Abstract
Background
Breast reconstruction is offered to improve quality of life for women after mastectomy for breast cancer, but information regarding the long-term patient-reported outcomes of different reconstruction procedures is currently lacking. The Brighter study aimed to evaluate long-term patient-reported outcomes after immediate breast reconstruction (IBR) in a population-based cohort.
Methods
Women who underwent mastectomy with IBR for breast cancer in England between 1 January 2008 and 31 March 2009 were identified from National Health Service Hospital Episode Statistics. Surviving women were invited to complete the BREAST-Q, EQ-5D-5L™, and ICECAP-A at least 12 years after the index procedure. Questionnaires were scored according to developers’ instructions and compared by IBR type.
Results
Some 1236 women underwent IBR; 343 (27.8 per cent) had 2-stage expander/implant, 630 (51.0 per cent) latissimus dorsi, and 263 (21.3 per cent) abdominal flap reconstructions, with a mean(s.d.) follow-up of 13.3(0.5) years. Women who underwent abdominal flap reconstruction reported higher scores in all BREAST-Q domains than those who had other procedures. These differences remained statistically significant and clinically meaningful after adjusting for age, ethnicity, geographical region, socioeconomic status, smoking, BMI, and complications. The greatest difference was seen in scores for satisfaction with breasts; women who had abdominal flap reconstructions reported scores that were 13.17 (95 per cent c.i. 9.48 to 16.87) points; P < 0.001) higher than those among women who had two-stage expander/implant procedures. Women who underwent latissimus dorsi reconstruction reported significantly more pain/discomfort on the EQ-5D-5L™, but no other differences between procedures were seen.
Conclusion
Long-term patient-reported outcomes are significantly better following abdominal flap reconstruction than other traditional procedure types. These findings should be shared with women considering IBR to help them make informed decisions about their surgical options.
Breast reconstruction is performed to improve quality of life for women with breast cancer, but long-term patient-reported outcome data to support informed decision-making are lacking. This population cohort study of 1236 women who underwent immediate breast reconstruction, with a mean of 13.3 years’ follow-up, showed that patients who had abdominal flap-based reconstruction reported significantly better scores in all BREAST-Q domains than those who had other types of reconstruction. These findings should be shared with women considering breast reconstruction to help them make fully informed decisions about their surgical options.
Introduction
Despite improvements in breast cancer treatment, up to 40 per cent of women undergo a mastectomy1,2. Mastectomy can significantly affect women’s well-being and body image, and breast reconstruction is offered to address this3. Decision-making for breast reconstruction, however, can be challenging. There are many types of reconstruction, and women require detailed, accurate information about the outcomes of different techniques to help them choose. Furthermore, as most women become long-term breast cancer survivors4, information about the long-term outcomes of different procedures, and particularly how these are perceived from the patient perspective, are becoming increasingly important.
Although multiple studies5–8 have compared the short-term patient-reported outcomes (PROs) of implant-based and autologous procedures, and suggested that the outcomes of tissue-based reconstructions may be superior, few studies have undertaken long-term follow up. The studies that have compared long-term PROs are often small or single-centre analyses9–12. Larger North American studies have reported outcomes at 413 and 814 years, but significant proportions of these women had undergone bilateral mastectomy and reconstruction, so the generalizability of these results to other settings is unclear. Furthermore, only the outcomes of implants and abdominal flaps have been compared. Both the UK Association of Breast Surgery15, and the patients and professionals participating in the UK breast cancer surgery James Lind Alliance Research Priority Setting Partnership16 have identified the need for long-term breast reconstruction outcome data as a key research priority.
The aim of the Brighter study was, therefore, to explore the impact of procedure type on the long-term PROs of immediate breast reconstruction (IBR) in a population-based cohort to provide much needed evidence to support informed decision-making for women considering breast reconstruction.
Methods
This population-based cohort study received full ethical approval from the UK Health Research Authority and Confidentiality Advisory Group (CAG) (REC reference 20/SW/0020, CAG reference 20/CAG/0021; IRAS ID 276030). The Brighter protocol provides a full description of the study design and methodology17. This article reports the PROs of the IBR cohort. The clinical outcome and cost analyses18 will be reported elsewhere.
Cohort identification and participant recruitment
Women undergoing unilateral mastectomy for breast cancer or ductal carcinoma in situ between 1 January 2008 and 31 March 2009 with or without breast reconstruction were identified by National Health Service (NHS) Digital and up-to-date contact details for the surviving cohort obtained from the NHS Personal Demographic service following Section 251 approval from the CAG. This cohort was selected to include all women who would have been included in the UK National Mastectomy and Breast Reconstruction Audit (NMBRA) for comparative purposes17,19.
Women aged less than 90 years, living independently (not nursing or care home residents) without evidence of cognitive impairment, defined as having codes for dementia in their Hospital Episode Statistics data record, were contacted and invited to complete validated PRO questionnaires either by post or online via a secure REDCap20 link according to participant preference. A second invitation letter was sent approximately 6 weeks after the first to optimize study participation. If no response was received after the second invitation, women were considered to have declined participation in the PRO study.
Receipt of IBR and type of reconstruction performed were determined by patient self-report. Only women who reported undergoing the three most commonly performed procedures—two-stage subpectoral expander/implant only reconstruction (without the use of mesh), latissimus dorsi (LD) flap with or without an implant, and abdominal flap reconstruction—were included in the analysis. This is because preliminary work suggested that other types of reconstruction were carried out infrequently, and small numbers of these reconstructions would preclude meaningful comparisons between procedure types.
Questionnaires
Participants were asked to complete three validated questionnaires: BREAST-Q, ED-5D-5L™ (EuroQol Group, Rotterdam, the Netherlands), and ICEpop CAPability measure for Adults (ICECAP-A), together with a study-specific questionnaire including participant demographics and details of surgery and treatments received. Respondents were also asked to complete a single item assessment of overall satisfaction with the outcomes of surgery on a five-point Likert scale (excellent, very good, good, fair, poor), consistent with the assessment made as part of the NMBRA21.
BREAST-Q
The BREAST-Q is a validated questionnaire that has been developed robustly for use in patients undergoing breast reconstruction surgery22,23. It consists of four main scales: satisfaction with breasts, physical well-being (chest), sexual well-being, and psychosocial well-being. Each scale is Rasch-transformed to give a score out of 100, with higher scores reflecting better outcomes. The minimum clinically important difference in BREAST-Q scores has recently been defined as being 4 points for the satisfaction with breast, psychosocial and sexual well-being domains, and 3 points for the physical well-being domain24.
