Abstract
Background
Chinese herbal medicine (CHM) has been increasingly used for atopic eczema. A previous version of this Cochrane review published in 2004 found some evidence of a possible benefit for oral ingestion of CHM for eczema, but the results were inconclusive and the evidence needs to be updated. We have expanded the scope of this review to include an assessment of the topical and oral effects of CHM for eczema.
Objectives
To assess the effects of oral ingestion and topical applications of CHM for the management of eczema in children and adults.
Search methods
We searched the following databases up to September 2012: the Cochrane Skin Group Specialised Register, CENTRAL in The Cochrane Library (2012, Issue 8), MEDLINE (from 1946), EMBASE (from 1974), AMED (from 1985), LILACS (from 1982), and CINAHL (from 1981). We searched the following from inception: SCOPUS, HERBMED, ProQuest, CQVIP, CNKI, and Wanfang Data. We also searched trials registers, handsearched conference proceedings, checked the reference lists of all included and excluded studies and review articles for further references to relevant trials, and contacted experts in Chinese medicine for unpublished studies.
Selection criteria
All randomised controlled trials (RCTs) in children and adults with eczema comparing CHM to placebo; no intervention; active controls, including acupuncture; or conventional medicines.
Data collection and analysis
Two authors selected the RCTs, extracted data, and assessed quality independently. We contacted study authors for missing data. We collected adverse events from the included studies.
Main results
We included 28 studies, with a total of 2306 participants. We assessed most of the studies at high 'risk of bias', particularly in blinding of participants and personnel, and there was substantial inconsistency between studies, so any positive effect of CHM must be treated with caution. We did not include the four studies from the previous version in this review, because they investigated a CHM product that has been withdrawn from the market since 2004.
Four studies (three oral and one topical) compared CHM to placebo. Pooled data from 2 studies showed the total effectiveness rate in the CHM group was higher (by risk ratio (RR) 2.09, 95% confidence interval (CI) 1.32 to 3.32; 2 studies; n = 85), and the itching visual analogue score (VAS) in the CHM group was 1.53 lower (by standardised mean difference (SMD), 95% CI 2.64 to 0.41; 2 Studies; n = 94) than the placebo group, where a lower VAS score indicates reduced itch. One study of 85 participants with moderate to severe eczema who received an oral CHM formula for 12 weeks reported a quality of life (QoL) score 2.5 lower in the CHM group (by difference in means (MD), 95% CI 4.77 to 0.23; 1 study; n = 85) than the placebo group, where a lower score indicates better QoL.
Twenty‐two studies and 1 arm from a study with a 4‐arm parallel controlled design compared CHM (5 oral, 6 topical, and 12 mixed oral and topical) to conventional medicines. The total effectiveness rate in the CHM groups was superior (RR 1.43, 95% CI 1.27 to 1.61; 21 studies; n = 1868; very low quality evidence), and the itching VAS in the CHM groups was 0.83 lower (SMD, 95% CI 1.43 to 0.22; 7 studies; n = 465) than the comparators.
Two studies compared combined oral and topical CHM to the same oral CHM formula alone. The total effectiveness rate in 1 study was not statistically significant (RR 1.13, 95% CI 0.78 to 1.63; 1 study; n = 20). In the other study, the itching VAS in the CHM group was 1.05 lower (MD, 95% CI 1.75 to 0.35; 1 study; n = 23) than the control group.
With regard to side‐effects, four studies did not give any report of adverse events. The other 24 studies reported minor adverse events, which were reversed soon after stopping CHM. One participant withdrew from one trial because of exacerbation of their condition after using the CHM intervention.
Eight studies received government funding.
Authors' conclusions
We could not find conclusive evidence that CHM taken by mouth or applied topically to the skin could reduce the severity of eczema in children or adults.
Well‐designed, adequately powered RCTs are needed to evaluate the efficacy and safety of CHM for managing eczema.
Keywords: Adult; Child; Humans; Administration, Oral; Administration, Topical; Dermatitis, Atopic; Dermatitis, Atopic/drug therapy; Dermatologic Agents; Dermatologic Agents/therapeutic use; Drugs, Chinese Herbal; Drugs, Chinese Herbal/administration & dosage; Drugs, Chinese Herbal/adverse effects; Randomized Controlled Trials as Topic
Plain language summary
Chinese herbal medicine taken by mouth or applied to the skin for atopic eczema in children and adults
Atopic eczema (eczema in short) is a common skin condition, where skin changes occur and cause redness, scaling, swelling, and skin thickening due to chronic scratching. It is associated with loss of sleep, self‐esteem, and quality of life. The frequency of eczema has increased over the past 10 years.
A former Cochrane review published in 2004 found some evidence of a possible benefit of using oral Chinese herbal medicine (CHM) for eczema; however, the results from only 4 included studies were inconclusive and need to be updated (those four studies have not been included in this update as they investigated a product that has been withdrawn from the market since 2004). As well as updating that review, we have also widened the scope of the review to assess the effects of topical CHM for eczema. We wrote a new protocol to expand the scope of this review.
This review included 28 randomised controlled trials (RCTs), with 2306 children and adults, of which 4 compared CHM to placebo, 22 to conventional medications, and 2 to CHM taken by mouth.
Most of the included studies reported a higher number of participants who had recovered and significantly improved, with less itching in the CHM groups than the control groups. Where CHM was compared to conventional drugs, although the total effectiveness rate outcome was superior with CHM, it was based on very low quality evidence. One study reported that the quality of life (QoL) score in the CHM group was better than in the placebo group after using a CHM formula taken by mouth for 12 weeks. We assessed most of the studies as at high 'risk of bias' and therefore not of good quality, and there was substantial inconsistency between the studies, so any positive effect in CHM must be treated with caution.
One study reported one severe adverse event. Minor adverse events were observed in 24 studies, including temporary elevation of enzymes in 3 cases, which was reversed soon after stopping CHM.
Eight included studies received government funding.
We could not find conclusive evidence that CHM taken by mouth or applied to the skin was of benefit to children or adults with eczema.
Well‐designed, adequately powered RCTs are needed to evaluate the efficacy and safety of CHM for eczema.
