Abstract
Oncostatin M (OSM) is a member of the interleukin-6 (IL-6) family of cytokines and has been found to have distinct anti-inflammatory and pro-inflammatory properties in various cellular and disease contexts. OSM signals through two receptor complexes, one of which includes OSMRβ. To investigate OSM-OSMRβ signaling in adult hematopoiesis, we utilized the readily available conditional Osmrfl/fl mouse model B6;129-Osmrtm1.1Nat/J, which is poorly characterized in the literature. This model contains loxP sites flanking exon 2 of the Osmr gene. We crossed Osmrfl/fl mice to interferon-inducible Mx1-Cre, which is robustly induced in adult hematopoietic cells. We observed complete recombination of the Osmrfl allele and loss of exon 2 in hematopoietic (bone marrow) as well as non-hematopoietic (liver, lung, kidney) tissues. Using a TaqMan assay with probes downstream of exon 2, Osmr transcript was lower in the kidney but equivalent in bone marrow, lung, and liver from Osmrfl/fl Mx1-Cre versus Mx1-Cre control mice, suggesting that transcript is being produced despite loss of this exon. Western blots show that liver cells from Osmrfl/fl Mx1-Cre mice had complete loss of OSMR protein, while bone marrow, kidney, and lung cells had reduced OSMR protein at varying levels. RNA-seq analysis of a subpopulation of bone marrow cells (hematopoietic stem cells) finds that some OSM-stimulated genes, but not all, are suppressed in Osmrfl/fl Mx1-Cre cells. Together, our data suggest that the B6;129-Osmrtm1.1Nat/J model should be utilized with caution as loss of Osmr exon 2 has variable and tissue-dependent impact on mRNA and protein expression.
INTRODUCTION
OSM, belonging to the IL-6 family, plays an important role in development, malignancy, and homeostasis of various tissue types1–5. OSM is primarily produced by mature activated hematopoietic cells such as monocytes, T lymphocytes, neutrophils, macrophages, and dendritic cells4,6,7. OSM was first isolated based on its ability to inhibit the proliferation of melanoma tumor cells, while having no significant effect on normal human fibroblasts6. Due to this unique characteristic, it was given the name oncostatin M, where “onco” referred to cancer, “statin” to its ability to inhibit cell proliferation, and “M” to melanoma. Despite the initial identification of OSM as a tumor suppressor, a pro-inflammatory role of OSM has been reported in colon cancer, breast cancer, pancreatic cancer, myeloma, brain tumors, chronic lymphocytic leukemia, hepatoblastoma and COVID-191,3,8. OSM, like IL-6, has been linked to tumor growth and is often found in high concentrations in the serum and tumor sites of patients and animal models of cancer1,3,8. Significantly increased Osm transcript production has also been associated with aging in both the human thymus and mouse hematopoietic stem cells (HSCs) compared to young tissues9,10. Human OSM interacts with two distinct receptor complexes termed type I and type II. The type I receptor complex contains leukemia inhibitory factor receptor alpha (LIFR) and interleukin 6 signal transducer (IL6ST; GP130), while the type II receptor complex contains oncostatin M receptor (OSMRβ) and IL6ST4,11–13. While recent studies have shown that OSM has a lower affinity for the type I receptor complex than the type II receptor complex14,15, much remains unknown about how OSM interacts with these complexes in different contexts. An additional complexity in studying OSM signaling is that while human OSM is known to signal through both the type I and type II receptor complexes, mouse OSM is reported to signal only through the type II receptor complex16–18.
To understand the role of OSM signaling in aging and disease in a physiologically relevant in vivo setting, mouse knockout models are essential. Two existing mouse models are commonly used to investigate loss of receptor complex II signaling through knockout of Osmr. The first, Osmrtm1Mtan, was reported by Tanaka et al. in 200319. This model disrupts the first coding exon of Osmr by knock-in of a lacZ and neomycin expression cassette into the proximal region and is non-conditional in nature19. These Osmr−/− mice were viable and fertile, born at expected Mendelian ratios, and had normal adult body weights19. Knockout of Osmr was confirmed by loss of mRNA in lung tissue19. This model exhibited hematopoiesis phenotypes showing reduced numbers of erythroid and megakaryocytic progenitors and their mature counterparts19. However, these were attributed to both cell-autonomous and cell non-autonomous effects of Osmr−/− on hematopoietic progenitor cells and non-hematopoietic cells in the bone marrow microenvironment19, which are best resolved by the use of a conditional knockout model. The second existing model, B6;129-Osmrtm1.1Nat/J, is a conditional knockout model in which loxP sites flank the first coding exon of the Osmr gene. Additionally, adjacent to the second loxP site is an Frt site remaining after excision of a PGK-neomycin selectable marker. This model was originally designed to study Osmr in the retina and is available in The Jackson Laboratory’s mouse repository; however, characterization of the model has not been published by the donating investigators. To investigate cell-autonomous effects of Osmr conditional knockout on hematopoiesis, we obtained the B6;129-Osmrtm1.1Nat/J (referred to as Osmrfl/fl) model and crossed these mice to an interferon-inducible Mx1-Cre allele20, which is commonly used in the study of adult hematopoiesis. We characterized Osmrfl/fl Mx1-Cre mice using classical methods such as the development of a PCR reaction to evaluate recombination of the Osmrfl allele, real-time PCR and RNA sequencing for Osmr mRNA transcript, and Western blotting to evaluate OSMRβ at the protein level. We investigated both hematopoietic tissue (bone marrow) as well as non-hematopoietic tissues (liver, lung, kidney) in which OSMRβ is also expressed. Our results demonstrate variable alterations in mRNA and protein expression in various tissues isolated from Osmrfl/fl Mx1-Cre compared to control Mx1-Cre mice.
