Abstract
The coronoid process is key to concentric elbow alignment. Malalignment can contribute to post-traumatic osteoarthritis. The aim of treatment is to keep the joint aligned while the collateral ligaments and fractures heal. The injury pattern is apparent in the shape and size of the coronoid fracture fragments: (1) coronoid tip fractures associated with terrible triad (TT) injuries; (2) anteromedial facet fractures with posteromedial varus rotational type injuries; and (3) large coronoid base fractures with anterior (trans-) or posterior olecranon fracture dislocations.
Each injury pattern is associated with specific ligamentous injuries and fracture characteristics useful in planning treatment. The tip fractures associated with TT injuries are repaired with suture fixation or screw fixation in addition to repair or replacement of the radial head fracture and reattachment of the lateral collateral ligament origin. Anteromedial facet fractures are usually repaired with a medial buttress plate. If the elbow is concentrically located on computed tomography and the patient can avoid varus stress for a month, TT and anteromedial facet injuries can be treated nonoperatively. Base fractures are associated with olecranon fractures and can usually be fixed with screws through the posterior plate or with an additional medial plate. If the surgery makes elbow subluxation or dislocation unlikely, and the fracture fixation is secure, elbow motion and stretching can commence within a week when the patient is comfortable.
Keywords: Ulnohumeral, Subluxation, Dislocation, Treatment, Pattern of injury, Terrible triad, Posteromedial varus rotational type injury, Olecranon fracture dislocation
Fracture of the coronoid usually occurs in association with elbow subluxation and dislocation.49 Because the coronoid fracture characteristics correspond to specific patterns of injury, it is usually possible to anticipate concomitant soft tissue injuries. The injury pattern can, therefore, guide surgical decision-making. Optimal outcomes are founded upon concentric reduction of the elbow. This narrative review aims to outline the current research in the overall management of coronoid fractures.
Anatomy
The coronoid process forms the distal/anterior aspect of the trochlear notch of the ulna. It is a key part of the intricate interdependence of the elbow’s various stabilizing components that maintain concentric alignment of the joint.
The coronoid process is pyramidal and protrudes anteriorly and medially. The trochlear notch has a central ridge that interdigitates with the groove of the trochlea of the distal humerus. This ridge divides the coronoid articular surface into medial and lateral facets. The lateral facet is relatively small and ends laterally as the sigmoid notch, articulating with the radial head. The medial facet extends medially beyond the surface of the ulna metaphysis.
The coronoid process resists varus and posteriorly directed stress.21,23 A notable portion of the anteromedial facet (AMF) of the coronoid process is not supported by the metaphysis of the ulna, making it relatively susceptible to fracture.15,54 Micro computed tomography (CT) reveals trabecular bone arrangement perpendicular to joint reaction forces,66 corresponding to biomechanical studies identifying the coronoid as an important osseous stabilizer serving as an anterior buttress for elbow stability.
Many ligaments and muscles insert into the coronoid process. The anterior bundle of the medial collateral ligament inserts on the sublime tubercle of the coronoid. The brachialis muscle, a dynamic stabilizer of the elbow joint, inserts on the distal volar base of the coronoid and the ulnar shaft.51 The elbow joint capsule attaches about 2 mm to 6 mm from the coronoid tip and conforms to the shape of the elbow’s articular surfaces, leaving the tip “free” of tendinous insertion with an intra-articular appearance on arthroscopy.1,7 In our experience, even the smallest coronoid tip fragments include this capsular insertion. Finally, the lateral collateral ligament (LCL) inserts on the supinator crest, an elongated bony prominence on the lateral side of the ulna.
Classification
The classification suggested by Regan and Morrey was based on coronoid height as assessed on a lateral radiograph: type 1 was described as an avulsion at the tip of the coronoid process, the fracture fragment of type 2 was described as more than an avulsion but less than 50% of the coronoid height, and type 3 involved more than 50% of the coronoid height. This classification brought attention to the coronoid, and newer classifications have tried to be more specific than the somewhat vague and ambiguous distinctions such as “avulsion” and the 50% height threshold.7,13,57
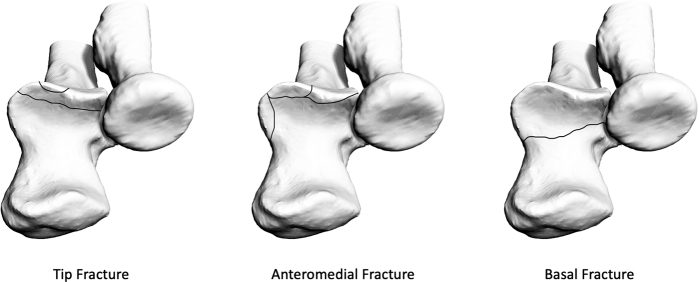
The Mayo classification, also known as the O'Driscoll classification, is based on the location, shape, and size of the coronoid fracture fragments and is divided into: type 1: tip fracture, type 2: AMF fracture, and type 3: base fracture (Fig. 1).43,48
Figure 1.
Mayo classification of coronoid process fractures. Used with permission of The Bone & Joint Journal, from de Klerk HH, Oosterhoff JHF, Schoolmeesters B, Nieboer P, Eygendaal D, Jaarsma RL, IJpma FFA, van den Bekerom MPJ, Doornberg JN; Traumaplatform 3D Consortium. Recognition of the pattern of complex fractures of the elbow using 3D-printed models. Bone Joint J. 2023 Jan;105-B(1):56-63.31; permission conveyed through Copyright Clearance Center, Inc.
