Abstract
The origins of contemporary orthopedics can be traced all the way back to antiquity. Despite the absence of modern imaging techniques, a few bright minds were able to lay the groundwork for understanding these fractures. This historical review will cover the process behind the various treatments for elbow fractures, such as splinting and casting, mobilization, amputation, fracture fixation, arthroplasty, and arthroscopy.
Keywords: History, Fractures, Splinting, Mobilization, Amputation, Fixation, Arthroplasty, Arthroscopy
The struggle to define the complexities of elbow trauma dates back to ancient Egypt. An examination of 6000 Nubian skeletons even showed that 31% had fractures of the ulna and/or radius.38 Many practitioners from the Greek and Roman empires and countries such as India experimented with treating these fractures without radiographic imaging. Even after thousands of years, the different treatments established by the innovative doctors mentioned in this historical review remain the cornerstone of modern care for elbow fractures.
(Patho)Anatomy
Anatomy has long been recognized and is known as one of the cornerstones of medical education. An Indian physician and surgeon around 600 B.C. named Sushruta was one of the first that proclaim that anatomic knowledge is needed to become a skillful and successful surgeon.13
In Sushruta’s series of surgical volumes known as Sushruta Samhita, the bones are divided into 5 types: flat bones (Kapala), small cubical bones (Rucaka), cartilages (Taruna), thin curved bones without a medullary cavity (Valaya), and long bones with a medullary cavity (Nalaka). Each type of bone reacts differently to trauma; cartilages bend, long bones break, flat bones show multiple cracks, and small bones get fragmented.14 In addition, he provides an in-depth account of the treatment of 12 varieties of fractures and 6 types of dislocations with respect to the position of broken fragments (Supplementary Appendix S1).14 By carefully describing the different clinical features, he was able to diagnose the different bone trauma in a time without modern tools like the X-ray.
After Sushruta, a Roman physician named Aulus Cornelius Celsus compiled all the medical knowledge of his time, between 25 B.C. and 50 A.D., in De Medicina. With this work, Celsus was the first to translate Greek nomenclature into Latin, resulting in the medical terms we use today. After being printed in 1478, De Medicina was used as the first medical and surgical textbook.26
The introduction of the X-ray by Wilhelm Conrad Roentgen (1845-1923) in 1895 made it possible to assess bone anatomy without cutting. Within the first year after discovery, the device caught the attention of the medical world (Fig. 1). A year after discovery, the first installation in a public clinic was put into operation in the ‘New General Hospital’ in Hamburg-Eppendorf, Germany.2 Today, the X-ray is part of standard practice in orthopedic surgery and can be seen in every hospital.
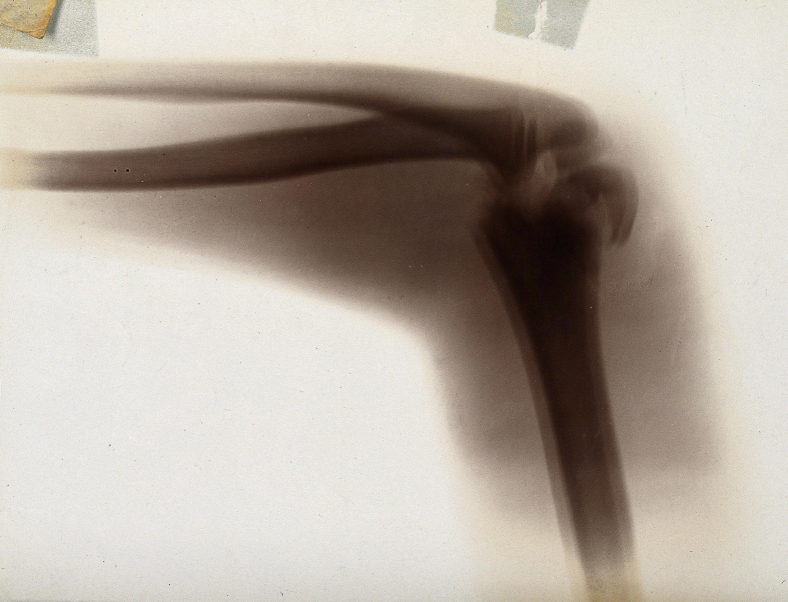
Figure 1.
The fracture and dislocation of bones in an elbow joint, viewed through x-ray. Photoprint from radiograph after Sir Arthur Schuster, 1896 (Public domain provided by Wellcome Collection).
Splinting and plastering
The rich history of various splint techniques stems from the instinctive reaction to immobilize the painful body part when there is physical discomfort. The easiest way to immobilize was then and is still the use of an extrinsic device.
