Abstract
Objective
Hearing loss has been pointed out as a potential predictor for cognitive decline. This study conducted a systematic review to evaluate the scientific evidence on the association between hearing loss in the elderly and cognitive decline, as well as whether race/color influences this relationship.
Method
The search for studies was performed in the following electronic databases: MedLine/PubMed Web of Science, Scopus and Virtual Health Library, and MedRkiv up to August 2022. Studies with epidemiological designs that assess the association between hearing loss and cognitive decline in the elderly were eligible for inclusion. Three independent reviewers performed the selection, data extraction and evaluation of the quality of the studies using the Newcastle-Ottawa Scale. A meta-analysis using a random effects model estimated the global association measurements (Beta coefficient: β) and their 95% confidence intervals (95%CI), and the Higgins and Thompson indicator (I2) was also estimated to assess statistical heterogeneity among the studies.
Results
5,207 records were identified in the database surveys, of which only 18 were eligible studies, totaling 19,551 individuals. Hearing loss was associated with cognitive decline in the elderly, with statistical significance: β = -0.13; 95%CI = -0.23 to -0.04; I2 = 98.70%). For black individuals, the magnitude of the association increased: β = -0.64; 95%CI = -3.36 to 2.07; I2 = 95.65%, but it was not statistically significant.
Conclusion
The findings of this systematic review showed the existence of a significant relationship between hearing loss and cognitive decline in the elderly, as well as signaling that among black individuals the magnitude of the association can be increased.
Introduction
Projections indicate that, by 2050, life expectancy will be 82 years for men and 86 for women in developing countries [1]. In Brazil, studies by the Brazilian Institute of Geography and Statistics projected that by 2060, a quarter of the population will be over 65 years old [2]. This fact engenders complex challenges in taking care of the health of the older person, including their hearing capacity, due to the inversion of the age pyramid.
Hearing loss among the elderly reduces quality of life, due to a decrease in daily activities and sociability, and may generate processes of loss of autonomy, social isolation, depression, and dementia resulting from a cognitive decline that seems to accompany it [3–6].
Impaired hearing and cognition are disabling conditions for the elderly. The impairment of cognitive functions is directly related to an individual´s reduced interaction in their social context, hindering daily life due to detrimental changes to the domains of attention, perception, executive functions, capacity for retention and application of knowledge in daily life [7]. So far, the effect of using hearing aids on cognitive functions is still unclear, since reports on the effects of using hearing aids have produced inconclusive results, but it is known that hearing aid use can affect immediate cognitive function [8] and there is recent evidence that long-term use may delay cognitive decline [9].
Cognitive decline has been indicated as a predictor of severe cognitive diseases such as dementia and can affect up to 33% of older adults aged 85 years and over [10,11]. This scenario is further aggravated by racial disparities in health that, often, black older people have faced throughout their lives [12–15]. Furthermore, evidence indicates that cognitive decline is among the most prevalent mental health problems in elderly black individuals [15].
The relationship between hearing loss and cognitive decline has already been investigated by some researchers [16–18]. However, the two problems have a complex chain of causality, so the underlying mechanisms that lead to the connection between the two are not yet well understood [19,20]. In addition, there is an insufficient number of studies that investigated the association between hearing loss and cognitive decline in minority populations, such as the elderly black population. Racial/ethnic and socioeconomic disparities exist in hearing health care and represent critical areas for research and intervention [21].
For the best of our knowledge, there is no systematic review with meta-analysis with a sample composed exclusively of the elderly. Previous systematic reviews involved mixed populations in relation to age group [17,22–24]. Thereby, the present systematic review with meta-analysis evaluated the scientific evidence on the association between hearing loss and cognitive decline in the elderly, as well as its magnitude among elderly black individuals.
Method
Registration and protocol
The protocol of this systematic review was registered in the International Prospective Registry of Systematic Reviews—PROSPERO DATABASE: CRD42022340230. This review followed the PRISMA—2020 Statement [25].
Eligibility criteria for studies
Cohort, cross-sectional, and case-control studies involving people aged 60 years or older were included. Initially, there was no linguistic restriction, and the data collection was conducted from March 4 up to August 1, 2022. Studies without a clear description of the diagnostic criteria for hearing loss and/or cognitive decline, such as those with self-reported information, were excluded. Studies involving samples of elderly people diagnosed with dementia were also excluded.
Information sources
The studies were searched using the following electronic databases; Medline/PubMed, Virtual Health Library—VHL, Web of Science and Scopus. The reference lists of the articles selected for systematic review, as well as specific databases containing texts from the gray literature, such as MedRkiv, were also examined.
