Abstract
[Purpose]
Continuous glucose monitoring (CGM) is on the rise as the prevalence of obesity and diabetes increases. This review aimed to explore the use of CGM and its potential novel applications in physical activity and nutrition management.
[Methods]
We searched PubMed, Web of Science, and Wiley Online Library databases using the keywords ‘continuous glucose monitor,’ ‘nutrition,’ ‘physical activity,’ and ‘numerical modeling.’
[Results]
Continuous blood glucose measurement is useful for individuals with obesity and diabetes. Long-term blood glucose data allow for personalized planning of nutritional composition, meal timing, and physical activity type and intensity, as well as help prevent hypoglycemia and hyperglycemia. Thus, understanding the limitations of CGM is important for its effective use.
[Conclusion]
CGM systems are being increasingly used to monitor and identify appropriate blood glucose controlling interventions. Blood glucose level is influenced by various factors such as nutrient composition, meal timing, physical activity, circadian rhythm, and cortisol levels. Numerical modeling can be used to analyze the complex relationship between stress, sleep, nutrition, and physical activity, which affect blood glucose levels. In future, blood glucose, sleep, and stress data will be integrated to predict appropriate lifestyle levels for blood glucose management. This integrated approach improves glucose control and overall wellbeing, potentially reducing societal costs.
Keywords: blood glucose, continuous glucose monitoring, data, diabetes, numerical modeling, obesity
INTRODUCTION
According to the energy balance concept, obesity is the accumulation of excess body fat as a result of an imbalance between calorie intake and calorie expenditure [1]. Obesity is an important public health issue because it can cause various health problems such as diabetes [2], high blood pressure [3,4], heart disease [5,6], stroke [7,8], and some cancers [9-11] as well as also be associated with physical limitations [12], poor quality of life (QOL) [13], and increased mortality risk [14,15]. World Health Organization (WHO) has recognized obesity as a global health crisis that affects people of all ages, sexes, and socioeconomic statuses [16]. The worldwide prevalence of obesity continues to rise and more than half of the global population is expected to become obese by 2030 [17].
Obesity rate has increased in South Korea as well, owing to changes in lifestyle and dietary habits. According to the 2018 Korea National Health and Nutrition Examination Survey, obesity and diabetes rates in South Korea were 35.7% and 14.4%, respectively [18]. In 2020, approximately 40% adults were classified as overweight or obese [19]. Current lifestyle, characterized by decreased physical activity, increased evening activity, and poor dietary habits, causes serious problems by promoting energy imbalance, which increases obesity and diabetes risk [20].
Insulin, a hormone produced by beta cells in the pancreas, plays a pivotal role in regulating blood glucose levels [21]. Insulin regulates blood sugar levels by stimulating glucose uptake from the bloodstream into cells, where it is utilized as energy or stored as glycogen. Insulin also prevents the liver from releasing excess glucose into blood [22]. The normal fasting blood glucose level range (measured after at least 8 h without food) is typically 70–100 mg/dL or 3.9–5.6 mmol/L [23]. Blood glucose levels measured 2 h after eating (postprandial) should not exceed 140 mg/dL (7.8 mmol/L). Individuals with obesity often experience type 1 or 2 diabetes, which are characterized by insufficient insulin production or decreased insulin sensitivity, respectively [24]. Thus, glucose control and improved insulin sensitivity are crucial in individuals with obesity, diabetes, and metabolic disorders [25,26]. Consistent high (hyperglycemia) or low (hypo-glycemia) sustained blood glucose levels have serious health consequences. Hyperglycemia causes diabetes, cardiovascular disease, and kidney disease [27,28]. Moreover, severe hypoglycemia causes consciousness loss, seizures, and even death if not treated immediately [29,30]. Frequent hypoglycemia also reduces an individual’s quality of life, as it can cause anxiety, fear of hypoglycemia, and avoidance of physical activity or social circumstances [31]. Both hyperglycemia and hypoglycemia causes cognitive impairment, which can affect concentration, memory, and decision making [32,33], as well as contribute to mood disorders, such as mood swings, irritability, and depression [34]. As the prevalence of obesity-related diseases increases, it becomes more important to find effective ways to manage blood glucose levels before they become diseased.
Continuous glucose monitoring (CGM) has resulted in a new era of blood glucose measurements and provides real-time insights into blood glucose levels [35]. It involves using small sensors under the skin to continuously measure glucose levels in the interstitial fluid surrounding cells [36,37]. The measurements are then transmitted to a receiver or smartphone application, which allows the individual to monitor glucose levels in real time. CGM has become increasingly important in blood glucose management as the prevalence of diabetes increases [38,39]. The technical and clinical use of CGM has been widely reviewed [40-45]. However, no reviews have focused on how their use in physical activity and nutrition management and their possible future applications. This review aimed to analyze how CGM has been used in physical activity and nutrition management and suggest possible future applications based on numerical modeling.
EXPLORING THE ROLE OF CGM IN PHYSICAL ACTIVITY AND NUTRITION MANAGEMENT
Unveiling the Vital Role: Importance of CGM Data
CGM data play an important role in diabetes management by providing valuable insights into blood glucose levels [46]. This continuous real-time information, collected every 1–15 min, is critical for individuals with diabetes [47].
CGM allows an understanding of blood glucose trends over long time periods such as hours, days, and even weeks [48,49]. CGM data can be used to understand how different factors, such as nutritional choices, physical activity, stress, and medication use, affect blood glucose levels [50-52]. Alerts to low or high blood glucose levels allow individuals to take immediate action to prevent rapid fluctuations in blood sugar [53]. It also evaluates the ratio of time spent within a pre-defined target blood glucose range, giving an excellent picture of blood glucose level maintenance within the recommended range (time-in-range; TIR) [54-57]. These findings provide a foundation for personalized therapeutic interventions. The impact of different foods on blood glucose levels can be observed using CGM [58]. By measuring the postprandial blood glucose changes in detail, individuals can make data-driven decisions regarding meal composition and timing, leading to balanced and manageable blood glucose control.