RESULTS
DNA Recombination in Bone Marrow Cells, Lung, Liver, and Kidney Cells of Osmrfl/fl Mx1-Cre Mice
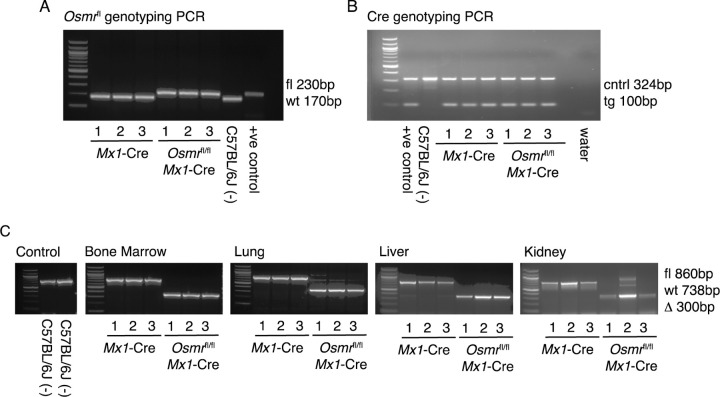
To generate an inducible Osmr knockout model, the B6;129-Osmrtm1.1Nat/J strain was crossed to Mx1-Cre20. Mx1-Cre is an interferon-inducible cre recombinase that is highly efficient in expression in progenitor and mature cells of the adult hematopoietic lineages. Thus, in the Osmrfl/fl Mx1-Cre model, the Osmrfl allele should remain unrecombined with wild-type expression at the transcript and protein levels prior to administration of the double-stranded RNA poly(I:C), which then induces an interferon response and expression of cre recombinase. After crossing B6;129-Osmrtm1.1Nat/J to Mx1-Cre to generate Osmrfl/fl Mx1-Cre and control Mx1-Cre animals, we genotyped three control and three experimental animals alongside positive (parental Osmrfl/fl and Mx1-Cre mice) and negative (wild-type C57BL/6J) controls. At the Osmr locus, genomic DNA from Osmrfl/fl Mx1-Cre mice contained a loxP site (230bp) and genomic DNA from control Mx1-Cre mice did not contain a loxP site (170bp), recognized by primers flanking exon 2 (Figure 1A). Genomic DNA from all Osmrfl/fl Mx1-Cre and control Mx1-Cre mice were also positive for the transgenic cre allele (100bp) (Figure 1B).
Figure 1. Recombination of the Osmrfl Locus in Tissues from Osmrfl/fl Mx1-Cre Mice.
Agarose gel electrophoresis (2% agarose) of PCR-amplified products. In all gels a 100bp ladder was used for size estimation located in lane 0. (A) Genotyping PCR for Osmr<tm1.1Nat>. Lanes 1–3 use genomic DNA samples from Mx1-Cre control mice, lanes 4–6 use genomic DNA samples from Osmrfl/fl Mx1-Cre mice, lane 7 uses genomic DNA from a wild-type C57BL/6J mouse and lane 8 uses a positive control Osmrfl/fl from a mouse confirmed by The Jackson Laboratory’s in-house genotyping service. (B) Genotyping PCR for Mx1-Cre. Lane 1 shows a positive control, lane 2 shows wild-type C57BL/6J, lanes 3–5 show Mx1-Cre control mice and lanes 6–8 show Osmrfl/fl Mx1-Cre mice. (C) Recombination PCR assay results in control, bone marrow, lung, liver, and kidney tissues. From left: Lanes 1–2 show wild-type C57BL/6J control mice. In the remaining images, samples are ordered as lanes 1–3 being Mx1-Cre control samples and lanes 4–6 being Osmrfl/fl Mx1-Cre samples.
Following injection with poly(I:C) to induce Mx1-Cre-mediated recombination of the Osmrfl locus, we isolated DNA from bone marrow, lung, liver, and kidney tissues. These tissues were selected based on expression of both Osmr and Mx1 transcripts using publicly available databases including the human protein atlas21–23, Mouse Genome Informatics24 and The Bgee suite24. A recombination PCR assay was designed to assess Osmrfl recombination efficiency. The primers generate a product spanning the loxP-flanked exon 2 and bind to both the wild-type and modified Osmr loci generating product sizes of ~860bp for the floxed (fl) allele, 738bp for the wild-type (wt) allele and ~300bp for the recombined (∆) allele. This PCR assay detected a ~300bp recombined allele in all tissue samples from Osmrfl/fl Mx1-Cre mice (Figure 1C), demonstrating that recombination of the Osmrfl locus occurred efficiently following poly(I:C) injection in the bone marrow, lung, liver, and kidney.
