closed the bypass system the better: a pilot study on the effects of reduction of cardiotomy suction and passive venting on hemostatic activation during on-pump coronary artery bypass grafting. Perfusion 2005;20:285–8. [DOI] [PubMed] [Google Scholar]
- 67. Jegger D, Horisberger J, Jachertz M, Seigneul I, Tozzi P, Delay D et al. A novel device for reducing hemolysis provoked by cardiotomy suction during open heart cardiopulmonary bypass surgery: a randomized prospective study. Artif Organs 2007;31:23–30. [DOI] [PubMed] [Google Scholar]
- 68. Tanaka H, Oshiyama T, Narisawa T, Mori T, Masuda M, Kishi D et al. Clinical study of biocompatibility between open and closed heparin-coated cardiopulmonary bypass circuits. J Artif Organs 2003;6:245–52. [DOI] [PubMed] [Google Scholar]
- 69. Kiessling AH, Khalil M, Assaf O, Isgro F, Kretz KU, Saggau W. Blood-air interface during cardiopulmonary bypass. Asian Cardiovasc Thorac Ann 2004;12:198–201. [DOI] [PubMed] [Google Scholar]
- 70. Murphy GS, Hessel EA 2nd, Groom RC. Optimal perfusion during cardiopulmonary bypass: an evidence-based approach. Anesth Analg 2009;108:1394–417. [DOI] [PubMed] [Google Scholar]
- 71. Lindholm L, Westerberg M, Bengtsson A, Ekroth R, Jensen E, Jeppsson A. A closed perfusion system with heparin coating and centrifugal pump improves cardiopulmonary bypass biocompatibility in elderly patients. Ann Thorac Surg 2004;78:2131–8. [DOI] [PubMed] [Google Scholar]
- 72. Paparella D, Scrascia G, Rotunno C, Marraudino N, Guida P, De Palo M et al. A biocompatible cardiopulmonary bypass strategy to reduce hemostatic and inflammatory alterations: a randomized controlled trial. J Cardiothorac Vasc Anesth 2012;26:557–62. [DOI] [PubMed] [Google Scholar]
- 73. Nakahira A, Sasaki Y, Hirai H, Matsuo M, Morisaki A, Suehiro S et al. Cardiotomy suction, but not open venous reservoirs, activates coagulofibrinolysis in coronary artery surgery. J Thorac Cardiovasc Surg 2011;141:1289–97. [DOI] [PubMed] [Google Scholar]
- 74. Casalino S, Stelian E, Novelli E, De Jong A, Renzi L, Arellano F et al. Reduced transfusion requirements with a closed cardiopulmonary bypass system. J Cardiovasc Surg (Torino) 2008;49:363–9. [PubMed] [Google Scholar]
- 75. Dell'Amore A, Tripodi A, Cavallucci A, Guerrini F, Ronchi B, Zanoni S et al. Efficacy of a new oxygenator-integrated fat and leukocyte removal device. Asian Cardiovasc Thorac Ann 2010;18:546–50. [DOI] [PubMed] [Google Scholar]
- 76. Lagny MG, Gothot A, Hans GA, Koch JN, Blaffart F, Hella D et al. Efficacy of the RemoweLL cardiotomy reservoir for fat and leucocyte removal from shed mediastinal blood: a randomized controlled trial. Perfusion 2016;31:544–51. [DOI] [PubMed] [Google Scholar]
- 77. Issitt RW, Harvey I, Walsh B, Voegeli D. Quantification of lipid filtration and the effects on cerebral injury during cardiopulmonary bypass. Ann Thorac Surg 2017;104:884–90. [DOI] [PubMed] [Google Scholar]
- 78. Segers PA, Heida JF, de Vries I, Maas C, Boogaart AJ, Eilander S. Clinical evaluation of nine hollow-fibre membrane oxygenators. Perfusion 2001;16:95–106. [DOI] [PubMed] [Google Scholar]
- 79. Gu YJ, Boonstra PW, Graaff R, Rijnsburger AA, Mungroop H, van Oeveren W. Pressure drop, shear stress, and activation of leukocytes during cardiopulmonary bypass: a comparison between hollow fiber and flat sheet membrane oxygenators. Artif Organs 2000;24:43–8. [DOI] [PubMed] [Google Scholar]
- 80. De Somer D, Foubert L, Vanackere M, Dujardin D, Delanghe J, Van Nooten G. Impact of oxygenator design on hemolysis, shear stress, and white blood cell and platelet counts. J Cardiothorac Vasc Anesth 1996;10:884–9. [DOI] [PubMed] [Google Scholar]
- 81. Onorati F, Santini F, Raffin F, Menon T, Graziani MS, Chiominto B et al. Clinical evaluation of new generation oxygenators with integrated arterial line filters for cardiopulmonary bypass. Artif Organs 2012;36:875–85. [DOI] [PubMed] [Google Scholar]
- 82. Wendel HP, Philipp A, Weber N, Birnbaum DE, Ziemer G. Oxygenator thrombosis: worst case after development of an abnormal pressure gradient—incidence and pathway. Perfusion 2001;16:271–8. [DOI] [PubMed] [Google Scholar]
- 83. Hinz J, Molder JM, Hanekop GG, Weyland A, Popov AF, Bauer M et al. Reduced sevoflurane loss during cardiopulmonary bypass when using a polymethylpentane versus a polypropylene oxygenator. Int J Artif Organs 2013;36:233–9. [DOI] [PubMed] [Google Scholar]
- 84. Philipp A, Wiesenack C, Behr R, Schmid FX, Birnbaum DE. High risk of intraoperative awareness during cardiopulmonary bypass with isoflurane administration via diffusion membrane oxygenators. Perfusion 2002;17:175–8. [DOI] [PubMed] [Google Scholar]
- 85. Wiesenack C, Wiesner G, Keyl C, Gruber M, Philipp A, Ritzka M et al. In vivo uptake and elimination of isoflurane by different membrane oxygenators during cardiopulmonary bypass. Anesthesiology 2002;97:133–8. [DOI] [PubMed] [Google Scholar]
- 86. Nigro Neto C, Arnoni R, Rida BS, Landoni G, Tardelli MA. Randomized trial on the effect of sevoflurane on polypropylene membrane oxygenator performance. J Cardiothorac Vasc Anesth 2013;27:903–7. [DOI] [PubMed] [Google Scholar]
- 87. Saczkowski R, Maklin M, Mesana T, Boodhwani M, Ruel M. Centrifugal pump and roller pump in adult cardiac surgery: a meta-analysis of randomized controlled trials. Artif Organs 2012;36:668–76. [DOI] [PubMed] [Google Scholar]
- 88. Klein M, Mahoney CB, Probst C, Schulte HD, Gams E. Blood product use during routine open heart surgery: the impact of the centrifugal pump. Artif Organs 2001;25:300–5. [PubMed] [Google Scholar]
- 89. Andersen KS, Nygreen EL, Grong K, Leirvaag B, Holmsen H. Comparison of the centrifugal and roller pump in elective coronary artery bypass surgery—a prospective, randomized study with special emphasis upon platelet activation. Scand Cardiovasc J 2003;37:356–62. [DOI] [PubMed] [Google Scholar]
- 90. Babin-Ebell J, Misoph M, Mullges W, Neukam K, Elert O. Reduced release of tissue factor by application of a centrifugal pump during cardiopulmonary bypass. Heart Vessels 1998;13:147–51. [DOI] [PubMed] [Google Scholar]
- 91. Keyser A, Hilker MK, Diez C, Philipp A, Foltan M, Schmid C. Prospective randomized clinical study of arterial pumps used for routine on pump coronary bypass grafting. Artif Organs 2011;35:534–42. [DOI] [PubMed] [Google Scholar]
- 92. Hansbro SD, Sharpe DA, Catchpole R, Welsh KR, Munsch CM, McGoldrick JP et al. Haemolysis during cardiopulmonary bypass: an in vivo comparison of standard roller pumps, nonocclusive roller pumps and centrifugal pumps. Perfusion 1999;14:3–10. [DOI] [PubMed] [Google Scholar]
- 93. Scott DA, Silbert BS, Doyle TJ, Blyth C, Borton MC, O'Brien JL et al. Centrifugal versus roller head pumps for cardiopulmonary bypass: effect on early neuropsychologic outcomes after coronary artery surgery. J Cardiothorac Vasc Anesth 2002;16:715–22. [DOI] [PubMed] [Google Scholar]
- 94. Padayachee TS, Parsons S, Theobold R, Linley J, Gosling RG, Deverall PB. The detection of microemboli in the middle cerebral artery during cardiopulmonary bypass: a transcranial Doppler ultrasound investigation using membrane and bubble oxygenators. Ann Thorac Surg 1987;44:298–302. [DOI] [PubMed] [Google Scholar]
- 95. Pugsley W, Klinger L, Paschalis C, Treasure T, Harrison M, Newman S. The impact of microemboli during cardiopulmonary bypass on neuropsychological functioning. Stroke 1994;25:1393–9. [DOI] [PubMed] [Google Scholar]
- 96. Sellman M, Ivert T, Wahlgren NG, Knutsson E, Semb BK. Early neurological and electroencephalographic changes after coronary artery surgery in low-risk patients younger than 70 years. Thorac Cardiovasc Surg 1991;39:76–80. [DOI] [PubMed] [Google Scholar]
- 97. Padayachee TS, Parsons S, Theobold R, Gosling RG, Deverall PB. The effect of arterial filtration on reduction of gaseous microemboli in the middle cerebral artery during cardiopulmonary bypass. Ann Thorac Surg 1988;45:647–9. [DOI] [PubMed] [Google Scholar]
- 98. Sellman M, Holm L, Ivert T, Semb BK. A randomized study of neuropsychological function in patients undergoing coronary bypass surgery. Thorac Cardiovasc Surg 1993;41:349–54. [DOI] [PubMed] [Google Scholar]
- 99. Jabur GN, Sidhu K, Willcox TW, Mitchell SJ. Clinical evaluation of emboli removal by integrated versus non-integrated arterial filters in new generation oxygenators. Perfusion 2016;31:409–17. [DOI] [PubMed] [Google Scholar]
- 100. Stehouwer MC, Boers C, de Vroege R, Kelder JC, Yilmaz A, Bruins P. Clinical evaluation of the air removal characteristics of an oxygenator with integrated arterial filter in a minimized extracorporeal circuit. Int J Artif Organs 2011;34:374–82. [DOI] [PubMed] [Google Scholar]
- 101. Roosenhoff TP, Stehouwer MC, De Vroege R, Butter RP, Van Boven WJ, Bruins P. Air removal efficiency of a venous bubble trap in a minimal extracorporeal circuit during coronary artery bypass grafting. Artif Organs 2010;34:1092–8. [DOI] [PubMed] [Google Scholar]
- 102. Sahlman A, Ahonen J, Salo JA, Ramo OJ. No impact of a leucocyte depleting arterial line filter on patient recovery after cardiopulmonary bypass. Acta Anaesthesiol Scand 2001;45:558–63. [DOI] [PubMed] [Google Scholar]
