Abstract
Background:
The risk factors influencing the readmission within 90 days following total joint replacement (TJR) are complex and heterogeneous, and few systematic reviews to date have focused on this issue.
Methods:
Web of Science, Embase, PubMed, and Chinese National Knowledge Infrastructure databases were searched from the inception dates to December 2022. Relevant, published studies were identified using the following keywords: risk factors, rehospitalization, total hip replacement, total knee replacement, total shoulder replacement, and total joint replacement. All relevant data were collected from the studies that meet the inclusion criteria. The methodological quality of the studies was assessed using the Newcastle–Ottawa Scale (NOS).
Results:
Of 68,336 patients who underwent TJR, 1,269,415 (5.4%) were readmitted within 90 days. High American Society of Anesthesiologists (ASA) class (OR, 1.502; 95%CI:1.405–1.605; P < .001), heart failure (OR,1.494; 95%CI: 1.235–1.754; P < .001), diabetes (OR, 1.246; 95%CI:1.128–1.377; P < .001), liver disease (OR, 1.339; 95%CI:1.237–1.450; P < .001), drinking (OR, 1.114; 95%CI:1.041–1.192; P = .002), depression (OR, 1.294; 95%CI:1.223–1.396; P < .001), urinary tract infection (OR, 5.879; 95%CI: 5.119–6.753; P < .001), and deep vein thrombosis (OR, 10.007; 95%CI: 8.787–11.396; P < .001) showed statistically positive correlation with increased 90-day readmissions after TJR, but high blood pressure, smoking, and pneumonia had no significant association with readmission risk.
Conclusion:
The findings of this review and meta-analysis will aid clinicians as they seek to understand the risk factors for 90-day readmission following TJR. Clinicians should consider the identified key risk factors associated with unplanned readmissions and develop strategies to risk-stratify patients and provide dedicated interventions to reduce the rates of readmission and enhance the recovery process.
Keywords: 90-day readmissions, complications, readmission, TJR
1. Introduction
Total joint replacement (TJR) is an efficacious surgical treatment that aims to improve the function and quality of life of patients with joint diseases such as osteoarthritis and rheumatoid arthritis. Despite the success of TJR in reducing pain, improving mobility and maintaining motor function, a significant proportion of patients experience unplanned hospital readmissions within 90 days after surgery.[1,2] These readmissions can result in significant healthcare costs, increased morbidity, and decreased patient satisfaction. Identifying the risk factors for rehospitalization within 90 days after TJR is critical for developing effective strategies to prevent such readmissions.[3–5] Previous studies have reported several potential risk factors for rehospitalization, including patient demographic characteristics, comorbidities, and perioperative factors.[6,7] Many modifiable risk factors associated with short-term and long-term outcomes after TRJ were reported, including diabetes, hypertension, and body mass index. Specific complications linked to some of these comorbidities include surgical site infection, wound complications, acute kidney injury and deep vein thrombosis.[8–10] However, the strength and consistency of these associations have varied across studies. It is necessary to actively identify risk factors that affect the 90-day readmission after TJR to provide timely intervention and minimize the risk of complications, thereby reducing the incidence of repeated hospitalization.
Therefore, in this study, we explored the risk factors for rehospitalization within 90 days after TJR, which is of great significance to guide clinical medical personnel to minimize the risk of complications.
2. Methods
Ethical approval was not necessary as this study is a systematic review and meta-analysis. This systematic review and meta-analysis were conducted by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement guidelines. In this study, all methods were performed by the relevant guidelines and regulations.
2.1. Search strategy
Web of Science, Embase, PubMed and Chinese National Knowledge Infrastructure databases were searched from the inception dates to December 2022 using the keywords “risk factors,” “rehospitalization,” “total hip replacement,” “total knee replacement,” “total shoulder replacement,” “TJR,” “THR,” and “TKR,” “TSR,” “TJR.” To minimize the missing literature, references listed in the included studies were also traced to supplement relevant data.
2.2. Inclusion and exclusion criteria
The inclusion criteria for this meta-analysis were as follows: The study population were patients with TJR and the patients were aged ≥18 years; The patients presented unplanned hospital readmission within 90 days; Cohort study or case-control study design; The publication language of the article was limited to Chinese and English. The literature exclusion criteria for this meta-analysis were as follows: duplicate publications; studies with incomplete information or data for extraction; literature with low quality.
2.3. Literature screening and data extraction
Two authors separately performed selection and data collection. The full text of the studies which matched the topic of interest was accessed. If the full text was not, the article was excluded. The references of the full-text articles were screened by hand by the reviewers for inclusion. In case of disagreements, a third author took the final decision. During literature screening, first, the title and abstract were read. Then, after the exclusion of irrelevant literature, the full text of the preliminarily relevant articles was read to determine whether to include them in the final analysis. Data extraction encompassed the basic characteristics of the included studies, such as author, country, anticoagulant, age, gender, sample size, readmission time mean body mass index, hospital stay, operative time and risk factors.