ED-5D-5L™
The EQ-5D-5L™25 is a generic measure of health-related quality of life consisting of a descriptive system with five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The scores on the five dimensions can be presented as a health profile, or can be converted to a single index reflecting a preference-based quality-of-life score (utility) anchored at 1 (best health) and 0 (death) using a UK National Institute for Health and Care Excellence-recommended value set26. It also includes the EQ VAS, a vertical visual analogue scale on which patients self-report their health on a scale from ‘the best health you can imagine’ to ‘the worst health you can imagine’. The EQ-5D-5L™ has been used in previous breast reconstruction studies27,28.
ICECAP-A
ICECAP-A29 is a measure of well-being defined in a broader sense than health and covers five attributes: attachment, stability, achievement, enjoyment, and autonomy. A set of UK index values for ICECAP-A has been estimated using best–worst scaling30. It was hypothesized that ICECAP-A may be more sensitive to breast reconstruction-related concerns than the EQ-5D-5L™ and so it was used as an exploratory measure in this study.
Statistical analysis
Demographic characteristics are summarized as counts with percentages for categorical variables, and mean(s.d.) for continuous variables. These were compared in the responder and non-responder groups, and by the type of reconstruction received, using ANOVA and χ2 test for continuous and categorical variables respectively.
All questionnaires were scored according to the developers’ instructions, and scores for each of the main BREAST-Q scales, ICECAP-A score, individual EQ-5D-5L™ dimensions, utility, and the EQ VAS were compared by type of reconstruction performed. Multivariable linear regression was used to adjust for factors hypothesized from the literature13,31–33 to influence BREAST-Q scores, including age at mastectomy, ethnicity, socioeconomic deprivation assessed using Indices of Multiple Deprivation, geographical region of residence, smoking status, marital status, BMI at the time of mastectomy, surgical complications, and receipt of further surgery.
The single item concerning overall satisfaction with the outcome of surgery was dichotomized into ‘excellent, very good’ versus ‘good, fair, poor’ and compared across procedure types using χ2 statistics.
Results
Of 11 977 women invited to participate in the study, 4207 (35.7 per cent) completed the PRO questionnaires. Of these, 1236 (29.4 per cent) reported undergoing IBR with 1 of the 3 procedures of interest. This included 343 2-stage expander/implant reconstructions (27.8 per cent), 630 LD flap procedures (51.0 per cent), and 263 abdominal flap reconstructions (21.3 per cent). Responders were more likely to be older, white, and from the higher socioeconomic groups than non-responders (Table S1).
Demographic characteristics of the IBR cohort are summarized in Table 1. There were no differences between surgical groups with regard to age at the time of index mastectomy, socioeconomic or marital status, ethnicity or the receipt of further surgery (Table 1). Women who had an abdominal flap reconstruction had slightly higher BMIs, but were significantly less likely to have smoked at the time of reconstruction, than women who had expander/implant or LD flap reconstructions. There were also significant differences between the groups in postoperative complications; women who had two-stage expander/implant reconstruction more likely to have experienced complications requiring further surgery than those who underwent other types of reconstruction (93 women (27.9 per cent) in expander/implant group, 111 (18.2 per cent) in LD flap group, and 25 (9.8 per cent) in abdominal flap group; P < 0.001) (Table 1). Mean(s.d.) follow-up for the cohort was 13.3(0.5) years.
Table 1.
Respondent demographics by reconstruction type
| Expander/implant (n = 343) | LD flap (n = 630) |
Abdominal flap (n = 263) |
All patients (n = 1236) |
P* | |
|---|---|---|---|---|---|
| Age at index mastectomy (years), mean (s.d.) | 52.10 (9.47) | 51.20 (9.14) | 50.58 (7.73) | 51.32 (8.96) | 0.105† |
| Ethnicity | 0.568 | ||||
| White | 328 (97.9) | 606 (97.4) | 249 (96.5) | 1183 (97.4) | |
| Other | 7 (2.1) | 16 (2.6) | 9 (3.5) | 32 (2.6) | |
| Region | < 0.001 | ||||
| East Midlands | 31 (9.0) | 61 (9.7) | 22 (8.4) | 114 (9.2) | |
| East of England | 37 (10.4) | 73 (11.6) | 82 (31.2) | 192 (15.5) | |
| London | 45 (13.1) | 56 (8.9) | 30 (11.4) | 131 (10.6) | |
| North East | 13 (13.8) | 20 (3.2) | 7 (2.7) | 40 (3.2) | |
| North West | 41 (12.0) | 84 (13.3) | 20 (7.6) | 145 (11.7) | |
| South East | 61 (17.8) | 110 (17.5) | 40 (15.2) | 211 (17.1) | |
| South West | 44 (12.8) | 80 (12.7) | 23 (8.8) | 147 (11.9) | |
| West Midlands | 26 (7.6) | 56 (8.9) | 21 (8.0) | 103 (8.3) | |
| Yorkshire and Humber | 34 (9.9) | 83 (13.2) | 16 (6.1) | 133 (10.8) | |
| Other | 11 (3.2) | 7 (1.1) | 2 (0.8) | 20 (1.6) | |
| Indices of Multiple Deprivation | 0.729 | ||||
| 1 (most deprived) | 25 (7.6) | 56 (9.0) | 21 (8.1) | 102 (8.4) | |
| 2 | 61 (18.4) | 85 (13.7) | 43 (16.5) | 189 (15.6) | |
| 3 | 69 (20.9) | 141 (22.7) | 51 (19.5) | 261 (21.5) | |
| 4 | 85 (25.7) | 157 (25.2) | 69 (26.4) | 311 (25.6) | |
| 5 (least deprived) | 91 (27.5) | 183 (29.4) | 77 (29.5) | 351 (28.9) | |
| Smoking status | 0.010 | ||||
| Yes | 44 (13.0) | 80 (12.9) | 17 (6.6) | 141 (11.6) | |
| No | 292 (86.1) | 537 (86.5) | 235 (90.7) | 1064 (87.3) | |
| Prefer not to say | 3 (0.9) | 4 (0.6) | 7 (2.7) | 14 (1.2) | |
| BMI (kg/m2), mean (s.d.) | 24.14 (4.30) | 24.33 (3.59) | 25.80 (3.96) | 24.59 (3.93) | < 0.001† |
| Marital status | 0.062 | ||||
| Single | 39 (11.7) | 57 (9.3) | 15 (5.9) | 111 (9.3) | |
| Married | 209 (62.3) | 411 (67.2) | 173 (68.4) | 793 (66.1) | |
| Divorced or separated | 44 (13.2) | 72 (11.8) | 38 (15.0) | 154 (12.8) | |
| In a relationship | 35 (10.5) | 69 (11.3) | 26 (10.3) | 130 (10.8) | |
| Prefer not to say | 7 (2.1) | 3 (0.5) | 1 (0.4) | 11 (0.9) | |
| Complications resulting from surgery | < 0.001 | ||||
| Yes, managed in clinic or by GP | 43 (12.9) | 139 (22.8) | 63 (24.7) | 245 (20.5) | |
| Yes, I needed further surgery | 93 (27.9) | 111 (18.2) | 25 (9.8) | 229 (19.1) | |
| No | 197 (59.2) | 358 (59.0) | 167 (65.5) | 723 (60.4) | |
| Further surgery | 0.504 | ||||
| Yes | 233 (67.9) | 418 (66.4) | 185 (70.3) | 836 (67.6) | |
| No | 110 (32.1) | 212 (33.7) | 78 (29.7) | 400 (32.4) |
Values are n (%) unless otherwise indicated. LD, latissimus dorsi; GP, general practitioner. *χ2 test, except †ANOVA.
