Summary
Cardiovascular inequalities remain pervasive in the European countries. Disparities in disease burden is apparent among population groups based on sex, ethnicity, economic status or geography. To address this challenge, The Lancet Regional Health - Europe convened experts from a broad range of countries to assess the current state of knowledge of cardiovascular disease inequalities across Europe. This report presents the main challenges in Eastern Europe. There were pronounced variations in cardiovascular disease mortality rates across Eastern European countries with a remarkably high disease burden in the North-Eastern Europe. There were also significant differences in access and delivery to healthcare and unmet healthcare needs. Addressing the cardiovascular determinants of health and reducing health disparities in its many dimensions has long been a priority of the European Parliament's work through resolutions and by financing pilot projects. Yet, despite these efforts, few large-scale studies have been conducted to examine the feasibility of reducing cardiovascular disparities in Eastern Europe. There is an urgent need for improved data, measurements, reporting, and comparisons; and for dedicated, collaborative research. There is also a need for a broader understanding of the typology of actions needed to tackle cardiovascular inequalities and a clear political will.
Keywords: Cardiovascular diseases, Geography, Eastern Europe, Determinants of health
Key messages.
-
•
Countries in Eastern Europe have a much lower life expectancy compared with the rest of Europe. Inequalities in life expectancy mostly coincide with different rates of ischemic heart disease (IHD) deaths.
-
•
IHD mortality is dramatically higher in the North-Eastern European countries compared with Central-Eastern and South Eastern countries with age-standardised mortality rates per 100,000 inhabitants ranging from 399.2 in Ukraine to 71.3 in Poland.
-
•
Not only the IHD death rates are higher in the North-Eastern Europe, but deaths also occur at younger ages. This observation is a significant public health concern, as it not only represents a loss of life but also has broader implications for the healthcare systems, the workforce productivity, and the overall societal well-being.
-
•
High rates of risk factors for IHD, such as smoking, diabetes, hypercholesteremia and hypertension persist in the North-Eastern European countries, which may contribute to the development of cardiovascular diseases at a younger age.
-
•
In general, the higher is the country income level, the better is the cardiovascular health. However, IHD mortality cannot be entirely explained by income inequalities.
-
•
Eastern European countries with a relatively high IHD prevalence rates have high coronary revascularization rates, but this is not enough to reduce mortality from IHD equally in all countries.
-
•
There is an urgent need for improved analysis and reporting of data to describe the determinants of cardiovascular health across Eastern Europe. Policies may need to be tailored to individual countries rather than applying a one-size-fits-all approach.
Introduction
Cardiovascular disease (CVD) is the leading and largest cause of mortality globally. Ischemic heart disease (IHD) alone is the world's biggest killer, accountable for 8.9 million deaths worldwide (16% of the world's total deaths)1 and these numbers are projected to increase over time mostly due to the ageing of the population.1 This is an area of public health, scientific and socio-economic concern, and of significant geographical variation and heterogeneity.
Analysis of cardiovascular mortality data have shown significant inequalities, and health gaps between European countries, probability due to disparities in health care prevention and access, lifestyle factors, diet, and socioeconomic inequalities. The region of Eastern Europe has the highest CVD mortality in the world.2,3 As such the understanding of the distribution of CVD has become crucial as countries develop national strategies to reduce the burden of the disease.
Methods
Definition of Eastern European countries
Eastern Europe, as defined by the United Nations Statistics Division (UNSD),4 includes the countries of Bulgaria, Czechia, Hungary, Poland, Romania, Russian Federation, and Slovakia, as well as the republics of Belarus, Republic of Moldova, and Ukraine.4 In some sources, Eastern Europe is defined as the nations bordered by the Baltic and Barents seas on the north; the Adriatic, Black, and Caspian seas and the Caucasus Mountains on the south; and the Ural Mountains. Using this definition, the nations of Albania, Bosnia and Herzegovina, Croatia, Serbia, North Macedonia, and Montenegro, which the UNSD categorizes as Southern Europe, would be included.4 This definition also includes the Baltic Republics of Estonia, Latvia, and Lithuania, considered by the UN as Northern Europe.4 The boundaries of Eastern Europe, therefore, are subject to substantial overlap and variation depending on the context in which they are used, which makes demarcation difficult.4
The current study refers to all European countries listed above as they were previously ruled throughout the twentieth century by socialist regimes. As such, after the fall of socialism, these countries started a process of political, economic, and health system reform. The entire group of countries entered roughly similar directions of reform, despite differences in economic transition dynamics and the degree of government determination to implement reforms.5 As such, we are dealing with a relatively large group of countries that had similar starting points for cardiovascular health care transition.5 Unfortunately, there is still a gap in evidence concerning the impact of such reforms on health system performance in many of these countries.5
The current study attempts to analyse the determinants of cardiovascular health in Eastern Europe with regard to their influence on cardiovascular outcomes. Information is crucial as the greatest burden of CVD is present in low- and middle-income countries and a large proportion of the Eastern European countries are middle-income countries.6
Search strategy and selection criteria.
We identified published papers in English language from academic databases, mainly MEDLINE, through PubMed search using keywords such as “Central and Eastern Europe”, “Eastern Europe”, “former Soviet Union”, “Coronary heart disease mortality”, “IHD mortality”, “cardiovascular health”, “cardiovascular prevention”, “cardiovascular health promotion”, “CVD prevention”, “community-based”, and their combinations. We also searched for any relevant registry studies in the region. Finally, we included original data given as courtesy from public and private organizations in Eastern Europe. The data that support the findings of this study are drawn from publicly accessible databases, and there is no personally identifiable information about individuals. Therefore, ethical approval was not needed for this study.
