Abstract
SIGNIFICANCE
Although the myopia control efficacy of orthokeratology lenses has been established with clinical trials, reports of axial length change in non–study-based patient care are scarce. This study investigates the use of orthokeratology lenses for myopia control in a clinical population and compares axial elongation against those published in recent clinical investigations.
PURPOSE
This study aimed to investigate factors affecting axial elongation during use of orthokeratology lenses for myopia control in an academic clinical setting.
METHODS
This study was a retrospective consecutive case series from the Myopia Control Clinic at the Herbert Wertheim School of Optometry at the University of California, Berkeley (Berkeley, CA). Patients ranging from 5 to 18 years old using orthokeratology for at least 1 year were included in the study. Data from 102 patients' eyes were analyzed at baseline (before the initiation of treatment) and after 1 year of wear (12 ± 3 months). Multivariate analysis was undertaken to identify factors significantly associated with axial elongation over this period.
RESULTS
Mean (±standard deviation) spherical equivalent refraction and axial length at baseline were −2.54 (±1.21) D and 24.53 (±0.82) mm, respectively. By the 1-year follow-up, eyes had shown significant axial elongation (0.18 ± 0.24 mm; P < .001), which was found to be inversely correlated with age (P < .001). Race, sex, baseline axial length, and baseline refraction were not significantly associated with axial elongation.
CONCLUSIONS
Factors influencing axial length and the magnitude of axial elongation in our orthokeratology patient population are consistent with orthokeratology treatment groups from published randomized clinical trials and support the use of these lenses for myopia control in a clinical practice setting.

Myopia is caused by a mismatch between the refractive power of the eye and the eye's axial length, which typically results from excessive elongation of the eye during childhood and/or adolescence. A meta-analysis predicted that myopia (−0.50 D or less) and high myopia (−5.00 D or less) will affect nearly 5 billion people and 1 billion people, respectively, or approximately 50 and 10% of the world's population, by the year 2050.1 Although high myopia is considerably more prevalent in Asian countries, an eightfold increase in severe myopia has also been identified in the United States over a 30-year time span.2 This is especially concerning because the higher the degree of myopia, the higher the risk for associated complications including glaucoma, retinal detachment, and myopic maculopathy.3 Because myopia prevalence around the modern world has increased, there has been an increasing interest in controlling myopia progression to limit both the individual and public health consequences.
There is now convincing evidence that it is possible to slow the progression of myopia in children through optical, pharmaceutical, or behavioral interventions, collectively referred to as “myopia control.”4 Orthokeratology lenses, atropine eye drops, novel spectacle lenses, and multifocal soft contact lenses have all shown statistically significant and clinically meaningful results in multiple randomized clinical trials.5,6 The effectiveness of orthokeratology, specifically as a myopia-controlling treatment, has been demonstrated in many studies,7–13 and a meta-analysis found that orthokeratology produces a mean reduction in axial elongation of 0.26 mm after 2 years of treatment compared with controls.14 These reports have inspired an increased use of orthokeratology in clinical practice in young patients for this purpose. However, randomized clinical trials differ from clinical practice in that they create a highly controlled environment with specific inclusion and exclusion criteria and adherence to a pre-specified protocol, among other factors. Compliance with treatment is generally high, and subjects may be removed from analysis if compliance does not meet pre-specified levels. Although this type of research is critical in understanding the mechanisms of myopia control and treatment efficacy, it has been suggested that randomized clinical trials may not directly translate to the care of patients, because clinical study protocols may be difficult or impossible to replicate.15 Consequently, it would be valuable to know if the axial length changes reported in randomized clinical trials are comparable with the changes in axial length observed in clinical practice. The purpose of this study was to analyze axial elongation observed in patients undergoing overnight orthokeratology lens treatment in the Myopia Control Clinic at the Herbert Wertheim School of Optometry at the University of California, Berkeley (Berkeley, CA).
METHODS
Study Design
This study was a retrospective consecutive case series of patients who were seen at the UC Berkeley Herbert Wertheim School of Optometry Myopia Control Clinic, between the time that the clinic was first opened in August 2013 and January 2020. Regardless of the overall length of a patient's treatment, axial length changes from patients' first year of treatment were analyzed for this report. This research was reviewed by the institutional review board at the University of California, Berkeley, and conforms to the principles and applicable guidelines for the protection of human subjects in biomedical research. Health Insurance Portability and Accountability Act compliance was maintained by mining deidentified data, which were stored separately from clinic records.
Study Participants
Because this was a retrospective analysis, no participant recruitment was required. Rather, all patients presenting to the Myopia Control Clinic were considered. The patient population is primarily composed of children and adolescents from the San Francisco Bay Area and surrounding communities. Patients between the ages of 5 and 18 years at treatment initiation with no systemic diseases, no ocular diseases, and no prior myopia control treatment were considered eligible for this report. Specific inclusion and exclusion criteria are listed in Table 1. Cycloplegic refractive error (achieved using a single drop of either 1% cyclopentolate or 1% tropicamide, depending on the practitioner) and keratometry values were determined via autorefraction using the NIDEK Tonoref II (NIDEK, Gamagori, Japan) from an average of three measures per eye. Patient records were excluded from the analysis if there was no axial length measurement recorded at the baseline visit, the annual follow-up visit fell outside of the 1-year (±3 months) window, or the patient chose to pursue an alternative myopia control treatment, such as atropine drops or multifocal soft contact lenses. The follow-up visit restriction was chosen to facilitate the comparison of these results to those of previously published clinical trials.