The Mayo types are further subcategorized.48 Type 1 is subcategorized as ≤2 mm and >2 mm coronoid tip fractures. Type 2 is subcategorized as fractures involving the anteromedial rim, anteromedial rim plus tip, and anteromedial rim plus sublime tubercle with or without the involvement of the tip. Type 3 can be subcategorized as a coronoid base and body fracture (subtype 1) and a transolecranon basal coronoid fracture (subtype 2).
Recently, Watts et al introduced the Wrightington classification, based on the overall elbow injury pattern associated with specific coronoid fracture morphology.67 This classification specifies anticipated, associated soft tissue injuries in addition to the recognized bone injury patterns.
Patterns of injury
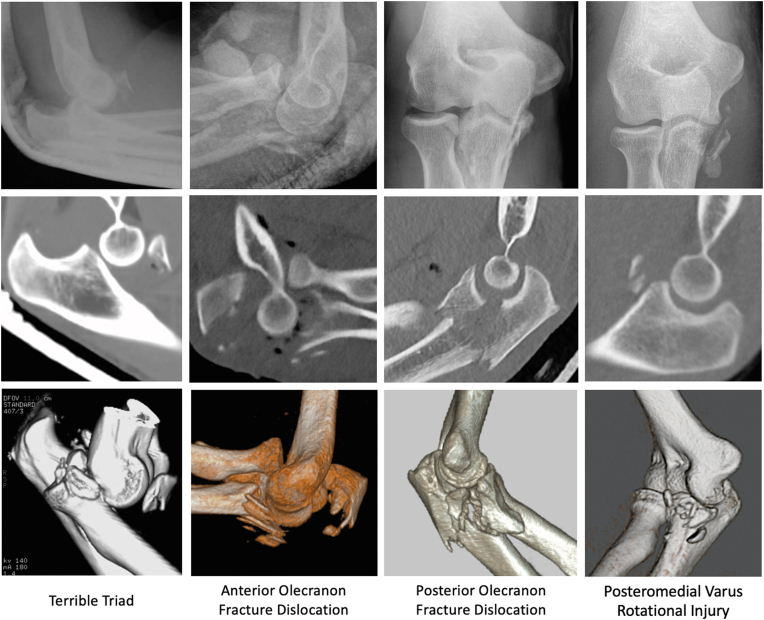
Three general injury patterns are associated with the 3 types of coronoid fractures in the Mayo classification.16,43 Tip fractures of the coronoid are associated with posterior dislocation of the elbow and fracture of the radial head, the so-called TT fracture dislocation of the elbow.14 AMF fractures are associated with avulsion of the LCL from the lateral epicondyle and subluxation rather than dislocation of the elbow (the so-called posteromedial varus rotational injury [PMVRI]).48 Fractures of the base of the coronoid are associated with olecranon fracture dislocation, which can occur in either an anterior or a posterior direction (Fig. 2).
Figure 2.
Elbow fracture patterns with coronoid involvement (Top row = X-ray, Middle row = 2D-CT, Bottom row = 3D-CT).
The TT injury pattern was named for the many complications that occur despite treatment. It is difficult to study the mechanism of injury because detailed videos of the injuries and detailed radiological studies are needed to correlate what happened to the body and arm with the pathophysiology of the coronoid and elbow.
AMF coronoid fractures are associated with either avulsion of the LCL and part or all of the common extensor origins from the lateral epicondyle or fracture of the olecranon.12,33,41,48 The anterior band of the MCL is generally intact unless the elbow dislocates. The injury pattern is proposed as a fall back into the flexed arm with the shoulder maximally, internally rotated, resulting in a varus force with a posteromedial rotation on the elbow.48 Collision between the trochlea and coronoid process causes the AMF shearing fracture.2
Olecranon fracture dislocations are associated with basilar coronoid fractures.16,43 Posterior olecranon fracture dislocations are characterized by a fracture of the olecranon and coronoid process, posterior displacement of the radius with respect to the capitellum (with an intact radioulnar relationship), and fracture of the radial head.16 The ulnotrochlear articular surfaces remain apposed, the MCL is usually intact on the fractured coronoid, and the LCL is avulsed in a subset of injuries. The brachialis seems relatively unaffected and is not a concern. The coronoid is often fragmented and can be challenging to align and secure.57 The pattern is thought to be caused by a fall on an outstretched hand. Many patients with posterior olecranon fracture dislocation are older and have diminished bone quality.
Anterior olecranon fracture dislocations feature anterior dislocation of the forearm with an intact radioulnar relationship. The coronoid fracture is often a single fragment. In this type of injury, the articular surfaces remain opposed, and the MCL and LCL are usually still attached to the coronoid fragment. Anterior olecranon fracture dislocations are thought to be caused by a direct blow to the posterior aspect of the flexed elbow. During the moment of impact on the back of the forearm, the humerus is driven through the trochlear notch of the ulna.
Other aspects of pathophysiology
One key aspect of traumatic elbow instability is that the collateral ligaments are usually avulsed from their epicondylar origins (along with some degree of the common flexor and extensor muscle origin) and that these normally heal well as long as the elbow remains concentric for 2-3 weeks.40 This is true even if the elbow is relocated months after injury.26 In our experience, tendon graft reconstruction is not usually necessary or helpful in the treatment of coronoid fractures and traumatic elbow instability.
