Abstract
Background:
High-contrast visual acuity (HCVA) changes with age, yet little is known about pediatric-specificage-and sex-normative values for low-contrast letter acuity (LCLA). We define maturational changes in monocular and binocular HCVA and LCLA in childhood and adolescence.
Methods:
Normally sighted youth (ages 5–20 years, without neurologic or ophthalmologic disease and best-corrected HCVA of 20/25 or better in each eye) were recruited. Mean monocular and binocular scores using Early Treatment Diabetic Retinopathy Study (for HCVA) and 2.5% and 1.25% Sloan (for LCLA) charts and the magnitude of binocular summation were calculated using 2-year bins. Relationships between scores and age were explored using scatterplots with Locally Weighted Scatterplot Smoothing (LOWESS) and analysis of variance that accounts for intereye correlation, followed by test of linear trend for age effect.
Results:
Among 101 (202 eyes) healthy participants (mean age 13 years, 42% males), monocular and binocular scores varied by age, with highest mean scores achieved in the 13 to 14–year age group for both HCVA and LCLA. Between the ages of 5 and 14.9 years, monocular scores increased linearly with age (0.76 letter/year for HCVA, 1.11 letters/year for 2.5% LCLA, and 0.97 letter/year for 1.25% LCLA; all P < 0.0001). Binocular HCVA scores also increased with age between 5 and 14.9 years (0.71 letters/year, P < 0.0001). The magnitude of binocular summation for HCVA or LCLA did not change with age.
Conclusions:
HCVA and LCLA abilities mature into adolescence, peak between 13 and 14.9 years of age, and then plateau into adulthood. Evaluation of patients with visual deficits should consider age-expected normal visual acuity.
Evaluation of visual acuity (VA) is an important aspect of routine health maintenance and is a pivotal metric in the assessment of patients with ophthalmologic and neurologic diseases. VA is typically assessed using Snellen and similar high-contrast visual acuity (HCVA) charts, such as Early Treatment Diabetic Retinopathy Study (ETDRS) charts (Fig. 1). By 6 years of age, children without refractive error or other visual impairments should achieve a Snellen acuity (high-contrast visual acuity [HCVA], Fig. 1) of 20/ 20 in each eye, although it is important to note that HCVA continues to subtly improve (achieving acuity better than 20/20) throughout childhood (1,2). Less is known about the influence of visual maturation with age on low-contrast letter acuity (LCLA, Fig. 1) scores.
FIG. 1.
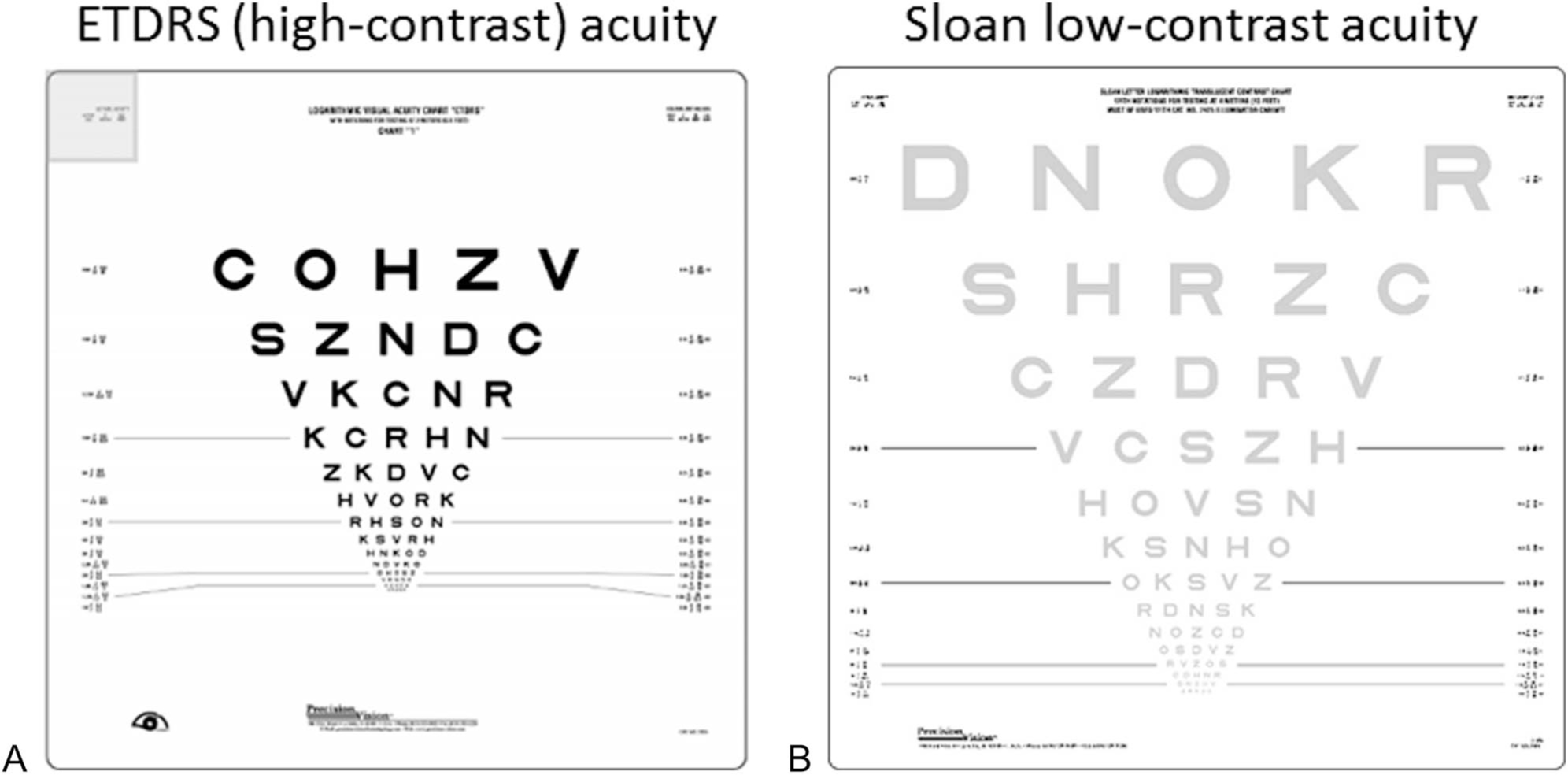
The visual acuity charts used include: (A) Early Treatment Diabetic Retinopathy Study (ETDRS) charts are high-contrast visual acuity charts and scored by the number of letters correctly identified (max 70 letters). B. Low-contrast letter acuity (LCLA) charts using 2.5% contrast; scoring is the same as for EDTRS charts. ETDRS and LCLA charts are typically administered at 2, 3, or 4 m using distinct charts calibrated for each distance. The 1.25% contrast charts (not pictured) are formatted similarly.