TABLE 1.
Inclusion criteria
| Age | • 5–18 y old at treatment onset |
| Refractive error | • Spherical equivalent myopia ≥−0.50 and ≤−6.00 D* • With-the-rule astigmatism (axes, 180 ± 30) ≤1.75 D* |
| Keratometry | • Flat K >37.00 D • Flat K (refractive correction) >36.00 D |
| Visual acuity | • Best-corrected visual acuity 20/20 or better |
| Ocular health | • Intraocular pressure ≤21 mmHg • No ocular diseases, including keratoconus (confirmed via pre-treatment corneal topography) |
| Other | • No systemic diseases • No history of OK or contact lens wear • No concurrent use of atropine |
*Indications for fitting Paragon CRT lenses. K = keratometry; OK = orthokeratology.
Treatment
Evaluation for orthokeratology treatment eligibility, lens fitting, training, and follow-up care was provided by third- and fourth-year student clinicians enrolled at the UC Berkeley School of Optometry, with oversight from resident optometrists and clinical faculty, per the school's standard procedures. All patients in this report were fitted with Paragon CRT (Corneal Reshaping Technology) or Paragon CRT Dual Axis (DA) lenses (Paragon Vision Sciences; CooperVision Specialty Eyecare, Mesa, AZ). These lenses combine a reverse-geometry design with a high-Dk gas-permeable material, HDS 100 (paflufocon D), and are Food and Drug Administration approved for overnight wear without age restrictions for the temporary reduction of myopia, not myopia control. They are indicated to correct myopia up to −6.00 D with or without astigmatism up to −1.75 D and are fully customizable by lens power, color, diameter, base curve, and center thickness. Both spherical and DA designs were prescribed to achieve the best fit for the patient. Generally, spherical lenses were indicated for patients with less than 0.75 D of corneal astigmatism, whereas DA designs were used to enhance the fit between the cornea and lens in eyes with greater than 0.75 D of corneal astigmatism, particularly in cases of limbus-to-limbus astigmatism. All lenses were evaluated by an attending optometrist who was certified to fit these lenses.
Lenses were considered dispensable when they met the following criteria: (1) the lens was centered on the cornea with sufficient movement, (2) the lens had an approximately 3- to 4-mm central treatment zone based on sodium fluorescein evaluation, (3) a uniform landing of the lens on the midperipheral corneal region was observed, and (4) appropriate edge lift was observed. An example of an ideal fitting lens is shown in Fig. 1. Lenses were dispensed after the patient and/or parent demonstrated appropriate lens application, removal, and care. Patients were provided with a DMV plunger (DMV Corporation, Zanesville, OH) for lens removal and a Boston Simplus starter kit (Bausch + Lomb, Bridgewater, NJ) for lens cleaning and care and were instructed to replace their contact lens case every 3 months. Once dispensed, lenses were prescribed for nightly use, with a minimum suggested wear time of 8 hours. Follow-up visits were scheduled for 1 day (the morning after the first night of lens wear), 1 week, 1 month, and then every 3 to 4 months thereafter.
FIGURE 1.

Standard sodium fluorescein pooling pattern for a properly fit Paragon CRT lens. An ideal-fitting Paragon CRT lens displaying an appropriate-sized treatment zone, good centration, and the characteristic “bull's-eye” sodium fluorescein pattern with good edge clearance.
Primary Outcome Measure
Axial length measurements were taken before treatment initiation (baseline) and 12 months after the start of treatment using the IOLMaster 500 (Zeiss Meditec, Dublin, CA). A single machine was used to collect this information by a resident optometrist, clinical faculty, or trained student clinician. For each axial length value, five consecutive measurements within 0.05 mm of each other were obtained per the manufacturer's recommendation, and the mean of these five measurements was calculated and documented and used as the primary outcome measure.
Statistical Methods
All statistical testing was performed using Stata, version 14 (College Station, TX). Student t tests were used for difference in comparisons of means between groups, and paired t tests were used to analyze changes in axial length at yearly follow-ups. A multivariable regression analysis was used to explore the impact of baseline axial length, baseline refraction (sphere, cylinder, and calculated spherical equivalent), sex, and ethnicity on axial length growth during the first year of treatment.
RESULTS
Charts from all patients who visited the UC Berkeley School of Optometry Myopia Control Clinic from November 3, 2013, to January 29, 2020, were reviewed. The report yielded a total of 11,375 visit records, which were reviewed, and 10,579 irrelevant visits were removed. A total of 796 patients were considered, of which 375 were using orthokeratology lenses. Orthokeratology wearers were excluded from our analysis if they were already using orthokeratology at the time of their initial visit in the Myopia Control Clinic (n = 35), there was no baseline axial length measurement listed in the report (n = 109), or their 1-year follow-up visit did not fall within the pre-determined interval of 1 year ± 3 months from the date that lens wear was initiated (n = 129). In total, 102 met all the inclusion criteria, as outlined in Fig. 2, and were included in our analysis.