Search strategies
The descriptors used and their synonyms were identified in the Medical Subject Headings (Medical Terms Titles)—MeSH. The keywords used for the search strategies were elderly, hearing loss, cognitive dysfunction and cognitive decline. The English terms employed were: Aged, Deafness, Hearing Loss, Cognitive Impairment, Cognitive Dysfunction and Cognitive Decline. The following Boolean operators were employed: AND and OR. The initial search strategy was adapted to the other electronic databases (Chart 1 in S1 File). To assess the quality of search strategies, the Peer Review Electronic Search Strategy—PRESS was used [26].
Study selection
All phases of this review were carried out independently by 3 reviewers. Disagreements in the evaluated phases were resolved among them [25]. After excluding duplicates, the studies were selected by reading titles and abstracts (D.C.S.O., S.S.C., and A.A.M), using the Rayyan program [27]. The reviewers were unaware of the decisions made by their peers during the selection process of the articles. A.G., A.A.M., and S.S.C. read the full text of the selected articles independently, and those which met the eligibility criteria were included in the systematic review.
Data extraction
The researchers (D.C.S.O., S.S.C., and A.A.M.) performed data extraction from the included articles using the following fields: author’s name, year of publication, place and year of study, objective, study design, sample size, criteria for the diagnosis of hearing loss and cognitive decline, association measurement, presence of confounding and modifier variables and the main findings.
Quality of studies
To evaluate the quality of the selected studies, the Newcastle—Ottawa quality assessment scale for cohort, case-control and adapted for cross-sectional studies were used [28,29]. The researchers (D.C.S.O, S.S.C. and A.A.M) performed the quality assessment of all studies, independently, and then the information was confronted until a consensus was reached among them.
Data analysis
Quantitative data analysis used Stata version17® statistical package (StataCorp LLC, College Station, TX, USA). Higgins and Thompson’s I-square indicator (I2) was used to evaluate statistical heterogeneity among studies [30]. To interpret the magnitude of the inconsistency of the data among the studies included in the meta-analysis, the percentage score of test I2 was used as follows: 0% to 40%: it may not be important, as it may indicate slight heterogeneity; 30% to 60%: moderate heterogeneity; 50% to 90%: substantial heterogeneity; 75% to 100%: very substantial heterogeneity. The diagnosis of the origin of heterogeneity was also performed in the studies, using visual inspection of the Galbraith chart [31]. Eventual publication biases were evaluated by inspection performed using the of the Begg funnel chart [32].
The selection of statistical methods considered the data of the association measurements between hearing loss and cognitive decline–expressed in the Beta coefficient (β) and its 95% confident interval (95%CI) of the linear regression model between the continuous variables of exposure and outcome. The estimates of coefficient β were standardized using Cohen’s d function [33].
Results
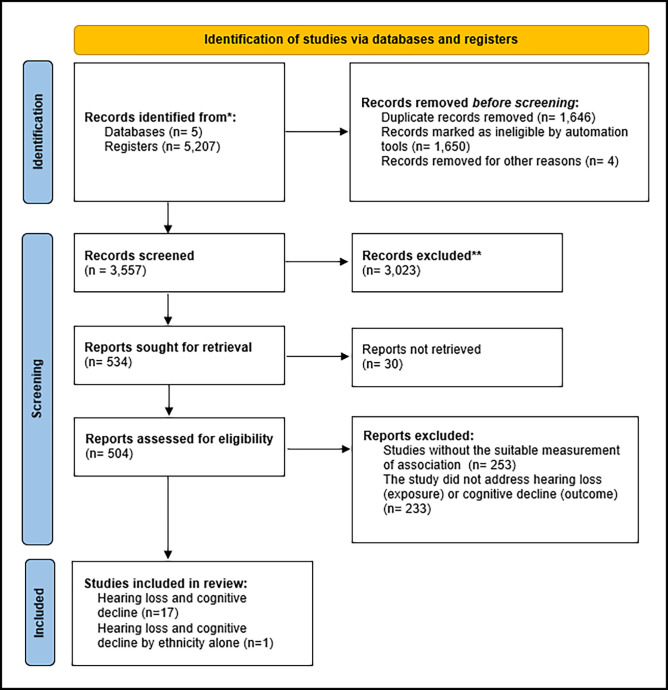
At the end of the search, 5,207 records were identified. Duplicate records were removed for reading titles and summaries. Of these, 504 articles were selected for complete reading and 18 articles met the eligibility criteria of this systematic review (Fig 1).
Fig 1. Flowchart of search, selection and inclusión of studies related to the association between hearing loss and cognitive decline in the elderly.