- 103. Loberg AG, Stallard J, Dunning J, Dark J. Can leucocyte depletion reduce reperfusion injury following cardiopulmonary bypass? Interact CardioVasc Thorac Surg 2011;12:232–7. [DOI] [PubMed] [Google Scholar]
- 104. Spencer S, Tang A, Khoshbin E. Leukodepletion for patients undergoing heart valve surgery. Cochrane Database Syst Rev 2013:CD009507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Whitaker DC, Newman SP, Stygall J, Hope-Wynne C, Harrison MJ, Walesby RK. The effect of leucocyte-depleting arterial line filters on cerebral microemboli and neuropsychological outcome following coronary artery bypass surgery. Eur J Cardiothorac Surg 2004;25:267–74. [DOI] [PubMed] [Google Scholar]
- 106. Leal-Noval SR, Amaya R, Herruzo A, Hernandez A, Ordonez A, Marin-Niebla A et al. Effects of a leukocyte depleting arterial line filter on perioperative morbidity in patients undergoing cardiac surgery: a controlled randomized trial. Ann Thorac Surg 2005;80:1394–400. [DOI] [PubMed] [Google Scholar]
- 107. Alexiou C, Tang AA, Sheppard SV, Smith DC, Gibbs R, Livesey SA et al. The effect of leucodepletion on leucocyte activation, pulmonary inflammation and respiratory index in surgery for coronary revascularisation: a prospective randomised study. Eur J Cardiothorac Surg 2004;26:294–300. [DOI] [PubMed] [Google Scholar]
- 108. Ranucci M, Balduini A, Ditta A, Boncilli A, Brozzi S. A systematic review of biocompatible cardiopulmonary bypass circuits and clinical outcome. Ann Thorac Surg 2009;87:1311–9. [DOI] [PubMed] [Google Scholar]
- 109. Mahmood S, Bilal H, Zaman M, Tang A. Is a fully heparin-bonded cardiopulmonary bypass circuit superior to a standard cardiopulmonary bypass circuit? Interact CardioVasc Thorac Surg 2012;14:406–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Landis RC, Brown JR, Fitzgerald D, Likosky DS, Shore-Lesserson L, Baker RA et al. Attenuating the systemic inflammatory response to adult cardiopulmonary bypass: a critical review of the evidence base. J Extra Corpor Technol 2014;46:197–211. [PMC free article] [PubMed] [Google Scholar]
- 111. Mangoush O, Purkayastha S, Haj-Yahia S, Kinross J, Hayward M, Bartolozzi F et al. Heparin-bonded circuits versus nonheparin-bonded circuits: an evaluation of their effect on clinical outcomes. Eur J Cardiothorac Surg 2007;31:1058–69. [DOI] [PubMed] [Google Scholar]
- 112. Svenmarker S, Haggmark S, Jansson E, Lindholm R, Appelblad M, Sandstrom E et al. Use of heparin-bonded circuits in cardiopulmonary bypass improves clinical outcome. Scand Cardiovasc J 2002;36:241–6. [DOI] [PubMed] [Google Scholar]
- 113. Ranucci M, Isgro G, Soro G, Canziani A, Menicanti L, Frigiola A. Reduced systemic heparin dose with phosphorylcholine coated closed circuit in coronary operations. Int J Artif Organs 2004;27:311–9. [DOI] [PubMed] [Google Scholar]
- 114.Institute of Medicine Committee on Data Standards for Patient Safety; Aspden P, Corrigan JM, Wolcott J, Erickson SM (eds). Patient Safety: Achieving a New Standard for Care. Washington, DC: National Academies Press (US; ), 2004. ISBN-10: 0-309-09077-6 [PubMed] [Google Scholar]
- 115. Weiser TG, Haynes AB. Ten years of the surgical safety checklist. Br J Surg 2018;105:927–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Spiess BD. The use of checklists as a method to reduce human error in cardiac operating rooms. Int Anesthesiol Clin 2013;51:179–94. [DOI] [PubMed] [Google Scholar]
- 117. Ginther R Jr, Fillingham R, Searles B, Darling E. Departmental use of perfusion crisis management drills: 2002 survey results. Perfusion 2003;18:299–302. [DOI] [PubMed] [Google Scholar]
- 118. Webb DP, Deegan RJ, Greelish JP, Byrne JG. Oxygenation failure during cardiopulmonary bypass prompts new safety algorithm and training initiative. J Extra Corpor Technol 2007;39:188–91. [PMC free article] [PubMed] [Google Scholar]
- 119. Spiess BD, Rotruck J, McCarthy H, Suarez-Wincosci O, Kasirajan V, Wahr J et al. Human factors analysis of a near-miss event: oxygen supply failure during cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2015;29:204–9. [DOI] [PubMed] [Google Scholar]
- 120. Petrik EW, Ho D, Elahi M, Ball TR, Hofkamp MP, Wehbe-Janek H et al. Checklist usage decreases critical task omissions when training residents to separate from simulated cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2014;28:1484–9. [DOI] [PubMed] [Google Scholar]
- 121. Groenenberg I, Weerwind PW, Everts PA, Maessen JG. Dutch perfusion incident survey. Perfusion 2010;25:329–36. [DOI] [PubMed] [Google Scholar]
- 122.The European Board of Cardiovascular Perfusion: Prebypass Checklist. https://www.ebcp.eu/login/files/b8192349de4ba7ced7dcb65c4f51ac29ae9d12c5.pdf (28 April 2019, date last accessed).
- 123. Flynn BC, de Perio M, Hughes E, Silvay G. The need for specialized preanesthesia clinics for day admission cardiac and major vascular surgery patients. Semin Cardiothorac Vasc Anesth 2009;13:241–8. [DOI] [PubMed] [Google Scholar]
- 124. Silvay G, Zafirova Z. Ten years experiences with preoperative evaluation clinic for day admission cardiac and major vascular surgical patients: model for “perioperative anesthesia and surgical home”. Semin Cardiothorac Vasc Anesth 2016;20:120–32. [DOI] [PubMed] [Google Scholar]
- 125. Kluger MT, Tham EJ, Coleman NA, Runciman WB, Bullock MF. Inadequate pre-operative evaluation and preparation: a review of 197 reports from the Australian incident monitoring study. Anaesthesia 2000;55:1173–8. [DOI] [PubMed] [Google Scholar]
- 126. Ausset S, Bouaziz H, Brosseau M, Kinirons B, Benhamou D. Improvement of information gained from the pre-anaesthetic visit through a quality-assurance programme. Br J Anaesth 2002;88:280–3. [DOI] [PubMed] [Google Scholar]
- 127. El-Essawi A, Hajek T, Skorpil J, Boning A, Sabol F, Ostrovsky Y et al. Are minimized perfusion circuits the better heart lung machines? Final results of a prospective randomized multicentre study. Perfusion 2011;26:470–8. [DOI] [PubMed] [Google Scholar]
- 128. Sakwa MP, Emery RW, Shannon FL, Altshuler JM, Mitchell D, Zwada D et al. Coronary artery bypass grafting with a minimized cardiopulmonary bypass circuit: a prospective, randomized trial. J Thorac Cardiovasc Surg 2009;137:481–5. [DOI] [PubMed] [Google Scholar]
- 129. Remadi JP, Rakotoarivelo Z, Marticho P, Benamar A. Prospective randomized study comparing coronary artery bypass grafting with the new mini-extracorporeal circulation Jostra System or with a standard cardiopulmonary bypass. Am Heart J 2006;151:198.. [DOI] [PubMed] [Google Scholar]
- 130. Anastasiadis K, Antonitsis P, Haidich AB, Argiriadou H, Deliopoulos A, Papakonstantinou C. Use of minimal extracorporeal circulation improves outcome after heart surgery; a systematic review and meta-analysis of randomized controlled trials. Int J Cardiol 2013;164:158–69. [DOI] [PubMed] [Google Scholar]
- 131. Harling L, Warren OJ, Martin A, Kemp PR, Evans PC, Darzi A et al. Do miniaturized extracorporeal circuits confer significant clinical benefit without compromising safety? A meta-analysis of randomized controlled trials. ASAIO J 2011;57:141–51. [DOI] [PubMed] [Google Scholar]
- 132. Kowalewski M, Pawliszak W, Kołodziejczak M, Navarese EP, Anisimowicz L. Anisimowicz L. 30-day mortality reduction with miniaturized extracorporeal circulation as compared to conventional cardiopulmonary bypass for coronary revascularization. Meta-analysis of randomized controlled trials. Int J Cardiol 2015;198:63–5. [DOI] [PubMed] [Google Scholar]
- 133. Phan K, Phan S, Yan TD. How firm is the evidence for miniaturized extracorporeal circulation versus conventional cardiopulmonary bypass for coronary revascularization? A trial sequential analysis. Int J Cardiol 2015;201:422–3. [DOI] [PubMed] [Google Scholar]
- 134. Abu-Omar Y, Cader S, Guerrieri Wolf L, Pigott D, Matthews PM, Taggart DP. Short-term changes in cerebral activity in on-pump and off-pump cardiac surgery defined by functional magnetic resonance imaging and their relationship to microembolization. J Thorac Cardiovasc Surg 2006;132:1119–25. [DOI] [PubMed] [Google Scholar]
- 135. Husebraten IM, Fiane AE, Ringdal MIL, Thiara A. Measurement of gaseous microemboli in the prime before the initiation of cardiopulmonary bypass. Perfusion 2018;33:30–5. [DOI] [PubMed] [Google Scholar]
- 136. Stehouwer MC, de Vroege R, Hoohenkerk GJF, Hofman FN, Kelder JC, Buchner B et al. Carbon dioxide flush of an integrated minimized perfusion circuit prior to priming prevents spontaneous air release into the arterial line during clinical use. Artif Organs 2017;41:997–1003. [DOI] [PubMed] [Google Scholar]
- 137. Benedetto U, Caputo M, Guida G, Bucciarelli-Ducci C, Thai J, Bryan A et al. Carbon dioxide insufflation during cardiac surgery: a meta-analysis of randomized controlled trials. Semin Thorac Cardiovasc Surg 2017;29:301–10. [DOI] [PubMed] [Google Scholar]
- 138. Ganguly G, Dixit V, Patrikar S, Venkatraman R, Gorthi SP, Tiwari N. Carbon dioxide insufflation and neurocognitive outcome of open heart surgery. Asian Cardiovasc Thorac Ann 2015;23:774–80. [DOI] [PubMed] [Google Scholar]
- 139. Keith JR, Puente AE. Deficiencies in the detection of cognitive deficits. Neuropsychology 2002;16:434–9. [PubMed] [Google Scholar]