Physical activity should be performed with care, particularly for people with diabetes because of the response of blood glucose levels to physical activity [59]. The effect of physical activity on blood glucose levels can be tracked using CGM. With CGM data, exercise routines and insulin doses can be fine-tuned to reduce exercise-induced blood glucose fluctuations and achieve consistent glucose management. CGM can help identify overnight blood glucose trends and help users determine the need for insulin adjustments [60]. This proactive approach can minimize the risk of nighttime hypoglycemia or hyperglycemia, thereby ensuring restful and safe sleep. CGM data can also be used to promote discussions with medical professionals at the point-of-care about appropriate treatment strategies and adjustments [61]. This will help to effectively improve overall diabetes management and personalize treatment plans to meet individual needs.
CGM Use for Enhancing Nutrition Insights
CGM is useful for understanding the complex relationship between nutrition, obesity, and diabetes.
This reveals how different foods and dietary patterns affect people with obesity. It is not the only solution for obesity management, but CGM can help analyze metabolic response to different foods and inform nutritional choices [62]. The effects on blood glucose differ for each individual and are influenced by several factors, such as genetics, metabolism, metagenomics, and diet. Therefore, personalized guidance may be more appropriate than one-size-fits-all impact guidelines [63]. A study comparing the effects of brown rice (BR) and white rice (WR) on 24 h glycemic and insulinemic responses of overweight Asian Indians found that BR consumption reduces the risk of diabetes and related complications by reducing 24 h glucose and fasting insulin responses [64]. This study suggests that BR is a healthier alternative to WR. CGM data can show how a particular meal affects blood glucose levels over time, allowing the design of a diet to promote blood glucose stability and prevent rapid blood glucose changes. Carbohydrate intake should be adjusted to manage blood glucose fluctuations owing to the complex relationship between the carbohydrates in different foods and blood glucose levels [64]. The pilot study explored the feasibility and safety of time-limited eating (TLE) combined with CGM in adolescents with obesity [65]. This study found high adherence to TLE and CGM with no significant differences in weight loss, energy intake, quality of life, or eating behavior [65]. This study found that intra-individual variability in nutrition-related lifestyle behaviors, such as meal timing, eating windows, food intake, movement behaviors, sleep conditions, and body weight, was significantly correlated with mean blood glucose levels66. Long sedentary period and total sleep duration are associated with glucose variability. Earlier dinners and shorter eating windows improve glucose control [66]. An effective weight management strategy can be developed by optimizing nutrient intake and meal timings based on glucose response.
CGM is also useful in assessing the relationship between glucose control and nutrition in individuals with diabetes [67]. This can help fine-tune insulin doses to match carbohydrate intake [68-70]. CGM data can help guide the timing of mealtime insulin doses, helping timely insulin administration to prevent postprandial blood glucose spikes [71-73]. This study investigated the effects of carbohydrate distribution on postprandial glucose peaks in individuals with type 2 diabetes [74]. Twenty-three participants were randomly assigned to four interventions, each with varying carbohydrate content. The results showed that even carbohydrate distribution did not enhance blood glucose control, although a carbohydrate lunch offered an optimal postprandial profile. This study examined for how high glycemic index (HGI) and low glycemic index (LGI) meals affected blood glucose levels in youths with type 1 diabetes [75]. The results showed low daytime mean blood glucose, blood glucose area (>180 mg/dL), and high blood glucose index when consuming LGI meals, but no differences in daytime blood glucose area (<70 mg/dL) between HGI and LGI [75]. Similar to obesity, people with diabetes can use CGM data to analyze the impact of meals on blood glucose levels, which can be used to guide nutritional composition.
CGM Use for Optimizing Physical Activity
CGM helps us understand the impact of physical activity on obesity and diabetes management.
The CGM provides data on how physical activity type and intensity affect blood glucose levels in people with obesity. This study compared the effects of high-intensity interval training (HIIT) and continuous moderate-intensity exercise on postprandial hyperglycemia in overweight or obese adults [76]. The results showed that HIIT significantly reduced the incremental area under the curve after dinner and postprandial glucose spikes after breakfast, suggesting that HIIT has a prolonged effect on postprandial hyperglycemia. CGM data can reveal the relationship between different forms of physical activity and glucose levels [76-78]. Thus, one can choose a physical activity that helps maintain stable glucose levels and avoid rapid glucose fluctuations, particularly in people with insulin resistance due to obesity [79]. This study investigated hypoglycemia during moderate-intensity exercise in non-obese and obese individuals with and without type 2 diabetes [80]. The results showed elevated glucose responses and high decrease in glucose concentration during the evening exercise. Obese males had high insulin drops. Moderate-intensity exercise decrease glucose concentrations; however, many remain asymptomatic [80]. Proper physical activity and meal timing around physical activity can also be planned based on CGM data. Pre-workout meals or snacks should be adjusted based on blood glucose levels to optimize energy levels and avoid glucose imbalance during physical activity. The insights gained from CGM can help plan physical activities to improve overall well-being.
CGM is also useful in people with diabetes. This study examined the effects of structured exercise on glucose levels in adults with type 2 diabetes [81]. The results showed that both acute and chronic exercise can improve 24 h glucose profiles, and the timing of exercise and participant sex influence the heterogeneity of acute glycemic improvements [81]. This can help make informed decisions about physical activity and timing based on CGM data. This systematic review examined the effects of exercise on glycemic control in type 2 diabetes [82]. According to a meta-analysis of 11 studies focusing on postprandial glucose, exercise significantly decreased average glucose concentrations and time spent in hyperglycemia, but did not affect the daily time spent in hypoglycemia or fasting glucose [82]. Physical exercise is crucial for managing type 1 diabetes; however, acute exercise increases the risk of dysglycemia [83]. The fear of hypoglycemia is a barrier to exercise. CGM and intermittently scanned CGM (isCGM) systems can help manage glycemic during exercise [83] and determine when to adjust the insulin dose before exercise, based on the glucose levels and expected effects of exercise. Since muscles become insulin-sensitive, this period is critical for optimizing glycemic control [84-87].
