Key Points
Question
Were there changes in provision of cancer care during the first year of the COVID-19 pandemic in the US?
Findings
In this cohort study including 3 504 342 patients diagnosed with cancer, there was a significant decrease in the number of cancer treatments initiated during the first year of the pandemic compared with the expected given previous years’ trends. There were no significant changes in the proportion of different nonelective cancer treatment modalities initiated except for breast cancer.
Meaning
The findings of this study suggest that the significant decrease in cancer treatments provided during the first year of the pandemic likely reflects a deficit in the number of diagnoses instead of changes in cancer treatment strategies.
Abstract
Importance
The COVID-19 pandemic led to disruptions in access to health care, including cancer care. The extent of changes in receipt of cancer treatment is unclear.
Objective
To evaluate changes in the absolute number, proportion, and cancer treatment modalities provided to patients with newly diagnosed cancer during 2020, the first year of the pandemic.
Design, Setting, and Participants
In this cohort study, adults aged 18 years and older diagnosed with any solid tumor between January 1, 2018, and December 31, 2020, were identified using the National Cancer Database. Data analysis was conducted from September 19, 2022, to July 28, 2023.
Exposure
First year of the COVID-19 pandemic.
Main Outcomes and Measures
The expected number of procedures for each treatment modality (surgery, radiotherapy, chemotherapy, immunotherapy, and hormonal therapy) in 2020 were calculated using historical data (January 1, 2018, to December 31, 2019) with the vector autoregressive method. The difference between expected and observed numbers was evaluated using a generalized estimating equation under assumptions of the Poisson distribution for count data. Changes in the proportion of different types of cancer treatments initiated in 2020 were evaluated using the additive outlier method.
Results
A total of 3 504 342 patients (1 214 918 in 2018, mean [SD] age, 64.6 [13.6] years; 1 235 584 in 2019, mean [SD] age, 64.8 [13.6] years; and 1 053 840 in 2020, mean [SD] age, 64.9 [13.6] years) were included. Compared with expected treatment from previous years’ trends, there were approximately 98 000 fewer curative intent surgical procedures performed, 38 800 fewer chemotherapy regimens, 55 500 fewer radiotherapy regimens, 6800 fewer immunotherapy regimens, and 32 000 fewer hormonal therapies initiated in 2020. For most cancer sites and stages evaluated, there was no statistically significant change in the type of cancer treatment provided during the first year of the pandemic, the exception being a statistically significant decrease in the proportion of patients receiving breast-conserving surgery and radiotherapy with a simultaneous statistically significant increase in the proportion of patients undergoing mastectomy for treatment of stage I breast cancer during the first months of the pandemic.
Conclusions and Relevance
In this large national cohort study, a significant deficit was noted in the number of cancer treatments provided in the first year of the COVID-19 pandemic. Data indicated that this deficit in the number of cancer treatments provided was associated with decreases in the number of cancer diagnoses, not changes in treatment strategies.
This cohort study examines changes in cancer diagnoses and treatment in the US during the first year of the COVID-19 pandemic.
Introduction
In March 2020, soon after the World Health Organization declared the COVID-19 outbreak a pandemic, US states and territories implemented policies and strategies limiting person-to-person interactions to reduce transmission in the community and accommodate the surge of emergent health care needs, leading to a reduction in the number of cancer screenings,1 diagnoses,2 and treatments.3,4
Furthermore, the immunosuppressive nature of cancer therapies, combined with frequent outpatient visits, required a balance between the risks associated with COVID-19 exposure and the risks associated with delaying provision of nonelective cancer treatment, which varied according to cancer site, stage, and cancer treatment modality.5,6,7,8,9,10,11 This study examined whether there were changes in the number of cancer treatments initiated and in the proportion of different cancer treatment modalities provided during 2020, the first year of the pandemic, compared with numbers expected from historical trends.