FIGURE 2.
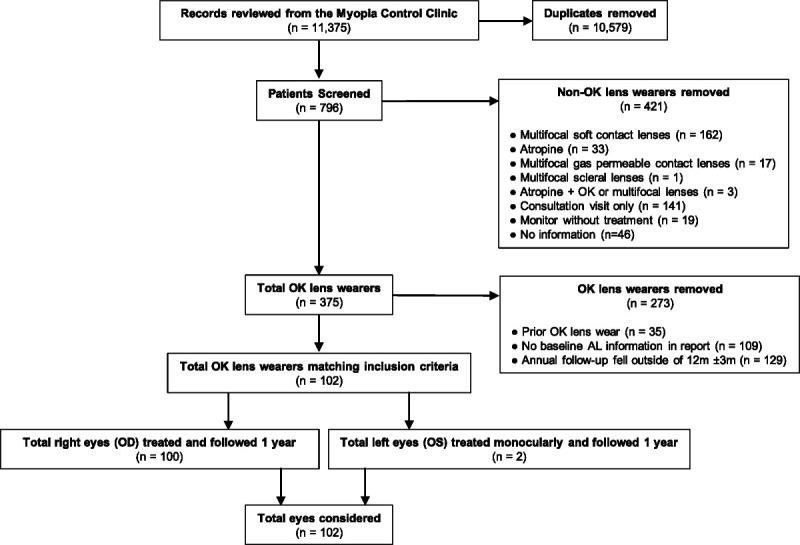
Flow diagram summarizing the search and review process for identifying qualified research patients from the UC Berkeley Myopia Control Clinic.
There were no significant differences between the right and left eyes in terms of baseline refractive error or axial length; therefore, only data from the right eyes were used for analysis, except in cases of monocular treatment when only the left eye was myopic. In total, 102 eyes (100 right eyes and 2 left eyes) from 102 patients were considered.
Baseline and demographic characteristics of patients included in the study are listed in Table 2. Patients ranged in age from 5 to 18 years, with an average age of 10.01 ± 2.43 years. Most patients were between the ages of 6 and 12 years as shown in Fig. 3. Most patients were female (n = 59 [58%]) and of Asian descent (n = 64 [63%]).
TABLE 2.
Baseline and demographic characteristics of participants
| Sex | |
| Female | n = 59 (58%) |
| Male | n = 43 (42%) |
| Race (self-reported) | |
| Asian | n = 64 (63%) |
| White | n = 25 (24%) |
| Black | n = 1 (1%) |
| Native Hawaiian or Pacific Islander | n = 2 (2%) |
| Decline to answer | n = 8 (8%) |
| Unknown (not answered) | n = 2 (2%) |
| Age, mean ± SD (y) | |
| Pooled | 10.01 ± 2.44 |
| Male | 10.19 ± 2.23 |
| Female | 9.88 ± 2.59 |
| Baseline axial length, mean ± SD (mm) | |
| Pooled | 24.53 ± 0.82 |
| Male | 24.71 ± 0.88 |
| Female | 24.41 ± 0.76 |
| Baseline refractive error, mean ± SD (D) | |
| Sphere | −2.31 ± 1.18 |
| Cylinder | −0.46 ± 0.39 |
| Spherical equivalent | −2.54 ± 1.12 |
SD = standard deviation.
FIGURE 3.
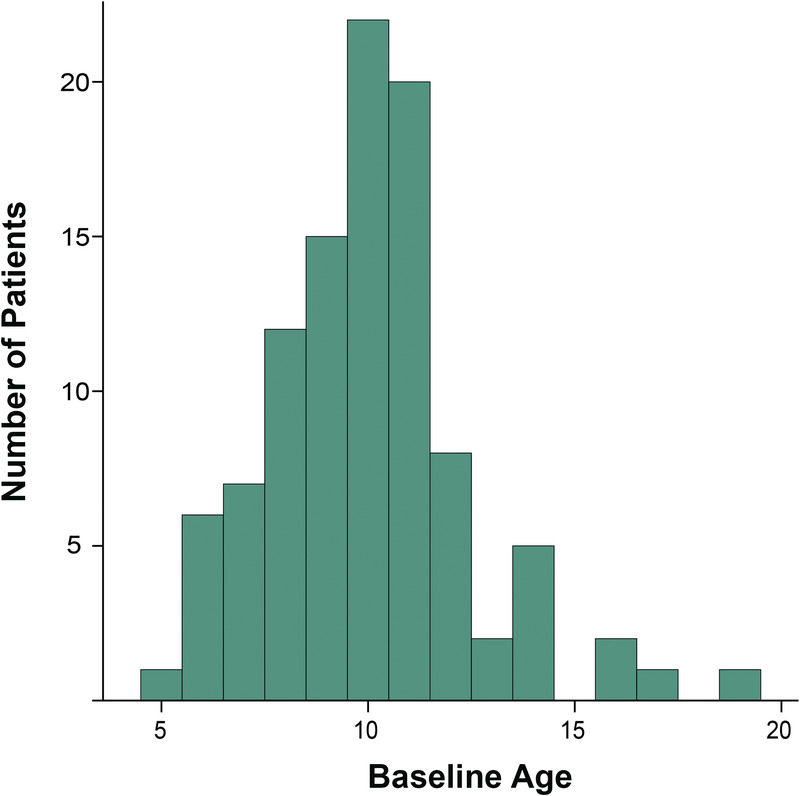
Distribution of age of patients at baseline. Although our inclusion criteria were broad, most treated patients were between the ages of 6 and 12 years, which is similar to most reported clinical trials.