LCLA uses letters of lower contrast (i.e., faint gray) and decreasing size on a white background using the same format as the ETDRS charts (Fig. 1). With decreasing letter size, the spatial frequency, measured using alternating sine wave gratings in cycles per degree, increases (Fig. 2) (3,4), and a greater difference in luminance between the letter and its surround is required to correctly identify the letter. Maximum viewing of low-contrast (1%) stimuli occurs at a spatial frequency of 3–5 cycles per degree, whereas smaller objects that are 30–60 cycles per degree can be detected at 100% contrast. The contrast sensitivity function varies with spatial frequency and differences in luminance (as shown in Fig. 2) but has also been shown to change with age. Gwiazda et al have previously demonstrated that adults (18–30 years, N = 15) detected lower contrast stimuli at the same spatial frequency (i.e., had a higher peak contrast sensitivity function) compared with infants (2–8 months, N = 83) and young children (3–8.6 years, N = 84) (5). This group did not study individuals between ages 8 years and adulthood; thus, changes in the contrast sensitivity function in adolescents is unknown.
FIG. 2.
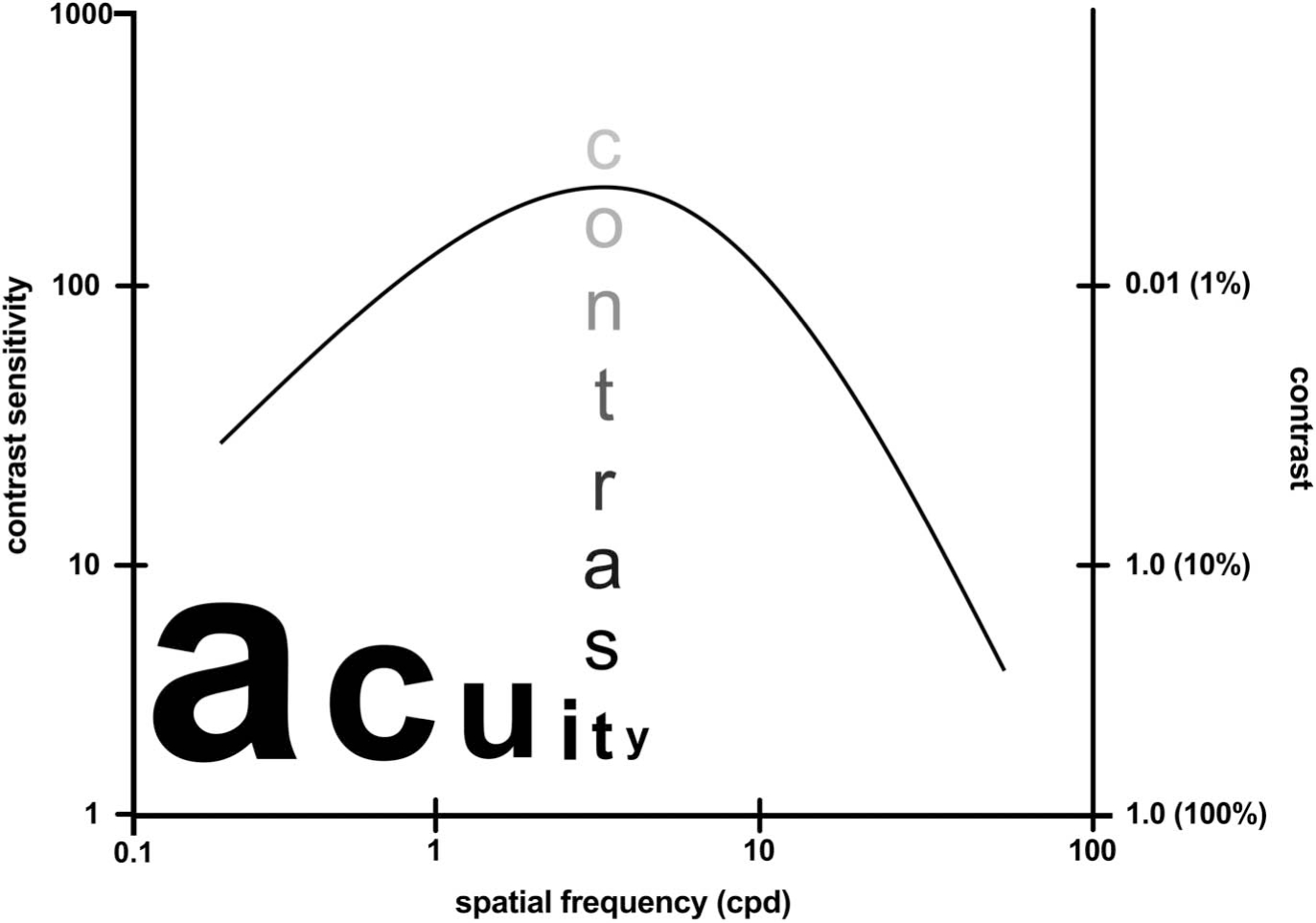
Contrast sensitivity function. Contrast sensitivity varies with spatial frequency. The spatial frequency of a letter is determined by the cycles per degree (cpd) of the visual angle using sine wave gratings. Contrast is defined as the luminance of an object compared with its surround. The contrast of sine wave gratings is defined as the difference in luminance between the gratings over their sum and is expressed as a percentage (i.e., 1.25% contrast). Decreasing letter size (as demonstrated by the word acuity in the figure) is associated with increasing spatial frequency. The maximum of human detection is 30–60 cpd at 100% contrast (2,3). The peak of the curve, which represents the maximal viewing of low-contrast objects, occurs at 3–5 cpd, as indicated by the word contrast (2,3). High- and low-contrast letter acuity charts alter the spatial frequency (letter size) and hold the contrast for each letter constant, whereas contrast sensitivity charts alter the contrast of the letters at a single spatial frequency (letter size). Reproduced with permission from (3).