In the care of patients, there is not a direct relationship between the amount of coronoid involved in the fracture and subluxation or dislocation of the elbow, perhaps because other injury factors are also important.3,46,53 In cadaveric studies, there is some correlation between coronoid fracture fragment size and resistance to various types of articular stresses. In the clinical setting, some of the most troublesome injuries involve relatively small coronoid fractures, which are likely markers of greater soft tissue injury. According to a study by Mathew et al, depending on the associated bony and soft tissue injuries, even as little as 10% missing coronoid can be associated with recurrent dislocation.38 In other words, mechanical properties do not always tell the whole story. In our experience, most basilar and AMF fractures are associated with subluxation rather than dislocation, with the anterior band of the MCL typically intact. Securing the coronoid fracture can, therefore, restore ligament function and elbow alignment.
Imaging
Specific patterns of traumatic elbow instability can be diagnosed with moderate interobserver reliability and reasonable accuracy using radiographs alone.14 When characteristics of the coronoid or radial head fractures are difficult to assess on radiographs, three-dimensional (3D) reconstructions of CT scans with subtraction of the distal humerus can be helpful compared with 2D images.35
Magnetic resonance imaging is not recommended since signal abnormalities of the ligaments may not correspond with ligament functional status and may not guide treatment. Examination maneuvers described for diagnosis of persistent ligament insufficiency, such as the lateral pivot shift test, posterolateral rotatory drawer, or moving valgus stress test, are not useful in awake patients with acute coronoid fractures.8,9,36,60,62 The pattern of the injury can be used to anticipate ligament insufficiency, which can be verified during an examination while the patient is under anesthesia and assessed upon operative exposure.
Treatment
The goal of the treatment of coronoid fractures is a concentric reduction of the ulnohumeral articulation. Residual malalignment can contribute to post-traumatic osteoarthritis.4 Some small coronoid tip fractures, selected TT injuries, and PMVRIs (AMF fractures) with no joint subluxation can be treated nonoperatively with avoidance of varus stress for 1 month and active, self-assisted stretching exercises, and including overhead gravity-assisted exercises.33 Most other coronoid fractures, including all base fractures, are considered for operative treatment.
If surgery is preferred, the Hotchkiss “Over-the-Top” approach using the plane between the flexor-pronator mass and the flexor carpi ulnaris (FCU) exposes the coronoid tip well.22 Although tip fractures of the coronoid are usually treated through the lateral exposure started by the injury. The FCU-Splitting approach, where the ulnar nerve runs, provides direct exposure to the AMF.42,48 The Taylor–Scham approach, in which the complete FCU-pronator teres mass is elevated, provides good access to the base of the coronoid.64 Finally, although less commonly utilized, an anterior approach, where the biceps is retracted radially and the brachialis is split along its midline to the level of the elbow'’s anterior capsule, can be used for direct visualization and access to the coronoid tip and trochlea, although it can be a relatively deep hole.28,55
Tip fractures
Tip fractures are associated with TT injuries and are often considered for repair. Repair or replacement of the radial head fracture and reattachment of the LCL origin to the lateral epicondyle can be sufficient for many TT injuries. If the elbow remains aligned under gravity stress after repair or replacement of the radial head fracture and reattachment of the LCL origin to the lateral epicondyle, then it may be reasonable to leave the coronoid untreated.27,30,52 On the other hand, in the absence of reliable identification of injuries at risk for subluxation and dislocation, repair of the coronoid tip fracture or temporary support of ulnohumeral joint alignment with an internal or external fixator is considered.
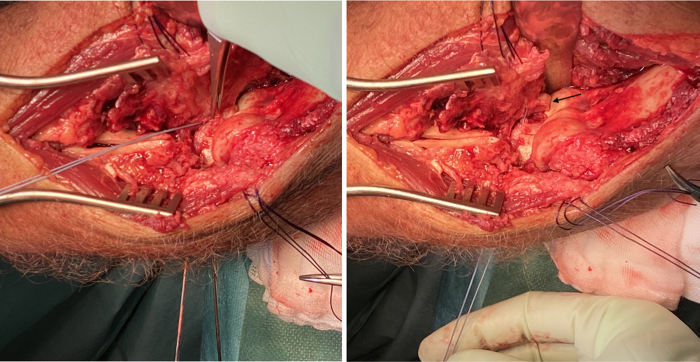
Tip fracture fragments are small and often best secured with a suture engaging the capsular insertion.16 Access to the tip fracture is through the lateral exposure with elevation of the origin of the radial wrist extensors of the lateral condylar ridge and the brachialis of the anterior humerus. The supinator can be split distally. The radial head fragments are moved out of the way or the radial head is resected. When the fracture fragment is large enough, the suture can be passed through drill holes in the fragment. A Keith needle or suture passer can be used to pass the suture through the drill holes in the ulna metaphysis (Fig. 3). It can be helpful to use a wire guide such as that in the anterior cruciate ligament reconstruction set to make the drill holes. It can be helpful to cross the drill holes to avoid skiving off the posterior surface of the ulna. Since concomitant injuries are common, the suture should not be tied until other injuries are addressed so that the elbow can be subluxated in order to place a radial head prosthesis.57
Figure 3.
Guiding the suture for fixation.