Tissue-Dependent Reduction in Osmr Transcript and Protein Expression Osmrfl/fl Mx1-Cre Mice
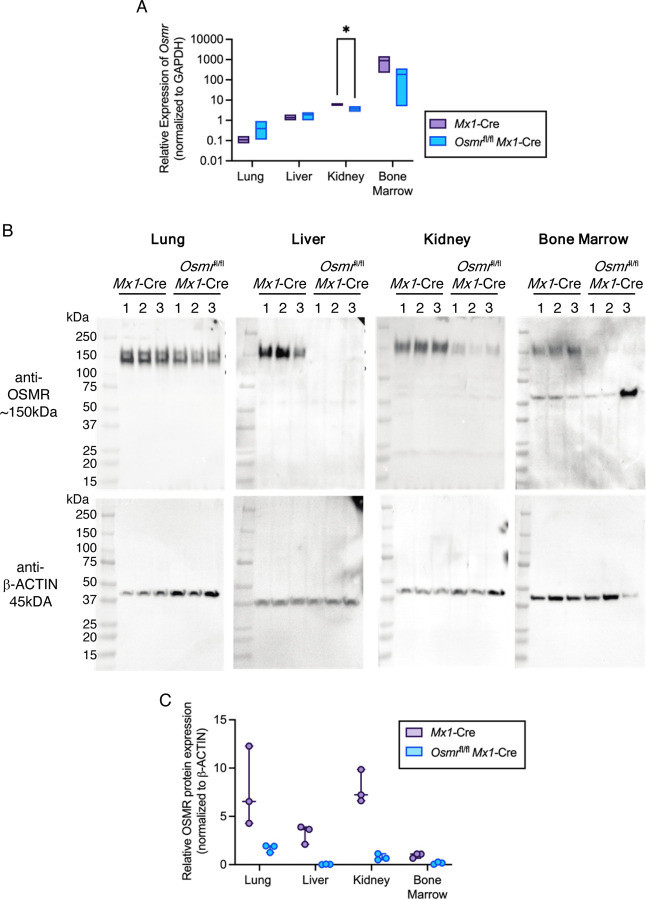
We next evaluated levels of Osmr transcript in cells from the lung, liver, kidney, and bone marrow of Osmrfl/fl Mx1-Cre and control Mx1-Cre animals. Following harvest, cells were flash-frozen and used for RNA extraction, cDNA synthesis and semi-quantitative real-time PCR. TaqMan probes annealing to a target amplicon spanning Osmr exons 17 and 18, downstream of exon 2 deletion, were used. In control Mx1-Cre mice, Osmr transcript was detected at a low level in lung cells and robustly detected in liver, kidney, and bone marrow (Figure 2A). In Osmrfl/fl Mx1-Cre mice, Osmr transcript in lung and liver was detected at similar levels as in control Mx1-Cre mice. In the kidney, Osmr transcript was significantly reduced in Osmrfl/fl Mx1-Cre mice compared to control Mx1-Cre. In the bone marrow, Osmr transcript trended toward a decrease in Osmrfl/fl Mx1-Cre mice compared to control Mx1-Cre.
Figure 2. Osmrfl/fl Mx1-Cre Mice Have Variable and Tissue-Dependent Osmr Expression at the Transcript and Protein Levels.
(A) Relative Osmr expression assessed by real-time PCR in lung, liver, kidney, and bone marrow from Mx1-Cre control and Osmrfl/fl Mx1-Cre mice (n = 3–4). Bars show low to high values with a line at the mean. *p < 0.05 by paired t test. (B) Western blots of cell lysates from lung, liver, kidney, and bone marrow probed with antibodies against OSMR and β-actin. (C) Relative protein expression assessed by Western blot imaging using ImageJ. OSMR band densities were normalized to β-actin (n = 3). Dots show individual bands/mice.
Given this tissue-dependent variation in Osmr transcript levels, we performed western blotting with a published OSMR antibody14,16,25,26 to quantify protein expression in the lung, liver, kidney, and bone marrow isolated from Osmrfl/fl Mx1-Cre and control Mx1-Cre mice. OSMR protein expression showed modest reduction in the lung of Osmrfl/fl Mx1-Cre mice compared to control Mx1-Cre mice (Figure 2B–C). OSMR expression in the liver was undetectable in Osmrfl/fl Mx1-Cre mice, and OSMR expression in the kidney and bone marrow were reduced to very low levels in Osmrfl/fl Mx1-Cre mice. Together, these data suggest that Osmrfl/fl Mx1-Cre mice have reduced OSMR in cell lysates prepared from lung, liver, kidney, and bone marrow and that the level of reduction in OSMR protein is tissue dependent.