Methods
We performed a retrospective cohort study including adults aged 18 years and older diagnosed with solid tumors between January 1, 2018, and December 31, 2020, using the National Cancer Database (NCDB), a nationwide hospital-based cancer registry jointly sponsored by the American College of Surgeons and the American Cancer Society, which includes approximately 70% of all patients with newly diagnosed cancer in the US.12 Trained tumor registrars abstract demographic, clinical, and treatment information from medical records, and NCDB data were determined to be reliable for evaluating the association of the pandemic with cancer care.13 This study was based on publicly available data and determined to be exempt from review by the institutional review board of the Morehouse School of Medicine in Atlanta, Georgia. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
To evaluate whether the changes in the number of cancer treatment procedures initiated in 2020 were an extension of patterns established in previous years, we first estimated the expected number of procedures for each treatment modality in 2020 using previous years’ monthly totals (January 1, 2018, through December 31, 2019) and the vector autoregressive method accounting for seasonality and random error. We then estimated the difference between expected and observed number of cancer treatments initiated using generalized estimating equations under assumptions of the Poisson distribution for count data. This analysis was conducted for all solid cancers combined (approximately 50 cancer sites, including 1 category for other cancer sites) and separately for each of the 8 most common stageable solid tumor sites: lung, female breast, colorectal (evaluated separately for colon and rectum due to differences in recommended treatment for each site and stage), kidney, uterus, prostate, and melanoma. We used the additive outlier method to identify variations from the expected percentage of individuals receiving each treatment modality (structural breaks) and interrupted time series analysis to identify changes in ongoing treatment patterns each month between January 1, 2019, and December 31, 2020, accounting for age, sex (male, female, and other/transgender/missing), seasonality, regional variation (state of residence at diagnosis with missing values included as a separate category), and random error. Cancer treatment modalities included surgery, radiotherapy, chemotherapy, immunotherapy, hormonal therapy, and watchful waiting (eTable 1 in Supplement 1). Treatment provided for palliative purposes was not included due to challenges with comparability between definitive and palliative treatment data. The clinical and socioeconomic characteristics including comorbidities, racialized and ethnic groups, and facility type are provided to show the diversity of the study population. NCDB guidelines recommend this information be self-reported. However, while data abstraction from medical records into the NCDB is highly standardized, the methods used at each facility that reports to NCDB to capture this information on medical records may vary.
Statistical Analysis
Data analysis was conducted from September 19, 2022, to July 28, 2023. All P values were 2-sided with a statistical significance threshold of 5%. All statistical analyses were performed using SAS, version 9.4 (SAS Institute Inc).
Results
A total of 3 504 342 patients (1 214 918 in 2018, mean [SD] age, 64.6 [13.6] years; 1 235 584 in 2019, mean [SD] age, 64.8 [13.6] years; and 1 053 840 in 2020, mean [SD] age, 64.9 [13.6] years) were included (Table 1). Compared with what was expected based on previous years’ trends in cancer treatment, there were 98 422 fewer curative intent surgical procedures performed: 38 850 fewer chemotherapy regimens initiated, 55 507 fewer radiotherapy regimens initiated, 6833 fewer immunotherapy regimens initiated, and 31 948 fewer hormonal therapy regimens initiated in 2020 (Table 2).