Summary of findings
Summary of findings for the main comparison. CHM compared to placebo.
| CHM compared to placebo for atopic eczema | ||||||
| Patient or population: Participants with atopic eczema Settings: Hospital outpatients Intervention: CHM Comparison: Placebo | ||||||
| Outcomes | Illustrative comparative risk* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | CHM | |||||
| Total effectiveness rate (Analysis 1.1) Clinician's rating Follow up: 2 to 4 weeks | Low¹ | RR 2.09 (1.32 to 3.32) | 85 (2 studies) | ⊕⊕⊝⊝ low²,³ | 2 additional studies did not report this outcome. A higher total effectiveness rate indicates improvement of the condition | |
| 1 per 100 | 2 per 100 (1 to 3) | |||||
| High¹ | ||||||
| 40 per 100 | 84 per 100 (53 to 100) | |||||
| Itching VAS (Analysis 1.2) Participant's rating. Scale from 1 to 10 Follow up: 4 to 12 weeks | The mean itching VAS ranged across control groups from 0.2 to 7.8 scores | The mean itching in VAS in the intervention groups was 1.53 standard deviations lower (2.64 to 0.41 lower) | 94 (2 studies) | ⊕⊕⊝⊝ low³,⁴ | Lower score indicates improvement of the condition. 2 additional studies did not report this outcome | |
| Overall severity score (Analysis 1.3) Clinician's rating. Scale from 1 to 80 Follow up: 2 to 16 weeks | The mean overall severity score ranged across control groups from 5.7 to 46.9 scores | The mean overall severity score in the intervention groups was 0.88 standard deviations lower (1.67 to 0.09 lower) | 239 (4 studies) | ⊕⊝⊝⊝ very low²,³,⁴ | Lower score indicates improvement of the condition | |
| QoL (Analysis 1.5) Participant's rating. Scale from 0 to 30 Follow up: 4 to 16 weeks | The mean QoL in the control groups was 10.1 scores | The mean QoL in the intervention groups was 2.5 lower (4.77 to 0.23 lower) | 85 (1 study) | ⊕⊕⊕⊝ moderate³ | Lower score indicates better quality of life. 3 additional studies did not report this outcome | |
| Adverse events (Analysis 1.7) Participant's report Follow up: 2 to 12 weeks | Low¹ | RR 0.71 (0.06 to 8.67) | 129 (2 studies) | ⊕⊕⊝⊝ low²,³ | 1 additional study reported numbers of adverse events that were greater than the total participants. Data were treated as adverse event 'count data' rather than participant level data, which could not be pooled with these 2 studies | |
| 1 per 100 | 1 per 100 (0 to 9) | |||||
| High¹ | ||||||
| 6 per 100 | 4 per 100 (0 to 52) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in the footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
¹The low and high assumed risk values are the two extreme numbers of the events taken from the control groups in the included studies. ²Unclear risk of bias in allocation concealment and high risk of bias in blinding of participants and personnel. ³Total number of events was less than 300. ⁴Unexplained heterogeneity.
1.1. Analysis.
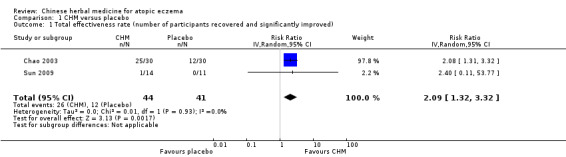
Comparison 1 CHM versus placebo, Outcome 1 Total effectiveness rate (number of participants recovered and significantly improved).
1.2. Analysis.
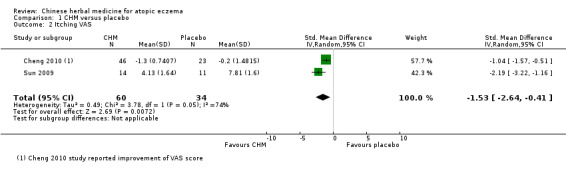
Comparison 1 CHM versus placebo, Outcome 2 Itching VAS.
1.3. Analysis.
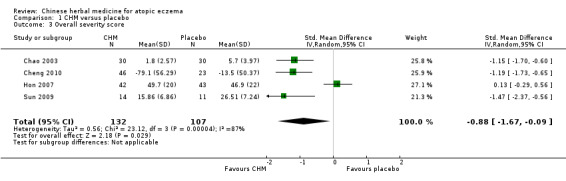
Comparison 1 CHM versus placebo, Outcome 3 Overall severity score.
1.5. Analysis.
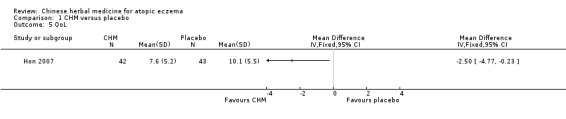
Comparison 1 CHM versus placebo, Outcome 5 QoL.
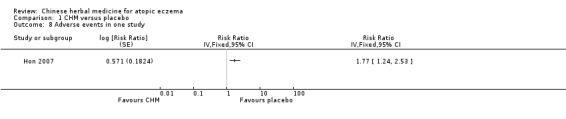
1.7. Analysis.
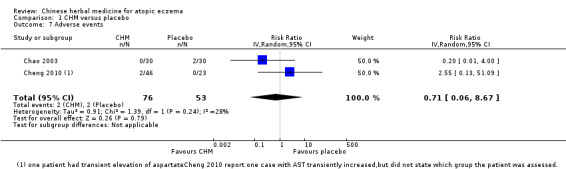
Comparison 1 CHM versus placebo, Outcome 7 Adverse events.
Summary of findings 2. CHM compared to drugs.