When compared with monocular acuity scores, binocular scores typically exceed the score of either eye alone, a phenomenon known as binocular summation (6). Using ETDRS charts, most people do not appreciate this additive acuity because the improvement is small. However, the magnitude of binocular summation increases at lower levels of contrast (6–8). The impact of age on binocular summation using LCLA has been evaluated in a cohort of 129 individuals (ages 3–85 years), demonstrating that the magnitude of binocular summation using LCLA was greatest in children ages 10–19 years and decreased in adulthood (8).
We sought to determine normative values for HCVA and LCLA monocular and binocular scores to define the age-expected maturational changes.
METHODS
Healthy youth (ages 5–20 years) were recruited from the Children’s Hospital of Philadelphia and through local advertisement (research flyers). Participants without a history of neurologic, ocular, or systemic disease were eligible, provided that the monocular best-corrected high-contrast acuity (assessed using the participant’s own glasses or contact lenses) was 48 letters (the Snellen equivalent of 20/25) or better in each eye. For those wearing corrective lenses, the subject’s refraction was obtained using an autorefractor. A subset of the healthy subjects (N = 29) have been previously reported as controls in a study of pediatric MS (7).
The study was approved by the institutional review board at the Children’s Hospital of Philadelphia. Written informed consent and child assent was obtained from the participants after explanation of the study objectives and procedures and review of individual risks.
Each participant underwent visual acuity testing beginning with the right eye, followed by the left eye, and then binocularly with the ETDRS charts at 2 m (different charts were used for each test to eliminate memorization). Next, LCLA was assessed using the Sloan 2.5% contrast (Precision Vision) chart (only a single chart is available in print), the right eye first for all participants, followed by the left eye, and then binocularly at 2 m. Finally, participants read the Sloan 1.25% contrast chart in the same manner and at the same distance. Participants were given as much time as they needed until they stated that they could not see any additional letters and were given a single prompt to continue to try. Tests were scored by the number of letters correctly identified (range 0–70 letters). All charts were mounted on a retroilluminated light box (Precision Vision, La Salle, IL) in a room without a window, and the room lights were turned off.
Only one Sloan chart is available for each level of contrast. Thus, the monocular right and left eye scores for each participant were compared to determine whether there was a learning effect (which would suggest higher scores for the left eye as this was consistently tested second). The proportion of participants who had higher monocular scores using the right eye and left eye as well as equal scoring for each chart was calculated. The mean interocular difference (right eye score minus left eye score) was also calculated.
Participants were grouped into age groups in 2-year epochs. The mean VA score was calculated for each age category. We first explored the associations of each VA measure with age using the scatterplot with Locally Weighted Scatterplot Smoothing (LOWESS) (9). We then performed an analysis of variance (ANOVA) to determine whether mean VA scores differed across age groups (age modeled as categorical variable without imposing linearity assumption). If ANOVA found the VA measure significantly differed across age groups (overall P, 0.05), we then determined the association of visual acuity scores with age using a linear regression model for the younger age group (<15 years) and for the older age group (≥15 years), where the age cutpoint of 15 years was approximated from cubic spline regression using STATA (Stata-Corp LLC, College Station, TX). For the analysis of association between age and monocular visual acuity measures, the intereye correlation was accounted for by using generalized estimating equations (10). These statistical analyses were performed in SAS v9.4 (SAS Institute Inc., Cary, NC), and two-sided P < 0.05 was considered statistically significant.
RESULTS
We enrolled 101 participants with a visual acuity better than 48 letters in each eye, contributing 202 eyes to the analysis. Six participants (6%, all aged >12 years) wore their glasses or corrective lenses during the testing; 5 of the 6 had minimal errors (the spherical equivalent was -0.75 or less); one participant did not have refraction recorded. Our study of 101 children (202 eyes) provided 92% power to detect a difference of 5 letters in monocular HCVA across age groups and almost 99% power to detect a difference of 7 letters in monocular low-contrast visual acuity. The mean age was 13.0 years (SD 4.5 years, range: 5–20 years); 42 (41.6%) participants were male (Table 1).
TABLE 1.
Demographics of study participants
| Age Category | Number of Participants (Number of Eyes) | Males (%) |
|---|---|---|
|
| ||
| 5–6 yrs | 9 (18) | 3 (33.3%) |
| 7–8 yrs | 18 (36) | 9 (50.0%) |
| 9–10 yrs | 13 (26) | 7 (53.8%) |
| 11–12 yrs | 11 (22) | 3 (27.3%) |
| 13–14 yrs | 10 (20) | 4 (40.0%) |
| 15–16 yrs | 15 (30) | 4 (26.7%) |
| 17–18 yrs | 15 (30) | 6 (40.0%) |
| 19–20 yrs | 10 (20) | 6 (60.0%) |
| Total | 101 (202) | 42 (41.6%) |
Mean monocular HCVA and LCLA scores are presented in Table 2 by age groups. Mean monocular visual acuity scores significantly varied by age for HCVA charts (P = 0.001), LCLA 2.5% charts (P = 0.005), and LCLA 1.25% charts (P = 0.0005) with highest mean acuity scores achieved in the 13- to 14-year-old age group.
TABLE 2.