Table 1. Characteristics of Individuals Diagnosed With Cancera .
| Characteristic | Diagnosis year, No. (%)b | ||
|---|---|---|---|
| 2018 (n = 1 214 918) | 2019 (n = 1 235 584) | 2020 (n = 1 053 840) | |
| Age, mean (SD), y | 64.6 (13.6) | 64.8 (13.6) | 64.9 (13.6) |
| Cancer site | |||
| Prostate | 137 920 (11.4) | 146 195 (11.9) | 117 646 (11.2) |
| Lung | 170 486 (14.1) | 172 056 (14.0) | 145 557 (13.8) |
| Breast | 223 870 (18.5) | 227 049 (18.4) | 197 668 (18.8) |
| Colon and rectum | 106 935 (8.8) | 105 532 (8.6) | 89 499 (8.5) |
| Bladder | 27 841 (2.3) | 28 458 (2.3) | 25 797 (2.5) |
| Melanoma | 45 038 (3.7) | 46 657 (3.8) | 38 006 (3.6) |
| Kidney | 52 930 (4.4) | 54 413 (4.4) | 46 090 (4.4) |
| Uterus | 50 959 (4.2) | 51 831 (4.2) | 45 314 (4.3) |
| Pancreas | 41 499 (3.4) | 42 322 (3.4) | 38 966 (3.7) |
| Oral cavity and pharynx | 37 935 (3.1) | 38 880 (3.2) | 34 698 (3.3) |
| Thyroid | 37 394 (3.1) | 37 517 (3.0) | 29 718 (2.8) |
| Cranial nerves and other nervous system | 35 473 (2.9) | 36 363 (3.0) | 29 730 (2.8) |
| Stomach | 18 813 (1.6) | 18 978 (1.5) | 16 041 (1.5) |
| Brain | 20 402 (1.7) | 20 165 (1.6) | 18 629 (1.8) |
| Ovary | 17 064 (1.4) | 16 682 (1.4) | 14 700 (1.4) |
| Liver | 26 339 (2.2) | 26 792 (2.2) | 22 710 (2.2) |
| Esophagus | 14 515 (1.2) | 15 052 (1.2) | 13 184 (1.3) |
| Cervix | 10 717 (0.9) | 10 880 (0.9) | 8990 (0.9) |
| Other | 135 932 (11.2) | 136 762 (11.1) | 118 215 (11.2) |
| Age group, y | |||
| 18-39 | 97 771 (8.1) | 97 994 (7.9) | 84 471 (8.0) |
| 40-64 | 461 280 (38.0) | 461 234 (37.4) | 387 541 (36.8) |
| 65-74 | 367 469 (30.3) | 379 217 (30.7) | 327 332 (31.1) |
| ≥75 | 287 636 (23.7) | 296 323 (24.0) | 253 831 (24.1) |
| Sex | |||
| Male | 548 115 (45.9) | 565 478 (46.2) | 481 323 (45.9) |
| Female | 645 764 (54.1) | 658 180 (53.8) | 567 726 (54.1) |
| Other/transgender/missing | 381 (0.0) | 354 (0.0) | 540 (0.1) |
| Stage at diagnosis | |||
| I | 430 007 (35.4) | 441 623 (35.7) | 367 149 (34.8) |
| II | 187 111 (15.4) | 188 884 (15.3) | 157 277 (14.9) |
| III | 170 536 (14.0) | 173 525 (14.0) | 148 918 (14.1) |
| IV | 203 605 (16.8) | 205 379 (16.6) | 184 385 (17.5) |
| Unstageablec | 223 659 (18.4) | 226 173 (18.3) | 196 111 (18.6) |
| Comorbidities | |||
| 0 | 863 907 (72.3) | 881 199 (72.0) | 747 138 (71.2) |
| 1 | 189 603 (15.9) | 195 944 (16.0) | 171 270 (16.3) |
| ≥2 | 140 750 (11.8) | 146 869 (12.0) | 131 181 (12.5) |
| Facility type | |||
| NCI designated | 190 020 (15.9) | 194 468 (15.9) | 144 891 (13.8) |
| Comprehensive | 407 392 (34.1) | 419 967 (34.3) | 372 761 (35.5) |
| Teaching | 264 112 (22.1) | 270 577 (22.1) | 234 513 (22.3) |
| Community | 64 818 (5.4) | 65 861 (5.4) | 57 563 (5.5) |
| Other/missing | 267 918 (22.4) | 273 139 (22.3) | 239 861 (22.9) |
| Region | |||
| New England | 69 238 (5.7) | 70 505 (5.7) | 60 269 (5.7) |
| Mid-Atlantic | 184 233 (15.2) | 191 446 (15.5) | 153 809 (14.6) |
| East North | 211 444 (17.4) | 214 859 (17.4) | 188 540 (17.9) |
| Great Lakes | 88 629 (7.3) | 87 986 (7.1) | 77 733 (7.4) |
| South | 263 390 (21.7) | 269 150 (21.8) | 234 081 (22.2) |
| Midwest | 81 111 (6.7) | 81 335 (6.6) | 71 194 (6.8) |
| West | 109 393 (9.0) | 110 785 (9.0) | 93 652 (8.9) |
| Mountain | 55 509 (4.6) | 55 038 (4.5) | 45 685 (4.3) |
| Pacific | 147 643 (12.2) | 151 202 (12.2) | 126 631 (12.0) |
| Missing | 4328 (0.4) | 3278 (0.3) | 2246 (0.2) |
| Racialized and ethnic groupsd | |||
| Hispanic | 80 908 (6.7) | 83 821 (6.8) | 70 967 (6.7) |
| Indigenous populations | 4391 (0.4) | 4371 (0.4) | 4044 (0.4) |
| Non-Hispanic Asian | 39 914 (3.3) | 41 324 (3.3) | 34 473 (3.3) |
| Non-Hispanic Black | 137 622 (11.3) | 140 702 (11.4) | 120 196 (11.4) |
| Non-Hispanic White | 930 201 (76.6) | 942 954 (76.3) | 803 055 (76.2) |
| Other/missing | 19 178 (1.6) | 19 585 (1.6) | 18 455 (1.8) |
| Pacific Islander | 2704 (0.2) | 2827 (0.2) | 2650 (0.3) |
Abbreviation: NCI National Cancer Institute.