If treatment is delayed and the tip fracture cannot be realigned and secured, a bone graft can be considered to enhance stability. The olecranon tip, radial head remnant, iliac crest, navicular bone, and costal grafts are described as options.5,18,29,68,69 During the reconstruction, the contralateral coronoid process can be used as a guide since it is similar in shape and size.70
AMF fractures
Nonoperative treatment may be considered if there is a concentric alignment of the ulnohumeral joint and the patient can be trusted to avoid varus stress.33,58 It is important to monitor radiographic alignment for the first month during nonoperative treatment.
Subtype 1 (anteromedial rim) fractures are often associated with a complete dislocation and—among elbow dislocations with no or only very small fractures—might be a marker for a higher potential for repeat dislocation. If there seems to be a tendency to subluxation or repeat dislocation, it is advised to consider operative treatment consisting of suturing this fragment (either open or arthroscopic) and reattaching the medial and LCL complexes and common flexor and extensor muscle origins to the epicondyles or, alternatively, using temporary fixation to keep the ulnohumeral joint aligned.
For single-fragment subtype 2 (anteromedial rim + tip) fractures, several studies have reported successful nonoperative treatment when there is a concentric reduction on 3D CT scans and the patient can be trusted to avoid varus stress (shoulder abduction) for 1 month.10,33,45,63 For 2-fragment fractures associated with ulnohumeral joint subluxation, it is recommended to secure the main anteromedial fragment with a buttress plate with less importance placed on the second, usually smaller, tip fragment.34,56 Arthroscopic-assisted fixation is an option for some small coronoid fractures that may not benefit from a buttress plate.12,50 There is an appeal to more limited soft-tissue dissection compared to open surgery.20
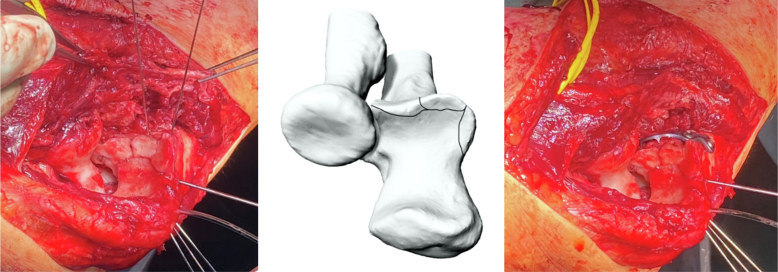
For subtype 3 (anteromedial rim + sublime tubercle) fractures, it is best to use a medial buttress plate (Fig. 4).34
Figure 4.
Buttress plate for anteromedial facet fracture.
Base fractures
Base fractures are usually fixed with screws through a posterior plate, with or without an additional medial plate.47 For single-fragment fractures, a posterior plate that wraps around the olecranon is sufficient. Most basilar coronoid fractures are large enough to secure with more than one screw.5 Sometimes, a coronoid base fracture is so fragmented that solid internal fixation is not possible. In that setting, an external fixator or internal joint stabilizer (IJS) may be considered to support elbow alignment. If this is not sufficient, one can always consider cross-pinning the joint with buried Steinman pins protected by a cast for one month and then remove the pins.
Outcomes
The TT injury is notorious for poor outcomes. Studies of patients treated in the 1970s and 1980s identified the presence of a coronoid fracture as associated with subluxation, dislocation, and arthrosis.6,25 A series published in 200259 described treatment without repair of the coronoid, varied treatment of the radial head, and no reattachment of the LCL to the lateral epicondyle, reporting a mean Broberg-Morrey score of 76 (categorically fair), 5 redislocations after surgery, and degenerative changes in 10 of the 11 patients (91%), most related to residual subluxation. The study by Pugh et al39 described a standard protocol involving fixation of the coronoid for Regan–Morrey type 2 and 3 or anterior capsule repair for type 1, repair or replacement of the radial head, reattachment of the LCL to the lateral epicondyle, and reattachment of the MCL when residual subluxation or dislocation occurred intraoperatively during extension after the other interventions. A hinged external fixator was recommended when stability could not be restored by the aforementioned steps. Eight of 36 (22%) had an unplanned second surgery: 4 for implant removal and elbow stiffness, 2 for heterotopic bone causing proximal radioulnar synostosis, 1 for a deep wound infection, and one for hinged external fixator to address unspecified loss of alignment. A systematic review in 201411 documented the mean Mayo Elbow Performance Score (MEPS) ranging from 78 to 95 (categorically good to excellent) and DASH (Disabilities of the Arm, Shoulder, and Hand) score ranging from 9 to 31. Subluxation or dislocation leading to another surgery was reported in 11 of the 16 studies, with a wide range from 3% to 45%. Three studies followed patients for a mean of 14 months, 27 months, and 35 months and reported ulnar neuropathy in 11%, 8%, and 25%, respectively.17,61,65 Degenerative changes were reported in 7 of the 16 studies, with most reporting rates lower than 38% after a mean of 1-5 years. In a study of buttress plate fixation of subtype 2 (46%) and 3 (54%) AMF fractures,32 3 of 24 patients (13%) had degenerative changes and there was a mean MEPS of 98, a mean of 1 year after surgery.
