Abstract
Background
Elevations of hepatic transaminase (serum alanine transaminase [ALT] and serum aspartate aminotransferase [AST]) levels in patients with acute coronary syndrome (ACS), although transient, may result in exclusions from clinical efficacy trials due to suspected liver disease. The aim of this study was to evaluate the concentrations of serum transaminases in ACS and relate these to currently accepted AST/ALT exclusion criteria from clinical trials.
Methods
One hundred consecutive patients with ACS were prospectively examined. Blood samples for AST, ALT, total bilirubin and troponin I concentration were obtained at the time of admission and after 6, 12 and 24 hours.
Results
Eighty percent of patients had elevated AST, and 47% ALT; 43% of patients characterized AST concentration > 3 × upper limit of normal (ULN) in at least one measurement, while 8% of patients presented ALT concentration > 3 × ULN. AST presented higher concentrations when compared to ALT, resulting in a high De-Ritis ratio at every time point. No significant or high correlations were found between the concentrations of serum transaminases, De-Ritis ratio and troponin I. Two different cut-off values of troponin I were adopted to define the amount of infarcted myocardium that distinguished 28–31% of individuals with “large infarction”. Among these patients, approximately 93% presented AST concentrations > 3 × ULN.
Conclusions
Hepatic transaminases are often elevated in ACS, with the majority of patients with more extensive myocardial injury presenting high concentrations of AST. In the setting of ACS, current transaminase thresholds for liver dysfunction used in clinical trials may lead to excessive and inadequate exclusions of patients with larger infarcts from such trials.
Keywords: serum alanine transaminase, serum aspartate aminotransferase, acute coronary syndrome, clinical trial, exclusion criteria
Introduction
Serum alanine transaminase (ALT) and serum aspartate aminotransferase (AST) are routinely used in clinical practice as basic markers of liver injury. ALT is predominantly derived from hepatocytes — which is a specific serum marker of liver disease. AST is derived not only from the liver, but also from the heart, red blood cells, skeletal muscles, kidney and is elevated after ischemic cell death in these tissues.
Apart from liver disease, these enzymes are often elevated in patients with acute coronary syndromes (ACS) [1], most commonly as a result of myocardial injury, but it is also a consequence of low cardiac output and arterial hypoperfusion. In 1954, AST was the first cardiac biomarker to be applied to aid diagnosis of acute myocardial infarction, but due to lack of specificity for cardiac tissue, it does not remain in use [2, 3]. Elevation in transaminases following ACS is usually transient and returns to normal limits within several days unless there is ongoing hemodynamic compromise or a low output state.
Liver tests, in particular ALT, AST and total bilirubin are still the key safety laboratory parameters used in controlled clinical trials (CCT) to screen for hepatic dysfunction [4]. Numerous studies require the exclusion of participants with AST or ALT that is 2–2.5 or 3 × upper limit of normal (ULN). This practice is based on “Hy’s Law”, articulated in 1999 — a recommendation to use a screening threshold of liver tests for use in CCT (ALT or AST > 3 × ULN and total bilirubin > 2 × ULN, that is not primarily cholestatic and is not caused by disease but by the drug) [5]. This recommendation is often misunderstood by trialists or regulatory authorities, as the vast majority of exclusion criteria are based only on the above-mentioned laboratory thresholds. It is noteworthy that elevated transaminases may reflect injury of liver cells, if injured, but not the severity of liver dysfunction and in case of AST, may have been derived from other tissues. Liver dysfunction then must be measured by other tests and take into account the clinical context, in terms of other possible causes or patient hepatic risk factors.
Significant elevation of AST and ALT levels during ACS, although transient, may result in exclusion of substantial numbers of patients from clinical efficacy trials and substantial selection bias. Moreover, the studies indicate that if no other causes of liver injury are identified, the elevations of serum transaminases are associated with more severe myocardial damage, systolic dysfunction and higher cardiac-related mortality in ACS patients [6]. Thus, participants in such clinical trials that exclude those with raised transaminases may not represent a real-world population with the disease.