There was no significant difference in baseline refractive error by sex (two-tailed t test, P = .48; Fig. 4A); however, male patients had longer axial lengths than female patients at baseline (one-tailed t test, P = .03; Fig. 4B), despite both sexes being well represented at all ages. Therefore, subgroup analyses of axial length changes were evaluated in addition to the pooled (total) group. Between ethnic groups, there were no significant differences (analysis of variance, P = .32); however, some ethnicities were not well represented. In addition, because Asian eyes have been reported to progress faster than other ethnicities,16 Asian versus non-Asian ethnicities were also compared. Asian eyes were not longer than non-Asian eyes at baseline (24.60 ± 0.11 vs. 24.48 ± 0.15 mm, respectively; P = .26), nor were their refractive errors different. Baseline refractive error was not significantly associated with age (P = .64; Fig. 5).
FIGURE 4.
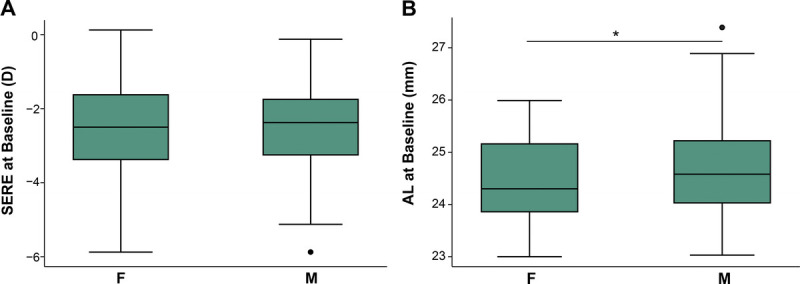
Baseline SEREs and ALs in male and female patients. Male and female patients had similar refractive errors at baseline (A), but male patients had longer ALs than female patients (B). ALs = axial lengths; SEREs = spherical equivalent refractive errors.
FIGURE 5.

Baseline axial length as a function of age. Axial length at baseline is highly dependent on the patient's age, with older patients having longer axial lengths. However, axial lengths were highly variable at all ages. The shaded area represents the 95% confidence interval.
Overall, there was a significant increase in axial length over the 12-month observational period (paired t test, P < .001) as shown in Fig. 6. One patient showed a biologically implausible reduction in axial length after 1 year (−1.89 mm), which is suspected to be due to a charting error and was therefore excluded from further analysis. The average increase in axial length was 0.18 ± 0.24 mm (mean ± standard deviation) overall: 0.16 ± 0.20 mm for female patients and 0.21 ± 0.29 mm for male patients. When comparing the change in axial length in male and female patients, the difference in the rate of axial elongation observed was not statistically significant, despite the baseline difference in axial length (two-sample t test with unequal variance, P = .55). There was no significant difference between ethnicities when considering the change in axial length over time (analysis of variance, P = .51) or comparing the change in axial length for Asian eyes versus non-Asian eyes (two-sample t test, P = .68).
FIGURE 6.
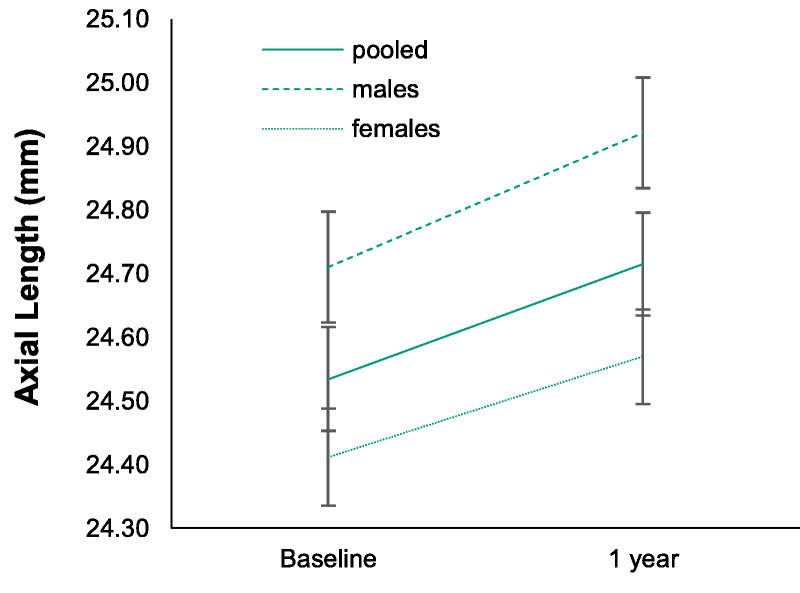
Change in AL over the treatment period. The mean ALs for the total group, male patients, and female patients are plotted over time. The baseline ALs for male and female patients were significantly different at baseline, with male patients having longer baseline ALs than female patients. However, the rate of axial elongation was similar between male patients. Error bars represent the standard error of the mean. AL = axial length.
