Abstract
Emerging technological advances hold potential to assist the long-term care (LTC) workforce in caring for an aging population in the home and LTC settings. Technology may alter workforce needs and mitigate rising workforce demand. This study identified and assessed emerging technologies that may assist, replace, and/or support recruitment and retention of the LTC workforce and identified barriers and facilitators to their implementation. We identified a variety of technologies with applications for LTC, created a taxonomy of technology types and functions across LTC settings, and conducted semi-structured interviews with a sample of company leaders to assess perceived impact of their products and services on the LTC workforce. Thematic analysis of those interviews found that technology is not currently positioned to replace the LTC workforce but may facilitate work and support worker recruitment and retention. More rigorous evaluation of technologies in LTC and financing mechanisms are needed to support widespread adoption.
Keywords: long-term care, health workforce, health technology, emerging technologies, taxonomy of technologies
Introduction
In 2020, about 17% of the U.S. population was age 65 or older; this number will increase to 22% by 2050 (Duffin, 2022). This trend in aging exists in many other parts of the world as well. In the same year, the United Nations estimated the world population aged 65 years or older at 727 million and projected that it will reach more than 1.5 billion by 2050, an increase from 9.3% to 16% (United Nations Department of Economic and Social Affairs Population Division, 2020).
Much has been written about the challenges that the aging population will create, including questions about who will manage the medical and social needs of people with disabilities and serious illness (Institute on Medicine [US] Committee on the Future Health Care Workforce for Older Americans, 2008). A 2018 survey by AARP found that 75% of adults aged 50 and over in the United States want to grow old in their home or community; yet, many are concerned about their ability to do so (Binette & Vasold, 2018). Aging in one’s home may present many challenges, including the need for help with personal care and activities of daily living (ADL), communicating with family who may live far away, supporting ongoing social engagement, ensuring personal safety, and the logistics of health monitoring. In addition, this older population tends to have higher disability rates and thus more often needs to age in long-term care (LTC) facilities such as assisted living and skilled nursing facilities (Houser et al., 2012). The projected increase in LTC residents is an important contributor to projected increases in demand for LTC workers and potential workforce shortages, which are expected to worsen in the coming decade (PHI, 2021; Spetz et al., 2015; U.S. Bureau of Labor Statistics, 2021). In this article, we define the LTC workforce as frontline health care workers who work in LTC settings, such as nursing homes, assisted living facilities, and in client/patient homes.
There is optimism that the adoption of emerging technologies in the home and/or LTC facilities may help older adults navigate physical, social, and cognitive challenges. A report from the National Science and Technology Council acknowledged the potential of emerging technology to support an aging population to address needs such as access to health care, personal mobility, and communications and social engagement (Task Force on Research and Development for Technology to Support Aging Adults, 2019). While the report discusses the importance of family caregivers, there is little discussion of the paid LTC workforce, who will be critical to using and supporting technology in LTC settings and in the home. An ethnographic study investigated whether health information technology could mitigate workforce shortages in LTC and found that while there were some promising efficiencies, there were also challenges in interoperability between communication systems, thus limiting impact (Qian et al., 2019).
Nevertheless, technological advances have the potential to substantially alter workforce needs and mitigate a portion of the rising workforce demand due to an aging population and the increasing chronic disease burden (Institute on Medicine [US] Committee on the Future Health Care Workforce for Older Americans, 2008; Spetz et al., 2015). Technology may alter the LTC workforce in several ways. A LeadingAge report suggests that technology in aging care could improve workforce efficiency, reduce workload, improve care coordination, increase timely services, and improve communication (LeadingAge, 2011). However, much of the emerging technology in LTC is in a developmental, concept testing, or prototype phase; there is also a general lack of published evidence of efficacy (Tak et al., 2010).
Our framework for studying the impact of technology on the LTC workforce was similar to that described by the LeadingAge Center for Aging Services Technologies (CAST). The model proposes a paradigm for geriatric care-enabled technology including sensors, wearable, and telehealth devices that collect activity and clinical data from individuals where they live. These data can then be made available to families, paid workers, and primary care teams with a goal of improving communication and quality of care for the aging adult (LeadingAge, 2011).
This article presents the results of an analysis of emerging health care technologies with regard to their potential to assist, replace, or support the recruitment and retention of the workforce in the home and LTC settings. The following research questions guided this study:
What types of technologies have been developed with an application in LTC and how might they be categorized? Relevance: The growth of technology in health care has been rapid. However, there have been few studies focused on adoption and availability of different types of technology in the LTC sector.
How might these types of technologies in LTC affect existing and future workforce needs? Relevance: Despite the current and projected shortages in the LTC workforce, there has been little research on how technology may mitigate shortages and/or facilitate the work. There has also been little research on costs and implementation in various LTC settings.
We summarize the results of a(n) literature review, technology scan and accompanying development of two taxonomies of emerging LTC technologies, and analysis of interviews with a sample of leaders from health technology companies that provide products and/or services in the categories created in the taxonomies.
New Contribution
There are few existing studies about the impact of technology on the LTC workforce. This study raises new questions about whether and how technology may facilitate LTC work. With current and projected workforce shortages, it is important to study whether technology might mitigate shortages or change the way work is performed.
Study Design and Methods
The research protocol was approved by the University of California San Francisco Institutional Review Board as exempt. We used a qualitative approach that included a nonsystematic literature search of formal and grey literature, a technology scan and subsequent taxonomy development, and semistructured interviews conducted with company leaders.