Demographic and social indices
Eastern European countries are made up of middle- and high-income countries as defined by the World Bank Gross National Income (GNI).7 As such, social determinants of health (i.e., income level, educational attainment, employment status, and environmental socioeconomic factors) may be consistently associated with cardiovascular outcomes.8,9 Despite this, the incidence of CVD in the last two decades has increased in some countries such as Estonia and decreased in some other countries such as Croatia and Czechia, being all of these Eastern European countries classified as high-income.2,10 Analysis of this phenomenon is still hindered by insufficient information. It is not known whether the risk-factor burden is higher in middle-income countries than in high-income countries, whether mortality after a cardiovascular event is higher in middle-income countries than in high-income countries, or whether both are true. To address these questions, we summarized and compared population structures and their GNI according to the World Bank.11 Although there is no universally agreed definition for continental subregions, comparisons were also attained by comparing subregions of Europe based on “The World Factbook”,12 specifically: Central-Eastern Europe (CEE), South-Eastern Europe (SEE) and “Eastern Europe” (in this report: North-Eastern Europe; NEE), the latter mainly consisting of the European part of the former Soviet Union.12
World Bank and World Health Organization
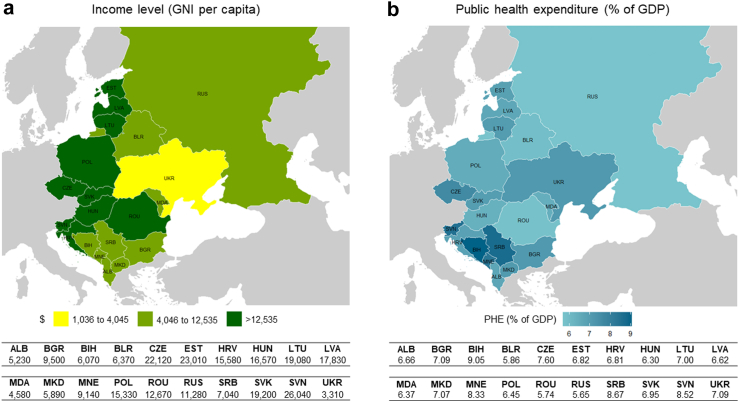
Using World Bank Atlas classification 2021 (calendar year 2019), middle-income economies are those with a GNI per capita between $1036 and $12,535 and high-income economies are those with a GNI per capita of more than $12,535.7 Croatia, Czechia, Estonia. Hungary, Latvia Lithuania, Poland, Romania, Slovenia, and Slovakia are high-income countries, the remaining Eastern European geographic areas are middle-income countries (Fig. 1a).7 Throughout the manuscript, the term ‘middle-income countries’ represents a composite of upper- and lower-middle-income countries.7 Data are also presented for the Eastern European countries, stratified according to the 2019 World Health Organization (WHO) definition of Current or Public Health Expenditure (PHE) values as percentage of gross domestic product (GDP) as shown in Fig. 1b.13
Fig. 1.
Income level (panel a) and current PHE as percentage of GDP (panel b). Panel a shows the country classifications by income level according to the World Bank. The classifications are based on the GNI per capita of calendar year 2019. Panel b shows current or public health expenditure (PHE) as percentage of gross domestic product (GDP) according to WHO-Global Health Observatory data repository. Year 2019 for all countries except Albania (2018). Colour gradient maps: the darker the colour the greater the values. Maps modified from © EuroGeographics for the administrative boundaries.
Data collection
The study reports a period of 15 years (2005–2019) in the Eastern European Countries. In some cases, substantial gaps in data availability were identified, so that we had to restrict the analysis to a small number of countries. Cardiovascular disease incidence, risk factors and mortality data come from the WHO-Global Health Observatory,14 WHO-European Health 2020 Indicators,15 WHO-Mortality Database,16 Global Burden of Disease Database,17 Eurostat Cardiovascular Diseases Statistics,18 European Cardiovascular Disease Statistics19 and the Organisation for Economic Co-operation and Development (OECD) Health at a Glance: Europe10 using the 2019, or nearest year available, update of age- and sex-specific mortality and risk factors data by country. General limitations of the data include choice of method for dealing with missing data used by the main providers, and lack of observational data in reporting practices by many of these countries. Moreover, different countries may have different diagnostic and certification practices, which might influence the methodology for deciding on cause of death. This may be particularly relevant in the elderly, where there may be several possible causes of cardiovascular death, which may produce an underestimation or an overestimation of the mortality rates from IHD. The scarcity of validated and unbiased data related to cardiovascular health in Eastern Europe hampers the ability to accurately assess the current status and trends. Future research efforts should focus on generating high-quality data to address this gap.
Age-standardised mortality rates
Ischemic heart disease deaths were standardised to the WHO standard European population, to allow comparison between populations with a different age distribution.16,20 All the countries that reported mortality data had age information to standardize the rates.16,20
Key observations
Life expectancy
Data on life expectancy at birth for both men and women reveal significant differences between European countries (Fig. 2, Tables S1 and S2). A male child born in the European Union will live to be 78.1 years old on average. On average, European Union women are 5.5 years older, reaching an age of 83.6.15 Countries in Eastern Europe have a much lower life expectancy compared with the rest of Europe.15 Considering the 2016 averages, there was a difference of more than 10 years between the countries with the lowest and highest life expectancy: 67.5 years for men and 77.3 years for women in Ukraine compared with 80.6 years for men and 84.3 years for women in Norway.15 Lithuania had the largest difference in life expectancy (10.7 years) between men (69.5 years) and women (80.2 years), while Sweden had the smallest difference (3.8 years) between men (80.3 years) and women (84.1 years).15 As the WHO indicators report, considerable differences also exist within the group of Eastern European countries even if classified as belonging to the same country income level.15 The average life expectancy in middle-income countries ranged between 67.5 (men) and 77.3 (women) years in Ukraine to 77.5 (men) and 81.8 (women) years in Albania. Other, large inequalities in life expectancy can be seen comparing women and men within some middle-income countries, with disparities of up to 8 years and more in Romania, Bulgaria and Russian Federation. Thus, depending upon their country of birth, Europeans could expect to have approximately 10 more (or less) years of life.15 Because the decline in CVD death was the main culprit of the largest increase in life expectancy during the last two decades overriding the effects of all other causes of mortality, the above reported inequalities in life expectancy may reveal different routes of CVD deaths in the Eastern European countries compared with their Western counterparts.
Fig. 2.
Trends in life expectancy at birth from 2005 to 2016 by geographical region and sex. Data from WHO-European Health 2020 Indicators in which life expectancy at birth is the average number of years a newborn could expect to live and reflects the overall mortality level of a population. Last available year 2016.15South-Eastern Europe: Albania, Bosnia and Herzegovina, Bulgaria, Croatia, Montenegro, North Macedonia, Romania and Serbia; Central Eastern Europe: Czechia, Hungary, Poland, Slovakia and Slovenia; North-Eastern Europe: Belarus, Estonia, Latvia, Lithuania, Republic of Moldova, Russian Federation and Ukraine.
Standardised mortality rates for ischemic heart disease
Cardiovascular disease causes over 4 million deaths per year in Europe, primarily from IHD.16,21 Strong health inequalities in the standardised mortality rates for IHD can be observed among the European countries (Fig. 3, Tables S3–S5).16,21 In general, the higher is the country income level, the better is the cardiovascular health. The highest age-standardised mortality rate for IHD is found in Ukraine (399.21 deaths per 100,000 inhabitants). Ukraine is a middle-income country with the lowest GNI per capita in Europe (3310 USD in 2019). However, mortality cannot be entirely explained by income inequalities. Strong geographical disparities are also apparent. Although the highest standardised mortality rates are always observed in Eastern Europe, they often are independent of the country income level. For example, Slovenia and Lithuania are both high-income countries. Despite this, age-standardised mortality rates range from approximately 45.8 deaths per 100,000 inhabitants in Slovenia, to around 222.4 per 100,000 in Lithuania. The association between income level and health disparities is, therefore, confined to the most disadvantaged Eastern European countries. The European Commission has argued that “to reduce the social-economic gradient in health, actions must be universal, but with a scale and intensity that is proportionate to the level of disadvantage”.22 This goal may be achieved by increasing the knowledge base on causes and interventions for IHD in each specific geographic area.