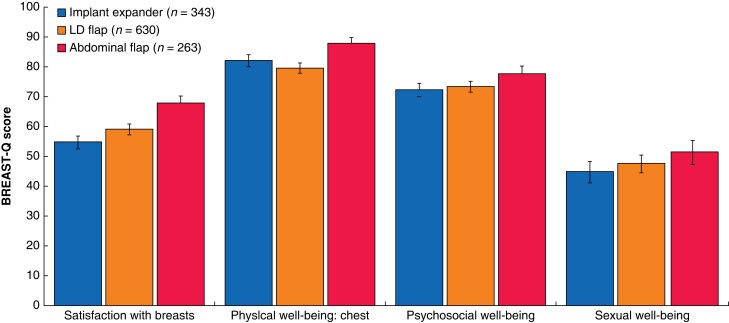
BREAST-Q and overall satisfaction with outcome
Women who received an abdominal flap reconstruction reported higher unadjusted mean scores across all BREAST-Q domains than those having other breast reconstruction procedures (Table 2 and Fig. 1). These differences in satisfaction with breasts (13.17 (95 per cent c.i. 9.48 to 16.87) points; P < 0.001), psychosocial well-being (5.41 (1.80 to 9.01) points; P = 0.003), physical well-being (5.65 (2.22 to 9.09) points; P = 0.001), and sexual well-being (6.79 (1.69 to 11.90) points; P = 0.009) remained statistically significant, and the means exceeded the established minimum clinically important difference for each domain24 after adjusting for potential confounders (Table 3). In the multivariable analysis, higher scores in all BREAST-Q domains were also strongly associated with older age at the initial reconstruction (aged 60 or over versus under 50 years), whereas lower scores in all domains were strongly associated with smoking at the time of reconstruction and experiencing postoperative complications (Table 3). Higher psychosocial well-being scores were strongly associated with higher socioeconomic status, whereas non-white ethnicity and higher BMI were strongly associated with lower physical well-being scores. The impact of marital status at the time of reconstruction was complex (Table 3).
Table 2.
Unadjusted BREAST-Q scores by reconstruction type
| Satisfaction with breasts (n = 1084) | Psychosocial well-being (n = 1177) | Physical well-being (n = 1055) | Sexual well-being* (n = 800) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean score | P† | n | Mean score | P† | n | Mean score | P† | n | Mean score | P† | |
| Implant/expander | 293 | 54.7 (52.4, 56.9) |
< 0.001 | 328 | 72.2 (70.0, 74.5) |
0.006 | 296 | 82.1 (80.0, 84.1) |
< 0.001 | 225 | 44.7 (41.4, 47.9) |
0.013 |
| LD flap | 555 | 59.0 (57.2, 60.7) |
597 | 73.3 (71.5, 75.0) |
532 | 79.5 (77.8, 81.3) |
390 | 47.4 (44.8, 50.0) |
||||
| Abdominal flap | 236 | 67.6 (65.0, 70.3) |
252 | 77.6 (74.9, 80.2) |
227 | 87.8 (85.6, 89.8) |
185 | 51.2 (47.7, 54.8) |
||||
Values in parentheses are 95% confidence intervals. *The sexual well-being scale was an optional part of the questionnaire and a proportion of respondents elected not to complete this section. LD, latissimus dorsi. †ANOVA.
Fig. 1.
Unadjusted BREAST-Q score by procedure type
Values are mean with 95% confidence interval.
Table 3.
Multivariable regression of BREAST-Q scores
| Satisfaction with breasts (n = 1009) | Psychosocial well-being (n = 1103) | Physical well-being (chest) (n = 990) | Sexual well-being (n = 760) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficicnt (95% c.i.) | P* | P† | Coefficicnt (95% c.i.) | P* | P† | Coefficicnt (95% c.i.) | P* | P† | Coefficicnt (95% c.i.) | P* | P† | |
| Procedure | ||||||||||||
| Expander/implant (reference) | ||||||||||||
| LD flap | 4.86 (1.92, 7.81) | 0.001 | < 0.001 | 1.60 (−1.26, 4.45) | 0.273 | 0.011 | −2.02 (−4.73, 0.68) | 0.143 | < 0.001 | 3.27 (−0.84, 7.37) | 0.119 | 0.029 |
| Abdominal flap | 13.17 (9.48, 16.87) | < 0.001 | 5.41 (1.80, 9.01) | 0.003 | 5.65 (2.22, 9.09) | 0.001 | 6.79 (1.69, 11.90) | 0.009 | ||||
| Age (years) | ||||||||||||
| < 50 (reference) | ||||||||||||
| 50–59 | 2.81 (0.06, 5.56) | 0.045 | 0.002 | 6.15 (3.46, 8.85) | < 0.001 | < 0.001 | 3.51 (0.95, 6.06) | 0.007 | 0.001 | 3.64 (−0.12, 7.40) | 0.058 | 0.002 |
| ≥ 60 | 6.39 (2.76, 10.02) | 0.001 | 11.30 (7.85, 14.75) | < 0.001 | 5.82 (2.52, 9.11) | 0.001 | 9.37 (3.82, 14.91) | 0.001 | ||||
| Ethnicity | ||||||||||||
| White (reference) | ||||||||||||
| Other | 4.36 (−4.39, 13.12) | 0.328 | 0.328 | −1.40 (−9.42, 6.61) | 0.731 | 0.728 | −11.92 (−19.29, −4.55) | 0.002 | 0.002 | 5.95 (−7.38, 19.28) | 0.381 | 0.381 |
| Region | ||||||||||||
| London (reference) | ||||||||||||
| North East | 1.63 (−6.15, 9.41) | 0.681 | −0.37 (−8.01, 7.28) | 0.925 | −5.24 (−12.63, 2.16) | 0.165 | −5.89 (−16.97, 5.20) | 0.298 | ||||
| North West | 0.69 (−4.62, 5.99) | 0.799 | −1.96 (−7.14, 3.22) | 0.458 | −1.81 (−6.74, 3.12) | 0.471 | −2.24 (−9.60, 5.12) | 0.551 | ||||