- 140. Lewis MC, Nevo I, Paniagua MA, Ben-Ari A, Pretto E, Eisdorfer S et al. Uncomplicated general anesthesia in the elderly results in cognitive decline: does cognitive decline predict morbidity and mortality? Med Hypotheses 2007;68:484–92. [DOI] [PubMed] [Google Scholar]
- 141. Lewis MS, Maruff P, Silbert BS, Evered LA, Scott DA. Detection of postoperative cognitive decline after coronary artery bypass graft surgery is affected by the number of neuropsychological tests in the assessment battery. Ann Thorac Surg 2006;81:2097–104. [DOI] [PubMed] [Google Scholar]
- 142. Selnes OA, Gottesman RF. Neuropsychological outcomes after coronary artery bypass grafting. J Int Neuropsychol Soc 2010;16:221–6. [DOI] [PubMed] [Google Scholar]
- 143. Chaudhuri K, Storey E, Lee GA, Bailey M, Chan J, Rosenfeldt FL et al. Carbon dioxide insufflation in open-chamber cardiac surgery: a double-blind, randomized clinical trial of neurocognitive effects. J Thorac Cardiovasc Surg 2012;144:646–53. [DOI] [PubMed] [Google Scholar]
- 144. Svenarud P, Persson M, van der Linden J. Effect of CO2 insufflation on the number and behavior of air microemboli in open-heart surgery: a randomized clinical trial. Circulation 2004;109:1127–32. [DOI] [PubMed] [Google Scholar]
- 145. Landenhed M, Al-Rashidi F, Blomquist S, Hoglund P, Pierre L, Koul B. Systemic effects of carbon dioxide insufflation technique for de-airing in left-sided cardiac surgery. J Thorac Cardiovasc Surg 2014;147:295–300. [DOI] [PubMed] [Google Scholar]
- 146. Cook DJ, Plochl W, Orszulak TA. Effect of temperature and PaCO2 on cerebral embolization during cardiopulmonary bypass in swine. Ann Thorac Surg 2000;69:415–20. [DOI] [PubMed] [Google Scholar]
- 147. Gorter KA, Stehouwer MC, Van Putte BP, Vlot EA, Urbanus RT. Acidosis induced by carbon dioxide insufflation decreases heparin potency: a risk factor for thrombus formation. Perfusion 2017;32:214–9. [DOI] [PubMed] [Google Scholar]
- 148. Protsyk V, Rasmussen BS, Guarracino F, Erb J, Turton E, Ender J. Fluid management in cardiac surgery: results of a survey in European Cardiac Anesthesia Departments. J Cardiothorac Vasc Anesth 2017;31:1624–9. [DOI] [PubMed] [Google Scholar]
- 149. Svendsen OS, Farstad M, Mongstad A, Haaverstad R, Husby P, Kvalheim VL. Is the use of hydroxyethyl starch as priming solution during cardiac surgery advisable? A randomized, single-center trial. Perfusion 2018;33:483–9. [DOI] [PubMed] [Google Scholar]
- 150. Vanhoonacker J, Ongenae M, Vanoverschelde H, Donadoni R. Hydroxyethyl starch 130/0.4 versus modified fluid gelatin for cardiopulmonary bypass priming: the effects on postoperative bleeding and volume expansion needs after elective CABG. Acta Anaesthesiol Belg 2009;60:91–7. [PubMed] [Google Scholar]
- 151. Mutter TC, Ruth CA, Dart AB. Hydroxyethyl starch (HES) versus other fluid therapies: effects on kidney function. Cochrane Database Syst Rev 2013:CD007594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Miles LF, Coulson TG, Galhardo C, Falter F. Pump priming practices and anticoagulation in cardiac surgery: results from the global cardiopulmonary bypass survey. Anesth Analg 2017;125:1871–7. [DOI] [PubMed] [Google Scholar]
- 153. Zacharias M, Mugawar M, Herbison GP, Walker RJ, Hovhannisyan K, Sivalingam P et al. Interventions for protecting renal function in the perioperative period. Cochrane Database Syst Rev 2013:CD003590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Saczkowski R, Bernier PL, Tchervenkov CI, Arellano R. Retrograde autologous priming and allogeneic blood transfusions: a meta-analysis. Interact CardioVasc Thorac Surg 2009;8:373–6. [DOI] [PubMed] [Google Scholar]
- 155. Sun P, Ji B, Sun Y, Zhu X, Liu J, Long C et al. Effects of retrograde autologous priming on blood transfusion and clinical outcomes in adults: a meta-analysis. Perfusion 2013;28:238–43. [DOI] [PubMed] [Google Scholar]
- 156. Hou X, Yang F, Liu R, Yang J, Zhao Y, Wan C et al. Retrograde autologous priming of the cardiopulmonary bypass circuit reduces blood transfusion in small adults: a prospective, randomized trial. Eur J Anaesthesiol 2009;26:1061–6. [DOI] [PubMed] [Google Scholar]
- 157. Vandewiele K, Bove T, De Somer FM, Dujardin D, Vanackere M, De Smet D et al. The effect of retrograde autologous priming volume on haemodilution and transfusion requirements during cardiac surgery. Interact CardioVasc Thorac Surg 2013;16:778–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Murphy GS, Szokol JW, Nitsun M, Alspach DA, Avram MJ, Vender JS et al. The failure of retrograde autologous priming of the cardiopulmonary bypass circuit to reduce blood use after cardiac surgical procedures. Anesth Analg 2004;98:1201–7. [DOI] [PubMed] [Google Scholar]
- 159. Finley A, Greenberg C. Review article: heparin sensitivity and resistance: management during cardiopulmonary bypass. Anesth Analg 2013;116:1210–22. [DOI] [PubMed] [Google Scholar]
- 160. Boer C, Meesters MI, Veerhoek D, Vonk A. Anticoagulant and side-effects of protamine in cardiac surgery: a narrative review. Br J Anaesth 2018;120:914–27. [DOI] [PubMed] [Google Scholar]
- 161. Ovrum E, Tangen G, Tollofsrud S, Skeie B, Ringdal MA, Istad R et al. Heparinized cardiopulmonary bypass circuits and low systemic anticoagulation: an analysis of nearly 6000 patients undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg 2011;141:1145–9. [DOI] [PubMed] [Google Scholar]
- 162. Shapira OM, Korach A, Pinaud F, Dabah A, Bao Y, Corbeau JJ et al. Safety and efficacy of biocompatible perfusion strategy in a contemporary series of patients undergoing coronary artery bypass grafting—a two-center study. J Cardiothorac Surg 2014;9:196.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Bauer A, Hausmann H, Schaarschmidt J, Szlapka M, Scharpenberg M, Eberle T et al. Is 300 seconds ACT safe and efficient during MiECC procedures? Thorac Cardiovasc Surg 2019;67:191–202. [DOI] [PubMed] [Google Scholar]
- 164. Avidan MS, Alcock EL, Da Fonseca J, Ponte J, Desai JB, Despotis GJ et al. Comparison of structured use of routine laboratory tests or near-patient assessment with clinical judgement in the management of bleeding after cardiac surgery. Br J Anaesth 2004;92:178–86. [DOI] [PubMed] [Google Scholar]
- 165. Hoenicka M, Rupp P, Muller-Eising K, Deininger S, Kunert A, Liebold A et al. Anticoagulation management during multivessel coronary artery bypass grafting: a randomized trial comparing individualized heparin management and conventional hemostasis management. J Thromb Haemost 2015;13:1196–206. [DOI] [PubMed] [Google Scholar]
- 166. Vonk AB, Veerhoek D, van den Brom CE, van Barneveld LJ, Boer C. Individualized heparin and protamine management improves rotational thromboelastometric parameters and postoperative hemostasis in valve surgery. J Cardiothorac Vasc Anesth 2014;28:235–41. [DOI] [PubMed] [Google Scholar]
- 167. Slight RD, Buell R, Nzewi OC, McClelland DB, Mankad PS. A comparison of activated coagulation time-based techniques for anticoagulation during cardiac surgery with cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2008;22:47–52. [DOI] [PubMed] [Google Scholar]
- 168. Radulovic V, Laffin A, Hansson KM, Backlund E, Baghaei F, Jeppsson A. Heparin and protamine titration does not improve haemostasis after cardiac surgery: a prospective randomized study. PLoS One 2015;10:e0130271.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Noui N, Zogheib E, Walczak K, Werbrouck A, Amar AB, Dupont H et al. Anticoagulation monitoring during extracorporeal circulation with the Hepcon/HMS device. Perfusion 2012;27:214–20. [DOI] [PubMed] [Google Scholar]
- 170. Teoh KH, Young E, Blackall MH, Roberts RS, Hirsh J. Can extra protamine eliminate heparin rebound following cardiopulmonary bypass surgery? J Thorac Cardiovasc Surg 2004;128:211–9. [DOI] [PubMed] [Google Scholar]
- 171. Koster A, Borgermann J, Gummert J, Rudloff M, Zittermann A, Schirmer U. Protamine overdose and its impact on coagulation, bleeding, and transfusions after cardiopulmonary bypass: results of a randomized double-blind controlled pilot study. Clin Appl Thromb Hemost 2014;20:290–5. [DOI] [PubMed] [Google Scholar]
- 172. Meesters MI, Veerhoek D, de Lange F, de Vries JW, de Jong JR, Romijn JW et al. Effect of high or low protamine dosing on postoperative bleeding following heparin anticoagulation in cardiac surgery. A randomised clinical trial. Thromb Haemost 2016;116:251–61. [DOI] [PubMed] [Google Scholar]
- 173. Hofmann B, Bushnaq H, Kraus FB, Raspe C, Simm A, Silber RE et al. Immediate effects of individualized heparin and protamine management on hemostatic activation and platelet function in adult patients undergoing cardiac surgery with tranexamic acid antifibrinolytic therapy. Perfusion 2013;28:412–8. [DOI] [PubMed] [Google Scholar]
- 174. Koster A, Faraoni D, Levy JH. Argatroban and bivalirudin for perioperative anticoagulation in cardiac surgery. Anesthesiology 2018;128:390–400. [DOI] [PubMed] [Google Scholar]
- 175. Warkentin TE, Koster A. Bivalirudin: a review. Expert Opin Pharmacother 2005;6:1349–71. [DOI] [PubMed] [Google Scholar]
