Abstract
Background
Pectoralis major (PM) tears have been shown to occur most frequently at the tendinous humeral insertion. However, no substantial updates on tear location have been published in 20 years or are based on relatively small sample sizes. The primary purpose of this study was to evaluate PM tear location based on magnetic resonance imaging (MRI). A secondary purpose was to evaluate agreement between MRI and intraoperative assessments of tear characteristics. We hypothesized that PM tears at the myotendinous junction (MTJ) occur at a higher rate than previously reported and that intraoperative and MRI assessments would demonstrate agreement in at least 80% of cases.
Materials and methods
An observational study of consecutive patients evaluated for a PM tear at a single institution between 2010 and 2022 was conducted. Patient demographics as well as MRI and intraoperative assessments of tear location, extent of tear, and muscle head involvement were collected from the electronic medical record. Agreement was calculated by comparing radiographic and intraoperative assessments per variable and reported as percentages. Data and statistical analysis were performed with SPSS software with a significance level set to P < .05.
Results
A total of 102 patients were included for analysis. Mean age was 35.8 ± 10.5 years and mean body mass index was 29.4 ± 4.8 kg/m2. 60.4% of the study population had tears of the MTJ, 34.9% of the tendinous humeral insertion, and 4.7% within the muscle belly, as determined intraoperatively. Complete tears had significantly higher agreement between MRI and intraoperative assessments relative to partial tears (83.9% and 62.5%, respectively; P ≤ .01).
Discussion
The majority of PM tears occurred at the MTJ. Preoperative MRI and intraoperative assessments agreed in 80% of cases, a value that was significantly higher for complete over partial tears. These findings demonstrate that tears of the MTJ are increasingly more common and support the use of MRI in preoperative planning for complete PM tears.
Keywords: Pectoralis major tears, Myotendinous junction, Magnetic resonance imaging, Clavicular head, Sternal head, Weightlifting, Preoperative planning
Pectoralis major (PM) tears are uncommon injuries that most frequently occur in young, active males and result in significant pain, weakness, and deformity.6,7,19 Historically, PM tears have been reported as work-related or trauma-related injuries.11,14,18,22 However, an increase in incidence of PM tendon tears in the past 2 decades has been seen with the increase in professional and recreational athletes participating in weightlifting and high-energy sports.7,14,18 These activities have been found to put the PM under maximum tension and stretch.3,4,14,18 Weightlifting movements, such as the bench press, place the shoulder in full extension and external rotation while pressing against significant forces in an anterior-to-posterior direction.18,21 Excessive tension on the maximally contracted PM muscle results in a higher proportion of tears occurring at or near the myotendinous junction (MTJ).2,17,24
PM tears can occur at the insertion site of the tendon on the humerus, within the tendon, at the MTJ, or within the muscle belly.6,14 These tears can be classified as full or partial thickness. Existing literature has described the complexity of the PM myotendinous anatomy and how it is commonly misinterpreted as tearing off the tendinous humeral insertion.8,9 Given that the PM consists of multilaminar muscle segments and a bilaminar tendon, cadaveric studies on PM anatomy have demonstrated inconsistencies in the number of muscle layers.9,12,24 This complexity of the myotendinous anatomy makes detailed assessment of PM tears challenging.6 Moreover, the pectoralis muscle (PM) exhibits variations in absolute fiber lengths, which enable a range of shortening velocities within the muscle.24 Studies on cadaveric specimens have reported that the fiber lengths in the clavicular head (CH) have a mean of 15.0 ± 0.8 cm, with longer fibers extending from superior to inferior regions. Conversely, the sternal head (SH) has a mean fiber length of 16.4 ± 1.2 cm, with the longest fibers located in the middle segments. In addition, the CH comprises 19% of the total PM volume, with a mean muscle volume of 55 ± 8 cm3, while the SH constitutes 81% of the PM volume, with a mean volume of 228 ± 61 cm3.9,24 Measurement of the mean distance from the superior to inferior aspect of the humeral footprint revealed that the SH insertion of the PM tendon was located at a distance of 42.1 mm, while the CH insertion was located at a mean distance of 56.6 mm.10 At the level of the MTJ, the 2 heads were fused, and the CH insertion was found to be longer than the SH insertion, measuring 56.6 mm and 42.1 mm, respectively. Additionally, a tendon overlap footprint length of 27.9 mm was observed.10
Magnetic resonance imaging (MRI) is the most commonly used imaging modality for diagnosis and preoperative evaluation of PM tears, providing surgeons with important information on presence, extent, and location of PM tears.14,18,19,22 Clinical management of PM tears is driven by tear characteristics. Existing literature on tear location shows the majority are of the tendinous insertion on the humerus.1,8,14 However, these studies have not been substantially updated in more than 20 years or are based on relatively small sample sizes and consequently may not accurately describe current tear pattern morphologies given the rapidly changing physical activity preferences in the general population.11,14,25 The primary objective of this study was to evaluate the location of PM tears. A secondary objective of this study was to determine the degree of agreement between MRI and intraoperative assessments of tear characteristics. We hypothesized that PM tears at the MTJ occur at a higher rate than previously reported and that intraoperative and MRI assessments would demonstrate agreement in at least 80% of cases.
