Abstract
Background
Smoking is a major public health concern and an important risk factor to consider during preoperative planning. Smoking has previously been reported as the single most important risk factor for developing postoperative complications after elective orthopedic surgery. However, there is limited literature regarding the postoperative complications associated with smoking following outpatient total shoulder arthroplasty (TSA). The purpose of this study was to investigate the association between smoking status and early postoperative complications following outpatient TSA using a large national database.
Methods
We queried the American College of Surgeons National Surgical Quality Improvement Program database for all patients who underwent TSA between 2015 and 2020. Smoking status in National Surgical Quality Improvement Program is defined as any episode of smoking with 12 months prior to surgery. Bivariate logistic regression was used to identify patient demographics, comorbidities, and complications significantly associated with current or recent smoking status in patients who underwent TSA with a length of stay (LOS) of 0. Multivariate logistic regression, adjusted for all significantly associated patient demographics and comorbidities, was used to identify associations between current or recent smokers and 30-day postoperative complications.
Results
22,817 patients were included in the analysis, 2367 (10.4%) were current or recent smokers and 20,450 (89.6%) were nonsmokers. These patients were further stratified based on LOS: 2428 (10.6%) patients had a LOS of 0 days, 15,267 (66.9%) patients had a LOS of 1 day, and 5122 (22.4%) patients had a LOS of 2 days. Within the outpatient cohort (LOS = 0), 202 (8.3%) patients were current or recent smokers and 2226 (91.7%) were nonsmokers. Multivariate logistic regression identified current or recent smoking status to be independently associated with higher rates of myocardial infarction (odds ratio [OR] 9.80, 95% confidence interval [CI] 1.48-64.96; P = .018), deep vein thrombosis (OR 20.05, 95% CI 1.63-247.38; P = .019), and readmission (OR 2.82, 95% CI 1.19-6.67; P = .018) following outpatient TSA. Readmission was most often due to pulmonary complication (n = 10, 22.7%).
Conclusion
Current or recent smoking status is independently associated with higher rates of myocardial infarction, deep vein thrombosis, and readmission following TSA performed in the outpatient setting. Current or recent smokers may benefit from an inpatient setting of minimum 2 nights. As outpatient TSA becomes increasingly popular, refining proper patient selection criteria is imperative to optimizing postoperative outcomes.
Keywords: Total shoulder arthroplasty, Reverse shoulder arthroplasty, Smoking, Tobacco, Ambulatory, Outpatient
Total shoulder arthroplasty (TSA) is an established procedure for treatment of end-stage glenohumeral arthritis to improve function, range of motion, strength, pain, and quality of life.11 Positive outcomes, including pain relief, patient satisfaction, and functional improvement have been observed in over 90% of cases for anatomic TSA.25 However, postoperative complications have been observed in about 10% of cases, most commonly due to glenohumeral component loosening, instability, and rotator cuff tear.7,31 Several factors, such as tobacco use, obesity, opioid use, and depression have also been reported to increase the risk of complications and worsen outcomes following TSA.20,24
A recent Morbidity and Mortality Weekly Report analyzed data from the 2020 National Health Interview Survey and estimated that 47.1 million United States adults are tobacco users.10 As such, smoking is a major public health concern and an important risk factor to consider during preoperative planning. Smoking has previously been reported as the single most important risk factor for developing postoperative complications after elective orthopedic surgery.23 For patients undergoing TSA, cigarette smoking is a common comorbidity. Preoperative smoking has been found to be associated with an increased risk of TSA complications, including periprosthetic infection, periprosthetic fractures, hardware loosening, postoperative infections, and increased narcotic use.3,11,39 Previous studies have reported complication rates for current smokers as high as 36%.37
All of these prior studies that identified smoking as a risk factor for complications following TSA have focused on inpatient surgeries. To our knowledge, there is limited literature regarding the postoperative complications associated with smoking following outpatient TSA. TSA performed in the ambulatory or outpatient setting is gaining popularity, with a reported 107% increase in outpatient shoulder arthroplasties between 2010 and 2014.5,8,21,26 The purpose of this study was to investigate the association between smoking status and postoperative complications following outpatient TSA using a large national database. A secondary objective of this study was to evaluate the effect of overnight stay on the postoperative complications associated with smoking in the outpatient population. We hypothesized that active smokers are at an increased risk of postoperative complications following outpatient TSA.
Methods
We queried the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database for all patients who underwent TSA between 2015 and 2020. This study was rendered exempt from approval by our University’s Institutional Review Board, as the National Surgical Quality Improvement Program (NSQIP) database is fully deidentified. The data within the NSQIP database are collected by trained Surgical Clinical Reviewers and obtained from over 600 hospitals in the United States. High fidelity is maintained through periodic auditing of the data.