Recognizing Constraints: Limitations
CGM has made great progress in diabetes management; however, its limitations are similar to those of other technologies. Thus, its limitations should be understood for effective data utilization and analysis. The accuracy of CGM has improved over time compared to that of traditional fingerstick method for blood glucose measurement, but it still exists [88-90]. As CGM sensors measure glucose levels in the interstitial fluid, they may not accurately match blood glucose levels, particularly when glucose level changes rapidly, such as after a meal or during exercise [89]. There might be a slight latency between blood glucose level changes and blood glucose readings with CGM, which affects the timing of appropriate interventions during rapid blood glucose fluctuations; therefore, it is important to be aware of this [91]. Most CGM systems should be calibrated periodically using fingerstick measurements as inaccurate or infrequent calibration can affect data reliability [92-95]. Attaching a sensor to the CGM can be inconvenient [96]. Some individuals may experience difficulty in applying the sensor or irritation at the sensor site [43,97]. Skin reactions such as rash, itching, or inflammation may occur at the sensor attachment site with prolonged CGM sensor use. CGM use requires active user participation in sensor attachment, calibration, and data analysis. There may be inaccurate results owing to user errors or inappropriate procedures. Constant data stream from CGM devices can be stressful for some people. Constant monitoring and analysis causes “data fatigue” [98,99]. Technical issues with CGM devices, such as sensor failure or synchronization, can disrupt data collection and affect usability [100,101].
PERSPECTIVE ON THE FUTURE
Many institutions use CGM systems to monitor and identify appropriate interventions and possible applications. Researchers are also working to develop a noninvasive CGM102. The CGM era is dawning and substantial changes are expected in the future. CGM should be used to monitor feedback changes in blood glucose levels over time. However, very little work has been done to analyze and apply numerical modeling to CGM-generated data. The CGM data should be analyzed to develop possible numerical modeling techniques and prediction techniques to prepare for the future.
Figure 1.
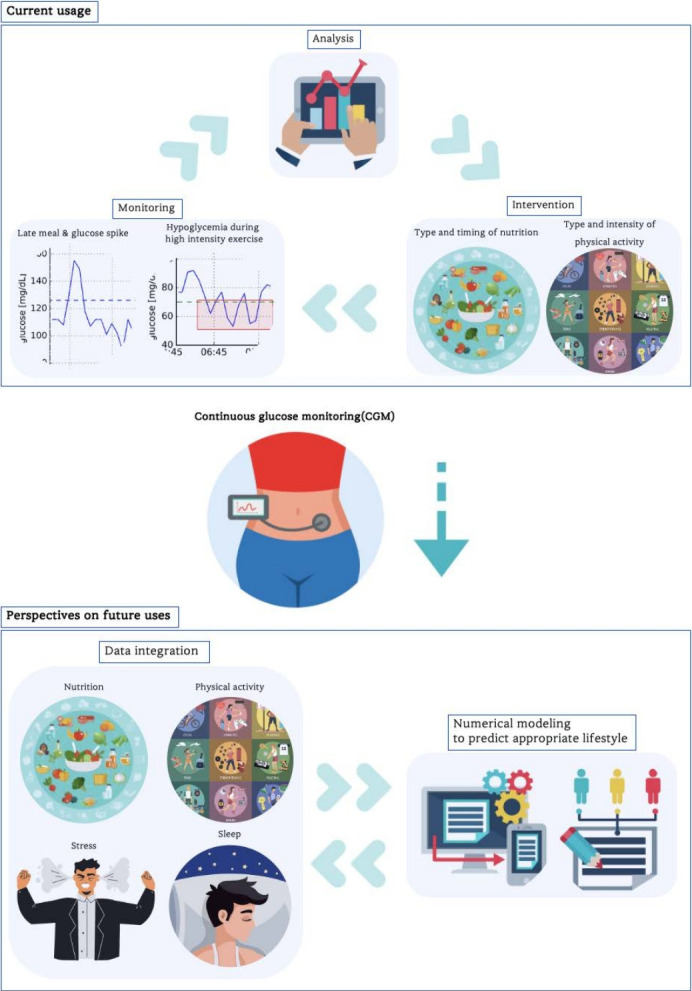
Illustration of perspectives on the current and potential use of continuous glucose monitoring.
Blood glucose is not simply the conversion of food into sugar; it is influenced by many factors, such as nutrient composition, meal timing, the presence or absence of physical activity, circadian rhythms, and cortisol levels, and therefore requires a systematic approach [103-106]. Wearable devices are ubiquitous, can track sleep patterns, and provide data on stress levels, such as heart rate variability. Stress disrupts sleep patterns, reduces sleep quality, and alters sleep duration. Sleep disruption can eventually affect glucose metabolism and regulate blood glucose levels. Numerical modeling, also known as computational or mathematical modeling, uses mathematical equations and computer simulations to represent and analyze complex real-world systems, phenomena, or processes. Numerical modeling can be used to analyze the complex relationships among stress, sleep, nutrition, and physical activity, which affect blood glucose levels. Currently, CGM data are used independently; however, in the future, blood glucose, sleep, and stress data will be integrated. Numerical models can be used to predict how stress-induced sleep disruption leads to specific blood glucose fluctuations. One study found that sleep deprivation was associated with nighttime blood glucose spikes. Machine learning algorithms can help identify specific sleep-related factors (such as bedtime routine and sleep duration) that have the greatest impact on blood glucose levels. Physical activity can reduce sleep deprivation-mediated blood glucose spikes [107]. Using the CGM, physical activity type and intensity can be determined and applied optimally. Some people experience an immediate blood glucose spike when stressed, whereas others may experience a delayed effect, indicating chronic stress. Chronic stress increases cortisol levels over time, which are likely to negatively affect cognitive function. Physical activity can reduce stress, contribute to cognitive function, and help manage blood glucose levels [108,109]. Armed with insights from CGM data, individuals can develop stress-management strategies that fit their unique patterns. For patients with diabetes, healthcare professionals can adjust medication dosages or insulin regimens based on stress-related blood glucose patterns. This integrated approach identifies the interconnectedness of stress, sleep, nutrition, and physical activity, which affect glucose control, allowing individuals to take a holistic approach to their health by improving not only glucose control, but also overall well-being. Based on these insights, appropriate lifestyle levels can be predicted for a growing number of individuals with obesity and diabetes, which could help reduce societal costs.