Data from January 1 2018 to December 31 2020 in the Commission on Cancer–Accredited Facilities National Cancer Database.
Sum of categories might not add to the totals due to exclusion of missing values.
Unstageable includes unknown stage and brain tumors.
Groups are reported as given in the database.
Table 2. Deficit in Cancer Treatment Events Reported to the National Cancer Database Compared With Expected in 2020 Overall.
| Treatment | Observed | Expected No. (SE) | Deficit No. (%) | P value |
|---|---|---|---|---|
| Surgery | 536 068 | 634 490.0 (988.9) | −98 422 (−15.5) | .003 |
| Chemotherapy | 281 739 | 320 589.0 (430.3) | −38 850 (−12.1) | .001 |
| Radiotherapy | 296 574 | 352 080.5 (375.6) | −55 507 (−15.8) | .001 |
| Immunotherapy | 91 989 | 98 822.4 (206.0) | −6833 (−6.9) | .07 |
| Hormone treatment | 183 997 | 215 945.0 (631.9) | −31 948 (−14.8) | .01 |
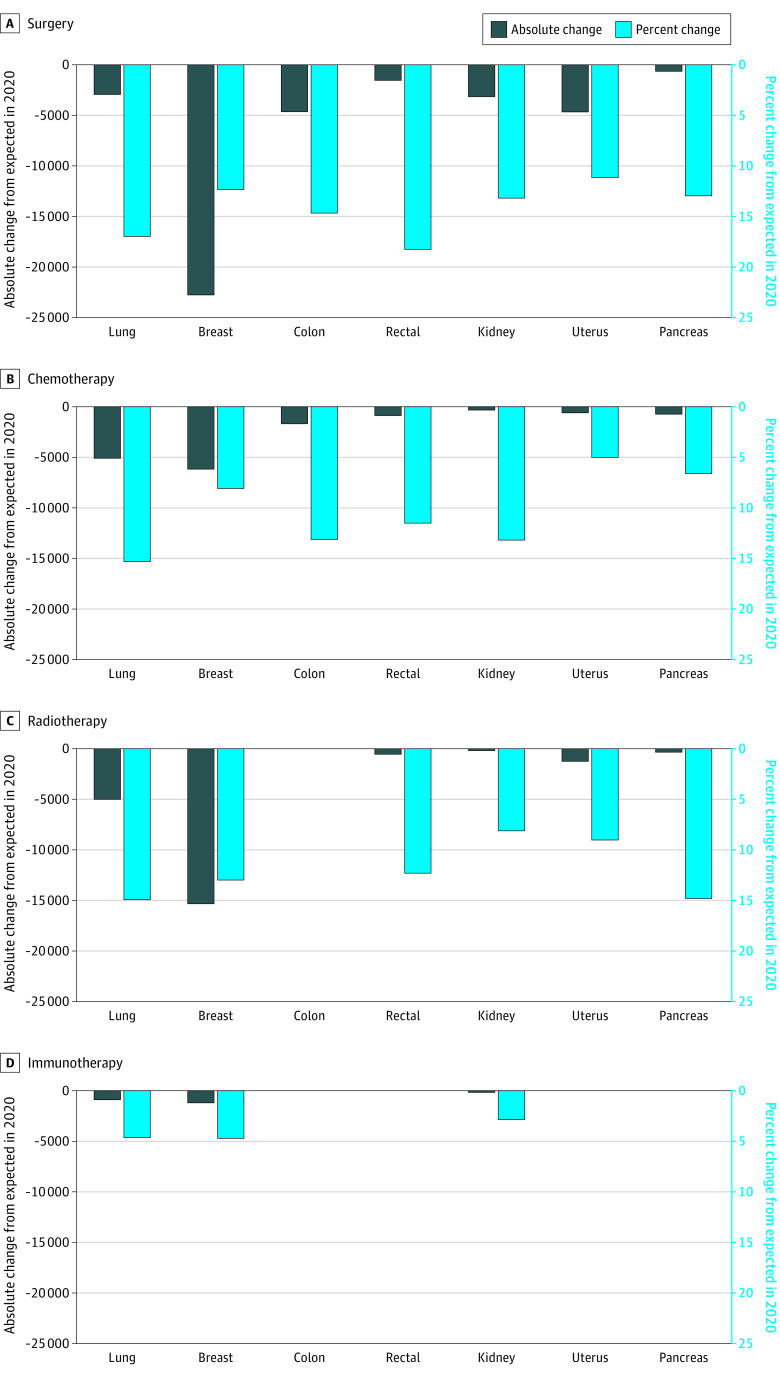
Decreases were especially large for recommended treatments of cancers frequently detected by screening, such as surgical procedures for breast, colon, and rectal cancers (Figure). The largest absolute deficit was in surgical procedures for breast cancer (22 208 fewer surgical procedures; 12.3% decrease), while the largest proportional decrease was in surgical procedures for rectal cancer (1529 fewer surgical procedures; 18.3% decrease), compared with the expected number of surgical procedures in 2020 (Figure). There were also statistically significant decreases in the number of chemotherapy regimens initiated for lung (5502 fewer regimens; 15.3% decrease), rectal (845 fewer regimens; 11.5% decrease), kidney (288 fewer regimens; 13.2% decrease), and pancreatic (696 fewer regimens; 6.6% decrease) cancer in 2020 (Figure). Because prostate cancer and melanoma are frequently treated in outpatient settings, leading to lower ascertainment in the NCDB,12 results for these cancer sites are presented only in eTable 1, eTable 2, and the eFigure in Supplement 1. The deficit in surgical procedures was greater among individuals diagnosed with stage I disease, while the largest deficits in chemotherapy and radiotherapy were for stages II to IV disease (eTable 2 in Supplement 1). In the evaluation of changes in cancer treatment in 3-month blocks, the greatest deficit for all treatments was observed during the second quarter of 2020, the first months of the pandemic in the US (eTable 3 in Supplement 1).
Figure. Absolute and Percent Deficit in Cancer Treatment Initiated in 2020 Compared With Expected by Treatment Modality and Cancer Site From the National Cancer Database.
Among individuals diagnosed with stage I breast cancer, there was a statistically significant decrease in the proportion of patients receiving breast-conserving surgery and radiotherapy with a simultaneous statistically significant increase in the proportion of patients undergoing mastectomy during the first months of the pandemic (eFigure in Supplement 1). There was no statistically significant change in the proportion of individuals receiving surgery, radiotherapy, or systemic therapy among individuals diagnosed with stages II to IV breast cancer or stages I to IV lung, colon, rectal, pancreas, uterine, or kidney cancers (eFigure in Supplement 1).