Current Procedural Terminology code 23472 was used to identify patients who underwent TSA, both anatomic and reverse, from 2015 to 2020. The NSQIP database automatically excludes patients younger than 18 years of age and trauma cases. Cases were also excluded if data were missing for the following variables: height/weight, readmission status, functional health status, American Society of Anesthesiologists (ASA) classification, discharge destination, length of stay (LOS), and current smoking status. Additionally, cases were excluded if patients had a LOS greater than 2 days.
Patient demographics, comorbidities, surgical characteristics, and 30-day postoperative complications were collected from the database. Patient demographics included age, gender, body mass index, functional status prior to surgery, ASA classification, smoking status, and steroid use for a chronic condition. Preoperative comorbidities included congestive heart failure, insulin-dependent and noninsulin-dependent diabetes mellitus, hypertension, chronic obstructive pulmonary disease (COPD), bleeding disorders, open wound/wound infection, and disseminated cancer. Surgical characteristics included operative duration in minutes, categorized as 0-79 minutes (25th percentile), 80-128 minutes, and ≥129 minutes (75th percentile), based on quartile times of the entire study population. Postoperative complications included sepsis, septic shock, pneumonia, reintubation, urinary tract infection, stroke, cardiac arrest, myocardial infarction (MI), bleeding transfusion, deep vein thrombosis (DVT), pulmonary embolism, failure to wean off ventilator, deep incisional surgical-site infection (SSI), superficial incisional SSI, organ/space SSI, wound dehiscence, readmission, reoperation, non-home discharge, and mortality.
The initial pool of patients was divided into two cohorts: current or recent smoker and nonsmoker. The NSQIP database defines a current smoker as a patient who has smoked cigarettes within the 12 months prior to admission for surgery. This variable does not include the use of cigars, pipes, chewing tobacco, marijuana, mechanical/electronic cigarettes, or hookah. These cohorts were further stratified based on LOS. The LOS variable provided in NSQIP represents the total length of hospital stay from admission to discharge. Therefore, patients with a LOS of 0 days were discharged on the same day as the procedure and were considered to have undergone outpatient procedures.
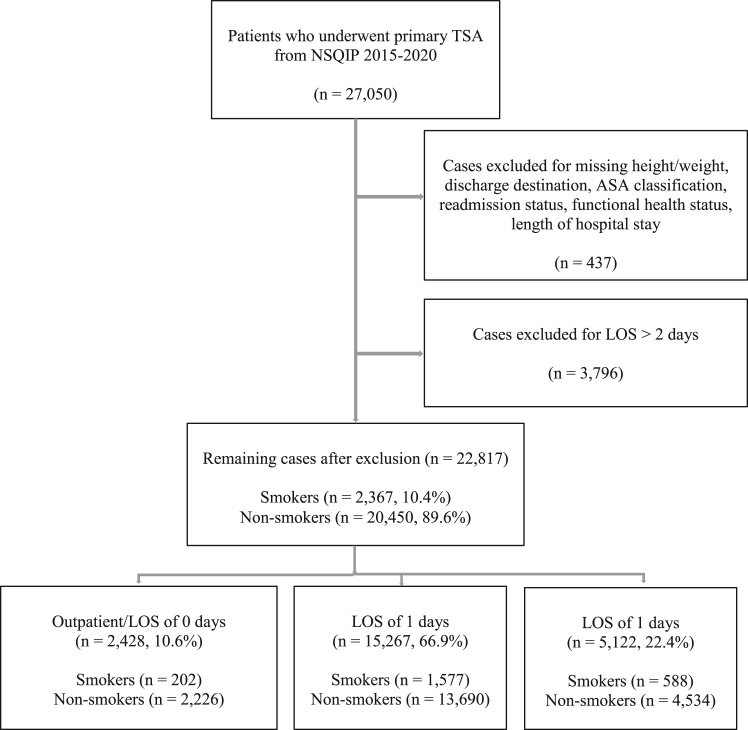
A total of 27,050 patients who underwent primary TSA were identified in NSQIP from 2015-2020. Cases were excluded for missing values: height/weight (152), discharge destination (11), ASA classification (29), functional health status prior to surgery (227), readmission status (2), and total LOS (16). Cases were also excluded for LOS > 2 days (3,796). The remaining 22,817 patients were stratified based on LOS: 0 days (n = 2,428, 10.6%), 1 day (n = 15,267, 66.9%), and 2 days (n = 5,122, 22.4%). Within the outpatient cohort (LOS = 0), 202 (8.3%) patients were current or recent smokers and 2226 (91.7%) were nonsmokers (Fig. 1).
Figure 1.
Strengthening the reporting of observational studies in epidemiology (STROBE) diagram with inclusion and exclusion criteria. TSA, total shoulder arthroplasty; NSQIP, National Surgical Quality Improvement Program; ASA, American Society of Anesthesiologists; LOS, length of stay.