The first proofs of splinting are from the Edwin Smith papyrus, which is thought to be the work of Imhotep. Imhotep is thought to have lived in the Nubian Desert around 2800 B.C.35,41 In ancient Egypt, gods were thought to create and control life.4 Imhotep, however, was among the first who did not base medical assessments on religious or spiritual beliefs.5 The papyrus notes 3 cases of humeral fractures describing reduction and splinting. Splints constructed of wood, bark, threads of date palm, coarse grass, and linen bandage were used to repair fractures (Fig. 2).
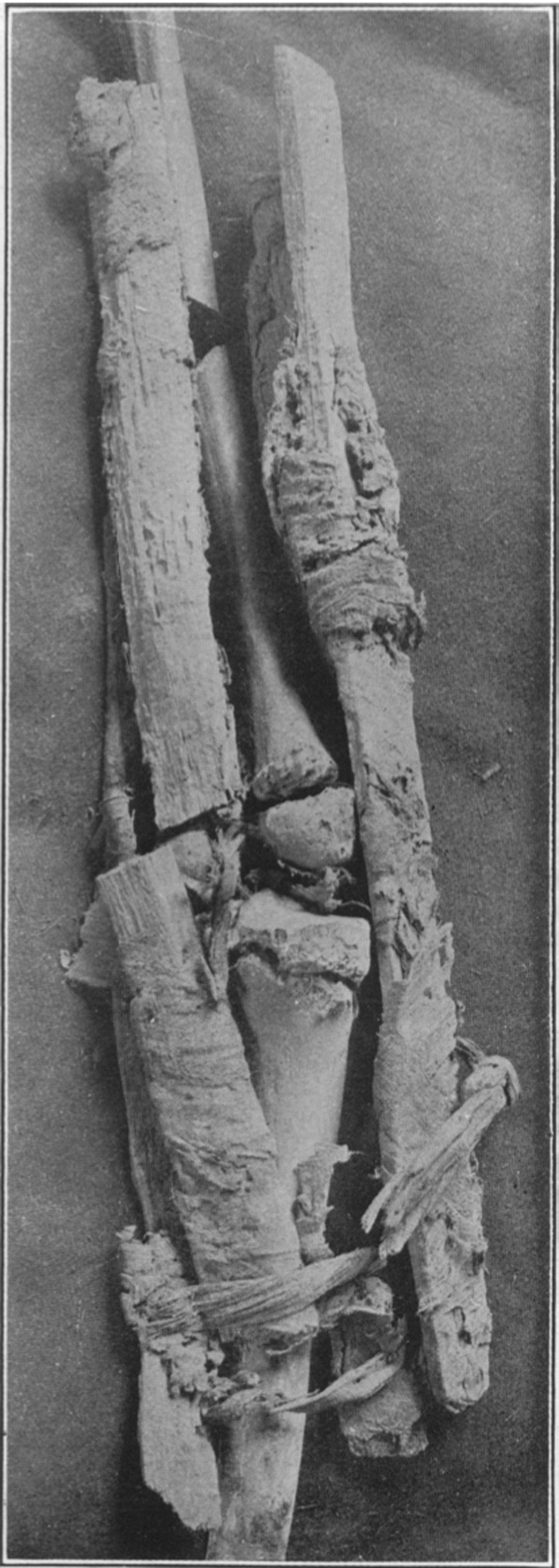
Figure 2.
Splint from Nubian Desert. Reprinted from British Medical Journal, Vol 1, no. 2465, Smith GE, THE MOST ANCIENT SPLINTS, p 736.2, Copyright 1908, with permission from British Medical Journal.