Exploring Transcriptional Alterations in Osmrfl/fl Mx1-Cre Hematopoietic Stem Cells (HSCs)
Given the reduction in OSMR protein detected in bone marrow lysates of Osmrfl/fl Mx1-Cre mice, we utilized this model to investigate Osmr signaling in hematopoietic stem cells (HSCs) which are a small subset of bone marrow hematopoietic cells. HSCs were prospectively isolated from the bone marrow of mice using fluorescence-activated cell sorting. HSCs from Osmrfl/fl Mx1-Cre and control Mx1-Cre mice were placed into serum-free media with or without 500ng/mL of recombinant murine OSM or vehicle control for 60min, then flash frozen for RNA sequencing (RNA-seq). Significantly differentially expressed genes were defined based on stringent cutoffs (p < 0.01 and log2(FC) > 3 or < −3) (Figure 3A, Supplemental Table 1). Consistent with our real-time PCR analysis of bone marrow cells, no difference in Osmr transcript abundance was observed in Osmrfl/fl Mx1-Cre HSCs compared to control Mx1-Cre HSCs (Figure 3B). We removed predicted genes and pseudogenes from this list, resulting in a total of 91 significantly differentially expressed genes between Osmrfl/fl Mx1-Cre and control Mx1-Cre HSCs. Of these, 59 genes were increased in expression and 32 were decreased in expression in Osmrfl/fl Mx1-Cre HSCs. The top differentially expressed genes based on fold change included increased expression of Gbp2b, Myh3, Cplx3, Gpr31c and decreased expression of Wdpcp, Lgalsl, Tesk2, Tigar. Functional annotation of differentially expressed genes in Osmrfl/fl Mx1-Cre compared to control Mx1-Cre HSCs identified enrichment of signatures related to proliferation, actin binding, RNA Pol II activity and protein binding, and depletion of signatures related to smoothened pathway signaling, intraciliary transport, and protein phosphorylation (Figure 3C). These data suggest that modest transcriptional differences are observed in HSCs isolated from Osmrfl/fl Mx1-Cre compared to Mx1-Cre mice, despite lack of detectable differences in Osmr transcript itself.
Figure 3. Differential Expression Analysis in Osmrfl/fl Mx1-Cre HSCs.
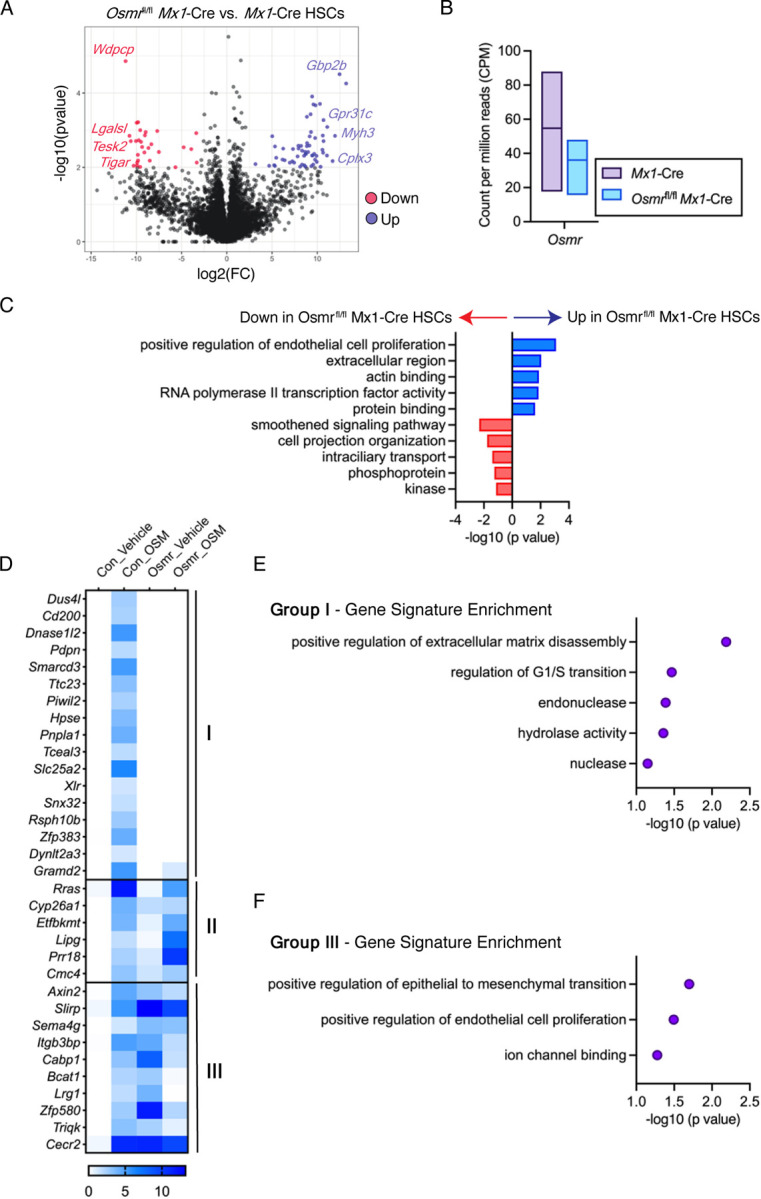
(A) Volcano plot showing differential gene expression of analysis of Osmrfl/fl Mx1-Cre vs. control Mx1-Cre HSCs (n = 3–6 biological replicates). Select significantly differentially expressed genes (p < 0.01, log2(FC) > 3 or < −3) are shown in red (down) or blue (up) font. (B) Count per million reads of Osmr transcript in control Mx1-Cre and Osmrfl/fl Mx1-Cre HSCs. Bars show low to high values with a line at the mean. (C) Gene signature enrichment within differentially expressed genes between Osmrfl/fl Mx1-Cre and control Mx1-Cre HSCs. (D) Heatmap of 37 genes induced by 60min OSM stimulation in control Mx1-Cre HSCs. Three patterns were observed: Group (I) genes were no longer induced by OSM in Osmrfl/fl Mx1-Cre HSCs, group (II) genes induced by OSM in both control Mx1-Cre and Osmrfl/fl Mx1-Cre HSCs, and group (III) genes induced by OSM in control Mx1-Cre HSCs but repressed by OSM in Osmrfl/fl Mx1-Cre HSCs. (E) Gene signature enrichment within group (I) genes. (F) Gene signature enrichment within group (III) genes.