A multivariable regression was used to consider the relationship between the independent variables, which included baseline axial length, baseline refraction, age, sex, and ethnicity, and the dependent variable, which was the change in axial length during the first year of treatment. Of these factors, the correlation between baseline age and change in axial length was observed to be highly significant (P < .001), meaning that younger patients exhibit faster axial elongation than older patients. The change in axial length was not significantly associated with the baseline axial length (Fig. 7A; P = .55) or the baseline spherical equivalent refractive error (Fig. 7B; P = .65). In addition, the change in axial length was not significantly associated with sex (P = .09) or ethnicity (P = .79; Fig. 8).
FIGURE 7.
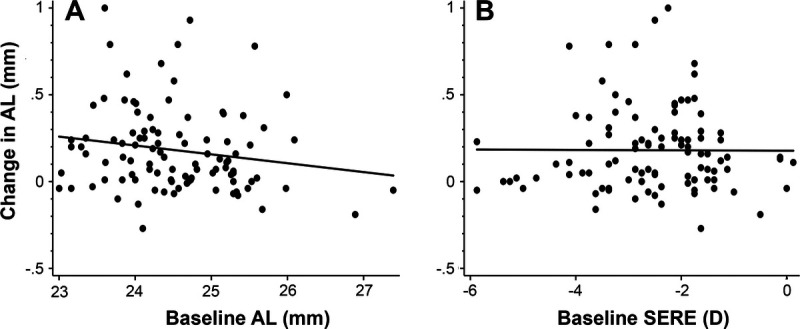
Change in AL during the first year of treatment compared with baseline AL and RE. (A) Change in AL versus baseline AL and (B) SE. AL = axial length; RE = refractive error; SE = spherical equivalent.
FIGURE 8.
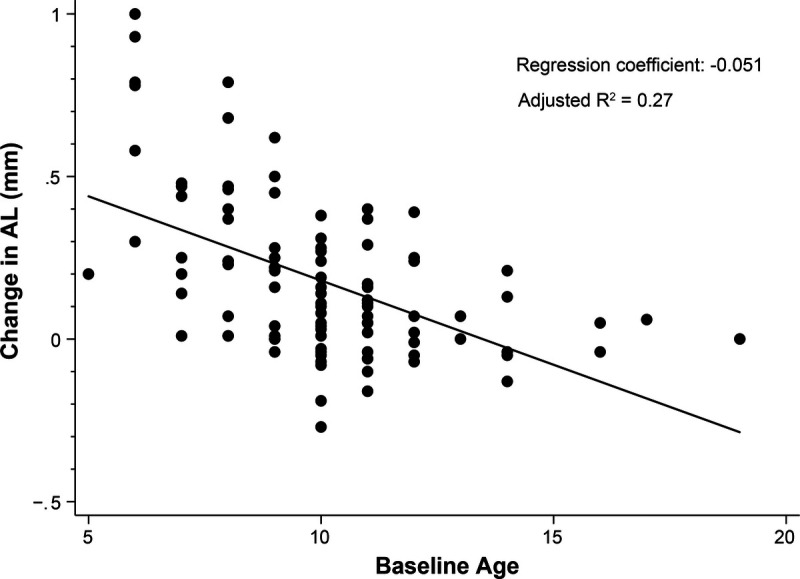
Change in AL during the first year of treatment versus baseline age. The change in AL was significantly related to the patients' age at baseline. AL = axial length.
DISCUSSION
The current study reports the axial length changes observed in neophyte contact lens wearers during their first year of orthokeratology treatment in an academic clinical practice. Orthokeratology is an accepted treatment for myopia control after consistent results from clinical trials that show slowed axial elongation compared with controls. However, it is unknown whether these results translate well to routine clinical care because of factors such as a relatively homogenous distribution of age and refractive error at baseline and strict rules regarding treatment compliance that are demanded of clinical trial participants. Therefore, this investigation sought to explore the relationship between data acquired in a standard optometric practice with data reported in contemporary clinical trials.
These data support that patients who self-select orthokeratology lenses in a clinical practice experience a comparable rate of axial length change with those assigned to treatment groups in clinical trials. The average change in axial length over the first year of treatment with overnight orthokeratology lenses in this study population was 0.18 ± 0.24 mm. Clinical trials and observational studies since the year 2010 that observed subjects younger than 18 years and that reported baseline axial length, axial elongation, and age ranges for the subjects are summarized in Table 3. Most treatment group progression means fall within the range of 0.15 to 0.20 mm/y (range, 0.02 to 0.27 mm/y; Table 3), whereas the axial elongation in the control groups ranged from 0.28 to 0.39 mm/y. These results are strongly encouraging of using orthokeratology lenses for the purpose of myopia control outside of the strict settings of clinical trials.
TABLE 3.