However, the materials used in Imhotep's period were not easily moldable to the injured joint. When armor emerged in European wars, blacksmiths were asked to use adaptable metals to make splints to treat injuries.17 In 1883, Friedrich Gustav Ernst described and illustrated a rack-and-pinion extension splint for elbow injuries in his book Orthopaedic Apparatus (Fig. 3).16 The use of metal in manufacturing splints made them more easily produced and standardized in practice. Alessandro Codivilla (1861-1912) brought the relationship between surgery and splinting to light not long after. This was the first set-up on the importance of post-treatment rehabilitation. In the early 1900s, plaster of Paris became widely accepted as a means of immobilizing fractures.17
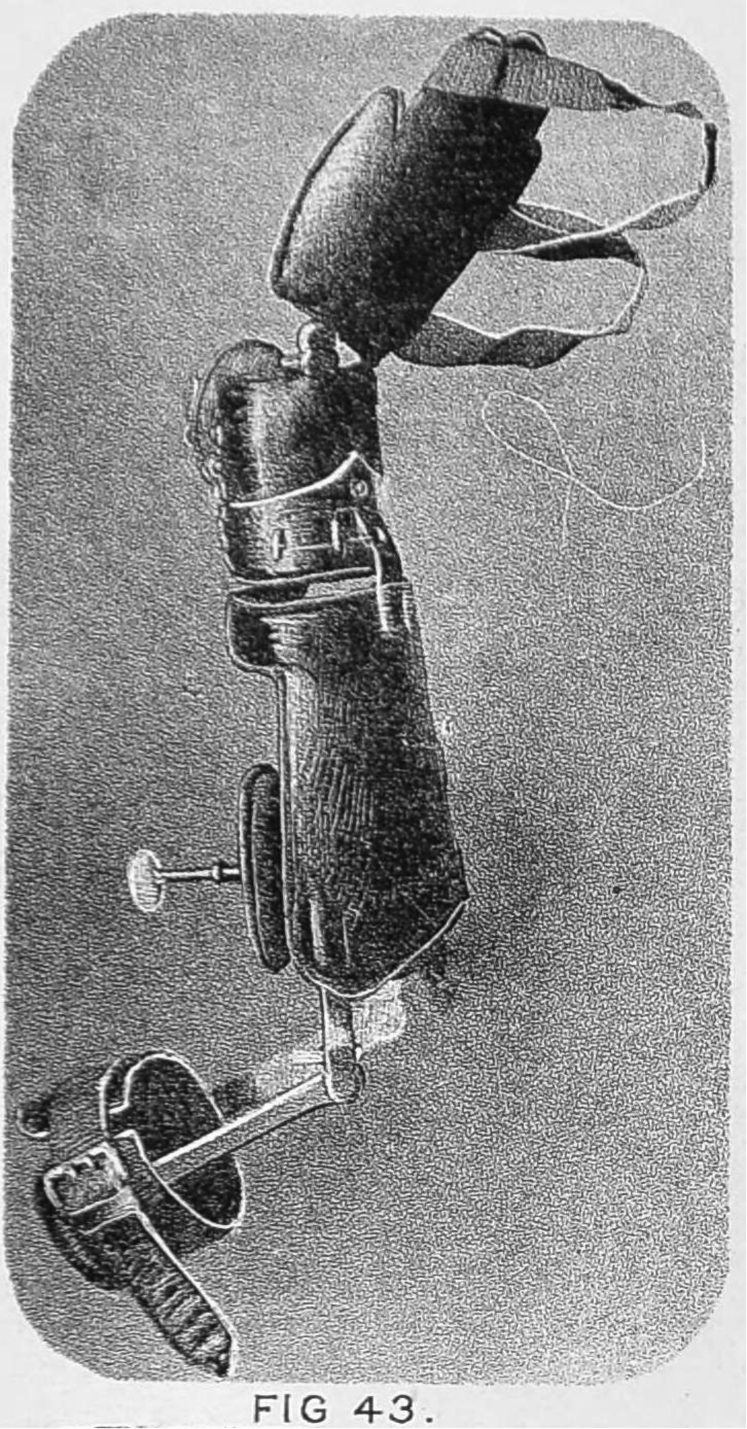
Figure 3.
Illustrated splint by Friedrich G. Ernst from Orthopaedic Apparatus (Public domain provided by Wellcome Collection).
Mobilization
Despite ever-improving immobilization techniques through splints or plasters, stiffness remained a common complication. Centuries after the Egyptian physician Imhotep, Celsus stated in De Medicina that a broken elbow requires mobilization for the tendons not to become fixed. Also, he warned against callus formation, which will prevent the elbow from flexing later.7
The potential risk of elbow contracture after trauma was emphasized by Ambroise Paré (1510-1590) in his surgical treatise Dix livres de la Chirurgie, avec Le Magasin des Instruments necessaires à icelle in 1564.30 He states:
“Left by the too long rest of the tyed up part and as it were glue …. Which falls abundantly into the joint of the elbow whence the stiffness and unmoveableness thereafter may be neither bended nor extended”
In his book, Paré suggested passively mobilizing the elbow. The German surgeon Lorenz Heister (1683-1758), a contemporary of Paré, also recognized the role of early passive and active mobilization to treat stiffness postfracture:21
“The joint for a long time without action… It will be very proper to foment the rigid part with emollient fomentations and baths; to rub it frequently with oils and fats of animals, and to move it backwards and forwards frequently with your hands till shall recover its natural faculty of moving”
Today, early mobilization after trauma or surgery is still the best way to prevent stiffness. However, there is still debate about how many days after surgery mobilization should be started.19
Amputation
Amputations were performed to save lives by sacrificing an irreparably damaged limb. However, complications such as hemorrhages and septic shock frequently resulted in the opposite effect.36
Amputations are already described in ancient Egyptian papyri. Religious beliefs played an important role in the medical care of Ancient Egypt. Bodies needed to be intact for the afterlife when buried. However, this belief led to amputation, a procedure that could save one’s life, being feared because it could affect the amputee in the afterlife. To avoid this fear, prostheses were made of leather and wood to replace an amputated limb in the afterlife (Fig. 4).27
Figure 4.