All statistical analyses were conducted using SPSS Software version 26.0 (IBM Corp., Armonk, NY, USA). Bivariate logistic regression was used to identify patient demographics and comorbidities significantly associated with current or recent smoking status in patients who underwent TSA with a LOS of 0. Bivariate logistic regression was also used to identify 30-day postoperative complications significantly associated with current or recent smoking status.
Multivariate logistic regression, adjusted for all significantly associated patient demographics and comorbidities, was used to identify associations between current or recent smoking status and 30-day postoperative complications. Afterwards, multivariate logistic regression was used to compare the complication rates between LOS cohorts to determine the effect of overnight stay on current or recent smokers. Odds ratios (ORs) were reported with 95% confidence intervals (CIs). The level of statistical significance was set at P < .05.
Results
Patient demographics and comorbidities significantly associated with current or recent smoking status in the outpatient cohort were age 40-64 (P < .001), ASA classification ≥3 (P = .008), and COPD (P < .001) (Table I).
Table I.
Patient demographics/comorbidities for outpatient total shoulder arthroplasty patients of smoking vs. nonsmoking status within 1 year preoperatively.
| Characteristic | Nonsmoker |
Smoker |
P value | ||
|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||
| Total | 2226 | 100.0% | 202 | 100.0% | |
| Age | <.001 | ||||
| 18-39 | 14 | 0.6% | 7 | 3.5% | |
| 40-64 | 705 | 31.7% | 113 | 55.9% | |
| 65-74 | 948 | 42.6% | 65 | 32.2% | |
| ≥75 | 559 | 25.1% | 17 | 8.4% | |
| Body mass index (kg/m2) | .405 | ||||
| <18.5 | 13 | 0.6% | 3 | 1.5% | |
| 18.5-29.9 | 1201 | 54.0% | 106 | 52.5% | |
| 30-34.9 | 612 | 27.5% | 52 | 25.7% | |
| 35-39.9 | 269 | 12.1% | 25 | 12.4% | |
| ≥40 | 126 | 5.7% | 16 | 7.9% | |
| Gender | .319 | ||||
| Female | 1040 | 46.7% | 87 | 43.1% | |
| Male | 1186 | 53.3% | 115 | 56.9% | |
| Functional status prior to surgery | .762 | ||||
| Independent | 2218 | 99.6% | 201 | 99.5% | |
| Dependent | 8 | 0.4% | 1 | 0.5% | |
| ASA classification | .008 | ||||
| 1-2 | 1274 | 57.2% | 96 | 47.5% | |
| ≥3 | 952 | 42.8% | 106 | 52.5% | |
| Congestive heart failure | .999 | ||||
| No | 2224 | 99.9% | 202 | 100.0% | |
| Yes | 2 | 0.1% | 0 | 0.0% | |
| Diabetes mellitus | .750 | ||||
| No diabetes | 1947 | 87.5% | 174 | 86.1% | |
| Noninsulin dependent diabetes | 202 | 9.1% | 19 | 9.4% | |
| Insulin dependent diabetes | 77 | 3.5% | 9 | 4.5% | |
| Hypertension requiring medication | .760 | ||||
| No | 956 | 42.9% | 89 | 44.1% | |
| Yes | 1270 | 57.1% | 113 | 55.9% | |
| COPD | <.001 | ||||
| No | 2163 | 97.2% | 183 | 90.6% | |
| Yes | 63 | 2.8% | 19 | 9.4% | |
| Bleeding disorders | .630 | ||||
| No | 2182 | 98.0% | 197 | 97.5% | |
| Yes | 44 | 2.0% | 5 | 2.5% | |
| Open wound/wound infection | .163 | ||||
| No | 2224 | 99.9% | 201 | 99.5% | |
| Yes | 2 | 0.1% | 1 | 0.5% | |
| Disseminated cancer | 1.000 | ||||
| No | 2225 | 100.0% | 202 | 100.0% | |
| Yes | 1 | 0.0% | 0 | 0.0% | |
| Steroid use for chronic condition | .942 | ||||
| No | 2151 | 96.6% | 195 | 96.5% | |
| Yes | 75 | 3.4% | 7 | 3.5% | |
| Operative duration (min) | .188 | ||||
| 0-79 | 551 | 24.8% | 56 | 27.7% | |
| 80-128 | 1152 | 51.8% | 91 | 45.0% | |
| ≥129 | 523 | 23.5% | 55 | 27.2% | |
ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease.
Bold P values indicate statistical significance with P < .05.
Bivariate logistic regression was used to identify 30-day postoperative complications significantly associated with current or recent smoking status in the outpatient cohort (Table II). We identified higher rates of MI (P = .029), DVT (P = .011), superficial incisional SSI (P = .049), and readmission (P = .021) in current or recent smokers.