Literature Review and Technology Scan
Databases used for peer-reviewed literature searches included PubMed, Google Scholar, and the Cumulative Index of Nursing and Allied Health Literature. Each search string was comprised of three search terms, where each search term was from one of three categories: setting, workforce, and technology. Setting terms included “long-term care,” “long term care,” “home care,” “assisted living,” “skilled nursing facilities,” and “nursing homes”; workforce terms included “workforce,” “health workforce,” and “home care workforce”; and technology terms included “technology,” “technologies,” “health technology,” “health technologies,” “emerging technology,” and “emerging technologies.” Grey literature (e.g., reports to Congress and from organizations such as LeadingAge and the Paraprofessional Healthcare Institute) was found on Google, in Aging 2.0 conference attendance materials, and company websites of emerging health technologies. Inclusion criteria for literature (e.g., studies, articles, and reports) included literature that was published in or translated to English, was published within the past 20 years, and discussed the impact of technology on the health workforce. Exclusion criteria included literature that discussed health technologies that were not used in LTC settings or were not used by the aging and/or disabled population. All literature was stored in EndNote®.
From January through May 2018, the team also conducted a series of technology scans via Google solely intended to inform the taxonomies and identify subjects for the interviews. The scans were repeated once a month for 5 months and utilized the same search strings as the peer-reviewed and grey literature review. Inclusion criteria for the taxonomy and interviewee selection included detailed product information on the company website, information provided in English, consistent online presence of the product (industry instability was indicated by the removal of several companies’ webpages during the 5-month search period), and a perception of potential impact on the LTC workforce upon initial review. Exclusion criteria included companies with products/services that were not used in the home or in LTC settings. All information about identified technology companies, products, and services was stored in Evernote®.
Taxonomy Development
Taxonomy development is a system of classifying complex phenomena according to a set of common conceptual domains (Bradley et al., 2007). This method is useful in the study of dimensions of variables and the relationships among variables, which then informs coding these variables into concepts or categories. Related concepts form a taxonomy when those concepts are linked together. This method was well-suited to categorizing emerging technologies because the myriad products and services found in the technology scan had elements that could be categorized according to similar functions or targeted needs in LTC. This method has evidence of previous use in diverse fields such as policy analysis (Chapman et al., 2016; Usman et al., 2017) and clinical outcomes research (Dovey et al., 2002). Previous research on developing a taxonomy of technology defined four attributes for improving quality of life: technologies that address specific needs; technologies that focus on compensating for, prevention of, maintenance of, or enhancing functions; passive versus interactive technologies; and level of technology systems’ intelligence (Schulz, 2013). Other research developed a framework for evaluating the adoption of and challenges to the scale-up of health care technologies in seven domains, including factors such as illness or condition, the specific technology, adopter systems (e.g., caregivers), organization, and societal context (Greenhalgh et al., 2017). Our study’s taxonomies focus on technology’s workforce implications; however, all of these domains are important to understand when considering challenges to widespread adoption.
Once our three-member research team reached agreement that new products/services were no longer being identified from the technology scans (after 5 months), we began developing taxonomies to describe the technologies. To create the taxonomies, each team member reviewed the Evernote® file to create technological domains by function and type. After independently creating these domains, the team compared theirs to one another. We initially grouped technology types and functions together into 15 domains: telehealth, robot/voice control, electronic health record interoperability, workforce education, remote monitoring (RM), wearable/device, family caregiver support, alarm/alert systems, recruitment/staffing, facility/home health management, documentation, online patient and employer engagement, online care management, home-to-clinic communication, and assisted living. However, while discussing these groupings, we saw the value in distinguishing between technology type and function to describe the technologies more accurately. Through an iterative process of combining, collapsing, and defining the individual domains, the team developed consensus on categories for the taxonomy domains.
Semistructured Interviews
The study’s scope allowed for one company interview in each taxonomic category of technology type and/or function. The criteria for selecting companies to interview included those whose technologies appeared to offer the most comprehensive services, appeared to be past the earliest stages of product development, had products/services that were likely to impact the workforce, and agreed to a telephone or in-person interview. Interview requests were sent to 16 companies, and 13 agreed to be interviewed. The interviewee(s) at each company included the CEO, COO, marketing and sales managers, product developers, and/or other individuals on the leadership team who had the most knowledge about product/service history and capabilities. At the request of some companies, interviews were conducted with a group of two to three of the company’s senior leaders. At the beginning of the interview, we read an information sheet guaranteeing confidentiality and assuring voluntary participation. Interviews were 1 hr in duration, recorded, and conducted by the research team.
Data Analysis
All team members independently reviewed the interview transcripts, stored in Dedoose®, and created qualitative analysis codes. Then, the team established a coding scheme together by identifying patterns of meaning from the content to form initial themes and reviewed the initial themes using a thematic analysis approach (Braun & Clarke, 2006; Pope & Mays, 2006). Analytic memos, or min-analyses, were written during data analysis to help identify patterns and relationships between themes. The team then iteratively consolidated the initial themes into overarching patterns and final themes and reconvened at regular intervals to ensure concordance. Using this iterative process, the team identified a final set of themes that represented the potential impact of these technologies on the LTC workforce.
Findings
Literature Review
The literature review identified a combination of 31 peer-reviewed articles, reports and government documents, and books that described or discussed technology’s impact on the LTC workforce. Highlights of this literature, summarized below, revealed little evidence of the impact of technology in facilitating the work of LTC workers.