Acknowledgments
This research was supported by a College of Education, Korea University Grant (2023).
The authors have no financial, consulting, institutional, or other relationships that may lead to bias or conflicts of interest.
REFERENCES
- 1.Hill JO, Levine JS, Saris WHM. Handbook of Obesity. CRC Press; Boca Raton, FL: 2003. [Google Scholar]
- 2.Klein S, Gastaldelli A, Yki-Järvinen H, Scherer PE. Why does obesity cause diabetes? Cell Metab. 2022;34:11–20. doi: 10.1016/j.cmet.2021.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanaka M. Improving obesity and blood pressure. Hypertens Res. 2020;43:79–89. doi: 10.1038/s41440-019-0348-x. [DOI] [PubMed] [Google Scholar]
- 4.Becton LJ, Shatat IF, Flynn JT. Hypertension and obesity: epidemiology, mechanisms and clinical approach. Indian J Pediatr. 2012;79:1056–61. doi: 10.1007/s12098-012-0777-x. [DOI] [PubMed] [Google Scholar]
- 5.Duflou J, Virmani R, Rabin I, Burke A, Farb A, Smialek J. Sudden death as a result of heart disease in morbid obesity. Am Heart J. 1995;130:306–13. doi: 10.1016/0002-8703(95)90445-x. [DOI] [PubMed] [Google Scholar]
- 6.Alpert MA, Hashimi MW. Obesity and the Heart. AJMS. 1993;306:117–23. doi: 10.1097/00000441-199308000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Dehlendorff C, Andersen KK, Olsen TS. Body mass index and death by stroke: no obesity paradox. JAMA Neurol. 2014;71:978–84. doi: 10.1001/jamaneurol.2014.1017. [DOI] [PubMed] [Google Scholar]
- 8.Katsiki N, Ntaios G, Vemmos K. Stroke, obesity and gender: a review of the literature. Maturitas. 2011;69:239–43. doi: 10.1016/j.maturitas.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 9.Khandekar MJ, Cohen P, Spiegelman BM. Molecular mechanisms of cancer development in obesity. Nat Rev Cancer. 2011;11:886–95. doi: 10.1038/nrc3174. [DOI] [PubMed] [Google Scholar]
- 10.Wolin KY, Carson K, Colditz GA. Obesity and cancer. The Oncologist. 2010;15:556–65. doi: 10.1634/theoncologist.2009-0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jebb S. Obesity: causes and consequences. Women’s Health Medicine. 2004;1:38–41. [Google Scholar]
- 12.Doll HA, Petersen SE, Stewart‐Brown SL. Obesity and physical and emotional well‐being: associations between body mass index, chronic illness, and the physical and mental components of the SF‐36 questionnaire. Obes Res. 2000;8:160–70. doi: 10.1038/oby.2000.17. [DOI] [PubMed] [Google Scholar]
- 13.Fontaine K, Barofsky I. Obesity and health‐related quality of life. Obes Rev. 2001;2:173–82. doi: 10.1046/j.1467-789x.2001.00032.x. [DOI] [PubMed] [Google Scholar]
- 14.Solomon CG, Manson JE. Obesity and mortality: a review of the epidemiologic data. Am J Clin Nutr. 1997;66:1044S–50S. doi: 10.1093/ajcn/66.4.1044S. [DOI] [PubMed] [Google Scholar]
- 15.Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5:161. doi: 10.21037/atm.2017.03.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. 2009. [Google Scholar]
- 17. Lobstein T, Jackson-Leach R, Powis J, Brinsden H, Gray M. World obesity atlas 2023. 2023. [Google Scholar]
- 18.Rhee EJ. Prevalence and current management of cardiovascular risk factors in Korean adults based on fact sheets. Endocrinol Metab. 2020;35:85–94. doi: 10.3803/EnM.2020.35.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang YS, Han BD, Han K, Jung JH, Son JW. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr. 2022;31:169–77. doi: 10.7570/jomes22024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hauner H. Obesity and diabetes. Textbook of Diabetes. 2017:215–28. [Google Scholar]
- 21.Rorsman P, Renström E. Insulin granule dynamics in pancreatic beta cells. Diabetologia. 2003;46:1029–45. doi: 10.1007/s00125-003-1153-1. [DOI] [PubMed] [Google Scholar]
- 22.Ahmed B, Sultana R, Greene MW. Adipose tissue and insulin resistance in obese. Biomed Pharmacother. 2021;137:111315. doi: 10.1016/j.biopha.2021.111315. [DOI] [PubMed] [Google Scholar]
- 23.Güemes M, Rahman SA, Hussain K. What is a normal blood glucose? ADC. 2016;101:569–74. doi: 10.1136/archdischild-2015-308336. [DOI] [PubMed] [Google Scholar]
- 24.Ozougwu J, Obimba K, Belonwu C, Unakalamba C. The pathogenesis and pathophysiology of type 1 and type 2 diabetes mellitus. J Physiol Pathophysiol. 2013;4:46–57. [Google Scholar]
- 25.Dong S, Lau H, Chavarria C, Alexander M, Cimler A, Elliott JP, Escovar S, Lewin J, Novak J, Lakey JRT. Effects of periodic intensive insulin therapy: an updated review. Curr Ther Res Clin Exp. 2019;90:61–7. doi: 10.1016/j.curtheres.2019.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Riccardi G, Giacco R, Rivellese AA. Dietary fat, insulin sensitivity and the metabolic syndrome. Clin Nutr. 2004;23:447–56. doi: 10.1016/j.clnu.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 27.Laakso M. Hyperglycemia and cardiovascular disease in type 2 diabetes. Diabetes. 1999;48:937–42. doi: 10.2337/diabetes.48.5.937. [DOI] [PubMed] [Google Scholar]
- 28.Braunwald E. Diabetes, heart failure, and renal dysfunction: the vicious circles. Prog Cardiovasc Dis. 2019;62:298–302. doi: 10.1016/j.pcad.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Cryer PE. Symptoms of hypoglycemia, thresholds for their occurrence, and hypoglycemia unawareness. Endocrinol Metab Clin North Am. 1999;28:495–500. doi: 10.1016/s0889-8529(05)70084-0. [DOI] [PubMed] [Google Scholar]