Summary table of the present study results and orthokeratology (OK) myopia control trials and retrospective clinical reports, 2010 to present
| Study | Location | Age (y) | n (OK) | Mean RE at baseline (D) | Mean AL at baseline (mm) | AL increase (mm/y) | Type | |
|---|---|---|---|---|---|---|---|---|
| OK group | Control group | |||||||
| Santodomingo-Rubido et al.16 | Spain | 6–12 | 61 (31) | −2.05 | 24.39 | 0.02 | 0.38 | CT |
| Charm and Cho13 | China | 8–11 | 28 (12) | −6.41 | 26.05 | 0.06 | 0.30 | CT |
| Pauné et al.17* | Spain | 10–15 | 35 (35) | −2.80 | 24.61 | 0.08 | O | |
| Jakobsen and Moller18 | Denmark | 6–12 | 60 (30) | −2.00 | 24.12 | 0.09 | 0.28 | CT |
| Kakita et al.9 | Japan | 8–16 | 92 (42) | −2.55 | 24.66 | 0.15 | 0.30 | CT |
| Chen et al.12 | China | 6–12 | 80 (43) | −2.46 | 24.37 | 0.15 | 0.36 | CT |
| Pauné et al.19 | Spain | 9–16 | 100 (29) | −3.44 | 24.77 | 0.15 | 0.28 | CT |
| Pauné et al.17* | Spain | 10–15 | 36 (36) | −3.41 | 24.69 | 0.16 | O | |
| Zhu et al.20 | China | 7–14 | 128 (65) | −4.29 | 24.91 | 0.16 | 0.39 | O |
| Guo et al.21 | China | 6–11 | 70 (70) | −2.62 | 24.45 | 0.17 | n/a | CT |
| Present study | Berkeley, CA | 5–18 | 102 (102) | −2.54 | 24.51 | 0.18 | O | |
| Qi et al.22 | China | 8–15 | 73 (73) | −3.22 | 24.86 | 0.18 | O | |
| Hiraoka et al.23 | Japan | 8–12 | 59 (29) | −1.89 | 24.09 | 0.19 | 0.38 | O |
| Lin et al.24 | China | 8–14 | 1176 (588) | −2.83 | 24.87 | 0.19 | 0.31 | O |
| Cho and Cheung8 | China | 6–10 | 78 (37) | −2.12 | 24.48 | 0.20 | 0.37 | CT |
| He et al.25 | China | 7–12 | 271 (141) | −2.74 | 24.71 | 0.27 | 0.38 | O |
*Two different lens types from the same clinical study. Age = age range; AL = axial length; n = number of subjects; (OK) = subjects treated with orthokeratology lenses; RE = refractive error; Type = type of trial (CT = prospective clinical trial; O = retrospective observational clinical study).
In the present study, there is a significant individual variability in the change of axial length during the first year of treatment, ranging from −0.3 to greater than +1 mm. The primary factor contributing to this large range of axial length change is the wide distribution of age for the current patient cohort. In this study, baseline age had a strong negative association with change in axial length, meaning that younger patients had more progression than older patients while using orthokeratology lenses. It is well known that there is a reduction in axial elongation with age. This age effect, in addition to the reduction in axial elongation that treatment provides, explains the trend observed in these data.
In the present study cohort, neither baseline axial length nor severity of myopia had a significant impact on axial elongation during orthokeratology treatment. This is consistent with several clinical investigations8,12,16,26 but contradictory to several other previous reports, in which orthokeratology lenses were observed to control myopia more effectively in participants with higher magnitudes of myopia at baseline.9,24,27,28 In comparing the features of this study with previous clinical reports, although the age range of the subjects in the present study was broader than most trials (ages 5 to 18 years were included), the mean age of the study population (10 years) was similar to most published studies (Table 3). There were more female (58%) than male patients in the current study and significantly more patients of Asian ethnicity (63%) than any other racial background. Male patients in this study population had a significantly longer axial length (by approximately 0.30 mm) than female patients at baseline, although there was no significant difference in spherical equivalent refractive error by sex in this patient cohort (Figs. 3A, B). It is well established that male patients have longer axial lengths than female patients in age-matched groups.26
One factor that could account for the observed differences across trials is the different topographical changes induced by orthokeratology lenses. Despite the same brand of orthokeratology lenses used in all patients in the study, factors such as the size of the treatment zone, the magnitude and width of the paracentral steepening, and the asphericity of the central flattened area varied significantly among patients, likely resulting in different “myopia control dosages.” Although the exact dose-dependent relationship between the orthokeratology lens–induced corneal topographic changes and its myopia control efficacy is unclear, results from a recent study suggest that topographical changes such as smaller treatment zone and more dramatic paracentral steepening may be beneficial for the myopia control effect of orthokeratology treatment.17 As research and development in the orthokeratology lens industry continue to evolve alongside improved understanding of the myopia control mechanism of orthokeratology lenses, there is likely to be improved efficacy and better consistency with designing more customized lenses based on the patients' age, level of myopia, corneal shape, pupil size, and angle κ, among other factors.
Interestingly, there were 10 patients who displayed a clinically meaningful decrease in axial length of at least 0.05 mm during their first year of treatment (Fig. 7). The cause of this apparent shortening of axial length remains unclear, although it has been reported in previous clinical trials.7,8 One possible contributing factor was the influence from diurnal variation of axial length. Patients in our clinic are scheduled at their convenience, regardless of the time of day. Significant diurnal variations in axial length have been well documented with an average amplitude of approximately 30 μm (range, 9 to 112 μm).29 The axial length measured with an interferometry-based platform such as the IOLMaster 500 is from the apex of the anterior surface of the cornea to the retinal pigment epithelium. Therefore, variations in axial length could be due to changes in the anterior segment, posterior segment, or a combination of the two. Potential contributing factors to the reduction in axial length are (1) an actual decrease in axial length, (2) increased choroidal thickness,30 and (3) reduced corneal epithelial thickness.31 The relative contributions of these potential influences are yet to be quantified.