One study12 of arthroscopic-assisted reduction and cannulated screw, suture, or K-wire fixation (ARIF) of subtype 2 AMF coronoid fractures along with LCL reattachment to the epicondyle tear (usually done open) reported a mean MEPS of 98 with a mean flexion of 135 degrees and a mean flexion contracture (extension) of 9 degrees an average of 28 months after surgery. A nonrandomized study50 that compared ARIF with ORIF for Regan-Morrey type 2 and 3 coronoid fractures in posteromedial varus rotational pattern injuries documented no differences in pain intensity, MEPS, and Disabilities of the Arm, Shoulder, and Hand (DASH) scores a mean of 2 years after surgery. Two of 10 (20%) patients undergoing ORIF had ulnar neuropathy. In the ARIF group, an unspecified tingling discomfort was present for a week in 1 of the 15 (7%) patients.
Postoperative recovery
When the fixation is secure, the patient can begin active, self-assisted stretching exercises for the forearm and elbow within a week. Doing the exercises in an overhead position adds gravity assistance of concentric alignment and elbow flexion.37 In the first month, while the LCL origin is healing back to the epicondyle, shoulder abduction is avoided during exercises.36
Future perspectives
There are several areas for future investigation to improve the treatment of coronoid fractures. First, we need more evidence regarding which fractures can be safely treated nonoperatively. In our experience, if the elbow can stay concentrically reduced and the radial head fracture creates little or no block to forearm rotation, nonoperative treatment is an option. This is possible for many TT and AMF injuries.
For TT injuries with a tendency toward subluxation or dislocation; what are the indications for fixing a small tip fracture? Is there a role for screws, or is suture sufficient? What is the role of ignoring the coronoid fracture and using a temporary IJS to maintain alignment?
For smaller AMF fractures, is suture fixation an option, and can this be achieved arthroscopically? Or is it reasonable to apply an IJS without coronoid fixation? For subtype 2 AMF fractures, when should a tip fragment be secured and when is it sufficient to secure the large AMF fragment alone?
For coronoid base fractures, what are the best techniques to maintain a concentric reduction if the coronoid fracture is too fragmented for secure fixation? Is an IJS or external fixator sufficient, or is cross pinning for about a month important?
When planning surgery, is virtual reduction of CT images of coronoid fracture fragments helpful?44 What about the printing of 3D models, which is more readily available and may help surgeons recognize the elbow fracture pattern and plan the surgery?19,31 Could 3D printing may be used to produce intraoperative tools as patient-specific plates combined with drilling guides, and would that be an advantage?24
Disclaimers:
Funding: HK reports receipt of support by the Stichting Prof. Michaël-van Vloten Fonds, Stichting Anna Fonds, Het Scholten-Cordes Fonds, and USC Scholarship Foundation.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
No institutional review board approval was required for this narrative review.
References
- 1.Ablove R.H., Moy O.J., Howard C., Peimer C.A., S’Doia S. Ulnar coronoid process anatomy: possible implications for elbow instability. Clin Orthop. 2006;449:259–261. doi: 10.1097/01.blo.0000218729.59838.bc. [DOI] [PubMed] [Google Scholar]
- 2.Al-Ani Z., Wright A., Ricks M., Watts A.C. Posteromedial rotatory instability of the elbow: what the radiologist needs to know. Eur J Radiol. 2021;141 doi: 10.1016/j.ejrad.2021.109819. [DOI] [PubMed] [Google Scholar]
- 3.Beingessner D.M., Dunning C.E., Stacpoole R.A., Johnson J.A., King G.J.W. The effect of coronoid fractures on elbow kinematics and stability. Clin Biomech Bristol Avon. 2007;22:183–190. doi: 10.1016/j.clinbiomech.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Bellato E., Kim Y., Fitzsimmons J.S., Hooke A.W., Berglund L.J., Bachman D.R., et al. Role of the lateral collateral ligament in posteromedial rotatory instability of the elbow. J Shoulder Elbow Surg. 2017;26:1636–1643. doi: 10.1016/j.jse.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 5.Bellato E., Rotini R., Marinelli A., Guerra E., O’Driscoll S.W. Coronoid reconstruction with an osteochondral radial head graft. J Shoulder Elbow Surg. 2016;25:2071–2077. doi: 10.1016/j.jse.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Broberg M.A., Morrey B.F. Results of treatment of fracture-dislocations of the elbow. Clin Orthop. 1987:109–119. [PubMed] [Google Scholar]
- 7.Cage D.J., Abrams R.A., Callahan J.J., Botte M.J. Soft tissue Attachments of the ulnar coronoid process: an Anatomic study with radiographic correlation. Clin Orthop. 1995:154–158. [PubMed] [Google Scholar]