- 30.Ryan C, Gurtunca N, Becker D. Hypoglycemia: a complication of diabetes therapy in children. Pediatr Clin North Am. 2005;52:1705–33. doi: 10.1016/j.pcl.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 31.Fidler C, Elmelund Christensen T, Gillard S. Hypoglycemia: an overview of fear of hypoglycemia, quality-of-life, and impact on costs. J Med Econ. 2011;14:646–55. doi: 10.3111/13696998.2011.610852. [DOI] [PubMed] [Google Scholar]
- 32.Kodl CT, Seaquist ER. Cognitive dysfunction and diabetes mellitus. Endocr Rev. 2008;29:494–511. doi: 10.1210/er.2007-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perantie DC, Lim A, Wu J, Weaver P, Warren SL, Sadler M, White NH, Hershey T. Effects of prior hypoglycemia and hyperglycemia on cognition in children with type 1 diabetes mellitus. Pediatr Diabetes. 2008;9:87–95. doi: 10.1111/j.1399-5448.2007.00274.x. [DOI] [PubMed] [Google Scholar]
- 34.Penckofer S, Quinn L, Byrn M, Ferrans C, Miller M, Strange P. Does glycemic variability impact mood and quality of life? Diabetes Technol Ther. 2012;14:303–10. doi: 10.1089/dia.2011.0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klonoff DC. Continuous glucose monitoring: roadmap for 21st century diabetes therapy. Diabetes Care. 2005;28:1231–9. doi: 10.2337/diacare.28.5.1231. [DOI] [PubMed] [Google Scholar]
- 36.Klonoff DC. A review of continuous glucose monitoring technology. Diabetes Technol Ther. 2005;7:770–5. doi: 10.1089/dia.2005.7.770. [DOI] [PubMed] [Google Scholar]
- 37.Ajjan RA, Cummings MH, Jennings P, Leelarathna L, Rayman G, Wilmot EG. Accuracy of flash glucose monitoring and continuous glucose monitoring technologies: implications for clinical practice. Diab Vasc Dis Res. 2018;15:175–84. doi: 10.1177/1479164118756240. [DOI] [PubMed] [Google Scholar]
- 38.Ajjan RA. How can we realize the clinical benefits of continuous glucose monitoring? Diabetes Technol Ther. 2017;19:S27–S36. doi: 10.1089/dia.2017.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yoshii H, Mita T, Katakami N, Okada Y, Osonoi T, Aso K, Kurozumi A, Wakasugi S, Sato F, Ishii R, Gosho M, Shimomura I, Watada H. The importance of continuous glucose monitoring-derived metrics beyond HbA1c for optimal individualized glycemic control. J Clin Endocrinol Metab. 2022;107:e3990–e4003. doi: 10.1210/clinem/dgac459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mian Z, Hermayer KL, Jenkins A. Continuous glucose monitoring: review of an innovation in diabetes management. Am J Med Sci. 2019;358:332–9. doi: 10.1016/j.amjms.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 41.Rodbard D. Continuous glucose monitoring: a review of successes, challenges, and opportunities. Diabetes Technol Ther. 2016;18:S3–S13. doi: 10.1089/dia.2015.0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rodbard D. Continuous glucose monitoring: a review of recent studies demonstrating improved glycemic outcomes. Diabetes Technol Ther. 2017;19:S25–S37. doi: 10.1089/dia.2017.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vashist SK. Continuous glucose monitoring systems: a review. Diagnostics. 2013;3:385–412. doi: 10.3390/diagnostics3040385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Klonoff DC, Ahn D, Drincic A. Continuous glucose monitoring: a review of the technology and clinical use. Diabetes Res Clin Pract. 2017;133:178–92. doi: 10.1016/j.diabres.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 45.Vaddiraju S, Burgess DJ, Tomazos I, Jain FC, Papadimitrakopoulos F. Technologies for continuous glucose monitoring: current problems and future promises. J Diabetes Sci Technol. 2010;4:1540–62. doi: 10.1177/193229681000400632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schembre SM, Liao Y, Jospe MR. Continuous glucose monitors as wearable lifestyle behavior change tools in obesity and diabetes. Obesity and Diabetes. 2020:591–603. [Google Scholar]
- 47.Battelino T, Danne T, Bergenstal RM, Amiel SA, Beck R, Biester T, Bosi E, Buckingham BA, Cefalu WT, Close KL, Cobelli C, Dassau E, DeVries JH, Donaghue KC, Dovc K, Doyle FJ, Garg S, Grunberger G, Heller S, Heinemann L, Hirsch IB, Hovorka R, Jia W, Kordonouri O, Kovatchev B, Kowalski A, Laffel L, Levine B, Mayorov A, Mathieu C, Murphy HR, Nimri R, Norgaard K, Parkin CG, Renard E, Rodbard D, Saboo B, Schatz D, Stoner K, Urakami T, Weinzimer SA, Phillip M. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42:1593–603. doi: 10.2337/dci19-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lawton J, Blackburn M, Allen J, Campbell F, Elleri D, Leelarathna L, Rankin D, Tauschmann M, Thabit H, Hovorka R. Patients’ and caregivers’ experiences of using continuous glucose monitoring to support diabetes self-management: qualitative study. BMC Endocr Disord. 2018;18:12. doi: 10.1186/s12902-018-0239-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vigersky RA, Fonda SJ, Chellappa M, Walker MS, Ehrhardt NM. Short-and long-term effects of real-time continuous glucose monitoring in patients with type 2 diabetes. Diabetes Care. 2012;35:32–8. doi: 10.2337/dc11-1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Adu MD, Malabu UH, Malau-Aduli AE, Malau-Aduli BS. Enablers and barriers to effective diabetes self-management: A multi-national investigation. PLoS One. 2019;14:e0217771. doi: 10.1371/journal.pone.0217771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hermanns N, Ehrmann D, Shapira A, Kulzer B, Schmitt A, Laffel L. Coordination of glucose monitoring, self-care behaviour and mental health: achieving precision monitoring in diabetes. Diabetologia. 