2.4. Methodological quality assessment
Two authors independently used the Newcastle-Ottawa scale (NOS) to evaluate the quality of included studies. If any disagreements occurred during the evaluation process, they were resolved through discussion. The total NOS score is 9 points, and literature with NOS ≥ 7 points are generally considered high-quality.
2.5. Statistical analysis
SPSS 16.0 software was used for statistical analyses in this meta-analysis. For the meta-analyses, whenever possible, outcomes were converted to a standard scale. For all variables with the same outcome, MDs or standardized MDs with a 95% CI were calculated. A fixed effect model or a random effect model was adopted according to the heterogeneity of the included studies, and Cochran Q and I2 statistics were used to test the heterogeneity. A fixed-effects model was used when I2 < 50%. Otherwise, a random-effects model was chosen. Publication bias was evaluated by using funnel plots, and asymmetry was assessed with Egger test. In this meta-analysis, P < .05 was considered that the difference was statistically significant between groups.
3. Results
3.1. Literature search and screening results
The process of selecting studies is presented in Figure 1. The initial database research resulted in 1350 articles. Of those identified articles, 427 were excluded as they were duplicates. A further 895 articles were excluded as they did not match the eligibility criteria: not reporting data on the insufficient follow-up time (N = 385), not clearly reporting the risk factors (N = 45), inadequate study design or aim (N = 84), insufficient data (N = 45), poor level of evidence (N = 84). Finally, 16 studies were included: 15 Case-control and 1 Cohort.
Figure 1.
Flow chart of the identification and inclusion of articles.
3.2. Basic characteristics and quality assessment of included literature
A total of 16 studies were identified for inclusion in the current review that reported on a total of 12,69,415 TJR patients, and 68,336 (5.38%) patients experienced unplanned hospital readmissions within 90 days after TJR. The basic characteristics of the studies are shown in Table 1. The quality of the included studies was evaluated. 2 articles had a NOS score of 7, 13 papers had a NOS score of 8, and 1 article had a NOS score of 9. The quality assessment of all articles was ≧ 7 points, suggesting that the overall quality of the included articles was high (Table 1).
Table 1.
Characteristics of studies used for meta-analysis of risk factors for readmission after total joint replacement (TJR).
| Study | Country | Study design | Age (mean ± SD) | Gender (M/F) | BMI category | Sample size | Readmitted (N) | Readmitted (%) | Hospital stay (d) | Operative time (min) | Risk factors | NOS scores |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ricciard et al (2016)[11] | USA | Cohort | 66.1 ± 9.4 | 46.7%/53.3% | 29.3 ± 6.1 | 180 | 60 | NA | NA | 84.4 ± 24.6 | 8 | 9 |
| White et al (2018)[12] | USA | Case-control | 69.62 ± 13.18 | 42.3%/57.5% | NA | 274,851 | 15,273 | 5.56 | 4.00 | NA | 2, 3, 4, 5, 7, 12 | 8 |
| Lehtonen et al (2018)[13] | USA | Case-control | 68.49 | 43.7%/56.3% | NA | 137,209 | 4668 | 3.4 | NA | NA | 9, 10, 11, 12 | 8 |
| Urish et al (2018)[14] | USA | Case-control | 66 | 57%/43% | NA | 224,465 | 7816 | 3.48 | NA | NA | 2, 4, 12, | 8 |
| Belmont et al (2016)[15] | USA | Case-control | 66.2 ± 10.9 | 52.7%/47.3% | NA | 1754 | 108 | 6.16 | NA | NA | 5, 9, 10, 12 | 8 |
| Keswani et al (2016)[16] | USA | Case-control | 67.2 ± 11.2 | 49%/51% | NA | 4977 | 318 | 6.4 | NA | 136.00 | 1, 2, 6, 11 | 8 |
| Keswani(2016)[16] | USA | Case-control | 68.1 ± 13.3 | 45%/55% | NA | 5135 | 409 | 7.9 | NA | 154.00 | 1, 2, 6, 11 | 8 |
| Paxton et al (2015)[17] | USA | Case-control | 70.5 ± 10.2 | 41%/59% | NA | 12,030 | 436 | 3.62 | 3.40 | NA | 1, 2, 3, 4, 5, 12 | 8 |
| Schairer et al (2013)[18] | USA | Case-control | 58.3 ± 15.8 | 38.7%/61.3% | NA | 1416 | 93 | 6.57 | NA | NA | 6 | 8 |