| Yorkshire and Humber | 0.10 (−5.33, 5.53) | 0.971 | 0.09 (−5.37, 5.18) | 0.973 | −2.71 (−7.85, 2.42) | 0.300 | −1.76 (−9.29, 5.77) | 0.647 | ||||
| East Midlands | 1.72 (−3.92, 7.35) | 0.550 | 0.984 | 0.77 (−4.72, 6.27) | 0.782 | 0.951 | −2.59 (−7.77, 2.58) | 0.326 | 0.741 | 0.32 (−7.60, 8.23) | 0.937 | 0.925 |
| West Midlands | −0.22 (−5.97, 5.53) | 0.940 | −2.34 (−7.93, 3.24) | 0.410 | −3.72 (−9.05, 1.60) | 0.170 | −1.04 (−8.87, 6.79) | 0.794 | ||||
| East of England | −1.42 (−6.46, 3.62) | 0.580 | 0.17 (−4.72, 5.06) | 0.945 | −1.74 (−6.40, 2.93) | 0.466 | −2.31 (−9.38, 4.77) | 0.523 | ||||
| South East | −0.25 (−4.68, 5.19) | 0.920 | 0.53 (−4.24, 5.31) | 0.827 | −0.88 (−5.38, 3.62) | 0.702 | −3.82 (−10.61, 2.97) | 0.270 | ||||
| South West | 1.54 (−3.79, 6.86) | 0.571 | 1.34 (−3.81, 6.49) | 0.610 | 0.63 (−4.27, 5.54) | 0.800 | −2.77 (−10.19, 4.66) | 0.464 | ||||
| Other | −0.09 (−10.66, 10.48) | 0.987 | 0.72 (−9.43, 10.86) | 0.890 | −3.24 (−12.65, 6.18) | 0.500 | −8.44 (−22.65, 5.78) | 0.244 | ||||
| IMD | ||||||||||||
| Most deprived quintile (reference) | ||||||||||||
| Least deprived four quintiles | 1.08 (−3.65, 5.80) | 0.654 | 0.654 | 6.31 (0.007) | 0.007 | 1.71, 10.91 | −0.70 (−5.09, 3.69) | 0.753 | 0.753 | 5.22 (−1.24, 11.67) | 0.113 | 0.113 |
| Smoker | ||||||||||||
| No (reference) | ||||||||||||
| Yes | −6.51 (−10.49, −2.54) | 0.001 | 0.005 | −7.88 (−11.75, −4.02) | 0.000 | < 0.001 | −6.78 (−10.48, −3.08) | 0.000 | 0.001 | −9.34 (−14.72, −3.96) | 0.001 | 0.001 |
| Prefer not to say | −0.52 (−12.00, 10.96) | 0.929 | −11.21 (−22.86, 0.43) | 0.059 | 2.65 (−8.33, 13.64) | 0.636 | −13.85 (−29.18, 1.47) | 0.076 | ||||
| BMI (kg/m2) | ||||||||||||
| ≤ 30 (reference) | ||||||||||||
| > 30 | −0.78 (−3.86, 2.30) | 0.619 | 0.619 | −2.48 (−5.43, 0.48) | 0.100 | 0.096 | −3.39 (−6.28, −0.50) | 0.022 | 0.022 | −3.81 (−8.21, 0.59) | 0.090 | 0.090 |
| Marital status | ||||||||||||
| Married (reference) | ||||||||||||
| Single | −8.06 (−12.52, −3.61) | 0.000 | −6.86 (−11.06, −2.65) | 0.001 | −2.81 (−6.85, 1.23) | 0.172 | −17.34 (−23.96, −10.71) | 0.000 | ||||
| Divorced or separated | −0.96 (−4.74, 2.82) | 0.617 | 0.002 | −3.94 (−7.60, −0.28) | 0.035 | < 0.001 | −1.33 (−4.84, 2.17) | 0.455 | 0.602 | −14.11 (−19.73, −8.48) | 0.000 | < 0.001 |
| In a relationship | −4.20 (−8.29, −0.10) | 0.045 | −4.62 (−8.63, −0.61) | 0.024 | 0.02 (−3.84, 3.88) | 0.992 | −4.32 (−9.58, 0.95) | 0.108 | ||||
| Prefer not to say | 7.59 (−6.41, 21.60) | 0.288 | 14.79 (−0.45, 30.02) | 0.057 | 3.74 (−9.05, 16.54) | 0.566 | 18.89 (−2.50, 40.27) | 0.083 | ||||
| Complications after surgery | ||||||||||||
| No (reference) | ||||||||||||
| Yes, managed in clinic or by GP | −5.73 (−8.89, −2.58) | < 0.001 | < 0.001 | −3.16 (−6.26, −0.06) | 0.046 | < 0.001 | −6.02 (−8.97, −3.08) | < 0.001 | < 0.001 | −2.63 (−7.02, 1.76) | 0.240 | 0.110 |
| Yes, I needed further surgery | −8.50 (−11.94, −5.06) | < 0.001 | −6.89 (−10.15, −3.63) | < 0.001 | −6.58 (−9.69, −3.47) | < 0.001 | −4.53 (−9.08, 0.31) | 0.052 | ||||
| Further surgery to breasts | ||||||||||||
| Yes (reference) | ||||||||||||
| No | −0.08 (−2.83, 2.67) | 0.955 | 0.955 | 2.39 (−0.27, 5.05) | 0.078 | 0.074 | 3.51 (1.01, 6.02) | 0.006 | 0.006 | 3.52 (−0.38, 7.43) | 0.077 | 0.072 |
LD, latissiumus dorsi; IMD, Indices of multiple deprivation. *P for coefficients of co-variable within each category; †P for likelihood ratio test of impact of co-variable on regression model.
Considering overall satisfaction with the outcome of the reconstruction, almost three-quarters of women who underwent abdominal flap reconstruction (187 of 254, 73.6 (95 per cent c.i. 67.8 to 78.9) per cent) considered their outcome to be excellent or very good compared with just over half of those who had two-stage expander/implant procedures (175 of 330, 53.0 (47.5 to 58.5) per cent) (P < 0.001) (Table 4).
Table 4.
Overall satisfaction with outcome of surgery by immediate breast reconstruction type
| Implant expander (n = 330) |
LD flap (n = 615) |
Abdominal flap (n = 254) |
P* | |
|---|---|---|---|---|
| Good, fair, poor | 155 (47.0) | 226 (36.8) | 67 (26.4) | < 0.001 |
| Excellent, very good | 175 (53.0) | 389 (63.3) | 187 (73.6) |
Values are n (%). LD, latissimus dorsi. *χ2 test.