The goal of the present study was to evaluate the concentrations of serum liver transaminases in patients with ACS in contemporary practice and attempt to indicate the subgroup of patients that might be hypothetically eligible for clinical trials, irrespective of conventionally accepted AST/ALT exclusion criteria.
Methods
In this single-center observational study, 100 consecutive patients with ACS were examined and admitted to the Cardiology Department of University Hospital No. 1 in Bydgoszcz, Poland, from July 1, 2018 to February 28, 2019. Patients were treated for ST-elevation and non-ST elevation myocardial infarction (STEMI and NSTEMI) in accordance with dedicated guidelines of the European Society of Cardiology. The study protocol complies with the declaration of Helsinki and was approved by the local ethics committee of Nicolaus Copernicus University in Torun, Poland.
Peripheral blood samples for AST, ALT, AST/ALT ratio (De-Ritis) and troponin I concentrations were obtained at the time of admission and after 6, 12 and 24 hours following admission. Total bilirubin concentrations were assessed at admission and after 24 hours. According to local guidelines, an abnormal ALT level was defined as a serum concentration > 50 U/L for men and 40 U/L for women; for AST > 40 U/L and > 35 U/L, respectively. Enzyme activities were measured at a local laboratory using commercially available enzymatic assays (Roche Diagnostics, Austria).
Statistical analysis
The normality of the distribution was verified using the Shapiro-Wilk test. Continuous variables are presented as median and interquartile range (IQR) or mean ± standard deviation (SD), categorical variables as absolute frequencies and percentages. The comparison between two variables was performed with the Mann-Whitney U test or appropriate Student t-test according to the distribution. For comparison of more than two variables the Kruskal-Wallis test or ANOVA was used based on the normality of data distribution. Analyses of correlations were performed using the Pearson or Spearman test as required. A two-sided p value < 0.05 was considered significant. STATISTICA version 13.1 was used to perform the analyses.
Results
Baseline characteristics of the group are presented in Table 1. History of liver disease or known alcohol addiction was noted in only 5 and 2 individuals, respectively. Amongst patients with documented prior liver disease, patients mainly suffered from liver cirrhosis (n = 3), or previous hepatitis type B (n = 1) or C (n = 1). All STEMI patients were treated with primary percutaneous coronary intervention (PCI). Of those presenting with NSTEMI, 20% were treated with a non-invasive strategy, 77% with PCI and 3% with coronary artery bypass grafting.
Table 1.
Baseline characteristics of the study group.
| Parameter | N = 100 |
|---|---|
| Age, years [SD] | 67 [12] |
| Sex, male | 71 |
| Myocardial infarction: | |
| STEMI | 65 |
| NSTEMI | 35 |
| Statin treatment prior to ACS: | |
| No | 78 |
| Yes | 22 |
| History of liver disease: | |
| No | 95 |
| Yes | 5 |
| History of alcohol abuse: | |
| No | 98 |
| Yes | 2 |
ACS — acute coronary syndrome; NSTEMI — non-ST segment myocardial infarction; STEMI — ST-segment myocardial infarction; SD — standard deviation
Using the definitions of abnormal transaminase levels described previously, 80% of patients had elevated AST, and 47% had elevated ALT in at least one measurement. In the current study population, 43% of patients had at least one AST concentration > 3 × ULN, while 8% of patients had at least one ALT concentration > 3 × ULN. Mean baseline bilirubin concentration was 0.68 (0.51) mg/dL (normal range 0.2–1.1 mg/dL) and did not differ from concentrations at 24 hours (0.89 [0.43], p > 0.05).