| Roger et al (2019)[19] | USA | Case-control | 66 ± 12 | 44.8%/55.2% | NA | 1663 | 51 | 3.06 | NA | NA | 2, 5, 6, 8 | 7 |
| Cantrell et al (2020)[20] | USA | Case-control | 67.7 | 45.4%/54.6% | NA | 10,031 | 855 | 8.5 | 5.07 | 153.70 | 9, 10, 11, 12 | 8 |
| Workman et al (2020)[21] | USA | Case-control | 68.5 ± 10.9 | 40.48%/59.52% | NA | 7482 | 210 | 2.8 | NA | NA | 2 | 7 |
| Goltz et al (2019)[22] | USA | Case-control | 66.847 | 43%/57% | 31.18 | 10,022 | 497 | 5 | NA | NA | 3, 7, 8 | 8 |
| Loppini et al (2021)[23] | Italy | Case-control | 55 | 60.1%/39.9% | NA | 521 | 46 | 0.9 | NA | NA | 1, 2, 3, 5, 6, 12 | 8 |
| Phruetthiphat et al (2020)[24] | USA | Case-control | 63.7 + 15.5 | 54.8%/45.2% | NA | 1226 | 42 | 3.4 | 4.00 | 111.40 | 1 | 8 |
| Phruetthiphat et al (2020)[24] | USA | Case-control | 64.0 + 11.1 | 17.9%/82.1% | NA | 1256 | 28 | 2.2 | 4.20 | 101.10 | 2, 5, | 8 |
| Ali Adam et al (2019)[25] | UK | Case-control | NA | 42.2%/57.8% | NA | 566,323 | 37, 195 | 6 | NA | NA | 2, 3, 4, 5, 7, 8, 11, 12 | 8 |
| Chaudhry et al (2020)[26] | USA | Case-control | NA | NA | 28 ± 6.6 | 3292 | 91 | 2.7 | NA | NA | 1, 2, 4, 6, | 8 |
| Chaudhry et al (2020)[26] | USA | Case-control | NA | NA | 30 ± 6.6 | 5582 | 140 | 2.5 | NA | NA | 1, 2 | 8 |
1, American Society of Anesthesiologists Classification; 2, diabetes; 3, liver disease; 4, heart failure; 5, high blood pressure; 6, smoking; 7, drinking; 8, depression; 9, urinary tract infection; 10, deep vein thrombosis; 11, pneumonia; 12, kidney disease.
BMI = body mass index, NA = not available, NOS = Newcastle-Ottawa scale.
3.3. Meta-analysis
3.3.1. Sensitivity and heterogeneity analysis.
Between-study heterogeneity was examined and significant heterogeneity (P < .05) was detected in some risk factors, so the random-effects model was adopted; otherwise, the fixed-effect model was utilized. The sensitivity analysis was carried out through sequential exclusion of any one individual study, and the results showed that our conclusion was robust and credible (Table 2).
Table 2.
Sensitivity and heterogeneity analysis of risk factors.
| Risk factors | No. of studies | Heterogeneity | Model | Synthesis result | |||
|---|---|---|---|---|---|---|---|
| I2 (%) | P | OR | 95% CI | P | |||
| ASA Classification | 7 | 39.6 | .128 | Fixed-effects | 1.502 | 1.405~1.605 | .000 |
| Diabetes | 12 | 73.7 | .000 | Random-effects | 1.246 | 1.128~1.377 | .000 |
| Liver disease | 5 | 0.0 | .946 | Fixed-effects | 1.339 | 1.237~1.450 | .000 |
| Heart failure | 5 | 95.2 | .000 | Random-effects | 1.389 | 1.061~1.818 | .017 |
| High blood pressure | 7 | 71.9 | .002 | Random-effects | 1.025 | 0.953~1.102 | .510 |
| Smoking | 6 | 78.9 | .000 | Random-effects | 1.043 | 0.776~1.402 | .781 |
| Drinking | 3 | 28.5 | .247 | Fixed-effects | 1.114 | 1.041~1.192 | .002 |
| Depression | 4 | 1.5 | .385 | Fixed-effects | 1.294 | 1.223~1.396 | .000 |
| Urinary tract infection | 3 | 41.8 | .180 | Fixed-effects | 5.879 | 5.119~6.753 | .000 |
| Deep vein thrombosis | 3 | 28.8 | .246 | Fixed-effects | 10.007 | 8.787~11.396 | .000 |
| Pneumonia | 5 | 99.1 | .000 | Random-effects | 2.088 | 0.558~7.811 | .274 |
| Kidney disease | 7 | 96.4 | .000 | Random-effects | 1.925 | 1.416~2.618 | .000 |
ASA = American society of anesthesiologists.
3.3.2. Meta-analysis of readmission within 90 days risk factors.
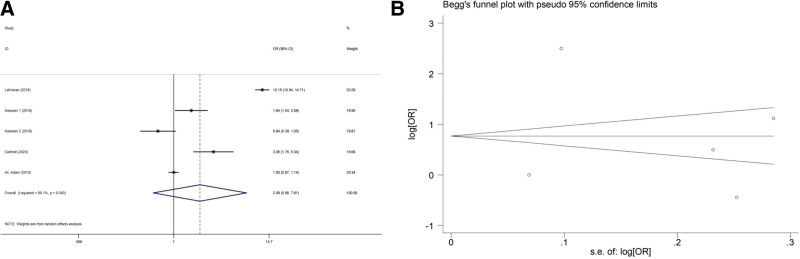
American society of anesthesiologists (ASA) classification
There was no significant heterogeneity (I2 = 39.6%, P = .128) among 7 included studies. Each study was excluded one by one, and the results of meta-analysis showed that there was no significant change in the combined effect. A fixed effects model analysis was conducted to yield a pooled OR of 1.502 (95% CI, 1.405–1.605), and the difference was statistically significant (P < .001), suggesting that higher American society of anesthesiologists (ASA) classification was associated with a higher risk of unplanned 90-day readmission after TJR (Fig. 2).