EQ-5D-5L™ and ICECAP-A
There were no differences in EQ-5D-5L™ VAS or overall utility scores, irrespective of the type of procedure performed (Tables S2 and S3). Comparison of individual EQ-5D-5L™ dimension scores across procedure types, however, showed that women who underwent LD reconstructions reported significantly more moderate or severe pain/discomfort than those who had other types of reconstruction (129 of 605 (21.3 per cent) versus 49 of 328 (14.9 per cent) for expander/implant and 39 of 251 (15.5 per cent) for abdominal flap reconstructions; P = 0.008) (Table 5). There were no differences in other dimensions of the EQ-5D-5L™, and ICECAP-A scores were similar across all procedure groups (Table S4).
Table 5.
EQ-5D-5L™ dimension scores by reconstruction type
| Implant expander (n = 343) |
LD flap (n = 630) |
Abdominal flap (n = 263) |
P* | |
|---|---|---|---|---|
| Mobility | ||||
| No problems | 265 (80.6) | 450 (74.1) | 193 (76.9) | 0.184 |
| Slight problems | 28 (8.5) | 93 (15.3) | 36 (14.3) | |
| Moderate problems | 21 (6.4) | 42 (6.9) | 14 (5.6) | |
| Severe problems | 15 (4.6) | 21 (3.5) | 8 (3.2) | |
| Unable to walk about | 0 (0) | 1 (0.2) | 0 (0) | |
| Total | 329 (100) | 607 (100) | 251 (100) | |
| Self-care | ||||
| No problems | 304 (92.7) | 559 (92.2) | 235 (94.0) | 0.723 |
| Slight problems | 16 (4.9) | 27 (4.5) | 6 (2.4) | |
| Moderate problems | 7 (2.1) | 17 (2.8) | 9 (3.6) | |
| Severe problems | 1 (0.3) | 2 (0.3) | 0 (0) | |
| Unable to wash/dress | 0 (0) | 1 (0.2) | 0 (0) | |
| Total | 328 (100) | 606 (100) | 250 (100) | |
| Usual activities | ||||
| No problems | 232 (70.5) | 421 (69.5) | 181 (72.4) | 0.874 |
| Slight problems | 61 (18.5) | 120 (19.8) | 46 (18.4) | |
| Moderate problems | 24 (7.3) | 49 (8.1) | 15 (6.0) | |
| Severe problems | 10 (3.0) | 14 (2.3) | 8 (3.2) | |
| Unable to do | 2 (0.6) | 2 (0.3) | 0 (0) | |
| Total | 329 (100) | 606 (100) | 250 (100) | |
| Pain/discomfort | ||||
| None | 145 (44.2) | 237 (39.2) | 133 (53.0) | 0.008 |
| Slight | 134 (40.9) | 239 (39.5) | 79 (31.5) | |
| Moderate | 32 (9.8) | 96 (15.9) | 24 (9.6) | |
| Severe | 13 (4.0) | 26 (4.3) | 12 (4.8) | |
| Extreme | 4 (1.2) | 7 (1.2) | 3 (1.2) | |
| Total | 328 (100.0) | 605 (100) | 251 (100) | |
| Anxiety/depression | ||||
| None | 193 (58.7) | 353 (58.4) | 145 (57.8) | 0.897 |
| Slight | 99 (30.1) | 169 (27.9) | 75 (29.9) | |
| Moderate | 31 (9.4) | 61 (10.1) | 22 (8.8) | |
| Severe | 5 (1.5) | 18 (3.0) | 8 (3.2) | |
| Extreme | 1 (0.3) | 4 (0.7) | 1 (0.4) | |
| Total | 329 (100) | 605 (100) | 251 (100) |
Values are n (%). LD, latissimus dorsi. *χ2 test.
Discussion
This large population-based cohort study evaluated long-term PROs at a mean of 13.3 years after IBR, and compared outcomes following the three procedures most commonly performed at that time. It demonstrated that women who had abdominal flap reconstruction reported higher long-term levels of satisfaction with breasts, and physical, psychosocial, and sexual well-being than those who underwent other types of reconstruction. Women who had LD flap reconstruction reported greater satisfaction with breasts than those who had two-stage subpectoral expander/implant reconstruction, but there were no other differences between the groups. Women who received a traditional two-stage expander/implant reconstruction reported the lowest scores across all BREAST-Q scales 13 years after surgery. This important and novel information highlights how different IBR procedures continue to affect the well-being of women treated for breast cancer many years after surgery and for a significant amount of their remaining 22–28-year life expectancy34. As such, it should be shared routinely with women considering surgery to allow them to make fully informed decisions about reconstructive options.
These findings are consistent with those of other shorter studies13,14 suggesting that the PROs of abdominal flap reconstruction are superior to those after implant-based procedures. A large single-centre North American cohort study14 of 3268 women suggested that adjusted scores for satisfaction with breasts were 16.77 and 22.02 points higher at 5 and 7 years after surgery after abdominal flap reconstruction compared with implant-based procedures. These differences are much higher than the 13-point difference at 13 years in the present study. Notably, almost two-thirds of patients in the North American cohort had bilateral surgery, which may partially explain these findings. Furthermore, these women all had surgery at a single large specialist centre, so the extent to which the results are generalizable is unclear and the outcomes of LD flap reconstruction were not assessed. This present population-based cohort included women who had the three most commonly performed IBR procedures in England. It should, therefore, be more representative of long-term outcomes of IBR in a wider group of patients.
Similar findings were noted in a small cross-sectional North American study35 that evaluated aesthetic satisfaction with breast reconstruction over time in 219 women, with a median follow-up of 6.5 years. In that study, although women who had implant-based procedures were initially more satisfied with the outcome of the reconstruction, satisfaction decreased markedly over time, whereas women who underwent autologous reconstruction became more satisfied with the results. Approximately 40 per cent of women who had implant-based procedures reported being satisfied with the cosmetic outcome of the reconstruction at 10 years, compared with approximately 75 per cent of those who underwent autologous procedures35. These findings are consistent with those at 13 years reported here.
The reason for the superiority of autologous procedures is likely to be that tissue-based reconstructions behave more like a natural breast, developing ptosis over time and changing with the weight of the patient. By contrast, for women with unilateral implant-based reconstruction, asymmetry will become more marked over time and complications such as capsular contracture are more likely to develop, requiring further interventions to maintain acceptable cosmetic results.
Despite the marked differences between procedure types highlighted with the BREAST-Q, there were no differences between the surgical groups in overall scores for either the generic measures of health (EQ-5D-5L™) or well-being (ICECAP-A). The lack of discriminatory value has previously been reported for the EQ-5D-5L™27,28, but this is a novel and unanticipated finding for the well-being measure. These results are likely to reflect the brevity of both generic measures as they do not include aspects of outcome, such as satisfaction with breast appearance, that differ between procedure types and are important to women. In addition, both measures compress all aspects of health/well-being into a single scale anchored at 0 and 1. This means that small but potentially important differences are not evident, even in large sample sizes. When individual dimensions of the EQ-5D-5L™ were compared, however, differences were seen in the levels of pain/discomfort reported in the LD group. This was notable, and suggests that chronic pain may be a more significant long-term issue for these women than previously reported36.
