Abstract
Background
Patients with diabetes mellitus who undergo arthroscopic rotator cuff repair (aRCR) have an increased risk of postoperative complications when compared to nondiabetics. To further investigate these complications, we used a large national database to determine the 30-day postoperative complications associated with insulin-dependent and non-insulin-dependent diabetics following aRCR.
Methods
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database was queried for all patients who underwent aRCR between 2015 and 2020. The study population was categorized into cohorts based on diabetes mellitus status: non-insulin-dependent diabetes mellitus (NIDDM), insulin-dependent diabetes mellitus (IDDM), and no diabetes. Multivariate analysis, adjusted for confounding demographics and comorbidities, was used to determine independently associated complications.
Results
There were 39,877 cases of aRCR in NQSIP included in this study. Diabetics comprised 6575 (16.7%) of these cases, with 4758 being NIDDM (11.9%) and 1817 being IDDM (4.6%). Bivariate logistic regression found both NIDDM and IDDM cohorts to be significantly associated with higher body mass index, ASA class ≥3, hypertension, chronic obstructive pulmonary disease, bleeding disorders, and preoperative wounds or infection (P < .001). NIDDM was an independently associated risk factor for sepsis (odds ratio [OR], 2.77; 95% confidence interval [CI]: 1.01-7.58; P = .047). IDDM was an independently associated risk factor for pneumonia (OR, 2.49; 95% CI: 1.13-5.48; P = .023), readmission (OR, 1.617; 95% CI: 1.19-2.33; P = .003), myocardial infarction (OR, 0.50; 95% CI: 0.12-1.00; P = .048), and on a ventilator >48 hours (OR, 5.63; 95% CI: 1.40-22.62; P = .015).
Conclusion
NIDDM is an independent risk factor for sepsis, while IDDM is an independent risk factor for pneumonia, readmission, myocardial infarction, and remaining on a ventilator for greater than 48 hours following aRCR.
Keywords: Diabetes, Shoulder arthroscopy, Rotator cuff repair, Complications, Insulin, Arthroscopic rotator cuff repair
The number of adults with diabetes in the United States is projected to almost triple in number and double in prevalence by 2060.14 Though a metabolic disease, diabetes produces profound systemic effects and is frequently associated with musculoskeletal disorders. These include disorders affecting the upper limb, such as adhesive capsulitis, rotator cuff tendinopathy, and limited joint mobility disorder.5,22,31
Rotator cuff tears and tendinopathies are among the most common causes of shoulder disabilities in diabetics.15 Rechardt et al23 noted that both diabetes types 1 and 2 were associated with greater occurrence of shoulder pain and rotator cuff tendinitis in the male population. Arthroscopic rotator cuff repair (aRCR) surgery presents a safe, effective, and less invasive option to restore function and limit pain. As such, the rates of aRCR have increased by 1.6% annually over the past decade.30 A study by Huang et al8 found that diabetes was an independent risk factor for the need for RCR surgeries. As diabetes may be a common comorbidity in patients undergoing aRCR, understanding the postoperative complications associated with diabetes can allow for better risk stratification and operative planning.
Although complications following aRCR are uncommon, the relationship between diabetes and postoperative complications following aRCR has been well described in the literature.2,4 A study by Borton et al2 found that diabetic patients were 2 times more likely to experience postoperative cuff retear. Another study by Cancienne et al3 correlated greater hemoglobin usually seen as A1C with a greater risk of infection following aRCR. To our knowledge, there are no large database investigations into the impact of diabetes on postoperative complications following aRCR. The goal of this study was to elucidate the postoperative complications associated with non-insulin-dependent diabetes mellitus (NIDDM) and insulin-dependent diabetes mellitus (IDDM) undergoing aRCR. We hypothesized that both NIDDM and IDDM were independent risk factors for postoperative complications.
Methods
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database provides patient medical chart information for preoperative, intraoperative, and 30-day postoperative outcomes. Over 600 hospitals contribute to the database, with data collected by trained surgical clinical reviewers who regularly maintain its reliability and confidentiality. The NSQIP database was used to build a retrospective cohort of all patients that underwent aRCR over a period of 2015-2020. An institutional review board exemption for this study was provided by our institution as NSQIP data are completely deidentified.