A few key reports broadly described different technologies that that have the potential to assist aging adults (LeadingAge, 2011; Task Force on Research and Development for Technology to Support Aging Adults, 2019) as well as informal and paid caregivers (LeadingAge, 2011). While there were some suggestions that the workforce may be more efficient with these technologies (Task Force on Research and Development for Technology to Support Aging Adults, 2019), barriers to spread and implementation, including Internet connectivity, privacy issues, and affordability, were discussed as issues of concern (Greenhalgh et al., 2017; LeadingAge, 2011). One key study addressed patient and worker perspectives of the use of technology in LTC, finding that various stakeholders had differing perspectives on which technologies were needed and what was needed to implement them (Peek et al., 2016).
Several studies focused on a particular type of technology (e.g., robots) (Arthanat et al., 2020; Hung et al., 2022; Kangasniemi et al., 2019; Pirhonen et al., 2020), specific conditions (e.g., dementia) (Arthanat et al., 2020; Gettel et al., 2021), and/or specific settings (e.g., assisted living) (Pirhonen et al., 2020). Robotics research is of particular interest as of late. Some felt that that robotics can and will aid nurses and caregivers, although will not act as a replacement for staff (Tietze & McBride, 2020), and others acknowledged the potential of robotics if barriers to adoption were addressed (Arthanat et al., 2020). Conversely, others suggested that robots might increase staff workload due to care and maintenance needs (Hung et al., 2022).
Technology Scan and Taxonomy
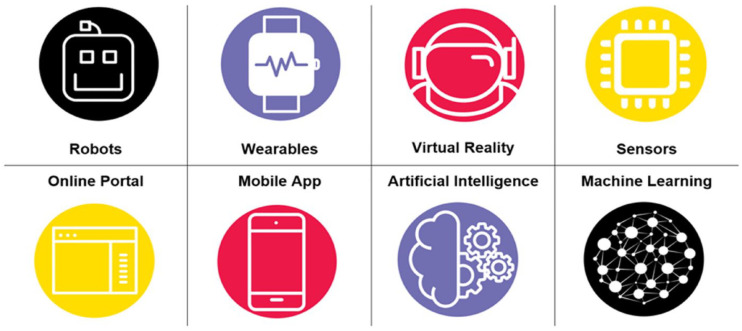
The technology scan identified 115 companies with products or services that met our criteria. Our research team’s consensus process placed these technologies into two separate taxonomies. The technology type taxonomy contained eight categories: robots, wearables, virtual reality, sensors, machine learning, artificial intelligence, online portal, and mobile app (Figure 1). The technology function taxonomy contained 10 categories: RM, alarms/alert systems, workforce recruitment and retention, workforce education, online care management, facility staff management, socialization and games, home-to-health team communication, behavioral health management, and care coordination (Figure 2). We found these categories, technology type and technology function, to be distinct from one another, although many companies incorporated multiple elements in their product/service.
Figure 1.
Taxonomy of Technology Types.
Figure 2.
Taxonomy of Technology Functions.
Table 1 provides a summary of each interviewed company and includes information on product/service taxonomic type(s) and function category(ies), their targeted customer(s), the site(s) in which each of their products was used, and the potential workforce impact. Tables 2 and 3 list the potential workforce impact of these technologies according to each technology type and function, respectively. Many technologies had overlapping types and functions and could have been placed in multiple categories. For example, a sensor could also be a wearable. For purposes of selecting interviewees in each category, we organized technologies by their primary feature and function as described in product/service materials.
Table 1.
Interviewee Summary.
| Company name | Technology type(s) | Technology function(s) | Targeted customer(s) | Site(s) for technology use | Potential workforce impact |
|---|---|---|---|---|---|
| Alma’s House | Robots; sensors | Alarms and alert systems; RM; socialization and games | Individuals with dementia/aging | Dementia Villages; In-home | Extends workforce; system/service integration for efficient/impactful workforce |
| Arena | Machine learning | Workforce recruitment and retention | Health care facilities (e.g., academic medical centers, acute-care hospitals, and long-term care facilities) | Assisted Living; Health Systems; Hospitals | Data insights for workforce practices and visibility; workforce matching |
| Canary Health | Online portal | Workforce education | Caregivers; diabetics; individuals with chronic disease(s) | In-home | Teaches/Educates workforce |
| CarePredict | Machine learning; sensors; wearables | Alarms and alert systems; facility staff management; RM | Individuals requiring home care; long-term care facilities | Assisted Living; In-home; Memory Care; Retirement Communities | Data insights for workforce practices and visibility; extends workforce |
| ClearCare | Mobile app; online portal | Facility staff management; online care management | Home care agencies | In-home | Data insights for workforce practices and visibility; system/service integration for efficient/impactful workforce |
| Intuition Robotics (ElliQ) | Robots | Alarms and alert systems; socialization and games | Individuals aging at home | In-home | Extends workforce |
| Embodied Laboratories | Virtual reality | Workforce education | Health professionals; health care workers; hospital systems; long-term care/senior care facilities | VR laboratory | Teaches/Educates workforce |
| GrandCare® | Online portal; sensors | Alarms and alert systems; home-to-health team communication; online care management; RM; socialization and games | Individuals aging at home | In-home | Extends workforce; system/service integration for efficient/impactful workforce |
| Honor | Machine learning; mobile app; online portal | Workforce education; workforce recruitment and retention | Non-medical home care agencies | In-home | Data insights for workforce practices and visibility; teaches/educates workforce; workforce matching |
| La Valeriane® | Mobile app | Care coordination | Health care professionals; home care agencies; individuals aging at home | Adult Day Care Centers; Assisted Living; In-home; Independent Living; Nursing Homes | Care plan development |
| LifePod™ | Artificial intelligence | Alarms and alert systems; online care management | Individuals aging at home | In-home | Extends workforce |
| UnaliWear™ | Artificial intelligence; sensors; wearables | Alarms and alert systems; RM | Individuals aging at home | In-home | Extends workforce |
| VisibleHand | Mobile app; sensors; wearables | Alarms and alerts; behavioral health management; facility staff management | Addiction treatment centers; hospitals; skilled nursing facilities | Addiction Treatment Centers; Hospitals; Skilled Nursing Facilities | Care plan development; data insights for workforce practices and visibility |
Note. RM = remote monitoring; VR = virtual reality.
