Abstract
Nontraumatic exertional syncope can be an ominous event reflecting profound arterial hypotension, cerebral hypoperfusion, and transient loss-of consciousness that occurs most commonly in patients with underlying cardiovascular disease. In contradistinction, transient loss-of-consciousness in “healthy adults” is typically vasovagal syncope related to exaggerated orthostatic cardiovascular responses attributed to a hyper-reactive autonomic nervous system. In the present report, a 34 yo male presents to the hospital emergency department (ED) for a sudden loss of consciousness and fall ultimately related to cardiac syncope ascribed to chronic recreational marijuana use complicated by coronary vasospasm.
Keywords: Syncope, Marijuana, Vasoconstriction, Vasospasm
Introduction
Syncope in erect individuals after exhaustive exercise of short duration is commonly reported and sometimes related to persistent post-exercise peripheral arterial vasodilation with impaired venous return [1]. Other reported events are attributed to excessive vagal response leading to a post-exertional sinus pause with ventricular asystole [2]. Marijuana users have increased risk of cardiac dysrhythmia associated with tachycardia, bradycardia, chest pain, and/or unexplained syncope [3]. In one example, a 40 yo was hospitalized for syncope related to loss of sinoatrial activity with ventricular asystole after strenuous exercise, which was heralded by several post-exertion, near syncope events during a 6 month period of marijuana use. In contradistinction, the present case describes syncope in the context of chronic marijuana use due to chronic coronary constriction and vasospasm.
Case Report
History of presentation: The patient is a 34-year-old male with no significant medical history who presents to the hospital for a syncopal event. The patient was intimate with his wife in the shower, “felt hot”, and stepped into the bedroom. He lost consciousness and fell to the floor where his spouse found him, wet from the shower and “shaking”, possibly shivering. Consciousness returned in a few minutes without confusion. The event was not associated with tongue biting, tonic-clonic movements of extremities, or bowel/bladder incontinence. He was brought to the ED by his wife for further evaluation. When interviewed, the patient denied current chest pain/pressure, chest tightness, palpitations, shortness of breath, nausea, vomiting, or fevers at the time or prior to the event. He endorsed recent loose stools following initiation of daily prune juice for constipation a few days earlier. Patient notes frequent upper respiratory congestion relieved by expectoration of mucous. No recent changes of diet or medications were expressed.
Past Medical History:
Gunshot wound in back without complications or surgery (2019). No use of tobacco products. Daily recreational use of marijuana since age 19. Recreational alcohol use with the last drink a few days prior to admission. He is married with one child.
Differential diagnosis:
Vasovagal, orthostatic, cardiogenic (arrhythmia, ischemia) syncope.
Investigations:
The patient was managed under informed obtained upon hospital admission and for the specific procedures described. In the Emergency Department, the presentation ECG revealed modest inferior lead ischemic changes (Figure 1) associated with mildly increased serial high sensitivity troponin levels (hs-TnI, ng/L): 69, 139, 114, 111.
Figure 1:

Presentation ECG in 34 yo male following syncope and associated with increased hs-TnI. Convex ST segments with T-wave inversions are appreciated in the inferior leads (III, AVF) consistent with ischemia (arrows).
The patient was heparinized. Telemetry recorded no ectopy over the hospitalization. Stress echocardiography revealed normal cardiac structure and function at rest. He exercised to 12 Mets using a modified Bruce protocol without symptoms or significant ECG changes. Peak stress images revealed a new transient inferior basal aneurysm resolved with rest (Figure 2).
Figure 2:
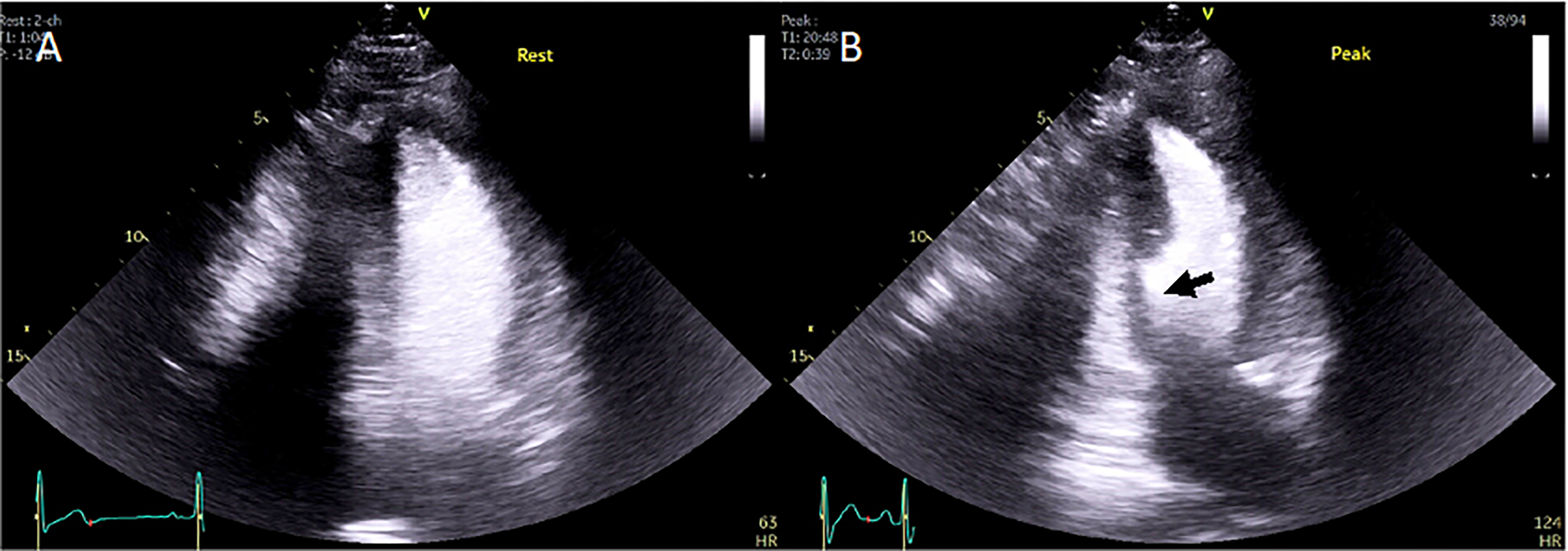
Rest and peak microbubble contrast enhanced images from exercise stress echocardiographic study showing a transient inferior basal aneurysm appreciated at peak exercise (12 Mets). Arrow points to inferior basal aneurysm seen in the 2-chamber view at peak stress. Inferior segment hypokinesis was noted in the short axis view (not shown).