Fig. 3.
Trends in age-standardised IHD death rates/100,000 population, by geographical region, sex and age group, from 2005 to 2019 (or nearest year). Data from the WHO-European mortality database.16 Mortality levels and trends are estimated from data on deaths by cause/age/sex and mid-year population by age/sex. Colour gradient maps: the darker the colour the greater the values. Maps modified from © EuroGeographics for the administrative boundaries.
Eastern European subregions and mortality rates for ischemic heart disease
Following 2005, the IHD mortality gradually decreased in the CEE countries, first in Czechia, and Poland. Studies have suggested that likewise to Western Europe, more than half the IHD mortality decline in the Czechia and Poland can be explained by changes in risk factors.23,24 By contrast, IHD mortality dramatically increased in the NEE countries, and improved only by 2010. Substantial disparities are still present in 2019 between NEE and CEE countries, with age-standardised IHD mortality rates per 100,000 inhabitants ranging from 399.2 in Ukraine to 71.3 in Poland (Fig. 3, Tables S3–S5). With regard to SEE, the magnitude of the fall in IHD mortality widely varies across different countries. For example, 10-year decreases in IHD age-standardised mortality rates ranged from 40% in Croatia (164.2 versus 97.8) to 11% in Bulgaria (116.1 versus 102.1).
Disadvantaged, vulnerable or marginalized groups
Disadvantaged, vulnerable or marginalized groups are defined by the WHO as those who, “due to factors usually considered outside their control, do not have the same opportunities as other, more fortunate groups in society”.25 Examples might include inequities in the delivery of cardiovascular care in the elderly, women, and non-white patients.3,25,26 Disadvantage takes many other forms, such as unemployed people, refugees and others who are socially excluded. Although low socioeconomic status has been associated with CVD mortality and can be considered a target for intervention,27 we did not summarize variations in outcomes by socioeconomic deprivation because this relates to wider determinants of global health which has been illustrated elsewhere.28 As well, it is unknown how many people of non-European descent live in East Europe, because most of these countries do not track ethnicity in their census. Accordingly, we focused on disparities in cardiovascular care and outcomes only by age and sex.
Standardised mortality rates for ischemic heart disease stratified by age
Not only the IHD death rates are higher in NEE than CEE and SEE countries, but they also occur at younger ages (Fig. 3, Tables S6–S8).16 The premature mortality from IHD (<65 years) in 2019 among men in Latvia, Lithuania, and Belarus (70.4, 78.9 and 159.7 per 100,000 inhabitants, respectively) is more than twice higher than in Poland and Serbia (29.9 and 34.9 per 100,000, respectively). The dramatic East-West gap in premature IHD mortality is striking even when comparing the above reported data for CEE and SEE with those of Germany and Spain (19.9 and 15 per 100,000 inhabitants, respectively). Among women, when comparing NEE, CEE and SEE each other and to other countries in Western Europe, the premature mortality shows similar patterns as for men though at lower rates.
Standardised mortality rates for ischemic heart disease stratified by sex
The women to men rate ratios for IHD death are presented by country (Fig. 4).16,19 Mortality from IHD in women is higher than in men in almost all of the Eastern European countries with a mean ratio of approximately 1.2. However, there are large sex differences in death rates from IHD across Eastern Europe and between East and West Europe. For instance, Slovakia, with one of the highest IHD prevalence rates, has one of the highest women to men ratios (1.56). Also, Ukraine, with the highest IHD prevalence rate, has the women to men ratio close to the mean (1.22). By contrast, the women to men rate ratio in Spain remains one of the lowest in Europe (0.77). Of note, IHD prevalence rate in Spain is much lower than those in the Eastern European countries. These data suggest that women proportionally die for IHD much more in Eastern Europe than in its Western counterpart. This view is further supported by some other observations. For example, there is a 11-fold difference in female death rates from IHD in France versus Lithuania (14.6 deaths versus 163.6 per 100,000 women) and a 8-fold difference in male death rates from IHD in France versus Lithuania (39.8 deaths versus 314.1 per 100,000 men) (Tables S4 and S5). It is hard to identify the exact causes of these large outcome variations between women and men in different countries. The relative contribution of preventive strategies and medical interventions varies from country to country. Studies have suggested inequalities in access to cardiovascular healthcare for women in many geographic areas the world.29, 30, 31, 32, 33, 34
Fig. 4.
Women to men rate ratios for age-standardised IHD death, by country. The source of the data is the WHO-European mortality database.16 Mortality is age-standardised on the basis of the standard European population.
Incidence and prevalence of ischemic heart disease
Between 2005 and 2019, most Eastern European countries reported an increase in the number of new CVD cases (Tables S9 and S10).17 Of these, approximately 50% represented new IHD cases. The largest increase of over 40% have been reported in Albania and Slovenia among both men and women. The largest decrease in incidence over this period was reported in Poland among both women and men (by approximately 33%).17 However, these crude incidence numbers do not consider differences between populations in terms of size and age composition. Therefore, we also analysed how the prevalence of IHD has changed during these years (Table S11). Age-standardised prevalence rates for IHD were higher in men than women in all Eastern European countries. Among these countries, IHD prevalence rates tended to be relatively higher in NEE countries and lower in CEE and SEE countries. Indeed, the age-standardised IHD prevalence rate in the Eastern European countries ranged from 2727/100,000 in Poland to 5388/100,000 in Estonia among men and from 1685/100,000 in Poland to 3584/100,000 in Ukraine among women.17 Acknowledging disparities in the incidence and prevalence of the disease is crucial, as interventions and policies may need to be tailored to individual countries rather than applying a one-size-fits-all approach.
Unmet healthcare need
According to Eurostat, more than 20% of the European population declared they had an unmet healthcare need in 2019 that was due to finances, distance/transport or waiting lists.21 The most common reason was that it was too expensive. Notably, there were very large inequalities among the countries of Eastern Europe even if these countries were classified as high-income. Latvia, a NEE country, had the largest share of persons reporting that medical costs pose a high financial burden (27%).21 The share of those declaring that paying for medical care caused no financial burden was largest in CEE countries such as Czechia and Slovakia (all less than 10%) than in SEE countries, such as Serbia and Croatia (all more than 15%).21 These geographical differences, therefore, need to be explored. The data presented here focus on three reasons: the care was too expensive, the distance to travel too far or waiting times too long. Other specific barriers to meet the healthcare need may include for instance, lack of health insurance coverage and high levels of private (‘out-of-pocket’) expenditure.21 Lack of primary and secondary prevention and access to health services are critical factors to address cardiovascular health inequalities in disadvantaged communities and may largely explain the above reported differences. Medical care contributes to about 37% of the decline in IHD mortality in Poland as shown using the IMPACT model in Eastern Europe.24,35 However, these results should be cautiously generalisable to many CEE and SEE countries, but not to NEE countries, which experienced more complicated trends in mortality.