Discussion
In this large comprehensive national study, we found a significant decrease in the number of treatments provided for solid tumors during the first year of the COVID-19 pandemic. The deficit was especially large among treatments provided for early-stage cancers frequently detected by screening. For most cancer sites and stages evaluated, there was no statistically significant change in the type of cancer treatment provided during the first year of the pandemic. Only among individuals diagnosed with stage I breast cancer was a decrease noted in breast-conserving surgery and radiotherapy and an increase in receipt of mastectomy, possibly to reduce the risk of COVID-19 exposure with daily radiotherapy visits during the first months of the pandemic. Therefore, decreases in the number of cancer treatments provided were from decreases in number of cancer diagnoses—not changes in treatment strategies.13
Strengths and Limitations
Strengths of this study include national hospital-based data covering more than 70% of all cancer cases in the US.12 Furthermore, strict data quality and completeness standards for collecting demographic, tumor, and treatment information (including dates), enhance the reliability of the study results.14 In addition, evaluating both absolute number and proportion of cancer treatment procedures in each month of 2020 (which were compared with expected numbers and proportions estimated accounting for regional and seasonal variability, as well as historical trends) allows for more accurate identification of disruptions in cancer care during the first year of the pandemic.
This study also has limitations. First, the NCDB is a hospital-based (not a population-based) cancer registry. Therefore, patterns of care might not be representative of the entire US population, especially for treatment modalities commonly provided in outpatient settings, such as chemotherapy. Second, the NCDB only collects information on first treatment initiation, with no information on systemic therapy agents used, modes of administration (intravenous or oral), or treatment completion. However, first treatment information is collected even when provided outside of the reporting facility, strengthening the generalizability of our findings. Additionally, the demographic and clinical characteristics of patients in the NCDB are comparable to those from population-based cancer registries.12
Conclusions
This cohort study found statistically significant deficits in the number of cancer treatments provided during the first year of the COVID-19 pandemic. The decreases are likely resulting from the decrease in the number of patients diagnosed with cancer, not changes in treatment strategy. Future studies should evaluate whether clinical (eg, COVID-19 infection, comorbidity), socioeconomic, and facility characteristics are associated with changes in cancer treatment initiation during the first year of the pandemic.
