Abstract
Studies on the trends in the prevalence of rheumatoid arthritis (RA) and osteoarthritis (OA) are limited, particularly during the COVID-19 pandemic. This study aimed to analyze the temporal trend of RA and OA in South Korean adults from 1998 to 2021, including the COVID-19 pandemic period. The Korea National Health and Nutrition Examination Survey (KNHANES) data on adults aged ≥ 19 years were analyzed to investigate the prevalence of RA and OA from 1998 to 2021. The prevalence trends were compared by the years, and βdiff (β difference) was calculated. Odds ratios (ORs) were computed for each disease to examine changes in disease prevalence before and during the pandemic in order to determine the impact of the pandemic on disease prevalence. Among 163,221 Korean adults, the prevalence of RA and OA showed a steady decrease from 2005 (RA: from 1.91% in 2005–2007 to 1.55% in 2016–2019 and OA: from 9.75% in 2005–2007 to 8.27% in 2016–2019), but there was a slight increased after the onset of the COVID-19 pandemic (RA: from 1.23% in 2020 to 1.36% in 2021 and OA: from 8.04% in 2020 to 8.27% in 2021). Vulnerable groups, including participants aged ≥ 60 years (versus 19–60 years, ratio of ORs: 1.222; 95% CI 1.011–1.477), urban residents (ratio of ORs: 1.289; 95% CI 1.007–1.650), and participants with higher education level (ratio of ORs: 1.360; 95% CI 1.119–1.653) showed higher ORs of OA, whereas no particularly vulnerable population was observed for RA. Our findings provide an insight into the long-term trends of RA and OA among adult population and highlight a novel perspective on the impact of COVID-19 on disease prevalence.
Subject terms: Rheumatoid arthritis, Osteoarthritis
Introduction
Previous studies have suggested that the global prevalence rate of rheumatoid arthritis (RA) has remained consistent among decades1. However, in South Korea, several studies have reported a decrease in the prevalence of RA before the COVID-19 pandemic, followed by an increase during the pandemic2. They only provided information on RA prevalence from 2016 to 2020, where the impact of the pandemic to RA has not been reviewed. For this reason, we conducted a study on the prevalence trends of RA and OA between 1998 and 2021. Similar trends have been observed in the prevalence rate of osteoarthritis (OA) globally, with an increasing trend; however, in South Korea, it decreased before the pandemic and increased during the pandemic3,4.
Social distancing policy especially forcing to close the public gym facilities during the COVID-19 pandemic influenced domestic health concern2,5,6. Moreover, changes in physical activity, dietary habits, and mental health due to the COVID-19 restrictions may have influenced these prevalence rates7. However, further analysis and research are needed to determine the direct relationship between RA, OA, and the COVID-19 pandemic. Furthermore, some medications used to treat RA, such as corticosteroids and disease-modifying antirheumatic drugs, may suppress the immune system and increase the risk of infection8, thereby, making the patients more vulnerable to COVID-19 and its complications8. Therefore, it is crucial for patients with RA and COVID-19 to prioritize their health management9.
This study aimed to investigate the long-term trends in the prevalence of RA and OA using a representative large-scale dataset from 1998 to 2021. Additionally, we analyzed the specific social strata that were vulnerable during the COVID-19 period. Furthermore, our research findings may provide valuable information for developing policies for the treatment and prevention of these conditions following the COVID-19 pandemic.
Methods
Patient selection and data collection
This study utilized data from the Korea National Health and Nutrition Examination Survey (KNHANES) conducted between 1998 and 2021 by the Korea Centers for Disease Control and Prevention Agency (KDCA)10,11. The study population included adults aged ≥ 19 years, and the collected data included information on age, sex, residence, body mass index (BMI), education level, income, alcohol consumption, smoking status, and history of RA and OA12. We conducted our research focusing on the adult population, which ranges above 19 years in South Korea. A nationally representative sample of 163,221 participants was used to investigate the prevalence of RA and OA before and during the COVID-19 pandemic. The survey was conducted over 24 years and the number of participants surveyed in each year group was as follows: 51,515 in 1998–2001; 26,996 in 2005–2007; 20,070 in 2008–2010; 17,601 in 2011–2013; 17,129 in 2014–2016; 18,469 in 2017–2019; 5839 in 2020; and 5,602 in 2021.
The research protocol was approved by the Institutional Review Board of Kyung Hee University (KHUH 2022-06-042) and KDCA, and all participants provided written informed consent. Moreover, the KNHANES offers accessible public access to its data, which can be utilized as a valuable resource for diverse epidemiological investigations. This research adhered to the ethical guidelines established by relevant national and institutional review boards for human research and followed the 1975 Helsinki Declaration, as amended in 2008.
Ascertainment of RA and OA
The objective of our study was to investigate the risk factors related to the two most common types of arthritis, RA and OA, over a period of 24 years from 1998 to 2021. To achieve our research objective, we surveyed a large sample of participants and asked them the question: “Have you ever been diagnosed with RA or OA by a doctor?” Based on their answers, we categorized the participants into three groups: RA, OA, and both13. We collected data on various potential risk factors associated with the development of RA and OA, such as age, sex, lifestyle habits, and socioeconomic status. We conducted statistical analyses to examine the associations between these risk factors and the development of RA and OA and to identify any patterns or trends that emerged over 24 years.
Covariates
Covariates included age (19–29, 30–39, 40–49, 50–59, 60–69, 70–79, and ≥ 80 years), sex, region of residence (urban and rural)14–16, BMI group, household income (lowest, second, third, and highest quartile), education level (elementary school or lower, middle school, high school, and college or higher education), alcohol consumption (1–5 days/month, ≥ 6 days/month, and non-drinker), and smoking status (non-smoker, ex-smoker, and smoker). BMI was categorized into underweight (< 18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23–25 kg/m2), and obese (≥ 25.0 kg/m2) according to the Asian-Pacific guidelines17,18.
Statistical analyses
The results of this study were presented using qualitative data expressed as proportions or percentages. Weighted multivariate regression model analyses were conducted to compare the estimates of each related factor before and during the COVID-19 pandemic, with weighted odds ratios (ORs) with 95% confidence intervals (CIs)19. The prevalence of RA and OA was calculated using data from the KNHANES, spanning from 1998 to 2021, stratified by year group. Weighted complex sampling analysis was performed to ensure accurate estimation. Binomial or linear logistic regression models were used to compute the ORs with 95% CIs or β-coefficients with 95% CIs. To ensure robustness of the main findings, a stratification analysis was performed using variables such as sex, educational level, region of residence, and income in all the regression models. Furthermore, the ratio of ORs was calculated to estimate the interaction term of each risk factor and identify groups that were more vulnerable to the patient with RA and OA during the pandemic. Overall, this study aimed to provide a comprehensive analysis of the impact of the COVID-19 pandemic on the prevalence of RA and OA and to identify the factors that contribute to vulnerability to these conditions. The SAS software (version 9.4; SAS Institute, Cary, NC, USA) was used for statistical analyses, with a two-sided test, and a p-value ≤ 0.05 was considered statistically significant19.
Results
We recruited 163,221 participants from 1998 to 2021 with the following distribution of characteristics: age (19–29 years, 18.18% [95% CI 17.82 to 18.53]; 30–39 years, 20.88% [20.47 to 21.29]; 40–49 years, 21.70% [21.35 to 22.06]; 50–59 years, 17.85% [17.56 to 18.14]; 60–69 years, 11.88% [11.64 to 12.12]; 70–79 years, 7.38% [7.19 to 7.58]; and ≥ 80 years, 2.13% [2.03 to 2.23]) and sex (male, 49.39% [49.14 to 49.64] and female, 50.61% [50.36 to 50.86]). These results are presented in Table 1.
Table 1.