Methods
Study design
An observational study of consecutive patients undergoing evaluation of PM tears at a single institution between 2010 and 2022 was conducted. Institutional review board approval was obtained (STUDY19030196); data were collected from the electronic medical record (EMR) and entered into an institutional REDCap database (UL1-TR-001857). Initially, the EMR was queried for all patients being evaluated for a PM tear and treated either operatively or nonoperatively by 7 fellowship-trained sports medicine orthopedic surgeons between 2010 and 2022. Patients were eligible for inclusion if they received a formal diagnosis of having a primary PM tear confirmed by MRI imaging. Radiographic confirmation was defined as having a PM tear diagnosed on MRI with a corresponding radiology report. Subjects were excluded if they had ipsilateral upper extremity injury or were missing an MRI report detailing tear characteristics per Tietjen classification in the EMR (Table I).6,23 Agreement was determined by comparing MRI imaging and intraoperative assessments per variable and reported as percentages for subjects who underwent operative treatment. Only patients undergoing operative treatment were included in the MRI v intraoperative assessment analysis (n = 71). Patients undergoing nonoperable treatment were included in the analysis of tear location as determined by MRI (n = 31). Reasons for nonoperative management were successful trial of nonoperative management, lost to follow-up, nonoperable tear, or related to significant comorbidities. Successful trial of nonoperative management was defined as return to preinjury activity following completion of physical therapy. This consisted of an initial period of immobilization for 1-2 weeks, followed by passive shoulder range of motion, followed by isometric motions of the glenohumeral and scapulothoracic joints, and then transitioned to active range of motion beginning until 8 to 12 weeks postinjury, depending on individual progression. Loading and strengthening was then initiated at 12 weeks postinjury and rehabilitation continued until individuals were able to return to their previous level of activity without restriction. Nonoperable tears were tears deemed nonoperable given chronicity, difficult location of tear, or individual’s activity level and expectations. Two cases were managed nonoperatively due to significant comorbidities, one related to poorly controlled diabetes mellitus and another related to extensive psychiatric illness.
Table I.
PM tear classification∗.
| Extent of tear | |
| Grade I | Contusion or sprain |
| Grade II | Partial tear |
| Grade III | Complete tear |
| Location of tear | |
| A | Muscle origin |
| B | Muscle belly |
| C | Myotendinous junction |
| D | Muscle tendon |
PM, pectoralis major.