This work has several limitations that require consideration. First, even though every attempt was made to optimize engagement and response rates, including co-developing study materials with patients, only 1236 women participated in the study. Although it is not possible to determine response rates precisely owing to UK legislation mandating that participants are given the opportunity to opt out of having their routinely collected healthcare data used in research, based on the numbers of women who had IBR registered in the UK 2007–2008 NMBRA19,37 and allowing for a 20–25 per cent mortality rate at 12 years4, it could be estimated that response rates in this study were between 40 and 50 per cent. This is lower than ideal, but reasonable given that invitations to participate were sent 12–13 years after the initial surgery. Women who completed the questionnaires, however, were older, more affluent, and more likely to be white than non-responders. This response bias has been reported in other breast reconstruction studies38, and may mean that the views reported here may not be representative of the breast reconstruction community more generally.
Previous PRO data for this cohort were not available, meaning that it is not possible to make any definitive comments regarding how outcomes have changed over time. The initial aim of the study was to link these data to the original NMBRA cohort17 that included 18-month PROs, but changes in UK data protection legislation meant that the NMBRA data were no longer available for linkage. Without NMBRA data, patient self-report of IBR and the type of procedure received was used as the basis for this study. This introduces the possibility of recall bias as women may not accurately remember details of procedures and events that occurred over 12 years previously. Although this is possible, breast cancer and breast reconstruction are highly salient events in any woman’s life. This would make significant issues with recall bias unlikely.
Patient satisfaction and health-related quality of life are complex constructs that are likely to be influenced by multiple factors. Although attempts were made to control for several potential confounders, it is acknowledged that other factors may have been important. Specifically, the impact of cancer stage and adjuvant treatments could not be assessed as it was not possible to obtain linked oncological or treatment data.
Finally, it could be argued that this study evaluated the outcomes of historical procedures that do not reflect current practice. This is particularly relevant to women in the implant-based group, all of whom would have received two-stage subpectoral expander/implant reconstructions without the use of mesh, which is no longer the standard of care in the UK39. Indeed, the practice of implant-based reconstruction has evolved significantly over the past 12–13 years with the introduction of mesh-assisted subpectoral39 and, more recently, pre-pectoral40 techniques, aimed at improving patient-reported and cosmetic outcomes of implant-based procedures41. Evidence to support the benefits of mesh-assisted reconstruction, however, remains limited, and BREAST-Q scores at 18 months after one- and two-stage prosthetic procedures were shown to be broadly comparable in a large prospective cohort study42, irrespective of whether mesh was used. Long-term outcome data for these techniques are also currently lacking. A recent small retrospective study43, with a median of 62 months follow-up, suggested that women who had mesh-assisted reconstruction were significantly more satisfied with the outcomes of reconstruction (BREAST-Q scores 62 versus 55) than those who had reconstruction using standard two-stage submuscular techniques. It should be noted, however, that the study was very small and there was a high proportion of bilateral procedures in the mesh-assisted group. Further evolution of the technique has resulted prepectoral mesh-assisted implant reconstruction becoming the new standard of care in the UK. Again, although short-term outcomes of prepectoral and subpectoral mesh-assisted reconstructions appear to be broadly comparable44, work is needed to evaluate long-term PROs prospectively in this group. Despite these limitations, particularly with regard to the applicability of the findings to modern implant-based techniques, the present study has generated much needed information regarding the long-term PROs of IBR, and how they vary by procedure performed, to support informed decision-making.
Several decision aids have been developed to help women make decisions about breast reconstruction surgery45 including, most recently, BRECONDA46 and PEGASUS47. These, in particular, BRECONDA, have been shown to improve satisfaction with information and reduce decisional conflict in well designed clinical trials46. Neither of these tools, however, include long-term outcomes, which may influence patient decision-making. Integration of information about the need for further surgery over time and how different types of reconstruction are perceived in the longer term from a patient perspective may therefore add to their value. Determining how best to communicate and share this complex information with patients, however, is challenging and further qualitative work with patients and key stakeholders is needed to determine how best to use these findings to support informed decision-making.
The present study has added significantly to the evidence regarding long-term breast reconstruction outcomes, but well designed, large-scale prospective longitudinal studies are still needed in this area. Such studies are time-consuming and expensive, so pragmatic registry-based approaches, including routine PRO assessment and linkage to routinely collected clinical outcome data, is essential. In the UK, the Flap Registry48 already collects PROs at 12 months, but further work is needed to extend the PRO timeline and consider how the PROs of implant reconstruction could also be assessed. Breast reconstruction is performed to improve quality of life after mastectomy, so it is vital that this information is collected moving forward to support women in making fully informed decisions about reconstruction options.
Supplementary Material
Acknowledgements
The authors thank all the patients who participated in the Brighter study.
Contributor Information
Leigh Johnson, Translational Health Sciences, Bristol Medical School, Bristol, UK.
Paul White, Applied Statistics Group, University of the West of England, Bristol, UK.
Ranjeet Jeevan, Department of Plastic Surgery, Manchester University NHS Foundation Trust, Manchester, UK.
John Browne, School of Public Health, University College Cork, Cork, Ireland.
Carmel Gulliver-Clarke, Department of Breast Surgery, Western Sussex Hospitals NHS Foundation Trust, Worthing, UK.
Joe O’Donoghue, Department of Plastic Surgery, Royal Victoria Infirmary, Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK.
Syed Mohiuddin, Translational Health Sciences, Bristol Medical School, Bristol, UK.
William Hollingworth, Translational Health Sciences, Bristol Medical School, Bristol, UK.
Patricia Fairbrother, Independent Cancer Patients Voice (ICPV), UK.
Mairead MacKenzie, Independent Cancer Patients Voice (ICPV), UK.
Chris Holcombe, Linda McCartney Centre, Royal Liverpool and Broadgreen University Hospital, Liverpool, UK.
Shelley Potter, Translational Health Sciences, Bristol Medical School, Bristol, UK; Bristol Breast Care Centre, Southmead Hospital, Bristol, UK.