- 176. Dyke CM, Smedira NG, Koster A, Aronson S, McCarthy HL 2nd, Kirshner R et al. A comparison of bivalirudin to heparin with protamine reversal in patients undergoing cardiac surgery with cardiopulmonary bypass: the EVOLUTION-ON study. J Thorac Cardiovasc Surg 2006;131:533–9. [DOI] [PubMed] [Google Scholar]
- 177. Ranucci M, Baryshnikova E, Simeone F, Ranucci M, Scolletta S. Moderate-degree acidosis is an independent determinant of postoperative bleeding in cardiac surgery. Minerva Anestesiol 2015;81:885–93. [PubMed] [Google Scholar]
- 178. Hajjar LA, Almeida JP, Fukushima JT, Rhodes A, Vincent JL, Osawa EA et al. High lactate levels are predictors of major complications after cardiac surgery. J Thorac Cardiovasc Surg 2013;146:455–60. [DOI] [PubMed] [Google Scholar]
- 179. Stephan H, Weyland A, Kazmaier S, Henze T, Menck S, Sonntag H. Acid-base management during hypothermic cardiopulmonary bypass does not affect cerebral metabolism but does affect blood flow and neurological outcome. Br J Anaesth 1992;69:51–7. [DOI] [PubMed] [Google Scholar]
- 180. Patel RL, Turtle MR, Chambers DJ, James DN, Newman S, Venn GE. Alpha-stat acid-base regulation during cardiopulmonary bypass improves neuropsychologic outcome in patients undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg 1996;111:1267–79. [DOI] [PubMed] [Google Scholar]
- 181. Murkin JM, Martzke JS, Buchan AM, Bentley C, Wong CJ. A randomized study of the influence of perfusion technique and pH management strategy in 316 patients undergoing coronary artery bypass surgery. II. Neurologic and cognitive outcomes. J Thorac Cardiovasc Surg 1995;110:349–62. [DOI] [PubMed] [Google Scholar]
- 182. Base EM, Standl T, Lassnigg A, Skhirtladze K, Jungheinrich C, Gayko D et al. Efficacy and safety of hydroxyethyl starch 6% 130/0.4 in a balanced electrolyte solution (Volulyte) during cardiac surgery. J Cardiothorac Vasc Anesth 2011;25:407–14. [DOI] [PubMed] [Google Scholar]
- 183. De Oliveira GS Jr, Knautz JS, Sherwani S, McCarthy RJ. Systemic magnesium to reduce postoperative arrhythmias after coronary artery bypass graft surgery: a meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth 2012;26:643–50. [DOI] [PubMed] [Google Scholar]
- 184. Klinger RY, Thunberg CA, White WD, Fontes M, Waldron NH, Piccini JP et al. Intraoperative magnesium administration does not reduce postoperative atrial fibrillation after cardiac surgery. Anesth Analg 2015;121:861–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Healthcare Improvement Scotland: SIGN 152, Cardiac Arrhythmias in Coronary Artery Heart Disease. https://www.sign.ac.uk/assets/sign152.pdf (24 July 2019, date last accessed).
- 186. Vedel AG, Holmgaard F, Rasmussen LS, Langkilde A, Paulson OB, Lange T et al. High-target versus low-target blood pressure management during cardiopulmonary bypass to prevent cerebral injury in cardiac surgery patients: a randomized controlled trial. Circulation 2018;137:1770–80. [DOI] [PubMed] [Google Scholar]
- 187. Charlson ME, Peterson JC, Krieger KH, Hartman GS, Hollenberg JP, Briggs WM et al. Improvement of outcomes after coronary artery bypass II: a randomized trial comparing intraoperative high versus customized mean arterial pressure. J Cardiac Surgery 2007;22:465–72. [DOI] [PubMed] [Google Scholar]
- 188. Gold JP, Charlson ME, Williams-Russo P, Szatrowski TP, Peterson JC, Pirraglia PA et al. Improvement of outcomes after coronary artery bypass. A randomized trial comparing intraoperative high versus low mean arterial pressure. J Thorac Cardiovasc Surg 1995;110:1302–11. [DOI] [PubMed] [Google Scholar]
- 189. Siepe M, Pfeiffer T, Gieringer A, Zemann S, Benk C, Schlensak C et al. Increased systemic perfusion pressure during cardiopulmonary bypass is associated with less early postoperative cognitive dysfunction and delirium. Eur J Cardiothorac Surg 2011;40:200–7. [DOI] [PubMed] [Google Scholar]
- 190. Kanji HD, Schulze CJ, Hervas-Malo M, Wang P, Ross DB, Zibdawi M et al. Difference between pre-operative and cardiopulmonary bypass mean arterial pressure is independently associated with early cardiac surgery-associated acute kidney injury. J Cardiothorac Surg 2010;5:71.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Haase M, Bellomo R, Story D, Letis A, Klemz K, Matalanis G et al. Effect of mean arterial pressure, haemoglobin and blood transfusion during cardiopulmonary bypass on post-operative acute kidney injury. Nephrol Dial Transplant 2012;27:153–60. [DOI] [PubMed] [Google Scholar]
- 192. Hori D, Nomura Y, Ono M, Joshi B, Mandal K, Cameron D et al. Optimal blood pressure during cardiopulmonary bypass defined by cerebral autoregulation monitoring. J Thorac Cardiovasc Surg 2017;154:1590–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Hori D, Max L, Laflam A, Brown C, Neufeld KJ, Adachi H et al. Blood pressure deviations from optimal mean arterial pressure during cardiac surgery measured with a novel monitor of cerebral blood flow and risk for perioperative delirium: a pilot study. J Cardiothorac Vasc Anesth 2016;30:606–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Fischer GW, Levin MA. Vasoplegia during cardiac surgery: current concepts and management. Semin Thorac Cardiovasc Surg 2010;22:140–4. [DOI] [PubMed] [Google Scholar]
- 195. Noto A, Lentini S, Versaci A, Giardina M, Risitano DC, Messina R et al. A retrospective analysis of terlipressin in bolus for the management of refractory vasoplegic hypotension after cardiac surgery. Interact CardioVasc Thorac Surg 2009;9:588–92. [DOI] [PubMed] [Google Scholar]
- 196. Maslow AD, Stearns G, Butala P, Batula P, Schwartz CS, Gough J et al. The hemodynamic effects of methylene blue when administered at the onset of cardiopulmonary bypass. Anesth Analg 2006;103:2–8. [DOI] [PubMed] [Google Scholar]
- 197. Papadopoulos G, Sintou E, Siminelakis S, Koletsis E, Baikoussis NG, Apostolakis E. Perioperative infusion of low-dose of vasopressin for prevention and management of vasodilatory vasoplegic syndrome in patients undergoing coronary artery bypass grafting—a double-blind randomized study. J Cardiothorac Surg 2010;5:17.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Cai Y, Mack A, Ladlie BL, Martin AK. The use of intravenous hydroxocobalamin as a rescue in methylene blue-resistant vasoplegic syndrome in cardiac surgery. Ann Card Anaesth 2017;20:462–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Magruder JT, Crawford TC, Harness HL, Grimm JC, Suarez-Pierre A, Wierschke C et al. A pilot goal-directed perfusion initiative is associated with less acute kidney injury after cardiac surgery. J Thorac Cardiovasc Surg 2017;153:118–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Blessing JM, Riley JB. Lean flow: optimizing cardiopulmonary bypass equipment and flow for obese patients—a technique article. J Extra Corpor Technol 2017;49:30–5. [PMC free article] [PubMed] [Google Scholar]
- 201. Alston RP, Anderson A, Sanger K. Is body surface area still the best way to determine pump flow rate during cardiopulmonary bypass? Perfusion 2006;21:139–47. [DOI] [PubMed] [Google Scholar]
- 202. Ranucci M, Romitti F, Isgro G, Cotza M, Brozzi S, Boncilli A et al. Oxygen delivery during cardiopulmonary bypass and acute renal failure after coronary operations. Ann Thorac Surg 2005;80:2213–20. [DOI] [PubMed] [Google Scholar]
- 203. de Somer F, Mulholland JW, Bryan MR, Aloisio T, Van Nooten GJ, Ranucci M. O2 delivery and CO2 production during cardiopulmonary bypass as determinants of acute kidney injury: time for a goal-directed perfusion management? Crit Care 2011;15:R192.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Magruder JT, Dungan SP, Grimm JC, Harness HL, Wierschke C, Castillejo S et al. Nadir oxygen delivery on bypass and hypotension increase acute kidney injury risk after cardiac operations. Ann Thorac Surg 2015;100:1697–703. [DOI] [PubMed] [Google Scholar]
- 205. Ellis RJ, Wisniewski A, Potts R, Calhoun C, Loucks P, Wells MR. Reduction of flow rate and arterial pressure at moderate hypothermia does not result in cerebral dysfunction. J Thorac Cardiovasc Surg 1980;79:173–80. [PubMed] [Google Scholar]
- 206. Slogoff S, Reul GJ, Keats AS, Curry GR, Crum ME, Elmquist BA et al. Role of perfusion pressure and flow in major organ dysfunction after cardiopulmonary bypass. Ann Thorac Surg 1990;50:911–8. [DOI] [PubMed] [Google Scholar]
- 207. Kolkka R, Hilberman M. Neurologic dysfunction following cardiac operation with low-flow, low-pressure cardiopulmonary bypass. J Thorac Cardiovasc Surg 1980;79:432–7. [PubMed] [Google Scholar]
- 208. Bennett MJ, Rajakaruna C, Bazerbashi S, Webb G, Gomez-Cano M, Lloyd C. Oxygen delivery during cardiopulmonary bypass (and renal outcome) using two systems of extracorporeal circulation: a retrospective review. Interact CardioVasc Thorac Surg 2013;16:760–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Demers P, Elkouri S, Martineau R, Couturier A, Cartier R. Outcome with high blood lactate levels during cardiopulmonary bypass in adult cardiac operation. Ann Thorac Surg 2000;70:2082–6. [DOI] [PubMed] [Google Scholar]