Table II.
Bivariate analysis of 30-day postoperative complications following outpatient total shoulder arthroplasty in patients of smoking vs. nonsmoking status within 1 year preoperatively.
| Postoperative complication | Nonsmoker (n = 2226) |
Smoker (n = 202) |
P value | ||
|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||
| Sepsis | 1 | 0.04% | 0 | 0.00% | 1.000 |
| Septic shock | 0 | 0.00% | 0 | 0.00% | - |
| Pneumonia | 6 | 0.27% | 1 | 0.50% | .573 |
| Reintubation | 1 | 0.04% | 0 | 0.00% | 1.000 |
| Urinary tract infection | 11 | 0.49% | 2 | 0.99% | .365 |
| Stroke | 1 | 0.04% | 0 | 0.00% | 1.000 |
| Cardiac arrest | 0 | 0.00% | 0 | 0.00% | - |
| Myocardial infarction | 3 | 0.13% | 2 | 0.99% | .029 |
| Bleeding transfusions | 3 | 0.13% | 1 | 0.50% | .259 |
| Deep vein thrombosis | 1 | 0.04% | 2 | 0.99% | .011 |
| Pulmonary embolism | 3 | 0.13% | 1 | 0.50% | .259 |
| Failure to wean off ventilator | 1 | 0.04% | 0 | 0.00% | 1.000 |
| Deep incisional SSI | 1 | 0.04% | 0 | 0.00% | 1.000 |
| Superficial incisional SSI | 4 | 0.18% | 2 | 0.99% | .049 |
| Organ/space SSI | 6 | 0.27% | 0 | 0.00% | .999 |
| Wound dehiscence | 1 | 0.04% | 0 | 0.00% | 1.000 |
| Readmission | 36 | 1.62% | 8 | 3.96% | .021 |
| Reoperation | 22 | 0.99% | 1 | 0.50% | .497 |
| Non-home discharge | 11 | 0.49% | 2 | 0.99% | .351 |
| Mortality | 1 | 0.04% | 0 | 0.00% | 1.000 |
SSI, surgical site infection.
Bold P values indicate statistical significance with P < .05.
After adjusting for significantly associated patient demographics and comorbidities reported in Table I, multivariate logistic regression identified current or recent smoking status to be independently associated with higher rates of MI (OR 9.80, 95% CI 1.48-64.96; P = .018), DVT (OR 20.05, 95% CI 1.63-247.38; P = .019), and readmission (OR 2.82, 95% CI 1.19-6.67; P = .018) following outpatient TSA (Table III). Superficial incisional SSI (P = .061) was not identified to be an independently associated complication in the multivariate analysis.
Table III.
Multivariate analysis of 30-day postoperative complications following outpatient total shoulder arthroplasty in patients of smoking vs. nonsmoking status within 1 year preoperatively, adjusted for significantly associated patient demographics/comorbidities.
| Postoperative complication | OR | 95% CI | P value |
|---|---|---|---|
| Myocardial infarction | 9.80 | 1.48-64.96 | .018 |
| Deep vein thrombosis | 20.05 | 1.63-247.38 | .019 |
| Superficial incisional SSI | 5.38 | 0.93-31.22 | .061 |
| Readmission | 2.82 | 1.19-6.67 | .018 |
OR, odds ratio; CI, confidence interval; SSI, surgical site infection.
Bold P values indicate statistical significance with P < .05.
Multivariate logistic regression, adjusted for significantly associated patient demographics and comorbidities, was used to determine the effect of overnight stay on the significant postoperative complications identified in Table III. After overnight stay (LOS = 1), MI (P = .260) and DVT (P = .591) were no longer significant complications (Table IV). However, readmission (OR 1.48; 95% CI 1.07-2.05; P = .020) remained a significant complication in current or recent smokers after overnight stay in the hospital. After 2 overnight stays in the hospital, readmission (P = .658) was no longer significant.
Table IV.
Effect of overnight stay on 30-day postoperative complications following outpatient total shoulder arthroplasty in patients of smoking status.
| Postoperative complication | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Myocardial infarction | .260 | ||
| Outpatient | Reference | – | |
| Length of stay = 1 day | 2.22 | 0.55-8.86 | |
| Deep vein thrombosis | .591 | ||
| Outpatient | Reference | – | |
| Length of stay = 1 day | 1.32 | 0.48-3.60 | |
| Readmission | .020 | ||
| Outpatient | Reference | – | |
| Length of stay = 1 day | 1.48 | 1.07-2.05 | |
| Readmission | .658 | ||
| Outpatient | Reference | – | |
| Length of stay = 2 days | 1.12 | 0.68-1.83 |
CI, confidence interval.
Bold P values indicate statistical significance with P < .05.