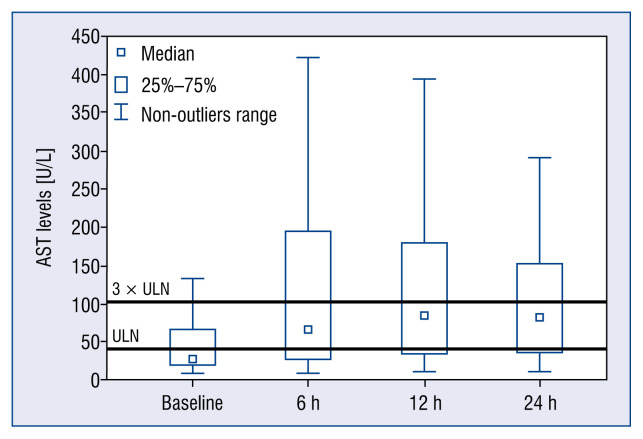
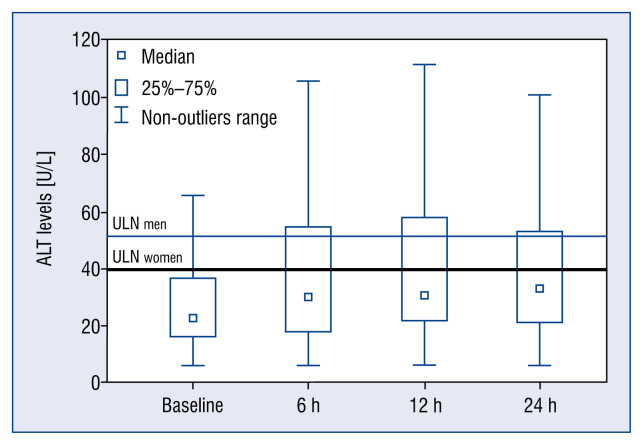
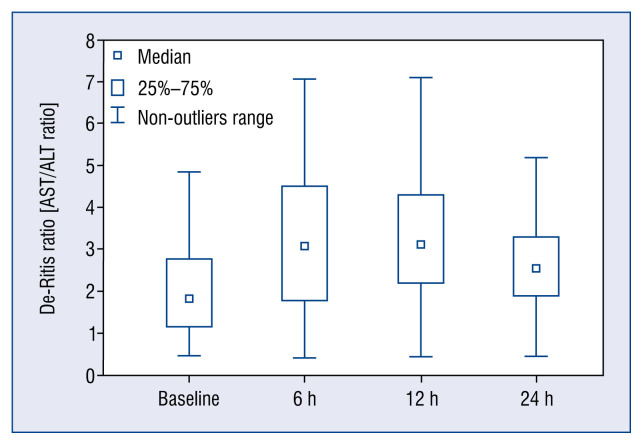
Concentrations of troponin I are presented in Figure 1. Transaminase concentrations began to rise during first 6 hours from admission, reaching a peak mostly at 12 hours (Figs. 2, 3). Elevation of AST levels were higher than ALT, resulting in high De-Ritis ratio at every time point (Fig. 4). Elevation of AST concentration > 3 × ULN was detected in 13% of patients at the time of admission, in 34% of patients at 6 hours, in 43% at 12 hours and in 38% of cases 24 hours post-admission. Similar to AST, the concentrations of ALT > 3 × ULN were detected in 4% of patients at the time of admission, in 8% of patients at 6 hours, 6% of patients at 12 hours and in 4% of patients at 24 hours post-admission.
Figure 1.
Median serum concentrations of troponin I at baseline and after 6, 12 and 24 hours from admission; p < 0.001, Friedman ANOVA.
Figure 2.
Median serum concentrations of aspartate aminotransferase (AST) at baseline and after 6, 12 and 24 hours from admission; p < 0.001, Friedman ANOVA; ULN — upper limit of normal.
Figure 3.
Median serum concentrations of alanine transaminase (ALT) at baseline and after 6, 12 and 24 hours from admission; p < 0.001, Friedman ANOVA; ULN — upper limit of normal.