- 210. Smulter N, Lingehall HC, Gustafson Y, Olofsson B, Engstrom KG, Appelblad M et al. Disturbances in oxygen balance during cardiopulmonary bypass: a risk factor for postoperative delirium. J Cardiothorac Vasc Anesth 2018;32:684–90. [DOI] [PubMed] [Google Scholar]
- 211. Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg 2007;104:51–8. [DOI] [PubMed] [Google Scholar]
- 212. Svenmarker S, Hannuksela M, Haney M. A retrospective analysis of the mixed venous oxygen saturation as the target for systemic blood flow control during cardiopulmonary bypass. Perfusion 2018;33:453–62. [DOI] [PubMed] [Google Scholar]
- 213. Ranucci M, Johnson I, Willcox T, Baker RA, Boer C, Baumann A et al. Goal-directed perfusion to reduce acute kidney injury: a randomized trial. J Thorac Cardiovasc Surg 2018;156:1918–27. [DOI] [PubMed] [Google Scholar]
- 214. Haines N, Wang S, Undar A, Alkan T, Akcevin A. Clinical outcomes of pulsatile and non-pulsatile mode of perfusion. J Extra Corpor Technol 2009;41:P26–9. [PMC free article] [PubMed] [Google Scholar]
- 215. Mavroudis C. To pulse or not to pulse. Ann Thorac Surg 1978;25:259–71. [DOI] [PubMed] [Google Scholar]
- 216. Sievert A, Sistino J. A meta-analysis of renal benefits to pulsatile perfusion in cardiac surgery. J Extra Corpor Technol 2012;44:10–4. [PMC free article] [PubMed] [Google Scholar]
- 217. Nam MJ, Lim CH, Kim HJ, Kim YH, Choi H, Son HS et al. A meta-analysis of renal function after adult cardiac surgery with pulsatile perfusion. Artif Organs 2015;39:788–94. [DOI] [PubMed] [Google Scholar]
- 218. Lim CH, Nam MJ, Lee JS, Kim HJ, Kim JY, Shin HW et al. A meta-analysis of pulmonary function with pulsatile perfusion in cardiac surgery. Artif Organs 2015;39:110–7. [DOI] [PubMed] [Google Scholar]
- 219. Sezai A, Shiono M, Nakata K, Hata M, Iida M, Saito A et al. Effects of pulsatile CPB on interleukin-8 and endothelin-1 levels. Artif Organs 2005;29:708–13. [DOI] [PubMed] [Google Scholar]
- 220. Driessen JJ, Dhaese H, Fransen G, Verrolst P, Rondelez L, Gevaert L et al. Pulsatile compared with nonpulsatile perfusion using a centrifugal pump for cardiopulmonary bypass during coronary artery bypass grafting. Effects on systemic haemodynamics, oxygenation, and inflammatory response parameters. Perfusion 1995;10:3–12. [DOI] [PubMed] [Google Scholar]
- 221. Koning NJ, Vonk AB, van Barneveld LJ, Beishuizen A, Atasever B, van den Brom CE et al. Pulsatile flow during cardiopulmonary bypass preserves postoperative microcirculatory perfusion irrespective of systemic hemodynamics. J Appl Physiol (1985) 2012;112:1727–34. [DOI] [PubMed] [Google Scholar]
- 222. Onorati F, Santarpino G, Tangredi G, Palmieri G, Rubino AS, Foti D et al. Intra-aortic balloon pump induced pulsatile perfusion reduces endothelial activation and inflammatory response following cardiopulmonary bypass. Eur J Cardiothorac Surg 2009;35:1012–9. [DOI] [PubMed] [Google Scholar]
- 223. Landoni G, Augoustides JG, Guarracino F, Santini F, Ponschab M, Pasero D et al. Mortality reduction in cardiac anesthesia and intensive care: results of the first International Consensus Conference. Acta Anaesthesiol Scand 2011;55:259–66. [DOI] [PubMed] [Google Scholar]
- 224. Lomivorotov VV, Efremov SM, Kirov MY, Fominskiy EV, Karaskov AM. Low-cardiac-output syndrome after cardiac surgery. J Cardiothorac Vasc Anesth 2017;31:291–308. [DOI] [PubMed] [Google Scholar]
- 225. Cecconi M, Rhodes A. Goal-directed therapy: time to move on? Anesth Analg 2014;119:516–8. [DOI] [PubMed] [Google Scholar]
- 226. Goepfert MS, Richter HP, Zu Eulenburg C, Gruetzmacher J, Rafflenbeul E, Roeher K et al. Individually optimized hemodynamic therapy reduces complications and length of stay in the intensive care unit: a prospective, randomized controlled trial. Anesthesiology 2013;119:824–36. [DOI] [PubMed] [Google Scholar]
- 227. McKendry M, McGloin H, Saberi D, Caudwell L, Brady AR, Singer M. Randomised controlled trial assessing the impact of a nurse delivered, flow monitored protocol for optimisation of circulatory status after cardiac surgery. BMJ 2004;329:258.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Osawa EA, Rhodes A, Landoni G, Galas FR, Fukushima JT, Park CH et al. Effect of perioperative goal-directed hemodynamic resuscitation therapy on outcomes following cardiac surgery: a randomized clinical trial and systematic review. Crit Care Med 2016;44:724–33. [DOI] [PubMed] [Google Scholar]
- 229. Parke RL, McGuinness SP, Gilder E, McCarthy LW, Cowdrey KA. A randomised feasibility study to assess a novel strategy to rationalise fluid in patients after cardiac surgery. Br J Anaesth 2015;115:45–52. [DOI] [PubMed] [Google Scholar]
- 230. Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg 2000;90:1052–9. [DOI] [PubMed] [Google Scholar]
- 231. Li P, Qu LP, Qi D, Shen B, Wang YM, Xu JR et al. Significance of perioperative goal-directed hemodynamic approach in preventing postoperative complications in patients after cardiac surgery: a meta-analysis and systematic review. Ann Med 2017;49:343–51. [DOI] [PubMed] [Google Scholar]
- 232. Wang S, Undar A. Vacuum-assisted venous drainage and gaseous microemboli in cardiopulmonary bypass. J Extra Corpor Technol 2008;40:249–56. [PMC free article] [PubMed] [Google Scholar]
- 233. Colangelo N, Torracca L, Lapenna E, Moriggia S, Crescenzi G, Alfieri O. Vacuum-assisted venous drainage in extrathoracic cardiopulmonary bypass management during minimally invasive cardiac surgery. Perfusion 2006;21:361–5. [DOI] [PubMed] [Google Scholar]
- 234. Pappalardo F, Corno C, Franco A, Giardina G, Scandroglio AM, Landoni G et al. Reduction of hemodilution in small adults undergoing open heart surgery: a prospective, randomized trial. Perfusion 2007;22:317–22. [DOI] [PubMed] [Google Scholar]
- 235. Gambino R, Searles B, Darling EM. Vacuum-assisted venous drainage: a 2014 safety survey. J Extra Corpor Technol 2015;47:160–6. [PMC free article] [PubMed] [Google Scholar]
- 236. Goksedef D, Omeroglu SN, Balkanay OO, Denli Yalvac ES, Talas Z, Albayrak A et al. Hemolysis at different vacuum levels during vacuum-assisted venous drainage: a prospective randomized clinical trial. Thorac Cardiovasc Surg 2012;60:262–8. [DOI] [PubMed] [Google Scholar]
- 237. Jones TJ, Deal DD, Vernon JC, Blackburn N, Stump DA. Does vacuum-assisted venous drainage increase gaseous microemboli during cardiopulmonary bypass? Ann Thorac Surg 2002;74:2132–7. [DOI] [PubMed] [Google Scholar]
- 238. Fang WC, Helm RE, Krieger KH, Rosengart TK, DuBois WJ, Sason C et al. Impact of minimum hematocrit during cardiopulmonary bypass on mortality in patients undergoing coronary artery surgery. Circulation 1997;96(9 Suppl): II-194–9. [PubMed] [Google Scholar]
- 239. Swaminathan M, Phillips-Bute BG, Conlon PJ, Smith PK, Newman MF, Stafford-Smith M. The association of lowest hematocrit during cardiopulmonary bypass with acute renal injury after coronary artery bypass surgery. Ann Thorac Surg 2003;76:784–91. [DOI] [PubMed] [Google Scholar]
- 240. Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah A. Adverse effects of low hematocrit during cardiopulmonary bypass in the adult: should current practice be changed? J Thorac Cardiovasc Surg 2003;125:1438–50. [DOI] [PubMed] [Google Scholar]
- 241. Ariturk C, Ozgen ZS, Kilercik M, Ulugol H, Okten EM, Aksu U et al. Comparative effects of hemodilutional anemia and transfusion during cardiopulmonary bypass on acute kidney injury: a prospective randomized study. Heart Surg Forum 2015;18:E154–60. [DOI] [PubMed] [Google Scholar]
- 242. Shehata N, Burns LA, Nathan H, Hebert P, Hare GM, Fergusson D et al. A randomized controlled pilot study of adherence to transfusion strategies in cardiac surgery. Transfusion 2012;52:91–9. [DOI] [PubMed] [Google Scholar]
- 243. Ranucci M, Castelvecchio S, Ditta A, Brozzi S, Boncilli A, Baryshnikova E et al. Transfusions during cardiopulmonary bypass: better when triggered by venous oxygen saturation and oxygen extraction rate. Perfusion 2011;26:327–33. [DOI] [PubMed] [Google Scholar]
- 244.Society of Thoracic Surgeons Blood Conservation Guideline Task Force, Ferraris VA, Brown JR, Despotis GJ, Hammon JW, Reece TB, Saha SP. et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. Ann Thorac Surg 2011;91:944–82. [DOI] [PubMed] [Google Scholar]
- 245. Spiess BD. Treating heparin resistance with antithrombin or fresh frozen plasma. Ann Thorac Surg 2008;85:2153–60. [DOI] [PubMed] [Google Scholar]
- 246. Williams MR, D’Ambra AB, Beck JR, Spanier TB, Morales DLS, Helman DN et al. A randomized trial of antithrombin concentrate for treatment of heparin resistance. Ann Thorac Surg 2000;70:873–7. [DOI] [PubMed] [Google Scholar]
- 247. Lemmer JH Jr, Despotis GJ. Antithrombin III concentrate to treat heparin resistance in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg 2002;123:213–7. [DOI] [PubMed] [Google Scholar]
- 248. Casbard AC, Williamson LM, Murphy MF, Rege K, Johnson T. The role of prophylactic fresh frozen plasma in decreasing blood loss and correcting coagulopathy in cardiac surgery. A systematic review. Anaesthesia 2004;59:550–8. [DOI] [PubMed] [Google Scholar]