Access to coronary revascularization in ischemic heart disease
Although there appears to be a well reported association between the use of coronary revascularization for IHD and improved outcomes36,37 our study reveals that this is not a consistent finding across Eastern European countries.18 Fig. 5a provides an overview of the rates per 100,000 inhabitants for coronary revascularization in some selected Eastern European countries. Percutaneous coronary intervention (PCI) was the most frequently employed method of coronary revascularization followed by coronary artery bypass graft (CABG). Among Eastern European countries there was a wide range in the utilization of PCI procedures. In general, Eastern European countries with a relatively high IHD prevalence rates (Table S12) had high PCI rates. Estonia and Poland had PCI rates of 219.9 and 258.8, and the rate ratios between IHD prevalence and PCI per 100,000 inhabitants were approximately similar: 4.1% and 3.5%, respectively. However, whilst Poland reported a lower age-sex standardised rate of 30-day mortality per 100 admissions after acute myocardial infarction (4.7%), Estonia reported much higher mortality (9.2%) (Fig. 5b). A constellation of factors is likely to contribute to this finding including the fact that there is a heterogeneous approach to the data reporting, with a particular paucity of data about the number of patients with ST-Segment Elevation Myocardial infarction (STEMI) as a marker of the severity of IHD, the mode of reperfusion therapy provided in STEMI38, 39, 40 and the number of patients with STEMI who did not receive timely reperfusion therapy or even who did not receive any reperfusion therapy.39,40 It is difficult to discuss mortality post IHD with no reference to how revascularization rate differences came into play.
Fig. 5.
PCI and CABG per 100,000 inhabitants, performed in hospitals, year 2019 (panel a) and age-sex standardised 30-day mortality rate after hospital admission for acute myocardial infarction based on unlinked data, year 2019 or nearest (panel b). Panel a: The source of data is Eurostat Health Care database, in which data are collected according to the classification ICD-9-CM. Procedures density rates are used to describe the frequency of services rendered, expressed in per 100,000 inhabitants of the by respective population. Panel b: the source of data is OECD-Health at a Glance: Europe 2022, in which 30-day case-fatality are measured as the percentage of patients aged 45 and over following hospital admission for acute myocardial infarction. It counts only deaths, that occurred in the hospital where the patient was initially admitted. Rates are age-standardised to the 2010 OECD population aged 45 and over admitted to hospital for acute myocardial infarction.
Possible drivers of inequalities in reperfusion therapy across Eastern European countries
The lack of uniformity in reporting care and outcomes across the Eastern European countries hinders realistic comparison within Eastern European countries and externally with the Western counterparts. For example, time delays to reperfusion therapy in STEMI varies substantially by Eastern European country.41, 42, 43, 44, 45 In Romania, 81.8% of the STEMI population were admitted within 12 h of symptom onset.46 Yet, only 69.5% of the STEMI population were admitted within 12 h in Bulgaria.44 About 10% of patients still did not receive reperfusion therapy within 24 h, with late presentation as the most often reported reason.47 Inconsistency between-country measurements of quality standards for reperfusion therapy precludes detailed comparative effectiveness reporting.
Comparison of primary PCI data with health expenditures as percentage of gross domestic products
The International Survey of Acute Coronary Syndromes (ISACS-TC) project recognized the barriers produced by a lack of information and compiled detailed data concerning the relationship among PHE values and treatment and outcomes of patients with STEMI in some Eastern European countries.48 Comparison of primary PCI data with PHE failed to find a crude relationship between wealth measures and primary PCI provision. Rates of reperfusion therapy by PCI were greater in high PHE hospitals, but 30-day absolute all-cause mortality was around 8% in both low and high PHE hospitals.48 However, the odds of mortality became consistently lower in high PHE compared with low PHE hospitals, when time from symptom onset to admission ≤6 h was included in the analysis (OR: 0.71, 95% CI: 0.56–0.89).48 These data indicate that excessive delay of the invasive treatment reduces the advantages of primary PCI. A network of PCI centres should be supported by an effective and rapid patient transportation system. Timely access to the invasive treatment is more common in high compared with low PHE hospitals.
Supply and demand factors for PCI procedures
The Eurostat data suggest that the number of PCI procedures that are required for a good quality of care is likely to be determined by supply and demand factors (Fig. 5a and Table S12). Most countries in Eastern Europe have relatively reduced supply factors compared with a relatively increased demand.18 This issue is difficult and may be clarified with the following example. Lithuania and France have similar supply factors, namely the rates of PCI (324.3 and 288.7 per 100,000 inhabitants, respectively), but the demand is quite different being the prevalence of IHD much higher in Lithuania than in France (5700 versus 1882 per 100,000 inhabitants).18 Thus, triaging IHD patients with PCI ranges from a proportion of 5.7% in Lithuania to 15.3% in France. It follows that PCI is more frequently undertaken to treat and improve prognosis of IHD in France compared with Lithuania. This may be one reason for a greater reduction in 30-day mortality from acute myocardial infarction in France (5.6%) compared with Lithuania (9.3%) (Fig. 5b).10
Inequalities in risk factors for cardiovascular health
Most of the decline in IHD mortality can be attributed to change in the incidence of the disease, which, in turn, is related to the exposure to modifiable CVD risk factors such as smoking, low physical activity, hypertension, hypercholesterolemia, obesity and diabetes.3,9,49, 50, 51 Changes in mortality trends may also be explained by changes in dietary behaviours such as fruit and vegetable consumption and fat intake.52,53 Earlier findings demonstrated that trends in IHD were partly explained by changes in traditional risk factors (hypertension, hypercholesterolemia, smoking and diabetes). Traditional risk factors accounted for over 70% of the risk of an acute IHD event.54 In this study, therefore, we mainly focused on the established traditional risk factors for which available data are more robust than for other risk factors.54
Smoking
Fig. 6a and Table S13 show the prevalence of smoking from 2005 to 2019 in the populations of the Eastern European countries.55 Among men, the prevalence of smoking was generally highest in the NEE countries. Indeed, in five of the seven NEE countries more than 40% of men are smokers (Moldova: 44.5%, Latvia: 47.6%, Ukraine: 40.7%, Belarus: 41.4% and Russian Federation: 41.5%). Smoking rates were also high in the SEE countries ranging from ranging from 42.6% of Bosnia and Herzegovina to 32.3% of Montenegro). In CEE countries, the smoking rates among men were generally less than 36%. The opposite pattern was true for women, among whom smoking prevalence rates were very low in NEE countries (less than 23% in Moldova, Ukraine, Belarus, Russian Federation, Lithuania, Estonia, and Latvia), low in CEE countries (26.5% in Czechia, 25.4% in Slovakia), and higher in SEE countries (39% in Serbia, 35.6% in Croatia, 31.3% in Montenegro). The current report did not investigate the number of cigarettes smoked and types of cigarettes available, such as low-tar cigarettes, because the systematic Reports of the US Surgeon General have concluded that the use of low-tar and light cigarettes has not influenced the overall disease risk.56 In summary, public heath focus should remain on preventing smoking initiation and facilitating quitting. Although tobacco-related burden in women is lower than in men globally, female smokers are more vulnerable to develop coronary artery disease than their counterparts.57,58 As such, a sex-specific call to action is crucial to raise awareness of the devastating impact of smoking on women's health, especially in SEE countries.