Table 2.
Potential Workforce Impact by Technology Type.
| Technology type | Potential workforce impact |
|---|---|
| Robots | Extends workforce; system/service integration for efficient/impactful workforce |
| Wearables | Care plan development; data insights for workforce practices and visibility; extends workforce |
| Virtual reality | Teaches/educates workforce |
| Sensors | Care plan development; data insights for workforce practices and visibility; extends workforce; system/service integration for efficient/impactful workforce |
| Online portal | Data insights for workforce practices and visibility; extends workforce; system/service integration for efficient/impactful workforce; teaches/educates workforce; workforce matching |
| Mobile app | Care plan development; data insights for workforce practices and visibility; system/service integration for efficient/impactful workforce; teaches/educates workforce; workforce matching |
| Artificial intelligence | Extends workforce |
| Machine learning | Data insights for workforce practices and visibility; extends workforce; teaches/educates workforce; workforce matching |
Table 3.
Potential Workforce Impact by Technology Function.
| Technology function | Potential workforce impact |
|---|---|
| RM | Data insights for workforce practices and visibility; extends workforce; system/service integration for efficient/impactful workforce |
| Workforce education | Data insights for workforce practices and visibility; teaches/educates workforce; workforce matching |
| Home-to-health team communication | Extends workforce; system/service integration for efficient/impactful workforce |
| Alarms and alert systems | Care plan development; data insights for workforce practices and visibility; extends workforce; system/service integration for efficient/impactful workforce |
| Socialization and games | Extends workforce; system/service integration for efficient/impactful workforce |
| Workforce recruitment and retention | Data insights for workforce practices and visibility; teaches/educates workforce; workforce matching |
| Facility staff management | Care plan development; data insights for workforce practices and visibility; extends workforce; system/service integration for efficient/impactful workforce |
| Care coordination | Care plan development |
| Online care management | Data insights for workforce practices and visibility; extends workforce; system/service integration for efficient/impactful workforce |
| Behavioral health management | Care plan development; data insights for workforce practices and visibility |
Note. RM = remote monitoring.
Semistructured Interviews
The research team’s qualitative analysis of interviews identified three main themes; existing technology can assist the workforce and support workforce recruitment and retention but cannot replace the workforce.
Technologies That Assist the Workforce
The team found that technology could assist the workforce in four ways by extending the reach of the workforce, facilitating workforce training, integrating systems/services for improved workforce efficiency and impact, and enhancing care plan development.
Extending the Reach of the Workforce
Some technologies may extend the overall reach of workforce members by providing services remotely that were previously provided in face-to-face visits. Depending on situational circumstances, such technologies could allow workforce members the ability to (a) reallocate time to noncaregiving activities to reduce the time burden of providing care, (b) reallocate time to additional caregiving activities to provide more care, and/or (c) have more/better data on patient/client health status that might indicate health changes and thus need for in-person care.
Several technologies with a variety of functions have the potential to assist the workforce in these ways, such as RM. Four of the interviewed companies offered RM technologies as part of their suite of services, most of which focused on providing care to individuals aging in their homes. Examples included integrated glucometers and blood pressure devices to measure health indicators and motion/contact sensors to detect falls. Results and updates provided by these RM devices can be sent to caregivers or other health care team members as desired. If significant changes in health conditions are detected, alerts are sent to emergency medical services and clinical staff. With these RM technologies and subsequent alert systems in place, workforce members in the home and in LTC facilities do not have to be present at all times to intervene and ensure that patients are appropriately assisted when they need help. One interviewee said, “I see this technology as adjunct to the home care worker, and this is how my customers see it, too . . . [this product] can cover additional watch/monitor hours when aides are not able to be there in person.”
Technology can also extend reach by providing clinical reminders/alerts to patients for activities such as taking medications. Four of the interviewed companies included this as a service, two of which incorporated voice-first technology. A representative from one of these voice-first companies explained why their technology facilitates this activity when the worker is not present: “[Our product] provides a sense of connectedness that penetrates socialization and is a new way to remind people to adhere to their protocol without requiring a person calling them in real time or being there physically.”
Other technologies focused on providing alternatives for companionship and social support when workers and/or informal caregivers were unable to be present. This type of technology was primarily used in the home. One such company’s product was a nonhumanoid, lifelike robot that can socialize with the client on its own as well as connect the client with workers, friends, and/or family members virtually. The interviewee explained the value of their product’s features and capabilities that can improve workforce reach:
We are trying to augment caregiving—we are not here to replace family members, friends, pets, or professional caregivers. Caregivers can’t focus on companionship because they are focused on keeping people healthy. “I wish that I could spend more time with my caregiver,” and vice versa, are comments that we get from caregivers and the people that they are caring for. But, shortages of staff time, staff, and money do not always allow for this relationship building to happen.