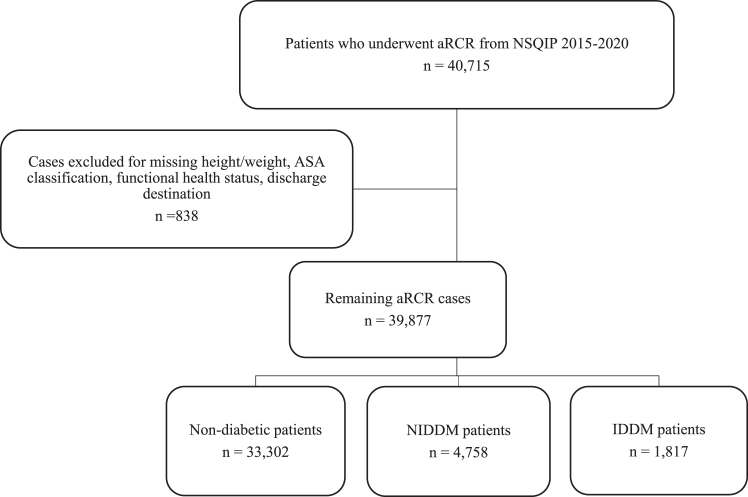
We identified aRCR procedure data using the Current Procedural Terminology (CPT) code 29287. The NSQIP database automatically excludes patients under the age of 18 years. A total of 40,715 patients who underwent aRCR between 2015 and 2020 were identified, of which 838 exclusions were made for the following missing data: discharge destination (n = 7), height or weight (n = 320), American Society of Anesthesiologists (ASA) classification (n = 56), and preoperative functional health status (n = 455). This yielded a total value of 39,877 patients, of which 33,302 were non-diabetic, 4758 (14.3%) were NIDDM, and 1817 (4.6%) were IDDM. (Fig. 1)
Figure 1.
Case selection schematic. aRCR, arthroscopic rotator cuff repair; NSQIP, National Surgical Quality Improvement Program; NIDDM, non-insulin-dependent diabetes mellitus; IDDM, insulin-dependent diabetes mellitus; ASA, American Society of Anesthesiologists.
The NSQIP database records whether patients are treated with insulin- or non-insulin-dependent methods. This allowed us to further substratify patients. NIDDM was used to describe diabetics utilizing therapy with non-insulin agents for a period longer than 2 weeks and within 30 days prior to surgery. IDDM was used to describe diabetics dependent on therapy requiring insulin agents with or without additional non-insulin agents. The non-diabetic population included non-diabetics and diabetics that did not require pharmacological therapy.
The data collected included the demographics, comorbidities, and 30-day postoperative complication data for each cohort. The patient demographics consisted of age, gender, body mass index (BMI), smoking status, ASA classification, preoperative functional status, and preoperative use of steroids. The preoperative comorbidities explored were hypertension, severe chronic obstructive pulmonary disease (COPD), open wounds or infection, disseminated cancer, bleeding disorders, progressive renal insufficiency/acute renal failure, and hospitalization prior to surgery.
The complications that occurred in the 30 days following operation were also analyzed. The complications were as follows: sepsis, septic shock, pneumonia, unplanned reintubation, urinary tract infection, stroke or cerebrovascular accident, cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, bleeding transfusions within the first 72 hours postoperation, deep vein thrombosis, pulmonary embolism, on a ventilator >48 hours, deep incisional surgical site infection (SSI), superficial incisional SSI, organ/space SSI, wound dehiscence, readmission, reoperation, nonhome discharge, mortality, and length of hospital stay greater than 2 days.
Statistical analyses were performed using SPSS Software (version 26.0; IBM Corp., Armonk, NY, USA). The patient demographics and comorbidities of NIDDM and IDDM were compared to the non-diabetic cohort using bivariate logistic regression. To determine whether diabetes was an independent risk factor for complications, multivariate logistic regression adjusted for all significantly associated patient demographics and comorbidities, was used to identify associations between NIDDM and IDDM and postoperative complications. Odds ratios (ORs) were reported with 95% confidence intervals (CIs). The level of statistical significance was set at P < .05.
Results
The most prevalent age group for those with NIDDM and IDDM undergoing aRCR was 60-69 years, comprising 39.7% and 40.1% of their cohorts, respectively. When compared to the nondiabetic cohort, NIDDM was significantly associated with older age groups (P < .001), BMI > 35 (P < .001), ASA classification ≥ 3 (P < .001), smoking status (P = .002), hypertension (P < .001), COPD (P < .001), bleeding disorders (P < .001), and preoperative wounds or infection (P < .001). Compared to the nondiabetic cohort, IDDM was significantly associated with greater BMI (P < .001), dependent functional status (P < .001), ASA classification ≥ 3 (P < .001), hypertension (P < .001), COPD (P < .001), bleeding disorders (P < .001), preoperative wounds or infection (P < .001), preoperative renal failure (P < .001), and hospitalization prior to surgery (P < .017). (Table I)
Table I.