- 249. Desborough M, Sandu R, Brunskill SJ, Doree C, Trivella M, Montedori A et al. Fresh frozen plasma for cardiovascular surgery. Cochrane Database Syst Rev 2015:CD007614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Barry AE, Chaney MA, London MJ. Anesthetic management during cardiopulmonary bypass: a systematic review. Anesth Analg 2015;120:749–69. [DOI] [PubMed] [Google Scholar]
- 251. Uhlig C, Bluth T, Schwarz K, Deckert S, Heinrich L, De Hert S et al. Effects of volatile anesthetics on mortality and postoperative pulmonary and other complications in patients undergoing surgery: a systematic review and meta-analysis. Anesthesiology 2016;124:1230–45. [DOI] [PubMed] [Google Scholar]
- 252. Bignami E, Guarnieri M, Pieri M, De Simone F, Rodriguez A, Cassara L et al. Volatile anaesthetics added to cardiopulmonary bypass are associated with reduced cardiac troponin. Perfusion 2017;32:547–53. [DOI] [PubMed] [Google Scholar]
- 253. Landoni G, Lomivorotov VV, Nigro Neto C, Monaco F, Pasyuga VV, Bradic N et al. Volatile anesthetics versus total intravenous anesthesia for cardiac surgery. N Engl J Med 2019;380:1214–25. [DOI] [PubMed] [Google Scholar]
- 254. Nussmeier NA, Lambert ML, Moskowitz GJ, Cohen NH, Weiskopf RB, Fisher DM et al. Washin and washout of isoflurane administered via bubble oxygenators during hypothermic cardiopulmonary bypass. Anesthesiology 1989;71:519–25. [DOI] [PubMed] [Google Scholar]
- 255. Zhou JX, Liu J. Dynamic changes in blood solubility of desflurane, isoflurane, and halothane during cardiac surgery. J Cardiothorac Vasc Anesth 2001;15:555–9. [DOI] [PubMed] [Google Scholar]
- 256. Liu EH, Dhara SS. Monitoring oxygenator expiratory isoflurane concentrations and the bispectral index to guide isoflurane requirements during cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2005;19:485–7. [DOI] [PubMed] [Google Scholar]
- 257. Chandran Mahaldar DA, Gadhinglajkar S, Sreedhar R. Sevoflurane requirement to maintain bispectral index-guided steady-state level of anesthesia during the rewarming phase of cardiopulmonary bypass with moderate hypothermia. J Cardiothorac Vasc Anesth 2013;27:59–62. [DOI] [PubMed] [Google Scholar]
- 258. Doi M, Gajraj RJ, Mantzaridis H, Kenny GN. Effects of cardiopulmonary bypass and hypothermia on electroencephalographic variables. Anaesthesia 1997;52:1048–55. [DOI] [PubMed] [Google Scholar]
- 259. Mathew JP, Weatherwax KJ, East CJ, White WD, Reves JG. Bispectral analysis during cardiopulmonary bypass: the effect of hypothermia on the hypnotic state. J Clin Anesth 2001;13:301–5. [DOI] [PubMed] [Google Scholar]
- 260. Ng KT, Alston RP, Just G, McKenzie C. Assessing the depth of isoflurane anaesthesia during cardiopulmonary bypass. Perfusion 2018;33:148–55. [DOI] [PubMed] [Google Scholar]
- 261. Grocott HP, Sato Y, Homi HM, Smith BE. The influence of xenon, nitrous oxide and nitrogen on gas bubble expansion during cardiopulmonary bypass. Eur J Anaesthesiol 2005;22:353–8. [DOI] [PubMed] [Google Scholar]
- 262. Houltz E, Caidahl K, Hellstrom A, Gustavsson T, Milocco I, Ricksten SE. The effects of nitrous oxide on left ventricular systolic and diastolic performance before and after cardiopulmonary bypass: evaluation by computer-assisted two-dimensional and Doppler echocardiography in patients undergoing coronary artery surgery. Anesth Analg 1995;81:243–8. [DOI] [PubMed] [Google Scholar]
- 263. Hudson RJ, Thomson IR, Jassal R. Effects of cardiopulmonary bypass on sufentanil pharmacokinetics in patients undergoing coronary artery bypass surgery. Anesthesiology 2004;101:862–71. [DOI] [PubMed] [Google Scholar]
- 264. Hudson RJ, Thomson IR, Jassal R, Peterson DJ, Brown AD, Freedman JI. Cardiopulmonary bypass has minimal effects on the pharmacokinetics of fentanyl in adults. Anesthesiology 2003;99:847–54. [DOI] [PubMed] [Google Scholar]
- 265. Michelsen LG, Holford NH, Lu W, Hoke JF, Hug CC, Bailey JM. The pharmacokinetics of remifentanil in patients undergoing coronary artery bypass grafting with cardiopulmonary bypass. Anesth Analg 2001;93:1100–5. [DOI] [PubMed] [Google Scholar]
- 266. Hammaren E, Yli-Hankala A, Rosenberg PH, Hynynen M. Cardiopulmonary bypass-induced changes in plasma concentrations of propofol and in auditory evoked potentials. Br J Anaesth 1996;77:360–4. [DOI] [PubMed] [Google Scholar]
- 267. Pandit JJ, Andrade J, Bogod DG, Hitchman JM, Jonker WR, Lucas N et al. 5th National Audit Project (NAP5) on accidental awareness during general anaesthesia: summary of main findings and risk factors. Br J Anaesth 2014;113:549–59. [DOI] [PubMed] [Google Scholar]
- 268. Harper NJN, Cook TM, Garcez T, Lucas DN, Thomas M, Kemp H et al. Anaesthesia, surgery, and life-threatening allergic reactions: management and outcomes in the 6th National Audit Project (NAP6). Br J Anaesth 2018;121:172–88. [DOI] [PubMed] [Google Scholar]
- 269. Dieleman JM, Nierich AP, Rosseel PM, van der Maaten JM, Hofland J, Diephuis JC et al. Intraoperative high-dose dexamethasone for cardiac surgery: a randomized controlled trial. JAMA 2012;308:1761–7. [DOI] [PubMed] [Google Scholar]
- 270. Whitlock RP, Devereaux PJ, Teoh KH, Lamy A, Vincent J, Pogue J et al. Methylprednisolone in patients undergoing cardiopulmonary bypass (SIRS): a randomised, double-blind, placebo-controlled trial. Lancet 2015;386:1243–53. [DOI] [PubMed] [Google Scholar]
- 271. Dvirnik N, Belley-Cote EP, Hanif H, Devereaux PJ, Lamy A, Dieleman JM et al. Steroids in cardiac surgery: a systematic review and meta-analysis. Br J Anaesth 2018;120:657–67. [DOI] [PubMed] [Google Scholar]
- 272. Myles PS, Dieleman JM, Forbes A, Heritier S, Smith JA. Dexamethasone for Cardiac Surgery trial (DECS-II): rationale and a novel, practice preference-randomized consent design. Am Heart J 2018;204:52–7. [DOI] [PubMed] [Google Scholar]
- 273. Haga KK, McClymont KL, Clarke S, Grounds RS, Ng KY, Glyde DW et al. The effect of tight glycaemic control, during and after cardiac surgery, on patient mortality and morbidity: a systematic review and meta-analysis. J Cardiothorac Surg 2011;6:3.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Tsai LL, Jensen HA, Thourani VH. Intensive glycemic control in cardiac surgery. Curr Diab Rep 2016;16:25.. [DOI] [PubMed] [Google Scholar]
- 275. Habertheuer A, Kocher A, Laufer G, Andreas M, Szeto WY, Petzelbauer P et al. Cardioprotection: a review of current practice in global ischemia and future translational perspective. Biomed Res Int 2014;2014:1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Ovrum E, Tangen G, Tollofsrud S, Oystese R, Ringdal MA, Istad R. Cold blood cardioplegia versus cold crystalloid cardioplegia: a prospective randomized study of 1440 patients undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg 2004;128:860–5. [DOI] [PubMed] [Google Scholar]
- 277. Ovrum E, Tangen G, Tollofsrud S, Oystese R, Ringdal MA, Istad R. Cold blood versus cold crystalloid cardioplegia: a prospective randomised study of 345 aortic valve patients. Eur J Cardiothorac Surg 2010;38:745–9. [DOI] [PubMed] [Google Scholar]
- 278. Guru V, Omura J, Alghamdi AA, Weisel R, Fremes SE. Is blood superior to crystalloid cardioplegia? A meta-analysis of randomized clinical trials. Circulation 2006;114(1 Suppl): I331–8. [DOI] [PubMed] [Google Scholar]
- 279. Sa MP, Rueda FG, Ferraz PE, Chalegre ST, Vasconcelos FP, Lima RC. Is there any difference between blood and crystalloid cardioplegia for myocardial protection during cardiac surgery? A meta-analysis of 5576 patients from 36 randomized trials. Perfusion 2012;27:535–46. [DOI] [PubMed] [Google Scholar]
- 280. Günday M, Bingöl H. Is crystalloid cardioplegia a strong predictor of intra-operative hemodilution? J Cardiothorac Surg 2014;9:23.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Dagenais F, Pelletier LC, Carrier M. Antegrade/retrograde cardioplegia for valve replacement: a prospective study. Ann Thorac Surg 1999;68:1681–5. [DOI] [PubMed] [Google Scholar]
- 282. Gates RN, Laks H, Drinkwater DC, Pearl JM, Zaragoza AM, Lewis W et al. Gross and microvascular distribution of retrograde cardioplegia in explanted human hearts. Ann Thorac Surg 1993;56:410–6. [DOI] [PubMed] [Google Scholar]
- 283. Radmehr H, Soleimani A, Tatari H, Salehi M. Does combined antegrade-retrograde cardioplegia have any superiority over antegrade cardioplegia? Heart Lung Circ 2008;17:475–7. [DOI] [PubMed] [Google Scholar]
- 284. Onorati F, Renzulli A, De Feo M, Santarpino G, Gregorio R, Biondi A et al. Does antegrade blood cardioplegia alone provide adequate myocardial protection in patients with left main stem disease? J Thorac Cardiovasc Surg 2003;126:1345–51. [DOI] [PubMed] [Google Scholar]
- 285. Siddiqi S, Blackstone EH, Bakaeen FG. Bretschneider and del Nido solutions: are they safe for coronary artery bypass grafting? If so, how should we use them? J Card Surg 2018;33:229–34. [DOI] [PubMed] [Google Scholar]
- 286. Li Y, Lin H, Zhao Y, Li Z, Liu D, Wu X et al. Del Nido cardioplegia for myocardial protection in adult cardiac surgery: a systematic review and meta-analysis. Asaio J 2018;64:360–7. [DOI] [PubMed] [Google Scholar]
- 287. Allen BS, Buckberg GD, Schwaiger M, Yeatman L, Tillisch J, Kawata N et al. Early recovery of regional wall motion in patients following surgical revascularization after eight hours of acute coronary occlusion. J Thorac Cardiovasc Surg 1986;92:636–48. [PubMed] [Google Scholar]