Figure 2.
(A) Forest plot showing the relationship between American society of anesthesiologists (ASA) classification and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of ASA classification.
Diabetes
High level of heterogeneity (I2 = 73.7%, P < .001) was present among 12 included studies. Sensitivity analysis was conducted by excluding studies from the analysis one by one, and a random-effects model instead of a fixed-effects model was also used to test the robustness of the meta-analysis results (Fig. 3), suggesting that diabetes was associated with a higher risk of unplanned 90-day readmission after TJR (OR = 1.246, 95%CI: 1.128–1.377, P < .001).
Figure 3.
(A) Forest plot showing the relationship between diabetes and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of diabetes.
Liver disease
There was no significant heterogeneity (I2 = 0.0%, P = .941) among 5 included studies. The fixed effects model showed that liver disease was associated with a higher risk of unplanned 90-day readmission after TJR (OR = 1.339, 95%CI: 1.237–1.450, P < .001) (Fig. 4).
Figure 4.
(A) Forest plot showing the relationship between liver disease and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of liver disease.
Heart failure
For the high heterogeneity (I2 = 95.2%, P < .001), we conducted the sensitivity analysis and found the heterogeneity was attributed to the study by Ali Adam et al.[11] After excluding this study, the heterogeneity significantly decreased to 71.4%, and heart failure was associated with a higher risk of unplanned 90-day readmission after TJR (OR = 1.494, 95%CI: 1.235–1.754, P < .001) (Fig. 5).
Figure 5.
(A) Forest plot showing the relationship between heart failure and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of heart failure.
High blood pressure
High level of heterogeneity (I2 = 71.9%, P = .002) was present among 7 included studies. Similarly, sensitivity analysis results showed no obvious change in effect values when single studies were excluded one by one and then subjected to Meta-analysis, suggesting more stable study results. However, when the random-effects model analysis was performed, no significant difference was detected (OR = 1.025, 95%CI: 0.953–1.102, P = .510) (Fig. 6).
Figure 6.
(A) Forest plot showing the relationship between high blood pressure and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of high blood pressure.
Smoking
There was a significantly high level of heterogeneity across the included studies (I2 = 78.9%, P < .001). Sensitivity analysis results showed no obvious change in effect values when single studies were excluded one by one. Random-effect model analysis revealed no statistically significant correlation between smoking and the risk of unplanned 90-day readmission after TJR (OR = 1.043; 95% CI 0.776–1.402, P = .781) (Fig. 7).
Figure 7.
(A) Forest plot showing the relationship between smoking and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of smoking.
Drinking
There was no significant heterogeneity (I2 = 28.5%, P = .247) among 3 included studies. The fixed effects model showed that drinking was associated with a higher risk of unplanned 90-day readmission after TJR (OR = 1.114, 95%CI: 1.041–1.192, P = .002) (Fig. 8).
Figure 8.
(A) Forest plot showing the relationship between drinking and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of drinking.
Depression
There was no heterogeneity between the study (I2 = 1.5%, P = .385), the fixed-effect model was used and indicating that depression was associated with a higher risk of unplanned 90-day readmission after TJR (OR = 1.294, 95%CI: 1.223–1.396, P = .002) (Fig. 9).
Figure 9.
(A) Forest plot showing the relationship between depression and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of depression.
Urinary tract infection
There was no significant heterogeneity (I2 = 41.8%, P = .180) among 3 included studies. The fixed effects model showed that urinary tract infection was associated with a higher risk of unplanned 90-day readmission after TJR (OR = 5.879, 95%CI: 5.119–6.753, P < .001) (Fig. 10).
Figure 10.
(A) Forest plot showing the relationship between urinary tract infection and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of urinary tract infection.
Deep vein thrombosis
There was no heterogeneity between the study (I2 = 28.8%, P = .246), the fixed-effect model was used and indicating that deep vein thrombosis was associated with a higher risk of unplanned 90-day readmission after TJR (OR = 10.007, 95%CI: 8.787–11.396, P < .001) (Fig. 11).
Figure 11.
(A) Forest plot showing the relationship between deep vein thrombosis and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of deep vein thrombosis.
Pneumonia
A relatively high level of heterogeneity (I2 = 99.1%, P < .001) was present among 5 included studies. Sensitivity analysis was conducted by excluding studies from the analysis one by one. Random-effects model showed no statistically significant correlation between pneumonia and the risk of unplanned 90-day readmission after TJR (OR = 2.088, 95%CI: 0.558~7.811, P = .274) (Fig. 12).
Figure 12.
(A) Forest plot showing the relationship between pneumonia and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of pneumonia.