Patient demographics and comorbidities for nondiabetics, noninsulindependent diabetics, and insulin-dependent diabetics.
| Normal (nondiabetic) |
NIDDM (non-insulin dependent) |
IDDM (insulin dependent) |
|||
|---|---|---|---|---|---|
| Number (%) | Number (%) | P value | Number (%) | P value | |
| Overall | 33,302 (100.0) | 4758 (100.0) | 1817 (100.0) | ||
| Sex | .702 | .092 | |||
| Female | 13,529 (40.6) | 1904 (40.0) | 775 (42.7) | ||
| Male | 19,762 (59.4) | 2854 (60.0) | 1042 (57.3) | ||
| Age, yr | <.001 | .986 | |||
| >50 | 7119 (21.4) | 444(9.3) | 208 (11.5) | ||
| 50-59 | 11,005 (33.0) | 1457 (30.6) | 574 (31.6) | ||
| 60-69 | 10,666 (32.0) | 1886 (39.7) | 729 (40.1) | ||
| ≥70 | 4152 (13.6) | 971 (20.4) | 305 (16.8) | ||
| BMI (kg/mˆ2) | <.001 | <.001 | |||
| <18.5 | 160 (0.5) | 10 (0.2) | 2 (0.1) | ||
| 18.5-29.9 | 17,956 (54.0) | 1518 (32.0) | 489 (26.9) | ||
| 30-34.9 | 8842(26.6) | 1548 (32.5) | 518 (28.5) | ||
| 35-39.9 | 3385 (10.2) | 953 (20.0) | 412 (22.7) | ||
| ≥40 | 2459 (7.4) | 729 (15.3) | 396 (21.8) | ||
| Functional status prior to surgery | .570 | <.001 | |||
| Independent | 33,203 (99.7) | 4470 (99.6) | 1791 (98.6) | ||
| Dependent | 99 (0.7) | 18 (0.4) | 26 (1.4) | ||
| ASA classification | <.001 | <.001 | |||
| ≤2 | 23,921 (71.8) | 1737 (36.5) | 422 (23.2) | ||
| ≥3 | 9381 (28.2) | 3021 (63.5) | 1395 (76.8) | ||
| Smoker | .002 | .457 | |||
| No | 29,324 (85.0) | 4127 (86.7) | 1557 (85.7) | ||
| Yes | 4978 (15.0) | 61 (13.3) | 260 (14.3) | ||
| Steroid use | .626 | .626 | |||
| No | 32,637 (98.0) | 4668 (98.1) | 1764 (97.1) | ||
| Yes | 665 (2.0) | 90 (1.9) | 53 (2.9) | ||
| Comorbidities | |||||
| Disseminated cancer | 18 (0.1) | 3 (0.1) | .805 | 1 (0.1) | .986 |
| Open wound/infection | 20 (0.1) | 11 (0.2) | <.0001 | 7 (0.4) | <.001 |
| HTN | 12,772 (38.4) | 3668 (77.1) | <.001 | 1479 (81.4) | <.001 |
| COPD | 838 (2.5) | 172 (3.6) | <.001 | 103 (5.7) | <.001 |
| Bleeding disorder | 373 (1.1) | 104 (2.2) | <.001 | 64 (3.5) | <.0001 |
| ARF | 1 (0.0) | 0 (0.0) | 1.000 | 3 (0.2) | <.001 |
| Hospitalization to operation (>1) | 98 (0.0) | 21 (0.0) | .056 | 11 (0.0) | .017 |
BMI, body mass index; ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease; HTN, Hypertension; ARF, acute renal failure.
Bold P values indicate statistical significance with P < .05.
Postoperative complications were compared between diabetic and nondiabetic cohorts (Table II). Compared to the nondiabetic cohort, NIDDM was significantly associated with sepsis (P = .005), unplanned reintubation (P = .027), cardiac arrest (P = .008), deep incisional SSI (P < .001), length of hospital stay greater than 2 days (P < .001), and readmission (P < .001). Compared to the nondiabetic cohort, IDDM was significantly associated with higher rates of pneumonia (P < .001), unplanned reintubation (P = .003), cardiac arrest (P = .040), myocardial infarction (P = .001), on a ventilator > 48 hours (P < .001), deep incisional SSI (P < .001), readmission (P < .001), nonhome discharge (P < .001), length of hospital stay greater than 2 days (P < .001), and mortality (P = .011).
Table II.