Figure 4.
De-Ritis ratio (aspartate aminotransferase/alanine transaminase [AST/ALT]) at the time points: at baseline and after 6, 12 and 24 hours from admission. De-Ritis ratio calculated when AST or/and ALT concentration was above the upper limit of normal (n = 42).
Serum concentrations of troponin I correlated with ALT (r = 0.60, p < 0.001), AST (r = 0.86, p < 0.001) and De-Ritis ratio (r = 0.71, p < 0.001). Based on these results, the aim was to assess AST and ALT levels in relation to infarct size, estimated by troponin I release. Peak values of troponin, AST and ALT were observed mostly at 12 hours from admission; thus, the analyses were performed at this time point. For the purpose of this study, two different cut-off values of troponin I were adopted to define the amount of infarcted myocardium, named “large infarction”: 1) troponin I concentration > 50 000 ng/L; 2) troponin I concentration ≥ 3rd quartile, that is ≥ 4111.9 ng/L. Based on this definition, 28–31% of the patients had “large infarction”. Among these patients, approximately 93% had AST concentration > 3 × ULN. The same analysis was performed for ALT. Results are shown in Table 2.
Table 2.
Proportions of patients with “large infarction” and significantly elevated aspartate aminotransferase (AST), alanine transaminase (ALT) concentrations as well as De-Ritis ratio > 1.
| Definition of large infarction | Definition met (number of patients) | Proportion of patients with AST level > 3 × ULN | Proportion of patients with ALT level > 3 × ULN | Proportion of patients with De-Ritis ratio > 1 |
|---|---|---|---|---|
| Troponin I > 50 000 ng/L | 28 | 92.9% (26) | 17.9% (5) | 28 (100%) |
| Troponin I ≥ 3rd quartile | 31 | 93.5% (29) | 16.1% (5) | 31 (100%) |
ULN — upper limit of normal
Discussion
Consistent with other authors, it was confirmed that in the present diagnostic and treatment era of ACS, transaminase elevation commonly occurs. Moreover, it was confirmed that the relation of transaminase concentration to enzymatic estimations of infarct size, as defined by troponin I level. The present study documents that the majority of patients with more extensive myocardial injury present with high concentrations of AST, above 3 times ULN. Based on these results, the use of conventionally-accepted biochemical exclusion criteria for liver dysfunction, adopted for the purpose of clinical trials, would result in exclusion of 13–43% of patients with ACS from clinical trials during the first 24 hour post-admission. Taken together, despite the small sample size of the current study, it was shown that currently used criteria for liver dysfunction may not mirror liver-specific dysfunction in the setting of ACS and may not be suitable.
Elevated serum transaminase activity in ACS patients has been ascribed to hypoxic liver injury (HLI) [7, 8]. Circulatory failure in ACS (arterial hypoperfusion, low cardiac output) directly influence hepatic blood flow, resulting in hepatocellular dysfunction and elevation of AST and ALT. It is usually a transient and reversible condition. The typical laboratory finding in HLI is the elevation in transaminase and lactate dehydrogenase (LDH) levels. Transaminase and LDH levels peak 1–3 days after the acute event and return to normal within 7–10 days, unless there is persistent hemodynamic compromise. Other laboratory findings are mild elevations of serum bilirubin, alkaline phosphatase and prolongation of prothrombin time. Nevertheless, HLI alone cannot explain the elevation in transaminases observed in ACS patients. It is now evident that AST and ALT release in these patients is attributed primarily to myocardial rather than hepatic origin [1, 9]. In the present study, AST concentrations were relatively higher than ALT concentrations, resulting in high De-Ritis ratio at every time point. Moreover, the correlation between AST and troponin I, was greater than that between ALT and troponin. These findings directly indicate predominant extrahepatic origin of AST release.