2022;65:1883–94. doi: 10.1007/s00125-022-05685-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Holzer R, Bloch W, Brinkmann C. Continuous glucose monitoring in healthy adults—possible applications in health care, wellness, and sports. Sensors. 2022;22:2030. doi: 10.3390/s22052030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Duckworth C, Guy MJ, Kumaran A, O’Kane AA, Ayobi A, Chapman A, Marshall P, Boniface M. Explainable machine learning for real-time hypoglycemia and hyperglycemia prediction and personalized control recommendations. J Diabetes Sci Technol. 2022:19322968221103561. doi: 10.1177/19322968221103561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lu J, Ma X, Zhou J, Zhang L, Mo Y, Ying L, Lu W, Zhu W, Bao Y, Vigersky RA, Jia W. Association of time in range, as assessed by continuous glucose monitoring, with diabetic retinopathy in type 2 diabetes. Diabetes Care. 2018;41:2370–6. doi: 10.2337/dc18-1131. [DOI] [PubMed] [Google Scholar]
- 55.Yoo JH, Kim JH. Time in range from continuous glucose monitoring: a novel metric for glycemic control. Diabetes Metab J. 2020;44:828–39. doi: 10.4093/dmj.2020.0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yapanis M, James S, Craig ME, O’Neal D, Ekinci EI. Complications of diabetes and metrics of glycemic management derived from continuous glucose monitoring. J Clin Endocrinol Metab. 2022;107:e2221–e36. doi: 10.1210/clinem/dgac034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Raj R, Mishra R, Jha N, Joshi V, Correa R, Kern PA. Time in range, as measured by continuous glucose monitor, as a predictor of microvascular complications in type 2 diabetes: a systematic review. BMJ Open Diabetes Res Care. 2022;10:e002573. doi: 10.1136/bmjdrc-2021-002573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Freckmann G, Hagenlocher S, Baumstark A, Jendrike N, Gillen RC, Rössner K, Haug C. Continuous glucose profiles in healthy subjects under everyday life conditions and after different meals. J Diabetes Sci Technol. 2007;1:695–703. doi: 10.1177/193229680700100513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Riddell M, Perkins BA. Exercise and glucose metabolism in persons with diabetes mellitus: perspectives on the role for continuous glucose monitoring. J Diabetes Sci Technol. 2009;3:914–23. doi: 10.1177/193229680900300439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Block JM. Continuous glucose monitoring: changing diabetes behavior in real time and retrospectively. J Diabetes Sci Technol. 2008;2:484–9. doi: 10.1177/193229680800200320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Litchman ML, Allen NA, Colicchio VD, Wawrzynski SE, Sparling KM, Hendricks KL, Berg CA. A qualitative analysis of real-time continuous glucose monitoring data sharing with care partners: to share or not to share? Diabetes Technol Ther. 2018;20:25–31. doi: 10.1089/dia.2017.0285. [DOI] [PubMed] [Google Scholar]
- 62.Hall H, Perelman D, Breschi A, Limcaoco P, Kellogg R, McLaughlin T, Snyder M. Glucotypes reveal new patterns of glucose dysregulation. PLoS Biol. 2018;16:e2005143. doi: 10.1371/journal.pbio.2005143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Berry S, Valdes A, Davies R, Delahanty L, Drew D, Chan AT, Segata N, Franks P, Spector T. Predicting personal metabolic responses to food using multi-omics machine learning in over 1000 twins and singletons from the UK and US: the PREDICT I study (OR31-01-19) Curr Dev Nutr. 2019;3:3130642. [Google Scholar]
- 64.Mohan V, Spiegelman D, Sudha V, Gayathri R, Hong B, Praseena K, Anjana RM, Wedick NM, Arumugam K, Malik V, Ramachandran S, Bai MR, Henry JK, Hu FB, Willett W, Krishnaswamy K. Effect of brown rice, white rice, and brown rice with legumes on blood glucose and insulin responses in overweight Asian Indians: a randomized controlled trial. Diabetes Technol Ther. 2014;16:317–25. doi: 10.1089/dia.2013.0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vidmar AP, Naguib M, Raymond JK, Salvy SJ, Hegedus E, Wee CP, Goran MI. Time-limited eating and continuous glucose monitoring in adolescents with obesity: a pilot study. Nutrients. 2021;13:3697. doi: 10.3390/nu13113697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Peters B, Koppold-Liebscher DA, Schuppelius B, Steckhan N, Pfeiffer AF, Kramer A, Michalsen A, Pivovarova-Ramich O. Effects of early vs. late time-restricted eating on cardiometabolic health, inflammation, and sleep in overweight and obese women: a study protocol for the chronofast trial. Front Nutr. 2021;8:765543. doi: 10.3389/fnut.2021.765543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yoshimura E, Hamada Y, Hatanaka M, Nanri H, Nakagata T, Matsumoto N, Shimoda S, Tanaka S, Miyachi M, Hatamoto Y. Relationship between intra-individual variability in nutrition-related lifestyle behaviors and blood glucose outcomes under free-living conditions in adults without type 2 diabetes. Diabetes Res Clin Pract. 2023;196:110231. doi: 10.1016/j.diabres.2022.110231. [DOI] [PubMed] [Google Scholar]
- 68.Pettus J, Edelman SV. Recommendations for using real-time continuous glucose monitoring (rtCGM) data for insulin adjustments in type 1 diabetes. J Diabetes Sci Technol. 2017;11:138–47. doi: 10.1177/1932296816663747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Riddell MC, Milliken J. Preventing exercise-induced hypoglycemia in type 1 diabetes using real-time continuous glucose monitoring and a new carbohydrate intake algorithm: an observational field study. Diabetes Technol Ther. 2011;13:819–25. doi: 10.1089/dia.2011.0052. [DOI] [PubMed] [Google Scholar]