Next, we utilized our RNA-seq dataset to explore how control Mx1-Cre versus Osmrfl/fl Mx1-Cre HSCs respond to stimulation with recombinant OSM. Using the same stringent cutoffs defined above to identify significantly upregulated genes, control Mx1-Cre HSCs had 37 genes increased in expression following OSM stimulation compared to vehicle treatment (Figure 3D, Supplemental Table 2). Examining these 37 genes in Osmrfl/fl Mx1-Cre HSCs stimulated with OSM (Supplemental Table 3) revealed several patterns; (I) 17 genes were no longer induced by OSM in Osmrfl/fl Mx1-Cre HSCs, (II) 6 genes were induced by OSM in both control Mx1-Cre and Osmrfl/fl Mx1-Cre HSCs, and (III) 10 genes were induced by OSM in control Mx1-Cre HSCs but repressed by OSM in Osmrfl/fl Mx1-Cre HSCs. The 17 genes that were induced by OSM in control Mx1-Cre HSCs but not induced in Osmrfl/fl Mx1-Cre HSCs were enriched for signatures of extracellular matrix disassembly, G1/S transition, endonuclease, and hydrolase activity (Figure 3E). In contrast, the 10 genes that were induced by OSM in control Mx1-Cre HSCs but repressed by OSM in Osmrfl/fl Mx1-Cre HSCs were enriched for signatures of epithelial to mesenchymal transition, endothelial cell proliferation and ion channel binding (Figure 3F). These data suggest that a subset of genes transcriptionally upregulated in response to OSM signaling in control Mx1-Cre HSCs are no longer upregulated in response to OSM in Osmrfl/fl Mx1-Cre HSCs, consistent with genetic knockout and functional loss of OSMR. However, as a subset of OSM signaling target genes are increased in expression in Osmrfl/fl Mx1-Cre HSCs, and other genes are no longer induced by OSM signaling, these results suggest that there is an incomplete loss of OSMRβ and/or that these genes are not bona fide targets of OSM-OSMRβ signaling.
DISCUSSION
Our data show that Osmrfl/fl Mx1-Cre mice have near-complete recombination of the genomic Osmrfl locus in bone marrow, lung, liver, and kidney tissue. However, the extent of reduction in Osmr transcript and OSMRβ protein expression in Osmrfl/fl Mx1-Cre tissues compared to Mx1-Cre tissues was dependent upon the tissue type examined. These findings are consistent with a previous study of the B6;129-Osmrtm1.1Nat/J model showing reduced OSMRβ, as opposed to a complete knockout, in K5+ epidermis14,16,25,26. Additionally, despite the lack of observable differences in Osmr transcript expression in HSCs isolated from Osmrfl/fl Mx1-Cre compared to Mx1-Cre mice, we observed alterations in the levels of other transcripts. Focusing on genes induced by OSM signaling in control Mx1-Cre HSCs, we found that only some of these genes are no longer induced by OSM signaling in Osmrfl/fl Mx1-Cre HSCs. We interpret this data to mean that residual OSMRβ expression in Osmrfl/fl Mx1-Cre HSCs permits some OSM signaling to occur. In addition, HSCs with reduction or loss of OSMRβ appear to incur compensatory activation of OSM-stimulated genes indicating a more complex, tissue-dependent regulation of OSM-OSMRβ signaling than was previously understood.
Future studies will be necessary to understand the mechanisms underlying tissue-dependent differences in Osmr transcript abundance and OSMRβ protein abundance in the B6;129-Osmrtm1.1Nat/J model. It is possible that tissue-dependent differences in transcript isoforms and/or splicing underly differences in abundance of transcript and protein. For example, transcripts lacking exon 2 may be sufficient to produce OSMRβ protein in the lung but not the liver or bone marrow. The appearance of two high molecular weight bands in the OSMRβ western blot in the lung but not in other tissues is consistent with multiple protein products being present in this tissue. In the bone marrow, a lower molecular weight band was visible in the OSMRβ western blot, which may indicate a shorter OSMRβ isoform that is still produced in Osmrfl/fl Mx1-Cre cells.
Utilizing mouse models to understand the role of OSM signaling in human pathophysiology is essential but is an inherent challenge due to the previously characterized differences in receptor binding between mice and humans. Other studies have reported novel and innovative tools to aid in overcoming this challenge. For example, with the knowledge that specific charged residues in the AB loop of OSM are crucial for selection of binding to receptor complex I versus complex II, “humanized” murine OSM variants have been generated to gain more accurate insights into the role of human OSM in mouse models16. In addition, a potent and specific inhibitor of OSM signaling has been engineered using a receptor fusion protein that contains the ligand binding domains of murine OSMRβ and murine GP13027. This construct can be delivered into cells using viral vectors and has been used in multiple studies investigating the hematopoietic stem cell niche in the bone marrow and the role of OSM in irritable bowel disease26,28. Using this construct to generate transgenic animals would be very useful for future in vivo studies. Moving forward, we advise that other tools be utilized in parallel to the B6;129-Osmrtm1.1Nat/J model and/or that studies include a detailed characterization of Osmr transcript and protein levels in the tissue and cell type of focus.