Fig. 6.
Age-standardised prevalence estimates of risk factors stratified by sex. The source of data is the WHO-Global Health Observatory.14,55 Error bars indicate 95% credible intervals. Data are presented as percentages, or percentages (95% credible intervals). Mean total cholesterol (mmol/l) and mean systolic blood pressure (mmHg) levels are presented as means (95% credible intervals). For summary exposure values (SEV)77 the source of data is the 2019 Global Burden of Disease (GBD) study.17 SEV is a measure of a population's exposure to a risk factor that takes into account the extent of exposure by risk level and the severity of that risk's contribution to disease burden. SEV are reported on a scale from 0% to 100%. Error bars indicate 95% uncertainty intervals (UI).
Cholesterol
Trends in serum cholesterol have been of interest for a long time because of the causal association with IHD.59 The WHO Global Health Observatory provides age-standardised national estimates of the prevalence of elevated blood cholesterol levels for several European countries (Fig. 6b and Table S14).14,60 Raised blood cholesterol (6.2 mmol/L) among adults aged 18 years and over tended to be higher in NEE and CEE countries (18.0% in Latvia, 17% in Lithuania, 18.1% in Slovenia, 17.9% in Hungary) and lower in SEE countries (12.1% in Romania, 14.3% in Croatia). In the overall Eastern European countries with the exception of Poland, raised blood cholesterol tended to be more common in women than in men. By contrast, raised blood cholesterol tended to be more common among men than women in Western European countries as shown, for example, by the data presented by Spain (17.1% vs 15.4%). There is not a satisfactory explanation for the large sex related variations in cholesterol level among Western and Eastern European countries and within NEE and CEE versus SEE countries. Researchers have argued that many Eastern European countries are middle-income countries and as such they may have neither the resources nor the infrastructure for a widespread use of statin in prevention therapy, especially among traditionally marginalized groups such as women and those living in rural settings.61 Others have reminded that substantial falls in cholesterol are unlikely to be obtained simply by an increased use of statins.3,62, 63, 64 In 2018, subregions with the highest proportion of statin use included Eastern Europe.65 We therefore believe that unhealthy diets together with lack of physical activity may be the most important determinants of the wide variations in cholesterol levels across sexes and across Eastern European countries.
Diabetes and adiposity
Over the past 8–10 years, the prevalence of diabetes has increased globally across Europe, and in most Eastern European regions. In both men and women, age-standardised fasting raised blood glucose was notably more common in NEE countries compared with CEE and SEE countries (Fig. 6c and Table S15).14,66 The estimated prevalence in men ranged from 8.9% in Lithuania to 7.3% in Romania or Serbia. Among women, the prevalence was highest in Moldova (8.4%) and lowest in Croatia and Slovakia (6.3%). Notably, fasting raised blood glucose was more frequent in men than women in most Eastern European countries with two countries in which this was not the case, both in NEE: Moldova and Russian Federation (Fig. 6c and Table S15). Substantial inequalities also exist with regard to the proportion of adults who are overweight or obese.14,67 The proportion of overweight adults in men (18 years and over, including people with a body mass index [BMI] of more than 25 kg/m2) varied between 59.1% in Bosnia and Herzegovina to 69% in Czechia, while that of the overweight women ranged from 46.6% in Bosnia and Herzegovina to 56.4% in Lithuania (Fig. 6d and Tables S16 and S17). In summary, these data suggest that people of NEE countries are disproportionately affected by diabetes both in women and men and tend to develop this condition at a relatively lower BMI than individuals from CEE and SEE countries. These observations may motivate further studies on diabetic genetics in different ethnic groups.68
Hypertension
Estimates of mean systolic blood pressure (SBP) among adults aged 18 years and above were consistently higher among men than women in all Eastern European countries (Fig. 6e and Table S18).14,69 Mean systolic blood pressure showed regional variations with higher levels generally in NEE and CEE countries and lower levels in SEE countries. For example, in men the mean systolic blood pressure ranged from 130 mmHg in Russian Federation to 138 mmHg in Slovenia, while in women it ranged from approximately 130 mm Hg in Moldova, Albania, Bosnia and Herzegovina and Ukraine to 120 mmHg in Slovakia. Previous work has shown that a 1 mmHg population-wide SBP reduction is associated with 13.3 fewer heart failure events per 100,000 person-years in white populations.70 As such population-wide interventions to reduce blood pressure in NEE and CEE countries are urgently required. Little is known about the causes for different trends in blood pressure. Drivers probably include reduced salt, intake, increased consumption of fruits and vegetables that are sources of potassium, and the use of antihypertensive treatments in older people.3
Psycho-socio-economic determinants of cardiovascular health
Psychosocial factors may increase the risk of CVD, but relatively few studies on this issue have been undertaken in Eastern Europe. The HAPIEE (Health, Alcohol and Psychosocial factors In Eastern Europe) study is a cohort study that assessed the effects of dietary factors, alcohol consumption and psychosocial factors on the health of men and women aged 45–69 years in four countries of Central and Eastern Europe (Czechia, Lithuania, Poland and Russian Federation). The study found that people who were unemployed, single, with less wealth, who have no social life with friends and relatives, and who are depressed were more likely to die from CVD.71 This study also found that these social stress factors were independent of one another. Another study with data collected in Lithuania within the framework of the HAPIEE registry suggested an independent association between psychological stress and outcomes in overweight and obese people.72 However, the HAPIEE study was unable to clarify why death from IHD is more common in Russian Federation, when compared to lower rates of mortality in Central European countries. Many socioeconomic variables are associated with psychosocial factors, including income level, education level and ethnicity. How these factors should be assessed and quantified in a reliable and reproducible manner across different countries remains to be determined.
Addressing health inequalities in ischemic heart disease mortality in Eastern Europe
The MONICA Project73 was initiated to assess prospectively the influence of changes in major risk factors on variation in IHD mortality in the 1980s and early 1990s in 21 countries (Box 1).73 The IHD death rates declined in most MONICA Western European sites, by an average of 2.7% per year in men and 2.1% per year in women, although they unexpectedly rose in most Eastern European countries.74 Our report indicates that health inequalities and inequities in access to cardiovascular healthcare still persist both between the Western and Eastern European countries and within the Eastern European countries. It is important, therefore, to refocus research towards regional differences into cardiovascular care.
Box 1. The MONICA Project.