Bivariate analysis of 30-d postoperative complications in nondiabetic, non-insulindependent diabetic, and insulin-dependent diabetic patients.
| Normal (non-diabetic) |
NIDDM (non-insulin dependent) |
IDDM (insulin dependent) |
|||
|---|---|---|---|---|---|
| Number (%) | Number (%) | P value | Number (%) | P value | |
| Sepsis | 14 (0.0) | 7 (0.2) | .005 | 2 (0.1) | .172 |
| Septic shock | 2 (0.0) | 0 (0.0) | .999 | 1 (0.1) | .070 |
| Pneumonia | 39 (1.1) | 7 (0.2) | .578 | 9 (0.5) | <.001 |
| Reintubation | 7 (0.0) | 4 (0.1) | .027 | 3 (0.2) | .003 |
| Urinary tract infection | 60 (0.2) | 13 (0.3) | .173 | 6 (0.3) | .157 |
| Stroke | 9 (0.0) | 1 (0.0) | .811 | 0 (0.0) | .999 |
| Cardiac arrest | 9 (0.0) | 3 (0.1) | .008 | 1 (0.1) | .040 |
| Myocardial infarction | 18 (0.1) | 5 (0.1) | .188 | 5 (0.3) | .001 |
| Bleeding transfusions | 2 (0.0) | 1 (0.0) | .306 | 1 (0.1) | .07 |
| Deep vein thrombosis | 46 (0.1) | 8 (0.2) | .608 | 3 (0.2) | .764 |
| Pulmonary embolism | 58 (0.2) | 6 (0.1) | .451 | 2 (0.1) | .523 |
| Remaining on a ventilator > 48 h | 4 (0.0) | 1 (0.0) | .617 | 4 (0.2) | <.001 |
| Deep incisional SSI | 20 (0.0) | 11 (.2) | <.001 | 7 (0.4) | <.001 |
| Superficial incisional SSI | 44 (0.1) | 4 (0.1) | .386 | 3 (0.2) | .709 |
| Organ/space SSI | 12 (0.0) | 1 (0.0) | .604 | 1 (0.1) | .684 |
| Wound dehiscence | 5 (0.0) | 1 (0.0) | .758 | 0 (0.0) | .999 |
| Readmission | 284 (0.9) | 65 (1.4) | <.001 | 44 (2.4) | <.001 |
| Reoperation | 87 (0.3) | 9 (0.2) | .356 | 9 (0.05) | .067 |
| Nonhome discharge | 146 (0.4) | 25 (0.5) | .268 | 21 (1.2) | <.001 |
| Mortality | 4 (0.0) | 2 (0.0) | .148 | 2 (0.1) | .011 |
| Length of total hospital stay >2 d | 382 (0.0) | 103 (0.0) | <.001 | 49 (0.0) | <.001 |
SSI, surgical space infection.
Bold P values indicate statistical significance with P < .05.
After controlling for significant patient demographics and comorbidities, multivariate regression analysis identified complications independently associated with the NIDDM and IDDM compared to the nondiabetic cohort (Table III). NIDDM was an independent risk factor for sepsis (OR, 2.77; 95% CI: 1.01-7.58; P = .047). IDDM was an independent risk factor pneumonia (OR, 2.49; 95% CI: 1.13-5.48; P = .023), readmission (OR, 1.67; 95% CI: 1.21-2.33; P = .003), myocardial infarction (OR, 0.50; 95% CI: 0.12-1.00; P = .048), and on a ventilator > 48 hours (OR, 5.63; 95% CI: 1.40-22.62; P = .015).
Table III.
Multivariate analysis of 30-d postoperative complications in nondiabetic, noninsulin-dependent diabetic, and insulin-dependent diabetic patients.
| NIDDM (noninsulin dependent) |
IDDM (insulin dependent) |
|
|---|---|---|
| OR, P value (95% CI) | OR, P value (95% CI) | |
| Sepsis | 2.77, .047 (1.101-7.58) | - |
| Pneumonia | - | 2.49, .023 (1.13-5.48) |
| Reintubation | 2.15, .248 (0.59-7.82) | 2.90, .121 (0.75-11.17) |
| Deep incisional SSI | 1.58, .573 (0.32-7.70) | 1.36, .769 (0.16-11.50) |
| Readmission | 1.09, .562 (0.82-1.45) | 1.67, .003 (1.19-2.33) |
| Cardiac arrest | 0.10, .054 (0.10-1.04) | 0.505, .548 (0.05-4.68) |
| Nonhome discharge | - | 1.17, .539 (0.70-1.94) |
| Myocardial infarction | - | 0.50, .048 (0.12-1.00) |
| Remaining on a ventilator > 48 h | - | 5.63, .015 (1.40-22.62) |
| Mortality | - | 3.74, .132 (0.67-20.86) |
| Length of hospital stay > 2 d | 1.11, .417 (0.86-1.42) | 1.07, .708 (0.75-1.52) |
OR, odds ratio; CI, confidence interval; SSI, surgical space infection.