| CHM compared to drugs for atopic eczema | ||||||
| Patient or population: Participants with atopic eczema Settings: Hospital outpatients Intervention: CHM Comparison: Drugs | ||||||
| Outcomes | Illustrative comparative risk* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Drugs | CHM | |||||
| Total effectiveness rate (Analysis 2.1) Clinician's rating Follow up: 2 to 52 weeks | Low¹ | RR 1.43 (1.27 to 1.61) | 1868 (21 studies) | ⊕⊝⊝⊝ very low²,³,⁴,⁵ | A higher total effectiveness rate indicates improvement of the condition | |
| 20 per 100 | 29 per 100 (25 to 32) | |||||
| High¹ | ||||||
| 90 per 100 | 100 per 100 (100 to 100) | |||||
| Total effectiveness rate with subgroup analysis ‐ individualised treatment Clinician's rating Follow up: 4 to 8 weeks | Low¹ | RR 1.50 (1.30 to 1.74) | 567 (7 studies) | ⊕⊕⊝⊝ low²,³,⁴ | ||
| 20 per 100 | 30 per 100 (26 to 35) | |||||
| High¹ | ||||||
| 70 per 100 | 100 per 100 (91 to 100) | |||||
| Total effectiveness rate with subgroup analysis ‐ non‐individualised treatment Clinician's rating Follow up: 2 to 52 weeks | Low¹ | RR 1.37 (1.17 to 1.60) | 1301 (14 studies) | ⊕⊝⊝⊝ very low²,³,⁴,⁵ | ||
| 20 per 100 | 27 per 100 (23 to 32) | |||||
| High¹ | ||||||
| 90 per 100 | 100 per 100 (100 to 100) | |||||
| Itching VAS (Analysis 2.3) Participant's rating. Scale from 0 to 10 Follow up: 2 to 12 weeks | The mean itching VAS ranged across control groups from 0.3 to 5.75 scores | The mean itching VAS in the intervention groups was 0.83 standard deviations lower (1.43 to 0.22 lower) | 465 (7 studies) | ⊕⊕⊝⊝ low²,³,⁵ | Lower score indicates improvement of the condition. 16 additional studies did not report this outcome | |
| Overall severity score (Analysis 2.4) Clinician's rating. Scale from 0 to 103 Follow up: 2 to 12 weeks | The mean overall severity score ranged across control groups from 0.3 to 70.82 scores | The mean overall severity score in the intervention groups was 0.97 standard deviations lower (1.23 to 0.71 lower) | 1062 (15 studies) | ⊕⊕⊝⊝ low²,³,⁵ | Lower score indicates improvement of the condition. 8 additional studies did not report this outcome | |
| Adverse events (Analysis 2.6) Participant's reports Follow up: 2 to 52 weeks | Low¹ | RR 0.44 (0.32 to 0.61) | 1396 (15 studies) | ⊕⊕⊝⊝ low²,³,⁴ | 4 additional studies did not report this outcome | |
| 1 per 100 | 0 per 100 (0 to 1) | |||||
| High¹ | ||||||
| 60 per 100 | 26 per 100 (19 to 37) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in the footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
¹The low and high assumed risk values are the two extreme numbers of the events taken from the control groups in the included studies. ²Unclear risk of bias in allocation concealment and high risk of bias in blinding participants and personnel. ³High risk of bias in blinding of outcome assessment. ⁴High risk of bias in other potential sources of bias. ⁵Unexplained heterogeneity.
2.1. Analysis.
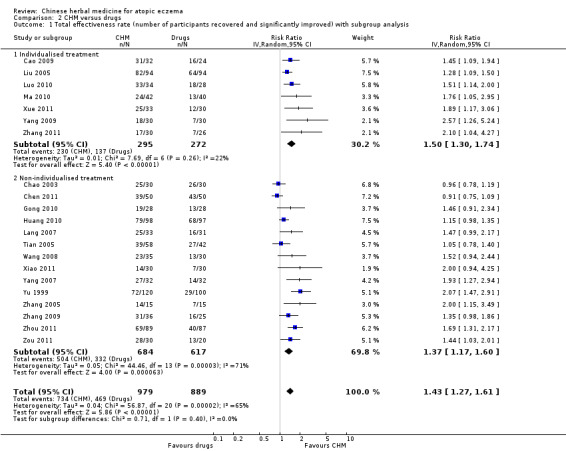
Comparison 2 CHM versus drugs, Outcome 1 Total effectiveness rate (number of participants recovered and significantly improved) with subgroup analysis.
2.3. Analysis.
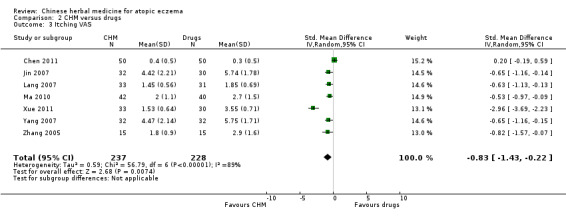
Comparison 2 CHM versus drugs, Outcome 3 Itching VAS.
2.4. Analysis.
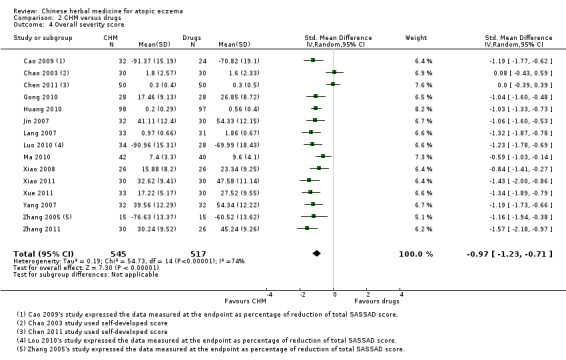
Comparison 2 CHM versus drugs, Outcome 4 Overall severity score.
2.6. Analysis.
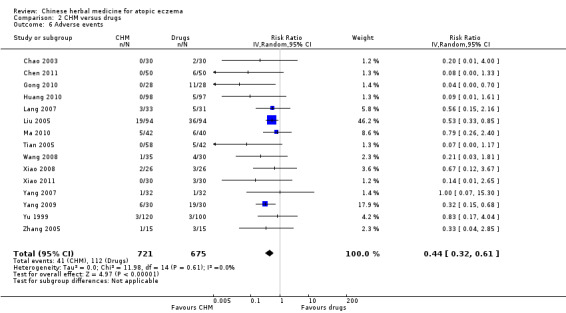
Comparison 2 CHM versus drugs, Outcome 6 Adverse events.
Summary of findings 3. Combination of oral and topical CHM compared to same oral CHM.
| Combination of oral and topical CHM compared to same oral CHM for atopic eczema | ||||||
| Patient or population: Participants with atopic eczema Settings: Hospital outpatients Intervention: Combination of oral and topical CHM Comparison: Same oral CHM | ||||||
| Outcomes | Illustrative comparative risk* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| CHM (oral) | CHM (combination of oral and topical) | |||||
| Total effectiveness rate (Analysis 3.1) Clinician's rating Follow up: 4 to 24 weeks | Moderate | RR 1.13 (0.78 to 1.63) | 20 (1 study) | ⊕⊕⊝⊝ low¹,² | 1 additional study did not report this outcome. A higher total effectiveness rate indicates improvement of the condition | |
| 80 per 100 | 90 per 100 (62 to 100) | |||||
| Overall severity score (Analysis 3.5) Clinician's rating. Scale from 0 to 103 Follow up: 4 to 24 weeks | The mean overall severity score in the control groups was 21.02 scores | The mean overall severity score in the intervention groups was 3.43 lower (7.01 lower to 0.15 higher) | 20 (1 study) | ⊕⊕⊝⊝ low¹,² | Lower score indicates improvement of the condition. 1 additional study was a within‐patient design; data were analysed separately | |
| QoL (Analysis 3.6) Participant's rating. Scale from 0 to 30 Follow up: 4 to 24 weeks | The mean QoL in the control groups was 5.8 scores | The mean QoL in the intervention groups was 0.9 higher (2.89 lower to 4.69 higher) | 20 (1 study) | ⊕⊕⊝⊝ low¹,² | Lower score indicates better quality of life. 1 additional study did not report this outcome | |
| Adverse events (Analysis 3.7) Participant's report Follow up: 4 to 12 weeks | Moderate | RR 1 (0.07 to 13.87) | 20 (1 study) | ⊕⊕⊝⊝ low¹,² | 1 additional study was a within‐patient study, and data on adverse events were analysed separately in this review | |
| 10 per 100 | 10 per 100 (1 to 100) | |||||
| Itching VAS (Analysis 3.3) Participant's rating. Scale from 0 to 10 Follow up: 1 to 2 weeks | The mean itching VAS in the control groups was 5.76 scores | The mean itching VAS in the intervention groups was 1.05 lower (1.75 to 0.35 lower) | 22 (1 study) | ⊕⊕⊝⊝ low¹,²,³ | Lower score indicates improvement of the condition. This was a within‐patient study | |
| Skin lesion score (Analysis 3.4) Clinician's rating. Scale from 0 to 24 Follow up: 1 to 2 weeks | The mean skin lesion score in the control groups was 9.05 scores | The mean skin lesion score in the intervention groups was 1.59 lower (2.92 to 0.26 lower) | 22 (1 study) | ⊕⊕⊝⊝ low¹,²,³ | Lower score indicates improvement of the condition. This was a within‐patient study | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
¹Unclear risk of bias in allocation concealment and high risk of bias in blinding of participants and personnel. ²Total number of events was less than 300. ³High risk of bias in incomplete outcome data.