-
•
The WHO Multinational MONItoring of Trends and Determinants in CArdiovascular Disease (MONICA) project aimed to prospectively evaluate the impact of trends in major risk factors for cardiovascular disease—including blood pressure, cigarette smoking and serum cholesterol, and later BMI—and in 28-day case-fatality on change in IHD mortality.73
-
•
IHD risk factors, incidence, case fatality, and mortality were measured in 38 communities in 21 countries, mainly in Europe but also in Australia, China, and North America. Data for the main study were collected for a period of ten years or more in each centre, from the early 1980s to the mid-1990s.73
-
•
The focus was on premature mortality, which at that time was defined as death in people aged <65 years. There are enormous differences between different populations. In men, Glasgow in the United Kingdom and North Karelia in Finland have eight to ten times the coronary event rate of Beijing in China. Similarly, among women, Glasgow has roughly ten times the rate of Beijing and Toulouse in France.75
Conclusions
There is an urgent need for improved analysis and reporting of data to describe the determinants of cardiovascular health across Europe, and an ongoing need for interventions able to tackle to cardiovascular health inequalities (Box 2, Box 3). One major limitation is the significant heterogeneity in healthcare systems, socioeconomic conditions, and cultural practices across Eastern European countries. A better understanding of the causes of the inequalities in IHD risk in the Eastern European countries will not only help to mitigate the unequal burden of IHD, but also enable the identification of new causative pathways that are relevant to IHD risk for the population and the communities at large. Policies may need to be tailored to individual countries rather than applying a one-size-fits-all approach.
Box 2. Recommendations to reduce disparities in cardiovascular care and outcomes in Eastern Europe.
-
•
Nationwide cardiovascular care registries
We recommend the collection and reporting of systematic population-based data and nationwide registry data to improve our understanding of why the West-East gap in IHD mortality continues in Europe, and to document its variations within the Eastern European countries.
-
•
International cardiac networks
There is inter-country variation in cardiovascular care delivery, which cannot be captured only by nationwide registry data. Our data support the recommendation from the EUR-Observational Research Programme (EORP) that networks of hospitals should work together in terms of action at international level. There is a need for comparisons and for dedicated, collaborative research.
-
•
Inequalities for ethnic and/or geographic areas
There are vulnerable groups in specific geographic areas. Significant disparities in age-standardised IHD mortality rates are present between NEE and CEE or SEE countries. The NEE countries face multiple barriers to access cardiovascular health care and therefore do not obtain the care they need. Globalization seems to have contributed to a higher prevalence of cardiovascular risk factors in NEE countries. Access to and delivery of equitable primary prevention strategies and implementation of public health policies are of upmost importance in these countries to reduce IHD mortality.
-
•
Inequalities by age and sex
A woman in Lithuania is 11 times more likely to die from IHD than a woman in France, while for men the gap is 8 times. Slovakia has one of the highest women to men ratios of death after IHD (1.56). By contrast, the women to men rate ratio of death in Spain is the lowest in Europe (0.77). Countries in Eastern Europe have a much lower life expectancy compared with the rest of Europe with a difference of approximately 10 years between with the lowest and highest life expectancy. Knowledge on specific subgroups, such as women and older people in regions with higher cardiovascular mortality, may provide a basis for regional designing of cardiovascular risk management and prevention strategies aimed at improving health equity.
Box 3. Specific health care reforms recently implemented or planned in some Eastern European countries76.
-
•
Increase of the overall budget for the health system (Czechia, Estonia, Latvia and Poland).
-
•
Improved access to primary care (Poland, Romania).
-
•
Improved waiting list management (Hungary, Lithuania, Latvia, North Macedonia Slovenia).
-
•
Improved access to health promotion and disease prevention for specific vulnerable groups (Estonia, Romania).
Contributors
EC and RB conceived of the study. EC, OM and RB and planned the methodology, that was reviewed by all authors. EC, OM, NF and RB conducted the search. EC, OM, NF and RB reviewed the literature and conducted the analysis. EC and RB wrote the original draft of the paper. EC, OM and NF produced the manuscript figures and tables. EC, OM, NF, MD, SK, DM, ZV and RB participated in the interpretation, reviewing and editing drafts and critically revised the manuscript for intellectual content.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
No specific funding was received for the preparation of this manuscript. The authors declare no conflicts of interest.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanepe.2023.100698.
Appendix A. Supplementary data
References
- 1.World Health Organization The global health observatory. Global health estimates: life expectancy and leading causes of death and disability. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death Available at:
- 2.Lindstrom M., DeCleene N., Dorsey H., et al. Global burden of cardiovascular diseases and risks collaboration, 1990-2021. J Am Coll Cardiol. 2022;80(25):2372–2425. doi: 10.1016/j.jacc.2022.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Ezzati M., Obermeyer Z., Tzoulaki I., Mayosi B.M., Elliott P., Leon D.A. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol. 2015;12(9):508–530. doi: 10.1038/nrcardio.2015.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations Statistics Division (UNSD) https://unstats.un.org/unsd/methodology/m49/ Avaiable at:
- 5.Romaniuk P., Szromek A.R. The evolution of the health system outcomes in Central and Eastern Europe and their association with social, economic and political factors: an analysis of 25 years of transition. BMC Health Serv Res. 2016;16:95. doi: 10.1186/s12913-016-1344-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bovet P., Paccaud F. Cardiovascular disease and the changing face of global public health: a focus on low and middle income countries. Publ Health Rev. 2011;33(2):397–415. [Google Scholar]
- 7.The World Bank World Bank country and lending groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- 8.World Health Organization Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 Avaiable at:
- 9.Harper S., Lynch J., Smith G.D. Social determinants and the decline of cardiovascular diseases: understanding the links. Annu Rev Public Health. 2011;32:39–69. doi: 10.1146/annurev-publhealth-031210-101234. [DOI] [PubMed] [Google Scholar]
- 10.OECD/European Union. Health at a Glance: Europe 2022: State of Health in the EU Cycle. OECD Publishing; Paris: 2022. [Google Scholar]
- 11.The World Bank World Bank open data. https://data.worldbank.org/
- 12.The world factbook. https://www.cia.gov/the-world-factbook/
- 13.World Health Organization. Global Health Observatory data repository. Current health expenditure (CHE) as percentage of gross domestic product (GDP) (%). https://apps.who.int/gho/data/node.main.GHEDCHEGDPSHA2011?lang=en. Accessed February 5, 2023.
- 14.World Health Organization The global health observatory. Noncommunicable diseases: risk factors. https://www.who.int/data/gho/data/themes/topics/noncommunicable-diseases-risk-factors
- 15.World Health Organization European health information gateway. Health 2020 indicators database. https://gateway.euro.who.int/en/datasets/health-2020-indicators/
- 16.World Health Organization. European health information gateway. European mortality database. https://gateway.euro.who.int/en/datasets/european-mortality-database/. Accessed February 10, 2023.