- 288. Fan Y, Zhang AM, Xiao YB, Weng YG, Hetzer R. Warm versus cold cardioplegia for heart surgery: a meta-analysis. Eur J Cardiothorac Surg 2010;37:912–9. [DOI] [PubMed] [Google Scholar]
- 289. Mallidi HR, Sever J, Tamariz M, Singh S, Hanayama N, Christakis GT et al. The short-term and long-term effects of warm or tepid cardioplegia. J Thorac Cardiovasc Surg 2003;125:711–20. [DOI] [PubMed] [Google Scholar]
- 290. Caputo M, Dihmis WC, Bryan AJ, Suleiman MS, Angelini GD. Warm blood hyperkalaemic reperfusion ('hot shot') prevents myocardial substrate derangement in patients undergoing coronary artery bypass surgery. Eur J Cardiothorac Surg 1998;13:559–64. [DOI] [PubMed] [Google Scholar]
- 291. Filsoufi F, Rahmanian PB, Castillo JG, Chikwe J, Adams DH. Predictors and early and late outcomes of respiratory failure in contemporary cardiac surgery. Chest 2008;133:713–21. [DOI] [PubMed] [Google Scholar]
- 292. Sohn N, Marcoux J, Mycyk T, Krahn J, Meng Q. The impact of different biocompatible coated cardiopulmonary bypass circuits on inflammatory response and oxidative stress. Perfusion 2009;24:231–7. [DOI] [PubMed] [Google Scholar]
- 293. Warren OJ, Tunnicliffe CR, Massey RM, Wallace S, Smith AJ, Alcock EM et al. Systemic leukofiltration does not attenuate pulmonary injury after cardiopulmonary bypass. Asaio J 2008;54:78–88. [DOI] [PubMed] [Google Scholar]
- 294. Issitt R, Ball J, Bilkhoo I, Mani A, Walsh B, Voegeli D. Leukocyte filtration of the cardiotomy suction. Does it affect systemic leukocyte activation or pulmonary function? Perfusion 2017;32:574–82. [DOI] [PubMed] [Google Scholar]
- 295. Onorati F, Santini F, Mariscalco G, Bertolini P, Sala A, Faggian G et al. Leukocyte filtration ameliorates the inflammatory response in patients with mild to moderate lung dysfunction. Ann Thorac Surg 2011;92:111–21. [DOI] [PubMed] [Google Scholar]
- 296. Mair P, Hoermann C, Mair J, Margreiter J, Puschendorf B, Balogh D. Effects of a leucocyte depleting arterial line filter on perioperative proteolytic enzyme and oxygen free radical release in patients undergoing aortocoronary bypass surgery. Acta Anaesthesiol Scand 1999;43:452–7. [DOI] [PubMed] [Google Scholar]
- 297. Luciani GB, Menon T, Vecchi B, Auriemma S, Mazzucco A. Modified ultrafiltration reduces morbidity after adult cardiac operations: a prospective, randomized clinical trial. Circulation 2001;104:I253–9. [DOI] [PubMed] [Google Scholar]
- 298. Torina AG, Petrucci O, Oliveira PP, Severino ES, Vilarinho KA, Lavagnoli CF et al. The effects of modified ultrafiltration on pulmonary function and transfusion requirements in patients underwent coronary artery bypass graft surgery. Rev Bras Cir Cardiovasc 2010;25:59–65. [DOI] [PubMed] [Google Scholar]
- 299. Santini F, Onorati F, Telesca M, Menon T, Mazzi P, Berton G et al. Selective pulmonary pulsatile perfusion with oxygenated blood during cardiopulmonary bypass attenuates lung tissue inflammation but does not affect circulating cytokine levels. Eur J Cardiothorac Surg 2012;42:942–50. [DOI] [PubMed] [Google Scholar]
- 300. Santini F, Onorati F, Telesca M, Patelli F, Berton G, Franchi G et al. Pulsatile pulmonary perfusion with oxygenated blood ameliorates pulmonary hemodynamic and respiratory indices in low-risk coronary artery bypass patients. Eur J Cardiothorac Surg 2011;40:794–803. [DOI] [PubMed] [Google Scholar]
- 301. Kiessling AH, Guo FW, Gokdemir Y, Thudt M, Reyher C, Scherer M et al. The influence of selective pulmonary perfusion on the inflammatory response and clinical outcome of patients with chronic obstructive pulmonary disease undergoing cardiopulmonary bypass. Interact CardioVasc Thorac Surg 2014;18:732–9. [DOI] [PubMed] [Google Scholar]
- 302. Schreiber JU, Lance MD, de Korte M, Artmann T, Aleksic I, Kranke P. The effect of different lung-protective strategies in patients during cardiopulmonary bypass: a meta-analysis and semiquantitative review of randomized trials. J Cardiothorac Vasc Anesth 2012;26:448–54. [DOI] [PubMed] [Google Scholar]
- 303. Bignami E, Guarnieri M, Saglietti F, Maglioni EM, Scolletta S, Romagnoli S et al. Different strategies for mechanical VENTilation during CardioPulmonary Bypass (CPBVENT 2014): study protocol for a randomized controlled trial. Trials 2017;18:264.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304. Heinrichs J, Lodewyks C, Neilson C, Abou-Setta A, Grocott HP. The impact of hyperoxia on outcomes after cardiac surgery: a systematic review and narrative synthesis. Can J Anaesth 2018;65:923–35. [DOI] [PubMed] [Google Scholar]
- 305. Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM 3rd et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg 2009;87:36–44. [DOI] [PubMed] [Google Scholar]
- 306. Colak Z, Borojevic M, Bogovic A, Ivancan V, Biocina B, Majeric-Kogler V. Majeric-Kogler V. Influence of intraoperative cerebral oximetry monitoring on neurocognitive function after coronary artery bypass surgery: a randomized, prospective study. Eur J Cardiothorac Surg 2015;47:447–54. [DOI] [PubMed] [Google Scholar]
- 307. Kara I, Erkin A, Saclı H, Demirtas M, Percin B, Diler MS et al. The effects of near-infrared spectroscopy on the neurocognitive functions in the patients undergoing coronary artery bypass grafting with asymptomatic carotid artery disease: a randomized prospective study. Ann Thorac Cardiovasc Surg 2015;21:544–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308. Rogers CA, Stoica S, Ellis L, Stokes EA, Wordsworth S, Dabner L et al. Randomized trial of near-infrared spectroscopy for personalized optimization of cerebral tissue oxygenation during cardiac surgery. Br J Anaesth 2017;119:384–93. [DOI] [PubMed] [Google Scholar]
- 309. Lei L, Katznelson R, Fedorko L, Carroll J, Poonawala H, Machina M et al. Cerebral oximetry and postoperative delirium after cardiac surgery: a randomised, controlled trial. Anaesthesia 2017;72:1456–66. [DOI] [PubMed] [Google Scholar]
- 310. Serraino GF, Murphy GJ. Effects of cerebral near-infrared spectroscopy on the outcome of patients undergoing cardiac surgery: a systematic review of randomised trials. BMJ Open 2017;7:e016613.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311. Avidan MS, Zhang L, Burnside BA, Finkel KJ, Searleman AC, Selvidge JA et al. Anesthesia awareness and the bispectral index. N Engl J Med 2008;358:1097–108. [DOI] [PubMed] [Google Scholar]
- 312. Avidan MS, Jacobsohn E, Glick D, Burnside BA, Zhang L, Villafranca A et al. Prevention of intraoperative awareness in a high-risk surgical population. N Engl J Med 2011;365:591–600. [DOI] [PubMed] [Google Scholar]
- 313. Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev 2014:CD003843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314. Shann KG, Likosky DS, Murkin JM, Baker RA, Baribeau YR, DeFoe GR et al. An evidence-based review of the practice of cardiopulmonary bypass in adults: a focus on neurologic injury, glycemic control, hemodilution, and the inflammatory response. J Thorac Cardiovasc Surg 2006;132:283–90. [DOI] [PubMed] [Google Scholar]
- 315. Apostolakis EE, Koletsis EN, Baikoussis NG, Siminelakis SN, Papadopoulos GS. Strategies to prevent intraoperative lung injury during cardiopulmonary bypass. J Cardiothorac Surg 2010;5:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316. Djaiani G, Fedorko L, Borger MA, Green R, Carroll J, Marcon M et al. Continuous-flow cell saver reduces cognitive decline in elderly patients after coronary bypass surgery. Circulation 2007;116:1888–95. [DOI] [PubMed] [Google Scholar]
- 317. De Somer F, Van Belleghem Y, Caes F, Francois K, Van Overbeke H, Arnout J et al. Tissue factor as the main activator of the coagulation system during cardiopulmonary bypass. J Thorac Cardiovasc Surg 2002;123:951–8. [DOI] [PubMed] [Google Scholar]
- 318. Aldea GS, Soltow LO, Chandler WL, Triggs CM, Vocelka CR, Crockett GI et al. Limitation of thrombin generation, platelet activation, and inflammation by elimination of cardiotomy suction in patients undergoing coronary artery bypass grafting treated with heparin-bonded circuits. J Thorac Cardiovasc Surg 2002;123:742–55. [DOI] [PubMed] [Google Scholar]
- 319. Albes JM, Stohr IM, Kaluza M, Siegemund A, Schmidt D, Vollandt R et al. Physiological coagulation can be maintained in extracorporeal circulation by means of shed blood separation and coating. J Thorac Cardiovasc Surg 2003;126:1504–12. [DOI] [PubMed] [Google Scholar]
- 320. Rubens FD, Boodhwani M, Mesana T, Wozny D, Wells G, Nathan HJ et al. The cardiotomy trial: a randomized, double-blind study to assess the effect of processing of shed blood during cardiopulmonary bypass on transfusion and neurocognitive function. Circulation 2007;116:I-89–97. [DOI] [PubMed] [Google Scholar]
- 321. Wang G, Bainbridge D, Martin J, Cheng D. The efficacy of an intraoperative cell saver during cardiac surgery: a meta-analysis of randomized trials. Anesth Analg 2009;109:320–30. [DOI] [PubMed] [Google Scholar]
- 322. Attaran S, McIlroy D, Fabri BM, Pullan MD. The use of cell salvage in routine cardiac surgery is ineffective and not cost-effective and should be reserved for selected cases. Interact CardioVasc Thorac Surg 2011;12:824–6. [DOI] [PubMed] [Google Scholar]