Facilitating Workforce Training via Novel Teaching/Education Approaches
Two technologies focused on workforce education using novel teaching and educational approaches, one via virtual reality and another through client-centered design, to improve workers’ understanding of their patients’ condition(s) and how to best care for them. A third technology incorporated educational components into their larger effort to improve the home care experience by embedding trainings into their portal to make them easily accessible.
One company, focused on workforce education, emphasized their goal of transforming training by providing workers with educational tools to help patients make lasting, positive changes to their health. Through an asynchronous, client-centered online course, workers learned how to teach clients about their condition, self-care, and self-efficacy. The interviewee explained the intended effect of these training techniques on workers’ clients:
These short, six-week programs are not magic. It’s really about transforming the way that people think, which in turn transforms people’s actions, which transforms wellbeing. By increasing someone’s self-efficacy and confidence, they can set a goal, accomplish it, and empower themselves. Having this transformation allows profound changes to happen under their control.
Taking a different approach, another company provided virtual reality worker training that simulates caregiving scenarios for particular diseases and disabilities that are common among older populations. The interviewed representative from this company explained they believe that
Virtual reality is the best training tool. It’s a tool you can use to put people in situations that are too expensive to replicate or too difficult to replicate. You can do a deep dive into the [patient’s] brain, which is impossible to do in real life.
The interviewee further explained the value of the content that they produced in-house, with actors, to the learning process for trainees:
The complete immersive experience is important. In order to achieve it, you need to see real people. Embodied cognition and the concept of presence learning is key because the body affects learning. This is the idea that you can trick your brain into recalling memories that are not your own.
A third company incorporated ongoing worker training into its app for the nonmedical home care workers it supports. This interviewee explained the difficulty of establishing formalized training procedures for this group of workers:
Training is a tricky subject because the “right” amount of training depends on the [caregiver], client, and agency mix. In essence, this is part of the reason why there was a need for something like [our product]—to form some kind of standard.
These newly developed trainings, which build off established trainings from organizations like the Alzheimer’s Association, are embedded into the app for ease of access. Because this company works with many home care agencies, supervisors from individual agencies often set the details of the training program(s); this allowed for the flexibility and customization needed to fit the needs of each particular agency and/or worker.
Integrating Systems/Services for an Efficient and Impactful Workforce
Many of the technologies integrated workforce management systems and/or care delivery data systems that could communicate across health care teams to enhance the efficiency and impact of the workforce. Two companies and one international organization focused on these types of integration. The latter organization created a testing site for multiple technologies aimed at creating a fully dementia-friendly physical and social living environment. This included a combination of low and high technologies such as light sources in appropriate areas, infrared sensors to detect client movement, and placing furniture strategically. This setting also incorporated well-being technology (e.g., dolls or toys that resemble children or other living beings), easily accessible lines of communication with friends and family, and iPads programmed with memory training tools. This unique, nonprofit partnership between engineering teams and health care experts collaborated on concept design, development, and testing. In describing how these components work together to impact the workforce, the interviewees said,
[Our system provides] more efficient and optimized care, where we can give our users improved safety and higher levels of independence. We are able [to create such a living space] because we look at things from the user’s point of view. The more person-centered our approach becomes, the philosophy becomes ‘tech where possible, and health professionals when needed.
Another company focused on systems to manage workers and business operations more efficiently. In effort to create an all-in-one home care platform, one of their goals was to optimize operations by making improvements in areas such as worker scheduling, billing and payroll, and workers’ access to information. This optimization “improves lower-level tasks to increase the amount of time that be dedicated to other activities.” The interviewee further explained that
By transferring some of these hands-on activities to hands-off, this leaves more time for hands-on activities that actually need to stay hands-on. [Workers can] spend less time on the “prep work” that is necessary to provide care, and more time on the bigger issues of client care—overall, this increases [worker] impact.
Other integration systems focused more heavily on managing different sources of health/activity monitoring for individuals living at home with the goal of identifying when in-person care is most needed. An interviewee from one such company said,
It is our hope to create greater efficiency, and we designed [our product] around this idea. You will always need the RN and the trained person to help you understand what your vitals mean, how and why to take them, and tell you what to do with the results. But how much of that time do you want people to spend driving around [to see clients], especially to see those that don’t actually need attention that day?
The interviewee further explained, “It’s not so much about reducing the number of visits. You should think of it more like visiting the people who really need help in that day.”
Enhancing Care Plan Development
Two interviewed companies had products that focused on creating new and/or enhancing care plan development and documentation tools. In doing so, these technologies aimed to use insights gathered from those tools to gain more clarity into what clients really need. One interviewee explained how their tool’s design improved care plan development:
Our app is “smart” because it assesses three dimensions of daily living—cognitive health, physical condition, and a combination of these two, rather than an ADL/instrumental activities of daily living (IADL) checklist. This allows for 245 levels of assessment . . . which is very precise, allowing for an in-depth assessment, which then creates a good care plan.
However, the use of such tools can lead to a requirement of more documentation for workforce members or, at the very least, more time to learn how to document in a new way, which this company noted as a barrier to product use: “the app creates more of a time burden, which is difficult for some health professionals.” Despite this challenge, the improved documentation tool was perceived as valuable to the workforce: “ . . . many [health professionals] recognize that the app is good and produces results.”Another company explained how their product, which tracks patient behaviors that would have otherwise gone unnoticed to illustrate a more holistic and clearer picture of the patient, allows for enhanced care plan development: “this software helps track which interventions are effective vs. not effective so that care plans can be more effective. This way, care plans are based on behavior patterns rather than in-the-moment reactions.”