Kidney disease
Significant heterogeneity was not found in the 7 included studies (I2 = 1.5%, P = .385), and the sensitivity analysis showed that the conclusion was not altered by excluding any individual study. A fixed effects model analysis was conducted and suggesting that kidney disease was associated with a higher risk of unplanned 90-day readmission after TJR (OR = 1.925, 95%CI: 1.416–2.618, P < .001) (Fig. 13).
Figure 13.
(A) Forest plot showing the relationship between kidney disease and unplanned 90-d readmission after total joint replacement (TJR). (B) Begg funnel plot for publication bias of kidney disease.
3.3.3. Publication bias.
Egger test was utilized to examine the potential publication bias of the studies. Egger test was statistically significant for depression (t = 19.79, P = .003), indicating publication bias. There was no significant publication bias in ASA Classification(t = 0.82, P = .498), diabetes (t = 0.17, P = .872), liver disease (t = −0.72, P = .522), heart failure (t = 0.09, P = .931), high blood pressure (t = 0.19, P = .855), smoking (t = −0.99, P = .376), drinking (t = 0.67, P = .625), urinary tract infection (t = −1.84, P = .317), deep vein thrombosis (t = −1.08, P = .476), pneumonia (t = 0.12, P = .909) and kidney disease (t = 1.62, P = .167).
4. Discussion
Hospital readmission rates following TJR have been proposed as an important indicator of patient health outcomes, reducing the readmission rate during the first 90 days after hospital discharge is important to decrease the economic burden on the healthcare system and improve patient post-discharge outcomes. In previous studies, multiple demographic characteristics (increasing age, male sex, black race, morbid obesity), preoperative comorbidities (heart failure, diabetes, liver disease), and postoperative complications (surgical site infection, wound complications) were associated with higher rates of readmission following TJR.[12–15] Moreover, positive cancer history and high BUN has been reported to have a significant positive association with higher readmission rates.[15,16] Our analysis of the data from 1269,415 patients found that the overall 90-day readmission rate following TJR was 5.4%, many risk factors were associated with higher rates of readmission following TJR, including high ASA class, heart failure, diabetes, liver disease, drinking, depression, urinary tract infection, and deep vein thrombosis, but high blood pressure, smoking, and pneumonia had no significant association with readmission risk, which are consistent with other studies.
A variety of studies have highlighted the ASA classification as a reliable prognosticator for perioperative morbidity.[17] Patients with higher ASA classes are at risk of developing higher rates of postoperative medical complications after multiple orthopedic procedures.[18] Moreover, high ASA class was associated with the highest odds of readmission. Patients with ASA class 4 had more than twice the odds of readmission compared to ASA class 2. Similarly, patients with ASA class 3 had 1.43 times increased odds of readmission than ASA class 2 patients, while a prolonged length of hospital stay was associated with a higher risk of readmission. Multiple retrospective studies of individual institutions report similar findings.[12,19–21] The ASA classification system is widely utilized and available as a reliable predictor of readmission risk after TJR. In addition, heart failure is associated with longer hospital stays, higher readmission rates, and death. Saucedo et al also reported heart failure as a common reason for readmission.[22]
Specific comorbidities (liver disease, diabetes, urinary tract infection, and deep vein thrombosis) and drinking were found to be significantly associated with readmission in this study. Liver disease, spanning a spectrum from nonalcoholic fatty liver disease to cirrhosis, has long been established as a systemic disorder with far-reaching implications across multiple organ systems.[23,24] Recent research has highlighted the intricate interplay between liver dysfunction and musculoskeletal health. Liver disease is characterized by metabolic derangements, chronic inflammation, and alterations in coagulation factors, the prothrombotic state associated with liver dysfunction may predispose patients to thromboembolic events post-operatively, all of which can potentially influence the outcomes of TJR.[25,26] Significantly, these systemic repercussions have demonstrated a propensity to elevate the vulnerability to complications, encompassing infections, hindered wound healing, and compromised bone metabolism, which frequently ensue following surgical interventions.[27] Additionally, the compromised hepatic function could potentially impact the clearance of anesthetic agents and pain medications, rendering the management of postoperative pain more challenging.[28] Furthermore, the nexus between liver disease and alterations in crucial micronutrient levels, such as vitamin D, merits Acknowledgments, given the pivotal role of these micronutrients in bone health and remodeling.[29] Moreover, there is an obvious association between alcohol intake and cirrhosis, alcohol intake increases the risk of infection in cirrhosis patients. The number of total TJR performed is on the increase. Thus, it is also likely that more cirrhosis patients will undergo TJR, particularly with the rapid emergence of obesity-related liver disease known as nonalcoholic fatty liver disease.[30] It might be expected that these patients with drinking are more likely to experience liver complications postoperatively. The present study showed patients with drinking had a higher risk for 90-day readmissions. Moreover, patients with defined drinking had postoperative complications, longer postoperative lengths of stay, higher total hospital charges, and were at increased risk of dislocations, revisions, liver complications, and 90-day readmissions compared to patients without drinking, in line with the previous study.[31,32] Patients with diabetes, regardless of severity (no diabetes, controlled-uncomplicated, controlled-complicated, and uncontrolled), were at higher risk for TJR readmissions than the no-diabetes group. However, controlled-complicated diabetes had the largest odds for TJR readmissions and complications, and the risks for TJR readmissions were comparable to uncontrolled diabetes.[33] In our study, patients with diabetes were associated with higher rates of readmission following TJR, which reflected prior authors’ conclusions.