Qualitative analysis
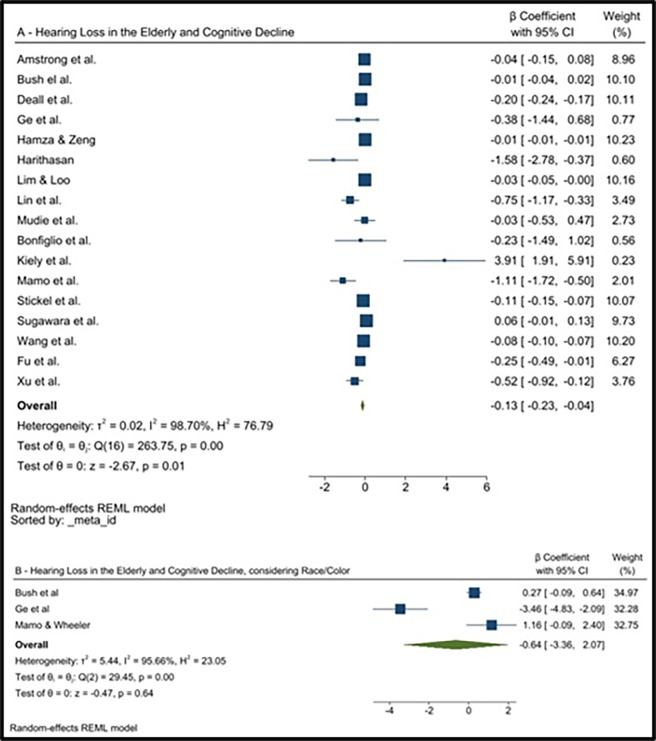
The 18 studies considered for this review included 19,551 participants. Of which, for the analysis of the association between hearing loss in the elderly and cognitive decline, regardless of race/color, 17 articles totaled 19,407 elderly people, consisting of meta-analytical model I [34–50] (Fig 2A).
Fig 2. Forest plot of the meta-analysis with association measurements: Beta coefficient (p) and 95% confidence intervals (95%CI): Between hearing loss and cognitive decline in the elderly, regardless of race/color (N = 17), and among black individuals (N = 3).
When considering the influence of race/color on the association, only 3 studies were included [37,38,40], with a total of 1,333 participants, representing meta-analytical model II (Fig 2B).
In both models, the investigations were observational. In meta-analytical model I, the number of studies were 6 (35.3%) cross-sectional, 10 (58.8%) cohort and 1 (5.9%) case-control. Most investigations occurred in the North American region 9 (52.9%). The others were developed in Asia.
In addition, in the aforementioned model, 16 (88.2%) presented ≤ 25 dB as a criterion of normal hearing level, 1 (5.9%) ≤ 40 dB and 1 (5.9%) ≤ 20 dB. Regarding the diagnosis of cognitive decline, 10 records (58.2%) used the Mini-Mental State Examination [51]; and 7 (41.2%) used other tests for definition (Table 1).
Table 1. General characteristics of the studies used in the meta-analysis without the race/color/ethnicity approach.
(N = 17).
| Characteristic | N | % |
|---|---|---|
| Study design | ||
| Cohort | 6 | 35.3 |
| Cross-sectional | 10 | 58.8 |
| Case-control | 1 | 5.9 |
| Geographic region | ||
| North America | 9 | 52.9 |
| Asia | 8 | 47.1 |
| Diagnosis of hearing loss | ||
| Normal hearing level ≤ 25 dB | 15 | 88.2 |
| Normal hearing level ≤ 40 dB | 1 | 5.9 |
| Normal hearing level ≤ 20 dB | 1 | 5.9 |
| Diagnosis of cognitive decline | ||
| Mini-Mental State Examination | 10 | 58.8 |
| Other tests * | 7 | 41.2 |
| Sample size ** | ||
| ≤ 313 | 9 | 52.94 |
| > 313 | 8 | 47.06 |
| Methodological quality | ||
| Moderate: 5–6 points | 1 | 5.9 |
| High: 7–9 points | 16 | 91.4 |
| Year of publication | ||
| ≤ 2020 | 10 | 58.8 |
| > 2020 | 7 | 41.2 |
| Funding | ||
| Yes | 12 | 70.6 |
| No | 2 | 11.8 |
| Not informed | 3 | 17.6 |
* Other tests used to diagnose cognitive decline can be found in Chart 2 in S1 File.
** Median as cut-off point.
However, for meta-analytical model II, all studies were conducted in North America 3 (100.0%) and were cross-sectional (Table 1). In this model, the criterion adopted for defining hearing loss was greater than 25 dB in the three studies included. Three different cognitive decline definition criteria were used: Mini-Mental State Examination [52]; a Telephone Interview for Cognitive (TIC) Status [37] and Consortium to Establish a Registry for Alzheimer’s Disease–CERAD [38]. Chart 2 in S1 File provides more information about these criteria used to assess cognitive function.