METHODS
Animals
C57BL/6J (JAX:000664) mice were obtained from The Jackson Laboratory. B6;129-Osmrtm1.1Nat/J (JAX: 011081) were crossed to B6.Cg-Tg(Mx1-cre)1Cgn/J mice (JAX:003556). In all experiments, experimental and control mice carried a single copy of the Mx1-Cre transgenic allele. To induce Mx1-Cre, mice were intraperitoneally injected once every other day for five total injections with 15 mg/kg high molecular weight polyinosinic-polycytidylic acid (polyI:C) (InvivoGen). Mice used for experiments were at least 10-weeks following polyI:C administration. Tissues with medium-to-high expression of Mx1 and Osmr were selected using publicly available databases such as the human protein atlas21–23, Mouse Genome Informatics24 and The Bgee suite24. The Jackson Laboratory’s Institutional Animal Care and Use Committee approved all experiments.
Genotyping and Recombination PCR
Genomic DNA was extracted from lysed peripheral blood samples using the DNeasy Blood & Tissue Kit (Qiagen) for genotyping. Genotyping primers were used as suggested on the B6;129-Osmrtm1.1Nat/J (JAX: 011081) mice webpage (protocol ID 29086 and 23692). Images were taken using the InGenuis LHR2 Gel imaging system (Syngene). Recombination of the Osmrfl locus was evaluated by PCR using the following primers: Forward: 5’-GGAAATACCTTGGCAGTGGTG and Reverse: 5’-GCTACCAAACCTCGGTAATCC.
Osmr mRNA Expression
RNA was isolated using the RNeasy Minikit (Qiagen) and cDNA was made using the qPCR Bio cDNA synthesis kit (PCR Biosystems). Quantitative PCR was performed using TaqMan™ Fast Advanced Master Mix (Applied Biosystems) on the QuantStudio 7 Real-Time PCR System (ThermoFisher Scientific). mRNA expression levels for Osmr (Taqman probe #Mm01307326_m1) were calculated relative to the housekeeping gene, Gapdh (Taqman probe # Mm99999915_g1).
RNA Sequencing
Bone marrow (BM) cells were isolated from Osmrfl/fl Mx1-Cre and Mx1-Cre control mice from pooled and crushed femurs, tibiae, iliac crests, sternums, forepaws, and spinal columns of individual mice. BM mononuclear cells (MNCs) were isolated by 1X Red Blood Cell lysis Buffer (eBioscience) and stained with a combination of fluorochrome-conjugated antibodies: c-Kit (BD Biosciences, BioLegend clone 2B8), Sca-1 (BioLegend clone D7), CD150 (BioLegend clone TC15-12F12.2), CD48 (BioLegend clone HM48-1), FLT3 (BioLegend clone A2F10), (Lin) marker mix (B220 (BD Biosciences, BioLegend clone RA3-6B2), and the 4′,6-diamidino-2-phenylindole (DAPI). 2,000 hematopoietic stem cells (HSCs) were sorted based on the cell surface marker combination: Lin- Sca-1+ c-Kit+ Flt3- CD150+ CD48- on a FACSAria into StemSpan SFEM II media with SCF (100 ng/ml, BioLegend), TPO (50 ng/ml, Peprotech), with or without OSM (500 ng/ml, BioLegend) and incubated at 37°C for 60min. RNA preparation, sequencing and analysis was performed following a previously published method29. Significantly differentially expressed genes were identified based on criteria of p < 0.01 and log2(FC)>3 or <−3. Predicted genes and pseudogenes were removed from the list of significantly differentially expressed genes before downstream comparisons were performed. The DAVID bioinformatics resource30,31 was used for functional annotation of significantly differentially expressed gene lists.
Western Blotting for OSMRβ
Total protein was extracted from snap frozen tissues with a Tissue Lyser II (Qiagen) using 5mm Bead Beater balls (Qiagen) after the addition of 50mM HEPES pH 7.5 (Gibco) and 6M urea (Sigma-Aldrich) at 1.5mL per 200mg tissue. Insoluble material was spun out at 21,000 x g for 20m. Total protein concentration of each sample was determined by microBCA (ThermoFisher). SDS-PAGE gel samples were prepared. Two 4–15% Mini-PROTEAN TGX Precast, 1.0mm, 15-well, SDS-PAGE Gel (Bio-Rad) were loaded with 25ug total protein per well. The gels were run at 150V for 1h at room temperature in Tris·Glycine·SDS buffer (Bio-Rad) then transferred overnight at 4°C at 40mAmp to 0.22mm PVDF (Bio-Rad) in Tris·Glycine buffer (Bio-Rad) with 10% methanol. The blots were placed in Block (2% BSA + 4% Dry Milk) at room temperature for 1h. The blots were then placed in primary antibody Polyclonal Goat IgG anti-mouse OSMR (R&D systems AF662) diluted in fresh block at 1:2500 and incubated on an orbital shaker at 4°C overnight. Then the blots were washed with TBS with 0.03% Tween 20 (TBS-T) for 15min and three more washes for 5 minutes each. Then the blots were placed in Peroxidase AffiniPure Bovine Anti-Goat IgG (H+L)(Jackson Immuno Research) diluted 1:5,000 in block. The blots rotated for 1h at room temperature and then were washed with TBS-T for 15min and three more washes for 5 minutes each. The blot was then developed with (ThermoFisher) SuperSignal West Pico Plus reagents (ThermoFisher) and visualized with a Syngene G-Box. The blots were then stripped with Restore™ PLUS Western Blot Stripping Buffer (ThermoFisher) at room temperature for 5min. The blots were re-blocked and then incubated with β-actin (Cell Signaling Technology clone D6A8) at 1:5000 for 1h at room temperature. Then the blots were washed with TBS-T for 15min and three more washes for 5 minutes each. Then the blots were placed in Goat Anti-Rabbit IgG (H+L)-HRP (Bio-Rad) diluted 1:5,000 in block. The blots rotated for 1h at room temperature and then were washed with TBS-T for 15min and three more washes for 5 minutes each. The blot was then developed with (ThermoFisher) SuperSignal West Femto Maximum Sensitivity reagents (ThermoFisher) and visualized with a Syngene G-Box. Images were quantified by ImageJ by relative intensity, adjusted for background and normalized to β-ACTIN expression per sample.