Prosthetic toe found on mummy (Public domain provided by The University of Manchester; from Egyptian toes likely to be the world’s oldest prosthetics by dr. Finch (2012); accessible by https://www.manchester.ac.uk/discover/news/egyptian-toes-likely-to-be-the-worlds-oldest-prosthetics/).
Hippocrates recommended amputation distally to the limb's gangrenous demarcation.27 This was possibly due to the loss of tissue sensation, making it less painful for the patients. Celsus, however, recommended cutting between the healthy and gangrenous tissue.15,27 In addition, he described using a flap of skin to cover the stump and vinegar-soaked lint to cover to wound as an attempt to avoid infections.
Due to the introduction of firearms in conventional warfare, soft-tissue damage and comminuted fracture were seen more frequently.22 Mainly gangrenous extremities were amputated. Paré stated that the limb should be amputated proximal to the gangrene through the healthy tissue. Despite saving lives with this, he discovered that some soldiers preferred to commit suicide rather than live without limbs or with terrible wounds. To replace the functionality of the amputated limb, Paré wrote works about artificial limbs he fitted on his amputees (Fig. 5).23
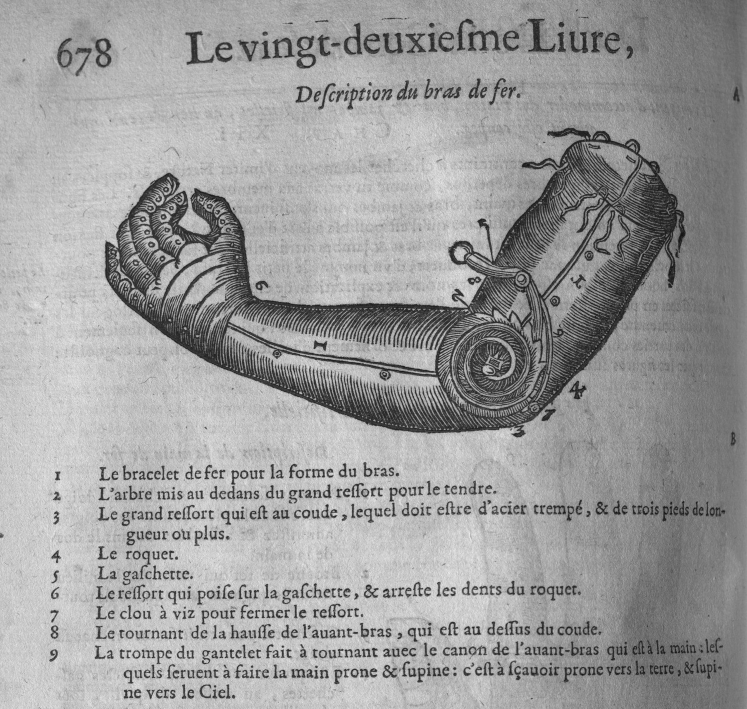
Figure 5.
Artificial Arm designed by Paré (Courtesy of the New York Academy of Medicine Library).18
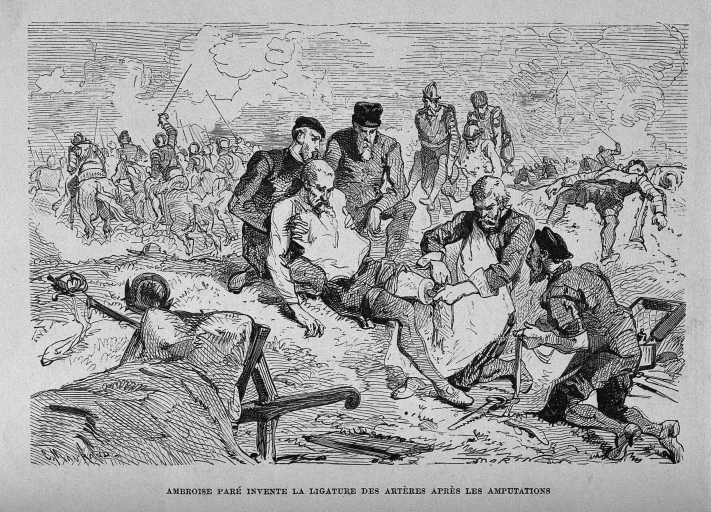
However, excessive blood loss was still a common complication after amputation and was life-threatening. Paré rediscovered the technique of using ligatures to stop the blood from a severed artery and vein by effective compression (Fig. 6).31 By using ligatures, the need for cauterization of bleeding vessels, which was done primarily with difficult-to-control tools such as fire or boiling oil, was eliminated. However, the use of ligatures was thought to be too time-consuming. Not long after Paré, another French surgeon named Morell introduced the application of a tourniquet during the battle of Flanders in 1674.36 With the introduction of the tourniquet by Jean-Louis Petit at the Royal Scientific Academy of Paris in 1718, compression of arterioles became a well-known standard practice for amputations to stop excessive bleeding.37
Figure 6.