In both models, in general, the evaluation of the quality of the studies was classified as high, with averages of 7.94 (± 0.86). There is variation from moderate to high quality (6 to 9 points), with no article classified as low quality (Charts 3 and 4 in S1 File). In the selected investigations, covariables age and gender were considered as potential confounding factors in all individual studies.
Hearing loss and cognitive decline
The summary measurement of the meta-analytical model I estimated a significant association between hearing loss and cognitive decline, regardless of race/color (β = -0.13; 95%CI = -0.23 to -0.04), with I2 of 98.70% representing high heterogeneity among the studies (Fig 2A). A Galbraith graph was performed, showing some outlier studies but the removal of these did not change either the association measurement or the value of statistical heterogeneity (Fig 1).
The global association measurement of meta-analytical model II showed that among blacks, although the overall measurement was higher than the previous one, statistical significance was not maintained, and heterogeneity remained high: β = -0.64; 95%CI = -3.36 to 2.07; I2 = 95.66% (Fig 2B).
For the meta-analytical model I, publication bias was investigated and asymmetry in the visual analyses of the included studies were observed (Fig 2).
Discussion
The main findings of this systematic review with meta-analysis showed that there was an association between hearing loss and cognitive decline in the elderly, regardless of race/color, statistically significant. As far as we know, this is the only systematic review with meta-analysis with a sample composed exclusively of the elderly. The present study presented results similar to those published in previous systematic reviews, which involved mixed populations in relation to age group [17,22–24].
The mechanisms that can promote hearing loss, and, subsequently, become a risk factor for cognitive decline in the elderly, have not yet been completely clarified [17]. Some scholars argue that the degradation of the vascular system in the course of life is an underlying factor, which predisposes the elderly to both hearing loss and cognitive decline, since in the course of life, in general, there is physiological reduction of auditory and brain functions [52].
However, others argue that the reduction of auditory acuity generates difficulties in speech perception, reducing the speed of processing and understanding of language and, consequently, leading the individual to have memory loss, lack of attention and difficulty in developing logical thoughts. According to the above-mentioned theory, there is an important causal relationship between hearing loss and cognitive capacity restriction [53–56].
Furthermore, according to this investigation, in relation to the specific analytical measurement target for black elderly, the findings indicated that the magnitude of the global association measurement (β = -0.64) between hearing loss and cognitive decline was approximately 5 times higher than that estimated in the model in which the item race/color was not considered (β = -0.13). However, there was no statistical significance of the association among black elderly, probably because there were only 3 individual investigations [37,38,40], which presented different characteristics of the population groups involved, with a sample size, which, even having been increased through this meta-analysis, did not have enough power to answer the hypothesis raised.
It is important to highlight that of the synthesis studies that evaluated the association, none of them presented the specific meta-analytical measurement for race/color. The absence of these measurements in previous studies is the main finding of this meta-analysis. Although it is recognized that there are weaknesses in this inference, due to the low statistical power conferred by the insufficient number of studies and the high estimated heterogeneity among them [57].
However, in synthesis investigations, the absence of scientific evidence of quality, according to specific characteristics such as race/color, may be reflections of scarce and limited individual studies on the topic. In other words, the gap in knowledge cannot categorically mean the absence of the influence of race/color on the association between hearing loss and cognitive decline.
This gap may represent an important obstacle to the diagnosis of the auditory health situation of black elderly, since rational decision-making in health, which aims to combat racial inequities, should be based on qualified scientific evidence [58–61].
Although the information resulting from the research, disaggregated by race/color, has been neglected throughout the history of Health Sciences [62], this scenario is changing slowly, in Brazil and in the world. It has already been recognized that the research of health problems by race represents an important step towards the creation of an indispensable process of deconstruction of the centuries old social structure which weakens the black population and promotes the maintenance of health inequities [59,60,62].
Regarding the high heterogeneity identified in the two meta-analysis models, this can be attributed to the different classification systems of cognitive decline, different types of methodological designs and the peculiarities of the sociodemographic characteristics of the population groups that comprised the samples of the individual studies. Most of the selected studies used the Mini-Mental State Examination to diagnose cognitive decline and approximately 40% used other tests that must have contributed greatly to the difference between them. It is known that substantial measurements of heterogeneity in meta-analysis may represent the existence of bias in global estimates and, for this reason, constitute a source of concern with the evidence found [57].
