Abstract
A drug concoction called tusi has emerged in Latin America and in Europe and is now beginning to acquire popularity in the United States. “Tusi” is a phonetic translation of “2C,” a series of psychedelic phenethylamines. The concoction is also sometimes referred to as “pink cocaine” as it typically comes in the form of pink powder. However, despite its name, the concoction rarely contains 2C series drugs. Multiple drug checking studies have found that the majority of tusi samples contain ketamine, often combined with 3,4-methylenedioxymethamphetamine (MDMA), methamphetamine, cocaine, opioids, and/or new psychoactive substances. The tusi phenomenon complicates the drug landscape because it has the potential to confuse both people who use it and researchers alike. People using may think the drug is 2C/2C-B, and they may also be unaware that the concoction tends to consist of ketamine and a wide variety of other drugs. Unintentional exposure to its contents can lead to increased risk of adverse effects. The tusi phenomenon also has the potential to complicate drug research as unknown exposure to drugs like ketamine and MDMA will lead to underreporting of use. A combination of self-report and toxicological testing may be needed to inform the most accurate estimates of use. Both researchers and people at risk for use need to be informed about this new concoction. Drug researchers need to be cognizant about the way they query use, and people at risk for using need to be educated about the possible contents of tusi and associated dangers.
Keywords: Tusi, ketamine, new psychoactive substances, club drugs
A drug concoction called tusi has emerged in recent years in Latin America and in Europe and is now beginning to acquire popularity in the United States (US). “Tusi” is a phonetic translation of “2C,” a series of psychedelic phenethylamines that is particularly prevalent among nightlife attendees (1,2). Sometimes the concoction is referred to as “tusibi,” a phonetic translation of 2C-B, a common 2C series drug. Despite recent news stories focusing on tusi use, there is a dearth of scientific literature focusing on this new concoction. In this piece, I argue that tusi has begun to complicate the drug landscape due to confusion regarding what this concoction is, what it contains, and how to assess and report use in research settings.
The real 2C-B: a brief history and epidemiology
2C is the name of a specific family of phenethylamines with stimulant, psychedelic, and often entactogenic properties. There are dozens of 2C compounds, but the most prevalent and well-known were first synthesized by Alexander Shulgin in the 1970s and 1980s (3). 2C-B (2,5-dimethoxy-4-bromophenethylamine) is the most common and most desired compound of the 2C series drugs (1,4). Effects tend to include euphoria, a sense of well-being, changes in perception, and slight hallucination (1,5,6). Effects are commonly described as a “light” high compared to other psychedelics and effects are often compared to effects of lysergic acid diethylamide (LSD) and 3,4-methylenedioxymethamphetamine (MDMA) combined (1).
2C-B began to emerge as a recreational drug, particularly in rave scenes, in the 1990s, although the drug was commonly disguised as MDMA, also known as ecstasy (5). Despite prevalence being somewhat rare, by the early 2000s, 2C-B had been encountered by law enforcement in 48 US states (7). Few epidemiological drug surveys query 2C or 2C-B use, but the drug appears to be particularly prevalent in Spain (8,9). In the Netherlands, detection of 2C series drugs in poisonings and in forensic and consumer drug samples increased between 2013 and 2017 (10). In the US, detection of 2C series drugs in drug seizures appeared to increase from 2006 to 2015 with an uptick in 2C-B seizures in 2019 (11–13). Although national drug surveys in the US do not query 2C use, type-in responses on the largest national drug survey suggest increases in lifetime use since the early 2000s (4). Within the New York City nightclub-attending population, in 2016, lifetime prevalence of 2C use was estimated to be 4.9%, with 62.0% of attendees unfamiliar with this class of drugs (14). Between 2017 and 2022, past-year 2C series use was estimated to be 2–3% among nightclub-attending populations in New York City (2), with estimated past-month use increasing from 0.2% in 2017 to 2.1% in 2022 (15). In addition, reported willingness to use these drugs if offered increased from 1.9% to 4.5% between 2017 and 2019 (16). Given the increasing demand for 2C series drugs (based on survey and seizure data) (13,16), this created an opportunity for illicit manufacturers to create and market a cheaper copycat version of the drug.