Cardiac catheterization was performed. Both the right and left coronary vessels appeared small with slow contrast flow but without thrombotic obstruction. Intracoronary infusion of nicardipine was administered and promptly “plumped” the vascular bed, increased contrast flow rate and revealed arterial branches unappreciated at baseline (Figure 3) consistent with a diagnosis of chronic vasoconstriction with vasospasm.
Figure 3:

Cardiac angiograms of the left coronary circulation obtained at baseline (A) and following intracoronary infusion of nicardipine (B). Coronary vessels with slow flow were “plumped” with the calcium channel blocker associated with increased, rapid contrast perfusion and visualization of coronary branches unseen initially due to vasoconstriction (see arrows). Analogous findings were reported in the right coronary circulation.
Management (medical/interventions):
The patient was revealed to have chronic baseline vasoconstriction with susceptibility to vasospasm with exertion, and was prescribed amlodipine 5mg, which was well tolerated, along with recommendations to curtail or discontinue marijuana use, in accordance with AHA/ACC guidelines for the “Management of Patients With Unstable Angina and Non–ST-Segment Elevation Myocardial Infarction” and management of coronary vasospasm, e.g. Prinzmetal angina. He was referred for cardiology follow-up.
Follow-up:
Telephone follow-up revealed reduced use of marijuana but discontinuance of amlodipine due to cost. The patient failed to follow-up in clinic, but was urged to do so and continue use of daily medicine, which could be acquired through the Medicine clinic, if cost was a factor.
Discussion
Medical marijuana is increasingly used in the context of cancer, multiple sclerosis, epilepsy, Parkinson’s, and other neurodegenerative diseases mostly with non-life threatening off-target effects [4]. However, recreational cannabis was anecdotally associated with adverse cardiovascular (CV) effects since 1972 [5–8]and has been the subject of clinical studies [9,10] and reviews [11] that corroborate CV risks as published in 2016 by the WHO, “The Health and Social Effects of Nonmedical Cannabis Use report”. Even secondary marijuana smoke exposure can have negative cardiovascular impact [12]. A preponderance of scientific evidence has identified THC binding to the cannabinoid receptor 1 (CB1R) as a cause for endothelial dysfunction [13]. The receptor is abundantly expressed in the brain and in the heart on cardiomyocytes, smooth muscle cells, and vascular endothelial cells. Over the last 10 years, increased marijuana availability and demand have paralleled selective genetic breeding of cannabis with THC content increasing from 2–3% up to 18–20% currently [11]. “Designer drugs”, which are psychoactive synthetic cannabinoids with potencies 10 times to 200 times greater than THC, are increasingly available for recreational use [11]. This “healthy” patient had underlying chronic vasoconstriction in the heart associated with slow blood flow perfusion with susceptibility to vasospasm. These effects are likely systemic for him, and maybe shared to varying degrees by millions of individuals in the US. Given the increasing prevalence of recreational marijuana use, the concept of “cannabis-use-disorder” or CUD has emerged to categorize compelled personal use of marijuana [14,15]. As of 2023, availability of cannabis has increased rapidly: 18 states have legalized marijuana for medical and recreational use, 17 more allow medical use, and 9 more have approved CBD/low Δ9 tetrahydrocannabinol (THC) use.
Conclusion
While many harken back to the low potency marijuana from the 60’s and 70’s when considering legalization, the medical community must recognize that the increased availability of high potency cannabis may have epidemic level impact with various multi-organ presentations including motor vehicle trauma [14]. The cardiovascular spectrum of disease can occur at any age from direct or indirect exposure to cannabis and present as endothelial dysfunction inducing vasoconstriction, vasospasm, or myocardial infarction.