- 8.Camp C.L., Smith J., O’Driscoll S.W. Posterolateral rotatory instability of the elbow: Part I. Mechanism of injury and the posterolateral rotatory drawer test. Arthrosc Tech. 2017;6:e401–e405. doi: 10.1016/j.eats.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camp C.L., Smith J., O’Driscoll S.W. Posterolateral rotatory instability of the elbow: Part II. Supplementary examination and dynamic imaging techniques. Arthrosc Tech. 2017;6:e407–e411. doi: 10.1016/j.eats.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan K., Faber K.J., King G.J.W., Athwal G.S. Selected anteromedial coronoid fractures can be treated nonoperatively. J Shoulder Elbow Surg. 2016;25:1251–1257. doi: 10.1016/j.jse.2016.02.025. [DOI] [PubMed] [Google Scholar]
- 11.Chen H., Liu G., Wu L. Complications of treating terrible triad injury of the elbow: a systematic review. PLoS One. 2014;9 doi: 10.1371/journal.pone.0097476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colozza A., Menozzi M., Perna L., Cavaciocchi M., Martini I., Galavotti C., et al. Results of arthroscopically assisted reduction and fixation of anteromedial facet coronoid fractures at short-term follow-up. J Shoulder Elbow Surg. 2022;31:1890–1897. doi: 10.1016/j.jse.2022.03.026. [DOI] [PubMed] [Google Scholar]
- 13.Doornberg J.N., van Duijn J., Ring D. Coronoid fracture height in terrible-triad injuries. J Hand Surg. 2006;31:794–797. doi: 10.1016/j.jhsa.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Doornberg J.N., Guitton T.G., Ring D., Science of Variation Group Diagnosis of elbow fracture patterns on radiographs: interobserver reliability and diagnostic accuracy. Clin Orthop. 2013;471:1373–1378. doi: 10.1007/s11999-012-2742-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doornberg J.N., de Jong I.M., Lindenhovius A.L.C., Ring D. The anteromedial facet of the coronoid process of the ulna. J Shoulder Elbow Surg. 2007;16:667–670. doi: 10.1016/j.jse.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Doornberg J.N., Ring D. Coronoid fracture patterns. J Hand Surg. 2006;31:45–52. doi: 10.1016/j.jhsa.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 17.Egol K.A., Immerman I., Paksima N., Tejwani N., Koval K.J. Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis. 2007;65:263–270. [PubMed] [Google Scholar]
- 18.Erhart S., Lutz M., Deml C., Sitte I., Angermann P. Restoring independency with an osteochondral graft of the navicular for coronoid process reconstruction. Arch Orthop Trauma Surg. 2017;137:225–232. doi: 10.1007/s00402-016-2623-5. [DOI] [PubMed] [Google Scholar]
- 19.Fillat-Gomà F., Marcano-Fernández F.A., Coderch-Navarro S., Martínez-Carreres L., Berenguer A. 3D printing innovation: New insights into upper extremity surgery planning. Injury. 2021;52:S117–S124. doi: 10.1016/j.injury.2021.01.048. [DOI] [PubMed] [Google Scholar]
- 20.Fink Barnes L.A., Parsons B.O., Hausman M. Arthroscopic management of elbow fractures. Hand Clin. 2015;31:651–661. doi: 10.1016/j.hcl.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Hartzler R.U., Llusa-Perez M., Steinmann S.P., Morrey B.F., Sanchez-Sotelo J. Transverse coronoid fracture: when does it have to be fixed? Clin Orthop. 2014;472:2068–2074. doi: 10.1007/s11999-014-3477-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hotchkiss R.N., Kasparyan G.N. The medial “over the top” approach to the elbow. Tech Orthop. 2000;15:105–112. [Google Scholar]
- 23.Hull J.R., Owen J.R., Fern S.E., Wayne J.S., Boardman N.D. Role of the coronoid process in varus osteoarticular stability of the elbow. J Shoulder Elbow Surg. 2005;14:441–446. doi: 10.1016/j.jse.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 24.IJpma F.F.A., Meesters A.M.L., Merema B.B.J., Ten Duis K., de Vries J.-P.P.M., Banierink H., et al. Feasibility of imaging-based 3-dimensional models to design patient-specific Osteosynthesis plates and drilling guides. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.37519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Josefsson P.O., Gentz C.F., Johnell O., Wendeberg B. Dislocations of the elbow and intraarticular fractures. Clin Orthop. 1989:126–130. [PubMed] [Google Scholar]
- 26.Jupiter J.B., Ring D. Treatment of unreduced elbow dislocations with hinged external fixation. J Bone Joint Surg. Am. 2002;84:1630–1635. doi: 10.2106/00004623-200209000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Kaneshiro Y., Yano K., Yokoi T., Sakanaka H., Fukuda M., Hidaka N. Is repair of a small coronoid fracture required in the surgical treatment of terrible triad injury of the elbow? J Hand Surg Asian-pac Vol. 2022;27:345–351. doi: 10.1142/S2424835522500412. [DOI] [PubMed] [Google Scholar]
- 28.Kang L.-Q., Ding Z.-Q., Sha M., Hong J.-Y., Chen W. A minimally invasive anterior approach to reduction and screw fixation of coronoid fractures. J Hand Surg Eur Vol. 2010;35:224–227. doi: 10.1177/1753193409352285. [DOI] [PubMed] [Google Scholar]
- 29.Kholinne E., Kwak J.-M., Kim H., Sun Y., Koh K.-H., Jeon I.-H. Osteochondral reconstruction for post-traumatic coronoid deficiency. J Orthop Surg Hong Kong. 2020;28 doi: 10.1177/2309499020968606. [DOI] [PubMed] [Google Scholar]