ACKNOWLEDGEMENTS
This work was supported by National Institutes of Health grants R01DK118072, R01AG069010, U01AG077925, and an EvansMDS Discovery Research Grant to J.J.T. This work was supported in part by the NIH/NCI Cancer Center Support Grant P30CA034196. J.J.T. was supported by a Leukemia & Lymphoma Society Scholar Award and The Dattels Family Endowed Chair. L.S.S. was supported by F31DK127573 and The Tufts University Scheer-Tomasso Fund philanthropic gift. We thank Drs. Jeremy Nathans and Amir Rattner for providing detailed information regarding the design of the B6;129-Osmrtm1.1Nat/J allele. We thank all members of the Trowbridge Lab, particularly Jayna Mistry, for experimental support and manuscript editing. We thank the Scientific Services at The Jackson Laboratory including flow cytometry and genome technologies. We thank Elli Hartig, Carol Bult, Ryan Tewhey, Cliff Rosen, and Phil Hinds for discussion and input into this work.
Footnotes
Data Availability
Raw RNA-seq data is available at the Gene Expression Omnibus under GSE236693 and GSE244544.
CONFLICT OF INTEREST DISCLOSURE
J.J.T. has previously received research support from H3 Biomedicine, Inc., and patent royalties from Fate Therapeutics.
Supplemental Table 1. Differential Gene Expression Analysis of Osmrfl/fl Mx1-Cre vs. Control Mx1-Cre HSCs from RNA-Seq Data. See Excel file.
Supplemental Table 2. Differential Gene Expression Analysis of OSM-Stimulated vs. Vehicle-Treated Control Mx1-Cre HSCs from RNA-Seq Data. See Excel file.
Supplemental Table 3. Differential Gene Expression Analysis of OSM-Stimulated vs. Vehicle-Treated Osmrfl/fl Mx1-Cre HSCs from RNA-Seq Data. See Excel file.
REFERENCES
- 1.Masjedi A. et al. Oncostatin M: A mysterious cytokine in cancers. Int Immunopharmacol 90, 107158 (2021). https://doi.org: 10.1016/j.intimp.2020.107158 [DOI] [PubMed] [Google Scholar]
- 2.Houben E., Hellings N. & Broux B. Oncostatin M, an Underestimated Player in the Central Nervous System. Front Immunol 10, 1165 (2019). https://doi.org: 10.3389/fimmu.2019.01165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen M. et al. Exploring the oncostatin M (OSM) feed-forward signaling of glioblastoma via STAT3 in pan-cancer analysis. Cancer Cell Int 21, 565 (2021). https://doi.org: 10.1186/s12935-021-02260-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka M. & Miyajima A. Oncostatin M, a multifunctional cytokine. Rev Physiol Biochem Pharmacol 149, 39–52 (2003). https://doi.org: 10.1007/s10254-003-0013-1 [DOI] [PubMed] [Google Scholar]
- 5.Stephens J. M. & Elks C. M. Oncostatin M: Potential Implications for Malignancy and Metabolism. Curr Pharm Des 23, 3645–3657 (2017). https://doi.org: 10.2174/1381612823666170704122559 [DOI] [PubMed] [Google Scholar]
- 6.Zarling J. M. et al. Oncostatin M: a growth regulator produced by differentiated histiocytic lymphoma cells. Proc Natl Acad Sci U S A 83, 9739–9743 (1986). https://doi.org: 10.1073/pnas.83.24.9739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malik N. et al. Molecular cloning, sequence analysis, and functional expression of a novel growth regulator, oncostatin M. Mol Cell Biol 9, 2847–2853 (1989). https://doi.org: 10.1128/mcb.9.7.2847-2853.1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Araujo A. M. et al. Stromal oncostatin M cytokine promotes breast cancer progression by reprogramming the tumor microenvironment. J Clin Invest 132 (2022). https://doi.org: 10.1172/JCI148667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flohr Svendsen A. et al. A comprehensive transcriptome signature of murine hematopoietic stem cell aging. Blood 138, 439–451 (2021). https://doi.org: 10.1182/blood.2020009729 [DOI] [PubMed] [Google Scholar]
- 10.Sempowski G. D. et al. Leukemia inhibitory factor, oncostatin M, IL-6, and stem cell factor mRNA expression in human thymus increases with age and is associated with thymic atrophy. J Immunol 164, 2180–2187 (2000). https://doi.org: 10.4049/jimmunol.164.4.2180 [DOI] [PubMed] [Google Scholar]
- 11.Auguste P. et al. Signaling of type II oncostatin M receptor. J Biol Chem 272, 15760–15764 (1997). https://doi.org: 10.1074/jbc.272.25.15760 [DOI] [PubMed] [Google Scholar]
- 12.Mosley B. et al. Dual oncostatin M (OSM) receptors. Cloning and characterization of an alternative signaling subunit conferring OSM-specific receptor activation. J Biol Chem 271, 32635–32643 (1996). https://doi.org: 10.1074/jbc.271.51.32635 [DOI] [PubMed] [Google Scholar]