General characteristics of Korean adults, in the data obtained from the KNHANES from 1998 to 2021 (n = 163,221).
| Total | 1998–2001 | 2005–2007 | 2008–2010 | 2011–2013 | 2014–2016 | 2017–2019 | 2020 | 2021 | |
|---|---|---|---|---|---|---|---|---|---|
| Overall, n | 163,221 | 51,515 | 26,996 | 20,070 | 17,601 | 17,129 | 18,469 | 5839 | 5602 |
| Age (years), weighted % (95% CI) | |||||||||
| 19–29 | 18.18 (17.82 to 18.53) | 19.90 (19.21 to 20.58) | 21.34 (20.55 to 22.12) | 18.80 (17.72 to 19.87) | 17.59 (16.63 to 18.55) | 16.78 (15.83 to 17.73) | 16.51 (15.57 to 17.45) | 16.19 (14.65 to 17.72) | 15.91 (14.10 to 17.73) |
| 30–39 | 20.88 (20.47 to 21.29) | 25.85 (24.89 to 26.81) | 24.20 (23.19 to 25.20) | 22.23 (21.09 to 23.36) | 20.55 (19.44 to 21.66) | 19.06 (17.91 to 20.21) | 17.75 (16.67 to 18.84) | 16.77 (14.85 to 18.69) | 16.32 (14.61 to 18.04) |
| 40–49 | 21.70 (21.35 to 22.06) | 23.47 (22.65 to 24.28) | 23.22 (22.41 to 24.03) | 22.55 (21.60 to 23.51) | 21.95 (20.92 to 22.99) | 21.13 (20.22 to 22.03) | 20.18 (19.21 to 21.15) | 19.35 (17.61 to 21.09) | 18.99 (17.27 to 20.70) |
| 50–59 | 17.85 (17.56 to 18.14) | 13.87 (13.31 to 14.42) | 14.69 (14.13 to 15.25) | 17.11 (16.35 to 17.87) | 18.85 (18.06 to 19.64) | 20.02 (19.17 to 20.88) | 20.13 (19.35 to 20.91) | 20.03 (18.60 to 21.46) | 19.78 (18.25 to 21.31) |
| 60–69 | 11.88 (11.64 to 12.12) | 11.29 (10.71 to 11.87) | 10.24 (9.77 to 10.70) | 10.45 (9.88 to 11.02) | 10.83 (10.22 to 11.43) | 12.06 (11.38 to 12.73) | 13.62 (12.87 to 14.36) | 15.04 (13.65 to 16.43) | 16.06 (14.75 to 17.38) |
| 70–79 | 7.38 (7.19 to 7.58) | 5.35 (4.98 to 5.72) | 5.85 (5.47 to 6.23) | 6.92 (6.42 to 7.42) | 7.94 (7.36 to 8.52) | 8.27 (7.72 to 8.82) | 8.41 (7.81 to 9.00) | 8.85 (7.71 to 9.98) | 8.93 (7.80 to 10.06) |
| ≥ 80 | 2.13 (2.03 to 2.23) | 0.28 (0.21 to 0.35) | 0.47 (0.37 to 0.57) | 1.95 (1.72 to 2.17) | 2.28 (2.01 to 2.55) | 2.69 (2.41 to 2.96) | 3.40 (3.04 to 3.77) | 3.78 (3.05 to 4.50) | 4.01 (3.28 to 4.74) |
| Sex, weighted % (95% CI) | |||||||||
| Male | 49.39 (49.14 to 49.64) | 47.46 (47.10 to 47.82) | 49.63 (49.16 to 50.10) | 49.55 (48.89 to 50.21) | 49.48 (48.76 to 50.20) | 49.59 (48.87 to 50.31) | 49.80 (49.07 to 50.53) | 49.84 (48.73 to 50.95) | 49.82 (48.52 to 51.12) |
| Female | 50.61 (50.36 to 50.86) | 52.54 (52.18 to 52.90) | 50.37 (49.90 to 50.84) | 50.45 (49.79 to 51.11) | 50.52 (49.80 to 51.24) | 50.41 (49.69 to 51.13) | 50.20 (49.47 to 50.93) | 50.16 (49.05 to 51.27) | 50.18 (48.88 to 51.48) |
| Region of residence, weighted % (95% CI) | |||||||||
| Urban | 82.15 (81.14 to 83.16) | 80.86 (79.98 to 81.74) | 81.29 (79.72 to 82.87) | 80.07 (76.87 to 83.28) | 80.73 (77.41 to 84.05) | 83.26 (80.33 to 86.19) | 84.68 (81.74 to 87.61) | 84.57 (79.45 to 89.68) | 83.80 (78.76 to 88.84) |
| Rural | 17.85 (16.84 to 18.86) | 19.14 (18.26 to 20.02) | 18.71 (17.13 to 20.28) | 19.93 (16.72 to 23.14) | 19.27 (15.95 to 22.59) | 16.74 (13.81 to 19.67) | 15.32 (12.39 to 18.26) | 15.43 (10.32 to 20.55) | 16.20 (11.16 to 21.24) |
| BMI group, weighted % (95% CI) | |||||||||
| Underweight | 3.52 (3.39 to 3.65) | 1.12 (0.92 to 1.31) | 1.44 (1.21 to 1.67) | 4.69 (4.33 to 5.05) | 4.79 (4.37 to 5.20) | 4.31 (3.94 to 4.69) | 3.92 (3.57 to 4.26) | 4.13 (3.45 to 4.81) | 4.17 (3.57 to 4.78) |
| Normal weight and overweight | 49.31 (48.82 to 49.81) | 15.90 (13.93 to 17.87) | 20.53 (18.61 to 22.44) | 63.19 (62.34 to 64.04) | 62.22 (61.30 to 63.14) | 61.47 (60.55 to 62.39) | 60.81 (59.91 to 61.70) | 56.40 (54.78 to 58.03) | 57.52 (55.80 to 59.24) |
| Obesity | 27.05 (26.68 to 27.41) | 7.46 (6.50 to 8.43) | 10.59 (9.53 to 11.64) | 31.49 (30.65 to 32.33) | 32.51 (31.57 to 33.44) | 33.99 (33.04 to 34.94) | 34.78 (33.90 to 35.67) | 38.15 (36.60 to 39.71) | 36.89 (35.11 to 38.68) |
| Unknown | 20.12 (19.52 to 20.72) | 75.52 (72.54 to 78.51) | 67.44 (64.47 to 70.41) | 0.63 (0.46 to 0.80) | 0.48 (0.36 to 0.61) | 0.23 (0.13 to 0.33) | 0.49 (0.36 to 0.63) | 1.31 (0.98 to 1.65) | 1.41 (1.01 to 1.81) |
| Level of education, weighted % (95% CI) | |||||||||
| Elementary school or lower education | 15.10 (14.77 to 15.43) | 20.42 (19.49 to 21.35) | 17.99 (17.16 to 18.82) | 18.32 (17.22 to 19.41) | 15.32 (14.30 to 16.34) | 12.87 (12.00 to 13.74) | 11.37 (10.46 to 12.28) | 8.74 (7.32 to 10.16) | 9.85 (8.31 to 11.40) |
| Middle school | 9.49 (9.27 to 9.70) | 12.26 (11.70 to 12.83) | 10.67 (10.14 to 11.21) | 10.49 (9.90 to 11.08) | 9.56 (8.99 to 10.13) | 8.43 (7.88 to 8.98) | 7.94 (7.37 to 8.51) | 7.16 (6.19 to 8.13) | 7.14 (6.20 to 8.09) |