A major limitation of this report is the lack of a contemporary control/comparison group. Because axial length is not a routine clinical measure, it was not possible to generate comparative axial length data for myopic patients who were not prescribed a myopia control treatment. Another concern of this retrospective study is regarding the generalizability of these findings, given that the study took place at an academic medical center, which may not directly translate to other primary care settings. However, given that this would likely bias the patient population presented here toward being faster progressors, these results are very encouraging for the use of orthokeratology for myopia control in general practice. Finally, to facilitate comparison with clinical studies investigating orthokeratology for myopia control, it was pre-determined that only patients for whom there were axial length data at baseline and 12 ± 3 months from the baseline would be included, which resulted in a high percentage of patients being excluded from the study. Of all patients being treated with orthokeratology lenses, only 102 were included in the current study. Nonetheless, the risk of selection bias due to high percentage of chart exclusion was low, as there was no significant differences in the age, baseline axial length and refractive error, sex, or ethnicity between the included and the excluded patient records, and there is no reason to believe that patients who returned in our pre-specified follow-up interval would differ in their axial length progression from those who returned outside of that window.
CONCLUSIONS
This study supports that factors influencing axial length and the magnitude of axial elongation observed in clinic-based patients using overnight orthokeratology lenses are comparable with those seen in myopia control trials. In addition, the axial elongation was observed to be negatively correlated with age and not significantly associated with race, sex, baseline axial length, or refractive error. Considering the strong age effect and the irreversible nature of axial elongation, orthokeratology treatment should be initiated as early as possible regardless of the initial level of myopia.
Footnotes
Funding/Support: None of the authors have reported funding/support.
Conflict of Interest Disclosure: The authors ML and SS serve as consultants for CooperVision Specialty EyeCare, which manufactures the lenses used in this report (Paragon CRT and CRT Dual Axis). However, the company did not support or sponsor this research in any way. ML acts as a consultant for Essilor International.
Author Contributions and Acknowledgments: Conceptualization: SS; Data Curation: MH, SS; Formal Analysis: MH, SS; Funding Acquisition: SS; Methodology: MH, SS; Resources: SS; Supervision: SS; Validation: ML; Visualization: SS; Writing — Original Draft: MH, SS; Writing — Review & Editing: ML.
The authors thank Dr. Kathryn Richdale for her time and attention to early drafts of this article. In addition, the authors thank the UC Berkeley School of Optometry Myopia Control Clinic and the associated professors and student clinicians whose patient encounters over the last 7 years are reflected in this study. Finally, many thanks to Nathan Moy for his time in generating the reports of clinic data used in this analysis.
Contributor Information
Michelle Holmes, Email: michelleholmes@me.com.
Maria Liu, Email: marialiu75@berkeley.edu.
REFERENCES
- 1.Holden BA Fricke TR Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036–42. [DOI] [PubMed] [Google Scholar]
- 2.Vitale S, Sperduto RD, Ferris FL, 3rd. Increased Prevalence of Myopia in the United States between 1971–1972 and 1999–2004. Arch Ophthalmol 2009;127:1632–9. [DOI] [PubMed] [Google Scholar]
- 3.Flitcroft DI. The Complex Interactions of Retinal, Optical and Environmental Factors in Myopia Aetiology. Prog Retin Eye Res 2012;31:622–60. [DOI] [PubMed] [Google Scholar]
- 4.Kang P. Optical and Pharmacological Strategies of Myopia Control. Clin Exp Optom 2018;101:321–32. [DOI] [PubMed] [Google Scholar]
- 5.Walline JJ Lindsley KB Vedula SS, et al. Interventions to Slow Progression of Myopia in Children. Cochrane Database Syst Rev 2020;1:CD004916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lam CS Tang WC Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) Spectacle Lenses Slow Myopia Progression: A 2-year Randomised Clinical Trial. Br J Ophthalmol 2020;104:363–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho P, Cheung SW, Edwards M. The Longitudinal Orthokeratology Research in Children (LORIC) in Hong Kong: A Pilot Study on Refractive Changes and Myopic Control. Curr Eye Res 2005;30:71–80. [DOI] [PubMed] [Google Scholar]
- 8.Cho P, Cheung SW. Retardation of Myopia in Orthokeratology (ROMIO) Study: A 2-year Randomized Clinical Trial. Invest Ophthalmol Vis Sci 2012;53:7077–85. [DOI] [PubMed] [Google Scholar]