3.1. Analysis.
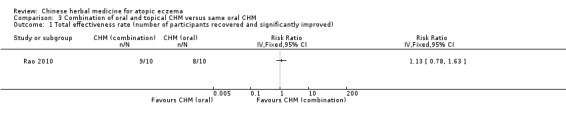
Comparison 3 Combination of oral and topical CHM versus same oral CHM, Outcome 1 Total effectiveness rate (number of participants recovered and significantly improved).
3.5. Analysis.
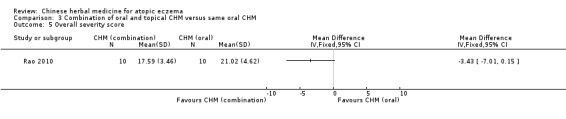
Comparison 3 Combination of oral and topical CHM versus same oral CHM, Outcome 5 Overall severity score.
3.6. Analysis.
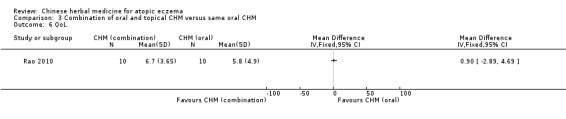
Comparison 3 Combination of oral and topical CHM versus same oral CHM, Outcome 6 QoL.
3.7. Analysis.
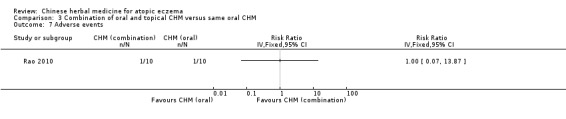
Comparison 3 Combination of oral and topical CHM versus same oral CHM, Outcome 7 Adverse events.
3.3. Analysis.
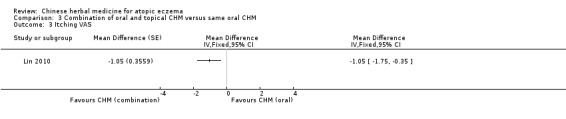
Comparison 3 Combination of oral and topical CHM versus same oral CHM, Outcome 3 Itching VAS.
3.4. Analysis.
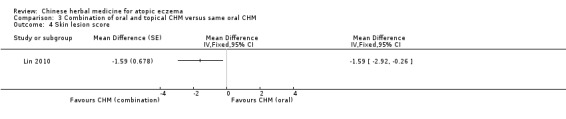
Comparison 3 Combination of oral and topical CHM versus same oral CHM, Outcome 4 Skin lesion score.
Background
Description of the condition
Atopic eczema is a common skin condition, which affects around one in five children in developed countries. In 2009, the International Study of Asthma and Allergies in Childhood (ISAAC) published data on symptoms of eczema (Odhiambo 2009). In this study, the authors found in 6 to 7 year‐old children from 143 centres in 60 countries, disease prevalence ranged from 0.9% in India to 22.5% in Ecuador. Amongst 13 to 14 year‐olds from 230 centres in 96 countries, disease prevalence was found to range from 0.2% in China to 24.6% in Colombia. Industrialised countries have previously been reported to have higher disease prevalence (Kerdel 2003; Schultz‐Larsen 2002), although data from this most recent ISAAC study (Odhiambo 2009) suggest that eczema is a disease in developing countries as well, especially in Latin America and some countries in Africa. The prevalence of atopic eczema has increased over the last 10 years in both developed and developing countries, especially in those aged 6 to 7 years (Williams 2008), for reasons that are unclear. The causes of atopic eczema are still not fully understood, but probably involve an interaction between genetic factors that determine the integrity of the skin barrier and immune responses, and environmental factors, such as early‐life gut bacteria; humidity; irritation from soaps; microbes, such as Staphylococcus aureus; and allergens, such as house dust mites. Most children with atopic eczema improve with time, but around 40% persist with the condition into adulthood (Williams 2000).
There was no such terminology as 'atopic eczema' in the classical literature of ancient Chinese medicine. The definition of 'Si Wan Feng' (wind of the four fossae) in Chinese medicine however correlates to atopic eczema in conventional medicine based on the comparison of Chinese medical literature records and the descriptions of clinical features in conventional medicine. 'Si Wan Feng' in Chinese medicine was officially defined as atopic eczema in the Criteria of Diagnosis and Therapeutic Effect of Disease and Syndromes in Traditional Chinese Medicine published by the State Administration of Traditional Chinese Medicine, China (SATCM 1994). Although the term 'atopic' eczema is frequently used, not all people with typical atopic eczema are truly atopic; that is, they do not demonstrate specific immunoglobulin E (IgE) antibodies to common environmental allergens, such as house dust mite, pollens, grass, and foods (Flohr 2008). In accordance with the World Allergy Organisation recommendations on nomenclature (Johansson 2004), we used the term 'eczema' throughout this review.
Eczema is characterised by poorly demarcated redness of the skin and associated surface changes, such as scaling, swelling (oedema), accentuation of the hair follicles, and skin thickening (lichenification) as a result of chronic scratching. Eczema is an itchy skin condition, which can result in sleep loss for the child and family members. The stigma of a visible skin disease can affect a person's self‐esteem, and severe disease is associated with a poor quality of life (QoL) (Schmid‐Ott 2003).