| High school | 29.97 (29.58 to 30.36) | 37.35 (36.39 to 38.31) | 35.57 (34.67 to 36.48) | 30.24 (29.22 to 31.27) | 29.29 (28.19 to 30.39) | 25.49 (24.48 to 26.50) | 25.86 (24.87 to 26.84) | 26.47 (24.65 to 28.29) | 27.34 (25.50 to 29.18) |
| College or higher education | 41.37 (40.79 to 41.94) | 29.88 (28.63 to 31.13) | 35.73 (34.52 to 36.95) | 40.25 (38.64 to 41.86) | 39.97 (38.40 to 41.54) | 43.74 (42.12 to 45.37) | 49.39 (47.66 to 51.11) | 49.83 (46.59 to 53.08) | 50.16 (47.12 to 53.21) |
| Unknown | 4.08 (3.89 to 4.28) | 0.09 (0.04 to 0.14) | 0.03 (0.00 to 0.05) | 0.70 (0.55 to 0.86) | 5.86 (5.31 to 6.41) | 9.47 (8.68 to 10.26) | 5.45 (4.87 to 6.03) | 7.80 (6.51 to 9.10) | 5.50 (4.53 to 6.46) |
| Household income, weighted % (95% CI) | |||||||||
| Lowest quartile | 16.99 (16.57 to 17.41) | 22.79 (21.52 to 24.05) | 18.02 (17.01 to 19.03) | 16.81 (15.71 to 17.90) | 16.04 (14.88 to 17.21) | 15.76 (14.61 to 16.91) | 15.67 (14.53 to 16.82) | 15.08 (12.88 to 17.29) | 14.11 (12.10 to 16.12) |
| Second quartile | 24.86 (24.41 to 25.31) | 24.49 (23.45 to 25.53) | 25.80 (24.78 to 26.83) | 25.45 (24.22 to 26.69) | 27.01 (25.70 to 28.33) | 23.79 (22.55 to 25.03) | 24.30 (23.10 to 25.50) | 22.10 (19.96 to 24.24) | 22.79 (20.72 to 24.87) |
| Third quartile | 28.55 (28.10 to 29.00) | 25.43 (24.45 to 26.42) | 28.50 (27.54 to 29.47) | 28.76 (27.58 to 29.93) | 28.58 (27.38 to 29.77) | 29.91 (28.55 to 31.27) | 28.52 (27.39 to 29.65) | 29.24 (27.12 to 31.37) | 30.07 (27.91 to 32.22) |
| Highest quartile | 29.60 (28.98 to 30.23) | 27.29 (25.84 to 28.74) | 27.67 (26.28 to 29.07) | 28.99 (27.31 to 30.66) | 28.37 (26.76 to 29.97) | 30.54 (28.68 to 32.39) | 31.50 (29.79 to 33.22) | 33.57 (30.09 to 37.05) | 33.03 (29.29 to 36.77) |
| Smoking status, weighted % (95% CI) | |||||||||
| Smoker | 19.26 (18.90 to 19.63) | 9.23 (8.07 to 10.39) | 11.42 (10.28 to 12.55) | 27.20 (26.40 to 27.99) | 24.02 (23.07 to 24.98) | 21.69 (20.82 to 22.57) | 20.73 (19.88 to 21.59) | 19.30 (17.81 to 20.80) | 18.27 (16.81 to 19.73) |
| Ex-smoker | 16.52 (16.26 to 16.79) | 2.63 (2.24 to 3.02) | 7.42 (6.65 to 8.18) | 19.83 (19.18 to 20.47) | 18.55 (17.86 to 19.23) | 19.83 (19.13 to 20.54) | 22.27 (21.59 to 22.94) | 23.82 (22.66 to 24.98) | 25.02 (23.70 to 26.33) |
| Non-smoker | 45.61 (45.10 to 46.12) | 17.81 (15.63 to 19.98) | 22.25 (20.23 to 24.28) | 52.55 (51.80 to 53.31) | 53.76 (52.86 to 54.65) | 56.67 (55.78 to 57.57) | 56.98 (56.13 to 57.84) | 56.87 (55.43 to 58.32) | 56.71 (55.05 to 58.37) |
| Unknown | 18.60 (17.86 to 19.33) | 70.34 (66.74 to 73.93) | 58.91 (55.24 to 62.58) | 0.42 (0.31 to 0.54) | 3.67 (3.30 to 4.05) | 1.81 (1.50 to 2.11) | 0.01 (0.00 to 0.03) | 0.00 (0.00 to 0.00) | 0.00 (0.00 to 0.00) |
| Alcohol consumption, weighted % (95% CI) | |||||||||
| Non-drinker | 12.08 (11.69 to 12.47) | 14.91 (13.05 to 16.77) | 13.99 (12.45 to 15.52) | 11.76 (11.17 to 12.35) | 12.18 (11.45 to 12.92) | 12.21 (11.50 to 12.92) | 9.75 (9.16 to 10.34) | 9.82 (8.67 to 10.97) | 9.70 (8.56 to 10.83) |
| 1–5 days/month | 51.21 (50.75 to 51.68) | 11.11 (9.68 to 12.54) | 18.66 (16.83 to 20.49) | 63.98 (63.00 to 64.95) | 62.24 (61.23 to 63.25) | 63.42 (62.42 to 64.42) | 67.00 (66.12 to 67.88) | 68.13 (66.62 to 69.65) | 70.46 (68.95 to 71.96) |
| 6 ~ 30 days/month | 18.11 (17.81 to 18.42) | 3.64 (3.13 to 4.15) | 8.45 (7.61 to 9.28) | 23.84 (23.03 to 24.65) | 21.90 (21.09 to 22.72) | 22.57 (21.75 to 23.38) | 23.23 (22.47 to 24.00) | 22.05 (20.72 to 23.38) | 19.85 (18.55 to 21.14) |
| Unknown | 18.60 (17.86 to 19.33) | 70.34 (66.74 to 73.93) | 58.91 (55.24 to 62.58) | 0.42 (0.31 to 0.54) | 3.67 (3.30 to 4.05) | 1.81 (1.50 to 2.11) | 0.01 (0.00 to 0.03) | 0.00 (0.00 to 0.00) | 0.00 (0.00 to 0.00) |
BMI body mass index, CI confidence interval, KNHANES Korea National Health and Nutrition Examination Survey.
*According to the Asian-Pacific guidelines, the BMI is divided into four groups: underweight (< 18.5 kg/m2), normal (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), and obese (≥ 25 kg/m2).
Table 2 illustrate the prevalence of RA, OA between pre-pandemic and during the pandemic. The prevalence of RA and OA showed a U-curve between pre-pandemic and during the pandemic (RA: from 1.46% [95% CI 1.38 to 1.54] in 2005–2019; 1.23% [0.92 to 1.54] in 2020; and 1.36% [1.02 to 1.69] in 2021, OA: from 7.68% [7.49 to 7.88] in 2005–2019; 8.04% [7.18 to 8.89] in 2020; and 8.27% [7.35 to 9.19] in 2021) (Table S1).
Table 2.
National trends of the prevalence of RA and OA before and during the COVID-19 pandemic, weighted % (95% CI), in the data obtained from the KNHANES.