Technologies That Support Workforce Recruitment and Retention
The team found that technology could support workforce recruitment and retention by offering workforce matching services and improving workforce deployment models.
Workforce Matching
Two companies focused on workforce matching services; one matched home care workers to clients, and the other matched health care workers to jobs. These matching processes aimed to provide workers and clients with a better work experience and enhance worker job satisfaction, with the added intention of improving retention, according to interviewees.
The company that matched workers to clients “gives [workers] more control over their own lives, allows for more available work, and professionalizes the work . . . the app makes [the workers] smarter because it gives them more tools, which allows them to see the whole picture.” “Tools” included additional information about clients, such as if they had pets, any known allergies, or other living situations that could guide workers’ decisions about whether they would be a good match for a particular client, because their product “allows [workers] to work for the clientele that they want to work for and filters out those with conditions that they don’t want to or can’t handle.” Subsequently, the use of this technology has led to “retention rates that are twice as good as those of ‘normal’ home care aides.” The interviewee explained that this result is probably due to the product “allow[ing] [workers] to optimize their time and provid[ing] them with consistent hours.”
The company that matched workforce members with particular jobs aimed to “find [the workforce member] the right job match.” This could include “suggest[ing] other roles that the person might be a successful fit for, even if it’s not a job that they originally applied for” to ultimately “help workers find work where they will be successful.” By doing so, this product aimed to “give people a more stable workplace and creates a better environment for them and everyone around them.” The interviewee also commented on the positive effects they found of improved employee retention, as a result of the technology’s use, on the workforce’s delivery of care: “We’ve seen that as retention is improved, quality metrics and patient metrics, mortality rates, and incidents of falls also improve.”
Workforce Deployment
Four companies recorded and analyzed location-tracking, scheduling, shift, and/or client behavior observation data to gain insights about workforce deployment in LTC facilities. Subsequently, these companies made data-informed adjustments and changes to improve workforce staffing models. Another company gathered data from job applications, puzzle-solving, and third parties to apply predictive analytics to strengthen employers’ hiring decisions.
Two companies emphasized the importance of workforce visibility to inform staffing deployment decisions. One utilized wearables, worn by workers and patients, to collect location and activity tracking data for this purpose as well as to improve workers’ ability to perform their jobs. The interviewee explained how their technology promoted workforce visibility:
Our technology helps retain high performers because it allows organizations to see who the high performers are while also showing who really is not doing their job. It also helps organizations figure out how many staff should be allocated per building, per floor, and per shift.
The interviewee also described how their product made workers’ jobs easier: “We are not trying to replace staff. We pull information to make things easier for staff. It’s about human augmentation.” Another company that utilized machine learning explained how putting data in the hands of their workers positively influenced workforce visibility: “[Our technology] projects the trajectory of the [worker] over time with data . . . which allows the [workers] to see if they are trending in a negative or positive way.”
Two companies described the importance of relying on observational data rather than anecdotal perceptions to provide accurate, actionable insights for workforce deployment. One interviewee explained, “you can’t rely on what [workers] tell you are their ‘absolute requests’ because, in reality, some of those requests are not truly deal breakers. Observational data matters more than what [a worker] says they will or will not do.” Another interviewee explained how hiring practices and retention rates were improved using predictive analytic models that rely on observational data rather than on managers’ rankings of employees: “We found these data [on forced employee rankings] to be very unreliable. In one example, the forced ranks changed significantly even after four months . . . Because of these lessons learned, we can now build more accurate models out of the gate.”
Technology Does not Replace the Workforce
There was little mention from interviewees about the potential for technologies to replace workers, and none of the interviewees made a strong claim that their products or services, as currently configured and functioning, could replace workers. One interviewee stated that
Robots and humans are still about 30 years apart from each other. It will be a while before we get to the point where robots may replace humans. Until then, device intervention . . . could impact the world by making it so that fewer hours are required for care.
Discussion and Implications
Our research focused on emerging technologies aimed at improving the care of older and/or disabled adults and how those technologies might impact the workforce in the home and LTC settings. The CAST paradigm for technology-enabled geriatric care envisions a system where technology products and services work to streamline care, enhance communication between the caregiving team, improve quality of care and life, and potentially lower costs of care (LeadingAge, 2011). The impact of that paradigm on the workforce has potential for creating greater efficiency, better data, more effective monitoring, and preventive interventions. These technologies may also lead to more satisfied clients and workers. However, challenges to widespread adoption remain, such as patient/client acceptance, ease of use, Internet connectivity (especially in rural areas), privacy concerns, cost-effectiveness, regulatory standards, and reimbursement (Greenhalgh et al., 2017; LeadingAge, 2011; Qian et al., 2019; Schulz, 2013; Tak et al., 2010; Taylor et al., 2016; U.S. Department of Health and Human Services Office of Disability Aging and Long-Term Care Policy and the National Opinion Research Center, 2012).
The looming workforce shortages in LTC are cause for concern (Institute on Medicine [US] Committee on the Future Health Care Workforce for Older Americans, 2008; Spetz et al., 2015) and lend importance to research of technology’s ability to assist the workforce, which could mitigate these shortages. It is worth considering whether technology could eventually take the place of workers. Although none of our study interviewees reported that replacement of the workforce is on or near the horizon, there is considerable speculation of robots’ potential to assist with nursing services. Findings show that while robots could assist with hospital-based nursing services in functions such as lifting patients from beds and chairs, delivering supplies and medication dispensing systems, and fall detection devices, further research and evaluation are needed on functionality impact on nursing practice (Carter-Templeton et al., 2018; Kangasniemi et al., 2019; Tietze & McBride, 2020). Furthermore, much of this technology is still in development or requires human presence to participate in its use (Woollaston, 2015). Other studies and reports focused on robotics’ potential to create social interactions in place of humans, which found that while robots may enhance staff capacity and fulfill certain social roles, concerns such as privacy, cost, safety, resident confusion, decreasing human connection, and the potential to increase workload for staff in cleaning and maintaining the robots were of import (Abbasi, 2017; Hung et al., 2022; Pirhonen et al., 2020).