The above classification system was based on Tietjen et al.23
Data sources
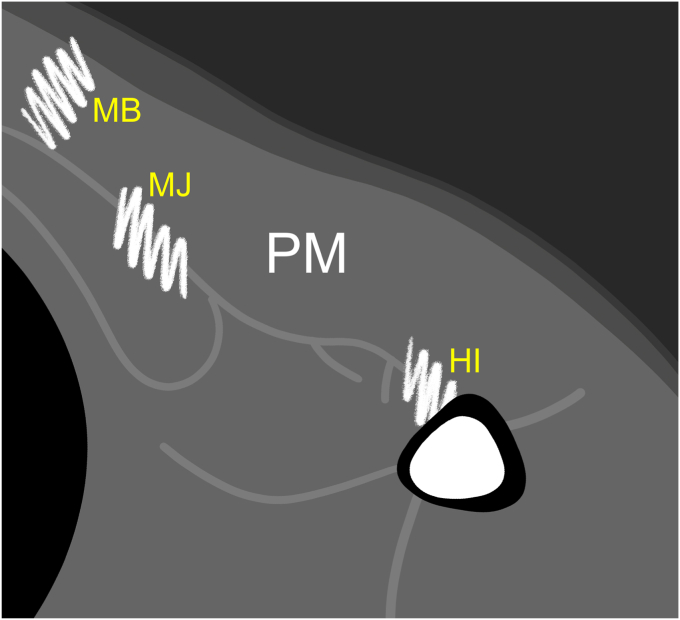
Patient demographics including surgeon, patient age, sex, body mass index, mechanism of injury, and risk factors were obtained from the EMR. Risk factors analyzed included anabolic steroid use, any prior upper extremity surgery, and smoking tobacco. PM tear characteristics were characterized by board-certified musculoskeletal radiologists during preoperative assessment. Intraoperative findings were collected from the orthopedic surgeon’s operative report. Tear characteristics, including tear location, extent of tear, and muscle head involvement were recorded. PM tear location and extent of tear were analyzed according to Tietjen classification (Table I). PM tear locations were described as tears of the insertion of the humerus, MTJ, muscle belly, or other (Fig. 1). Extent of tear was categorized according to MRI reports with grade II (G2) or partial-thickness tears classified as partial tears and grade III (G3) or full-thickness tears classified as complete tears.6,23 PM muscle head involvement was classified as involving the SH, CH, or both sternal and CHs. Intraoperative assessment was considered the gold standard for determining PM tear characteristics.
Figure 1.
MRI pectoralis major tear locations. HI depicts PM avulsion tear of the humeral insertion. MJ depicts PM tear within the myotendinous junction. MB depicts tear within PM muscle belly. PM, pectoralis major.
Imaging studies consisted of routine MRI studies performed on 1.5-T MRI scanners. MRI units included Siemens Espree and Avanto wide bore units using the Syngo MR B19 software package (Siemens Medical Solutions, Malvern, PA, USA) and General Electric 450 wide bore and GE Signa units using the DV24.0 software package (General Electric Medical Systems, Milwaukee, WI, USA). Sequence design is standardized across the University of Pittsburgh Medical Center facilities selected. The routine MRI protocol consists of the following sequences: Axial T1 (5.00 mm thk; 6.00 sp), Axial T2 (5.00 mm thk; 6.00 sp), fat-suppressed T2 (5.00 mm thk; 6.00 sp), sagittal T1 (5.00 mm thk; 6.00 sp), fat suppressed T2 (5.00 mm thk; 6.00 sp), coronal T1 (4.00 mm thk; 4.16 sp), and fat-suppressed T2 (4.00 mm thk; 4.16 sp).
Statistical analysis
Demographic and clinical characteristics, as well as radiographic measurements, were presented with means and standard deviations for normally distributed continuous variables. Categorical and nominal variables were presented as percentages. PM tear agreement was calculated by comparing radiographic tear characteristics to intraoperative assessments per variable and was reported as percentages. Differences between categorical or nominal variables between groups were tested with chi-squared or Fisher’s exact tests. Data and statistical analysis were performed with SPSS Statistics (Version 27.0.1.0; SPSS IBM Corp., Armonk, NY, USA). All analyses were conducted using SPSS software with a significance level set to P < .05.