Readmission in the outpatient smoking cohort was most often due to pulmonary complication (n = 10, 22.7%) (Table V). Pulmonary complications included pneumonia, acute respiratory failure, COPD, shortness of breath, and breathing abnormality. The most common surgical site related reason for readmission was wound complication (n = 4, 9.1%).
Table V.
Reasons for 30-day readmission in the outpatient smoking cohort following TSA.
| Reason | Number | Percent |
|---|---|---|
| Total | 44 | 100% |
| Nonsurgical site related | ||
| Pulmonary complications | 10 | 22.7% |
| Thromboembolic complications | 4 | 9.1% |
| Unrelated orthopedic complications | 4 | 9.1% |
| Neurologic complications | 4 | 9.1% |
| Sepsis | 3 | 6.8% |
| Endocrine complications | 3 | 6.8% |
| Cardiovascular complications | 1 | 2.3% |
| Renal complications | 1 | 2.3% |
| Gastrointestinal complications | 1 | 2.3% |
| Urinary tract infection | 1 | 2.3% |
| Surgical site related | ||
| Wound complications | 4 | 9.1% |
| Pain | 1 | 2.3% |
| Dislocation of prosthesis | 1 | 2.3% |
| Other complications/unspecified | 6 | 13.6% |
TSA, total shoulder arthroplasty.
Discussion
In this study, we used a large national database to analyze smoking as a risk factor for postoperative complications following TSA performed in the outpatient setting from 2015 to 2020. Our analysis included 22,817 patients, of which 2367 (10.4%) were identified as current or recent smokers. The outpatient cohort included 2428 patients, of which 202 (8.3%) were current or recent smokers. Through bivariate analysis, we identified current or recent smoking status in the outpatient cohort to be significantly associated with age 40-64, ASA classification ≥3, and COPD. After controlling for these significantly associated variables, we identified current or recent smoking status in the outpatient cohort to be independently associated with higher rates of MI, DVT, and readmission. We further identified that MI and DVT were no longer significant after 1 night in the hospital, and readmission was no longer significant after 2 nights in the hospital.
In recent years, outpatient TSA has become increasingly popular, with a reported 107% increase in outpatient shoulder arthroplasties between 2010 and 2014.5,8,21,26 The movement towards outpatient TSA reflects several factors including annual increases in the number of TSA performed and an increasing emphasis on cost-effective health care, without compromising patient safety and surgical outcomes.15,26,32,33,35,38 As the surgical volume of outpatient TSA trends upwards, utilizing preoperative risk stratification to minimize adverse outcomes is increasingly valuable to surgeons. Prior studies have shown no difference in complication rates and outcomes for TSA between outpatient and inpatient cohorts. Studies have also shown that patient selection is the most critical factor for predicting outpatient TSA success. However, there is currently no established algorithm for patient selection for outpatient TSA procedures.36 Understanding how patient factors, such as smoking status, impact postoperative complications following outpatient TSA can aid surgeons in identifying patients that are more at risk for complications when deciding between the outpatient or inpatient setting.
Both patient and procedure related factors and variables have been identified as risk factors for complications following TSA. These include male gender, increased age, functional status, ASA class ≥3, history of cardiac disease, hematocrit < 38%, operating time > 2 hours, steroid use, tobacco use, obesity, opioid use, and depression.4,6,19,20,24 Although many prior studies have investigated postoperative complications following TSA, few studies have evaluated patients undergoing TSA specifically in the outpatient setting. Leroux et al used a large national database to determine and compare the 30-day adverse events and readmission rates for inpatient vs. outpatient TSA.18 Their results showed that there were no significant differences in both the 30-day adverse event rate and readmission rate between cohorts.18 Cimino et al performed a systematic review that included studies evaluating the outcomes of TSA or reverse TSA in an outpatient setting and found that there were no significant differences in infection, revision, or 90-day readmission rates when comparing outpatient to inpatient procedures.9 Basques et al retrospectively compared outcomes of outpatient vs. inpatient TSA in 123,347 Medicare patients and found that outpatient TSA had fewer complications including readmission, thromboembolic events, surgical site infection, and blood transfusion.5 Additionally, they found that outpatients were generally younger with lower rates of comorbidities, which may indicate that patient selection has already taken place. Therefore, the evaluation of risk factors in the outpatient cohort should be considered in the setting of patient selection already being done based on each surgeon’s preexisting criterion.
Further, many studies have previously identified smoking as a risk factor for readmission following shoulder arthroplasty. Smoking has also been identified as a risk factor in other orthopedic procedures, including total knee arthroscopy and total hip arthoscopy.16 However, to our knowledge, our study is the first to analyze smoking as a risk factor for postoperative complications in patients undergoing TSA specific to the outpatient setting.