Funding
This work was funded by a National Institute for Health Research (NIHR) Research for Patient Benefit Programme Grant (PB-PG-0817-20020), and supported by the NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol and the NIHR Applied Research Collaboration West. S.P. is an NIHR Clinician Scientist (CS-2016-16-019). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author contributions
Leigh Johnson (Data curation, Formal analysis, Methodology, Project administration, Writing—review & editing), Paul White (Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Writing—review & editing), Ranjeet Jeevan (Funding acquisition, Methodology, Writing—review & editing), John Browne (Formal analysis, Funding acquisition, Methodology, Writing—review & editing), Carmel Gulliver-Clarke (Funding acquisition, Methodology, Writing—review & editing), Joe O’Donoghue (Conceptualization, Funding acquisition, Methodology, Writing—review & editing), Syed Mohiuddin (Formal analysis, Funding acquisition, Methodology, Writing—review & editing), William Hollingworth (Formal analysis, Funding acquisition, Methodology, Supervision, Writing—review & editing), Patricia Fairbrother (CRediT contribution not specified), Mairead MacKenzie (Formal analysis, Funding acquisition, Methodology, Writing—review & editing), Chris Holcombe (Formal analysis, Funding acquisition, Methodology, Writing—review & editing), and Shelley Potter (Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing—original draft).
Disclosure
The authors declare no conflict of interest.
Data availability
Data will be made available on reasonable request from the corresponding author.
Supplementary material
Supplementary material is available at BJS online.
References
- 1. Rubenstein RN, Stern CS, Plotsker EL, Haglich K, Tadros AB, Mehrara BJet al. Effects of COVID-19 on mastectomy and breast reconstruction rates: a national surgical sample. J Surg Oncol 2022;126:205–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. MacNeill F, Irvine T. Breast Surgery. GIRFT Programme National Speciality Report. 2021. https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/02/BreastSurgeryReport-Mar21o-EMBARGOED.pdf (accessed 3 March 2023) [Google Scholar]
- 3. Harcourt D, Rumsey N. Psychological aspects of breast reconstruction: a review of the literature. J Adv Nurs 2001;35:477–487 [DOI] [PubMed] [Google Scholar]
- 4. Cancer Research UK . Breast Cancer Statistics.https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer (accessed 3 March 2023)
- 5. Eltahir Y, Krabbe-Timmerman IS, Sadok N, Werker PMN, de Bock GH. Outcome of quality of life for women undergoing autologous versus alloplastic breast reconstruction following mastectomy: a systematic review and meta-analysis. Plast Reconstr Surg 2020;145:1109–1123 [DOI] [PubMed] [Google Scholar]
- 6. Toyserkani NM, Jørgensen MG, Tabatabaeifar S, Damsgaard T, Sørensen JA. Autologous versus implant-based breast reconstruction: a systematic review and meta-analysis of Breast-Q patient-reported outcomes. J Plast Reconstr Aesthet Surg 2020;73:278–285 [DOI] [PubMed] [Google Scholar]
- 7. Char S, Bloom JA, Erlichman Z, Jonczyk MM, Chatterjee A. A comprehensive literature review of patient-reported outcome measures (PROMs) among common breast reconstruction options: what types of breast reconstruction score well? Breast J 2021;27:322–329 [DOI] [PubMed] [Google Scholar]
- 8. Khajuria A, Prokopenko M, Greenfield M, Smith O, Pusic AL, Mosahebi A. A meta-analysis of clinical, patient-reported outcomes and cost of DIEP versus implant-based breast reconstruction. Plastic Reconstr Surg Glob Open 2019;7:e2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fontein DBY, Oros M, Held L, Giovanoli P, Pusic AL, Lindenblatt N. Patient-reported outcomes in free-flap breast reconstructive surgery over time (PRO-BREST). Breast Care (Basel) 2022;17:272–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wolska J, Ammari T, Turnbull A, Johns N, Stafova D, Mensa Met al. Comparison of long-term outcomes of breast conservation and reconstruction after mastectomy using BREAST-Q. J Plast Reconstr Aesthet Surg 2022;75:2930–2940 [DOI] [PubMed] [Google Scholar]
- 11. Shiraishi M, Sowa Y, Tsuge I, Kodama T, Inafuku N, Morimoto N. Long-term patient satisfaction and quality of life following breast reconstruction using the BREAST-Q: a prospective cohort study. Front Oncol 2022;12:815498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. He S, Ding B, Li G, Huang Y, Han C, Sun Jet al. Comparison of outcomes between immediate implant based and autologous reconstruction: 15-year, single-center experience in a propensity score-matched Chinese cohort. Cancer Biol Med 2021;19:1410–1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santosa KB, Qi J, Kim HM, Hamill JB, Wilkins EG, Pusic AL. Long-term patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg 2018;153:891–899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nelson JA, Allen RJ Jr, Polanco T, Shamsunder M, Patel AR, McCarthy CMet al. Long-term patient-reported outcomes following postmastectomy breast reconstruction: an 8-year examination of 3268 patients. Ann Surg 2019;270:473–483 [DOI] [PubMed] [Google Scholar]
- 15. Cutress R, McIntosh S, Potter S, Goyal A, Kirwan C, Harvey Jet al. Opportunities and priorities for breast surgical research. Lancet Oncol 2018;19:e521–e533 [DOI] [PubMed] [Google Scholar]
- 16. Potter S, Fairhurst K, Cowan K, Vincent S, Lewis I, Cutress RIet al. Identifying research priorities in breast cancer surgery: a UK priority setting partnership with the James Lind Alliance. Breast Cancer Res Treat 2023;197:39–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Johnson L, Holcombe C, O’Donoghue JM, Jeevan R, Browne J, Fairbrother Pet al. Protocol for a national cohort study to explore the long-term clinical and patient-reported outcomes and cost-effectiveness of implant-based and autologous breast reconstruction after mastectomy for breast cancer: the brighter study. BMJ Open 2021;11:e054055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mohiuddin S, Hollingworth W, Glynn J, Jones T, Johnson L, Potter Set al. Secondary healthcare costs after mastectomy and immediate breast reconstruction for women with breast cancer in England: a population-based cohort study. Br J Surg 2023;110:1171–1179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jeevan R, Cromwell D, Browne J, van der Meulen J, Pereira J, Caddy Cet al. First Annual Report of the National Mastectomy and Breast Reconstruction Audit 2008. https://digital.nhs.uk/data-and-information/publications/statistical/national-mastectomy-and-breast-reconstruction-audit-annual-report/national-mastectomy-and-breast-reconstruction-audit-annual-report-2008 (accessed 3 March 2023).