Bold P values indicate statistical significance with P < .05.
When comparing the significant comorbidities of IDDM patients with significant complications, we identified hypertension to be the most important factor in augmenting the rate of complications (Table IV). Of the IDDM patients with pneumonia, failure-to-wean off ventilator, and readmission, 60%, 20%, and 70%, respectively, had hypertension. The accumulation of comorbidities did not further augment their risk.
Table IV.
Risk assessment of significant complications and comorbidities in insulin-dependent diabetes mellitus patients.
| Comorbidities | Pneumonia (n = 9) | Ventilation (n = 4) | Readmission (n = 44) |
|---|---|---|---|
| HTN only | 6 (0.6) | 1 (0.2) | 31 (0.7) |
| COPD only | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| BLD only | 1 (0.1) | 1 (0.2) | 1 (0.0) |
| HTN + COPD | 0 (0.0) | 2 (0.5) | 5 (0.1) |
| HTN + BLD | 0 (0.0) | 0 (0.0) | 3 (0.06) |
| COPD + BLD | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| HTN + COPD + BLD | 0 (0.0) | 0 (0.0) | 0 (0.0) |
HTN, hypertension; COPD, chronic obstructive pulmonary disease; BLD, bleeding disorder.
Discussion
The present study investigated the data of 39,877 patients, of which 33,302 were non-diabetic, 4758 (14.3%) were NIDDM, and 1817 (4.6%) were IDDM. Following bivariate analysis, we determined NIDDM to be significantly associated with sepsis, reintubation, cardiac arrest, deep incisional SSI, and readmission. IDDM was significantly associated with pneumonia, reintubation, cardiac arrest, myocardial infarction, remaining on a ventilator >48 hours, deep incisional SSI, nonhome discharge, and mortality. We controlled for significantly associated patient demographics and comorbidities and identified NIDDM as an independent risk factor for sepsis. IDDM was found to be an independent risk factor for pneumonia, readmission, myocardial infarction, and remaining on a ventilator >48 hours. Despite these identified associations, the risk of complication following aRCR is rare, especially within the first 30 days. Our study may be affected by selection bias for patients in the hospital setting. Nevertheless, these complications are clinically pertinent and may be important to acknowledge during the assessment of a patient.
Musculoskeletal compromise is a frequent complication of diabetic pathology. As the prevalence of the disease increases, the number of orthopedic procedures on diabetic patients should grow. RCR is especially a common procedure in diabetics.8 Diabetes-associated suboptimal glycemic control, obesity, and cardiovascular disorders may play a role.24 The underlying mechanism could be attributed to nonenzymatic glycation and vascular distress.26 The chronic hyperglycemia observed in diabetes is responsible for increased advanced glycosylation end products (AGEs); accumulation of AGEs within joints can cause the load-bearing collagen proteins found in tendons and ligaments to crosslink, manifesting in biomechanical disturbance.29 Furthermore, the association of AGEs with their endothelial receptor produces oxidative stress and the release of inflammatory cytokines, increasing vessel stiffness and permeability.6 This aggravates the vascular environment seen in diabetes, leading to the disproportionate expression of type III collagen in tenocytes, causing greater weakness to force and susceptibility to rupture.18
Insulin dependence is a reflection of pancreatic insufficiency, a condition that may result from longer duration of diabetes, poor glycemic control, and advanced disease.20 Based on previous studies on orthopedic procedures, we held the assumption that insulin dependence would prove to be a greater risk factor for complications following aRCR.7,9,16,17 Consistent with our hypothesis, there was a difference among the complications correlated with diabetes between the IDDM and NIDDM cohorts.
Based on our analysis, diabetic patients were males generally of older age, with 60% and 56.9% of the NIDDM and IDDM cohorts, being over the age of 60 years, respectively. In addition, 67.8% of NIDDM and 73% of IDDM diabetics were obese, with a BMI over 30 kg/m2. Within the obese IDDM population, 21.8% had a BMI over 40 kg/m2, classifying them as severely obese patients. These results agree with the literature; Quan et al21 noted that in open RCR surgery, the mean BMI for diabetic patients, of which most were male, was over 34 kg/m2. Similarly, Golvinaux et al7 found that diabetic patients undergoing lumbar fusion were of greater BMI, older age, and male. Obesity has been found to be an independent predictor of postoperative complications following aRCR, including pulmonary complications and nonhome discharge.10
IDDM was independently associated with greater risk of contracting postoperative pneumonia, comparable to the findings of Bohl et al,1 which found both cohorts of diabetes undergoing lumbar fusion to have an increased chance of contracting pneumonia. Postoperative pneumonia may be a consequence of both a suppressed immune system inherent to diabetes and the concentrated hospital environment, as it is a common nosocomial infection.1 In addition, pneumonia frequently arises from prolonged mechanical ventilation.11 Though not explicitly examined by the present study, it is possible that postoperative pneumonia could be related to the IDDM cohort also having a greater risk of remaining on a ventilator for longer than 48 hours.