On the other hand, it is noteworthy that the methodological quality of the included studies was generally considered moderate to high, which represents one of the strengths of this meta-analysis [25]. There was an effort on the part of the studies to present adjusted measurements for potential classic confounding, such as age, gender and vascular factors, through the use of multiple analysis, giving greater robustness to the overall results [63].
As positive elements of this systematic review, we mention the insertion of five bibliographic bases, with studies of moderate to high methodological quality—in addition to the use of tools and procedures already validated in the scientific environment for studies of this nature. In this sense, the Peer Review of Electronic Research Strategies (PRESS [26] was used as an instrument to evaluate the quality of research strategies, in an attempt to increase the reliability of the selection of studies.
It was not the objective of this study, but it is suggested that future systematic reviews assess the possible factors that may influence cognitive decline, such as the type of hearing loss, mixed and sensorineural, as well as its laterality, that is, bilateral or predominantly unilateral. These factors are believed to have an impact on cognitive impairment. The accurate classification of hearing loss provides valuable insights into underlying mechanisms, potential risk factors, and appropriate interventions. This will contribute to a better understanding of the diverse effects of hearing loss within specific subgroups of the elderly population and aid in the development of personalized strategies for prevention and intervention. In addition, another relevant issue that needs to be investigated is the effect of using hearing aids on cognitive functions, since it is known that hearing aid use can affect immediate cognitive function [8] and there is recent evidence that long-term use may delay cognitive decline [9,64–66].
Finally, it is important to encourage robust scientific investigations that expand the knowledge about the hypothesis of an association between hearing loss and injuries such as cognitive decline in the elderly, without neglecting the valuable information disaggregated by race/ color, particularly in regions with intense racial inequities. The detailed investigation of the true auditory and general health condition of individuals from different groups is a powerful tool in addressing racial disparities.
Supporting information
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper.
Funding Statement
The research was funded by the Foundation for Research Support of the State of Bahia - Brazil (Fundação de Amparo à Pesquisa do Estado da Bahia - FAPESB) and by National Council for Scientific and Technological Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico – CNPq). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Felix J. Longevity Economics: a review of the bibliography Brazilian society on population aging. Anais VIII Meeting of the Brazilian Association of Health Economics. 2007;7–9. [Google Scholar]
- 2.IBGE BI of G and S. Projeção da População Brasileira: número de habitantes do país deve parar de crescer em 2047. 2023. [Google Scholar]
- 3.Lawrence BJ, Jayakody DMP, Bennett RJ, Eikelboom RH, Gasson N, Friedland PL. Hearing Loss and Depression in Older Adults: A Systematic Review and Meta-analysis. Gerontologist. United States; 2020;60:e137–54. doi: 10.1093/geront/gnz009 [DOI] [PubMed] [Google Scholar]
- 4.Russo I. Auditory rehabilitation of the elderly. Audiology Treaty. São Paulo: Campos; 2011. p. 773–85. [Google Scholar]
- 5.Scheffer JC, Fialho I de M, Scholze A da S. Routes of healing and care of elderly individuals with hearing loss. Saúde Soc. 2009;18:537–48. [Google Scholar]
- 6.Veras R, Mattos L. Audiology and aging: Literature review and current horizons. Brazilian journal of otorhinolaryngology. 2007;73:122–8. doi: 10.1016/s1808-8694(15)31134-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linden GJ, Lyons A, Scannapieco FA. Periodontal systemic associations: review of the evidence. J Periodontol. United States; 2013;84:S8–19. [DOI] [PubMed] [Google Scholar]
- 8.Kalluri S, Humes LE. Hearing technology and cognition. Am J Audiol. United States; 2012;21:338–43. doi: 10.1044/1059-0889(2012/12-0026) [DOI] [PubMed] [Google Scholar]
- 9.Sarant J, Harris D, Busby P, Maruff P, Schembri A, Lemke U, et al. The Effect of Hearing Aid Use on Cognition in Older Adults: Can We Delay Decline or Even Improve Cognitive Function? J Clin Med. Switzerland; 2020;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blennow K, de Leon MJ, Zetterberg H. Alzheimer’s disease. Lancet. England; 2006;368:387–403. [DOI] [PubMed] [Google Scholar]