Ambroise Paré, on the battlefield with a ligature to compress the artery of a soldier’s amputated leg. Wood engraving by Charles Maurand after E. Morin (Public domain provided by Wellcome Collection).
Over the centuries, many have tried to make this life-saving last resort less harmful. Although the procedure carries less risk today, it can greatly affect a patient's life. Fortunately, elbow amputations are rare in modern times.
Fracture fixation
In 1867, Joseph Lister (1827-1912) published his method of antisepsis. Later he described an antiseptic method for open reduction and internal fixation (ORIF) of the olecranon.1 The introduction of the antiseptic method changed the surgical treatment of fractures. Before Lister, surgeons hardly ever opened a joint or underwent an open procedure for a fracture that had not healed well after reduction.
Another individual of great influence was the Nobel laureate Emil Theodor Kocher (1841-1917). Kocher was a master of aseptic surgery and developed several surgical approaches and procedures for the elbow. He introduced a posterolateral approach that allows exposure of the distal humerus, radial head, and biceps tuberosity.6 This eponymous “Kocher approach” has been traditionally recommended for ORIF of elbow fractures. While the approach is taught as the interval between the anconeus and extensor muscles, in reality, it was a much greater extensile exposure.
Robert Danis (1880-1962) developed the principle-based methods of creating rigid internal fixation with self-developed plates and screws. His bone fragment repositioning and plate fixation technique influenced the development of the Swiss AO (Arbeitsgemeinschaft für Osteosynthesefragen) and continued to advance the outcomes of even the most challenging elbow fractures.9
ORIF is currently the gold standard for many elbow fractures. Although complications after ORIF, such as stiffness, ulnar nerve problems, and heterotopic ossifications, are decreasing in numbers, they are still a common problem.
Arthroplasty
In 1925, Robineau performed the first total elbow arthroplasty (TEA) using a prosthesis made of metal and vulcanized rubber.34 However, the ‘first generation’ of TEA designs resulted in many failure modes, such as component fractures and infections. In addition, there was little room for laxity in the linked implants, resulting in loosening due to stress at the implant-bone transition.39
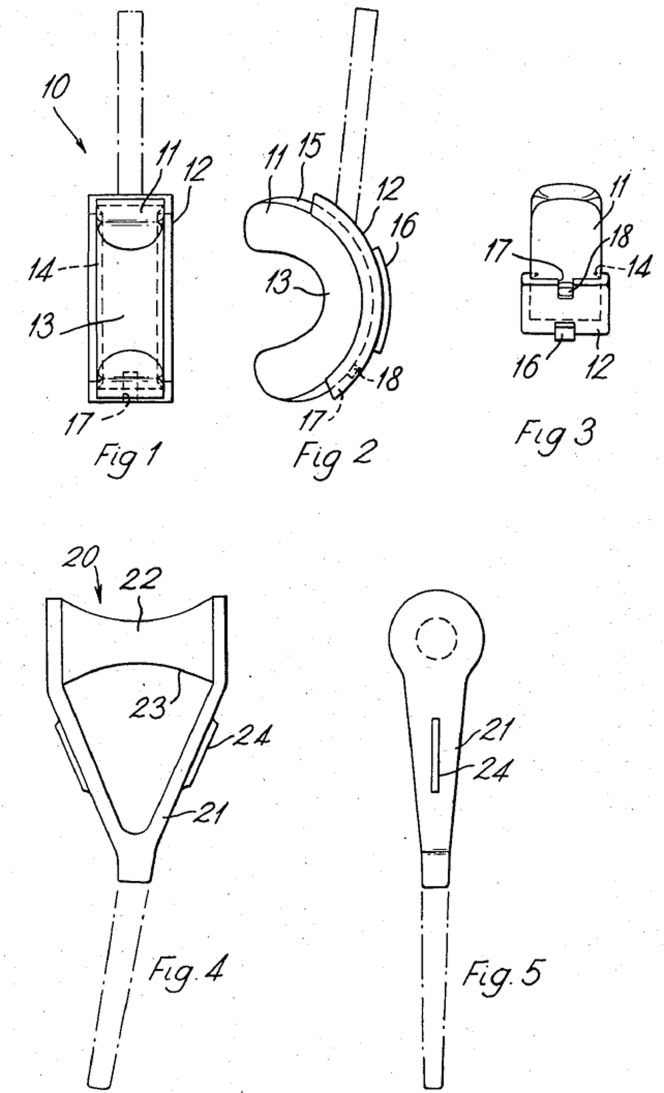
In 1972, the first modern TEA was performed by Dee (Fig. 7).12 Dee's technique differed from the others by the use of cement fixation. After this, many different TEA designs were introduced.8,33
Figure 7.