Enter: tusi
Tusi is a relatively new drug concoction that is marketed using the phonetic translation of “2C.” This name, especially when mentioned verbally, has great potential to incorrectly refer to 2C. This was likely an intentional marketing tactic. Variations in spelling include “tuci,” ”tucci,” and “tussi,” and tusibí and tucibí (17,18)—which even further misrepresent the specific compound 2C-B. The mixture is also sometimes referred to as “pink cocaine” (“cocaina rosada” in Spanish) despite cocaine rarely being a component of the concoction. Tusi is almost always found in the form of pink powder, often accompanied with a sweet smell resulting from food coloring (18). Tusi reportedly now has a relatively low cost in some areas with some reports suggesting a gram can now cost as little as $10 USD (19), although costs might shift as popularity continues to increase.
It is unknown to what extent people who use or seek tusi are aware of its potential contents. Most drug-checking studies reporting on its contents have been conducted in Latin America where the concoction appears to be most popular. Such studies have typically not found tusi to contain 2C/2C-B, but rather ketamine combined with MDMA, methamphetamine, cocaine, opioids, and/or new psychoactive substances (17). In fact, one study conducted in Chile found that 99% of submissions said to contain 2C contained ketamine and <1% contained actual 2C series drugs (17). A drug checking study that analyzed drug samples submitted at fixed sites and dance festivals throughout Colombia detected a wide range of drugs in tusi including ketamine, MDMA, 3,4-methylenedioxyamphetamine (MDA), cocaine, methamphetamine, synthetic cathinones, 1-(4-Bromo-2,5-dimethoxyphenyl)-2-aminopropane (DOB), local anesthetics such as lidocaine, and opioids such as oxycodone and tramadol (19). 2C-B was typically not detected. Energy Control, the leading drug checking organization in Spain, has also found that almost all samples of tusi submitted test positive for ketamine plus MDMA with or without additional drugs. Similar to other studies, 2C-B was rarely detected (18). Energy Control reports that, on average, a third (34%) of the volume of tested samples is ketamine and 11% MDMA. Similar mixtures of drugs detected in tusi have been reported on social media by drug checking organizations in the United Kingdom, Switzerland, Australia, and Canada (17).
With respect to the US, in December 2019, DrugsData.org, Erowid Center’s anonymous lab-based drug testing program published the first US result of a pink powder labeled as tucibi/tusi (containing ketamine, MDMA, and caffeine), and in January 2020, DanceSafe, a drug checking organization in the US, issued what appeared to be the first public alert in the US (20). Through 2022, there were 19 submissions of similar pink powder concoctions from within the US labeled as tusi or 2C-B (with samples analyzed by DrugsData). As shown in Figure 1, almost all samples (94.7%) contained ketamine as the main ingredient, and 84.2% contained a ketamine precursor called 1-[(2-chlorophenyl)(methylimino)methyl]cyclopentanol. Also similar to findings by other drug checking organizations, detection of MDMA was common, detection of cocaine was relatively rare, and 2C series compounds were not detected.
Figure 1.