- 323. Cheng DC, Martin J, Lal A, Diegeler A, Folliguet TA, Nifong LW et al. Minimally invasive versus conventional open mitral valve surgery: a meta-analysis and systematic review. Innovations 2011;6:84–103. [DOI] [PubMed] [Google Scholar]
- 324. Phan K, Xie A, Tsai YC, Black D, Di Eusanio M, Yan TD. Ministernotomy or minithoracotomy for minimally invasive aortic valve replacement: a Bayesian network meta-analysis. Ann Cardiothorac Surg 2015;4:3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325. Krapf C, Wohlrab P, Häußinger S, Schachner T, Hangler H, Grimm M et al. Remote access perfusion for minimally invasive cardiac surgery: to clamp or to inflate? Eur J Cardiothorac Surg 2013;44:898–904. [DOI] [PubMed] [Google Scholar]
- 326. Licker M, Diaper J, Cartier V, Ellenberger C, Cikirikcioglu M, Kalangos A et al. Clinical review: management of weaning from cardiopulmonary bypass after cardiac surgery. Ann Card Anaesth 2012;15:206–23. [DOI] [PubMed] [Google Scholar]
- 327. Vakamudi M. Weaning from cardiopulmonary bypass: problems and remedies. Ann Card Anaesth 2004;7:178–85. [PubMed] [Google Scholar]
- 328. Cui WW, Ramsay JG. Pharmacologic approaches to weaning from cardiopulmonary bypass and extracorporeal membrane oxygenation. Best Pract Res Clin Anaesthesiol 2015;29:257–70. [DOI] [PubMed] [Google Scholar]
- 329. Ogden SR, Culp WC Jr, Villamaria FJ, Ball TR. Developing a checklist: consensus via a modified delphi technique. J Cardiothorac Vasc Anesth 2016;30:855–8. [DOI] [PubMed] [Google Scholar]
- 330. Bruppacher HR, Alam SK, LeBlanc VR, Latter D, Naik VN, Savoldelli GL et al. Simulation-based training improves physicians' performance in patient care in high-stakes clinical setting of cardiac surgery. Anesthesiology 2010;112:985–92. [DOI] [PubMed] [Google Scholar]
- 331. Brovman EY, Gabriel RA, Dutton RP, Urman RD. Pulmonary artery catheter use during cardiac surgery in the United States, 2010 to 2014. J Cardiothorac Vasc Anesth 2016;30:579–84. [DOI] [PubMed] [Google Scholar]
- 332. Chiang Y, Hosseinian L, Rhee A, Itagaki S, Cavallaro P, Chikwe J. Questionable benefit of the pulmonary artery catheter after cardiac surgery in high-risk patients. J Cardiothorac Vasc Anesth 2015;29:76–81. [DOI] [PubMed] [Google Scholar]
- 333. Resano FG, Kapetanakis EI, Hill PC, Haile E, Corso PJ. Clinical outcomes of low-risk patients undergoing beating-heart surgery with or without pulmonary artery catheterization. J Cardiothorac Vasc Anesth 2006;20:300–6. [DOI] [PubMed] [Google Scholar]
- 334. Peyton PJ, Chong SW. Minimally invasive measurement of cardiac output during surgery and critical care: a meta-analysis of accuracy and precision. Anesthesiology 2010;113:1220–35. [DOI] [PubMed] [Google Scholar]
- 335. Schloglhofer T, Gilly H, Schima H. Semi-invasive measurement of cardiac output based on pulse contour: a review and analysis. Can J Anaesth 2014;61:452–79. [DOI] [PubMed] [Google Scholar]
- 336. Eltzschig HK, Rosenberger P, Loffler M, Fox JA, Aranki SF, Shernan SK. Impact of intraoperative transesophageal echocardiography on surgical decisions in 12, 566 patients undergoing cardiac surgery. Ann Thorac Surg 2008;85:845–52. [DOI] [PubMed] [Google Scholar]
- 337. Ionescu AA, West RR, Proudman C, Butchart EG, Fraser AG. Prospective study of routine perioperative transesophageal echocardiography for elective valve replacement: clinical impact and cost-saving implications. J Am Soc Echocardiogr 2001;14:659–67. [DOI] [PubMed] [Google Scholar]
- 338. Fanshawe M, Ellis C, Habib S, Konstadt SN, Reich DL. A retrospective analysis of the costs and benefits related to alterations in cardiac surgery from routine intraoperative transesophageal echocardiography. Anesth Analg 2002;95:824–7. [DOI] [PubMed] [Google Scholar]
- 339. Ramalingam G, Choi SW, Agarwal S, Kunst G, Gill R, Fletcher SN et al. Complications related to peri-operative transoesophageal echocardiography—a one-year prospective national audit by the Association of Cardiothoracic Anaesthesia and Critical Care. Anaesthesia 2019; doi:10.1111/anae.14734. [DOI] [PubMed] [Google Scholar]
- 340. Hahn RT, Abraham T, Adams MS, Bruce CJ, Glas KE, Lang RM et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesth Analg 2014;118:21–68. [DOI] [PubMed] [Google Scholar]
- 341.American Society of Anesthesiologists and Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Practice guidelines for perioperative transesophageal echocardiography. An updated report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Anesthesiology 2010;112:1084–96. [DOI] [PubMed] [Google Scholar]
- 342. Yamada T, Takeda J, Katori N, Tsuzaki K, Ochiai R. Hemodynamic effects of milrinone during weaning from cardiopulmonary bypass: comparison of patients with a low and high prebypass cardiac index. J Cardiothorac Vasc Anesth 2000;14:367–73. [DOI] [PubMed] [Google Scholar]
- 343. Lewis KP, Appadurai IR, Pierce ET, Halpern EF, Bode RH Jr. Prophylactic amrinone for weaning from cardiopulmonary bypass. Anaesthesia 2000;55:627–33. [DOI] [PubMed] [Google Scholar]
- 344. Kikura M, Sato S. The efficacy of preemptive Milrinone or Amrinone therapy in patients undergoing coronary artery bypass grafting. Anesth Analg 2002;94:22–30. [DOI] [PubMed] [Google Scholar]
- 345. Oztekin I, Yazici S, Oztekin DS, Goksel O, Issever H, Canik S. Effects of low-dose milrinone on weaning from cardiopulmonary bypass and after in patients with mitral stenosis and pulmonary hypertension. Yakugaku Zasshi 2007;127:375–83. [DOI] [PubMed] [Google Scholar]
- 346. Belletti A, Castro ML, Silvetti S, Greco T, Biondi-Zoccai G, Pasin L et al. The Effect of inotropes and vasopressors on mortality: a meta-analysis of randomized clinical trials. Br J Anaesth 2015;115:656–75. [DOI] [PubMed] [Google Scholar]
- 347. Mehta RH, Leimberger JD, van Diepen S, Meza J, Wang A, Jankowich R et al. Levosimendan in patients with left ventricular dysfunction undergoing cardiac surgery. N Engl J Med 2017;376:2032–42. [DOI] [PubMed] [Google Scholar]
- 348. Cholley B, Caruba T, Grosjean S, Amour J, Ouattara A, Villacorta J et al. Effect of levosimendan on low cardiac output syndrome in patients with low ejection fraction undergoing coronary artery bypass grafting with cardiopulmonary bypass: the LICORN randomized clinical trial. JAMA 2017;318:548–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349. Landoni G, Lomivorotov VV, Alvaro G, Lobreglio R, Pisano A, Guarracino F et al. Levosimendan for hemodynamic support after cardiac surgery. N Engl J Med 2017;376:2021–31. [DOI] [PubMed] [Google Scholar]
- 350. Chen QH, Zheng RQ, Lin H, Shao J, Yu JQ, Wang HL. Effect of levosimendan on prognosis in adult patients undergoing cardiac surgery: a meta-analysis of randomized controlled trials. Crit Care 2017;21:253.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351. Olsson A, Alfredsson J, Ramstrom S, Svedjeholm R, Kenny D, Hakansson E et al. Better platelet function, less fibrinolysis and less hemolysis in re-transfused residual pump blood with the Ringer's chase technique—a randomized pilot study. Perfusion 2018;33:185–93. [DOI] [PubMed] [Google Scholar]
- 352. Eichert I, Isgro F, Kiessling AH, Saggau W. Cell saver, ultrafiltration and direct transfusion: comparative study of three blood processing techniques. Thorac Cardiovasc Surg 2001;49:149–52. [DOI] [PubMed] [Google Scholar]
- 353. Vonk AB, Muntajit W, Bhagirath P, van Barneveld LJ, Romijn JW, de Vroege R et al. Residual blood processing by centrifugation, cell salvage or ultrafiltration in cardiac surgery: effects on clinical hemostatic and ex vivo rheological parameters. Blood Coagul Fibrinolysis 2012;23:622–8. [DOI] [PubMed] [Google Scholar]
- 354. Daane CR, Golab HD, Meeder JH, Wijers MJ, Bogers AJ. Processing and transfusion of residual cardiopulmonary bypass volume: effects on haemostasis, complement activation, postoperative blood loss and transfusion volume. Perfusion 2003;18:115–21. [DOI] [PubMed] [Google Scholar]
- 355. Campbell J, Holland C, Richens D, Skinner H. Impact of cell salvage during cardiac surgery on the thrombelastomeric coagulation profile: a pilot study. Perfusion 2012;27:221–4. [DOI] [PubMed] [Google Scholar]
- 356. Scrascia G, Rotunno C, Nanna D, Rociola R, Guida P, Rubino G et al. Pump blood processing, salvage and re-transfusion improves hemoglobin levels after coronary artery bypass grafting, but affects coagulative and fibrinolytic systems. Perfusion 2012;27:270–7. [DOI] [PubMed] [Google Scholar]
- 357. Whitlock R, Mathew J, Eikelboom J, Al-Saleh AM, Yuan F, Teoh K. Processed residual pump blood in cardiac surgery: the processed residual blood in cardiac surgery trial. Transfusion 2013;53:1487–92. [DOI] [PubMed] [Google Scholar]
- 358. Torina AG, Silveira-Filho LM, Vilarinho KA, Eghtesady P, Oliveira PP, Sposito AC et al. Use of modified ultrafiltration in adults undergoing coronary artery bypass grafting is associated with inflammatory modulation and less postoperative blood loss: a randomized and controlled study. J Thorac Cardiovasc Surg 2012;144:663–70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