Insulin dependence was also found to be a risk factor for myocardial infarction following aRCR. It is known that diabetes is closely linked to cardiovascular vascular disease, and myocardial infarction is a major cause of mortality in the diabetic population.13 Interestingly, other NSQIP database studies focused on lumbar fusion and ankle fractures that have not shown insulin dependence to be an independent risk factor for myocardial infraction.7,16
Finally, IDDM patients were found to be 1.67 times more likely to face unplanned readmission when compared to those without diabetes. Pneumonia, remaining on a ventilator for greater than 48 hours and myocardial infarction are all factors that may be related to unplanned readmission. Fundamentally, unplanned readmission serves as an indicator of overall complications and is a burden to patient recovery and satisfaction. In addition to IDDM being an independent predictor for the mentioned complications, we found that pre-existing comorbid hypertension may place patients within the IDDM cohort at an even higher risk.
Insulin dependence as a risk factor for postoperative SSI following aRCR has not been examined. Iorio et al9 reported that IDDM were more likely to experience superficial and deep SSI at a rate of 11.7% compared to the 1.4% discovered in NIDDM following total hip arthroplasty or total knee arthroplasty. Similarly, a study by Stepan et al27 found that a cohort of 1772 patients undergoing hand procedures with IDDM had increased rates of superficial SSIs. We found both IDDM and NIDDM to be associated with deep incisional infections (SSI); however, after adjusting for significant demographics and comorbidities, IDDM and NIDDM were not found be independently associated with any degree of SSI. These findings resemble reports on open RCR from Quan et al,21 which did not correlate superficial SSI with either diabetes subsets.
We found that NIDDM patients had an unexpected 2.77-fold risk of contracting sepsis postoperatively. A study on proximal humerus fractures found that their NIDDM cohort was associated with higher chance of postoperative sepsis.19 The present study did not find that IDDM was independently associated with sepsis. However, these results are not consistent with Liu et al16, who found that IDDM patients undergoing ankle fracture surgery were at significant risk for sepsis. Of note, patients with type II diabetes are less likely to use insulin than type I diabetics, yet with disease progression it may become necessary20; for that reason, we cannot classify NIDDM cohort as type II diabetics or associate the group with the increased rates of sepsis noticed in type II diabetics. Along with significant mortality, postoperative sepsis can lead to longer duration of stay, higher rates of readmission, greater resource utilization, and substantially increased healthcare costs.12 The present study’s findings suggest that preoperative and perioperative management personalized to diabetes status may reduce the overall burden of sepsis following aRCR.
By further stratifying the incidence of comorbidities in IDDM patients, we were able to develop a risk profile in which concomitant hypertension increased the risk of significantly associated complications of pneumonia, remaining on a ventilator >48 hours, and readmission. In terms of prevention, this encourages careful pre- and postoperative monitoring of those with comorbid hypertension. Further studies may yield better insight into the association between IDDM and hypertension, and whether adequate control of elevated blood pressure preoperatively can lead to better outcomes. As this study focused on aRCR performed in the hospital setting, it may also be beneficial to determine whether preoperative admission and postoperative monitoring would benefit these patients.
There are several limitations encountered by this study, intrinsic to the database used. Although the NSQIP provides with substantial and increasingly reliable patient data, our analysis is limited by the 30-day collection of information.25 As a result, complications beyond this time period are omitted. There are several occurrences found in diabetic patients that may arise following 30 days, including reduced functionality, decreased mobility, pain, and poor satisfaction.28 It is important to note that the NSQIP database only provides information on cases performed in the hospital setting, and therefore, does not include aRCR performed in the outpatient setting of ambulatory surgery centers. As over 500,000 RCRs are performed in the United States each year, our sample is not representative of all cases of aRCR. Our study likely has a selection bias for cases performed in the hospital vs. ambulatory surgery center and may not reflect the rates and risk of complications faced by patients in the outpatient setting. Furthermore, hemoglobin usually seen as A1C is not a collected variable that could prove to be useful in determining whether diabetic patients exhibited perioperative hyperglycemia, and if this had any effects on outcomes.3
Conclusion
NIDDM was an independent risk factor for sepsis. IDDM was an independent risk factor for pneumonia, readmission, myocardial infarction, and remaining on the ventilator >48 hours. Concomitant hypertension with IDDM seemed to augment the risk of complication. With an increasing prevalence of diabetes in the United States, our findings suggest that diabetic patients may benefit from careful cardiopulmonary examination prior to aRCR. Understanding the complications associated with specific comorbidities can help with optimizing postoperative patient outcomes.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this large deidentified database study.