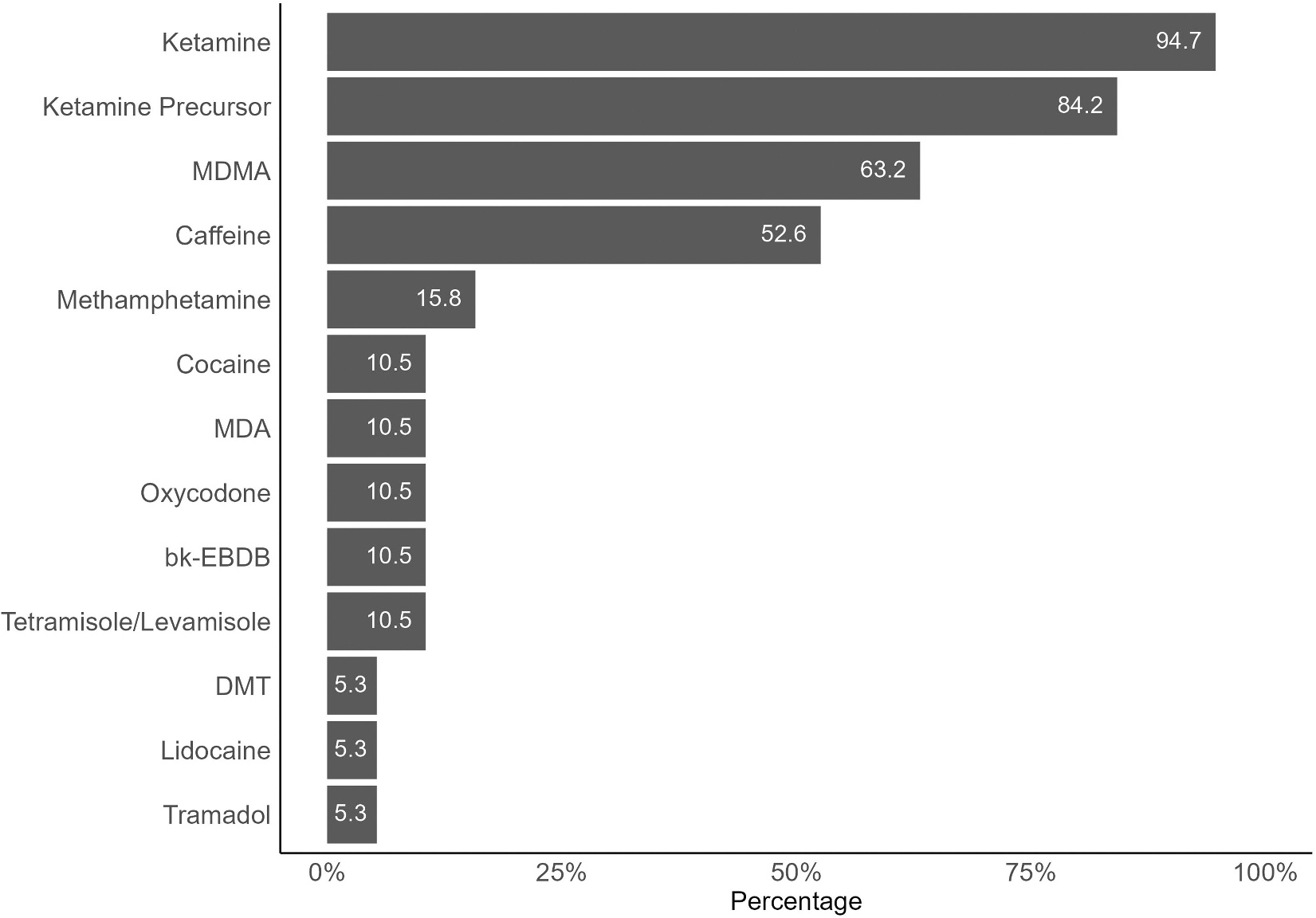
Contents of pink powder submissions labeled as tusi or 2C-B in the US, 2019–2022. Drugs detected within the 19 pink powder tusi/2C-B submissions to DrugsData between 2019 and 2022. The ketamine precursor is 1-[(2-chlorophenyl)(methylimino) methyl]cyclopentanol. MDMA = 3,4-methylenedioxymethamphetamine; MDA = 3,4-methylenedioxyamphetamine; bk-EBDB = β-keto-1,3-benzodioxolyl-N-ethylbutanamine (eutylone); DMT = N, N-dimethyltryptamine.
Studies focusing on people who use tusi are needed as this concoction increases in popularity. Specifically, information is needed regarding prevalence of use, characteristics of people who use, reasons for use, and effects experienced. The drug checking study in Colombia reported that the majority of people who used tusi were young adults age 18–29 and that 61.2% reported using once a month or more often (with 25.2% of the sample using once per week or more often) (19). Co-use of alcohol, ecstasy, and cocaine was common, and effects of tusi reportedly included euphoria, sedation, dizziness, vomiting, blacking out, and loss of consciousness. Studies assessing such information are needed in the US, especially as the drug spreads and the concoction begins to change.