Design for an endoprosthetic elbow joint by R. Dee.11
Over the past few decades, elbow arthroplasties have been performed more frequently and the indication for arthroplasty has changed from mostly postinflammatory to more (post)traumatic.10,20,29 Through the years, positive outcomes in terms of functional outcomes and revision rates have been achieved thanks to increased TEA surgical expertise and improved materials and designs. However, joint registries still show decreased TEA survival compared to total hip arthroplasty or total knee arthroplasty, leaving much room for improvement.40
Arthroscopy
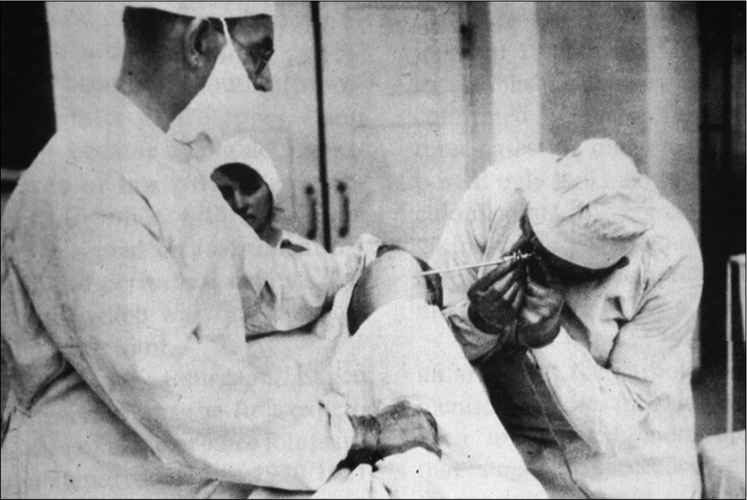
A Danish orthopedic surgeon named Severin Nordentoft (1866-1922) conducted the first arthroscopy known to have been recorded in 1912.25 This was the first time it was realized that endoscopy could be used to detect early musculoskeletal defects.3 In 1931, however, an article was published claiming that the elbow was unsuitable for examination with an arthroscope because the “needle” was too large for the small joint space (Fig. 8).32 This report put a stop to the growing interest in elbow arthroscopy. During the following decennia, the diameter of the arthroscopes decreased. The first arthroscope that reignited interest in elbow arthroscopy was the 1.7-mm arthroscope by Dr Masaki Watanabe in 1971.28 In 1974, the International Arthroscopy Association was founded to educate orthopedic surgeons on the value of arthroscopy. With this growth of interest, companies started to invest in developing arthroscopic instruments. With this improvement in technology, the results became better. Initially, the arthroscopes were used for diagnostic purposes and later for therapeutic purposes. This relatively new technique has had a major impact on fracture care in this century, providing smaller wounds and less complications.24
Figure 8.
E. Bircher performing arthroscopy in the 1920s with the original arthroscope. Reprinted from The Journal of Arthroscopic and Related Surgery, Vol 19, no. 7, Kieser CW, Jackson RW, Eugen Bircher (1882-1956), the first knee surgeon to use diagnostic arthroscopy, p 773., Copyright 2003, with permission from Elsevier.
Conclusion
We are privileged to have access to the knowledge of all these brilliant medical minds who developed the diagnostic and therapeutic strategies we use today. Only by studying the history of our surgical predecessors and keeping in mind how they pursued the unattainable, often in spite of criticism, will we remain inspired to emulate them and continue the progress they made. The introduction of various imaging modalities and supercomputers brings us ever closer to understanding these complex fractures.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflict of Interest: One or more of the authors (H.K.) has received funding from De Stichting Prof. Michaël-van Vloten Fonds (the Hague, the Netherlands), the Stichting het Scholten-Cordes Fonds (the Hague, the Netherlands), and the USC Scholarship Foundation (Utrecht, the Netherlands), but this has no relation to this article. For the rest of the authors, each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
The editor making the decision to accept this paper for publication had no conflicts of interest related to the decision. Furthermore, peer review of this paper was handled independently of any author of this paper.