Mean monocular and binocular high- and low-contrast letter acuity scores and mean binocular summation in healthy children by age groups
| ETDRS (High-Contrast) |
Low-Contrast Letter Acuity (2.5% Contrast) |
Low-Contrast Letter Acuity (1.25% Contrast) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age (yrs) | N (Eyes) | Monocular Score, Mean (SD) | Binocular Score, Mean (SD) | Binocular Summation, Mean (SD) | Monocular Score, Mean (SD) | Binocular Score, Mean (SD) | Binocular Summation, Mean (SD) | Monocular Score, Mean (SD) | Binocular Score, Mean (SD) | Binocular Summation, Mean (SD) |
|
| ||||||||||
| 5–6 | 9 (18) | 52.6 (2.1) | 54.2 (1.9) | 1.2 (1.2) | 26.1 (3.7) | 37.1 (2.0) | 9.9 (2.3) | 19.2 (3.1) | 29.8 (2.4) | 9.0 (1.7) |
| 7–8 | 18 (36) | 54.9 (3.6) | 57.5 (3.5) | 1.6 (3.4) | 28.8 (6.2) | 37.9 (6.8) | 8.8 (4.7) | 19.5 (6.5) | 31.6 (5.9) | 11.8 (3.7) |
| 9–10 | 13 (26) | 55.3 (3.8) | 57.0 (2.5) | 2.4 (2.0) | 26.5 (8.6) | 34.2 (3.5) | 10.4 (4.6) | 17.0 (7.9) | 26.7 (3.4) | 10.2 (5.0) |
| 11–12 | 11 (22) | 57.6 (3.1) | 60.3 (3.0) | 2.1 (2.0) | 32.3 (7.4) | 40.0 (9.9) | 8.5 (6.2) | 23.4 (5.7) | 32.6 (7.6) | 8.8 (5.1) |
| 13–14 | 10 (20) | 59.2 (3.0) | 60.6 (2.5) | 0.8 (0.8) | 36.5 (6.6) | 40.8 (6.3) | 5.8 (1.6) | 27.1 (6.3) | 34.8 (5.8) | 9.6 (5.0) |
| 15–16 | 15 (30) | 57.2 (3.7) | 60.7 (3.4) | 1.7 (3.2) | 27.1 (5.1) | 37.0 (3.7) | 7.1 (4.5) | 17.8 (5.5) | 31.3 (4.7) | 12.3 (4.7) |
| 17–18 | 15 (30) | 57.4 (4.5) | 61.0 (3.3) | 1.6 (2.5) | 30.6 (5.5) | 39.9 (3.1) | 7.1 (4.0) | 24.0 (6.3) | 33.7 (5.2) | 8.5 (4.3) |
| 19–20 | 10 (20) | 58.2 (3.6) | 61.7 (2.5) | 1.6 (1.4) | 31.8 (5.1) | 39.9 (2.8) | 5.8 (4.4) | 24.3 (4.5) | 34.5 (4.4) | 8.9 (5.1) |
| Total | 101 (202) | 56.5 (4.0) | 59.2 (3.7) | 1.7 (2.4) | 29.8 (6.9) | 38.2 (4.7) | 7.9 (4.5) | 21.2 (6.8) | 31.8 (5.4) | 10.2 (4.8) |
| All | Overall P value | 0.001 | <0.0001 | 0.96 | 0.005 | 0.054 | 0.23 | 0.0005 | 0.03 | 0.19 |
Each chart contains 70 letters. A score of 55 letters identified correctly is the Snellen equivalent of 20/20.
As shown in Figure 3, the increase in visual acuity scores with age was nonlinear. A cubic spline regression using 3 knots demonstrated an inflection in slope for monocular scores at approximately 13 years (12.9 for HCVA and 13.005 for LCLA 2.5% and 1.25%). Thus, we fit linear regression models separately for participants younger than 15 years and participants aged 15 years or older. The HCVA increased linearly between ages 5 and younger than 15 years (slope 0.76 letter/year P < 0.0001), but the increase was not significant between ages 15–20 years (slope = 0.14 letter/year, P = 0.6). Similarly, monocular LCLA increased linearly up to age 15 years (slope 1.11 letters/ year, P < 0.0001 for LCLA 2.5%; and 0.97 letter/year, P < 0.0001 for LCVA 1.25%).
FIG. 3.
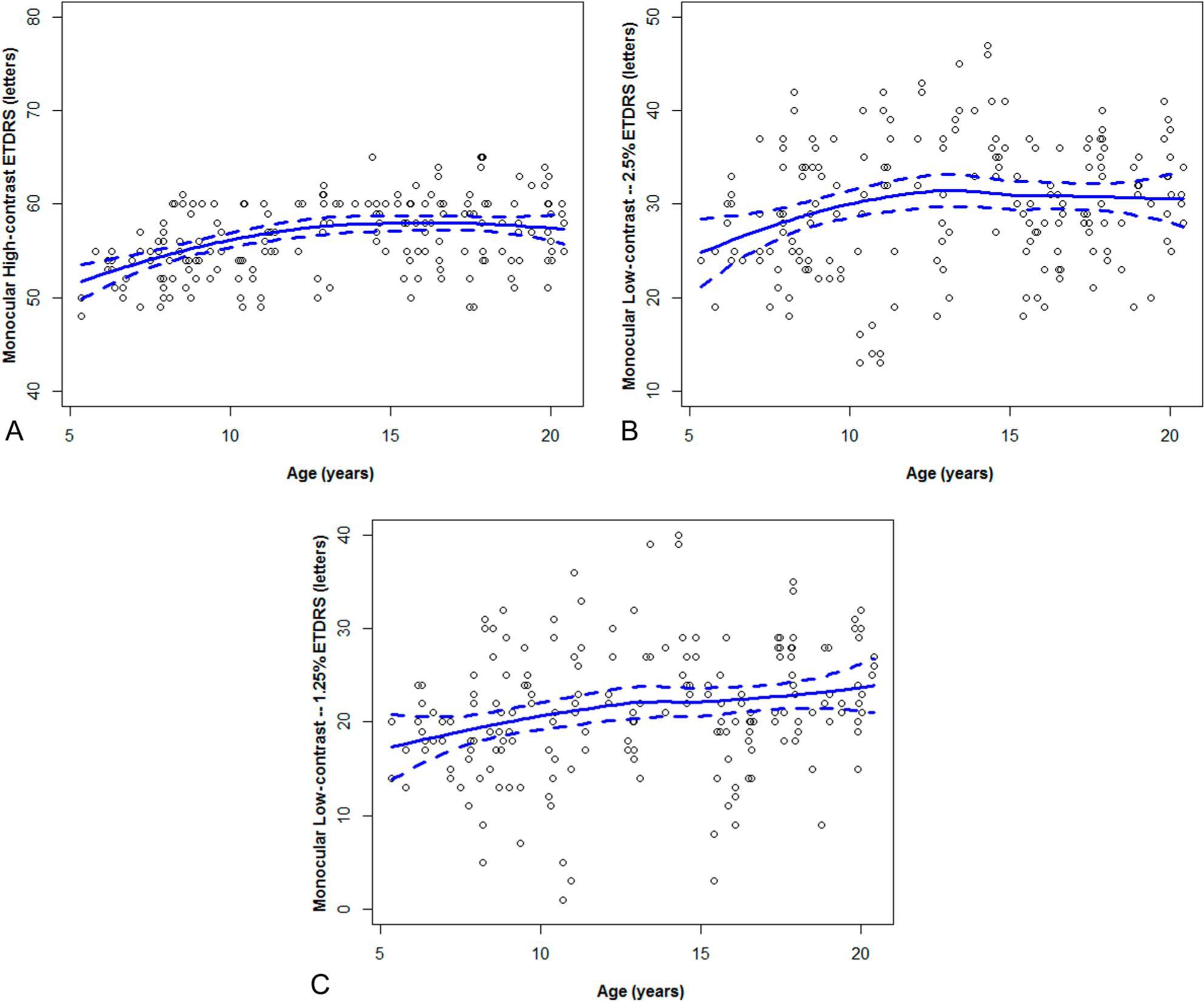
Monocular scores in healthy children using (A) ETDRS chart, (B) 2.5% contrast, and (C) 1.25% contrast charts. Monocular scores increase in younger children with an inflection in slope as determined by spline regression at 13 years of age for HCVA and LCLA. The increase in scores with age is linear (P < 0.0001 for all graphs) in children younger than 15 years. HCVA, high-contrast visual acuity; LCLA, low-contrast letter acuity.
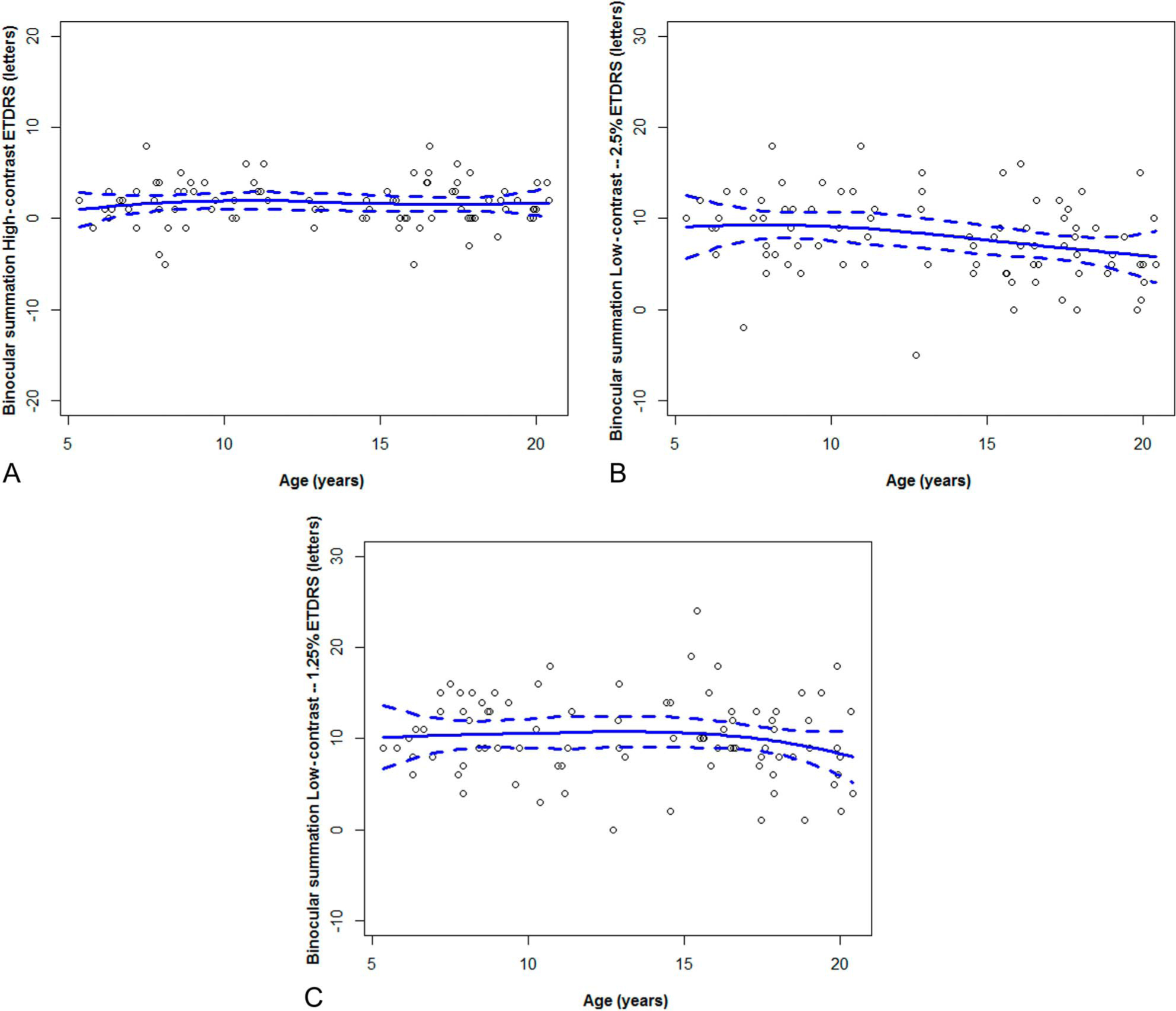
Mean binocular high- and low-contrast acuities are listed in Table 2, with the highest scores also clustering in the 13-to 14-year age group. Binocular HCVA showed significant change with age (P < 0.0001), most notably before age 15 years (Fig. 4). Cubic spline regression with 3 knots demonstrated an inflection in slope at age 14.4 years. The slope for binocular HCVA was 0.71 letters/year, or 7.1 letters between ages 5 and younger than 15 years (P =0.0002),butnolonger increased between ages 15–20 years (P = 0.69). Across all age groups, the binocular LCLA scores varied slightly with age for LCVA 2.5% (P = 0.054) and LCVA 1.25% (P = 0.03). However, the test of linearity of VA association with age was not significant in either the younger children (<15 years) or the older cohort (≥15 years).
FIG. 4.
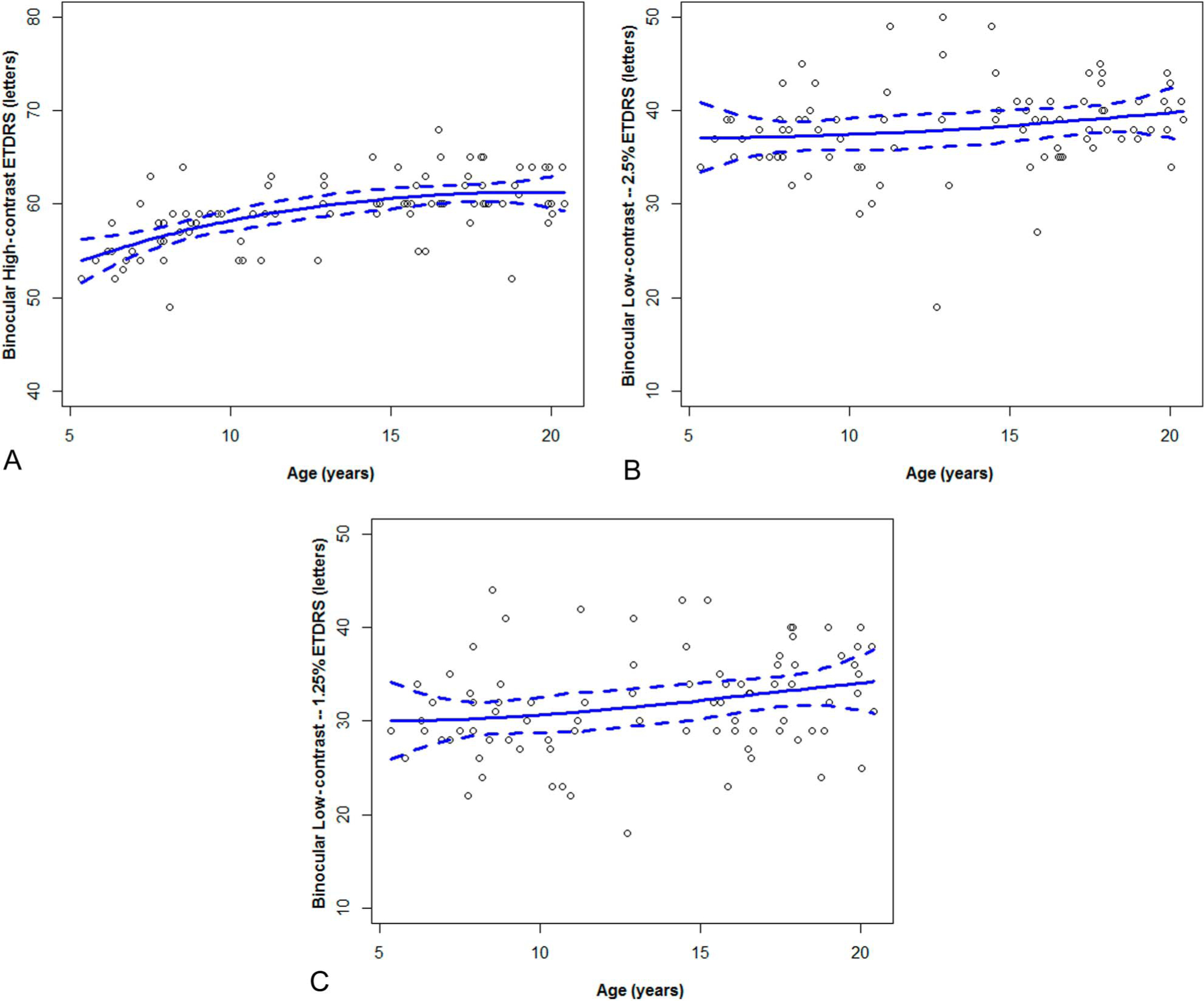
Binocular scores in healthy children using (A) ETDRS, (B) 2.5% contrast, and (C) 1.25% contrast charts. Binocular high-contrast visual acuity scores increase with age (P < 0.0001), with a linear increase in childhood until 14.4 years of age (P = 0.0002) but not in the 15 to 20-year-old participants (P = 0.69). For low-contrast visual acuity, although there was difference in scores across the age span (2.5% charts, P = 0.054; and 1.25% charts, P = 0.03), a linear trend was not found in children younger than 15 years or children older than 15 years (all P > 0.09).
The magnitude of binocular summation did not differ by age (Table 2 and Fig. 5). The mean mag binocular summation for all subjects was 1.7 (standard deviation [SD] 2.4) letters using HCVA, 7.9 (SD 4.5) letters using 2.5% LCLA, and 10.2 (SD 4.8) letters for 1.25% LCLA.
FIG. 5.
Binocular summation in healthy children using (A) ETDRS, (B) 2.5% contrast, and (C) 1.25% contrast charts. The magnitude of binocular summation does not significantly vary by age using HCVA (P = 0.96) or LCLA (P = 0.23 for 2.5% charts and P = 0.19 for 1.25% charts). HCVA, high-contrast visual acuity; LCLA, low-contrast letter acuity.
None of the visual metrics differed as a function of sex. To evaluate the possibility of a learning effect, especially using the LCLA charts, we determined their interocular difference (Table 3). For HCVA, 46% of participants had a higher right eye monocular score, 34% had a higher left eye monocular score, 20% correctly identified the same number of letters with each eye, and their mean interocular difference (right eye minus left eye) was 1.1 (SD 3.7) letters (difference in mean scores by the age group: P = 0.23). Using the LCLA charts, the proportions with higher scoring were as follows: 2.5% charts: 54% right eye greater, 36% gnitudelefteyeofgreater,10% equalscores,withmeaninterocular difference of 0.8 (SD 5.0) letters (difference in mean score by the age group: P = 0.02); and 1.25%: 53% right eye greater, 36% left eye greater, and 11% equal scores, with mean interocular difference of 0.6 (SD 4.6) letters (difference in mean score by the age group: P = 0.08). We also explored whether the interocular difference (right minus left monocular score) increased linearly with age (Table 3). A negative mean score (indicating that, on average, left eye scores were greater than the right eye scores) occurred in the younger age groups but not the groups younger than 15 years of age (for whom right eye scores were greater). The test for linear trend for the interocular difference was significant using HCVA (P = 0.049) and LCLA 2.5% (P = 0.002) but not LCLA 1.25% (P = 0.12).