Complicating the drug landscape
The tusi phenomenon complicates the drug landscape because it has the potential to confuse both people who use and researchers alike. With respect to people who use, given the drug concoction’s name, people may assume the drug is 2C/2C-B. Since many partiers are unfamiliar with 2C series drugs (14), there is also potential for people to simply think this is a new (and perhaps benign) drug – especially given that the powder is pink with a sweet scent. The concoction’s other name, “pink cocaine,” may also lead some to believe this is a form of cocaine. This is an issue because cocaine is often used to balance out the effects of alcohol and unintentional ketamine use combined with alcohol use can lead to adverse reactions (21,22). Regardless of what people who use believe is in this concoction, batches tend to greatly fluctuate regarding which drugs and how much of them are mixed in. As such, this concoction may lead to unpredictable effects. Pre-mixed combinations of various drugs can also interact and have synergistic effects. This situation is even further complicated by the fact that many people in scenes that use tusi (e.g., party scenes) engage in polydrug use (19) which can lead to larger than planned doses or even further unintentional drug combinations. Tusi can also contain highly potent stimulants such as methamphetamine, which can be particularly dangerous or unpleasant if unknowingly consumed. As tusi acquires more popularity as a mystery powder, more people may create their own drug amalgamations to sell under its name, and similar to the current cocaine situation in the US (23), fentanyls may begin to appear in tusi, which will increase potential for overdose and death. A task force in California has already seized 4.4 lbs. of pink powder containing ketamine and despropionyl fentanyl (24), but this is a fentanyl precursor, which is thought to be relatively inactive (25).
The tusi phenomenon also has the potential to complicate drug research. While toxicology studies tend to be more focused on testing which substances people have been exposed to, clinical, epidemiological, and social science studies that rely primarily on self-report can be affected. Most drug surveys do not query the use of actual 2C series drugs, so it is unlikely that such surveys will begin to ask specifically about tusi. Those who add questions about this concoction may assume tusi and 2C are the same product and collect unreliable data. It is also important to differentiate between what a product is called and what drug or drugs are present in the product. In this case, currently, ketamine appears to be the most common and most abundant drug present in tusi. While the two leading national drug surveys in the US do query ketamine use, “correct” responses to questions about use would depend on the participant knowing they were exposed to ketamine in tusi. As such, use of drugs such as ketamine or MDMA that was present in tusi will likely be underreported. Similarly, the use of synthetic cathinones (“bath salts”) is commonly underreported among people who use ecstasy because they are unaware that the ecstasy they used contained these compounds (26,27). Prevalence of ketamine use already appears to be increasing in the US (28), and increasing use of tusi will further drive increases, but estimated increases would likely depend on people knowing that they actually used ketamine. Studies focusing on both self-report and toxicological testing may be needed to inform the most accurate estimates of drug use.
Recommendations
While the use of tusi will likely remain relatively rare in comparison to more common drugs, this new concoction has the potential to become a new fad in the US, similar to Molly – a powder deceptively marketed as pure MDMA (29). Both researchers and people at risk for use need to be educated about this new concoction. Drug researchers who focus on the use of party drugs and novel drugs in particular need to be aware of the increasing popularity of this concoction and be aware of its likely contents and associated effects. Researchers must also be aware that there will be confusion regarding self-reported use as some people who use may think it is actually 2C or cocaine. While drug checking studies have focused on tusi use, more epidemiology studies (e.g., drug surveys) – in the US and in other countries – are needed for us to better understand prevalence of use. When asking about use of 2C drugs and/or tusi, surveys need to clearly differentiate between the two and perhaps define each drug for participants so they can differentiate. Although, in many cases, participants will likely not be able to differentiate. As such, when possible, biospecimen testing (e.g., of hair, saliva, urine) can be added to survey studies as this can help deduce unknown exposure to drugs contained in such concoctions (30). People at risk for using tusi need to be educated about the possible contents of this concoction and associated dangers. Education of those at risk can be accomplished by targeting high-risk populations directly (e.g., as they enter party venues) and through targeted social media efforts. While most tusi today contains ketamine as the main ingredient, this could change, and contents certainly vary greatly across batches. Similarly, two decades ago, Molly became marketed as a new and pure powder form of MDMA/ecstasy, but soon thereafter the drug tended to become so adulterated that it often contained little to no MDMA (29). Tusi will likely remain a mystery powder to many people who use, and it will become more dangerous if people begin mixing in drugs like fentanyl. Testing the drug before use can help people deduce what it actually contains and decide whether or not they feel it is safe to use but the first step to acquiring knowledge about this concoction is education.