References
- 1.Bohl D.D., Mayo B.C., Massel D.H., Iantorno S.E., Ahn J., Basques B.A., et al. Incidence and risk factors for pneumonia after posterior lumbar fusion procedures: an ACS-NSQIP study. Spine. 2016;41:1058–1063. doi: 10.1097/BRS.0000000000001389. [DOI] [PubMed] [Google Scholar]
- 2.Borton Z., Shivji F., Simeen S., Williams R., Tambe A., Espag M., et al. Diabetic patients are almost twice as likely to experience complications from arthroscopic rotator cuff repair. Shoulder Elbow. 2020;12:109–113. doi: 10.1177/1758573219831691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cancienne J.M., Deasey M.J., Kew M.E., Werner B.C. The association of perioperative glycemic control with adverse outcomes within 6 months after arthroscopic rotator cuff repair. Arthroscopy. 2019;35:1771–1778. doi: 10.1016/j.arthro.2019.01.035. [DOI] [PubMed] [Google Scholar]
- 4.Dhar Y., Anakwenze O.A., Steele B., Lozano S., Abboud J.A. Arthroscopic rotator cuff repair: impact of diabetes mellitus on patient outcomes. Phys Sportsmed. 2013;41:22–29. doi: 10.3810/psm.2013.02.1995. [DOI] [PubMed] [Google Scholar]
- 5.Gerrits E.G., Landman G.W., Nijenhuis-Rosien L., Bilo H.J. Limited joint mobility syndrome in diabetes mellitus: a minireview. World J Diabetes. 2015;6:1108–1112. doi: 10.4239/wjd.v6.i9.1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldin A., Beckman J.A., Schmidt A.M., Creager M.A. Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation. 2006;114:597–605. doi: 10.1161/CIRCULATIONAHA.106.621854. [DOI] [PubMed] [Google Scholar]
- 7.Golinvaux N.S., Varthi A.G., Bohl D.D., Basques B.A., Grauer J.N. Complication rates following elective lumbar fusion in patients with diabetes: insulin dependence makes the difference. Spine. 2014;39:1809–1816. doi: 10.1097/BRS.0000000000000506. [DOI] [PubMed] [Google Scholar]
- 8.Huang S.W., Wang W.T., Chou L.C., Liou T.H., Chen Y.W., Lin H.W. Diabetes mellitus increases the risk of rotator cuff tear repair surgery: a population-based cohort study. J Diabetes Complications. 2016;30:1473–1477. doi: 10.1016/j.jdiacomp.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Iorio R., Williams K.M., Marcantonio A.J., Specht L.M., Tilzey J.F., Healy W.L. Diabetes mellitus, hemoglobin A1C, and the incidence of total joint arthroplasty infection. J Arthroplasty. 2012;27:726–729.e1. doi: 10.1016/j.arth.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Kashanchi K.I., Nazemi A.K., Komatsu D.E., Wang E.D. Level of obesity is directly associated with complications following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2021;30:1581–1587. doi: 10.1016/j.jse.2020.09.029. [DOI] [PubMed] [Google Scholar]
- 11.Koenig S.M., Truwit J.D. Ventilator-associated pneumonia: diagnosis, treatment, and prevention. Clin Microbiol Rev. 2006;19:637–657. doi: 10.1128/CMR.00051-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lakomkin N., Sathiyakumar V., Wick B., Shen M.S., Jahangir A.A., Mir H., et al. Incidence and predictive risk factors of postoperative sepsis in orthopedic trauma patients. J Orthop Traumatol. 2017;18:151–158. doi: 10.1007/s10195-016-0437-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leon B.M., Maddox T.M. Diabetes and cardiovascular disease: epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes. 2015;6:1246–1258. doi: 10.4239/wjd.v6.i13.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin J., Thompson T.J., Cheng Y.J., Zhuo X., Zhang P., Gregg E., et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metr. 2018;16:9. doi: 10.1186/s12963-018-0166-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin T.T., Lin C.H., Chang C.L., Chi C.H., Chang S.T., Sheu W.H. The effect of diabetes, hyperlipidemia, and statins on the development of rotator cuff disease: a nationwide, 11-year, longitudinal, population-based follow-up study. Am J Sports Med. 2015;43:2126–2132. doi: 10.1177/0363546515588173. [DOI] [PubMed] [Google Scholar]