- 9.Kakita T, Hiraoka T, Oshika T. Influence of Overnight Orthokeratology on Axial Elongation in Childhood Myopia. Invest Ophthalmol Vis Sci 2011;52:2170–4. [DOI] [PubMed] [Google Scholar]
- 10.Walline JJ, Jones LA, Sinnott LT. Corneal Reshaping and Myopia Progression. Br J Ophthalmol 2009;93:1181–5. [DOI] [PubMed] [Google Scholar]
- 11.Santodomingo-Rubido J Villa-Collar C Gilmartin B, et al. Myopia Control with Orthokeratology Contact Lenses in Spain: A Comparison of Vision-related Quality-of-life Measures between Orthokeratology Contact Lenses and Single-vision Spectacles. Eye Contact Lens 2013;39:153–7. [DOI] [PubMed] [Google Scholar]
- 12.Chen C, Cheung SW, Cho P. Myopia Control Using Toric Orthokeratology (TO-SEE Study). Invest Ophthalmol Vis Sci 2013;54:6510–7. [DOI] [PubMed] [Google Scholar]
- 13.Charm J, Cho P. High Myopia-partial Reduction Ortho-K: A 2-year Randomized Study. Optom Vis Sci 2013;90:530–9. [DOI] [PubMed] [Google Scholar]
- 14.Si JK Tang K Bi HS, et al. Orthokeratology for Myopia Control: A Meta-analysis. Optom Vis Sci 2015;92:252–7. [DOI] [PubMed] [Google Scholar]
- 15.Jampol LM, Schmidt-Erfurth UM. Clinical Practice Settings vs Clinical Trials: Is Artificial Intelligence the Answer? JAMA Ophthalmol 2020;138:5–6. [DOI] [PubMed] [Google Scholar]
- 16.Santodomingo-Rubido J Villa-Collar C Gilmartin B, et al. Long-term Efficacy of Orthokeratology Contact Lens Wear in Controlling the Progression of Childhood Myopia. Curr Eye Res 2017;42:713–20. [DOI] [PubMed] [Google Scholar]
- 17.Pauné J Fonts S Rodriguez L, et al. The Role of Back Optic Zone Diameter in Myopia Control with Orthokeratology Lenses. J Clin Med 2021;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jakobsen TM, Moller F. Control of Myopia Using Orthokeratology Lenses in Scandinavian Children Aged 6 to 12 Years. Eighteen-month Data from the Danish Randomized Study: Clinical study Of Near-sightedness; Treatment with Orthokeratology Lenses (CONTROL Study). Acta Ophthalmol 2022;100:175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pauné J Morales H Armengol J, et al. Myopia Control with a Novel Peripheral Gradient Soft Lens and Orthokeratology: A 2-year Clinical Trial. Biomed Res Int 2015;2015:507572–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhu MJ Feng HY He XG, et al. The Control Effect of Orthokeratology on Axial Length Elongation in Chinese Children with Myopia. BMC Ophthalmol 2014;14:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo B Cheung SW Kojima R, et al. One-year Results of the Variation of Orthokeratology Lens Treatment Zone (VOLTZ) Study: A Prospective Randomised Clinical Trial. Ophthalmic Physiol Opt 2021;41:702–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qi Y Liu L Li Y, et al. Factors Associated with Faster Axial Elongation after Orthokeratology Treatment. BMC Ophthalmol 2022;22:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hiraoka T Kakita T Okamoto F, et al. Long-term Effect of Overnight Orthokeratology on Axial Length Elongation in Childhood Myopia: A 5-year Follow-up Study. Invest Ophthalmol Vis Sci 2012;53:3913–9. [DOI] [PubMed] [Google Scholar]
- 24.Lin W Li N Lu K, et al. The Relationship between Baseline Axial Length and Axial Elongation in Myopic Children Undergoing Orthokeratology. Ophthalmic Physiol Opt 2023;43:122–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.He M Du Y Liu Q, et al. Effects of Orthokeratology on the Progression of Low to Moderate Myopia in Chinese Children. BMC Ophthalmol 2016;16:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hyman L Gwiazda J Hussein M, et al. Relationship of Age, Sex, and Ethnicity with Myopia Progression and Axial Elongation in the Correction of Myopia Evaluation Trial. Arch Ophthalmol 2005;123:977–87. [DOI] [PubMed] [Google Scholar]
- 27.Wang B, Naidu RK, Qu X. Factors Related to Axial Length Elongation and Myopia Progression in Orthokeratology Practice. PLoS One 2017;12:e0175913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fu AC Chen XL Lv Y, et al. Higher Spherical Equivalent Refractive Errors Is Associated with Slower Axial Elongation Wearing Orthokeratology. Cont Lens Anterior Eye 2016;39:62–6. [DOI] [PubMed] [Google Scholar]
- 29.Chakraborty R, Read SA, Collins MJ. Diurnal Variations in Axial Length, Choroidal Thickness, Intraocular Pressure, and Ocular Biometrics. Invest Ophthalmol Vis Sci 2011;52:5121–9. [DOI] [PubMed] [Google Scholar]
- 30.Read SA Fuss JA Vincent SJ, et al. Choroidal Changes in Human Myopia: Insights from Optical Coherence Tomography Imaging. Clin Exp Optom 2019;102:270–85. [DOI] [PubMed] [Google Scholar]
- 31.Lau JK Wan K Cheung SW, et al. Weekly Changes in Axial Length and Choroidal Thickness in Children during and following Orthokeratology Treatment with Different Compression Factors. Trans Vis Sci Tech 2019;8:9. [DOI] [PMC free article] [PubMed] [Google Scholar]