Footnotes
Institutional review board approval was not required for this editorial.
This study was performed in Boston, MA, USA.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2023.01.005.
Supplementary data
References
- 1.Bartonícek J., Rammelt S. Early history of operative treatment of patellar fractures. Int Orthop. 2015;39:2303–2308. doi: 10.1007/s00264-015-2768-9. [DOI] [PubMed] [Google Scholar]
- 2.Behling R. X-ray sources: 125 years of developments of this intriguing technology. Phys Med. 2020;79:162–187. doi: 10.1016/j.ejmp.2020.07.021. [DOI] [PubMed] [Google Scholar]
- 3.Bennett K., Kamineni S. History of elbow arthroscopy. J Arthrosc Surg Sports Med. 2020;1:23–31. doi: 10.25259/JASSM_7_2020. [DOI] [Google Scholar]
- 4.Brazier Y. What was ancient Egyptian medicine like? [internet] 2018. https://www.medicalnewstoday.com/articles/323633 Available at:
- 5.Brien J.H. Imhotep: the real father of medicine? An iconoclastic view [internet] https://www.healio.com/news/pediatrics/20141203/imhotep-the-real-father-of-medicine-an-iconoclastic-view Available at:
- 6.Bumbasirević M.Z., Zagorac S.G., Lesić A.R. Emil Theodor Kocher (1841-1917)--orthopaedic surgeon and the first surgeon Nobel prize winner. Acta Chir Iugosl. 2013;60:7–11. doi: 10.2298/aci1303007b. [DOI] [PubMed] [Google Scholar]
- 7.Celsus. LacusCurtius • Celsus — on medicine — book VIII [internet] https://penelope.uchicago.edu/Thayer/E/Roman/Texts/Celsus/8*.html Available at:
- 8.Cooney WP, Morrey BF. Elbow arthroplasty: historical perspective and emerging concepts. In: Morrey's the elbow and its disorders. Lippincott Williams & Wilkins: Philadelphia, PA; 2009. p. 705-19.
- 9.Dauwe J., Nijs S., Gueorguiev B., Richards R.G. In Memoriam: Robert Danis, an inspiration for Maurice Müller and origins of the AO foundation. Acta Orthop Belg. 2020;86:577–579. [Google Scholar]
- 10.Day J.S., Lau E., Ong K.L., Williams G.R., Ramsey M.L., Kurtz S.M. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19:1115–1120. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Dee R. Endoprosthetic elbow joint [internet] 1974. https://patents.google.com/patent/US3852831A/en#citedBy Available at:
- 12.Dee R. Total replacement arthroplasty of the elbow for rheumatoid arthritis. J Bone Joint Surg Br. 1972;54:88–95. [PubMed] [Google Scholar]
- 13.Deepa B., Pushpalatha K. Contributions of Sushruta to anatomy. Anat J Afr. 2014;3:362–365. doi: 10.4314/aja.v3i2. [DOI] [Google Scholar]
- 14.Deshpande P.J., Sharma K.R., Prasad G.C. Contribution of Suśruta to the fundamentals of orthopaedic surgery. Indian J Hist Sci. 1970;5:13–35. [PubMed] [Google Scholar]
- 15.Ellis H. Greenwich Medical Media; London, UK: 2001. A history of surgery [internet] [Google Scholar]
- 16.Ernst F.G. Sprague; Philadelphia, PA: 1883. Orthopaedic apparatus: a series of illustrated plates, with corresponding descriptions of the various forms of mechanism employed in the treatment and cure of the numerous deformities of the human body. [Google Scholar]
- 17.Fess E.E. A history of splinting: to understand the present, view the past. J Hand Ther. 2002;15:97–132. doi: 10.1053/hanthe.2002.v15.0150091. [DOI] [PubMed] [Google Scholar]
- 18.Goldberg J. On Paré and prosthetics [internet]. Books Health Hist. 2014. https://nyamcenterforhistory.org/2014/12/19/on-pare-and-prosthetics/ Available at:
- 19.Harding P., Rasekaba T., Smirneos L., Holland A.E. Early mobilisation for elbow fractures in adults. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD008130.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Heijink A., Kodde I.F., Mulder P.G.H., Veltman E.S., Kaas L., van den Bekerom M.P.J., et al. Radial head arthroplasty: a systematic review. JBJS Rev. 2016;4:e3. doi: 10.2106/JBJS.RVW.15.00095. [DOI] [PubMed] [Google Scholar]
- 21.Heister L. A general system of surgery: in three parts: containing the doctrine and management of wounds, fractures, luxations, tumors, and ulcers, of all kinds. To which is prefixed, an introduction concerning the nature, origin, progress, and improvements of surgery. London: J. Hodges; 1750. pages 161-162 in Part II, Chapter IV, Section IV.