- 11.Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. England; 2020;396:413–46. doi: 10.1016/S0140-6736(20)30367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oliveira BLCA de Thomaz EBAF, Silva RA da. The association between skin color/race and health indicators in elderly Brazilians: a study based on the Brazilian National Household Sample Survey (2008). Cad Saude Publica. Brazil; 2014;30:1438–52. doi: 10.1590/0102-311x00071413 [DOI] [PubMed] [Google Scholar]
- 13.Rabelo DF, Silva J da, Rocha NMFD, Gomes HV, Araújo LF de. Black population racism and aging. Revista Kairós: Gerontologia. 2018;21:193–215. [Google Scholar]
- 14.Silva A. Black population: from historical iniquities to the search for full citizenship in old age. Treaty of Geriatrics and Gerontology. Rio de Janeiro: Guanabara Koogan; 2022. p. 1336–44. [Google Scholar]
- 15.Silva A da, Rosa TE da C, Batista LE, Kalckmann S, Louvison MCP, Teixeira DS da C, et al. Racial inequities and aging: analysis of the 2010 cohort of the Health, Welfare and Aging Study (SABE). Revista brasileira de epidemiologia = Brazilian journal of epidemiology. 2019;21 Suppl 02 Suppl 02:e180004. [DOI] [PubMed] [Google Scholar]
- 16.Fortunato S, Forli F, Guglielmi V, De Corso E, Paludetti G, Berrettini S, et al. A review of new insights on the association between hearing loss and cognitive decline in ageing. Acta Otorhinolaryngol Ital. Italy; 2016;36:155–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loughrey DG, Kelly ME, Kelley GA, Brennan S, Lawlor BA. Association of Age-Related Hearing Loss With Cognitive Function, Cognitive Impairment, and Dementia: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. United States; 2018;144:115–26. doi: 10.1001/jamaoto.2017.2513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yuan J, Sun Y, Sang S, Pham JH, Kong W-J. The risk of cognitive impairment associated with hearing function in older adults: a pooled analysis of data from eleven studies. Sci Rep. England; 2018;8:2137. doi: 10.1038/s41598-018-20496-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jafari Z, Kolb BE, Mohajerani MH. Age-related hearing loss and tinnitus, dementia risk, and auditory amplification outcomes. Ageing Res Rev. England; 2019;56:100963. doi: 10.1016/j.arr.2019.100963 [DOI] [PubMed] [Google Scholar]
- 20.Uchida Y, Sugiura S, Nishita Y, Saji N, Sone M, Ueda H. Age-related hearing loss and cognitive decline—The potential mechanisms linking the two. Auris Nasus Larynx. Netherlands; 2019;46:1–9. doi: 10.1016/j.anl.2018.08.010 [DOI] [PubMed] [Google Scholar]
- 21.Nieman CL, Marrone N, Szanton SL, Thorpe RJJ, Lin FR. Racial/Ethnic and Socioeconomic Disparities in Hearing Health Care Among Older Americans. J Aging Health. United States; 2016;28:68–94. doi: 10.1177/0898264315585505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lau K, Dimitriadis PA, Mitchell C, Martyn-St-James M, Hind D, Ray J. Age-related hearing loss and mild cognitive impairment: a meta-analysis and systematic review of population-based studies. J Laryngol Otol. England; 2022;136:103–18. doi: 10.1017/S0022215121004114 [DOI] [PubMed] [Google Scholar]
- 23.Lee SJ. The Relationship between Hearing Impairment and Cognitive Function in Middle-Aged and Older Adults: A Meta-Analysis. Commun Sci Disord. The Korean Academy of Speech-Language Pathology and Audiology; 2018;23:378–91. [Google Scholar]
- 24.Utoomprurkporn N, Woodall K, Stott J, Costafreda SG, Bamiou DE. Hearing-impaired population performance and the effect of hearing interventions on Montreal Cognitive Assessment (MoCA): Systematic review and meta-analysis. Int J Geriatr Psychiatry. England; 2020;35:962–71. doi: 10.1002/gps.5354 [DOI] [PubMed] [Google Scholar]
- 25.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. United States; 2016;75:40–6. [DOI] [PubMed] [Google Scholar]
- 27.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS One. 2016;11:e0147601. doi: 10.1371/journal.pone.0147601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wells G, Shea B, O’Conneell D, Peterson J, Welch V, Loso M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [Internet]. The Ottawa Hospital: Research Institute.; 2014. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Google Scholar]
- 30.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. [Internet]. 5.1.0. London: Cochrane Collaboration; 2011. Available from: https://training.cochrane.org/handbook/archive/v5.1/ [Google Scholar]