During the surgery, patients are required to maintain specific positions, such as supine position, for an extended period to facilitate the surgical procedure. This position can slow down blood flow in the lower limb veins, increasing the risk of clot formation. Additionally, tissue damage and inflammatory reactions occurring during the surgery can also contribute to the development of blood clots. Furthermore, underlying medical conditions play a crucial role in shaping deep vein thrombosis risk. Coagulation disorders, both congenital and acquired, heighten the potential for thrombus formation.[34] Conditions that predispose individuals to hypercoagulable states, such as Factor V Leiden mutation and prothrombin gene mutations, amplify the risk of postoperative deep vein thrombosis.[35] Furthermore, chronic illnesses including heart failure and chronic obstructive pulmonary disease contribute to a proinflammatory and hypercoagulable state, thereby increasing the likelihood of thrombus development.[36] The overall incidence of deep vein thrombosis following TJR in patients without thromboprophylaxis ranged around 40% to 70%, patients who have a major risk of deep vein thrombosis should preoperatively receive prophylactic anticoagulation treatment.[37] Deep vein thrombosis frequently occurs in TJR patients receiving orthopedic surgery, despite prophylactic measures for its prevention.[15] In the context of TJR, depression assumes particular significance due to its potential to impact surgical outcomes through multiple pathways. Depressive symptoms have been linked to modifications in pain perception, diminished pain tolerance, and augmented susceptibility to postoperative pain.[38,39] This altered pain processing may lead to suboptimal pain management and compromised rehabilitation efforts, subsequently affecting the functional recovery and overall satisfaction of TJR patients. Furthermore, depression can exert its influence on the recovery process and outcomes following TJR surgery through its impact on pain perception, immune function, inflammation, and neuroendocrine pathways. Brander et al reported that preoperative depression was significantly associated with poor functional outcome scores following TJR.[40] Similarly, Singh et al showed that depression was associated with pain, functional limitation, and persistent use of pain medications after revision TJR at 5-year follow-up.[41] These initial studies prompted further investigation of the relationship between depression and TJR outcomes. Moreover, depression is linked to dysregulation of the immune and inflammatory systems. The chronic inflammatory state often observed in depressed individuals can impede wound healing and increase the susceptibility to post-operative infections.[42] Additionally, depression has been correlated with hormonal imbalances, including elevated cortisol levels, which may further contribute to impaired tissue repair and unfavorable surgical outcomes.[43] More recent literature suggests that depressed patients may also be at higher risk for complications after TJR and incur greater costs for surgery.[44] Based upon the results of this review, depression is a comorbidity that may have a substantial impact on the complications, outcomes, and readmission associated with TJR. It is crucial to recognize that additional research is necessary to fully understand the underlying mechanisms and develop evidence-based interventions that can optimize outcomes for individuals with depression undergoing TJR. By acknowledging and addressing the impact of depression on the surgical process, healthcare providers have the opportunity to enhance patient care, promote better postoperative recovery, and ultimately improve the overall well-being of individuals undergoing TJR.
The findings of our study indicate that factors such as a high ASA class, heart failure, diabetes, liver disease, alcohol consumption, depression, urinary tract infection, and deep vein thrombosis may significantly contribute to the heightened risk of 90-day readmissions following TJR. Further therapeutic interventions ought to be implemented in order to mitigate the occurrence and advancement of readmissions subsequent to TJR.
The limitations of this meta-analysis should not be ignored. Some unpublished papers and conference abstracts were excluded, which could have potentially affected the final obtained results. Furthermore, heterogeneity was observed within this meta-analysis, necessitating additional validation of the conclusions through more consistent, prospective, and substantial sample-size studies.
5. Conclusions
The present meta-analysis showed that high ASA class, heart failure, diabetes, liver disease, drinking, depression, urinary tract infection, and deep vein thrombosis had positive correlation with increased 90-day readmissions after TJR. Clinicians should consider the identified key risk factors associated with unplanned readmissions and develop strategies to risk-stratify patients and provide dedicated interventions to reduce the rates of readmission and enhance the recovery process.
Acknowledgments
We are grateful to all researchers of enrolled studies.
Author contributions
Conceptualization: Lingying Lin.
Data curation: Xirong Lian.
Methodology: Dongfu Zhang.
Writing – original draft: Liping Zeng, Aling Qiu.
Writing – review & editing: Hua Cai, Manli Chen.
Abbreviations:
- ASA
- American society of anesthesiologists
- NOS
- Newcastle-Ottawa scale
- TJR
- total joint replacement
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Zeng L, Cai H, Qiu A, Zhang D, Lin L, Lian X, Chen M. Risk factors for rehospitalization within 90 days in patients with total joint replacement: A meta-analysis. Medicine 2023;102:45(e35743).