Results
Demographic and baseline characteristics
A total of 207 patients were evaluated for a PM tear, with 102 patients found to have MRI-confirmed PM tears included for analysis. The remaining 105 patients were excluded from analysis, as 99 did not have a confirmed PM tear as evaluated with MRI and 6 were missing a formal MRI report. Of the 102 patients included for analysis, 71 underwent operative management, while 31 were managed nonoperatively. The mean age was 35.8 ± 10.5 years (range: 20-45), 100 (98.1%) were male, and the mean body mass index was 29.4 ± 4.8 kg/m2. The most common mechanism of injury was weightlifting (66.7%), followed by trauma (17.6%), sport-related injury (10.8%), and manual labor (4.9%). Five (4.8%) patients confirmed active anabolic steroid use, 11 (10.6%) had prior upper extremity surgery, and 6 (5.8%) were current tobacco smokers. Reasons for nonoperative management were successful trial of nonoperative management (21, 67.7%), lost to follow-up (4, 12.9%), nonoperable tear (4, 12.9%), and comorbidities (2, 6.5%).
Regarding tear location, 60.4% of the entire study population had tears of the MTJ, 34.9% of the tendinous insertion on the humerus, and 4.7% within the muscle belly. A complete PM tear was present in 63.7% of patients and a partial tear was present in 36.3% of patients. Tears of the sternal muscle head occurred in 81.4% of patients and of both the sternal and clavicular muscle heads in 18.6% of patients (Table II). In patients managed operatively, 60.6% had complete SH tears, 18.3% had partial SH tears, 18.3% had complete sternal and CH tears, and 2.8% had partial sternal and CH tears (Table II).
Table II.
Pectoralis major tear characteristics as assessed with magnetic resonance imaging.
| Tear characteristic | Total no. of tears | Operative tears | Nonoperative tears | Overall percentage∗ (%) |
|---|---|---|---|---|
| Muscle head | ||||
| Sternal | 83 | 56 | 27 | 81.4 |
| Sternal + clavicular | 19 | 15 | 4 | 18.6 |
| Extent of tear | ||||
| Complete | 65 | 56 | 9 | 63.7 |
| Partial | 37 | 15 | 22 | 36.3 |
| Tear location | ||||
| Insertion on humerus | 37 | 30 | 7 | 34.9 |
| Myotendinous junction | 64 | 39 | 25 | 60.4 |
| Muscle belly | 5 | 2 | 3 | 4.7 |
| Other | 0 | 0 | 0 | 0.9 |
Denotes percentage of tear characteristic compared to total number of patient tears per category.
Analysis of agreement between MRI and intraoperative assessments revealed significantly higher agreement for complete tears compared to partial tears (83.9% and 62.5%, respectively; P < .01). Complete tears of the SH had a significantly higher rate of agreement than complete tears of the sternal and CHs (81.4% and 46.2%, respectively; P = .01). Partial tears of the SH demonstrated 53.8% agreement between MRI and intraoperative assessments, while partial tears of the sternal and CHs had a 0% agreement (P = .47). Complete tears of the insertion on the humerus had higher agreement compared to complete tears of the MTJ (80.0% and 70.0%, respectively; P = .40). Overall, there was 83.0% agreement on tear location, 78.9% agreement on whether the tear was complete or partial, and 80.2% agreement on muscle head involvement between MRI and intraoperative assessments (Table III).
Table III.
Agreement between MRI and intraoperative assessments of pectoralis major tears.
| Tear characteristic` | No. of tears | Percentage (%) | Agreement∗ (%) | P value |
|---|---|---|---|---|
| Complete | 56 | 78.9 | 83.9 | < .01 |
| Partial | 15 | 21.1 | 60.0 | |
| Complete, sternal head | 43 | 60.6 | 81.4 | .01 |
| Complete, sternal + clavicular heads | 13 | 18.3 | 46.2 | |
| Partial, sternal head | 13 | 18.3 | 53.8 | .47 |
| Partial, sternal + clavicular heads | 2 | 2.8 | 0 | |
| Complete, humeral insertion site | 25 | 35.2 | 80 | .40 |
| Complete, myotendinous junction | 30 | 42.3 | 70 |
MRI, magnetic resonance imaging.
Significance is denoted in bold.
Denotes percentage agreement between MRI, radiographs, and intraoperative findings.