- 30.Kim B.-S., Kim D.-H., Byun S.-H., Cho C.-H. Does the coronoid always need to Be fixed in terrible triad injuries of the elbow? Mid-term Postoperative outcomes following a standardized protocol. J Clin Med. 2020;9:E3500. doi: 10.3390/jcm9113500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Klerk H.H., Oosterhoff J.H.F., Schoolmeesters B., Nieboer P., Eygendaal D., Jaarsma R., et al. Recognition of the pattern of complex fractures of the elbow using 3D-printed models. Bone Joint J. 2023;105-B:56–63. doi: 10.1302/0301-620X.105B1.BJJ-2022-0415.R2. [DOI] [PubMed] [Google Scholar]
- 32.Klug A., Buschbeck S., Gramlich Y., Buckup J., Hoffmann R., Schmidt-Horlohé K. Good outcome using anatomically pre-formed buttress plates for anteromedial facet fractures of the coronoid-a retrospective study of twenty-four patients. Int Orthop. 2019;43:2817–2824. doi: 10.1007/s00264-019-04354-6. [DOI] [PubMed] [Google Scholar]
- 33.Lanzerath F., Hackl M., Wegmann K., Müller L.P., Leschinger T. The treatment of anteromedial coronoid facet fractures: a systematic review. J Shoulder Elbow Surg. 2021;30:942–948. doi: 10.1016/j.jse.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 34.Lee H.-D., Jung Y.-J., Oh J.-K., Moon J.-G. Morphological characteristics of fractures of the anteromedial facet of the coronoid in posteromedial rotatory instability of the elbow: a three-dimensional CT remodeling study. J Shoulder Elbow Surg. 2021;30:1527–1536. doi: 10.1016/j.jse.2020.09.040. [DOI] [PubMed] [Google Scholar]
- 35.Lindenhovius A., Karanicolas P.J., Bhandari M., van Dijk N. Ring D, Collaboration for Outcome Assessment in Surgical Trials. Interobserver reliability of coronoid fracture classification: two-dimensional versus three-dimensional computed tomography. J Hand Surg. 2009;34:1640–1646. doi: 10.1016/j.jhsa.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 36.Lowery M., Massey P. StatPearls Publishing; Treasure Island (FL): 2022. Coronoid fractures in: StatPearls.http://www.ncbi.nlm.nih.gov/books/NBK544236/ [cited 2022 Sep 27]. Available from: [Google Scholar]
- 37.Manocha R.H.K., Banayan S., Johnson J.A., King G.J.W. Overhead arm positioning in the rehabilitation of elbow dislocations: an in vitro biomechanical study. J Hand Ther. 2022;35:245–253. doi: 10.1016/j.jht.2022.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Mathew P.K., Athwal G.S., King G.J.W. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009;17:137–151. doi: 10.5435/00124635-200903000-00003. [DOI] [PubMed] [Google Scholar]
- 39.McKee M.D., Pugh D.M.W., Wild L.M., Schemitsch E.H., King G.J.W. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Surgical technique. J Bone Joint Surg. Am. 2005;87 Suppl 1:22–32. doi: 10.2106/JBJS.D.02933. [DOI] [PubMed] [Google Scholar]
- 40.McKee M.D., Schemitsch E.H., Sala M.J., O’driscoll S.W. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg. 2003;12:391–396. doi: 10.1016/s1058-2746(03)00027-2. [DOI] [PubMed] [Google Scholar]
- 41.McLean J., Kempston M.P., Pike J.M., Goetz T.J., Daneshvar P. Varus posteromedial rotatory instability of the elbow: injury pattern and surgical experience of 27 acute Consecutive surgical patients. J Orthop Trauma. 2018;32:e469–e474. doi: 10.1097/BOT.0000000000001313. [DOI] [PubMed] [Google Scholar]
- 42.Mehta J.A., Bain G.I. Surgical approaches to the elbow. Hand Clin. 2004;20:375–387. doi: 10.1016/j.hcl.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 43.Mellema J.J., Doornberg J.N., Dyer G.S.M., Ring D. Distribution of coronoid fracture lines by specific patterns of traumatic elbow instability. J Hand Surg. 2014;39:2041–2046. doi: 10.1016/j.jhsa.2014.06.123. [DOI] [PubMed] [Google Scholar]
- 44.Mensel C., Gundtoft P.H., Brink O. Preoperative templating in orthopaedic fracture surgery: the past, present and future. Injury. 2022;53:S42–S46. doi: 10.1016/j.injury.2022.09.005. [DOI] [PubMed] [Google Scholar]
- 45.Moon J.-G., Bither N., Jeon Y.-J., Oh S.-M. Non surgically managed anteromedial coronoid fractures in posteromedial rotatory instability: three cases with 2 years follow-up. Arch Orthop Trauma Surg. 2013;133:1665–1668. doi: 10.1007/s00402-013-1846-y. [DOI] [PubMed] [Google Scholar]
- 46.Morrey B.F., An K.-N. Stability of the elbow: osseous constraints. J Shoulder Elbow Surg. 2005;14:174S–178S. doi: 10.1016/j.jse.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 47.Ochtman A.E.A., Ring D. Combined posterior and medial plate fixation of complex proximal ulna fractures. Injury. 2012;43:254–256. doi: 10.1016/j.injury.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 48.O’Driscoll S.W., Jupiter J.B., Cohen M.S., Ring D., McKee M.D. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–134. [PubMed] [Google Scholar]
- 49.O’Driscoll S.W., Jupiter J.B., King G.J., Hotchkiss R.N., Morrey B.F. The unstable elbow. Instr Course Lect. 2001;50:89–102. [PubMed] [Google Scholar]
- 50.Oh W.-T., Do W.-S., Oh J.-C., Koh I.-H., Kang H.-J., Choi Y.-R. Comparison of arthroscopy-assisted vs. open reduction and fixation of coronoid fractures of the ulna. J Shoulder Elbow Surg. 2021;30:469–478. doi: 10.1016/j.jse.2020.06.037. [DOI] [PubMed] [Google Scholar]