Description of the intervention
Current treatment for eczema has limitations. Topical administration of corticosteroids, as one of the standard first‐line therapies for the management of inflammatory episodes of eczema, can be associated with certain adverse events, such as skin thinning, if used for too long or in a too‐strong concentration for sensitive sites, such as the face where the skin is naturally thinner. Long‐term application of steroids has been a great concern to those using them and to healthcare professionals (Hanifin 2004). A study showed up to 72.5% of people who were using steroids (or their guardians) were concerned about the application of corticosteroids for the treatment of eczema (Charman 2000). New drugs for the treatment of eczema, such as tacrolimus and pimecrolimus (these two drugs are categorised as topical immunomodulators (TIMs) or calcineurin inhibitors), have been developed as second‐line therapies. However, issues regarding the long‐term safety of these new drugs, particularly the potential link between TIMs and cancer, have been raised (CDER 2005). Therefore, many eczema sufferers have chosen to use complementary and alternative medicine, including Chinese herbal medicine (CHM), for the management of eczema (Hon 2005).
How the intervention might work
In Chinese medicine, those with eczema are recognised as having a specific constitution that leads to internal dampness‐heat accumulated because of the reduced function of the spleen. Exposure to wind, dampness, and heat pathogens can trigger symptoms (Zhao 1983). Clinically, eczema is classified into the following patterns from a Chinese medicine viewpoint: accumulation of internal dampness, excess of dampness with spleen deficiency, or Yin deficiency with dryness of blood (Chen 1991). Chinese herbal medicine is one of the important components in Chinese medicine for prevention and treatment of diseases. Botanical resources, such as barks, seeds, flowers, roots, or animal or mineral substances, are prescribed and administered in the form of decoctions (liquids from extraction of herbs by boiling), pills, washing lotions, or ointments for conditions diagnosed by practitioners qualified to practice Chinese medicine or Oriental medicine. Chinese herbal medicines may be neither Chinese nor herbal; the term CHM in this review is used loosely to refer to any medicinal substances used within the paradigm of Chinese medicine practice. Chinese herbal medicines have been employed for the treatment of eczema for many years. They may be administered orally or topically or by a combination of oral ingestion and topical application (Chen 2001). Oral ingestion of CHM is under the guidance of the Chinese medicine pattern differentiation method, known as 'individualised treatment', whilst topical administrations have been devised with little or no consideration of pattern differentiation (Guo 2007; Zhou 2008).
Why it is important to do this review
The Cochrane systematic review on oral ingestion of CHM for eczema was published in 2004 (Zhang 2004). It is timely to update this review to take into account new evidence that has emerged in relation to oral ingestion of herbal interventions. Furthermore, there has been no systematic evaluation of the effectiveness and safety of the topical application of CHM for eczema.
We decided it would be best to review both oral ingestion and topical CHM since people with eczema are likely to be interested in both types of treatment. We therefore wrote a new protocol to plan for the expanded scope of this review.
Objectives
To assess the effects of oral ingestion and topical applications of CHM for the management of eczema in children and adults.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled clinical trials (RCTs) with or without blinding, regardless of language.
Types of participants
We included adults or children (from 1 month to 16 years old) with eczema. We accepted diagnostic criteria, such as the Hanifin and Rajka definition (Hanifin 1980) or the UK refinement (Williams 1994), when using the terms 'atopic eczema' or 'atopic dermatitis'. In the absence of explicit diagnostic criteria, we excluded adults diagnosed with 'eczema' or 'chronic eczema', but accepted children diagnosed with 'eczema' by physicians or dermatologists.
Types of interventions
Oral ingestion and topical applications of a single Chinese medicinal herb or formula, manufactured or clinician self‐designed Chinese medicinal formulae (a clinician self‐designed formula is usually composed of different types of Chinese herbs prescribed by a Chinese medicine practitioner who determines the selection of herbs based on a person's condition), compared to the following control interventions: placebo, no intervention, and active controls, including acupuncture or conventional medicines.
We also included trials with a combination of oral ingestion and topical interventions.
We excluded interventions based on individualised treatment unless there were appropriate control interventions.
Types of outcome measures
Primary outcomes
Percentage of trial participants with at least good or excellent improvement in terms of investigator global score. We included both short‐term (within six weeks) and long‐term (more than six weeks) improvement.
Percentage of trial participants with at least good or excellent improvement in terms of participants' or parents' global score. We included both short‐term (within six weeks) and long‐term (more than six weeks) improvement.
Secondary outcomes
Changes in participant‐ or parent‐rated global improvement in EASI (Eczema Area and Severity Index), SCORAD (Severity Scoring of Atopic Dermatitis), POEM (Patient‐oriented Eczema Measure), or SASSAD (Six Area, Six Sign Atopic Dermatitis) (Schmitt 2007) as stated in each of the trials in both the short‐term (within six weeks) and the long‐term (more than six weeks).
Changes in participant‐ or parent‐rated global improvement in quality of life, such as CDLQI (Children's Dermatology Life Quality Index) or DLQI (Dermatology Life Quality Index) in both the short‐term (within six weeks) and the long‐term (more than six weeks).
Adverse events.
Search methods for identification of studies
We aimed to identify all relevant RCTs regardless of language or publication status (published, unpublished, in press, or in progress).
Electronic searches
We searched the following databases up to 11 September 2012:
the Cochrane Skin Group Specialised Register using the following terms: ((Chinese and (herb* or medicin* or traditional or plant*)) or “traditional medicin*” or “traditional therap*” or ((orient* or herbal) and (medicin* or therap*)) or phytotherapy or phytopharmaceutic* or (plant and (medicin* or extract*))) AND (dermatitis OR (besnier* AND prurigo) OR eczema);
the Cochrane Central Register of Controlled Trials (CENTRAL), issue 8, 2012, in The Cochrane Library using the search strategy in Appendix 1;
MEDLINE via OVID (from 1946) using the strategy in Appendix 2;
EMBASE via OVID (from 1974) using the strategy in Appendix 3;
AMED via OVID (Allied and Complementary Medicine, from 1985) using the strategy in Appendix 4;
LILACS (Latin American and Caribbean Health Science Information database, from 1982) using the strategy in Appendix 5; and
CINAHL via EBSCO (Cumulative Index to Nursing and Allied Health Literature, from 1981) using the search strategy in Appendix 6.
A final prepublication search for this review was undertaken on 6 June 2013. Although it has not been possible to incorporate RCTs identified through this search within this review, we listed relevant references under Studies awaiting classification. We will incorporate them into the next update of the review.
We searched the following databases up to 13 September 2012:
Scopus (from 1996) using the terms (eczema or dermatitis) AND (Chinese) AND (random$);
HerbMed® (from 1998) using the terms (eczema or dermatitis) AND (Chinese) AND (random$); and
ProQuest (from 1938) using the terms (atopic eczema or atopic dermatitis) AND (Chinese medicine) AND (random$).