Acknowledgement
The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health. I would like to thank DrugsData.org – a project of Erowid Center (a 501(c)(3) non-profit educational organization) for providing access to their drug testing data on this substance and for providing permission to publish summary results. Similarly, I would like to thank the Massachusetts Drug Supply Data Stream and the Chicago Recovery Alliance for allowing me to present their drug test results published on DrugsData.org.
Funding
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number R01DA044207.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Palamar J, Acosta P. A qualitative descriptive analysis of effects of psychedelic phenethylamines and tryptamines. Hum Psychopharmacol. 2020;35:e2719. doi: 10.1002/hup.2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palamar JJ, Keyes KM. Trends in drug use among electronic dance music party attendees in New York City, 2016–2019. Drug Alcohol Depend. 2020;209:107889. doi: 10.1016/j.drugalcdep.2020.107889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shulgin A, Shulgin A. PIHKAL: a chemical love story. Berkeley, CA: Transform Press; 2014. [Google Scholar]
- 4.Palamar JJ, Le A. Use of new and uncommon synthetic psychoactive drugs among a nationally representative sample in the United States, 2005–2017. Hum Psychopharmacol. 2019;34:e2690. doi: 10.1002/hup.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United States Department of Justice. 2C-B (Nexus) reappears on the club drug scene. Washington, DC; 2001. https://www.justice.gov/archive/ndic/pubs0/665/665p.pdf. [Google Scholar]
- 6.Gonzalez D, Torrens M, Farre M. Acute effects of the novel psychoactive drug 2C-B on emotions. Biomed Res Int. 2015;2015:643878. doi: 10.1155/2015/643878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United States Drug Enforcement Administration. 4-Bromo-2,5-Dimethoxyphenethylamine: diversion control division. Drug Chem Eval Sect. 2020. https://www.deadiversion.usdoj.gov/drug_chem_info/bromo_dmp.pdf [Google Scholar]
- 8.González D, Ventura M, Caudevilla F, Torrens M, Farre M. Consumption of new psychoactive substances in a Spanish sample of research chemical users. Hum Psychopharmacol. 2013;28:332–40. doi: 10.1002/hup.2323. [DOI] [PubMed] [Google Scholar]
- 9.Caudevilla-Gálligo F, Riba J, Ventura M, González D, Farré M, Barbanoj MJ, Bouso JC. 4-Bromo-2,5-dimethoxyphenethylamine (2C-B): presence in the recreational drug market in Spain, pattern of use and subjective effects. J Psychopharmacol. 2012;26:1026–35. doi: 10.1177/0269881111431752. [DOI] [PubMed] [Google Scholar]
- 10.Hondebrink L, Nugteren-van Lonkhuyzen JJ, Hunault CC, van den Berg J, van der Gouwe D, van Riel A. New psychoactive substances (NPS) in the Netherlands: occurrence in forensic drug samples, consumer drug samples and poisons center exposures between 2013 and 2017. Addiction. 2020;115:716–25. doi: 10.1111/add.14868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S. Drug Enforcement Administration. 2C-Phenethylamines, Piperazines, and Tryptamines Reported in NFLIS, 2011–2015. Springfield, VA; 2017. [Google Scholar]
- 12.U.S. Drug Enforcement Administration. Forensic Laboratory Information System Special Report: Emerging 2C-Phenethylamines, Piperazines, and Tryptamines in NFLIS, 2006–2011; Springfield, VA; 2012. [Google Scholar]
- 13.U.S. Drug Enforcement Administration. National Forensic Laboratory Information System: NFLIS-Drug 2019 Annual Report; Springfield, VA: US; 2020. [Google Scholar]
- 14.Palamar JJ, Acosta P, Cleland CM. Attitudes and beliefs about new psychoactive substance use among electronic dance music party attendees. Subst Use Misuse. 2018;53:381–90. doi: 10.1080/10826084.2017.1327980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palamar JJ, Le A, Cleland CM, Keyes KM. Trends in drug use among nightclub and festival attendees in New York City, 2017–2022. Int J Drug Policy. 2023;115:104001. doi: 10.1016/j.drugpo.2023.104001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palamar JJ. Increasing willingness to use synthetic drugs if offered among electronic dance music party attendees, 2017–2019. J Psychoactive Drugs. 2020;52:324–33. doi: 10.1080/02791072.2020.1761574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United Nations Office on Drugs and Crime. ”Tuci”, “happy water”, “k-powdered milk” – is the illicit market for ketamine expanding?” 2022.