- 31.Dinnes J, Deeks J, Kirby J, Roderick P. A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy. Health Technol Assess. England; 2005;9:1–113, iii. doi: 10.3310/hta9120 [DOI] [PubMed] [Google Scholar]
- 32.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Espirito Santo H, Daniel F. Calcular e apresentar tamanhos do efeito em trabalhos científicos (1): As limitações do p < 0,05 na análise de diferenças de médias de dois grupos | Calculating and reporting effect sizes on scientific papers (1): p < 0.05 limitations in the analysis of mean differences of two groups. Portuguese Journal of Behavioral and Social Research. 2015;1:3–16. [Google Scholar]
- 34.Bonfiglio V, Umegaki H, Kuzuya M. A Study on the Relationship between Cognitive Performance, Hearing Impairment, and Frailty in Older Adults. Dement Geriatr Cogn Disord. Switzerland; 2020;49:156–62. [DOI] [PubMed] [Google Scholar]
- 35.Deal JA, Gross AL, Sharrett AR, Abraham AG, Coresh J, Carlson M, et al. Hearing impairment and missing cognitive test scores in a population-based study of older adults: The Atherosclerosis Risk in Communities neurocognitive study. Alzheimers Dement. United States; 2021;17:1725–34. [DOI] [PubMed] [Google Scholar]
- 36.Fu X, Liu B, Wang S, Eikelboom RH, Jayakody DMP. The Relationship Between Hearing Loss and Cognitive Impairment in a Chinese Elderly Population: The Baseline Analysis. Front Neurosci. Switzerland; 2021;15:749273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ge S, McConnell ES, Wu B, Pan W, Dong X, Plassman BL. Longitudinal Association Between Hearing Loss, Vision Loss, Dual Sensory Loss, and Cognitive Decline. J Am Geriatr Soc. United States; 2021;69:644–50. doi: 10.1111/jgs.16933 [DOI] [PubMed] [Google Scholar]
- 38.Hamza Y, Zeng F-G. Tinnitus Is Associated With Improved Cognitive Performance in Non-hispanic Elderly With Hearing Loss. Front Neurosci. Switzerland; 2021;15:735950. doi: 10.3389/fnins.2021.735950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harithasan D, Mukari SZ-MS, Ishak WS, Shahar S, Yeong WL. The impact of sensory impairment on cognitive performance, quality of life, depression, and loneliness in older adults. Int J Geriatr Psychiatry. England; 2020;35:358–64. doi: 10.1002/gps.5237 [DOI] [PubMed] [Google Scholar]
- 40.Harrison Bush AL, Lister JJ, Lin FR, Betz J, Edwards JD. Peripheral Hearing and Cognition: Evidence From the Staying Keen in Later Life (SKILL) Study. Ear Hear. United States; 2015;36:395–407. doi: 10.1097/AUD.0000000000000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kiely KM, Gopinath B, Mitchell P, Luszcz M, Anstey KJ. Cognitive, health, and sociodemographic predictors of longitudinal decline in hearing acuity among older adults. J Gerontol A Biol Sci Med Sci. United States; 2012;67:997–1003. doi: 10.1093/gerona/gls066 [DOI] [PubMed] [Google Scholar]
- 42.Lim MYL, Loo JHY. Screening an elderly hearing impaired population for mild cognitive impairment using Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA). Int J Geriatr Psychiatry. England; 2018;33:972–9. doi: 10.1002/gps.4880 [DOI] [PubMed] [Google Scholar]
- 43.Lin FR, Yaffe K, Xia J, Xue Q-L, Harris TB, Purchase-Helzner E, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. United States; 2013;173:293–9. doi: 10.1001/jamainternmed.2013.1868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mamo SK, Reed NS, Sharrett AR, Albert MS, Coresh J, Mosley TH, et al. Relationship Between Domain-Specific Cognitive Function and Speech-in-Noise Performance in Older Adults: The Atherosclerosis Risk in Communities Hearing Pilot Study. Am J Audiol. United States; 2019;28:1006–14. doi: 10.1044/2019_AJA-19-00043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mamo SK, Wheeler KA. The Combined Burden of Hearing Loss and Cognitive Impairment in a Group Care Setting for Older Adults. J Speech Lang Hear Res. United States; 2021;64:328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mudie LI, Varadaraj V, Gajwani P, Munoz B, Ramulu P, Lin FR, et al. Dual sensory impairment: The association between glaucomatous vision loss and hearing impairment and function. PLoS One. United States; 2018;13:e0199889. doi: 10.1371/journal.pone.0199889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stickel A, Tarraf W, Bainbridge K, Viviano R, Daviglus M, Dhar S, et al. Hearing Sensitivity, Cardiovascular Risk, and Neurocognitive Function: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). JAMA Otolaryngology—Head and Neck Surgery. 