We also searched the following databases in the Chinese language up to 13 September 2012:
CQVIP (Chongqing VIP Information Co., Ltd,) Chinese Scientific Journals Fulltext Database (from 1989) using the strategy in Appendix 7 in Chinese;
CNKI (China National Knowledge Infrastructure) (from 1979) using the strategy in Appendix 8 in Chinese;
Wanfang Data (from 1982) using the strategy in Appendix 9 in Chinese;
Chinese Scientific Journal Net (from 1994) (the database has been merged into CQVIP); and
China Proceedings of Conference Database (from 1994) (the database has been merged into CQVIP).
Trials Registers
We searched for reports of trials in the following trials databases up to 13 September 2012:
The metaRegister of Controlled Trials (www.controlled‐trials.com).
The US National Institutes of Health Ongoing Trials Register (www.clinicaltrials.gov).
The Australian New Zealand Clinical Trials Registry (www.anzctr.org.au).
The World Health Organization International Clinical Trials Registry platform (www.who.int/trialsearch).
The Ongoing Skin Trials Register (www.nottingham.ac.uk/ongoingskintrials).
Searching other resources
Handsearching
We handsearched the conference proceedings ‐ relevant to eczema ‐ of the First World Congress of Chinese Medicine from 2003 onwards. We also handsearched conference proceedings of the Conference of Skin Diseases: Integrating Chinese and Western Medicine 2007, and the 1st International Dermatology Academic Symposium of TCM and Integrated TCM‐WM (traditional Chinese medicine and Western medicine) 2009.
Reference lists
We checked the reference lists of all identified RCTs and review articles for further references to relevant trials.
Adverse effects
We did not perform a separate search for adverse effects of the target interventions. However, we examined data on adverse effects from the included studies we identified.
Correspondence
On 13 December 2011, 18 September 2012, and 17 June 2013, we contacted the clinicians, dermatologists, and experts in traditional Chinese medicine listed in Appendix 10 and requested information on any unpublished RCTs on our topic.
Data collection and analysis
If the data on the number of participants with each outcome measure were not available in the published paper, we contacted the study author for further information. We also contacted all study authors of included trials for their raw data where they had not reported the outcomes in such a way that meta‐analysis was possible.
Selection of studies
Two authors (SG and AWY) selected the trials or studies independently according to the inclusion criteria. We screened papers through reading the titles and abstracts and retrieved full texts of the potential included studies for further assessment. We resolved discrepancies of the assessments by discussion between SG and AWY. The other two team members, HCW and WZ, provided arbitrating advice when we could not achieve a consensus.
Data extraction and management
Two authors (SG and AWY) independently extracted the data from the included studies onto a data extraction form developed by the Cochrane Skin Group, which we modified to suit this review. We extracted characteristics of participants, interventions, and outcome measures. Data from each selected study consisted of the number of events (n) and participants (N) for dichotomous data; and number of participants (N), and mean and standard deviations (SD) for continuous data.
We resolved discrepancies in data extraction by discussion between SG and AWY or through other arbitrating team members, HCW and WZ, when we could not achieve a consensus.
Assessment of risk of bias in included studies
We adopted The Cochrane Collaboration's domain‐based evaluation for assessing risk of bias, which included the following domains:
(a) sequence generation; (b) allocation concealment; (c) blinding of participants, personnel, and outcome assessors; (d) incomplete outcome data (missing data were analysed by worst‐case scenarios. The funnel plot analysis was tested for potential publication bias); and (e) selective outcome reporting and other sources of bias.
We presented the risk of bias for each included study as part of its Characteristics of included studies table in the review, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We set an additional quality criterion of whether the study used published and validated scoring systems (i.e. EASI, SCORAD, POEM, or SASSAD) under the heading of "use of published validated scoring systems" to record the severity of the disease (Schmitt 2007).
Measures of treatment effect
The total effectiveness rate and the number of adverse events were dichotomous data. As the included studies compared the events in 2 groups, we expressed dichotomous data as risk ratios (RR) with 95% confidence intervals (CI). A higher total effectiveness rate indicates better improvement of the condition. We planned to express dichotomous data as number needed to treat (NNT). We planned to express NNTB (number needed to treat for an additional beneficial outcome) for beneficial outcome and NNTH (number needed to treat for an additional harmful outcome) for harmful events as recommended by theCochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The baseline event rate includes the control event rate (CER) and the experimental event rate (EER) for calculation of NNT. We planned to use a plausible range of CERs from the individual trials. An NNTB range of two to four should indicate that the interventions are effective, which should imply a beneficial outcome.
The scores of itching VAS, global symptom improvement scores, and QoL were continuous data. We expressed them as difference in means (MD) with 95% CI. As outcome scales used in the included studies were various, we also expressed the continuous data as standardised mean differences (SMD) with 95% CI, where different outcome scales were pooled.
Studies with multiple treatment groups
For studies with more than two interventions, we selected the comparison group that met the inclusion criteria.
Unit of analysis issues
We considered unit of analysis issues if a study involved measurements on different body parts, such as comparison of a site on one arm versus another site on the other arm for topical interventions. In this case, we treated the study as a 'within‐patient trial', and we performed a separate meta‐analysis as appropriate.
For cross‐over trials where participants were given different treatments in random sequence, we planned to undertake a separate meta‐analysis. The results from the first phase could be combined with those from the parallel trials if data were available.
We planned to combine the data from included parallel studies and the first period of included cross‐over studies in the meta‐analysis. We planned to include cross‐over studies only if their methods were appropriate as suggested in the Cochrane Handbook for Systematic Reviews of Interventions.
Dealing with missing data
We contacted the trial author of a study for more information if there were any missing data in the trial. We applied intention‐to‐treat (ITT) analysis to the included studies in which there were missing individuals.
Assessment of heterogeneity
We assessed heterogeneity (inconsistency) in included studies by using the I² statistic, which describes the percentage of variation across studies due to heterogeneity rather than by chance.
Assessment of reporting biases
We tested funnel plot asymmetry where there were more than 10 trials included in the meta‐analysis.
Data synthesis
We anticipated that the nature of the interventions would be quite diverse, and it was therefore unlikely that they would all estimate the same treatment effect. It was in fact that the studies in our review estimated different, yet related, intervention effects, and for this reason, we conducted a random‐effects model when attempting to pool data from several studies. We performed the meta‐analyses irrespective of the level of heterogeneity for the purpose of explanation of potential inconsistency across the included studies. When substantial heterogeneity was found (I² statistic greater than 50%), then we explored the sources of such heterogeneity by rechecking the data, and by subgroup analysis based on clinical and methodological diversity factors.
We performed meta‐analysis by using the inverse‐variance method in Review Manager 5 (RevMan), as outlined in the Cochrane Handbook for Systematic Reviews of Interventions, for effect estimates from the collected data.