It is clear that, for the purposes of clinical trials, elevation in transaminase levels cannot, in isolation, be used to identify hepatic dysfunction, in part due to the important myocardial source of such enzyme rise as well as the reversible nature of such enzymatic fluctuations in patients with ACS. With regard to the ACS population, the conventionally-accepted transaminase threshold values accepted for clinical trials [10, 11] seem to be too low and likely result in exclusion of patients with a primary cardiac cause for such enzyme elevation, without primary hepatic dysfunction. The differential diagnosis of serious liver insufficiency in ACS patients requires more clinical and laboratory investigation, including functional assessment of liver synthesis including tests of coagulation and albumin, as well as repetitive testing. The present study demonstrated that when troponin, AST and ALT concentrations were elevated, the De-Ritis ratio was high.
This study shows that 93% of ACS patients with severe myocardial injury as defined by troponin I level, have transaminase levels elevated > 3 times ULN. As far as the accepted liver-based screening criteria for CCT are concerned, it appears that a significant group of patients may be excluded from dedicated clinical trials. Moreover, the rest of participants may not be representative of the real-world population with the disease [12–14]. On the other hand, recent evidence suggests that elevated serum transaminases are associated with more severe myocardial damage along with worse short- and long-term clinical outcomes [6, 15, 16]. Regarding the prognostic potential of transaminases in ACS patients, particularly in relation to the severity of myocardial damage, accepted hepatic biochemistry-based exclusion criteria might limit the participation of high-risk patients in such trials. If clinical trials enroll only a highly selected population, the results may not be generalized to individuals at higher risk [17, 18]. There is, therefore, a gap in adequate recommendations for patient subgroups who are the highest risk and who may benefit most from new interventions in CCT.
Limitations of the study
The present study is limited mainly by the single center setting and the relatively small sample size. Additionally, it was not possible to sufficiently report the time intervals between symptom onset and hospital admission. Thus, enzyme dynamics may not reflect real ACS time course. Although this study is not representative of all ACS patients, it was assumed that it was sufficient to address important concerns regarding CCT exclusion criteria commonly used in these settings.
Conclusions
In conclusion, it was shown that accepted AST and ALT exclusion thresholds for liver dysfunction, adopted for the purpose of CCT, may not mirror liver-specific dysfunction in the setting of ACS. If data management in clinical trials are influenced by the clinical context in which each study drug or intervention will be used, there is a need for re-evaluation of existing biochemistry screening criteria for liver dysfunction in ACS patients. Such revised criteria would allow inclusion of more individuals at higher risk, and reduce the number of patients who screen-fail in CCT and who may therefore benefit from the studied intervention. Revision or expansion of eligibility criteria might, however, increase the heterogeneity of the study population, but this is likely to be offset by the greater benefit: risk ratio that is likely to be observed in the highest risk patients.
Footnotes
Conflict of interest: None declared
References
- 1.Lofthus DM, Stevens SR, Armstrong PW, et al. Pattern of liver enzyme elevations in acute ST-elevation myocardial infarction. Coron Artery Dis. 2012;23(1):22–30. doi: 10.1097/MCA.0b013e32834e4ef1. [DOI] [PubMed] [Google Scholar]
- 2.Karmen A, Wroblewski F, Laude JS. Transaminase activity in human blood. J Clin Invest. 1955;34(1):126–131. doi: 10.1172/JCI103055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laude JS, Wroblewski F, Karmen A. Serum glutamic oxaloacetic transaminase activity in human acute transmural myocardial infarction. Science. 1954;120(3117):497–499. doi: 10.1126/science.120.3117.497. [DOI] [PubMed] [Google Scholar]
- 4.FDA Guidance for Industry; Services USDoHaH, editor. Drug - induced liver injury: Premarketing Clinical Evaluation. 2009. http://www.fda.gov/Drugs/GuidanceComplianceRegulatory-Information/Guidances/default.html .