- 17.2019 Global burden of disease (GBD) study. https://vizhub.healthdata.org/gbd-results/
- 18.Eurostat Health care database. https://ec.europa.eu/eurostat/web/health/data/database
- 19.Wilkins E.W.L., Wickramasinghe K., Bhatnagar P., et al. European Heart Network; Brussels: 2017. European cardiovascular disease Statistics 2017.https://ehnheart.org/cvd-statistics.html Available at: [Google Scholar]
- 20.Ahmad O.B., Boschi-pinto C., Lopez A.D. World Health Organization; 2001. Age standardization of rates: a new WHO standard. GPE discussion paper series: No.31.https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf chrome-extension. [Google Scholar]
- 21.Eurostat. https://ec.europa.eu/eurostat/
- 22.European Commission . Publications Office; 2010. Directorate-general for employment, social affairs and inclusion, reducing health inequalities in the European union.https://data.europa.eu/doi/10.2767/96086 [Google Scholar]
- 23.Bruthans J., Cifkova R., Lanska V., et al. Explaining the decline in coronary heart disease mortality in the Czech Republic between 1985 and 2007. Eur J Prev Cardiol. 2014;21(7):829–839. doi: 10.1177/2047487312469476. [DOI] [PubMed] [Google Scholar]
- 24.Bandosz P., O'Flaherty M., Drygas W., et al. Decline in mortality from coronary heart disease in Poland after socioeconomic transformation: modelling study. BMJ. 2012;344:d8136. doi: 10.1136/bmj.d8136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization Glossary of terms used for health impact assessment (HIA) https://www.who.int/publications/m/item/glossary-of-terms-used-for-health-impact-assessment-hia Available at:
- 26.Mathers C.D., Stevens G.A., Boerma T., White R.A., Tobias M.I. Causes of international increases in older age life expectancy. Lancet. 2015;385(9967):540–548. doi: 10.1016/S0140-6736(14)60569-9. [DOI] [PubMed] [Google Scholar]
- 27.Stringhini S., Carmeli C., Jokela M., et al. Socioeconomic status and the 25 x 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet. 2017;389(10075):1229–1237. doi: 10.1016/S0140-6736(16)32380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schroder S.L., Richter M., Schroder J., Frantz S., Fink A. Socioeconomic inequalities in access to treatment for coronary heart disease: a systematic review. Int J Cardiol. 2016;219:70–78. doi: 10.1016/j.ijcard.2016.05.066. [DOI] [PubMed] [Google Scholar]
- 29.Wenger N.K., Lloyd-Jones D.M., Elkind M.S.V., et al. Call to action for cardiovascular disease in women: epidemiology, awareness, access, and delivery of equitable health care: a presidential advisory from the American heart association. Circulation. 2022;145(23):e1059–e1071. doi: 10.1161/CIR.0000000000001071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Poon S., Goodman S.G., Yan R.T., et al. Bridging the gender gap: insights from a contemporary analysis of sex-related differences in the treatment and outcomes of patients with acute coronary syndromes. Am Heart J. 2012;163(1):66–73. doi: 10.1016/j.ahj.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 31.Bugiardini R., Yan A.T., Yan R.T., et al. Factors influencing underutilization of evidence-based therapies in women. Eur Heart J. 2011;32(11):1337–1344. doi: 10.1093/eurheartj/ehr027. [DOI] [PubMed] [Google Scholar]
- 32.Bugiardini R., Estrada J.L., Nikus K., Hall A.S., Manfrini O. Gender bias in acute coronary syndromes. Curr Vasc Pharmacol. 2010;8(2):276–284. doi: 10.2174/157016110790887018. [DOI] [PubMed] [Google Scholar]
- 33.Vasiljevic-Pokrajcic Z., Mickovski N., Davidovic G., et al. Sex and age differences and outcomes in acute coronary syndromes. Int J Cardiol. 2016;217(Suppl):S27–S31. doi: 10.1016/j.ijcard.2016.06.217. [DOI] [PubMed] [Google Scholar]
- 34.He J., Gu D., Wu X., et al. Major causes of death among men and women in China. N Engl J Med. 2005;353(11):1124–1134. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 35.Ford E.S., Ajani U.A., Croft J.B., et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356(23):2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 36.Bhatt D.L., Roe M.T., Peterson E.D., et al. Utilization of early invasive management strategies for high-risk patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. JAMA. 2004;292(17):2096–2104. doi: 10.1001/jama.292.17.2096. [DOI] [PubMed] [Google Scholar]
- 37.Fox K.A., Steg P.G., Eagle K.A., et al. Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006. JAMA. 2007;297(17):1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- 38.Vasiljevic Z., Mickovski-Katalina N., Krljanac G., et al. Coronary care unit and primary percutaneous coronary intervention networks improve the standard of care: reperfusion therapy in ST elevation myocardial infarction in Serbia from 2002 to 2008. J Cardiovasc Med (Hagerstown) 2011;12(4):300–302. doi: 10.2459/JCM.0b013e328343e9f2. [DOI] [PubMed] [Google Scholar]
- 39.Cenko E., Ricci B., Kedev S., et al. Reperfusion therapy for ST-elevation acute myocardial infarction in Eastern Europe: the ISACS-TC registry. Eur Heart J Qual Care Clin Outcomes. 2016;2(1):45–51. doi: 10.1093/ehjqcco/qcv025. [DOI] [PubMed] [Google Scholar]
- 40.Smith F.G., Brogan R.A., Alabas O., et al. Comparative care and outcomes for acute coronary syndromes in Central and Eastern European Transitional countries: a review of the literature. Eur Heart J Acute Cardiovasc Care. 2015;4(6):537–554. doi: 10.1177/2048872614551545. [DOI] [PubMed] [Google Scholar]
- 41.Bugiardini R., Manfrini O., Majstorovic Stakic M., et al. Exploring in-hospital death from myocardial infarction in eastern Europe: from the international registry of acute coronary syndromes in transitional countries (ISACS-TC); on the behalf of the working group on coronary pathophysiology & microcirculation of the European society of cardiology. Curr Vasc Pharmacol. 2014;12(6):903–909. doi: 10.2174/157016111206141210122150. [DOI] [PubMed] [Google Scholar]
- 42.Benedek I., Gyongyosi M., Benedek T. A prospective regional registry of ST-elevation myocardial infarction in Central Romania: impact of the Stent for Life Initiative recommendations on patient outcomes. Am Heart J. 2013;166(3):457–465. doi: 10.1016/j.ahj.2013.03.033. [DOI] [PubMed] [Google Scholar]
- 43.Kristensen S.D., Laut K.G., Fajadet J., et al. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011: current status in 37 ESC countries. Eur Heart J. 2014;35(29):1957–1970. doi: 10.1093/eurheartj/eht529. [DOI] [PubMed] [Google Scholar]
- 44.Ganova-Iolovska M., Kalinov K., Geraedts M. Quality of care of patients with acute myocardial infarction in Bulgaria: a cross-sectional study. BMC Health Serv Res. 2009;9:15. doi: 10.1186/1472-6963-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hall M., Cenko E., Bueno H., Gale C.P. Contemporary roles of registries in clinical cardiology: insights from Western and Eastern European countries. Int J Cardiol. 2016;217(Suppl):S13–S15. doi: 10.1016/j.ijcard.2016.06.220. [DOI] [PubMed] [Google Scholar]