We reported studies relating to adverse events quantitatively.
Subgroup analysis and investigation of heterogeneity
We planned to perform subgroup analyses under the heading of "children (16 years old or under) with eczema versus adults with eczema", and "application of intervention based on Chinese medicine syndrome differentiation versus non‐individualisation formula" where there were at least moderate levels of heterogeneity across the included studies. We investigated the sources of heterogeneity including participant factors (e.g. age, diagnosis, sex, race, comorbidity), treatment factors (e.g. dosage, formulation), study factors (e.g. concordance rates, quality of reporting), and quality control for the Chinese herbal preparations (e.g. source, purity, preparation facilities) to explain such differences.
Sensitivity analysis
We planned to perform sensitivity analyses of the primary outcomes by excluding studies of low methodological quality. Where substantial heterogeneity existed between studies for the primary outcome (I² statistic > 50%), we were to seek sources for such heterogeneity, such as quality of disease definition or composition or dose of the herbal medication, and explore them in sensitivity analyses. However, we were unable to carry out these analyses due to the lack of data.
Results
Description of studies
Results of the search
We identified a total of 1740 records through thorough searches. We excluded 1674 records after screening the titles and abstracts. Of the remaining 66 records, we found that 3 were registered trials, and we classified them as 'ongoing studies'. We retrieved full texts of the remaining 63 records. Of these, we excluded 20 as they were not randomised controlled trials. We excluded another four studies because their comparison interventions did not meet the inclusion criteria of this review (see Excluded studies). We need further information about nine studies in order for us to make a decision about their inclusion or exclusion. We listed these in the 'Characteristics of studies awaiting classification' tables while we wait for further details from the trial investigators. Of the remaining 30 records, we found 1 was a protocol for a study that has been completed, but no final report has been published, and we added this to the 3 records we found that were ongoing trials. We listed details of these four registered trials in the 'Characteristics of ongoing studies' tables and hope that these can be included in a future revision of this review once the trial reports are published. We included 28 studies (from 29 records; 1 study was reported twice, and we have included the 2 identical trials under the same study ID: Hon 2007). We summarised the screening process in our 'Study selection flow diagram' (Figure 1).
1.
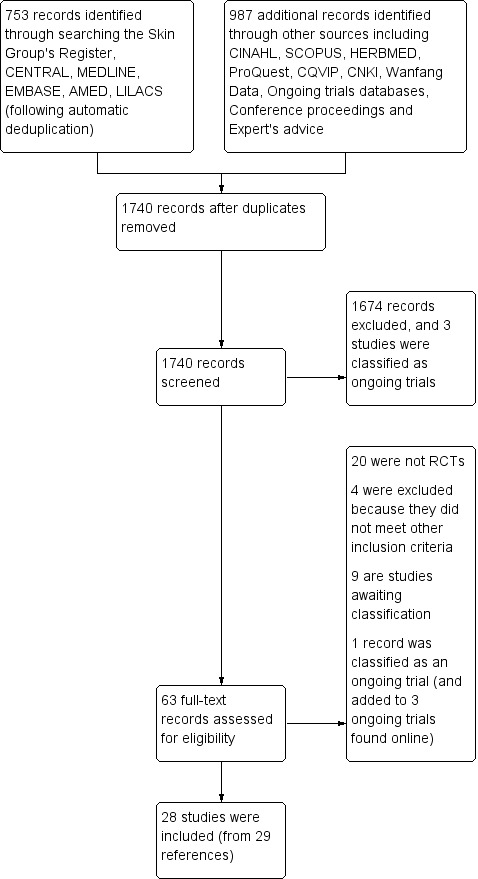
Study selection flow diagram
Included studies
We included 28 studies, with a total of 2306 participants.
Design
All 28 included studies were randomised controlled parallel clinical studies with oral ingestion or topical applications of CHM for eczema, except the Lin 2010 study, which used CHM topically on a randomised selected arm or leg of the participant for comparison with the other non‐treatment site on the same participant.
None of the included studies were cross‐over trials, but one study (Lin 2010) was a within‐patient trial, and we treated data as if they were obtained from the first phase of a cross‐over trial (Higgins 2011).
The sample sizes of the studies ranged from 25 to 220, with a total of 2306 participants aged from 12 days to 65 years.
We listed details of the included studies in the 'Characteristics of included studies' tables.
Setting
All of the included studies were conducted in public hospitals (most of them were in Chinese medicine teaching hospitals) in mainland China, Hong Kong, or Taiwan, where Chinese medicine has a long history of practice and widespread applications in the healthcare system. The majority of the included studies were published in Chinese. Two studies were printed in English (Cheng 2010; Hon 2007).
Treatment duration
Treatment duration ranged from 5 days to 16 weeks in the included studies. Among the 28 included studies, 13 studies reported follow‐up, and the follow‐up periods ranged from 4 to 52 weeks after treatment stopped.
Funding
Eight studies reported receiving funding or support from governments (Cheng 2010; Gong 2010; Hon 2007; Ma 2010; Sun 2009; Xue 2011; Yang 2007; Yu 1999).
Interventions
All of the studies used a combination of CHM originated from plants or animal or mineral products as an active intervention.
1. CHM versus placebo
We found four studies that compared CHM to placebo (Chao 2003; Cheng 2010; Hon 2007; Sun 2009). Three studies used oral ingestion of interventions (Cheng 2010; Hon 2007; Sun 2009), and one study administered the interventions via topical application (Chao 2003).
The Chao 2003 study was a four‐arm parallel randomised controlled trial. It treated 120 children aged from 1 to 38 months (mean = 7 months) with 5% (1st arm) or 10% (2nd arm) of Huangbai Zicao Diyu cream, econazole nitrate cream (Pevisone®) (3rd arm), or placebo (petroleum jelly) (4th arm), respectively, for 2 to 3 weeks. We did not use data from the 1st arm as the 2nd arm showed a higher effectiveness rate than the 1st arm. We analysed data from the 2nd arm compared to the 4th arm (CHM versus placebo) and the 2nd arm compared to the 3rd arm (CHM versus conventional medicines) in the Effects of interventions section.
The Cheng 2010 study randomised 71 participants with a mean age of 13 in a ratio of 2:1 who were treated with Chinese herbal decoction of Xiao‐Feng‐San granules or placebo for 8 weeks. Follow‐up assessment was done after an eight‐week treatment period. The Hon 2007 study recruited a total of 85 participants aged from 5 to 21 years (mean = 11 years) with moderate‐to‐severe eczema (objective SCORAD > 15). Chinese herbal medicine capsules containing 5 Chinese herbs or placebo were used for 12 weeks, and the study conducted follow‐up at week 16 of the trial period. The Sun 2009 study prescribed Jianpi Shenshi granules with 10 Chinese herbs or placebo to 25 participants aged from 3 to 20 years old (mean = 9 years) for 4 weeks. Follow‐up assessment was conducted at 24 weeks after the treatment period. All four studies allowed other medicines in both groups.