- 20. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jeevan R, Cromwell D, Browne J, van der Meulen J, Pereira J, Caddy Cet al. National Mastectomy and Breast Reconstruction Audit 2010. Third Annual Report . https://digital.nhs.uk/data-andinformation/publications/statistical/national-mastectomy-andbreast-reconstruction-audit-annual-report/national-mastectomy-andbreast-reconstruction-audit-annual-report-2010 (accessed 3 March 2023)
- 22. Pusic A, Klassen A, Scott A, Klok J, Ordeiro PG, Cano S. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 2009;124:345–353 [DOI] [PubMed] [Google Scholar]
- 23. Davies CF, Macefield R, Avery K, Blazeby JM, Potter S. Patient-reported outcome measures for post-mastectomy breast reconstruction: a systematic review of development and measurement properties. Ann Surg Oncol 2021;28:386–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Voineskos SH, Klassen AF, Cano SJ, Pusic AL, Gibbons CJ. Giving meaning to differences in BREAST-Q scores: minimal important difference for breast reconstruction patients. Plast Reconstr Surg 2019;145:11e–20e [DOI] [PubMed] [Google Scholar]
- 25. Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin Det al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual life Res 2011;20:1727–1736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ 2018;27:7–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kouwenberg CAE, de Ligt KM, Kranenburg LW, Rakhorst H, de Leeuw D, Siesling Set al. Long-term health-related quality of life after four common surgical treatment options for breast cancer and the effect of complications: a retrospective patient-reported survey among 1871 patients. Plast Reconstr Surg 2020;146:1–13 [DOI] [PubMed] [Google Scholar]
- 28. Kouwenberg CAE, Kranenburg LW, Visser MS, Busschbach JJ, Mureau MAM. The validity of the EQ-5D-5L in measuring quality of life benefits of breast reconstruction. J Plast Reconstr Aesthet Surg 2019;72:52–61 [DOI] [PubMed] [Google Scholar]
- 29. Al-Janabi H, Flynn T N, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res 2012;21:167–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Flynn TN, Huynh E, Peters TJ, Al-Janabi H, Clemens S, Moody Aet al. Scoring the Icecap—a capability instrument. Estimation of a UK general population tariff. Health Econ 2015;24:258–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Berlin NL, Momoh AO, Qi J, Hamill JB, Kim HM, Pusic ALet al. Racial and ethnic variations in one-year clinical and patient-reported outcomes following breast reconstruction. Am J Surg 2017;214:312–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Santosa KB, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG. Effect of patient age on outcomes in breast reconstruction: results from a multicenter prospective study. J Am Coll Surg 2016;223:745–754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pusic AL, Matros E, Fine N, Buchel E, Gordillo GM, Hamill JBet al. Patient-reported outcomes 1 year after immediate breast reconstruction: results of the Mastectomy Reconstruction Outcomes Consortium Study. J Clin Oncol 2017;35:2499–2506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Baade PD, Youlden DR, Andersson TML, Youl PH, Kimlin MG, Aitken JFet al. Estimating the change in life expectancy after a diagnosis of cancer among the Australian population. BMJ Open 2015;5:e006740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hu ES, Pusic AL, Waljee JF, Kuhn L, Hawley ST, Wilkins Eet al. Patient-reported aesthetic satisfaction with breast reconstruction during the long-term survivorship period. Plast Reconstr Surg 2009;124:1–8 [DOI] [PubMed] [Google Scholar]
- 36. Wattoo G, Nayak S, Khan S, Morgan J, Hocking H, MacInnes Eet al. Long-term outcomes of latissimus dorsi flap breast reconstructions: a single-centre observational cohort study with up to 12 years of follow up. J Plast Reconstr Aesthet Surg 2021;74:2202–2209 [DOI] [PubMed] [Google Scholar]
- 37. Jeevan R, Cromwell D, Browne J, van der Meulen J, Pereira J, Caddy Cet al. The National Mastectomy and Breast Reconstruction Audit. A National Audit of Provision and Outcomes of Mastectomy and Breast Reconstruction Surgery for Women in England. Second Annual Report. https://digital.nhs.uk/data-and-information/publications/statistical/national-mastectomy-and-breastreconstruction-audit-annual-report/national-mastectomy-and-breastreconstruction-audit-annual-report-2009 (accessed 3 March 2023)
- 38. Berlin NL, Hamill JB, Qi J, Kim HM, Pusic AL, Wilkins EG. Nonresponse bias in survey research: lessons from a prospective study of breast reconstruction. J Surg Res 2018;224:112–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Potter S, Conroy EJ, Cutress RI, Williamson PR, Whisker L, Thrush Set al. Short-term safety outcomes of mastectomy and immediate implant-based breast reconstruction with and without mesh (iBRA): a multicentre, prospective cohort study. Lancet Oncol 2019;20:254–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Harvey KL, Sinai P, Mills N, White P, Holcombe C, Potter S. Short-term safety outcomes of mastectomy and immediate prepectoral implant-based breast reconstruction: pre-BRA prospective multicentre cohort study. Br J Surg 2022;109:530–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Potter S, Mackenzie M, Blazeby J. Does the addition of mesh improve outcomes in implant-based breast reconstruction after mastectomy for breast cancer? BMJ 2018;362:k2607. [DOI] [PubMed] [Google Scholar]
- 42. Sewart E, Turner NL, Conroy EJ, Cutress RI, Skillman J, Whisker Let al. Patient-reported outcomes of immediate implant-based breast reconstruction with and without biological or synthetic mesh. BJS Open 2021;5:zraa063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wilson RL, Kirwan CC, O’Donoghue JM, Linforth RA, Johnson RK, Harvey JR. BROWSE: a multicentre comparison of nine year outcomes in acellular dermal matrix based and complete submuscular implant-based immediate breast reconstruction—aesthetics, capsular contracture and patient reported outcomes. Eur J Surg Oncol 2022;48:73–81 [DOI] [PubMed] [Google Scholar]
- 44. Harvey K, Sinai P, Mills N, White P, Holcombe C, Potter S. Patient-reported outcomes of prepectoral implant-based breast reconstruction: early results from the pre-BRA prospective multi-centre cohort study. Eur J Surg Oncol 2022;48:e189–ee90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Paraskeva N, Guest E, Lewis-Smith H, Harcourt D. Assessing the effectiveness of interventions to support patient decision making about breast reconstruction: a systematic review. Breast 2018;40:97–105 [DOI] [PubMed] [Google Scholar]
- 46. Sherman KA, Shaw LE, Winch CJ, Harcourt D, Boyages J, Cameron LDet al. Reducing decisional conflict and enhancing satisfaction with information among women considering breast reconstruction following mastectomy: results from the BRECONDA randomized controlled trial. Plast Reconstr Surg 2016;138:592e–602e [DOI] [PubMed] [Google Scholar]
- 47. Paraskeva N, Tollow P, Clarke A, White P, Powell JE, Cox DMet al. A multi-centred sequential trial comparing PEGASUS, an intervention to promote shared decision making about breast reconstruction with usual care. J Plast Reconstr Aesthet Surg 2022;75:1342–1351 [DOI] [PubMed] [Google Scholar]
- 48. Hazari A, Cole R, Fowler C, Schache A, Ho M, Nugent Met al. First UK National Flap Registry Report . 2019. https://www.e-dendrite.com/index.php/UKNFR2019 (accessed 3 March 2023)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on reasonable request from the corresponding author.