Contributor Information
Liping Zeng, Email: 632127399@qq.com.
Hua Cai, Email: x1209085627@outlook.com.
Aling Qiu, Email: 527590994@qq.com.
Dongfu Zhang, Email: 58864099@qq.com.
Lingying Lin, Email: 252196189@qq.com.
Xirong Lian, Email: 752716286@qq.com.
References
- [1].Lasater KB, McHugh MD. Reducing hospital readmission disparities of older black and white adults after elective joint replacement: the role of nurse staffing. J Am Geriatr Soc. 2016;64:2593–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Chambers MC, El-Othmani MM, Anoushiravani AA, et al. Reducing 30-day readmission after joint replacement. Orthop Clin North Am. 2016;47:673–80. [DOI] [PubMed] [Google Scholar]
- [3].Zmistowski B, Restrepo C, Hess J, et al. Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am. 2013;95:1869–76. [DOI] [PubMed] [Google Scholar]
- [4].Howie CM, Mears SC, Barnes CL, et al. Readmission, complication, and disposition calculators in total joint arthroplasty: a systemic review. J Arthroplasty. 2021;36:1823–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Morrell AT, Layon DR, Scott MJ, et al. Enhanced recovery after primary total hip and knee arthroplasty: a systematic review. J Bone Joint Surg Am. 2021;103:1938–47. [DOI] [PubMed] [Google Scholar]
- [6].Schwarzkopf R, Kaplan DJ, Friedlander S, et al. Outcomes of a first total knee arthroplasty are associated with outcomes of the subsequent contralateral total knee arthroplasty. J Arthroplasty. 2020;35:1534–9. [DOI] [PubMed] [Google Scholar]
- [7].Kheir MM, Carter Clement R, Derman PB, et al. Are there identifiable risk factors and causes associated with unplanned readmissions following total knee arthroplasty? J Arthroplasty. 2014;29:2192–6. [DOI] [PubMed] [Google Scholar]
- [8].Mednick RE, Alvi HM, Krishnan V, et al. Factors affecting readmission rates following primary total hip arthroplasty. J Bone Joint Surg Am. 2014;96:1201–9. [DOI] [PubMed] [Google Scholar]
- [9].George J, Piuzzi NS, Ng M, et al. Association between body mass index and thirty-day complications after total knee arthroplasty. J Arthroplasty. 2018;33:865–71. [DOI] [PubMed] [Google Scholar]
- [10].Jensen CB, Troelsen A, Baggesgaard Petersen P, et al. Influence of body mass index and age on day-of-surgery discharge, prolonged admission, and 90-day readmission after fast-track unicompartmental knee arthroplasty. Acta Orthop. 2021;92:722–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ali AM, Loeffler MD, Aylin P, et al. Predictors of 30-Day readmission after total knee arthroplasty: analysis of 566,323 procedures in the United Kingdom. J Arthroplasty. 2019;34:242–248.e1. [DOI] [PubMed] [Google Scholar]
- [12].Lehtonen EJ, Hess MC, McGwin G, et al. Risk factors for early hospital readmission following total knee arthroplasty. Acta Ortop Bras. 2018;26:309–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Keswani A, Lovy AJ, Robinson J, et al. Risk factors predict increased length of stay and readmission rates in revision joint arthroplasty. J Arthroplasty. 2016;31:603–8. [DOI] [PubMed] [Google Scholar]
- [14].Paxton EW, Inacio MCS, Singh JA, et al. Are there modifiable risk factors for hospital readmission after total hip arthroplasty in a US healthcare system? Clin Orthop Relat Res. 2015;473:3446–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Pugely AJ, Callaghan JJ, Martin CT, et al. Incidence of and risk factors for 30-day readmission following elective primary total joint arthroplasty: analysis from the ACS-NSQIP. J Arthroplasty. 2013;28:1499–504. [DOI] [PubMed] [Google Scholar]
- [16].D’Apuzzo M, Westrich G, Hidaka C, et al. All-Cause versus complication-specific readmission following total knee arthroplasty. J Bone Joint Surg Am. 2017;99:1093–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Herrera-Pérez M, Martín-Vélez P, González-Martín D, et al. Tibiotalocalcaneal nailing for osteoporotic ankle fractures in the frail patient: a narrative review with a clinical score proposal for the decision-making process. EFORT Open Rev. 2022;7:328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Pugely AJ, Martin CT, Gao Y, et al. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013;95:193–9. [DOI] [PubMed] [Google Scholar]
- [19].Tran A, Mai T, El-Haddad J, et al. Preinjury ASA score as an independent predictor of readmission after major traumatic injury. Trauma Surg Acute Care Open. 2017;2:e000128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Jain U, Salgado C, Mioton L, et al. Predictors of readmission after inpatient plastic surgery. Arch Plast Surg. 2014;41:116–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Bartz-Kurycki M, Wei S, Bernardi K, et al. Impact of cardiac risk factors on complications following cranial vault remodeling: analysis of the 2012 to 2016 National Safety Quality Improvement Program-Pediatric Database. J Craniofac Surg. 2019;30:442–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Saucedo JM, Marecek GS, Wanke TR, et al. Understanding readmission after primary total hip and knee arthroplasty: who’s at risk? J Arthroplasty. 2014;29:256–60. [DOI] [PubMed] [Google Scholar]