- 51.Ott N., Harland A., Knevels M., Hackl M., Leschinger T., Lanzerath F., et al. The role of the brachialis muscle in elbow stability with collateral ligament injury: a biomechanical investigation. Clin Biomech Bristol Avon. 2021;89 doi: 10.1016/j.clinbiomech.2021.105478. [DOI] [PubMed] [Google Scholar]
- 52.Papatheodorou L.K., Rubright J.H., Heim K.A., Weiser R.W., Sotereanos D.G. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop. 2014;472:2084–2091. doi: 10.1007/s11999-014-3471-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pollock J.W., Pichora J., Brownhill J., Ferreira L.M., McDonald C.P., Johnson J.A., et al. The influence of type II coronoid fractures, collateral ligament injuries, and surgical repair on the kinematics and stability of the elbow: an in vitro biomechanical study. J Shoulder Elbow Surg. 2009;18:408–417. doi: 10.1016/j.jse.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 54.Ramirez M.A., Stein J.A., Murthi A.M. Varus posteromedial instability. Hand Clin. 2015;31:557–563. doi: 10.1016/j.hcl.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 55.Reichel L.M., Milam G.S., Reitman C.A. Anterior approach for operative fixation of coronoid fractures in complex elbow instability. Tech Hand Up Extrem Surg. 2012;16:98–104. doi: 10.1097/BTH.0b013e31824e6a74. [DOI] [PubMed] [Google Scholar]
- 56.Rhyou I.H., Kim K.C., Lee J.-H., Kim S.Y. Strategic approach to O’Driscoll type 2 anteromedial coronoid facet fracture. J Shoulder Elbow Surg. 2014;23:924–932. doi: 10.1016/j.jse.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 57.Ring D. Fractures of the coronoid process of the ulna. J Hand Surg. 2006;31:1679–1689. doi: 10.1016/j.jhsa.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 58.Ring D., Horst T.A. Coronoid fractures. J Orthop Trauma. 2015;29:437–440. doi: 10.1097/BOT.0000000000000326. [DOI] [PubMed] [Google Scholar]
- 59.Ring D., Jupiter J.B., Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg. Am. 2002;84:547–551. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 60.Sanchez-Sotelo J., O’Driscoll S.W., Morrey B.F. Medial oblique compression fracture of the coronoid process of the ulna. J Shoulder Elbow Surg. 2005;14:60–64. doi: 10.1016/j.jse.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 61.Seijas R., Ares-Rodriguez O., Orellana A., Albareda D., Collado D., Llusa M. Terrible triad of the elbow. J Orthop Surg Hong Kong. 2009;17:335–339. doi: 10.1177/230949900901700319. [DOI] [PubMed] [Google Scholar]
- 62.Smith M.V., Lamplot J.D., Wright R.W., Brophy R.H. Comprehensive review of the elbow physical examination. J Am Acad Orthop Surg. 2018;26:678–687. doi: 10.5435/JAAOS-D-16-00622. [DOI] [PubMed] [Google Scholar]
- 63.Syed H., Cameron P., Phadnis J. Management of anteromedial coronoid fractures according to a protocol focused on instability assessment provides good outcomes with infrequent need for coronoid fixation. J Shoulder Elbow Surg. 2021;30:894–905. doi: 10.1016/j.jse.2020.07.038. [DOI] [PubMed] [Google Scholar]
- 64.Taylor T.K., Scham S.M. A posteromedial approach to the proximal end of the ulna for the internal fixation of olecranon fractures. J Trauma. 1969;9:594–602. doi: 10.1097/00005373-196907000-00004. [DOI] [PubMed] [Google Scholar]
- 65.Toros T., Ozaksar K., Sügün T.S., Kayalar M., Bal E., Ada S. The effect of medial side repair in terrible triad injury of the elbow. Acta Orthop Traumatol Turc. 2012;46:96–101. doi: 10.3944/AOTT.2012.2632. [DOI] [PubMed] [Google Scholar]
- 66.Viveen J., Perilli E., Zahrooni S., Jaarsma R.L., Doornberg J.N., Bain G.I. Three-dimensional cortical and trabecular bone microstructure of the proximal ulna. Arch Orthop Trauma Surg. 2021;143(1):213–223. doi: 10.1007/s00402-021-04023-7. [DOI] [PubMed] [Google Scholar]
- 67.Watts A.C., Singh J., Elvey M., Hamoodi Z. Current concepts in elbow fracture dislocation. Shoulder Elbow. 2021;13:451–458. doi: 10.1177/1758573219884010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wegmann K., Knowles N.K., Lalone E.E., Hackl M., Müller L.P., King G.J.W., et al. The shape match of the olecranon tip for reconstruction of the coronoid process: influence of side and osteotomy angle. J Shoulder Elbow Surg. 2019;28:e117–e124. doi: 10.1016/j.jse.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 69.Yasui Y., Uesugi A., Kataoka T., Kuriyama K., Hamada M. Reconstruction of the coronoid process using a costal osteochondral autograft for acute comminuted coronoid fracture: a case report. J Shoulder Elbow Surg. 2018;27:e167–e171. doi: 10.1016/j.jse.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 70.Zhang H.-L., Lin K.-J., Lu Y. Prediction of the size of the fragment in comminuted coronoid fracture using the contralateral side: an Analysis of Similarity of Bilateral ulnar coronoid morphology. Orthop Surg. 2020;12:1495–1502. doi: 10.1111/os.12780. [DOI] [PMC free article] [PubMed] [Google Scholar]