- 22.Hernigou P. Ambroise Paré II: Paré’s contributions to amputation and ligature. Int Orthop. 2013;37:769–772. doi: 10.1007/s00264-013-1857-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hernigou P. Ambroise Paré IV: the early history of artificial limbs (from robotic to prostheses) Int Orthop. 2013;37:1195–1197. doi: 10.1007/s00264-013-1884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsu J.W., Gould J.L., Fonseca-Sabune H., Hausman M.H. The emerging role of elbow arthroscopy in chronic use injuries and fracture care. Hand Clin. 2009;25:305–321. doi: 10.1016/j.hcl.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 25.Jackson R.W. A history of arthroscopy. Arthroscopy. 2010;26:91–103. doi: 10.1016/j.arthro.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Köckerling F., Köckerling D., Lomas C. Cornelius Celsus--ancient encyclopedist, surgeon-scientist, or master of surgery? Langenbecks Arch Surg. 2013;398:609–616. doi: 10.1007/s00423-013-1050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Markatos K., Karamanou M., Saranteas T., Mavrogenis A.F. Hallmarks of amputation surgery. Int Orthop. 2019;43:493–499. doi: 10.1007/s00264-018-4024-6. [DOI] [PubMed] [Google Scholar]
- 28.McGinty J.B., Burkhart S.S., Jackson R.W., Johnson D.H., Richmond J.C. 3rd ed. Lippincott Williams & Wilkins; Philadelphia: 2002. Operative arthroscopy. [Google Scholar]
- 29.Nestorson J., Rahme H., Adolfsson L. Arthroplasty as primary treatment for distal humeral fractures produces reliable results with regards to revisions and adverse events: a registry-based study. J Shoulder Elbow Surg. 2019;28:e104–e110. doi: 10.1016/j.jse.2018.07.035. [DOI] [PubMed] [Google Scholar]
- 30.Paré A. Dix livres de la chirurgie : avec le magasin des instrumens necessaires à icelle [internet]. 1564. https://gallica.bnf.fr/ark:/12148/bpt6k53751j Available at:
- 31.Paré A. Jean Gregoire; Lyon: 1664. Les Oeuvres d’Ambroise Paré. [Google Scholar]
- 32.Phillips N.J., Stanley D. (v) Arthroscopy of the elbow. Curr Orthop. 2002;16:355–361. doi: 10.1054/cuor.2002.0286. [DOI] [Google Scholar]
- 33.Prkić A., van Bergen C.J., The B., Eygendaal D. Total elbow arthroplasty is moving forward: review on past, present and future. World J Orthop. 2016;7:44–49. doi: 10.5312/wjo.v7.i1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robineau R. Contribution à l’Étude de la Prothèse Osseuse. Bull Mem Soc Nat Chir. 1927;53:886–896. [Google Scholar]
- 35.Saber A. Ancient Egyptian surgical heritage. J Invest Surg. 2010;23:327–334. doi: 10.3109/08941939.2010.515289. [DOI] [PubMed] [Google Scholar]
- 36.Sachs M., Bojunga J., Encke A. Historical evolution of limb amputation. World J Surg. 1999;23:1088–1093. doi: 10.1007/s002689900628. [DOI] [PubMed] [Google Scholar]
- 37.Saied A., Ayatollahi Mousavi A., Arabnejad F., Ahmadzadeh Heshmati A. Tourniquet in surgery of the limbs: a review of history, types and complications. Iran Red Crescent Med J. 2015;17 doi: 10.5812/ircmj.9588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smith G.E., Jones F.W. National Printing Department; Cairo: 1910. The archaeological survey of Nubia. Report for 1907-1908. Vol. 2, Report on the human remains. [Google Scholar]
- 39.Soni R.K., Cavendish M.E. A review of the Liverpool elbow prosthesis from 1974 to 1982. J Bone Joint Surg Br. 1984;66:248–253. doi: 10.1302/0301-620X.66B2.6707062. [DOI] [PubMed] [Google Scholar]
- 40.Welsink C.L., Lambers K.T.A., van Deurzen D.F.P., Eygendaal D., van den Bekerom M.P.J. Total elbow arthroplasty: a systematic review. JBJS Rev. 2017;5:e4. doi: 10.2106/JBJS.RVW.16.00089. [DOI] [PubMed] [Google Scholar]
- 41.Yousef J., Leow S.K.H., Morrison W. Plastic surgery in antiquity: an examination of ancient documents. Eur J Plast Surg. 2021;44:419–428. doi: 10.1007/s00238-020-01763-4. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.