- 70.Plis K, Bunescu R, Marling C, Shubrook J, Schwartz F. A machine learning approach to predicting blood glucose levels for diabetes management; Workshops at the Twenty-Eighth AAAI conference on artificial intelligence; 2014. [Google Scholar]
- 71.Bell KJ, Smart CE, Steil GM, Brand-Miller JC, King B, Wolpert HA. Impact of fat, protein, and glycemic index on postprandial glucose control in type 1 diabetes: implications for intensive diabetes management in the continuous glucose monitoring era. Diabetes Care. 2015;38:1008–15. doi: 10.2337/dc15-0100. [DOI] [PubMed] [Google Scholar]
- 72.Mangrola D, Cox C, Furman AS, Krishnan S, Karakas SE. Self blood glucose monitoring underestimates hyperglycemia and hypoglycemia as compared to continuous glucose monitoring in type 1 and type 2 diabetes. Endocr Pract. 2018;24:47–52. doi: 10.4158/EP-2017-0032. [DOI] [PubMed] [Google Scholar]
- 73.Schwartz S, Scheiner G. The role of continuous glucose monitoring in the management of type-1 and type-2 diabetes. Evidence Based Management of Diabetes. 2012:91–111. [Google Scholar]
- 74.Pearce KL, Noakes M, Keogh J, Clifton PM. Effect of carbohydrate distribution on postprandial glucose peaks with the use of continuous glucose monitoring in type 2 diabetes. Am J Clin Nutr. 2008;87:638–44. doi: 10.1093/ajcn/87.3.638. [DOI] [PubMed] [Google Scholar]
- 75.Nansel TR, Gellar L, McGill A. Effect of varying glycemic index meals on blood glucose control assessed with continuous glucose monitoring in youth with type 1 diabetes on basal-bolus insulin regimens. Diabetes Care. 2008;31:695–7. doi: 10.2337/dc07-1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Little JP, Jung ME, Wright AE, Wright W, Manders RJ. Effects of high-intensity interval exercise versus continuous moderate-intensity exercise on postprandial glycemic control assessed by continuous glucose monitoring in obese adults. Appl Physiol Nutr Metab. 2014;39:835–41. doi: 10.1139/apnm-2013-0512. [DOI] [PubMed] [Google Scholar]
- 77.Parker L, Shaw CS, Banting L, Levinger I, Hill KM, McAinch AJ, Stepto NK. Acute low-volume high-intensity interval exercise and continuous moderate-intensity exercise elicit a similar improvement in 24-h glycemic control in overweight and obese adults. Front Physiol. 2017;7:661. doi: 10.3389/fphys.2016.00661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang X, Tian XY, Miyashita M, Sun F, Huang WY, Zheng C, Sum MK, Wong SHS. Effects of accumulated versus continuous individualized exercise on postprandial glycemia in young adults with obesity. Eur J Sport Sci. 2023;23:1446–56. doi: 10.1080/17461391.2023.2177199. [DOI] [PubMed] [Google Scholar]
- 79.Roberts CK, Little JP, Thyfault JP. Modification of insulin sensitivity and glycemic control by activity and exercise. Med Sci Sports Exerc. 2013;45:1868–77. doi: 10.1249/MSS.0b013e318295cdbb. [DOI] [PubMed] [Google Scholar]
- 80.Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, Horton ES, Castorino K, Tate DF. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39:2065–79. doi: 10.2337/dc16-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Munan M, Oliveira CL, Marcotte-Chénard A, Rees JL, Prado CM, Riesco E, Boule NG. Acute and chronic effects of exercise on continuous glucose monitoring outcomes in type 2 diabetes: a meta-analysis. Front Endocrinol. 2020;11:495. doi: 10.3389/fendo.2020.00495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.MacLeod S, Terada T, Chahal B, Boule N. Exercise lowers postprandial glucose but not fasting glucose in type 2 diabetes: a meta‐analysis of studies using continuous glucose monitoring. Diabetes Metab Res Rev. 2013;29:593–603. doi: 10.1002/dmrr.2461. [DOI] [PubMed] [Google Scholar]
- 83.Moser O, Riddell MC, Eckstein ML, Adolfsson P, Rabasa-Lhoret R, van den Boom L, Gillard P, Norgaard K, Oliver NS, Zaharieva DP, Battelino T, de Beaufort C, Bergenstal RM, Buckingham B, Cengiz E, Deeb A, Heise T, Heller S, Kowalski AJ, Leelarathna L, Mathieu C, Stettler C, Tauschmann M, Thabit H, Wilmot EG, Sourij H, Smart CE, Jacobs PG, Bracken RM, Mader JK. Glucose management for exercise using continuous glucose monitoring (CGM) and intermittently scanned CGM (isCGM) systems in type 1 diabetes: position statement of the European Association for the Study of Diabetes (EASD) and of the International Society for Pediatric and Adolescent Diabetes (ISPAD) endorsed by JDRF and supported by the American Diabetes Association (ADA) Pediatr Diabetes. 2020;21:1375–93. doi: 10.1111/pedi.13105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dimitriadis G, Mitrou P, Lambadiari V, Maratou E, Raptis SA. Insulin effects in muscle and adipose tissue. Diabetes Res Clin Pract. 2011;93:S52–S9. doi: 10.1016/S0168-8227(11)70014-6. [DOI] [PubMed] [Google Scholar]
- 85.Tanaka Y, Ogata H, Park I, Ando A, Ishihara A, Kayaba M, Yajima K, Suzuki C, Araki A, Osumi H, Zhang S, Seol J, Takahashi K, Nabekura Y, Satoh M, Tokuyama K. Effect of a single bout of morning or afternoon exercise on glucose fluctuation in young healthy men. Physiol Rep. 2021;9:e14784. doi: 10.14814/phy2.14784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sengoku Y, Nakamura K, Ogata H, Nabekura Y, Nagasaka S, Tokuyama K. Continuous glucose monitoring during a 100-km race: a case study in an elite ultramarathon runner. Int J Sports Physiol Perform. 2015;10:124–7. doi: 10.1123/ijspp.2013-0493. [DOI] [PubMed] [Google Scholar]