Our study identified preoperative smoking status as a significant predictor for readmission following outpatient TSA. These findings suggest that smoking may be a relative contraindication for outpatient TSA, as current or recent smokers are at higher risk for readmission. Additionally, our study found that smokers may benefit from an inpatient setting of minimum 2 nights, as readmission was no longer a significant complication after 2 nights in the hospital. These findings reiterate the importance of preoperative smoking cessation and counseling for patients to reduce the likelihood of readmission following TSA, which has been demonstrated in prior literature.17,22,30,40
This study also identified smoking as a risk factor for postoperative complications following outpatient TSA, including MI and DVT within 30 days. Tobacco has been found to be the most important avoidable cause of cardiovascular diseases across the world.28 Studies have found that smoking negatively affects platelet function, causes damage to arterial endothelium, and development of atherosclerotic plaque.13 The association between smoking and postoperative DVT has also been well-established in the literature. Prior studies have found that tobacco promotes increased levels of tissue factor and factor VII, which activate the coagulation cascade.1,29 In addition, tobacco stimulates platelet aggregation and impairs fibrinolysis, increasing risk for DVT.13,34
There were several limitations to this study that warrant further discussion. One important limitation is that the NSQIP database does not differentiate between implant subtype for TSA. This would likely affect the results of the study, as anatomic and reverse TSA have been found to have different types of complications and complication rates.27 Additionally, NSQIP is limited to complication data within the 30-day postoperative period. Therefore, we could not account for all relevant complications associated with TSA in patients who actively smoke. Further studies with follow-up after 6 or 12 months would likely encompass more complications including loosening, infection, and periprosthetic fracture.14 Another limitation is that LOS 0 identified in the NSQIP database does not necessarily equate with outpatient intervention, as some admitted patients may be discharged between 6 to 23 hours and still qualify as LOS 0. In terms of smoking, patient smoking status in NSQIP is reported based on one year before surgery. This one-year limitation may inadequately capture the true duration and extent of smoking in the patients reported. Moreover, the NSQIP database does not differentiate between former smokers and never smokers. Additionally, NSQIP does not include alternative tobacco products, such electronic cigarettes, cigars, and chewing tobacco in the smoking variable. As such, patients who used electronic cigarettes, cigars, or chewing tobacco were placed in the nonsmoking group. Electronic cigarettes have been associated with increased surgical risk and approximately 10.8 million United States adults in 2020 were reported to be electronic cigarette users.2,12 Lastly, due to the nature of all statistical analyses, we cannot demonstrate causation but rather were able to show a statistical association between cigarette smoke use and risk of postoperative outpatient TSA complications.
Regardless of these limitations, we used a large national database to analyze smoking as a risk factor for complications following outpatient TSA. By assessing preoperative risk factors in the outpatient setting, we aid in the determination of a proper patient selection algorithm.
Conclusion
Current or recent smoking status is independently associated with higher rates of MI, DVT, and readmission following TSA performed in the outpatient setting. Current or recent smokers may benefit from an inpatient setting of minimum 2 nights, with MI and DVT no longer significant after one night, and readmission no longer significant after two nights. As outpatient TSA becomes increasingly popular, refining proper patient selection criteria is imperative to optimizing postoperative outcomes.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this study.
References
- 1.Al-Nasser B. Influence of tobacco smoking on Perioperative risk of venous thromboembolism. Turk J Anaesthesiol Reanim. 2020;48:11–16. doi: 10.5152/tjar.2019.08683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al Rifai M., Merchant A.T., Nambi V., Jia X., Gulati M., Valero-Elizondo J., et al. Temporal trends in E-cigarette use among U.S. Adults: behavioral risk factor Surveillance System, 2016 to 2018. Am J Med. 2020;133:e508–e511. doi: 10.1016/j.amjmed.2019.12.020. [DOI] [PubMed] [Google Scholar]