Discussion
The most important finding of this study is that PM tears are predominantly of the MTJ. In addition, strong agreement between preoperative MRI and intraoperative assessments was observed, a value that was significantly higher for complete compared to partial tears, which corroborates existing literature.6
One explanation for the increased incidence of PM tears of the MTJ relates to the increasing number of weightlifting injuries. Studies have shown that mechanism of injury does not impact extent of tear but rather affects tear location.5,22 In a study of military personnel with PM tears, those who experienced high-energy traumatic mechanisms of injury had a higher rate of avulsion tears of the insertion on the humerus.22 The present study supports prior studies demonstrating increased susceptibility of PM tears of the sternal division due to its short length and increased angle of attachment.8,22 When the shoulder is placed at 30 degrees of extension, the sternal muscle fibers demonstrate twice as much stretch compared to other PM fibers.22,24 This may explain why excessive eccentric loading during weightlifting with the shoulder abducted and externally rotated, such as when performing bench press, is one of the most common mechanisms of injury resulting in PM tears.10,16,22
When operative management of PM tears is indicated, careful consideration of tear characteristics is needed.3,6,13 Operative management has been shown to result in superior outcomes for complete and high-grade partial tears, while low-grade partial tears may be successfully managed nonoperatively.6,25 However, the sensitivity of MRI at identifying PM tears varies, with reported values between 67% and 100% depending on chronicity, location, and extent of the tear.6,22 This is especially true of PM tears of the MTJ, as these often confer increased operative complexity compared to tears of the insertion into the humerus.14,16 Operative management of tears of the humeral insertion site is relatively more straightforward, commonly involving cortical buttons, suture anchors, or bone tunnels as their location allows for direct reattachment to its native footprint.14,16 However, these techniques have limited use for more proximal injuries of the MTJ as these tears commonly result in substantial tendon retraction and tissue loss, preventing adequate reattachment to the footprint or potentially requiring graft reconstruction for extra length before subsequent reattachment to the humerus can be attained.13, 14, 15, 16 Recently, a novel technique for Achilles tendon allograft supplementation was described, citing larger graft size and superior biomechanical strength as advantages.20 In the present study, no difference was observed in the proportion undergoing allograft supplementation between those with MTJ and humeral avulsions tears, respectively (P = .680). Future studies are needed to discern whether the use of allograft supplementation influences clinical outcomes following MTJ and humeral avulsion tears. Notably, it has been shown to be difficult to distinguish between the MTJ and humeral insertion site in cadaveric studies which identified the distance between the 2 to be relatively short (< 5 cm).8,9 Given the relatively short tendinous insertion of the SH on the humerus, operative management of MTJ vs. humeral avulsion tears is unlikely to differ. While the present study is not geared toward assessing whether MTJ vs. humeral avulsion PM tears require different management strategies, this study reveals an increase in prevalence of MTJ tears. Nevertheless, accurate identification of PM tear patterns with MRI informs the surgeon and allows for more informed consideration of various operative approaches.
While changes in physical activities are likely the main driver for the increase in PM tears of the MTJ, difficulties in characterizing tears with MRI also contribute to a disproportionate number of PM tears reported at the humeral insertion site.8,9,12,24 A recent study found MRI to have a sensitivity of 93% at identifying tears of the SH bone-tendon junction but only 80% sensitivity at identifying tears of the MTJ.6 Additionally, MRI may be more accurate for complete tears, with a reported sensitivity of 100% for identifying complete tears of both sternal and CHs, compared to 80% and 67% sensitivity for partial tears of the sternal and CHs, respectively.6 The present study demonstrates that MRI can reliably detect complete tears but is significantly less accurate at detecting partial tears. This may reflect the pectoralis anatomy having bilaminar tendon layers and the inability of MRI to distinguish between these layers.8 Additionally, acute, complete tears are more easily visualized with MRI due to larger areas of soft-tissue edema, hematoma, or retraction.8,14 However, there may be utility in using MRI for preoperative planning for partial SH tears but not partial sternal and CH tears.3,6 In this investigation, MRI detected partial tears of the SH more accurately than partial tears of the sternal and CHs.