- 18.Energy Control. Tusi. https://energycontrol.org/sustancias/tusibi/ [Google Scholar]
- 19.Díaz Moreno M, Alarcon Ayala A, Quintero J, Morris V, Estrada Y. Échele Cabeza as a harm reduction project and activist movement in Colombia. Drug Habits Social Policy. 2022;23:4. doi: 10.1108/DHS-07-2022-0026. [DOI] [Google Scholar]
- 20.DanceSafe. #testit Alert: bag of pink powder sold in Sacramento, CA as 2C-B but actually contains caffeine, ketamine, and MDMA. 2020.
- 21.Miró Ò, Dargan PI, Wood DM, Dines AM, Yates C, Heyerdahl F, Hovda KE, Giraudon I, Galicia M. Epidemiology, clinical features and management of patients presenting to European emergency departments with acute cocaine toxicity: comparison between powder cocaine and crack cocaine cases. Clin Toxicol. 2019;57:718–26. doi: 10.1080/15563650.2018.1549735. [DOI] [PubMed] [Google Scholar]
- 22.Palamar JJ, Acosta P, Le A, Cleland CM, Nelson LS. Adverse drug-related effects among electronic dance music party attendees. Int J Drug Policy. 2019;73:81–87. doi: 10.1016/j.drugpo.2019.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DiSalvo P, Cooper G, Tsao J, Romeo M, Laskowski LK, Chesney G, Su MK. Fentanyl-contaminated cocaine outbreak with laboratory confirmation in New York City in 2019. Am J Emerg Med. 2020;40:103–05. doi: 10.1016/j.ajem.2020.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Fresno County Sheriff’s Office. HIDTA drug task force seizes $6.8 million in fentanyl and ketamine. https://www.fresnosheriff.org/media-relations/hidta-drug-task-force-seizes-6-8-million-in-fentanyl-and-ketamine.html
- 25.Kuip EJ, Zandvliet ML, Koolen SL, Mathijssen RH, van der Rijt CC. A review of factors explaining variability in fentanyl pharmacokinetics; focus on implications for cancer patients. Br J Clin Pharmacol. 2017;83:294–313. doi: 10.1111/bcp.13129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oliver CF, Palamar J, Salomone A, Simmons SJ, Philogene-Khalid H, Stokes-McCloskey N, Rawls S. Synthetic cathinone adulteration of illegal drugs. Psychopharmacology. 2018;236:869–79. doi: 10.1007/s00213-018-5066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palamar JJ, Salomone A, Gerace E, Di Corcia D, Vincenti M, Cleland CM. Hair testing to assess both known and unknown use of drugs amongst ecstasy users in the electronic dance music scene. Int J Drug Policy. 2017;48:91–98. doi: 10.1016/j.drugpo.2017.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palamar JJ, Rutherford C, Keyes KM. Trends in ketamine use, exposures, and seizures in the United States. Am J Public Health. 2021;111:2046–49. doi: 10.2105/AJPH.2021.306486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Palamar JJ. There’s something about Molly: the under-researched yet popular powder form of ecstasy in the United States. Subst Abus. 2017;38:15–17. doi: 10.1080/08897077.2016.1267070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palamar JJ, Salomone A, Keyes KM. Underreporting of drug use among electronic dance music party attendees. Clin Toxicol. 2021;59:185–92. doi: 10.1080/15563650.2020.1785488. [DOI] [PMC free article] [PubMed] [Google Scholar]