eTable 1. Treatment Modality for Selected Cancer Sites
eTable 2. Deficit in Cancer Treatment Events Reported to the NCDB Compared to Expected in 2020 by Cancer Site and Stage at Diagnosis
eTable 3. Deficit in Cancer Treatment Events Reported to the NCDB Compared to Expected in 2020 by Quarter (3-Month Blocks)
eFigure. Proportion of Patients Receiving Different Cancer Treatment Modalities for Each Cancer Site and Stage From January 2019 to December 2020 NCDB
Data Sharing Statement
References
- 1.Star J, Bandi P, Siegel RL, et al. Cancer screening in the United States during the second year of the COVID-19 pandemic. J Clin Oncol. 2023;41(27):4352-4359. doi: 10.1200/JCO.22.02170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yabroff KR, Wu XC, Negoita S, et al. Association of the COVID-19 pandemic with patterns of statewide cancer services. J Natl Cancer Inst. 2022;114(6):907-909. doi: 10.1093/jnci/djab122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parikh RB, Takvorian SU, Vader D, et al. ; PRACTICE Investigators . Impact of the COVID-19 pandemic on treatment patterns for patients with metastatic solid cancer in the United States. J Natl Cancer Inst. 2022;114(4):571-578. doi: 10.1093/jnci/djab225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spencer K, Jones CM, Girdler R, et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: a population-based study. Lancet Oncol. 2021;22(3):309-320. doi: 10.1016/S1470-2045(20)30743-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020;6(7):1108-1110. doi: 10.1001/jamaoncol.2020.0980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desai A, Gupta R, Advani S, et al. Mortality in hospitalized patients with cancer and coronavirus disease 2019: a systematic review and meta-analysis of cohort studies. Cancer. 2021;127(9):1459-1468. doi: 10.1002/cncr.33386 [DOI] [PubMed] [Google Scholar]
- 7.Kuderer NM, Choueiri TK, Shah DP, et al. ; COVID-19 and Cancer Consortium . Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907-1918. doi: 10.1016/S0140-6736(20)31187-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Q, Berger NA, Xu R. Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. JAMA Oncol. 2021;7(2):220-227. doi: 10.1001/jamaoncol.2020.6178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee LY, Cazier JB, Angelis V, et al. ; UK Coronavirus Monitoring Project Team . COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395(10241):1919-1926. doi: 10.1016/S0140-6736(20)31173-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee LYW, Cazier JB, Starkey T, et al. ; UK Coronavirus Cancer Monitoring Project Team . COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol. 2020;21(10):1309-1316. doi: 10.1016/S1470-2045(20)30442-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Banna G, Curioni-Fontecedro A, Friedlaender A, Addeo A. How we treat patients with lung cancer during the SARS-CoV-2 pandemic: primum non nocere. ESMO Open. 2020;5(2):e000765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mallin K, Browner A, Palis B, et al. Incident cases captured in the National Cancer Database compared with those in US population based central cancer registries in 2012-2014. Ann Surg Oncol. 2019;26(6):1604-1612. doi: 10.1245/s10434-019-07213-1 [DOI] [PubMed] [Google Scholar]
- 13.Nogueira LM, Palis B, Boffa D, Lum S, Yabroff KR, Nelson H. Evaluation of the impact of the COVID-19 pandemic on reliability of cancer surveillance data in the National Cancer Database. Ann Surg Oncol. 2023;30(4):2087-2093. doi: 10.1245/s10434-022-12935-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Cancer Registrars Association . Council on Certification History. 2022. Accessed September 10, 2022. https://www.ncra-usa.org/CTR/Certification-About
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Treatment Modality for Selected Cancer Sites
eTable 2. Deficit in Cancer Treatment Events Reported to the NCDB Compared to Expected in 2020 by Cancer Site and Stage at Diagnosis
eTable 3. Deficit in Cancer Treatment Events Reported to the NCDB Compared to Expected in 2020 by Quarter (3-Month Blocks)
eFigure. Proportion of Patients Receiving Different Cancer Treatment Modalities for Each Cancer Site and Stage From January 2019 to December 2020 NCDB
Data Sharing Statement