- [23].Kokkorakis M, Boutari C, Katsiki N, et al. From non-alcoholic fatty liver disease (NAFLD) to steatotic liver disease (SLD): an ongoing journey towards refining the terminology for thi s prevalent metabolic condition and unmet clinical need. Metabolism. 2023;147:155664. [DOI] [PubMed] [Google Scholar]
- [24].Yan T, Yan N, Wang P, et al. Herbal drug discovery for the treatment of nonalcoholic fatty liver disease. Acta Pharm Sin B. 2020;10:3–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Pradhan-Sundd T, Gudapati S, Kaminski TW, et al. Exploring the complex role of coagulation factor VIII in chronic liver disease. Cell Mol Gastroenterol Hepatol. 2021;12:1061–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Iglesias Morcillo M, Freuer D, Peters A, et al. Association between fatty liver index and blood coagulation markers: a population-based study. Lipids Health Dis. 2023;22:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Chen Q, Hao P, Wong C, et al. Development and validation of a novel nomogram of 1-year mortality in the elderly with hip fracture: a study of the MIMIC-III database. BMJ Open. 2023;13:e068465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Jones MR, Petro JA, Novitch MB, et al. Regional catheters for outpatient surgery-a comprehensive review. Curr Pain Headache Rep. 2019;23:24. [DOI] [PubMed] [Google Scholar]
- [29].Khan S, Ali A, Khan S, et al. Current therapies in alleviating liver disorders and cancers with a special focus on the potential of vitamin D. Nutr Metab (Lond). 2018;15:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Deleuran T, Vilstrup H, Overgaard S, et al. Cirrhosis patients have increased risk of complications after hip or knee arthroplasty. Acta Orthop. 2015;86:108–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Fang C, Cornell E, Dicken Q, et al. Coinfection of HIV and hepatitis C increases complication rates after total joint arthroplasty. SICOT J. 2020;6:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Goltz DE, Ryan SP, Howell CB, et al. A weighted index of elixhauser comorbidities for predicting 90-day Readmission after total joint arthroplasty. J Arthroplasty. 2019;34:857–64. [DOI] [PubMed] [Google Scholar]
- [33].Na A, Middleton A, Haas A, et al. Impact of diabetes on 90-day episodes of care after elective total Joint arthroplasty among medicare beneficiaries. J Bone Joint Surg Am. 2020;102:2157–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Dąbrowska D, Jabłońska E, Garley M, et al. The phenomenon of neutrophil extracellular traps in vascular diseases. Arch Immunol Ther Exp (Warsz). 2018;66:273–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Ulusan Z, Karadag AS, Tasar M, et al. Behcet’s disease and cardiovascular involvement: our experience of asymptomatic Behcet’s patients. Cardiovasc J Afr. 2014;25:63–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Vakharia RM, Adams CT, Anoushiravani AA, et al. Chronic obstructive pulmonary disease is associated with higher rates of venous thromboemboli following primary total knee arthroplasty. J Arthroplasty. 2020;35:2066–2071.e9. [DOI] [PubMed] [Google Scholar]
- [37].Wu CT, Chen B, Wang JW, et al. Plasma D-dimer is not useful in the prediction of deep vein thrombosis after total knee arthroplasty in patients using rivaroxaban for thromboprophylaxis. J Orthop Surg Res. 2018;13:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Arant KR, Katz JN, Neogi T. Quantitative sensory testing: identifying pain characteristics in patients with osteoarthritis. Osteoarthritis Cartilage. 2022;30:17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Edwards RR, Campbell C, Schreiber KL, et al. Multimodal prediction of pain and functional outcomes 6 months following total knee replacement: a prospective cohort study. BMC Musculoskelet Disord. 2022;23:302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Brander V, Gondek S, Martin E, et al. Pain and depression influence outcome 5 years after knee replacement surgery. Clin Orthop Relat Res. 2007;464:21–6. [DOI] [PubMed] [Google Scholar]
- [41].Singh JA, Lewallen D. Age, gender, obesity, and depression are associated with patient-related pain and function outcome after revision total hip arthroplasty. Clin Rheumatol. 2009;28:1419–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Wilson JM, Farley KX, Erens GA, et al. Preoperative depression is associated with increased risk following Revision total joint arthroplasty. J Arthroplasty. 2020;35:1048–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Lespasio M, Mont M, Guarino A. Identifying risk factors associated with postoperative infection following elective lower-extremity total joint arthroplasty. Perm J. 2020;24:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Ahn A, Snyder DJ, Keswani A, et al. The cost of poor mental health in total joint arthroplasty. J Arthroplasty. 2020;35:3432–6. [DOI] [PubMed] [Google Scholar]