| Year | Pre-pandemic (2005–2019) | During the pandemic | |
|---|---|---|---|
| 2020 | 2021 | ||
| RA | |||
| Overall | 1.46 (1.38 to 1.54) | 1.23 (0.92 to 1.54) | 1.36 (1.02 to 1.69) |
| Age group | |||
| Age (19–60 years) | 0.95 (0.87 to 1.02) | 0.56 (0.27 to 0.85) | 0.73 (0.40 to 1.06) |
| Age (≥ 60 years) | 3.40 (3.17 to 3.62) | 2.98 (2.20 to 3.77) | 2.89 (2.10 to 3.68) |
| Sex | |||
| Male | 0.74 (0.65 to 0.83) | 0.53 (0.28 to 0.78) | 0.82 (0.46 to 1.19) |
| Female | 2.16 (2.04 to 2.28) | 1.92 (1.34 to 2.51) | 1.89 (1.41 to 2.36) |
| Region of residence | |||
| Urban | 1.37 (1.29 to 1.46) | 1.21 (0.86 to 1.56) | 1.22 (0.86 to 1.59) |
| Rural | 1.85 (1.66 to 2.04) | 1.32 (0.71 to 1.93) | 2.05 (1.16 to 2.94) |
| BMI group | |||
| Underweight | 1.56 (1.11 to 2.01) | 0.42 (0.00 to 1.02) | 2.74 (0.47 to 5.01) |
| Normal weight and overweight | 1.55 (1.44 to 1.66) | 1.27 (0.84 to 1.70) | 1.38 (0.95 to 1.82) |
| Obesity | 1.61 (1.45 to 1.76) | 1.17 (0.75 to 1.59) | 1.11 (0.69 to 1.53) |
| Education | |||
| High school or lower education | 2.15 (2.03 to 2.27) | 2.14 (1.57 to 2.71) | 2.14 (1.61 to 2.67) |
| College or higher education | 0.65 (0.56 to 0.74) | 0.57 (0.26 to 0.87) | 0.81 (0.38 to 1.25) |
| Income | |||
| Income (lowest-second quartile) | 1.95 (1.83 to 2.08) | 1.94 (1.34 to 2.54) | 1.82 (1.26 to 2.38) |
| Income (third-highest quartile) | 1.10 (1.01 to 1.19) | 0.81 (0.50 to 1.11) | 1.09 (0.71 to 1.46) |
| OA | |||
| Overall | 7.68 (7.49 to 7.88) | 8.04 (7.18 to 8.89) | 8.27 (7.35 to 9.19) |
| Age group | |||
| Age (19–60 years) | 3.29 (3.15 to 3.43) | 2.35 (1.80 to 2.90) | 2.79 (2.19 to 3.39) |
| Age (≥ 60 years) | 24.36 (23.80 to 24.92) | 22.91 (20.86 to 24.97) | 21.69 (19.53 to 23.85) |
| Sex | |||
| Male | 3.27 (3.10 to 3.44) | 3.63 (2.86 to 4.40) | 4.07 (3.22 to 4.92) |
| Female | 11.99 (11.68 to 12.30) | 12.42 (10.99 to 13.85) | 12.44 (11.01 to 13.86) |
| Region of residence | |||
| Urban | 6.93 (6.73 to 7.14) | 7.81 (6.89 to 8.74) | 7.58 (6.65 to 8.52) |
| Rural | 11.09 (10.49 to 11.70) | 9.26 (6.58 to 11.94) | 11.81 (9.18 to 14.44) |
| BMI group | |||
| Underweight | 2.84 (2.31 to 3.37) | 3.07 (0.69 to 5.45) | 2.96 (1.10 to 4.82) |
| Normal weight and overweight | 6.86 (6.61 to 7.12) | 7.33 (6.32 to 8.34) | 7.23 (6.22 to 8.23) |
| Obesity | 11.28 (10.87 to 11.70) | 9.34 (7.94 to 10.74) | 10.14 (8.64 to 11.63) |
| Education | |||
| High school or lower education | 12.56 (12.26 to 12.86) | 15.87 (14.32 to 17.41) | 14.75 (13.08 to 16.42) |
| College or higher education | 1.77 (1.63 to 1.91) | 2.42 (1.76 to 3.08) | 3.36 (2.65 to 4.06) |
| Income | |||
| Income (lowest-second quartile) | 11.86 (11.52 to 12.20) | 13.31 (11.74 to 14.88) | 14.23 (12.41 to 16.05) |
| Income (third-highest quartile) | 4.64 (4.45 to 4.82) | 4.92 (4.12 to 5.71) | 4.78 (4.00 to 5.56) |
CI confidence interval, KNHANES Korea National Health and Nutrition Examination Survey, OA osteoarthritis, OR odds ratio, RA rheumatoid arthritis.
*Prevalence of RA, OA were available from 2005.
Table 3 and Fig. 1 show the national trends in the prevalence of overall RA and OA, as well as the prevalence of RA and OA separately, along with the β-coefficients of the ORs before and during the COVID-19 pandemic. A statistically significant decrease in the weighted prevalence of RA was observed pre-pandemic (2005–2007, 1.91% [95% CI 1.72 to 2.10]; 2008–2010, 1.79% [1.59 to 1.99]; 2011–2013, 1.40% [1.23 to 1.58]; 2014–2016, 1.49% [1.31 to 1.67]; 2017–2019, 1.55% [1.36 to 1.75]; and 2020, 1.23% [0.92 to 1.54]), whereas a slight increase was observed during the pandemic (2020, 1.23% [0.92 to 1.54] and 2021, 1.36% [1.02 to 1.69]). Similarly, decrease in the weighted prevalence of OA was observed before the pandemic (2005–2007, 9.75% [9.29 to 10.20]; 2008–2010, 8.60% [8.12 to 9.08]; 2011–2013, 7.97% [7.51 to 8.44]; 2014–2016, 8.06% [7.57 to 8.56]; 2017–2019, 8.42% [7.91 to 8.93]. A slight increase was observed during the pandemic (2020, 8.04% [7.18 to 8.89] and 2021, 8.27% [7.35 to 9.19]). Similar patterns and trends were observed for the prevalence of OA and RA stratified by age, sex, region of residence, education level, and household income (Table S2). While investigating the weighted OR in 2021 with respect to that of 2020 (reference), there was a surge regarding RA among underweight group (OR, 6.62 [1.28 to 34.36]).
Table 3.
National trend of the RA and OA prevalence and β-coefficients of the odds ratios before and during the COVID-19 pandemic, weighted % (95% CI), in the data obtained from the KNHANES.
| Year | Pre-pandemic | During the pandemic | Trends in the pre-pandemic era, β (95% CI) | Trends in the pandemic era, β (95% CI) | βdiff between 2005–2019 and 2019–2021 (95% CI) | Weighted odds of before and during the pandemic, OR (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005–2007 | 2008–2010 | 2011–2013 | 2014–2016 | 2017–2019 | 2020 | 2021 | 2020 versus 2017–2019 (reference) | 2021 versus 2020 (reference) | ||||
| RA | ||||||||||||