- 3.Althoff A.D., Reeves R.A., Traven S.A., Wilson J.M., Woolf S.K., Slone H.S. Smoking is associated with increased surgical complications following total shoulder arthroplasty: an analysis of 14,465 patients. J Shoulder Elbow Surg. 2020;29:491–496. doi: 10.1016/j.jse.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Anthony C.A., Westermann R.W., Gao Y., Pugely A.J., Wolf B.R., Hettrich C.M. What are risk factors for 30-day Morbidity and transfusion in total shoulder arthroplasty? A review of 1922 cases. Clin Orthop Relat Res. 2015;473:2099–2105. doi: 10.1007/s11999-014-4107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basques B.A., Erickson B.J., Leroux T., Griffin J.W., Frank R.M., Verma N.N., et al. Comparative outcomes of outpatient and inpatient total shoulder arthroplasty: an analysis of the Medicare dataset. Bone Joint Lett J. 2017;99-b:934–938. doi: 10.1302/0301-620x.99b7.Bjj-2016-0976.R1. [DOI] [PubMed] [Google Scholar]
- 6.Belmont P.J., Jr., Kusnezov N.A., Dunn J.C., Bader J.O., Kilcoyne K., Waterman B.R. Predictors of hospital readmission after total shoulder arthroplasty. Orthopedics. 2017;40:e1–e10. doi: 10.3928/01477447-20160915-06. [DOI] [PubMed] [Google Scholar]
- 7.Bohsali K.I., Bois A.J., Wirth M.A. Complications of shoulder arthroplasty. J Bone Joint Surg Am. 2017;99:256–269. doi: 10.2106/jbjs.16.00935. [DOI] [PubMed] [Google Scholar]
- 8.Cancienne J.M., Brockmeier S.F., Gulotta L.V., Dines D.M., Werner B.C. Ambulatory total shoulder arthroplasty: a comprehensive analysis of current trends, complications, readmissions, and costs. J Bone Joint Surg Am. 2017;99:629–637. doi: 10.2106/jbjs.16.00287. [DOI] [PubMed] [Google Scholar]
- 9.Cimino A.M., Hawkins J.K., McGwin G., Brabston E.W., Ponce B.A., Momaya A.M. Is outpatient shoulder arthroplasty safe? A systematic review and meta-analysis. J Shoulder Elbow Surg. 2021;30:1968–1976. doi: 10.1016/j.jse.2021.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Cornelius M.E., Loretan C.G., Wang T.W., Jamal A., Homa D.M. Tobacco product use among adults - United States, 2020. MMWR Morb Mortal Wkly Rep. 2022;71:397–405. doi: 10.15585/mmwr.mm7111a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deshmukh A.V., Koris M., Zurakowski D., Thornhill T.S. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14:471–479. doi: 10.1016/j.jse.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 12.Fracol M., Dorfman R., Janes L., Kulkarni S., Bethke K., Hansen N., et al. The surgical impact of E-cigarettes: a case report and review of the current literature. Arch Plast Surg. 2017;44:477–481. doi: 10.5999/aps.2017.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glantz S.A., Parmley W.W. Passive smoking and heart disease. Mechanisms and risk. JAMA. 1995;273:1047–1053. [PubMed] [Google Scholar]
- 14.Hatta T., Werthel J.D., Wagner E.R., Itoi E., Steinmann S.P., Cofield R.H., et al. Effect of smoking on complications following primary shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1–6. doi: 10.1016/j.jse.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 15.Huddleston H.P., Mehta N., Polce E.M., Williams B.T., Fu M.C., Yanke A.B., et al. Complication rates and outcomes after outpatient shoulder arthroplasty: a systematic review. JSES Int. 2021;5:413–423. doi: 10.1016/j.jseint.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson D.J., Castle J.P., Hartwell M.H., Baker H., Selley R.S., Nicolay R.W., et al. Smoking as a risk factor for readmission in arthroscopic surgery: a propensity matched analysis. J Surg Orthop Adv. 2019;28:272–276. https://www.jsoaonline.com/archive/2019/winter-2019/smoking-risk-factor-readmission-arthroscopic-surgery-propensity-matched-analysis/ Winter. [PubMed] [Google Scholar]
- 17.Kamma S.A., Pathapati R.K., Somerson J.S. Smoking cessation prior to total shoulder arthroplasty: a systematic review of outcomes and complications. Shoulder Elbow. 2022 doi: 10.1177/17585732221131916. 17585732221131916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leroux T.S., Basques B.A., Frank R.M., Griffin J.W., Nicholson G.P., Cole B.J., et al. Outpatient total shoulder arthroplasty: a population-based study comparing adverse event and readmission rates to inpatient total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25:1780–1786. doi: 10.1016/j.jse.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Lovy A.J., Keswani A., Beck C., Dowdell J.E., Parsons B.O. Risk factors for and timing of adverse events after total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1003–1010. doi: 10.1016/j.jse.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 20.Ma G.C., Bradley K.E., Jansson H., Feeley B.T., Zhang A.L., Ma C.B. Surgical complications after reverse total shoulder arthroplasty and total shoulder arthroplasty in the United States. J Am Acad Orthop Surg Glob Res Rev. 2021;5 doi: 10.5435/JAAOSGlobal-D-21-00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mehta N., Bohl D.D., Cohn M.R., McCormick J.R., Nicholson G.P., Garrigues G.E., et al. Trends in outpatient versus inpatient total shoulder arthroplasty over time. JSES Int. 2022;6:7–14. doi: 10.1016/j.jseint.2021.