- 13.Gearing D. P. et al. The IL-6 signal transducer, gp130: an oncostatin M receptor and affinity converter for the LIF receptor. Science 255, 1434–1437 (1992). https://doi.org: 10.1126/science.1542794 [DOI] [PubMed] [Google Scholar]
- 14.Walker E. C. et al. Oncostatin M promotes bone formation independently of resorption when signaling through leukemia inhibitory factor receptor in mice. J Clin Invest 120, 582–592 (2010). https://doi.org: 10.1172/JCI40568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sims N. A. Influences of the IL-6 cytokine family on bone structure and function. Cytokine 146, 155655 (2021). https://doi.org: 10.1016/j.cyto.2021.155655 [DOI] [PubMed] [Google Scholar]
- 16.Adrian-Segarra J. M. et al. The AB loop of oncostatin M (OSM) determines species-specific signaling in humans and mice. J Biol Chem 293, 20181–20199 (2018). https://doi.org: 10.1074/jbc.RA118.004375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drechsler J., Grotzinger J. & Hermanns H. M. Characterization of the rat oncostatin M receptor complex which resembles the human, but differs from the murine cytokine receptor. PLoS One 7, e43155 (2012). https://doi.org: 10.1371/journal.pone.0043155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ichihara M., Hara T., Kim H., Murate T. & Miyajima A. Oncostatin M and leukemia inhibitory factor do not use the same functional receptor in mice. Blood 90, 165–173 (1997). [PubMed] [Google Scholar]
- 19.Tanaka M. et al. Targeted disruption of oncostatin M receptor results in altered hematopoiesis. Blood 102, 3154–3162 (2003). https://doi.org: 10.1182/blood-2003-02-0367 [DOI] [PubMed] [Google Scholar]
- 20.Kuhn R., Schwenk F., Aguet M. & Rajewsky K. Inducible gene targeting in mice. Science 269, 1427–1429 (1995). https://doi.org: 10.1126/science.7660125 [DOI] [PubMed] [Google Scholar]
- 21.Uhlen M. et al. The human secretome. Sci Signal 12 (2019). https://doi.org: 10.1126/scisignal.aaz0274 [DOI] [PubMed] [Google Scholar]
- 22.Uhlen M. et al. A genome-wide transcriptomic analysis of protein-coding genes in human blood cells. Science 366 (2019). https://doi.org: 10.1126/science.aax9198 [DOI] [PubMed] [Google Scholar]
- 23.Uhlen M. et al. Proteomics. Tissue-based map of the human proteome. Science 347, 1260419 (2015). https://doi.org: 10.1126/science.1260419 [DOI] [PubMed] [Google Scholar]
- 24.Bastian F. B. et al. The Bgee suite: integrated curated expression atlas and comparative transcriptomics in animals. Nucleic Acids Res 49, D831–D847 (2021). https://doi.org: 10.1093/nar/gkaa793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang E. C. E., Dai Z., Ferrante A. W., Drake C. G. & Christiano A. M. A Subset of TREM2(+) Dermal Macrophages Secretes Oncostatin M to Maintain Hair Follicle Stem Cell Quiescence and Inhibit Hair Growth. Cell Stem Cell 24, 654–669 e656 (2019). https://doi.org: 10.1016/j.stem.2019.01.011 [DOI] [PubMed] [Google Scholar]
- 26.Bisht K. et al. Oncostatin M regulates hematopoietic stem cell (HSC) niches in the bone marrow to restrict HSC mobilization. Leukemia 36, 333–347 (2022). https://doi.org: 10.1038/s41375-021-01413-z [DOI] [PubMed] [Google Scholar]
- 27.Brolund L., Kuster A., Korr S., Vogt M. & Muller-Newen G. A receptor fusion protein for the inhibition of murine oncostatin M. BMC Biotechnol 11, 3 (2011). https://doi.org: 10.1186/1472-6750-11-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.West N. R. et al. Oncostatin M drives intestinal inflammation and predicts response to tumor necrosis factor-neutralizing therapy in patients with inflammatory bowel disease. Nat Med 23, 579–589 (2017). https://doi.org: 10.1038/nm.4307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schwartz L. S. et al. Oncostatin M is a Master Regulator of an Inflammatory Network in Dnmt3a -Mutant Hematopoietic Stem Cells. bioRxiv (2023). https://doi.org: 10.1101/2023.07.12.548764 [DOI] [Google Scholar]
- 30.Huang da W., Sherman B. T. & Lempicki R. A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc 4, 44–57 (2009). https://doi.org: 10.1038/nprot.2008.211 [DOI] [PubMed] [Google Scholar]
- 31.Sherman B. T. et al. DAVID: a web server for functional enrichment analysis and functional annotation of gene lists (2021 update). Nucleic Acids Res 50, W216–W221 (2022). https://doi.org: 10.1093/nar/gkac194 [DOI] [PMC free article] [PubMed] [Google Scholar]