| Overall | 1.91 (1.72 to 2.10) | 1.79 (1.59 to 1.99) | 1.40 (1.23 to 1.58) | 1.49 (1.31 to 1.67) | 1.55 (1.36 to 1.75) | 1.23 (0.92 to 1.54) | 1.36 (1.02 to 1.69) | − 0.097 (− 0.158 to − 0.036) | − 0.098 (− 0.293 to 0.097) | 0.000 (− 0.205 to 0.204) | 0.79 (0.59 to 1.05) | 1.11 (0.77 to 1.59) |
| Age group | ||||||||||||
| Age (19–60 years) | 1.43 (1.24 to 1.62) | 1.19 (0.99 to 1.39) | 0.91 (0.73 to 1.09) | 0.95 (0.76 to 1.15) | 0.84 (0.65 to 1.02) | 0.56 (0.27 to 0.85) | 0.73 (0.40 to 1.06) | − 0.141 (− 0.201 to − 0.082) | − 0.054 (− 0.242 to 0.134) | 0.087 (− 0.110 to 0.285) | 0.66 (0.38 to 1.16) | 1.31 (0.66 to 2.61) |
| Age (≥ 60 years) | 4.35 (3.72 to 4.99) | 4.28 (3.71 to 4.85) | 3.24 (2.75 to 3.73) | 3.29 (2.81 to 3.77) | 3.66 (3.12 to 4.20) | 2.98 (2.20 to 3.77) | 2.89 (2.10 to 3.68) | − 0.207 (− 0.389 to − 0.025) | − 0.377 (− 0.856 to 0.102) | − 0.170 (− 0.683 to 0.342) | 0.81 (0.59 to 1.11) | 0.97 (0.66 to 1.43) |
| Sex | ||||||||||||
| Male | 1.10 (0.90 to 1.31) | 0.89 (0.66 to 1.12) | 0.60 (0.41 to 0.80) | 0.78 (0.57 to 0.99) | 0.74 (0.52 to 0.96) | 0.53 (0.28 to 0.78) | 0.82 (0.46 to 1.19) | − 0.079 (− 0.147 to − 0.011) | 0.041 (− 0.173 to 0.255) | 0.120 (− 0.105 to 0.345) | 0.71 (0.41 to 1.24) | 1.56 (0.81 to 3.00) |
| Female | 2.71 (2.41 to 3.01) | 2.67 (2.35 to 2.99) | 2.19 (1.88 to 2.49) | 2.19 (1.89 to 2.48) | 2.36 (2.05 to 2.66) | 1.92 (1.34 to 2.51) | 1.89 (1.41 to 2.36) | − 0.114 (− 0.210 to − 0.019) | − 0.235 (− 0.513 to 0.042) | − 0.121 (− 0.415 to 0.173) | 0.81 (0.58 to 1.14) | 0.98 (0.66 to 1.46) |
| Region of residence | ||||||||||||
| Urban | 1.74 (1.53 to 1.94) | 1.59 (1.38 to 1.81) | 1.36 (1.17 to 1.55) | 1.44 (1.24 to 1.63) | 1.52 (1.30 to 1.73) | 1.21 (0.86 to 1.56) | 1.22 (0.86 to 1.59) | − 0.056 (− 0.123 to 0.011) | − 0.145 (− 0.357 to 0.067) | − 0.089 (− 0.312 to 0.133) | 0.80 (0.57 to 1.11) | 1.01 (0.66 to 1.55) |
| Rural | 2.68 (2.17 to 3.19) | 2.56 (2.08 to 3.05) | 1.59 (1.14 to 2.03) | 1.75 (1.31 to 2.20) | 1.78 (1.31 to 2.24) | 1.32 (0.71 to 1.93) | 2.05 (1.16 to 2.94) | − 0.265 (− 0.419 to − 0.111) | 0.145 (− 0.349 to 0.638) | 0.409 (− 0.108 to 0.927) | 0.74 (0.43 to 1.27) | 1.56 (0.82 to 2.96) |
| BMI group | ||||||||||||
| Underweight | 2.04 (0.54 to 3.54) | 1.21 (0.49 to 1.94) | 1.22 (0.29 to 2.15) | 2.30 (1.08 to 3.51) | 1.60 (0.61 to 2.58) | 0.42 (0.00 to 1.02) | 2.74 (0.47 to 5.01) | 0.123 (− 0.224 to 0.471) | 0.598 (− 0.633 to 1.828) | 0.474 (− 0.804 to 1.753) | 0.26 (0.06 to 1.23) | 6.62 (1.28 to 34.36) |
| Normal weight and overweight | 2.16 (1.73 to 2.59) | 1.79 (1.54 to 2.04) | 1.48 (1.25 to 1.71) | 1.41 (1.20 to 1.62) | 1.56 (1.30 to 1.82) | 1.27 (0.84 to 1.70) | 1.38 (0.95 to 1.82) | − 0.116 (− 0.210 to − 0.021) | − 0.090 (− 0.341 to 0.162) | 0.026 (− 0.243 to 0.295) | 0.81 (0.56 to 1.18) | 1.09 (0.68 to 1.73) |
| Obesity | 3.24 (2.46 to 4.01) | 1.85 (1.49 to 2.21) | 1.31 (1.02 to 1.61) | 1.54 (1.19 to 1.89) | 1.49 (1.19 to 1.80) | 1.17 (0.75 to 1.59) | 1.11 (0.69 to 1.53) | − 0.229 (− 0.364 to − 0.094) | − 0.189 (− 0.450 to 0.073) | 0.041 (− 0.254 to 0.335) | 0.78 (0.51 to 1.20) | 0.95 (0.55 to 1.63) |
| Education | ||||||||||||
| High school or lower education | 2.62 (2.33 to 2.90) | 2.50 (2.21 to 2.79) | 2.15 (1.87 to 2.43) | 2.39 (2.07 to 2.71) | 2.65 (2.29 to 3.01) | 2.14 (1.57 to 2.71) | 2.14 (1.61 to 2.67) | − 0.009 (− 0.110 to 0.092) | − 0.256 (− 0.580 to 0.067) | − 0.247 (− 0.586 to 0.092) | 0.80 (0.59 to 1.10) | 1.00 (0.68 to 1.46) |
| College or higher education | 0.65 (0.48 to 0.82) | 0.77 (0.53 to 1.02) | 0.58 (0.36 to 0.80) | 0.78 (0.56 to 1.00) | 0.70 (0.51 to 0.89) | 0.57 (0.26 to 0.87) | 0.81 (0.38 to 1.25) | 0.010 (− 0.053 to 0.072) | 0.060 (− 0.176 to 0.297) | 0.051 (− 0.194 to 0.295) | 0.82 (0.45 to 1.48) | 1.44 (0.67 to 3.07) |
| Income | ||||||||||||
| Income (lowest-second quartile) | 2.71 (2.39 to 3.02) | 2.27 (1.95 to 2.58) | 1.86 (1.56 to 2.17) | 2.01 (1.68 to 2.34) | 2.19 (1.87 to 2.51) | 1.94 (1.34 to 2.54) | 1.82 (1.26 to 2.38) | − 0.125 (− 0.226 to − 0.024) | − 0.189 (− 0.510 to 0.133) | − 0.064 (− 0.401 to 0.273) | 0.88 (0.62 to 1.25) | 0.94 (0.60 to 1.46) |
| Income (third-highest quartile) | 1.29 (1.09 to 1.49) | 1.44 (1.19 to 1.68) | 1.06 (0.84 to 1.27) | 1.15 (0.94 to 1.36) | 1.13 (0.90 to 1.36) | 0.81 (0.50 to 1.11) | 1.09 (0.71 to 1.46) | − 0.060 (− 0.130 to 0.009) | − 0.017 (− 0.237 to 0.203) | 0.043 (− 0.187 to 0.274) | 0.71 (0.46 to 1.09) | 1.35 (0.81 to 2.27) |
| OA | ||||||||||||
| Overall | 9.75 (9.29 to 10.20) | 8.60 (8.12 to 9.08) | 7.97 (7.51 to 8.44) | 8.06 (7.57 to 8.56) | 8.42 (7.91 to 8.93) | 8.04 (7.18 to 8.89) | 8.27 (7.35 to 9.19) | − 0.301 (− 0.457 to − 0.146) | − 0.075 (− 0.610 to 0.460) | 0.227 (− 0.331 to 0.784) | 0.95 (0.83 to 1.10) | 1.03 (0.87 to 1.23) |
| Age group | ||||||||||||
| Age (19–60 years) | 4.83 (4.48 to 5.17) | 4.21 (3.84 to 4.58) | 3.28 (2.92 to 3.64) | 3.27 (2.91 to 3.63) | 2.89 (2.56 to 3.23) | 2.35 (1.80 to 2.90) | 2.79 (2.19 to 3.39) | − 0.478 (− 0.586 to − 0.369) | − 0.056 (− 0.391 to 0.279) | 0.422 (0.069 to 0.774) | 0.81 (0.62 to 1.05) | 1.19 (0.86 to 1.65) |
| Age (≥ 60 years) | 34.53 (32.97 to 36.08) | 26.96 (25.65 to 28.27) | 25.57 (24.25 to 26.90) | 24.11 (22.83 to 25.38) | 24.63 (23.40 to 25.86) | 22.91 (20.86 to 24.97) | 21.69 (19.53 to 23.85) | − 2.011 (− 2.442 to − 1.580) | − 1.462 (− 2.728 to − 0.196) | 0.549 (− 0.789 to 1.886) | 0.91 (0.79 to 1.04) | 0.93 (0.78 to 1.11) |
| Sex | ||||||||||||
| Male | 4.79 (4.39 to 5.18) | 3.75 (3.32 to 4.18) | 3.08 (2.66 to 3.49) | 3.36 (2.91 to 3.81) | 3.28 (2.89 to 3.67) | 3.63 (2.86 to 4.40) | 4.07 (3.22 to 4.92) | − 0.327 (− 0.455 to − 0.200) | 0.396 (− 0.067 to 0.859) | 0.723 (0.243 to 1.203) | 1.11 (0.86 to 1.43) | 1.13 (0.83 to 1.53) |
| Female | 14.63 (13.92 to 15.35) | 13.36 (12.59 to 14.13) | 12.77 (11.99 to 13.54) | 12.69 (11.93 to 13.46) | 13.52 (12.68 to 14.36) | 12.42 (10.99 to 13.85) | 12.44 (11.01 to 13.86) | − 0.268 (− 0.517 to − 0.018) | − 0.541 (− 1.391 to 0.310) | − 0.273 (− 1.159 to 0.613) | 0.91 (0.77 to 1.06) | 1.00 (0.82 to 1.22) |
| Region of residence | ||||||||||||
| Urban | 8.26 (7.82 to 8.71) | 7.74 (7.25 to 8.24) | 7.21 (6.72 to 7.71) | 7.52 (7.00 to 8.04) | 7.75 (7.21 to 8.29) | 7.81 (6.89 to 8.74) | 7.58 (6.65 to 8.52) | − 0.112 (− 0.271 to 0.048) | − 0.083 (− 0.625 to 0.458) | 0.028 (− 0.536 to 0.593) | 1.01 (0.87 to 1.18) | 0.97 (0.80 to 1.17) |
| Rural | 16.20 (14.54 to 17.85) | 12.05 (10.55 to 13.55) | 11.15 (9.76 to 12.54) | 10.75 (9.21 to 12.29) | 12.14 (10.38 to 13.89) | 9.26 (6.58 to 11.94) | 11.81 (9.18 to 14.44) | − 0.933 (− 1.447 to − 0.420) | − 0.124 (− 1.742 to 1.495) | 0.810 (− 0.888 to 2.508) | 0.74 (0.51 to 1.06) | 1.31 (0.86 to 2.00) |
| BMI group | ||||||||||||
| Underweight | 6.21 (3.78 to 8.64) | 2.52 (1.54 to 3.50) | 2.04 (1.09 to 2.98) | 2.97 (1.70 to 4.24) | 3.31 (2.05 to 4.58) | 3.07 (0.69 to 5.45) | 2.96 (1.10 to 4.82) | − 0.112 (− 0.578 to 0.354) | − 0.176 (− 1.396 to 1.045) | − 0.064 (− 1.370 to 1.243) | 0.92 (0.38 to 2.23) | 0.96 (0.33 to 2.82) |
| Normal weight and overweight | 8.43 (7.51 to 9.36) | 7.03 (6.52 to 7.55) | 6.87 (6.33 to 7.42) | 6.68 (6.15 to 7.21) | 7.35 (6.78 to 7.92) | 7.33 (6.32 to 8.34) | 7.23 (6.22 to 8.23) | − 0.089 (− 0.298 to 0.121) | − 0.062 (− 0.644 to 0.519) | 0.026 (− 0.592 to 0.644) | 1.00 (0.83 to 1.19) | 0.99 (0.79 to 1.23) |
| Obesity | 14.39 (12.85 to 15.92) | 12.71 (11.77 to 13.65) | 11.02 (10.14 to 11.90) | 11.26 (10.35 to 12.17) | 10.86 (10.03 to 11.68) | 9.34 (7.94 to 10.74) | 10.14 (8.64 to 11.63) | − 0.679 (− 1.012 to − 0.346) | − 0.342 (− 1.226 to 0.542) | 0.337 (− 0.608 to 1.282) | 0.85 (0.70 to 1.02) | 1.10 (0.86 to 1.39) |
| Education | ||||||||||||
| High school or lower education | 14.10 (13.45 to 14.74) | 13.39 (12.68 to 14.10) | 13.51 (12.74 to 14.27) | 15.09 (14.21 to 15.96) | 16.10 (15.22 to 16.98) | 15.87 (14.32 to 17.41) | 14.75 (13.08 to 16.42) | 0.548 (0.304 to 0.792) | − 0.674 (− 1.619 to 0.272) | − 1.222 (− 2.198 to − 0.245) | 0.98 (0.86 to 1.13) | 0.92 (0.77 to 1.10) |
| College or higher education | 1.93 (1.63 to 2.23) | 1.70 (1.38 to 2.02) | 1.57 (1.23 to 1.91) | 2.01 (1.68 to 2.35) | 2.20 (1.87 to 2.53) | 2.42 (1.76 to 3.08) | 3.36 (2.65 to 4.06) | 0.103 (0.001 to 0.205) | 0.579 (0.186 to 0.972) | 0.476 (0.070 to 0.882) | 1.10 (0.80 to 1.52) | 1.40 (0.98 to 2.00) |
| Income | ||||||||||||
| Income (lowest-second quartile) | 15.07 (14.28 to 15.85) | 12.86 (12.05 to 13.67) | 12.15 (11.35 to 12.95) | 13.02 (12.05 to 13.99) | 13.71 (12.80 to 14.62) | 13.31 (11.74 to 14.88) | 14.23 (12.41 to 16.05) | − 0.239 (− 0.511 to 0.032) | 0.254 (− 0.754 to 1.262) | 0.493 (− 0.550 to 1.537) | 0.97 (0.82 to 1.14) | 1.08 (0.88 to 1.34) |
| Income (third-highest quartile) | 5.60 (5.20 to 5.99) | 5.48 (5.02 to 5.94) | 4.81 (4.34 to 5.29) | 4.82 (4.37 to 5.28) | 4.90 (4.44 to 5.35) | 4.92 (4.12 to 5.71) | 4.78 (4.00 to 5.56) | − 0.199 (− 0.337 to −0.060) | − 0.059 (− 0.510 to 0.392) | 0.140 (− 0.332 to 0.611) | 1.00 (0.83 to 1.22) | 0.97 (0.77 to 1.23) |
The numbers in bold indicate a significant difference (p < 0.05).
BMI body mass index, CI confidence interval, KNHANES Korea National Health and Nutrition Examination Survey, OA osteoarthritis, OR odds ratio, RA rheumatoid arthritis.
Figure 1.
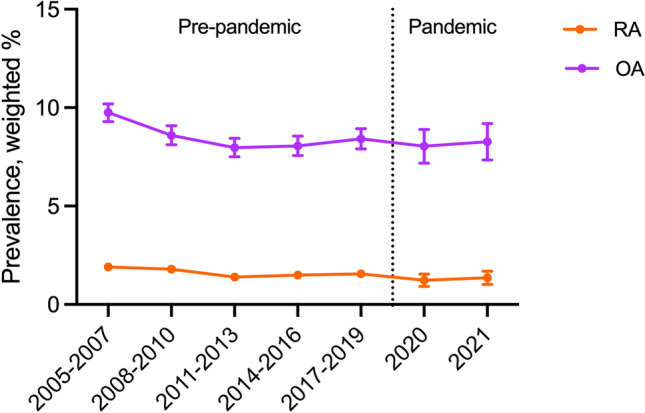
Seventeen-year trends in the prevalence of rheumatoid arthritis and osteoarthritis in South Korea, 2005–2021. OA osteoarthritis, RA rheumatoid arthritis.
Table 4 shows the pandemic-related effects on vulnerable groups of patients with RA and OA. A statistically significant difference was observed among vulnerable individuals with OA as follows: participants ≥ 60 years old (ratio of ORs 1.222 [95% CI 1.011 to 1.477]), urban residents (ratio of ORs 1.289 [1.007 to 1.650]), and participants with a high level of education (ratio of ORs 1.360 [1.119 to 1.653]). In contrast, no significant difference in pandemic-related effects was observed among vulnerable individuals with RA (Table S3).
Table 4.