2020;147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sugawara N, Sasaki A, Yasui-Furukori N, Kakehata S, Umeda T, Namba A, et al. Hearing impairment and cognitive function among a community-dwelling population in Japan. Ann Gen Psychiatry. England; 2011;10:27. doi: 10.1186/1744-859X-10-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang J, Wang F, Han P, Liu Y, Ma W, Zhang H, et al. Gender-specific associations of speech-frequency hearing loss, high-frequency hearing loss, and cognitive impairment among older community dwellers in China. Aging Clin Exp Res. Germany; 2022;34:857–68. doi: 10.1007/s40520-021-01990-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xu Y, Li Y, Guo D, Zhang X, Guo H, Cao H, et al. Association of Hearing Acuity and Cognitive Function Among a Low-Income Elderly Population in Rural China: A Population-Based Cross-Sectional Study. Front Neurosci. Switzerland; 2021;15:704871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. England; 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 52.Meneses C, Mário MP, Marchori LL de M, Melo JJ, Freitas ERFS de. Prevalence of hearing loss and associated factors in elderly population in Londrina, Paraná: preliminary study. 2010;12:384–92. [Google Scholar]
- 53.Camargo C, Lacerda ABM, Sampaio J, Lüders D, Massi G, Marques JM. Perception of elderly people about the restriction of participation related to hearing loss. 2018;30:736–47. [Google Scholar]
- 54.Mahmoudi E, Basu T, Langa K, McKee MM, Zazove P, Alexander N, et al. Can Hearing Aids Delay Time to Diagnosis of Dementia, Depression, or Falls in Older Adults? J Am Geriatr Soc. United States; 2019;67:2362–9. [DOI] [PubMed] [Google Scholar]
- 55.Souza VC, Lemos SMA. Participation restriction of adults and elderly users of an audiology clinic: association with auditory and social-environmental factors. Codas. Brazil; 2021;33:e20200212. [DOI] [PubMed] [Google Scholar]
- 56.Xavier IL, Teixeira AR, Olchik MR, Gonçalve AK, Lessa AH. Hearing screening and perceived participation restriction in the elderly. Audiol Commun Res. 2018;23:e1867. [Google Scholar]
- 57.Galvao T, Pereira M. Heterogeneidade e viés de publicação em revisões sistemáticas. Epidemiologia e serviços de saúde. 2014;23:775–8. [Google Scholar]
- 58.Araújo E, Costa M, Noronha C, Hogan V, Vines A, Araújo T. Desigualdades em saúde e raça/cor da pele: revisão da literatura do Brasil e dos Estados Unidos (1996–2005). Saúde Coletiva. 2010; [Google Scholar]
- 59.Brasil M da S. Guia de implementação do quesito: raça/cor /etnia. 2018; Available from: http://bvsms.saude.gov.br/bvs/publicacoes/guia_implementacao_raca_cor_etnia.pdf. [Google Scholar]
- 60.Silva NG, Barros S, Azevedo FC de, Batista LE, Policarpo VC. The race/color variable in studies of characterization of the users of Psychosocial Care Centers. Saúde e Sociedade. 2017;26:100–14. [Google Scholar]
- 61.Werneck J. Institutional racism and black population health. Saúde Soc. 2016;25:535–49. [Google Scholar]
- 62.Araujo EM, Lilly Caldwell K, Pereira Alves dos Santos M, Magalhães de Souza I, Lima Ferreira Santa Rosa P, Beatriz Silva dos Santos A, et al. COVID-19 morbimortality by race/skin color/ethnicity: the experience of Brazil and the United States. SciELO Preprints [Internet]. 2020; Available from: https://preprints.scielo.org/index.php/scielo/preprint/view/1318. [Google Scholar]
- 63.Brazil M of H of Brazil. Methodological guidelines: preparation of systematic review and meta-analysis of randomized clinical trials/ Ministry of Health, Secretariat of Science, Technology and Strategic Insumos, Department of Science and Technology. Brasilia: Ministry of Health of Brazil; 2012. [Google Scholar]
- 64.Issing C, Baumann U, Pantel J, Stöver T. Impact of Hearing Rehabilitation Using Cochlear Implants on Cognitive Function in Older Patients. Otol Neurotol. United States; 2021;42:1136–41. doi: 10.1097/MAO.0000000000003153 [DOI] [PubMed] [Google Scholar]
- 65.Mosnier I, Bebear J-P, Marx M, Fraysse B, Truy E, Lina-Granade G, et al. Improvement of cognitive function after cochlear implantation in elderly patients. JAMA Otolaryngol Head Neck Surg. United States; 2015;141:442–50. doi: 10.1001/jamaoto.2015.129 [DOI] [PubMed] [Google Scholar]
- 66.Sarant J, Harris D, Busby P, Maruff P, Schembri A, Dowell R, et al. The Effect of Cochlear Implants on Cognitive Function in Older Adults: Initial Baseline and 18-Month Follow Up Results for a Prospective International Longitudinal Study. Front Neurosci. Switzerland; 2019;13:789. doi: 10.3389/fnins.2019.00789 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper.