Abstract
Background:
Increased rates of pediatric eating disorders have been observed during the COVID-19 pandemic, but little is known about trends among adults. We aimed to evaluate rates of emergency department visits and hospital admissions for eating disorders among adolescents and adults during the pandemic.
Methods:
We conducted a population-based, repeated cross-sectional study using linked health administrative data for Ontario residents aged 10–105 years during the prepandemic (Jan. 1, 2017, to Feb. 29, 2020) and pandemic (Mar. 1, 2020, to Aug. 31, 2022) periods. We evaluated monthly rates of emergency department visits and hospital admissions for eating disorders, stratified by age.
Results:
Compared with expected rates derived from the prepandemic period, emergency department visits for eating disorders increased during the pandemic among adolescents aged 10–17 years (7.38 v. 3.33 per 100 000; incidence rate ratio [IRR] 2.21, 95% confidence interval [CI] 2.17–2.26), young adults aged 18–26 years (2.79 v. 2.46 per 100 000; IRR 1.13, 95% CI 1.10–1.16) and older adults aged 41–105 years (0.14 v. 0.11 per 100 000; IRR 1.15, 95% CI 1.07–1.24). Hospital admissions for eating disorders increased during the pandemic for adolescents (8.82 v. 5.74 per 100 000; IRR 1.54, 95% CI 1.54–1.54) but decreased for all adult age groups, especially older adults aged 41–105 years (0.21 v. 0.30 per 100 000; IRR 0.72, 95% CI 0.64–0.80).
Interpretation:
Emergency department visits for eating disorders increased among adolescents, young adults and older adults during the pandemic, but hospital admissions increased only for adolescents and decreased for all adult groups. Differential rates of acute care use for eating disorders by age have important implications for allocation of inpatient mental health resources.
Eating disorders and related symptomatology have increased globally among children and adolescents during the COVID-19 pandemic.1–6 A cross-sectional analysis of 6 pediatric tertiary care hospitals in Canada reported that the incidence of newly diagnosed anorexia nervosa increased from 24.5 to 40.6 cases per month and hospital admissions among these affected patients increased from 7.5 to 20.0 per month during the pandemic.7 Our previous work showed an overall 66% increase in emergency department visits and a 37% increase in hospital admissions for eating disorders among children and adolescents in Ontario, Canada during the first 10 months of the COVID-19 pandemic.3
Data on eating disorders in adult populations are limited but suggest a potential increase during the pandemic.8–10 The impact of the pandemic on adult eating disorders may be different than for youth experiencing unique stressors (e.g., academic concerns, social media, peer influence). Further, the health system response to eating disorders, capacity around treatment decisions and differing thresholds for admission by age may also contribute to potential differences.11 Nevertheless, eating disorders are prevalent among adult populations12,13 and carry a high mortality burden.14
Whether the COVID-19 pandemic is having a disparate impact on pediatric presentations for eating disorders compared with those of adults is not clear. Disparate service use is important to understand to guide funding, resource capacity and resource allocation as part of pandemic recovery planning. We sought to address evidence gaps by evaluating rates of acute care use (emergency department visits and hospital admissions) for eating disorders among adolescents and adults before and after the onset of the COVID-19 pandemic in Ontario, Canada.
Methods
Study design and population
We conducted a population-based, repeated cross-sectional study of all people aged 10–105 years living in Ontario, Canada, who were eligible for provincial health insurance. We used linked health administrative databases housed at ICES, an independent, nonprofit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement. We identified all emergency department visits and hospital admissions related to an eating disorder before (Jan. 1, 2017, to Feb. 29, 2020) and during (Mar. 1, 2020, to Aug. 31, 2022) the COVID-19 pandemic. We determined monthly rates of eating disorder emergency department visits and admissions by age group, including adolescents (10–17 yr), young adults (18–26 yr), adults (27–40 yr) and older adults (41–105 yr). We excluded non-Ontario residents, people with invalid birth dates and deaths within the study period, and those with missing data on sex. This study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist for cross-sectional studies.15
Data sources
We accessed data from several databases and linked them using unique ICES encoded identifiers. We identified the study population through the Registered Person’s Database, a registry of all people eligible for Ontario’s publicly funded health care through the Ontario Health Insurance Plan, and used this database to capture sociodemographic variables including date of birth, sex and postal code. The Ontario Marginalization Index for neighbourhood material deprivation combines Census information on income and education and was used as a measure of socioeconomic status. Quintiles are used to define the marginalization index, with 1 representing the least deprived and 5 representing the most deprived neighbourhoods. We determined urban or rural region of residence by the Rurality Index of Ontario score, which is a continuous and broader measure of rurality used for policy development purposes in Ontario based on census subdivision, linked with postal codes in the Statistics Canada Postal Code Conversion File to Canadian Census data. Rurality scores are on a 100-point scale, with rural residence defined as a score of 40 or higher. We identified emergency department visits using the National Ambulatory Care Reporting System, and hospital admissions from the Canadian Institute for Health Information’s Discharge Abstract Database and the Ontario Mental Health Reporting System.
Measures
We identified visits related to an eating disorder during the study period using diagnostic coding from the 9th and 10th revisions of the International Classification of Diseases and Related Health Problems and included visits with any eating disorder–related diagnostic code, unless the eating disorder did not contribute to the stay (Appendix 1, Supplemental eTable 1, available at www.cmaj.ca/lookup/doi/10.1503/cmaj.221318/tab-related-content). These diagnostic codes have been shown to have high specificity for presentations of eating disorders, and previous analyses have shown that separating those who are admitted to hospital for an eating disorder and those who attend the emergency department for an eating disorder results in distinct, clinically relevant populations.16 Individual eating disorders included anorexia nervosa, bulimia nervosa, other eating disorders and provisionally diagnosed eating disorders (Appendix 1, eTable 1). We quantified monthly rates of eating disorder–related emergency department visits and hospital admissions per 100 000 population during the prepandemic (Jan. 1, 2017, to Feb. 29, 2020) and pandemic periods (Mar. 1, 2020, to Aug. 31, 2022).
We ascertained sociodemographic and clinical characteristics of the population as of January 1 of each study year and included age, sex, rurality, neighbourhood-level material deprivation quintile, pre-existing mental health condition (i.e., any outpatient or acute claim with a mental health–related concern within 2 yr) and history of eating disorder–related visit (i.e., any acute claim with a relevant eating disorder diagnostic code within 2 years and lifetime lookback to 2002), using similar definitions as the primary outcome (Appendix 1, Supplemental eTable 1). Among people with an eating disorder–related emergency department visit or hospital admission, we reported the health care setting (i.e., community hospital, adult academic hospital or pediatric hospital).
Statistical analysis
We calculated monthly rates of outpatient mental health visits per 100 000 people in the Ontario study population in each study year. We used Poisson generalized estimating equations models for clustered count data to model the prepandemic trends and to predict expected rates of eating disorder–related emergency department visits and hospital admissions in the pandemic period in the absence of restrictions. The unit of analysis was the age group–sex–month stratum. The dependent variable was the count of events to the population in the stratum; the offset was the log of the stratum-specific population, and the working correlation structure was an autoregressive 1 model. The pre-COVID model included age group–sex indicators, a continuous linear term of months since Jan. 1, 2017, to estimate the trend, and pre-COVID month indicators to model seasonal variations, with April as the reference month, as in previous work.3
We computed expected rates after the pandemic onset (and 95% confidence intervals [CIs]) by applying the linear combination of prepandemic regression coefficients to the post-onset strata and exponentiating. We expressed the relative change in post-onset visit rates as an adjusted incidence rate ratio (IRR) of observed to expected rates by exponentiating the difference of observed and expected post-onset log rates and CIs.
We stratified models by sex and by clinically relevant life stages (ages 10–17 yr, 18–26 yr, 27–40 yr and 41–105 yr). These categories were also determined based on service provision across the age transitions within Ontario’s health care context. We conducted all analyses using SAS statistical software, version 9.4.
Ethics approval
Research ethics board review was not required as the data use was authorized under section 45 of Ontario’s Personal Health Information Protection Act.
Results
During the prepandemic period, a total of 5818 adolescents and adults had an eating disorder–related emergency department visit or hospital admission (Table 1). Of these, 2458 (42.2%, 88.0% female) were adolescents aged 10–17 years, 1701 (29.2%, 92.5% female) were young adults aged 18–26 years, 861 (14.8%, 91.4% female) were adults aged 27–40 years and 798 (13.7%, 77.6% female) were older adults aged 41–105 years (Table 1). Sociodemographic characteristics (i.e., rurality, material deprivation and pre-existing mental health–related condition or eating disorder) were relatively stable over the 3-year prepandemic period (Table 1). Among adolescents, 63.2% had a pre-existing mental health–related condition and 17.0% had a pre-existing eating disorder (2-yr lookback). The proportion of patients with pre-existing mental health-related conditions (86.9% for those aged 18–26 yr, 88.5% for those aged 27–40 yr and 71.4% for those aged 41–105 yr) and eating disorders (2-yr lookback; 28.7% for those aged 18–26 yr, 32.2% for those aged 27–40 yr and 21.1% for those aged 41–105 yr) was higher among adults (Table 1). Among adolescents, 44.8% had a diagnosis of anorexia nervosa, compared with 37.5% among those aged 18–26 years, 39.3% among those aged 27–40 years and 29.9% among those aged 41–105 years. In contrast, the proportion of patients with bulimia nervosa diagnoses (21.2% for those aged 18–26 yr, 26.2% for those aged 27–40 yr and 13.8% for those aged 41–105 yr) was higher among adults than adolescents (10.6%) (Table 1).
Table 1:
Sociodemographic and clinical characteristics of people aged 10–105 years with at least 1 eating disorder–related emergency department visit or hospital admission during the prepandemic (January 2017 to February 2020) and pandemic periods (March 2020 to August 2022)
| Characteristic | No. (%) of patients aged 10–17 yr* |
No. (%) of patients aged 18–26 yr* |
No. (%) of patients aged 27–40 yr* |
No. (%) of patients aged 41–105 yr* |
||||
|---|---|---|---|---|---|---|---|---|
| Prepandemic n = 2458 |
Pandemic n = 3903 |
Prepandemic n = 1701 |
Pandemic n = 1529 |
Prepandemic n = 861 |
Pandemic n = 770 |
Prepandemic n = 798 |
Pandemic n = 668 |
|
| Sex, female | 2164 (88.0) | 3527 (90.4) | 1573 (92.5) | 1438 (94.0) | 787 (91.4) | 691 (89.7) | 619 (77.6) | 549 (82.2) |
| Age, mean ± SD | 14.51 ± 1.81 | 14.38 ± 1.76 | 21.13 ± 2.50 | 21.18 ± 2.49 | 32.73 ± 3.94 | 32.52 ± 4.04 | 57.32 ± 13.93 | 58.15 ± 14.69 |
| Median (IQR) | 15 (13–16) | 15 (13–16) | 21 (19–23) | 21 (19–23) | 32 (29–36) | 32 (29–36) | 53 (46–66) | 54 (45–69) |
| Rural area | 238 (9.7) | 340 (8.7) | 137 (8.1) | 119 (7.8) | 67 (7.8) | 61 (7.9) | 77 (9.6) | 72 (10.8) |
| Material deprivation quintile | ||||||||
| Q5 (most deprived) | 390 (15.9) | 594 (15.2) | 309 (18.2) | 310 (20.3) | 223 (25.9) | 186 (24.2) | 203 (25.4) | 168 (25.1) |
| Q4 | 388 (15.8) | 543 (13.9) | 295 (17.3) | 245 (16.0) | 145 (16.8) | 133 (17.3) | 147 (18.4) | 134 (20.1) |
| Q3 | 425 (17.3) | 652 (16.7) | 291 (17.1) | 266 (17.4) | 115 (13.4) | 110 (14.3) | 137 (17.2) | 97 (14.5) |
| Q2 | 556 (22.6) | 921 (23.6) | 345 (20.3) | 323 (21.1) | 182 (21.1) | 145 (18.8) | 138 (17.3) | 130 (19.5) |
| Q1 (least deprived) | 666 (27.1) | 1137 (29.1) | 424 (24.9) | 365 (23.9) | 191 (22.2) | 192 (24.9) | 164 (20.6) | 128 (19.2) |
| Pre-existing MH condition (2-yr lookback) | 1554 (63.2) | 2392 (61.3) | 1478 (86.9) | 1321 (86.4) | 762 (88.5) | 666 (86.5) | 570 (71.4) | 474 (71.0) |
| Pre-existing eating disorder (lifetime lookback to 2002) | 456 (18.6) | 669 (17.1) | 718 (42.2) | 564 (36.9) | 420 (48.8) | 389 (50.5) | 269 (33.7) | 237 (35.5) |
| Pre-existing eating disorder (2-yr lookback) | 419 (17.0) | 615 (15.8) | 489 (28.7) | 390 (25.5) | 277 (32.2) | 238 (30.9) | 168 (21.1) | 137 (20.5) |
| Eating disorders † | ||||||||
| Anorexia nervosa | 1100 (44.8) | 1883 (48.2) | 638 (37.5) | 563 (36.8) | 338 (39.3) | 287 (37.3) | 239 (29.9) | 206 (30.8) |
| Bulimia nervosa | 260 (10.6) | 301 (7.7) | 361 (21.2) | 262 (17.1) | 226 (26.2) | 192 (24.9) | 110 (13.8) | 75 (11.2) |
| Other eating disorders‡ | 1533 (62.4) | 2417 (61.9) | 905 (53.2) | 897 (58.7) | 414 (48.1) | 377 (49.0) | 499 (62.5) | 435 (65.1) |
| Provisionally diagnosed eating disorders | 10 (0.4) | 11 (0.3) | 61 (3.6) | 44 (2.9) | 34 (3.9) | 18 (2.3) | 14 (1.8) | 14 (2.1) |
| Eating disorder–related ED visits | ||||||||
| Patients with an eating disorder–related ED visit | 1438 (58.5) | 2997 (78.6) | 1451 (85.3) | 1434 (93.8) | 598 (69.5) | 581 (75.5) | 386 (48.4) | 344 (51.5) |
| Setting, no. (%) of patients with eating disorder–related ED visit | ||||||||
| Community or small hospital | 626 (43.5) | 1251 (41.7) | 791 (54.5) | 703 (49.0) | 337 (56.4) | 299 (51.5) | 247 (64.0) | 218 (63.4) |
| Adult academic hospital | 101 (7.0) | 149 (5.0) | 605 (41.7) | 665 (46.4) | 223 (37.3) | 261 (44.9) | 113 (29.3) | 115 (33.4) |
| Pediatric academic hospital | 711 (49.4) | 1597 (53.3) | 55 (3.8) | 66 (4.6) | 38 (6.4) | 21 (3.6) | 26 (6.7) | 11 (3.2) |
| Eating disorder–related hospital admissions | ||||||||
| Patients with an eating disorder–related hospital admission | 2335 (95.0) | 3609 (92.5) | 1318 (77.5) | 1143 (74.8) | 766 (89.0) | 649 (84.3) | 637 (79.8) | 540 (80.8) |
| Setting, no. (%) of patients with eating disorder–related hospital admission | ||||||||
| Community or small hospital | 813 (34.8) | 1482 (41.1) | 715 (54.2) | 578 (50.6) | 377 (49.2) | 313 (48.2) | 345 (54.2) | 299 (55.4) |
| Adult academic hospital | 196 (8.4) | 241 (6.7) | 585 (44.4) | 549 (48.0) | 379 (49.5) | 322 (49.6) | 275 (43.2) | 227 (42.0) |
| Pediatric academic hospital | 1326 (56.8) | 1886 (52.3) | 18 (1.4) | 16 (1.4) | 10 (1.3) | 14 (2.2) | 17 (2.7) | 14 (2.6) |
| Length of hospital stay, d, mean ± SD | 23.25 ± 45.42 | 18.39 ± 33.09 | 31.04 ± 85.21 | 19.05 ± 27.65 | 30.04 ± 43.00 | 26.07 ± 37.46 | 36.05 ± 47.09 | 30.20 ± 40.93 |
| Median (IQR) | 12 (6–24) | 11 (5–20) | 12 (3–35) | 8 (3–25) | 17 (5–42) | 14 (5–31) | 21 (7–47) | 15 (7–37) |
Note: ED = emergency department, IQR = interquartile range, MH = mental health, SD = standard deviation.
Unless indicated otherwise.
Proportions do not add up to 100% because some people had diagnoses in more than 1 category.
Other eating disorders included atypical anorexia nervosa, atypical bulimia nervosa, pica, rumination disorder, feeding disorders of infancy and childhood, other eating disorders and unspecified eating disorders.
Emergency department visits for eating disorders
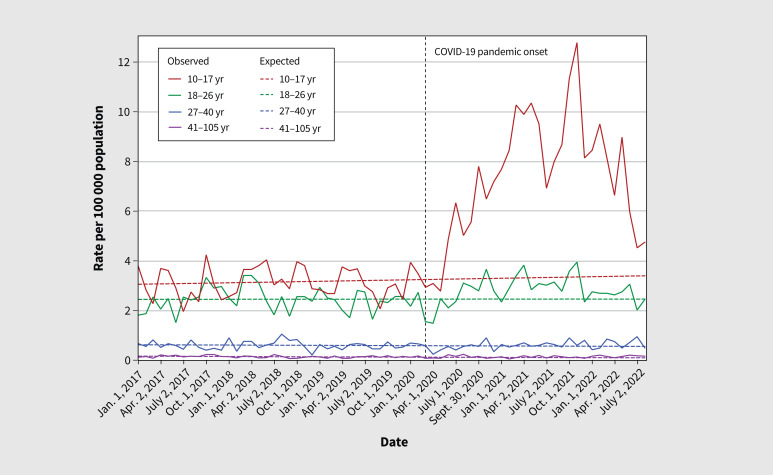
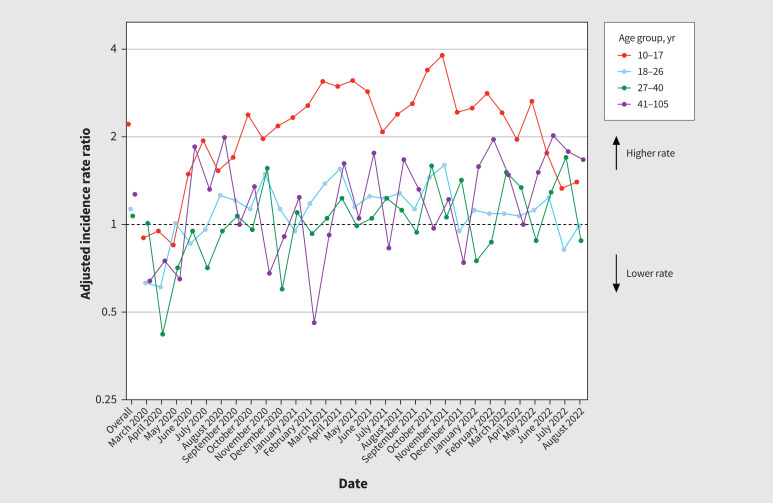
In the prepandemic period, the monthly rate of emergency department visits per 100 000 population for eating disorders was 3.33 for adolescents aged 10–17 years, 2.46 for young adults aged 18–26 years, 0.57 for adults aged 27–40 years and 0.11 for adults aged 41–105 years. Rates of emergency department visits were below expected levels for adolescents and young adults from March 2020 through to April and May 2020, followed by an increase above expected rates that was largely sustained until the end of the study period (August 2022). Overall, the rate of emergency department visits for eating disorders was 7.38 per 100 000 among adolescents (aged 10–17 yr) during the 30 months following the pandemic onset, corresponding to a 121% increase above expected (IRR 2.21, 95% CI 2.17–2.26). Emergency department visits for eating disorders peaked for adolescents in November 2021 (IRR 3.81, 95% CI 3.73–3.90; Figure 1, Figure 2 and Appendix 2, eTable 2, available at www.cmaj.ca/lookup/doi/10.1503/cmaj.221318/tab-related-content).
Figure 1:
Observed and expected rates (per 100 000 people) of eating disorder–related emergency department visits in Ontario by age group (10–17 yr, 18–26 yr, 27–40 yr, 41–105 yr), from January 2017 to August 2022.
Figure 2:
Adjusted monthly incidence rate ratios of observed versus expected eating disorder–related emergency department visits following the onset of the COVID-19 pandemic, modelled using prepandemic trends in Ontario, by age group. Sex, age group, year and seasonality (months) were used to predict expected rates.
Among young adults aged 18–26 years, emergency department visits for eating disorders during the pandemic period increased above expected by 13% (IRR 1.13, 95% CI 1.10–1.16), corresponding to a visit rate of 2.79 per 100 000. Emergency department visits for eating disorders among young adults peaked in November 2021 with a visit rate of 3.95 per 100 000 (IRR 1.60, 95% CI 1.56–1.65) (Figure 1, Figure 2 and Appendix 2, eTable 2).
Emergency department visit rates for eating disorders among adults aged 27–40 years were near expected levels throughout the pandemic period, with a visit rate of 0.61 per 100 000 (IRR 1.07, 95% CI 0.99–1.15). The observed rate of emergency department visits for adults aged 41–105 years was above the expected rate at 0.14 per 100 000 (IRR 1.15, 95% CI 1.07–1.24; Figure 1, Figure 2 and Appendix 3, eTable 3, available at www.cmaj.ca/lookup/doi/10.1503/cmaj.221318/tab-related-content).
Overall, analyses stratified by sex showed that the observed rate of emergency department visits for females was 63% above the expected rate (IRR 1.63, 95% CI 1.55–1.72), and the observed rate for males was around expected levels (IRR 1.14, 95% CI 0.99–1.31; Appendix 4, eTable 4, available at www.cmaj.ca/lookup/doi/10.1503/cmaj.221318/tab-related-content).
Hospital admissions for eating disorders
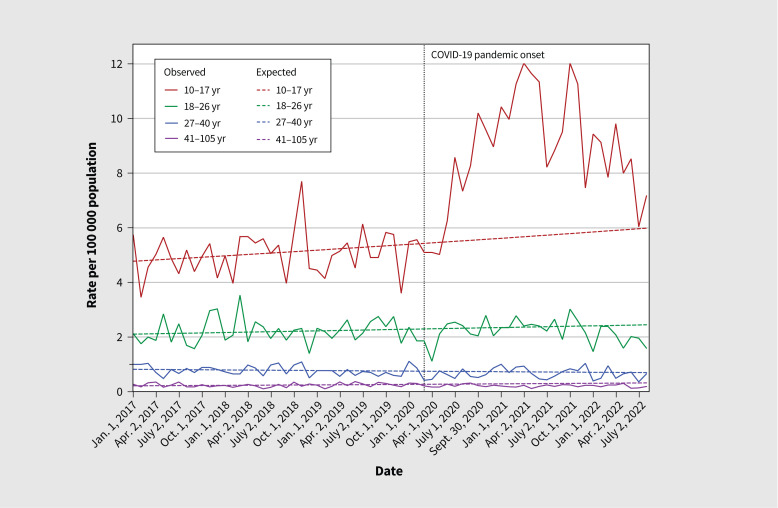
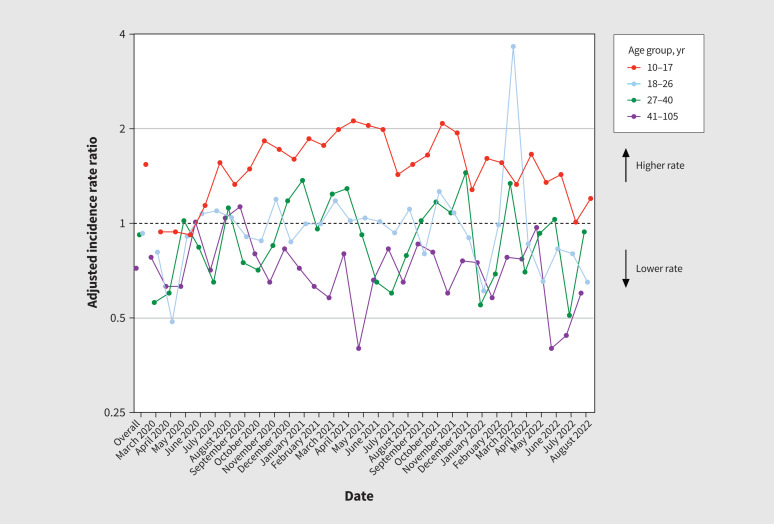
The prepandemic rate of hospital admissions for eating disorders was 5.74 for adolescents aged 10–17 years, 2.38 for young adults aged 18–26 years, 0.72 for adults aged 27–40 years and 0.30 for adults aged 41–105 years, per 100 000 population. As seen with emergency department visits, admissions for eating disorders among adolescents were below expected levels for the first 3 months following onset of the pandemic, followed by a sustained increase above expected through August 2022 (Figure 3, Figure 4 and Appendix 2, eTable 2). Overall, hospital admissions increased by 54% (IRR 1.54, 95% CI 1.54–1.54) above expected among adolescents, corresponding to a visit rate of 8.82 per 100 000 population. Hospital admissions peaked for adolescents in April 2021 (IRR 2.12, 95% CI 2.12–2.12) (Figure 3, Figure 4 and Appendix 2, eTable 2).
Figure 3:
Observed and expected rates (per 100 000 people) of eating disorder–related hospital admissions over time in Ontario by age group (10–17 yr, 18–26 yr, 27–40 yr, 41–105 yr), from January 2017 to August 2022.
Figure 4:
Adjusted monthly incidence rate ratios of observed versus expected eating disorder–related hospital admissions following the onset of the COVID-19 pandemic, modelled using prepandemic trends in Ontario, by age group. Sex, age group, year and seasonality (months) were used to predict expected rates.
Rates of hospital admissions for eating disorders among all adult age groups were near or below expected during the study period (Figure 3; Figure 4; Appendix 2, eTable 2; and Appendix 3, eTable 3). Hospital admissions for eating disorders among young adults decreased 7% below expected rates, with an overall rate of hospital admissions of 2.21 per 100 000. Admissions for adults aged 27–40 years decreased by 8% (IRR 0.92, 95% CI 0.90–0.94) below expected, with an overall rate of 0.66 per 100 000 (Figure 3, Figure 4 and Appendix 2, eTable 2). Among older adults aged 41–105 years, admissions for eating disorders decreased by 28% (IRR 0.72, 95% CI 0.64–0.80) below expected (Figure 3, Figure 4 and Appendix 3, eTable 3).
Overall, analyses stratified by sex showed that the observed rates of hospital admission for both females (IRR 1.25, 95% CI 1.16–1.35) and males (RR 1.13, 95% CI 1.08–1.17) were above expected (Appendix 4, eTable 4).
Interpretation
We observed a differential impact of the COVID-19 pandemic on acute eating disorder–related presentations among adolescents and adults in Ontario. For adolescents, the rate of emergency department visits and hospital admissions for eating disorders increased significantly compared with expected rates; we observed smaller increases in emergency department visits among young adults (18–26 yr) and older adults (41–105 yr). Hospital admissions decreased below expected rates for all adult age groups, with the greatest decrease observed among older adults.
Our findings are consistent with other global reports, with studies from the United States, Israel and Australia reporting increases in presentations for eating disorders among children, adolescents and young adults.4–7,17–20 In contrast, a study conducted in New Zealand reported a nonsignificant increase in pediatric hospital admissions.8 Unlike our results, the authors reported a near doubling in overall hospital admissions, driven by admissions for those older than 18 years.8 The reasons for this contrasting pattern are unclear; these findings do not align with the findings of most published studies, including our study.
A combination of risk factors — including isolation, increased time on social media, extended time spent with family, decreased access to care and fear of infection — may contribute to an increased risk of development or exacerbation of an eating disorder. 21–24 We previously showed a 10%–15% increase in use of pediatric mental health care in Ontario during the COVID-19 pandemic, with a disproportionate effect on school-aged and adolescent females.25 An overall rise in mental health disorders may be contributing to important comorbidities among those presenting with eating disorders. The magnitude of the increase in presentations for eating disorders among adolescents varies across studies, which may be partially explained by the hospital type, region, timing and length of pandemic period, access points for care, types of treatment available or the number of hospitals included.26
Fewer data are available on presentations for eating disorders during the pandemic among adult populations, although existing studies have reported an increase in hospital admissions, inpatient care and outpatient care;8–10 qualitative studies have reported an increase in eating disorder symptomatology among adults.27–32 Our finding that hospital admissions were lower than expected among older adults may reflect a decrease in non–COVID-19-related bed availability and capacity, redeployment of hospital resources and personnel and overall treatment delays. This may not be specific to eating disorders, given that others have reported decreases in hospital admissions and treatment delays for conditions including breast cancer, asthma, chronic obstructive pulmonary disease, heart failure and other psychiatric illnesses.33–36
Several mechanisms have been postulated as to why the COVID-19 pandemic may have triggered or exacerbated disordered eating behaviours. Increased concern about health and fitness during the pandemic may have contributed to new onset of disordered eating or to worsening symptomatology because of decreased opportunities to exercise, fear of weight gain and increased media focus on at-home workouts and general wellness.21,37–39 For those living alone, social isolation may contribute to eating disorders and lack of social interactions may permit disordered eating without fear of others noticing.21,37 For those living in a household with others, increased household stress may affect eating behaviours.21,37,40 Differences in patterns of acute care use for eating disorders by age are likely multifactorial. Eating disorders are more prevalent among young women than other demographic groups.41 The nature of eating disorders (particularly anorexia nervosa) is such that individuals fear weight gain and, therefore, hesitate to seek treatment for themselves.42 Pediatric patients may be more likely to receive care than adults as they are often living with parents or caregivers who choose to seek care if they are worried about their child’s eating behaviours or cognitions, or their weight. In many cases, pediatric patients lack capacity to make treatment decisions specifically related to their eating disorder, and health care providers frequently rely on substitute decision-makers (i.e., parents and caregivers).11 Furthermore, the threshold for hospital admission in adults with eating disorders is higher and is often reserved for times when a patient’s life is imminently at risk.11
Within the context of the COVID-19 pandemic, associated restrictions and hospital strain, additional factors differentially affected adults considering seeking care. For example, given that older adults were at higher risk of severe illness associated with COVID-19, they may have been more reluctant to attend the hospital. Furthermore, many emergency departments did not permit patients to have caretakers or support people with them in the hospital, and the media described how adult emergency departments were above capacity and had lengthy weight times, which could have deterred adults from seeking care. Lastly, some adult admissions may not have been appropriately coded as eating disorders if they were primarily for other medical issues such as bradycardia, electrolyte abnormalities or gastroparesis. Relatively few adult hospital beds are dedicated to eating disorders in Ontario, and it is uncommon for these patients to be admitted to general psychiatry units, where they may be more likely to be coded as eating disorder–related admissions. However, these limitations in coding for eating disorders were present both before and after the pandemic. Further qualitative work is required to understand the drivers of both trends in eating disorder behaviour as well as care-seeking behaviour in those with eating disorders.
Limitations
Our data included acute care visits to all community and academic hospitals in Ontario, Canada, and reflected population-level trends. Our results may not generalize to settings with different organization of health care services for eating disorders and where pandemic-related public health measures differed. We may have under-reported the clinical burden of eating disorders as our databases do not capture services delivered by other allied health professionals. Other limitations of health administrative data include the inability to quantify disease severity, potential coding errors, lag in data transfer and limited clinical information. Despite some of the concerns regarding the reliability and validity of administrative data, Kurdyak and colleagues16 previously showed that it is feasible to use health administrative data to measure the clinically relevant burden of eating disorders. In Ontario, ambulatory care physician visits are not specifically coded for eating disorders and, therefore, were not included in our analyses.
Conclusion
We observed a differential impact of the pandemic on use of acute care services for eating disorders by age after onset of the COVID-19 pandemic. Presentations to emergency departments and hospital admissions increased above expected levels among adolescents. Emergency department visits also increased above expected levels for both young (ages 18–26 yr) and older (ages 41–105 yr) adults. Hospital admissions decreased among all adult age groups. Our findings suggest differing use of mental health services by age. Health systems should focus on expanding system capacity and resources for adolescent and adult eating disorder programs. Further research is needed to determine the degree to which the surge in acute presentations is attributable to new eating disorders or exacerbation of pre-existing eating disorders.
Supplementary Material
Footnotes
Competing interests: Natasha Saunders reports receiving personal fees from The BMJ Group’s Archives of Diseases in Childhood and grants from the Canadian Institutes of Health Research (CIHR), the Ontario Ministry of Health, the Centre for Addiction and Mental Health and The Hospital for Sick Children. Astrid Guttmann reports funding from CIHR. No other competing interests were reported.
This article has been peer reviewed.
Contributors: Alene Toulany, Natasha Saunders, Paul Kurdyak, Astrid Guttmann and Therese Stukel contributed to study concept and design. Alene Toulany, Natasha Saunders, Paul Kurdyak, Rachel Strauss, Longdi Fu, Nicolette Joh-Carnella, Simon Chen, Astrid Guttmann and Therese Stukel contributed to data acquisition, analysis and interpretation. Alene Toulany and Nicolette Joh-Carnella drafted the manuscript. All of the authors revised it critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). This study was also supported by the MOH Grant 710 and the Canadian Institutes of Health Research Grant MS1-173069, both awarded to Natasha Saunders and Alene Toulany.
Data sharing: The data set from this study is held securely in coded form at ICES. Although legal data sharing agreements between ICES and data providers (e.g., health care organizations and governments) prohibit ICES from making the data set publicly available, access may be granted to those who meet prespecified criteria for confidential access, available at https://www.ices.on.ca/DAS (das@ices.on.ca). The full data set creation plan and underlying analytical code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Disclaimer: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOH or MLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the authors, and not necessarily those of CIHI. Geographical data are adapted from Statistics Canada, Postal CodeOM Conversion File Plus 2011 (Version 6D) and 2016 (Version 7B). This does not constitute endorsement by Statistics Canada of this project.
References
- 1.Tavolacci M-P, Ladner J, Déchelotte P. Sharp increase in eating disorders among university students since the COVID-19 pandemic. Nutrients 2021;13:3415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spettigue W, Obeid N, Erbach M, et al. The impact of COVID-19 on adolescents with eating disorders: a cohort study. J Eat Disord 2021;9:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toulany A, Kurdyak P, Guttmann A, et al. Acute care visits for eating disorders among children and adolescents after the onset of the COVID-19 pandemic. J Adolesc Health 2022;70:42–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haripersad YV, Kannegiesser-Bailey M, Morton K, et al. Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Arch Dis Child 2021;106:e15. [DOI] [PubMed] [Google Scholar]
- 5.Lin JA, Hartman-Munick SM, Kells MR, et al. The impact of the COVID-19 pandemic on the number of adolescents/young adults seeking eating disorder-related care. J Adolesc Health 2021;69:660–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Otto AK, Jary JM, Sturza J, et al. Medical admissions among adolescents with eating disorders during the COVID-19 pandemic. Pediatrics 2021;148:e2021052201. [DOI] [PubMed] [Google Scholar]
- 7.Agostino H, Burstein B, Moubayed D, et al. Trends in the incidence of new-onset anorexia nervosa and atypical anorexia nervosa among youth during the COVID-19 pandemic in Canada. JAMA Netw Open 2021;4:e2137395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hansen SJ, Stephan A, Menkes DB. The impact of COVID-19 on eating disorder referrals and admissions in Waikato, New Zealand. J Eat Disord 2021;9:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asch DA, Buresh J, Allison KC, et al. Trends in us patients receiving care for eating disorders and other common behavioral health conditions before and during the COVID-19 pandemic. JAMA Netw Open 2021;4:e2134913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Devoe DJ, Han A, Anderson A, et al. The impact of the COVID-19 pandemic on eating disorders: a systematic review. Int J Eat Disord 2023;56:5–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bryden P, Steinegger C, Jarvis D. The Ontario experience of involuntary treatment of pediatric patients with eating disorders. Int J Law Psychiatry 2010;33:138–43. [DOI] [PubMed] [Google Scholar]
- 12.Hudson JI, Hiripi E, Pope HG, Jr, et al. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biol Psychiatry 2007;61:348–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Volpe U, Tortorella A, Manchia M, et al. Eating disorders: What age at onset? Psychiatry Res 2016;238:225–7. [DOI] [PubMed] [Google Scholar]
- 14.Iwajomo T, Bondy SJ, de Oliveira C, et al. Excess mortality associated with eating disorders: population-based cohort study. Br J Psychiatry 2021; 219:487–93. [DOI] [PubMed] [Google Scholar]
- 15.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453–7. [DOI] [PubMed] [Google Scholar]
- 16.Kurdyak P, de Oliveira C, Iwajomo T, et al. Identifying individuals with eating disorders using health administrative data. Can J Psychiatry 2020;65:107–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matthews A, Kramer RA, Peterson CM, et al. Higher admission and rapid readmission rates among medically hospitalized youth with anorexia nervosa/atypical anorexia nervosa during COVID-19. Eat Behav 2021;43:101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldberg L, Ziv A, Vardi Y, et al. The effect of COVID-19 pandemic on hospitalizations and disease characteristics of adolescents with anorexia nervosa. Eur J Pediatr 2022;181:1767–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Springall G, Cheung M, Sawyer SM, et al. Impact of the coronavirus pandemic on anorexia nervosa and atypical anorexia nervosa presentations to an Australian tertiary paediatric hospital. J Paediatr Child Health 2022;58:491–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heeney C, Lee S, Gillman K, et al. Impact of the coronavirus pandemic on anorexia nervosa and atypical anorexia nervosa presentations. J Paediatr Child Health 2022;58:210–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernández-Aranda F, Casas M, Claes L, et al. COVID-19 and implications for eating disorders. Eur Eat Disord Rev 2020;28:239–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Touyz S, Lacey H, Hay P. Eating disorders in the time of COVID-19. J Eat Disord 2020;8:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katzman DK. The COVID-19 pandemic and eating disorders: a wake-up call for the future of eating disorders among adolescents and young adults. J Adolesc Health 2021;69:535–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooper M, Reilly EE, Siegel JA, et al. Eating disorders during the COVID-19 pandemic and quarantine: an overview of risks and recommendations for treatment and early intervention. Eat Disord 2022;30:54–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saunders NR, Kurdyak P, Stukel TA, et al. Utilization of physician-based mental health care services among children and adolescents before and during the COVID-19 pandemic in Ontario, Canada. JAMA Pediatr 2022;176:e216298. doi: 10.1001/jamapediatrics.2021.6298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saunders NR, Stukel TA, Strauss R, et al. Changes in hospital-based care seeking for acute mental health concerns among children and adolescents during the COVID-19 pandemic in Ontario, Canada, through September 2021. JAMA Netw Open 2022;5:e2220553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Branley-Bell D, Talbot CV. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. J Eat Disord 2020;8:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bryan DC, Macdonald P, Ambwani S, et al. Exploring the ways in which COVID-19 and lockdown has affected the lives of adult patients with anorexia nervosa and their carers. Eur Eat Disord Rev 2020;28:826–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phillipou A, Meyer D, Neill E, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int J Eat Disord 2020;53:1158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One 2020;15:e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schneider J, Pegram G, Gibson B, et al. A mixed-studies systematic review of the experiences of body image, disordered eating, and eating disorders during the COVID-19 pandemic. Int J Eat Disord 2023;56:26–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miskovic-Wheatley J, Koreshe E, Kim M, et al. The impact of the COVID-19 pandemic and associated public health response on people with eating disorder symptomatology: an Australian study. J Eat Disord 2022;10:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Papautsky EL, Hamlish T. Patient-reported treatment delays in breast cancer care during the COVID-19 pandemic. Breast Cancer Res Treat 2020;184:249–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sykes DL, Faruqi S, Holdsworth L, et al. Impact of COVID-19 on COPD and asthma admissions, and the pandemic from a patient’s perspective. ERJ Open Res 2021;7:00822–02020. doi: 10.1183/23120541.00822-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hall ME, Vaduganathan M, Khan MS, et al. Reductions in heart failure hospitalizations during the COVID-19 pandemic. J Card Fail 2020;26:462–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boldrini T, Girardi P, Clerici M, et al. Italian Network for Research on Mental Health during COVID-19 Pandemic. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: reduced psychiatric hospitalizations and increased suicidality. Prog Neuropsychopharmacol Biol Psychiatry 2021;110:110304. doi: 10.1016/j.pnpbp.2021.110304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dalle Grave R. Coronavirus disease 2019 and eating disorders [blog]. Psychology Today 2020. Mar. 21. Available: https://www.psychologytoday.com/blog/eating-disorders-the-facts/202003/coronavirus-disease-2019-and-eating-disorders (accessed 2020 Dec. 30).
- 38.Greenspan RE. Fitness content is everywhere during the coronavirus pandemic. Experts say it’s putting those with a history of eating disorders at risk. Insider 2020. Mar. 30. Available: https://www.insider.com/at-home-workouts-social-media-eating-disorder-community-2020-3 (accessed 2020 Dec. 30).
- 39.Weissman RS, Bauer S, Thomas JJ. Access to evidence-based care for eating disorders during the COVID-19 crisis. Int J Eat Disord 2020;53:369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Castellini G, Cassioli E, Rossi E, et al. The impact of COVID-19 epidemic on eating disorders: a longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int J Eat Disord 2020;53:1855–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smink FRE, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 2012;14:406–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guarda AS. Treatment of anorexia nervosa: insights and obstacles. Physiol Behav 2008;94:113–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.