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mills E., Eyawo O., Lockhart I., Kelly S., Wu P., Ebbert J.O. Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med. 2011;124:144–154.e8. doi: 10.1016/j.amjmed.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 23.Møller A.M., Pedersen T., Villebro N., Munksgaard A. Effect of smoking on early complications after elective orthopaedic surgery. J Bone Joint Surg Br. 2003;85:178–181. doi: 10.1302/0301-620x.85b2.13717. [DOI] [PubMed] [Google Scholar]
- 24.Morris B.J., Laughlin M.S., Elkousy H.A., Gartsman G.M., Edwards T.B. Preoperative opioid use and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:11–16. doi: 10.1016/j.jse.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Norris T.R., Iannotti J.P. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg. 2002;11:130–135. doi: 10.1067/mse.2002.121146. [DOI] [PubMed] [Google Scholar]
- 26.Ode G.E., Odum S., Connor P.M., Hamid N. Ambulatory versus inpatient shoulder arthroplasty: a population-based analysis of trends, outcomes, and charges. JSES Int. 2020;4:127–132. doi: 10.1016/j.jses.2019.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parada S.A., Flurin P.H., Wright T.W., Zuckerman J.D., Elwell J.A., Roche C.P., et al. Comparison of complication types and rates associated with anatomic and reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30:811–818. doi: 10.1016/j.jse.2020.07.028. [DOI] [PubMed] [Google Scholar]
- 28.Pechacek T.F., Asma S., Blair N., Eriksen M.P. Evidence-based Cardiology. 2002. Tobacco: global burden and community solutions; pp. 103–113. [Google Scholar]
- 29.Previtali E., Bucciarelli P., Passamonti S.M., Martinelli I. Risk factors for venous and arterial thrombosis. Blood Transfus. 2011;9:120–138. doi: 10.2450/2010.0066-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ring J., Shoaib A., Shariff R. Smoking cessation advice in limb reconstruction: an opportunity not to be missed. Injury. 2017;48:345–348. doi: 10.1016/j.injury.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Ross B.J., Wu V.J., McCluskey L.C., O'Brien M.J., Sherman W.F., Savoie F.H. Postoperative complication rates following total shoulder arthroplasty (TSA) vs. reverse shoulder arthroplasty (RSA): a nationwide analysis. Semin Arthroplasty. 2020;30:83–88. doi: 10.1053/j.sart.2020.05.006. 2020/07/01/ [DOI] [Google Scholar]
- 32.Schairer W.W., Nwachukwu B.U., Lyman S., Craig E.V., Gulotta L.V. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2015;24:91–97. doi: 10.1016/j.jse.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 33.Singh J.A., Ramachandran R. Age-related differences in the use of total shoulder arthroplasty over time: use and outcomes. Bone Joint Lett J. 2015;97-b:1385–1389. doi: 10.1302/0301-620x.97b10.35696. [DOI] [PubMed] [Google Scholar]
- 34.Tapson V.F. The role of smoking in coagulation and thromboembolism in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005;2:71–77. doi: 10.1513/pats.200407-038MS. [DOI] [PubMed] [Google Scholar]
- 35.Trofa D., Rajaee S.S., Smith E.L. Nationwide trends in total shoulder arthroplasty and hemiarthroplasty for osteoarthritis. Am J Orthop (Belle Mead NJ) 2014;43:166–172. [PubMed] [Google Scholar]
- 36.Vajapey S.P., Contreras E.S., Neviaser A.S., Bishop J.Y., Cvetanovich G.L. Outpatient total shoulder arthroplasty: a systematic review evaluating outcomes and cost-effectiveness. JBJS Rev. 2021;9:189. doi: 10.2106/jbjs.Rvw.20.00189. [DOI] [PubMed] [Google Scholar]
- 37.Walters J.D., George L.W., 2nd, Walsh R.N., Wan J.Y., Brolin T.J., Azar F.M., et al. The effect of current and former tobacco use on outcomes after primary reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2020;29:244–251. doi: 10.1016/j.jse.2019.05.045. [DOI] [PubMed] [Google Scholar]
- 38.Walters J.D., Walsh R.N., Smith R.A., Brolin T.J., Azar F.M., Throckmorton T.W. Bundled payment Plans are associated with notable cost Savings for ambulatory outpatient total shoulder arthroplasty. J Am Acad Orthop Surg. 2020;28:795–801. doi: 10.5435/jaaos-d-19-00441. [DOI] [PubMed] [Google Scholar]
- 39.Wells D.B., Holt A.M., Smith R.A., Brolin T.J., Azar F.M., Throckmorton T.W. Tobacco use predicts a more difficult episode of care after anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:23–28. doi: 10.1016/j.jse.2017.06.033. [DOI] [PubMed] [Google Scholar]
- 40.Wong J., Lam D.P., Abrishami A., Chan M.T., Chung F. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anaesth. 2012;59:268–279. doi: 10.1007/s12630-011-9652-x. [DOI] [PubMed] [Google Scholar]