Most company interviewees emphasized that their products/services were instead designed to complement the work of staff and thus benefit the workforce in some way, whether through optimizing their tasks, improving workers’ understanding of a patient’s situation, providing important updates about patients, improving workers’ ability to provide better-coordinated care, and/or illuminating important trends that may have otherwise gone unnoticed. The intended results of these benefits are largely to make the jobs of workers easier, more satisfying, and/or to improve the quality of care that workers provide to their patients. In addition, because many of these companies’ products/services included multiple elements or features, which was especially true of the products/services focused on systems and services integration, several technologies had the potential to impact the workforce in multiple ways.
Earlier reviews of technology have critiqued the lack of rigorous studies of the efficacy of much of the technology developed for LTC (Tak et al., 2010), and there continue to be few published studies of the outcomes of these emerging technologies (Armitage et al., 2020). A few interviewees noted they were developing research partnerships to study outcomes of their technologies. However, conducting a rigorous controlled trial of technology already in the field could present challenges to a company’s product/service and funding if efficacy is found to be limited. One example of a research and design partnership that included rigorous product and service evaluation before going to market was the international site selected for this study. The partnership was a developmental laboratory, which included input and evaluation from engineering and design teams, the government, and the health and social service sectors. This model could be adopted more widely if funding was found to support this approach.
There are several limitations to this study. The technology scan may have missed some technologies depending upon the search term(s) used and when the scan was conducted. In addition, we acknowledge that the scope of this project did not include a systematic review of the literature.
Due to project resources, we were only able to interview a limited number of companies; the interviewed companies may not be representative of all companies, products, and services in their particular technological type or function category. We conducted most of the interviews remotely and did not obtain real-world observations or collect data on whether products/services always worked as described. However, interviewees were open about the challenges they encountered with their products/services. This study did not include interviews of LTC providers nor individuals or families who use LTC services who might have additional and/or differing perspectives on the workforce implications of technology in LTC.
Conclusion
The rapidly aging population in the United States, coupled with a projected LTC worker shortage, is creating an increased need for LTC workers. The emergence of technology in care systems has the potential to assist the LTC workforce in doing their job as well as support worker recruitment and retention but is not currently capable of replacing workforce members. While emerging technology has the potential to assist the LTC workforce with efficiency, workload management, and staff training, many challenges to widespread adoption remain.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling US$533,932.00, with 0% financed with nongovernmental sources. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.
ORCID iDs: Jacqueline R. Miller  https://orcid.org/0000-0002-6535-1210
https://orcid.org/0000-0002-6535-1210
Joanne Spetz  https://orcid.org/0000-0003-3112-5511
https://orcid.org/0000-0003-3112-5511
References
- Abbasi J. (2017). Socially assistive robots help patients make behavioral changes. Journal of the American Medical Association, 317(24), 2472–2474. 10.1001/jama.2017.5682 [DOI] [PubMed] [Google Scholar]
- Armitage L. C., Kassavou A., Sutton S. (2020). Do mobile device apps designed to support medication adherence demonstrate efficacy? A systematic review of randomised controlled trials, with meta-analysis. BMJ Open, 10(1), Article e032045. 10.1136/bmjopen-2019-032045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthanat S., Begum M., Gu T., LaRoche D. P., Xu D., Zhang N. (2020). Caregiver perspectives on a smart home-based socially assistive robot for individuals with Alzheimer’s disease and related dementia. Disability and Rehabilitation: Assistive Technology, 15(7), 789–798. 10.1080/17483107.2020.1753831 [DOI] [PubMed] [Google Scholar]
- Binette J., Vasold K. (2018). 2018 Home and community preferences: A national survey of adults ages 18-plus. AARP. https://www.aarp.org/research/topics/community/info-2018/2018-home-community-preference.html [Google Scholar]
- Bradley E. H., Curry L. A., Devers K. J. (2007). Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Services Research, 42(4), 1758–1772. 10.1111/j.1475-6773.2006.00684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Carter-Templeton H., Frazier R. M., Wu L. T. H. W. (2018). Robotics in nursing: A bibliometric analysis. Journal of Nursing Scholarship, 50(6), 582–589. 10.1111/jnu.12399 [DOI] [PubMed] [Google Scholar]
- Chapman S. A., Spetz J., Lin J., Chan K., Schmidt L. A. (2016). Capturing heterogeneity in medical Marijuana Policies: A taxonomy of regulatory regimes across the United States. Substance Use & Misuse, 51(9), 1174–1184. 10.3109/10826084.2016.1160932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovey S. M., Meyers D. S., Phillips R. L., Jr., Green L. A., Fryer G. E., Galliher J. M., Kappus J., Grob P. (2002). A preliminary taxonomy of medical errors in family practice. Quality & Safety in Health Care, 11(3), 233–238. 10.1136/qhc.11.3.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffin E. (2022). Share of old age population (65 years and older) in the total U.S. population from 1950 to 2050. Statista. [Google Scholar]