TABLE 3.
Interocular difference (right eye minus left eye) by age groups
| Mean (SD) |
||||
|---|---|---|---|---|
| Age (yrs) | N (Participants) | ETDRS High-Contrast | Low-Contrast Acuity (2.5% Contrast) | Low-Contrast Acuity (1.25% Contrast) |
|
| ||||
| 5–6 | 9 | −0.78 (0.83) | −1.70 (3.15) | −0.13 (3.91) |
| 7–8 | 18 | 1.33 (3.83) | −0.28 (4.27) | −0.33 (4.96) |
| 9–10 | 13 | −0.23 (2.71) | −0.54 (3.97) | 1.92 (5.01) |
| 11–12 | 11 | 1.00 (2.45) | −1.70 (3.88) | −3.00 (5.46) |
| 13–14 | 10 | −0.10 (2.92) | 0.40 (5.32) | 0.10 (5.61) |
| 15–16 | 15 | 2.73 (3.63) | 4.13 (5.51) | 2.40 (3.92) |
| 17–18 | 15 | 1.27 (5.26) | 2.43 (5.40) | 1.93 (2.55) |
| 19–20 | 10 | 2.30 (4.19) | 2.00 (5.03) | 1.10 (3.45) |
| Total | 101 | 1.1 (3.70) | 0.8 (5.00) | 0.6 (4.60) |
| Overall P value (comparing the difference in mean scores across age groups) | 0.23 | 0.02 | 0.08 | |
| Linear trend P value | 0.049 | 0.002 | 0.12 | |
DISCUSSION
Mean monocular and binocular HCVA and LCLA scores increase in childhood, peak at approximately 13–14 years of age, and then plateau into early adulthood. Over the decade between 5 and and 15 years, we demonstrate a linear increase in monocular scores: HCVA 7.6 letters, LCLA (2.5% contrast) 11.1 letters, and LCLA (1.25% contrast) 9.7 letters. Given that clinically meaningful values established for adults are 5 letters for HCVA and 7 letters for LCLA, (11) the changes in scores that occur as a function of age are clinically relevant.
Our inclusion criteria required 48 letters correctly identified using the ETDRS chart for HCVA, the Snellen equivalent of 20/25 vision. Despite having conventionally defined “good vision,” we show that between ages 5 and and 15 years, children improve further in their detection of high-contrast letters. Understanding age-expected maximal HCVA is important to more fully appreciate subtle loss of vision that may occur in the context of medical disorders, even when the measured vision might still approximate 20/20 acuity. For example, for a child being evaluated for optic neuritis whose baseline visual acuity is 20/16, a measured acuity of 20/25 represents a 2-line difference.
We also explored the interocular difference in acuity scores. The mean interocular difference (right eye minus left eye) in healthy youth was small (HCVA 1.1 letters [SD 3.7]; LCLA 2.5% 0.8 letters [SD 5] and LCLA 1.25% 0.6 letters [SD 4.6]). Considering one SD above and below the mean (representing 68% of subjects), the interocular difference is less than 1-line for most individuals using HCVA and LCLA and could also be used in clinical practice to detect pathology.
Our findings of improved HCVA and LCLA up to age 13–14 years support recent findings regarding the role of occlusive therapy for amblyopia. In a study of 507 participants (ages 7–17 years) randomized to optical correction alone or optical correction plus occlusive therapy for the better eye (such as patching or atropine drops for 2–6 hours a day), HCVA scores improved between ages 7 and 12 years with the additional occlusive therapy (12). However, children ages 13–17 years did not have further improvements in HCVA with occlusive therapy. We show an even greater maturational change in LCLA as compared to HCVA, and it would be of interest to evaluate whether occlusive therapy also improves LCLA in individuals with amblyopia and whether this benefit also extends into mid-adolescence.
Monocular and binocular high-contrast and low-contrast visual acuity testing scores are the key outcomes of the Pediatric Optic Neuritis Prospective Outcomes Study (13). Clinical trials of MS therapies have included HCVA and LCLA testing scores as secondary outcomes. Optic neuritis in neuroinflammatory diseases may be associated with disease-related loss of acuity before the period of maximal visual acuity and may also cause alterations in age-expected improvement. This dual impact must be considered when evaluating the visual performance of these disorders. Patients with mild deficits may improve with age but not reach the expected improvement in vision, an important clinical outcome. Our work will assist in determining whether patients with optic neuritis or MS or other diseases differ from age-matched normal acuity.
Our study requires several considerations. Younger children often have a shorter attention span, may have more difficulty cooperating, or may be more likely to “give up” during testing. Against this confound, a greater proportion of participants (considering all ages) had higher monocular scores for HCVA and LCLA using the right eye compared with the left eye, which was tested second. If a learning effect or memorization was present, a higher score using the left eye would have occurred. Furthermore, we did not detect clinically significant differences between the right and left eye scores for HCVA or LCLA (1.25%) by age group nor did we see children “tire out” such that performance declined during testing (which would have been expected to influence binocular test scores because these were the last tests performed during a session). The LCLA 2.5% intereye scores did differ by the age group, and when we explored whether the interocular difference changed linearly instead of categorically by the age group, we also detected a positive linear trend using both HCVA and LCLA 2.5%, indicating greater mean right eye scores compared with left eye scores with increasing age. The mean interocular difference for younger age groups was often negative, indicating higher mean left eye scores; thus, a learning effect could have been present. However, even if a learning effect contributed, the interocular differences in monocular acuity for all charts were small (mean 1.1 letters for HCVA and less than one letter for LCLA) and were unlikely to influence the findings.