Difference between pre- and during the COVID-19 pandemic by the ratio of ORs on OA and RA, weighted % (95% CI), in the data obtained from the KNHANES.
| Variables | Overall (2005–2021) | Pre-COVID-19 pandemic (2005–2019) | COVID-19 pandemic (2020, 2021) | Ratio of OR (95% CI) | |
|---|---|---|---|---|---|
| Weighted OR (95%CI) | Weighted OR (95%CI) | Weighted OR (95%CI) | |||
| RA | |||||
| Age | 19–59 | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| ≥ 60 | 3.596 (3.248 to 3.980) | 3.553 (3.197 to 3.948) | 4.665 (3.145 to 6.919) | 1.313 (0.873 to 1.975) | |
| Sex | Female | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| Male | 0.335 (0.298 to 0.377) | 0.334 (0.295 to 0.379) | 0.348 (0.244 to 0.497) | 1.042 (0.715 to 1.519) | |
| Region | Urban | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| Rural | 1.433 (1.272 to 1.615) | 1.424 (1.257 to 1.614) | 1.502 (1.015 to 2.223) | 1.055 (0.699 to 1.592) | |
| Education | High school or less | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| College or more | 0.245 (0.214 to 0.280) | 0.241 (0.209 to 0.278) | 0.286 (0.192 to 0.427) | 1.187 (0.777 to 1.814) | |
| Income | High | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| Low | 1.885 (1.710 to 2.079) | 1.864 (1.683 to 2.066) | 2.004 (1.460 to 2.752) | 1.075 (0.770 to 1.500) | |
| OA | |||||
| Age | 19–59 | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| ≥ 60 | 8.852 (8.467 to 9.254) | 8.839 (8.442 to 9.254) | 10.799 (8.986 to 12.980) | 1.222 (1.011 to 1.477) | |
| Sex | Female | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| Male | 0.256 (0.244 to 0.268) | 0.253 (0.241 to 0.265) | 0.286 (0.243 to 0.337) | 1.130 (0.953 to 1.340) | |
| Region | Rural | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| Urban | 0.535 (0.501 to 0.571) | 0.523 (0.489 to 0.560) | 0.674 (0.531 to 0.854) | 1.289 (1.007 to 1.650) | |
| Education | High school or less | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| College or more | 0.117 (0.110 to 0.125) | 0.111 (0.103 to 0.119) | 0.151 (0.126 to 0.181) | 1.360 (1.119 to 1.653) | |
| Income | High | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) | 1.000 (reference) |
| Low | 2.864 (2.742 to 2.992) | 2.839 (2.712 to 2.971) | 3.129 (2.689 to 3.641) | 1.102 (0.941 to 1.291) | |
The numbers in bold indicate a significant difference (p < 0.05).
KNHANES Korea National Health and Nutrition Examination Survey, CI confidence interval, OA osteoarthritis, OR odds ratio, RA rheumatoid arthritis.
Discussion
Key results
The present study examined trends in the prevalence of RA and OA over a 24-year period from 1998 to 2021 and evaluated the differences in prevalence before and during the COVID-19 pandemic (n = 163,221). The prevalence of RA and OA consistently declined before the onset of the pandemic, but there was a slight increased during the pandemic. However slight increasing prevalence during pandemic was not statistically significant. Notably, patients with OA had a significantly high prevalence among vulnerable groups, including individuals aged ≥ 60 years, urban residents, and those with a high education level. Therefore, these findings suggest policy researchers should develop personalized policy proposals to address the needs of these groups during the pandemic.
Global epidemiology and mechanism
Previous studies have reported a global increase in the prevalence of RA and OA, before the COVID-19 pandemic20. However, in South Korea, the prevalence of both conditions has consistently declined, contrary to global trends21. Similar trends of decline in the prevalence of RA have been observed in Japan and Sweden as well22. A Japanese study found a correlation between a decrease in RA prevalence and changes in lifestyle factors, such as dietary habits and smoking, while a Swedish study has linked this decrease to improvements in medical accessibility for patients with RA16,23. Although we cannot accurately identify the specific reasons for the variation in RA prevalence across countries, we believe that factors, such as genetic, cultural disparities, and health level may have a significant impact24. In addition, increased BMI and muscle weakness are closely related to OA and RA, as these diseases are associated with factors that contribute to joint strain25,26.
During the COVID-19 pandemic, the social distancing policies and the closure of sports facilities significantly diminished the public health standards, which could generally explain the observed increase in the prevalence of RA and OA27,28.
RA is a complex disease with multiple factors contributing to its development, with genetics potentially being a significant factor29. Other studies have reported that numerous variables can affect the prevalence of RA30. Therefore, further research is warranted to investigate this matter thoroughly. An increase in the prevalence of OA and RA was the most prominent in the highly educated older adult population living in urban areas31. These individuals who were retired and had reduced health standards due to COVID-19 were most affected32. According to previous research, the domestic standard of physical activity among South Korean adult population exhibited a declining trend until 2017, followed by an upturn until 201933. In 2020, confronting the pandemic, there was a significant decline in physical activity. This pattern closely aligns with the prevalence trends in RA and OA, which could substantiate our hypothesis.
This finding suggests that OA may occur when physical activity falls below a certain threshold, which warrants further investigation. It is crucial to recognize this issue at a national level and implement policies to encourage exercise among the older adults, prevent the occurrence of OA, and provide the appropriate treatment for those with the disease.
Strengths and limitations
The present study is significant in utilizing population-based nationwide representative data to compare the trends and prevalence of RA and OA, both before and during the COVID-19 pandemic34. The use of national data is particularly noteworthy, as individual data collection during a pandemic could have been challenging. Furthermore, this study’s utilization of survey data collected from 1998 to 2021, spanning a period of 24 years, adds academic value to the research findings due to its long-term nature. However, this study has several limitations. First, data were collected only from Koreans, thus limiting generalizability of the results to other ethnic groups or countries. Further research with multiple ethnicities and different countries is necessary to examine the global impact of the COVID-19 pandemic35. Second, data on patients with separate covariate of RA and OA were only available from 2005–2021and information prior to 2005 was not available. Third, some variables in the study, such as height and weight, were self-reported, which may have introduced bias. To address this concern, the KDCA should include a question in the survey about when participants' heights and weights were last measured36. In addition, the diagnosis of RA and OA was self-reported, potentially resulting in a recall bias. Lastly, we substituted physical activity data from the previous study, since we were unable to conduct our own analysis of domestic physical activity levels.
Conclusion
Our study identified long-term trends in the prevalence of RA and OA spanning 24-years from 1998 to 2021, especially focusing on the COVID-19 pandemic. The results showed a consistent decline in the prevalence of both RA and OA until 2016 followed by an oscillation until 2021, where significant drop occurred in 2019. Notably, OA exhibited a higher prevalence among vulnerable groups, such as individuals over 60 years of age, urban residents, and those with a high education level. When investigating the RA prevalence trend, there was no specific vulnerable population. This outcome will help government policy researchers devise personalized healthcare policies targeting the vulnerable groups. While our study did not find any evidence of a relationship between the COVID-19 pandemic and the prevalence of RA, additional follow-up studies is needed to further explore this topic.
Supplementary Information
Funding
This research was supported by grants from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HV22C0233 and HE23C002800) and from the Ministry of Food and Drug Safety (grant number: 21153MFDS601) in 2023. The funders played no role in the study design, data collection, analysis, interpretation, or writing of the manuscript.
Author contributions
D.K.Y. had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version before submission. Study concept and design: J.P. and D.K.Y.; Acquisition, analysis, or interpretation of data: J.P. and D.K.Y.; Drafting of the manuscript: J.P. and D.K.Y.; Critical revision of the manuscript for important intellectual content: all authors; Statistical analysis: J.P. and D.K.Y.; Study supervision: J.P., M.C.Y., and D.K.Y. D.K.Y. supervised the study and is guarantor for this study. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Data availability
Data are available on reasonable request. Study protocol, statistical code: available from DKY (email: yonkkang@gmail.com). Data set: available from the Korea Disease Control and Prevention Agency (KDCA) through a data use agreement.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Myung Chul Yoo, Email: famousir@naver.com.
Dong Keon Yon, Email: yonkkang@gmail.com.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-46279-6.