- 5.Senior JR. How can ‚Hy’s law’ help the clinician? Pharmacoepidemiol Drug Saf. 2006;15(4):235–239. doi: 10.1002/pds.1210. [DOI] [PubMed] [Google Scholar]
- 6.Gao M, Cheng Yi, Zheng Y, et al. Association of serum transaminases with short- and long-term outcomes in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. BMC Cardiovasc Disord. 2017;17(1):43. doi: 10.1186/s12872-017-0485-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weisberg IS, Jacobson IM. Cardiovascular diseases and the liver. Clin Liver Dis. 2011;15(1):1–20. doi: 10.1016/j.cld.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Ebert EC. Hypoxic liver injury. Mayo Clin Proc. 2006;81(9):1232–1236. doi: 10.4065/81.9.1232. [DOI] [PubMed] [Google Scholar]
- 9.Giesen PL, Peltenburg HG, de Zwaan C, et al. Greater than expected alanine aminotransferase activities in plasma and in hearts of patients with acute myocardial infarction. Clin Chem. 1989;35(2):279–283. [PubMed] [Google Scholar]
- 10.Kubica J, Adamski P, Ostrowska M, et al. Morphine delays and attenuates ticagrelor exposure and action in patients with myocardial infarction: the randomized, double-blind, placebo-controlled IMPRESSION trial. Eur Heart J. 2015;37(3):245–252. doi: 10.1093/eurheartj/ehv547.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kubica J, Adamski P, Ostrowska M, et al. Influence of Morphine on Pharmacokinetics and Pharmacodynamics of Ticagrelor in Patients with Acute Myocardial Infarction (IMPRESSION): study protocol for a randomized controlled trial. Trials. 2015;16:198. doi: 10.1186/s13063-015-0724-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piątek Ł, Wilczek K, Kurzawski J, et al. Impact of routine invasive strategy on outcomes in patients with non-ST-segment elevation myocardial infarction during 2005–2014: A report from the Polish Registry of Acute Coronary Syndromes (PL-ACS) Cardiol J. 2020;27(5):583–589. doi: 10.5603/CJ.a2018.0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kubica J, Adamski P, Paciorek P, et al. Treatment of patients with acute coronary syndrome: Recommendations for medical emergency teams: Focus on antiplatelet therapies. Updated experts’ standpoint. Cardiol J. 2018;25(3):291–300. doi: 10.5603/CJ.a2018.0042. [DOI] [PubMed] [Google Scholar]
- 14.Konttila KK, Koivula K, Eskola MJ, et al. Poor long-term outcome in acute coronary syndrome in a real-life setting: Ten-year outcome of the TACOS study. Cardiol J. 2021;28(2):302–311. doi: 10.5603/CJ.a2019.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moon J, Kang W, Oh PC, et al. Serum transaminase determined in the emergency room predicts outcomes in patients with acute ST-segment elevation myocardial infarction who undergo primary percutaneous coronary intervention. Int J Cardiol. 2014;177(2):442–447. doi: 10.1016/j.ijcard.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Reinstadler SJ, Reindl M, Feistritzer HJ, et al. Prognostic significance of transaminases after acute ST-elevation myocardial infarction: insights from a cardiac magnetic resonance study. Wien Klin Wochenschr. 2015;127(21–22):843–850. doi: 10.1007/s00508-015-0868-6. [DOI] [PubMed] [Google Scholar]
- 17.Umińska JM, Ratajczak J, Buszko K, et al. Impact of mild therapeutic hypothermia on bioavailability of ticagrelor in patients with acute myocardial infarction after out-of-hospital cardiac arrest. Cardiol J. 2020;27(6):780–788. doi: 10.5603/CJ.a2019.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ratajczak J, Łach P, Umińska JM, et al. Mild therapeutic hypothermia after out-of-hospital cardiac arrest: What does really matter? Cardiol J. 2021;28(2):293–301. doi: 10.5603/CJ.a2019.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]