The present study is not without limitations. This study is retrospective in nature and consequently, acquisition and interpretation of MRI was not standardized. However, all cases followed the Tietjen classification and included relevant tear characteristics in the corresponding radiology report. Although this may affect the consistency of MRI-reported tear characteristics, intraoperative confirmation was used as the gold standard. Intraobserver and interobserver correlation coefficients were not feasible for the present study and the absence of this analysis represents a limitation. However, to ensure consistency and homogeneity in the MRI data, we employed the same MRI sequence and protocols for all MRIs and relied exclusively on musculoskeletal-trained radiologists for the image interpretation. Additionally, the present study lacks assessment of patient outcomes as it was out of the scope of the study’s purpose. Future studies incorporating patient-reported outcomes, measures of strength and range of motion, and complications are needed to investigate whether specific tear patterns correlate with clinical outcomes. Additionally, the increase in PM tears of the MTJ secondary to weightlifting warrants investigation of MRI protocols needed to distinguish between tears of the MTJ and humeral insertion site, particularly in the setting of partial tears.
Conclusion
This investigation demonstrated that PM tears are predominantly of the MTJ. Preoperative MRI was in agreement with intraoperative assessment in 80% of cases, a value that was significantly higher for complete tears than partial tears. These findings demonstrate that tears of the MTJ are increasingly more common and support the use of MRI in preoperative planning for complete PM tears.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: Dr. Lin discloses personal fees from Stryker and personal fees from Arthrex, Inc., outside the submitted work. Dr. Lesniak discloses personal fees from Wolters Kluwer Health- Lippincott Williams & Wilkins, outside the submitted work. The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
This study was approved by the local ethical committee (University of Pittsburgh Institutional Review Board; STUDY20030061).
Investigation performed by The Pittsburgh Shoulder Institute.
References
- 1.Bak K., Cameron E.A., Henderson I.J. Rupture of the pectoralis major: a meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc. 2000;8:113–119. doi: 10.1007/s001670050197. [DOI] [PubMed] [Google Scholar]
- 2.Berson B.L. Surgical repair of pectoralis major rupture in an athlete. Case report of an unusual injury in a wrestler. Am J Sports Med. 1979;7:348–351. doi: 10.1177/036354657900700608. [DOI] [PubMed] [Google Scholar]
- 3.Butt U., Mehta S., Funk L., Monga P. Pectoralis major ruptures: a review of current management. J Shoulder Elbow Surg. 2015;24:655–662. doi: 10.1016/j.jse.2014.10.024. [DOI] [PubMed] [Google Scholar]
- 4.de Castro Pochini A., Andreoli C.V., Belangero P.S., Figueiredo E.A., Terra B.B., Cohen C., et al. Clinical considerations for the surgical treatment of pectoralis major muscle ruptures based on 60 cases: a prospective study and literature review. Am J Sports Med. 2014;42:95–102. doi: 10.1177/0363546513506556. [DOI] [PubMed] [Google Scholar]
- 5.Chan A.G., Balazs G.C., Haley C.A., Posner M.A., Rue J.H., Owens B.D. Pectoralis major rupture in military Academy athletes. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119860157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang E.S., Zou J., Costello J.M., Lin A. Accuracy of magnetic resonance imaging in predicting the intraoperative tear characteristics of pectoralis major ruptures. J Shoulder Elbow Surg. 2016;25:463–468. doi: 10.1016/j.jse.2015.08.037. [DOI] [PubMed] [Google Scholar]
- 7.Connell D.A., Potter H.G., Sherman M.F., Wickiewicz T.L. Injuries of the pectoralis major muscle: evaluation with MR imaging. Radiology. 1999;210:785–791. doi: 10.1148/radiology.210.3.r99fe43785. [DOI] [PubMed] [Google Scholar]
- 8.ElMaraghy A.W., Devereaux M.W. A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg. 2012;21:412–422. doi: 10.1016/j.jse.2011.04.035. [DOI] [PubMed] [Google Scholar]