For this study, participants were allowed to wear their current corrective lenses. Only 6 subjects (all older than 12 years) wore corrective lenses. Refractive error was minimal (spherical equivalent was 20.75 or less), which was unlikely to have influenced the results. We cannot determine whether retinoscopy with subjective refraction would alter our findings as the correction of refractive error may improve with age (resulting in higher scores) due to increased participation and articulation of visual deficits; however, our methods are reflective of visual function in children’s daily lives. Finally, although we present a cross-sectional assessment of vision across the age span, it is important to confirm these maturational changes through serial testing of individuals over time in future longitudinal studies. A longitudinal study of cooperative subjects should also consider the impact of standardized refraction on these results.
In conclusion, our study demonstrated that the ability to perceive high- and low-contrast visual stimuli continues to increase into adolescence. Evaluation of visual change over time in pediatric patients with ophthalmologic and neurological disorders should consider the maturational expectations to more fully appreciate whether the trajectory of their visual performance differs from normative maturational change and whether such patients achieve age-expected maximal visual acuity. Clinical trials that include HCVA and LCLA scores as outcomes should ensure participants are compared with age-matched controls.
Acknowledgments
Study funded by NIH: K23NS069806, Waldman, PI.
A. T. Waldman has received research support from the NIH (NINDS K23NS069806, PI; R01NS071463, site investigator) related to the current work. A. M. Lavery has no commercial associations related to the current work. G. Liu has no commercial associations related to the current work other than what is included for G. T. Liu, below. R. A. Avery has received research support from the NIH (NIH-EY022673, PI) and has served as a nonrenumerated editor for Neuropediatrics. G. T. Liu has received royalties for Liu, Volpe, Galetta’s Neuro-Ophthalmology, Diagnosis, and Management, third Ed., 2019, Elsevier. G.-S. Ying has received funding from the NIH (NEI grant: P30 EY01583–26) unrelated to the current work. B. L. Banwell serves as an advisor to Novartis. She also serves as a non-remunerated advisor to Biogen, Sanofi, and Teva Neuroscience. The remaining author reports no conflicts of interest.
Contributor Information
Amy T. Waldman, Division of Child Neurology, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania; Department of Neurology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania; Department of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania.
Amy M. Lavery, Division of Child Neurology, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania.
Geraldine W. Liu, Division of Child Neurology, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania.
Robert A. Avery, Department of Neurology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania; Neuroophthalmology Service, Division of Ophthalmology, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania; Department of Ophthalmology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania.
Grant T. Liu, Department of Neurology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania; Neuroophthalmology Service, Division of Ophthalmology, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania; Department of Ophthalmology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania.
Maureen G. Maguire, Department of Ophthalmology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania.
Gui-shuang Ying, Department of Ophthalmology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania.
Brenda L. Banwell, Division of Child Neurology, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania; Department of Neurology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania; Department of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania.
REFERENCES
- 1.Eustis H Postnatal development. In: Wright K, ed. Pediatric Ophthalmology and Strabismus. St. Louis, MO: Mosby, 1995:45–59. [Google Scholar]
- 2.Ohlsson J, Villarreal G. Normal visual acuity in 17–18 year olds. Acta Ophthalmol Scand. 2005;83:487–491. [DOI] [PubMed] [Google Scholar]
- 3.Woods RL, Wood JM. The role of contrast sensitivity charts and the contrast letter charts in clinical practice. Clin Exp Optom 1995;78:43–57. [Google Scholar]
- 4.Ginsburg AP. Contrast sensitivity and functional vision. Int Ophthalmol Clin. 2003;43:5–15. [DOI] [PubMed] [Google Scholar]
- 5.Gwiazda J, Bauer J, Thorn F, Held R. Development of spatial contrast sensitivity from infancy to adulthood: psychophysical data. Optom Vis Sci. 1997;74:785–789. [DOI] [PubMed] [Google Scholar]
- 6.Pineles SL, Birch EE, Talman LS, Sackel DJ, Frohman EM, Calabresi PA, Galetta SL, Maguire MG, Balcer LJ One eye or two: a comparison of binocular and monocular low-contrast acuity testing in multiple sclerosis. Am J Ophthalmol. 2011;152:133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waldman AT, Hiremath G, Avery RA, Conger A, Pineles SL, Loguidice MJ, Talman LS, Galetta KM, Shumski MJ, Wilson J, Ford E, Lavery AM, Conger D, Greenberg BM, Ellenberg JH, Frohman EM, Balcer LJ, Calabresi PA. Monocular and binocular low-contrast visual acuity and optical coherence tomography in pediatric multiple sclerosis. Mult Scler Relat Disord. 2014;3:326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pineles SL, Velez FG, Yu F, Demer JL, Birch E. Normative reference ranges for binocular summation as a function of age for low contrast letter charts. Strabismus. 2014;22:167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cleveland WS, Devlin SJ, Grosse E. Regression by local fitting. J Econom 1988;37:87–114. [Google Scholar]
- 10.Liang KY, Zeger SL. Regression analysis for correlated data. Annu Rev Public Health. 1993;14:43–68. [DOI] [PubMed] [Google Scholar]
- 11.Talman LS, Bisker ER, Sackel DJ, Long DA, Galetta KM, Ratchford JN, Lile DJ, Farrell SK, Loguidice MJ, Remington G, Conger A, Frohman TC, Jacobs DA, Markowitz CE, Cutter GR, Ying GS, Dai Y, Maguire MG, Galetta SL, Frohman EM, Calabresi PA, Balcer LJ Longitudinal study of vision and retinal nerve fiber layer thickness in multiple sclerosis. Ann Neurol. 2010;67:749–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scheiman MM, Hertle RW, Beck RW, Edwards AR, Birch E, Cotter SA, Crouch ER, Cruz OA, Davitt BV, Donahue S, Holmes JM, Lyon DW, Repka MX, Sala NA, Silbert DI, Suh DW, Tamkins SM Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123:437–447. [DOI] [PubMed] [Google Scholar]
- 13.Pineles SL, Liu GT, Waldman AT, Lazar E, Kupersmith MJ, Repka MX; Pediatric Eye Disease Investigator Group and the Neuro-Ophthalmology Research Disease Investigator Consortium. Pediatric optic neuritis prospective outcomes study. J Neuroophthalmology 2016;36:115–117. [DOI] [PMC free article] [PubMed] [Google Scholar]