- Gettel C. J., Chen K., Goldberg E. M. (2021). Dementia care, fall detection, and ambient-assisted living technologies help older adults age in place: A scoping review. Journal of Applied Gerontology, 40(12), 1893–1902. 10.1177/07334648211005868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T., Wherton J., Papoutsi C., Lynch J., Hughes G., A’Court C., Hinder S., Fahy N., Procter R., Shaw S. (2017). Beyond adoption: A new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. Journal of Medical Internet Research, 19(11), Article e367. 10.2196/jmir.8775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houser A., Fox-Grange W., Ujvari K. (2012). Across the States 2012: Profiles of long term services and supports. AARP. https://www.aarp.org/home-garden/livable-communities/info-09-2012/across-the-states-2012-profiles-of-long-term-services-supports-AARP-ppi-ltc.html [Google Scholar]
- Hung L., Mann J., Perry J., Berndt A., Wong J. (2022). Technological risks and ethical implications of using robots in long-term care. Journal of Rehabilitation and Assistive Technologies Engineering, 9, 20556683221106917. 10.1177/20556683221106917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute on Medicine (US) Committee on the Future Health Care Workforce for Older Americans. (2008). Retooling for an aging America: Building the health care workforce. National Academies Press. 10.17226/12089 [DOI] [PubMed] [Google Scholar]
- Kangasniemi M., Karki S., Colley N., Voutilainen A. (2019). The use of robots and other automated devices in nurses’ work: An integrative review. International Journal of Nursing Practice, 25(4), Article e12739. 10.1111/ijn.12739 [DOI] [PubMed] [Google Scholar]
- LeadingAge. (2011). State of technology in aging services report. http://hweb.leadingage.org/State_of_Technology_in_Aging_Services_Report.aspx
- Peek S. T., Wouters E. J., Luijkx K. G., Vrijhoef H. J. (2016). What it takes to successfully implement technology for aging in place: Focus groups with stakeholders. Journal of Medical Internet Research, 18(5), Article e98. 10.2196/jmir.5253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- PHI. (2021). Caring for the future: The power and potential of America’s direct care workforce. https://www.phinational.org/wp-content/uploads/2021/01/Caring-for-the-Future-2021-PHI.pdf
- Pirhonen J., Melkas H., Laitinen A., Pekkarinen S. (2020). Could robots strengthen the sense of autonomy of older people residing in assisted living facilities?–A future-oriented study. Ethics and Information Technology, 22(2), 151–162. 10.1007/s10676-019-09524-z [DOI] [Google Scholar]
- Pope C., Mays N. (2006). Qualitative research in health care (3rd ed.). Blackwell Publishing. [Google Scholar]
- Qian S., Yu P., Bhattacherjee A. (2019). Contradictions in information technology mediated work in long-term care: An activity theoretic ethnographic study. International Journal of Nursing Studies, 98, 9–18. 10.1016/j.ijnurstu.2019.05.017 [DOI] [PubMed] [Google Scholar]
- Schulz R. (2013). Quality of life technology handbook. Taylor & Francis. [Google Scholar]
- Spetz J., Trupin L., Bates T., Coffman J. M. (2015). Future Demand for long-term care workers will be influenced by demographic and utilization changes. Health Affairs, 34(6), 936–945. 10.1377/hlthaff.2015.0005 [DOI] [PubMed] [Google Scholar]
- Tak S. H., Benefield L. E., Mahoney D. F. (2010). Technology for long-term care. Research in Gerontological Nursing, 3(1), 61–72. 10.3928/19404921-20091103-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Task Force on Research and Development for Technology to Support Aging Adults. (2019). Emerging technologies to support an aging population. https://trumpwhitehouse.archives.gov/wp-content/uploads/2019/03/Emerging-Tech-to-Support-Aging-2019.pdf
- Taylor A., Wade V., Morris G., Pech J., Rechter S., Kidd M., Carati C. (2016). Technology support to a telehealth in the home service: Qualitative observations. Journal of Telemedicine and Telecare, 22(5), 296–303. 10.1177/1357633X15601523 [DOI] [PubMed] [Google Scholar]
- Tietze M., McBride S. (2020). Robotics and the impact on nursing practice. https://www.nursingworld.org/~494055/globalassets/innovation/robotics-and-the-impact-on-nursing-practice_print_12-2-2020-pdf-1.pdf
- United Nations Department of Economic and Social Affairs Population Division. (2020). World population ageing: Highlights. https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/undesa_pd-2020_world_population_ageing_highlights.pdf
- U.S. Bureau of Labor Statistics. (2021). Occupational outlook handbook: Home health and personal care aides. https://www.bls.gov/ooh/healthcare/home-health-aides-and-personal-care-aides.htm
- U.S. Department of Health and Human Services Office of Disability Aging and Long-Term Care Policy and the National Opinion Research Center. (2012). Report to congress: Aging services technology study. https://aspe.hhs.gov/basic-report/report-congress-aging-services-technology-study
- Usman M., Britto R., Börstler J., Mendes E. (2017). Taxonomies in software engineering: A Systematic mapping study and a revised taxonomy development method. Information and Software Technology, 85, 43–59. https://doi.org/https://doi.org/10.1016/j.infsof.2017.01.006 [Google Scholar]
- Woollaston V. (2015, February 24). Meet Robear, the “Nurse” with the strength of a robot and face of a bear: Gentle droid giant lifts patients from beds and chairs. Daily Mail. https://www.dailymail.co.uk/sciencetech/article-2966380/Japans-Robear-Strength-robot-face-bear.html