- 87.Ogata H, Tokuyama K, Nagasaka S, Ando A, Kusaka I, Sato N, Goto A, Ishibashi S, Kiyono K, Struzik ZR, Yamamoto Y. Longrange correlated glucose fluctuations in diabetes. Methods Inf Med. 2007;46:222–6. [PubMed] [Google Scholar]
- 88.Freckmann G, Pleus S, Grady M, Setford S, Levy B. Measures of accuracy for continuous glucose monitoring and blood glucose monitoring devices. J Diabetes Sci Technol. 2019;13:575–83. doi: 10.1177/1932296818812062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Muñoz Fabra E, Díez J-L, Bondia J, Laguna Sanz AJ. A comprehensive review of continuous glucose monitoring accuracy during exercise periods. Sensors. 2021;21:479. doi: 10.3390/s21020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bailey TS, Alva S. Landscape of continuous glucose monitoring (CGM) and integrated CGM: accuracy considerations. Diabetes Technol Ther. 2021;23:S5–S11. doi: 10.1089/dia.2021.0236. [DOI] [PubMed] [Google Scholar]
- 91.McClatchey PM, McClain ES, Williams IM, Malabanan CM, James FD, Lord PC, Gregory JM, Cliffel DE, Wasserman DH. Fibrotic encapsulation is the dominant source of continuous glucose monitor delays. Diabetes. 2019;68:1892–901. doi: 10.2337/db19-0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Acciaroli G, Vettoretti M, Facchinetti A, Sparacino G. Calibration of minimally invasive continuous glucose monitoring sensors: stateof-the-art and current perspectives. Biosensors. 2018;8:24. doi: 10.3390/bios8010024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bequette BW. Continuous glucose monitoring: real-time algorithms for calibration, filtering, and alarms. J Diabetes Sci Technol. 2010;4:404–18. doi: 10.1177/193229681000400222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hoss U, Budiman ES. Factory-calibrated continuous glucose sensors: the science behind the technology. Diabetes Technol Ther. 2017;19:S44–S50. doi: 10.1089/dia.2017.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Goodarzi M, Sharma S, Ramon H, Saeys W. Multivariate calibration of NIR spectroscopic sensors for continuous glucose monitoring. TrAC Trends Anal Chem. 2015;67:147–58. [Google Scholar]
- 96.Sang M, Cho M, Lim S, Min IS, Han Y, Lee C, Shin J, Yoon K, Yeo WH, Lee T, Won SM, Jung Y, Heo YJ, Yu KJ. Fluorescent-based biodegradable microneedle sensor array for tether-free continuous glucose monitoring with smartphone application. Sci Adv. 2023;9:e. doi: 10.1126/sciadv.adh1765. adh1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Manasa G, Mascarenhas RJ, Shetti NP, Malode SJ, Mishra A, Basu S, Aminabhavi TM. Skin patchable sensor surveillance for continuous glucose monitoring. ACS Appl Bio Mater. 2022;5:945–70. doi: 10.1021/acsabm.1c01289. [DOI] [PubMed] [Google Scholar]
- 98.Kaylor MB, Morrow L. Alarm fatigue and sleep deprivation in carers of children using continuous glucose monitors. Diabetes Care for Children & Young People. 2022;11:1–6. [Google Scholar]
- 99.Anhalt H. Limitations of continuous glucose monitor usage. Diabetes Technol Ther. 2016;18:115–7. doi: 10.1089/dia.2016.0011. [DOI] [PubMed] [Google Scholar]
- 100.Facchinetti A. Continuous glucose monitoring sensors: past, present and future algorithmic challenges. Sensors. 2016;16:2093. doi: 10.3390/s16122093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhao C, Fu Y. Statistical analysis based online sensor failure detection for continuous glucose monitoring in type I diabetes. Chemom Intell Lab. 2015;144:128–37. [Google Scholar]
- 102.Villena Gonzales W, Mobashsher AT, Abbosh A. The progress of glucose monitoring—a review of invasive to minimally and non-invasive techniques, devices and sensors. Sensors. 2019;19:800. doi: 10.3390/s19040800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Russell WR, Baka A, Björck I, Delzenne N, Gao D, Griffiths HR, Hadjilucas E, Juvonen K, Lahtinen S, Lansink M, Loon LV, Mykkanen H, Ostman E, Riccardi G, Vinoy S, Weickert Mo. Impact of diet composition on blood glucose regulation. Crit Rev Food Sci Nutr. 2016;56:541–90. doi: 10.1080/10408398.2013.792772. [DOI] [PubMed] [Google Scholar]
- 104.ADA Physical activity/exercise and diabetes. Diabetes Care. 2004;27:s58–s62. [Google Scholar]
- 105.Tan E, Scott EM. Circadian rhythms, insulin action, and glucose homeostasis. Curr Opin Clin Nutr Metab Care. 2014;17:343–8. doi: 10.1097/MCO.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 106.Tabata I, Atomi Y, Miyashita M. Blood glucose concentration dependent ACTH and cortisol responses to prolonged exercise. Clin Physiol. 1984;4:299–307. doi: 10.1111/j.1475-097x.1984.tb00805.x. [DOI] [PubMed] [Google Scholar]
- 107.Sharma S, Kavuru M. Sleep and metabolism: an overview. Int J Endocrinol. 2010;2010:270832. doi: 10.1155/2010/270832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Abou Elmagd M. Benefits, need and importance of daily exercise. Int J Phys Educ Sports Health. 2016;3:22–7. [Google Scholar]
- 109.Eo SJ, Leem YH. Effects of exercise intensity on the reactive astrocyte polarization in the medial prefrontal cortex. Phys Act Nutr. 2023;27:19–24. doi: 10.20463/pan.2023.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]