- 9.Fung L., Wong B., Ravichandiran K., Agur A., Rindlisbacher T., Elmaraghy A. Three-dimensional study of pectoralis major muscle and tendon architecture. Clin Anat. 2009;22:500–508. doi: 10.1002/ca.20784. [DOI] [PubMed] [Google Scholar]
- 10.Ganokroj P., Midtgaard K., Elrick B.P., Dey Hazra R.O., Douglass B.W., Nolte P.C., et al. Qualitative and Quantitative anatomy of the humeral attachment of the pectoralis major muscle and structures at risk: a cadaveric study. Orthop J Sports Med. 2022;10 doi: 10.1177/23259671221121333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupton M., Johnson J.E. Surgical treatment of pectoralis major muscle ruptures: a systematic review and meta-analysis. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967118824551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee J., Brookenthal K.R., Ramsey M.L., Kneeland J.B., Herzog R. MR imaging assessment of the pectoralis major myotendinous unit: an MR imaging-anatomic correlative study with surgical correlation. AJR Am J Roentgenol. 2000;174:1371–1375. doi: 10.2214/ajr.174.5.1741371. [DOI] [PubMed] [Google Scholar]
- 13.Long M., Enders T., Trasolini R., Schneider W., Cappellino A., Ruotolo C. Pectoralis major tendon reconstruction using semitendinosus allograft following rupture at the musculotendinous junction. JSES Open Access. 2019;3:328–332. doi: 10.1016/j.jses.2019.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Magone K., Ben-Ari E., Gyftopoulos S., Virk M. Pectoralis major tendon tear: a critical analysis review. JBJS Rev. 2021;9:1–12. doi: 10.2106/JBJS.RVW.20.00224. [DOI] [PubMed] [Google Scholar]
- 15.Metzger P.D., Bailey J.R., Filler R.D., Waltz R.A., Provencher M.T., Dewing C.B. Pectoralis major muscle rupture repair: technique using unicortical buttons. Arthrosc Tech. 2012;1:e119–e125. doi: 10.1016/j.eats.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noufal A. A case report of a rupture of the musculotendinous junction of the pectoralis major in an athlete. Int J Surg Case Rep. 2021;87 doi: 10.1016/j.ijscr.2021.106428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park J.Y., Espiniella J.L. Rupture of pectoralis major muscle. A case report and review of literature. J Bone Joint Surg Am. 1970;52:577–581. [PubMed] [Google Scholar]
- 18.Petilon J., Carr D.R., Sekiya J.K., Unger D.V. Pectoralis major muscle injuries: evaluation and management. J Am Acad Orthop Surg. 2005;13:59–68. doi: 10.5435/00124635-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Provencher M.T., Handfield K., Boniquit N.T., Reiff S.N., Sekiya J.K., Romeo A.A. Injuries to the pectoralis major muscle: diagnosis and management. Am J Sports Med. 2010;38:1693–1705. doi: 10.1177/0363546509348051. [DOI] [PubMed] [Google Scholar]
- 20.Rivera P., Dhytadak D., Cunningham G. Reconstruction of chronic, retracted pectoralis major tendon tear with achilles tendon allograft. Arthrosc Tech. 2023;12:e449–e452. doi: 10.1016/j.eats.2022.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schepsis A.A., Grafe M.W., Jones H.P., Lemos M.J. Rupture of the pectoralis major muscle. Outcome after repair of acute and chronic injuries. Am J Sports Med. 2000;28:9–15. doi: 10.1177/03635465000280012701. [DOI] [PubMed] [Google Scholar]
- 22.Synovec J., Shaw K.A., Hattaway J., Wilson A.M., Chabak M., Parada S.A. Magnetic resonance imaging of pectoralis major injuries in an active duty military cohort: mechanism affects tear location. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120925019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tietjen R. Closed injuries of the pectoralis major muscle. J Trauma. 1980;20:262–264. doi: 10.1097/00005373-198003000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Wolfe S.W., Wickiewicz T.L., Cavanaugh J.T. Ruptures of the pectoralis major muscle. An anatomic and clinical analysis. Am J Sports Med. 1992;20:587–593. doi: 10.1177/036354659202000517. [DOI] [PubMed] [Google Scholar]
- 25.Zvijac J.E., Schurhoff M.R., Hechtman K.S., Uribe J.W. Pectoralis major tears: correlation of magnetic resonance imaging and treatment strategies. Am J Sports Med. 2006;34:289–294. doi: 10.1177/0363546505279573. [DOI] [PubMed] [Google Scholar]