- 16.Liu J.W., Ahn J., Nakonezny P.A., Lalli T., VanPelt M.D., Raspovic K.M., et al. Insulin dependence increases the risk of 30-day postoperative complications following ankle fracture surgery in patients with diabetes mellitus. J Foot Ankle Surg. 2021;60:917–922. doi: 10.1053/j.jfas.2021.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Lung B.E., Bisogno M., Kanjiya S., Komatsu D.E., Wang E.D. Early postoperative complications and discharge time in diabetic patients undergoing total shoulder arthroplasty. J Orthop Surg Res. 2019;14:9. doi: 10.1186/s13018-018-1051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Millar N.L., Reilly J.H., Kerr S.C., Campbell A.L., Little K.J., Leach W.J., et al. Hypoxia: a critical regulator of early human tendinopathy. Ann Rheum Dis. 2012;71:302–310. doi: 10.1136/ard.2011.154229. [DOI] [PubMed] [Google Scholar]
- 19.Patterson D.C., Shin J.I., Andelman S.M., Olujimi V., Parsons B.O. Increased risk of 30-day postoperative complications for diabetic patients following open reduction-internal fixation of proximal humerus fractures: an analysis of 1391 patients from the American College of Surgeons National Surgical Quality Improvement Program database. JSES Open Access. 2017;1:19–24. doi: 10.1016/j.jses.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piciucchi M., Capurso G., Archibugi L., Delle Fave M.M., Capasso M., Delle Fave G. Exocrine pancreatic insufficiency in diabetic patients: prevalence, mechanisms, and treatment. Int J Endocrinol. 2015;2015 doi: 10.1155/2015/595649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quan T., Manzi J.E., Chen F.R., Rauck R., Recarey M., Roszkowska N., et al. Diabetes status and postoperative complications for patients receiving open rotator cuff repair. Shoulder Elbow. 2022 doi: 10.1177/17585732211070531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ranger T.A., Wong A.M., Cook J.L., Gaida J.E. Is there an association between tendinopathy and diabetes mellitus? A systematic review with meta-analysis. Br J Sports Med. 2016;50:982–989. doi: 10.1136/bjsports-2015-094735. [DOI] [PubMed] [Google Scholar]
- 23.Rechardt M., Shiri R., Karppinen J., Jula A., Heliovaara M., Viikari-Juntura E. Lifestyle and metabolic factors in relation to shoulder pain and rotator cuff tendinitis: a population-based study. BMC Musculoskelet Disord. 2010;11:165. doi: 10.1186/1471-2474-11-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rizvi A.A., Chillag S.A., Chillag K.J. Perioperative management of diabetes and hyperglycemia in patients undergoing orthopaedic surgery. J Am Acad Orthop Surg. 2010;18:426–435. doi: 10.5435/00124635-201007000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Shiloach M., Frencher S.K., Jr., Steeger J.E., Rowell K.S., Bartzokis K., Tomeh M.G., et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons national surgical Quality Improvement Program. J Am Coll Surg. 2010;210:6–16. doi: 10.1016/j.jamcollsurg.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 26.Sozen T., Basaran N.C., Tinazli M., Ozisik L. Musculoskeletal problems in diabetes mellitus. Eur J Rheumatol. 2018;5:258–265. doi: 10.5152/eurjrheum.2018.18044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stepan J.G., Boddapati V., Sacks H.A., Fu M.C., Osei D.A., Fufa D.T. Insulin dependence is associated with increased risk of complications after upper Extremity surgery in diabetic patients. J Hand Surg Am. 2018;43:745–754.e4. doi: 10.1016/j.jhsa.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 28.Takahashi R., Kajita Y., Harada Y., Iwahori Y., Deie M. Clinical results of arthroscopic rotator cuff repair in diabetic and non-diabetic patients. J Orthop Sci. 2021;26:213–218. doi: 10.1016/j.jos.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 29.Xu K., Zhang L., Ren Z., Wang T., Zhang Y., Zhao X., et al. Evaluating the role of type 2 diabetes mellitus in rotator cuff tendinopathy: development and analysis of a novel rat model. Front Endocrinol. 2022;13 doi: 10.3389/fendo.2022.1042878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yanik E.L., Chamberlain A.M., Keener J.D. Trends in rotator cuff repair rates and comorbidity burden among commercially insured patients younger than the age of 65 years, United States 2007-2016. JSES Rev Rep Tech. 2021;1:309–316. doi: 10.1016/j.xrrt.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zreik N.H., Malik R.A., Charalambous C.P. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J. 2016;6:26–34. doi: 10.11138/mltj/2016.6.1.026. [DOI] [PMC free article] [PubMed] [Google Scholar]