References
- 1.Cross M, et al. The global burden of rheumatoid arthritis: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014;73:1316–1322. doi: 10.1136/annrheumdis-2013-204627. [DOI] [PubMed] [Google Scholar]
- 2.Ahn SM, et al. Incidence of rheumatic diseases during the COVID-19 pandemic in South Korea. Korean J. Intern. Med. 2023;38:248–253. doi: 10.3904/kjim.2022.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamood R, et al. Prevalence and incidence of osteoarthritis: A population-based retrospective cohort study. J. Clin. Med. 2021;10:4282. doi: 10.3390/jcm10184282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kang Y, Ahmad S. The emerging epidemics in recent: Mpox. Life Cycle. 2023;3:e3. doi: 10.54724/lc.2023.e3. [DOI] [Google Scholar]
- 5.Mistry SK, et al. A tale of osteoarthritis among older adults during the COVID-19 pandemic in Bangladesh: A repeated cross-sectional study. PLoS ONE. 2022;17:e0274838. doi: 10.1371/journal.pone.0274838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cleaton N, et al. COVID-19 prevalence and the impact on quality of life from stringent social distancing in a single large UK rheumatology centre. Ann. Rheum. Dis. 2021;80:e93. doi: 10.1136/annrheumdis-2020-218236. [DOI] [PubMed] [Google Scholar]
- 7.Schäfer C, Keyber G. Lifestyle factors and their influence on rheumatoid arthritis: A narrative review. J. Clin. Med. 2022;11:7179. doi: 10.3390/jcm11237179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shin YH, et al. Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: A nationwide cohort study. Lancet Rheumatol. 2021;3:e698–e706. doi: 10.1016/s2665-9913(21)00151-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Machado PM, et al. Impact of COVID-19 pandemic on the management of patients with RA: A survey of rheumatologists in six European countries. Rheumatol. Adv. Pract. 2023;7:rkac108. doi: 10.1093/rap/rkac108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koh HY, et al. Serum heavy metal levels are associated with asthma, allergic rhinitis, atopic dermatitis, allergic multimorbidity, and airflow obstruction. J. Allergy Clin. Immunol. Pract. 2019;7:2912–2915.e2912. doi: 10.1016/j.jaip.2019.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Kweon S, et al. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES) Int. J. Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park S, et al. National trends in physical activity among adults in South Korea before and during the COVID-19 pandemic, 2009–2021. JAMA Netw. Open. 2023;6:e2316930. doi: 10.1001/jamanetworkopen.2023.16930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hur N-W, Choi C-B, Uhm W-S, Bae S-C. The prevalence and trend of arthritis in Korea: Results from Korea National Health and Nutrition Examination Surveys. jkra. 2008;15:11–26. doi: 10.4078/jkra.2008.15.1.11. [DOI] [Google Scholar]
- 14.Yoo IK, Marshall DC, Cho JY, Yoo HW, Lee SW. N-Nitrosodimethylamine-contaminated ranitidine and risk of cancer in South Korea: A nationwide cohort study. Life Cycle. 2021;1:e1. doi: 10.54724/lc.2021.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JS, et al. Breastfeeding and impact on childhood hospital admissions: A nationwide birth cohort in South Korea. Nat. Commun. 2023;14:5819. doi: 10.1038/s41467-023-41516-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park S, et al. National trends in alcohol and substance use among adolescents from 2005 to 2021: A Korean serial cross-sectional study of one million adolescents. World J. Pediatr. 2023;19:1071–1081. doi: 10.1007/s12519-023-00715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoon SY, et al. National trends in the prevalence of chronic kidney disease among Korean adults, 2007–2020. Sci. Rep. 2023;13:5831. doi: 10.1038/s41598-023-33122-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eum S, et al. Ethnic and sex differences in the distributions of body mass index and waist circumference among adults: A binationally representative study in South Korea and the United States. Eur. Rev. Med. Pharmacol. Sci. 2023;27:1889–1903. doi: 10.26355/eurrev_202303_31555. [DOI] [PubMed] [Google Scholar]
- 19.Lee SW. Regression analysis for continuous independent variables in medical research: Statistical standard and guideline of Life Cycle Committee. Life Cycle. 2022;2:e3. doi: 10.54724/lc.2022.e3. [DOI] [Google Scholar]
- 20.Dewanjee S, et al. COVID-19 and rheumatoid arthritis crosstalk: Emerging association, therapeutic options and challenges. Cells. 2021;10:3291. doi: 10.3390/cells10123291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sung YK, Cho SK, Choi CB, Bae SC. Prevalence and incidence of rheumatoid arthritis in South Korea. Rheumatol. Int. 2013;33:1525–1532. doi: 10.1007/s00296-012-2590-2. [DOI] [PubMed] [Google Scholar]
- 22.Myasoedova E, Davis J, Matteson EL, Crowson CS. Is the epidemiology of rheumatoid arthritis changing? Results from a population-based incidence study, 1985–2014. Ann. Rheum. Dis. 2020;79:440–444. doi: 10.1136/annrheumdis-2019-216694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silman AJ, Pearson JE. Epidemiology and genetics of rheumatoid arthritis. Arthritis Res. Ther. 2002;4:1–8. doi: 10.1186/ar578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silman AJ, Pearson JE. Epidemiology and genetics of rheumatoid arthritis. Arthritis Res. 2002;4(Suppl 3):S265–272. doi: 10.1186/ar578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Challener GJ, et al. Body mass index trend and variability in rheumatoid arthritis. Clin. Rheumatol. 2022;41:349–355. doi: 10.1007/s10067-021-05919-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Darbandi M, et al. The burden of osteoarthritis due to high Body Mass Index in Iran from 1990 to 2019. Sci. Rep. 2023;13:11710. doi: 10.1038/s41598-023-37780-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee KJ, Seon SY, Noh B, An KO. Physical fitness changes in adolescents due to social distancing during the coronavirus disease pandemic in Korea. PeerJ. 2022;10:e14494. doi: 10.7717/peerj.14494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Di Giuseppe D, Bottai M, Askling J, Wolk A. Physical activity and risk of rheumatoid arthritis in women: A population-based prospective study. Arthritis Res. Ther. 2015;17:40. doi: 10.1186/s13075-015-0560-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deane KD, et al. Genetic and environmental risk factors for rheumatoid arthritis. Best Pract. Res. Clin. Rheumatol. 2017;31:3–18. doi: 10.1016/j.berh.2017.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Almoallim H, et al. A review of the prevalence and unmet needs in the management of rheumatoid arthritis in Africa and the Middle East. Rheumatol. Ther. 2021;8:1–16. doi: 10.1007/s40744-020-00252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cui A, et al. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29–30:100587. doi: 10.1016/j.eclinm.2020.100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joseph RP, et al. Physical activity among predominantly white middle-aged and older US adults during the SARS-CoV-2 pandemic: Results from a National Longitudinal Survey. Front. Public Health. 2021;9:652197. doi: 10.3389/fpubh.2021.652197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang HJ, et al. Nationwide changes in physical activity, nutrient intake, and obesity in South Korea during the COVID-19 pandemic era. Front. Endocrinol. 2022;13:965842. doi: 10.3389/fendo.2022.965842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Akkuzu G, et al. Inflammatory rheumatic diseases developed after COVID-19 vaccination: Presentation of a case series and review of the literature. Eur. Rev. Med. Pharmacol. Sci. 2023;27:2143–2151. doi: 10.26355/eurrev_202303_31587. [DOI] [PubMed] [Google Scholar]
- 35.Aliyu AA. Public health ethics and the COVID-19 pandemic. Ann. Afr. Med. 2021;20:157–163. doi: 10.4103/aam.aam_80_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stommel M, Schoenborn CA. Accuracy and usefulness of BMI measures based on self-reported weight and height: Findings from the NHANES & NHIS 2001–2006. BMC Public Health. 2009;9:421. doi: 10.1186/1471-2458-9-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request. Study protocol, statistical code: available from DKY (email: yonkkang@gmail.com). Data set: available from the Korea Disease Control and Prevention Agency (KDCA) through a data use agreement.