- 46.Tatu-Chitoiu G., Cinteza M., Dorobantu M., et al. In-hospital case fatality rates for acute myocardial infarction in Romania. CMAJ. 2009;180(12):1207–1213. doi: 10.1503/cmaj.081227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zeymer U., Ludman P., Danchin N., et al. Reperfusion therapies and in-hospital outcomes for ST-elevation myocardial infarction in Europe: the ACVC-EAPCI EORP STEMI registry of the European society of cardiology. Eur Heart J. 2021;42(44):4536–4549. doi: 10.1093/eurheartj/ehab342. [DOI] [PubMed] [Google Scholar]
- 48.Bugiardini R., Badimon L., Investigators I-T, Coordinators The international Survey of acute coronary syndromes in transitional countries (ISACS-TC): 2010-2015. Int J Cardiol. 2016;217(Suppl):S1–S6. doi: 10.1016/j.ijcard.2016.06.219. [DOI] [PubMed] [Google Scholar]
- 49.Laatikainen T., Critchley J., Vartiainen E., Salomaa V., Ketonen M., Capewell S. Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol. 2005;162(8):764–773. doi: 10.1093/aje/kwi274. [DOI] [PubMed] [Google Scholar]
- 50.Unal B., Critchley J.A., Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation. 2004;109(9):1101–1107. doi: 10.1161/01.CIR.0000118498.35499.B2. [DOI] [PubMed] [Google Scholar]
- 51.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Manfrini O., Bugiardini R. Behavioural risk factors and cardiovascular disease: are women at higher risk? Lancet. 2022;400(10355):788–789. doi: 10.1016/S0140-6736(22)01736-6. [DOI] [PubMed] [Google Scholar]
- 53.Walli-Attaei M., Rosengren A., Rangarajan S., et al. Metabolic, behavioural, and psychosocial risk factors and cardiovascular disease in women compared with men in 21 high-income, middle-income, and low-income countries: an analysis of the PURE study. Lancet. 2022;400(10355):811–821. doi: 10.1016/S0140-6736(22)01441-6. [DOI] [PubMed] [Google Scholar]
- 54.Greenland P., Knoll M.D., Stamler J., et al. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA. 2003;290(7):891–897. doi: 10.1001/jama.290.7.891. [DOI] [PubMed] [Google Scholar]
- 55.World Health Organization European health for all database (HFA-DB) https://gateway.euro.who.int/en/datasets/european-health-for-all-database/
- 56.U.S. Department of Health and Human Services . The health consequences of smoking: 50 years of progress. A report of the surgeon general. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2014. [Google Scholar]
- 57.Manfrini O., Yoon J., van der Schaar M., et al. Sex differences in modifiable risk factors and severity of coronary artery disease. J Am Heart Assoc. 2020;9(19) doi: 10.1161/JAHA.120.017235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vasiljevic Z., Scarpone M., Bergami M., et al. Smoking and sex differences in first manifestation of cardiovascular disease. Atherosclerosis. 2021;330:43–51. doi: 10.1016/j.atherosclerosis.2021.06.909. [DOI] [PubMed] [Google Scholar]
- 59.Keys A. Coronary heart disease--the global picture. Atherosclerosis. 1975;22(2):149–192. doi: 10.1016/0021-9150(75)90001-5. [DOI] [PubMed] [Google Scholar]
- 60.NCD Risk Factor Collaboration (NCD-RisC). Repositioning of the global epicentre of non-optimal cholesterol. Nature. 2020;582(7810):73–77. doi: 10.1038/s41586-020-2338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Marcus M.E., Manne-Goehler J., Theilmann M., et al. Use of statins for the prevention of cardiovascular disease in 41 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data. Lancet Glob Health. 2022;10(3):e369–e379. doi: 10.1016/S2214-109X(21)00551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bradley C.K., Wang T.Y., Li S., et al. Patient-reported reasons for declining or discontinuing statin therapy: insights from the PALM registry. J Am Heart Assoc. 2019;8(7) doi: 10.1161/JAHA.118.011765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Capewell S., Ford E.S. Why have total cholesterol levels declined in most developed countries? BMC Public Health. 2011;11:641. doi: 10.1186/1471-2458-11-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Luksiene D., Tamosiunas A., Baceviciene M., et al. Trends in prevalence of dyslipidaemias and the risk of mortality in Lithuanian urban population aged 45-64 in relation to the presence of the dyslipidaemias and the other cardiovascular risk factors. PLoS One. 2014;9(6) doi: 10.1371/journal.pone.0100158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Blais J.E., Wei Y., Yap K.K.W., et al. Trends in lipid-modifying agent use in 83 countries. Atherosclerosis. 2021;328:44–51. doi: 10.1016/j.atherosclerosis.2021.05.016. [DOI] [PubMed] [Google Scholar]
- 66.NCD Risk Factor. Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Replication DIG, Meta-analysis C, Asian Genetic Epidemiology Network Type 2 Diabetes C, et al. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat Genet. 2014;46(3):234–244. doi: 10.1038/ng.2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hardy S.T., Loehr L.R., Butler K.R., et al. Reducing the blood pressure-related burden of cardiovascular disease: impact of achievable improvements in blood pressure prevention and control. J Am Heart Assoc. 2015;4(10) doi: 10.1161/JAHA.115.002276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tillmann T., Pikhart H., Peasey A., et al. Psychosocial and socioeconomic determinants of cardiovascular mortality in Eastern Europe: a multicentre prospective cohort study. PLoS Med. 2017;14(12) doi: 10.1371/journal.pmed.1002459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Luksiene D., Tamosiunas A., Radisauskas R., Bobak M. The prognostic value of combined status of body mass index and psychological well-being for the estimation of all-cause and CVD mortality risk: results from a long-term cohort study in Lithuania. Medicina (Kaunas) 2022;58(11):1591. doi: 10.3390/medicina58111591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41(2):105–114. doi: 10.1016/0895-4356(88)90084-4. [DOI] [PubMed] [Google Scholar]
- 74.Tunstall-Pedoe H., Kuulasmaa K., Mahonen M., Tolonen H., Ruokokoski E., Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;353(9164):1547–1557. doi: 10.1016/s0140-6736(99)04021-0. [DOI] [PubMed] [Google Scholar]
- 75.Luepker R.V. WHO MONICA project: what have we learned and where to go from here? Publ Health Rev. 2011;33(2):373–396. [Google Scholar]
- 76.Baeten R., Spasova S., Vanhercke B., Coster S. Inequalities in access to healthcare. A study of national policies, European social policy network (ESPN), brussels: European commission. 2018. https://ec.europa.eu/social/main.jsp?catId=738&langId=en&pubId=8152&furtherPubs=yes Available at:
- 77.GBD 2019 Risk Factors Collaborators Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.