Learning Objectives
Case: A 34 yo male presents to the hospital emergency department (ED) for a sudden loss of consciousness and fall related to coronary vasospasm associated with marijuana use.
Appreciate the change that a 10 fold increase in commercially available marijuana potency and its enhanced potential cardiovascular impact.
Appreciate that specific THC receptors have been identified, particularly CB1R in the brain and heart vascular endothelium and smooth muscle cells.
Appreciate that patients of any age can present with atypical symptoms of vascular dysfunction including vasospasm, arrhythmia, and ischemia.
Funding:
Dr. Lanza’s salary was supported by NIH R01s: CA216840 and CA260855.
Abbreviations:
- CBD
Cannabidiol
- CB1R
Cannabinoid Receptor 1
- ECG
Electrocardiogram
- ED
Emergency Department
- Hs-Tni
High Sensitivity Troponin I
- Met
Metabolic Equivalent For Task
- THC
Δ9 Tetrahydrocannabinol
- WHO
World Health Organization
- Yo
Year Old
Footnotes
Disclosures: “The authors have nothing to disclose”.
Ethics and institutional review: This case report is submitted after careful review by the Washington University Human Research Protection Office.
References
- 1.Halliwill JR, Buck TM, Lacewell AN, Romero SA (2013) Postexercise hypotension and sustained postexercise vasodilatation: what happens after we exercise? Exp Physiol. 98:7–18. [DOI] [PubMed] [Google Scholar]
- 2.Huycke EC, Card HG, Sobol SM, Nguyen NX, Sung RJ (1987) Postexertional cardiac asystole in a young man without organic heart disease. Ann Intern Med. 106:844–5. [DOI] [PubMed] [Google Scholar]
- 3.Richards JR, Blohm E, Toles KA, Jarman AF, Ely DF, Elder JW (2020) The association of cannabis use and cardiac dysrhythmias: a systematic review. Clin Toxicol (Phila). 58:861–9. [DOI] [PubMed] [Google Scholar]
- 4.Zeine RR, Teasdale BW, eds (2023) Medical Cannabis and the Effects of Cannabinoids on Fighting Cancer, Multiple Sclerosis, Epilepsy, Parkinson’s, and Other Neurodegenerative Diseases. Hershey, PA, USA: IGI Global. [Google Scholar]
- 5.Basnet S, Mander G, Nicolas R (2009) Coronary vasospasm in an adolescent resulting from marijuana use. Pediatr Cardiol. 30:543–5. [DOI] [PubMed] [Google Scholar]
- 6.Bailly C, Merceron O, Hammoudi N, Dorent R, Michel PL (2010) Cannabis induced acute coronary syndrome in a young female. Int J Cardiol. 143:e4–6. [DOI] [PubMed] [Google Scholar]
- 7.Safaa AM, Markham R, Jayasinghe R (2012) Marijuana-induced recurrent acute coronary syndrome with normal coronary angiograms. Drug Alcohol Rev. 31:91–4. [DOI] [PubMed] [Google Scholar]
- 8.Gunawardena MD, Rajapakse S, Herath J, Amarasena N. (2014) Myocardial infarction following cannabis induced coronary vasospasm. BMJ Case Rep. 2014:bcr2014207020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE (2001) Triggering myocardial infarction by marijuana. Circulation. 103:2805–9. [DOI] [PubMed] [Google Scholar]
- 10.Cheung CP, Coates AM, Millar PJ, Burr JF (2021) Habitual cannabis use is associated with altered cardiac mechanics and arterial stiffness, but not endothelial function in young healthy smokers. J Appl Physiol (1985). 130:660–70. [DOI] [PubMed] [Google Scholar]
- 11.Piano MR (2017) Cannabis smoking and cardiovascular health: It’s complicated. Clin Pharmacol Ther. 102:191–3. [DOI] [PubMed] [Google Scholar]
- 12.Wang X, Derakhshandeh R, Liu J, Narayan S, Nabavizadeh P, Le S, Danforth OM, Pinnamaneni K, Rodriguez HJ, Luu E, Sievers RE, Schick SF, Glantz SA, Springer ML. (2016) One minute of marijuana secondhand smoke exposure substantially impairs vascular endothelial function. J Am Heart Assoc. 5:e003858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feng X, Xu S, Weng J (2022) Marijuana and endothelial dysfunction: new mechanism and therapy. Trends Mol Med. 28:613–5. [DOI] [PubMed] [Google Scholar]
- 14.Hasin DS (2018) US Epidemiology of cannabis use and associated problems. Neuropsychopharmacology. 43:195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weresa J, Pędzińska-Betiuk A, Mińczuk K, Malinowska B, Schlicker E. (2022) Why do marijuana and synthetic cannabimimetics induce acute myocardial infarction in healthy young people? Cells. 1:1142. [DOI] [PMC free article] [PubMed] [Google Scholar]