2. CHM versus conventional medicines (drugs)
We found 22 studies plus the Chao 2003 study where one of its 4 arms compared the effects of CHM to drugs.
a) Oral ingestion (five studies)
There were 62 participants aged from 10 to 52 years old, with a mean age of 20 years, randomly assigned to the treatment or control group in the Jin 2007 study. Jianpi Zhiyang granules with 12 CHMs or loratadine tablet (an antihistamine medication) were given to the participants for 4 weeks.
The Luo 2010 study recruited 62 children with a mean age of 9, who they treated with Xiao‐Feng‐San decoction and individualised modifications, loratadine, or another antihistamine drug for 16 weeks.
The Yang 2009 study used a formula containing 9 herbs and recruited 60 children or adults aged from 4 to 27 years, with a mean age of 16, for 4 weeks of treatment. The Yang 2009 study also used the loratadine tablet as the control intervention.
The Yu 1999 study had the largest sample size (220 participants) among the 28 included studies. Piyan Xiaojingyin granules II composed of more than 5 herbs were given to participants aged from 5 to 53 years old (mean = 13 years). The loratadine tablet was the control intervention, and both groups were supplied with saline or zinc oxide cream for 12 weeks. The study conducted follow‐up assessment at 52 weeks after the treatment period.
The Zhang 2011 study reported that they used a clinician self‐designed CHM formula with modifications based on individual cases or levocetirizine dihydrochloride tablets (an antihistamine medication) for treatment of 56 children aged from 2.5 to 14 years old (with a mean age of 7 years) for 8 weeks. The study conducted follow‐up assessment at 24 weeks after the 8‐week treatment period.
b) Topical application (six studies)
The Chao 2003 study compared the effects of CHM to econazole nitrate cream (Pevisone®), which was composed of 1% of econazole nitrate (antifungal medication) and 0.1% of triamcinolone acetonide (corticosteroid) in its 3rd arm.
The Chen 2011 study randomly entered 100 children (aged from 58 days to 2 years old) into the treatment or control groups, and they were treated with Huanglian Qingdai cream made from 6 herbs or mometasone furoate cream (a corticosteroid) for 2 weeks.
There were 65 boys and girls aged from 12 days to 11 months (mean = 5 months) in the Wang 2008 study, which used Chushi Zhiyang ointment, a manufactured CHM product made up of 13 Chinese herbs, topically for 1 week. The study employed vitamin B₆ cream (a moisturising agent) as the control intervention.
The Huang 2010 study recruited 195 participants aged from 3 months to 22 years old, with a mean age of 12 years, who were treated with Chushi Zhiyang ointment, which was the same CHM product used in the Wang 2008 study, or clobetasol propionate ointment (a corticosteroid) for 2 weeks. The study performed follow‐up assessment at 12 weeks after the treatment period.
The Zhou 2011 study treated 176 children aged 3 to 38 months old (mean = 10 months) with Cang Er Kushen lotion, which had 13 Chinese herbs, or calamine lotion (an anti‐itching agent), which they used topically as the control intervention for 2 weeks. The study conducted follow‐up assessment 24 weeks after the treatment period.
The Zou 2011 study randomised 50 children aged from 3 to 36 months, with a mean age of 16 months. Moist dressing with a CHM lotion composed of nine herbs and topical application with the same herbal powder mixed with sesame oil were used for two weeks. Boric acid solution (an antiseptic agent) and zinc oxide cream (a moisturising agent) served as control interventions.
c) Combination of oral ingestion and topical application (twelve studies)
The included studies in this group used CHM by oral ingestion and topical application in their treatment groups for comparison of the effect to the control groups.
The Cao 2009 study treated 56 children aged from 2 to 16 years (mean = 8 years) with Zhuling Jianpi Huashi decoction (which could be modified when the condition of an individual participant changed) or with oral ingestion of cetirizine hydrochloride drops (an antihistamine medication) for 1 to 4 weeks. There were 12 herbs in the Zhuling Jianpi Huashi decoction used in this study. The Zhang 2005 study also evaluated the same CHM decoction (although the name of the formula was changed).
The Gong 2010 study randomised 56 adults aged from 16 to 65 years old (mean = 37 years) into the treatment or control group and treated them with Liangxue Xiaofeng decoction composed of 13 herbs or oral ingestion of desloratidine (an antihistamine medication) for 4 weeks.
The Lang 2007 study used Shengui decoction with 8 herbs and Shidu ointment for the treatment group for 4 weeks, and oral ingestion of loratadine tablets and 1% hydrocortisone cream (a corticosteroid) topically as control interventions for 72 participants aged from 3 to 34 years old (mean = 17 years).
The Liu 2005 study recruited 184 children and adults aged from 3 months to 42 years old (mean not provided) for 4 to 8 weeks of treatment. The participants were treated with oral ingestion of Cangyi decoction with individualised modifications and Qingdai ointment and Huangbai lotion topically in the treatment group, or they were treated with terfenadine tablet (an antihistamine medication) and 0.025% dexamethasone cream (a corticosteroid) as control interventions. There were 12 herbs in the Cangyi decoction, and the ingredients of the topically used CHM interventions were unknown in this study.
The Ma 2010 study treated 82 children and adults aged from 7 to 33 years old (mean = 18 years) with loratadine tablet or Jianpi Runfu decoction containing 11 herbs. The oral ingestion of CHM could be modified based on the individual's condition in the study, and Zicao oil or butyl flufenamate cream (an anti‐inflammatory medication) was also used topically in the treatment group or control group, respectively, for four weeks.
The Tian 2005 study treated 100 participants (did not report the range of age) with oral ingestion of Fuyang granules composed of 5 herbs and used the same formula for topical application or oral ingestion of cyproheptadine tablet (an antihistamine medication) plus 3% sulphur cream (an antiseptic agent) externally for only 5 days.
The Xiao 2008 study used oral ingestion and external application of Machixian decoction as a basic formula, which was modified according to an individual's condition. The control interventions were chlorphenamine tablet (an antihistamine medication) and 3% boric acid solution. There were a total of 52 participants aged from 3 to 23 years old (mean = 13 years) in this study, and treatment duration was 8 weeks with follow‐up assessment at 12 weeks after the treatment period.
The Xiao 2011 study recruited 60 participants aged from 2 to 60 years old (mean = 12 years) and provided 4 weeks of treatment with Huailian decoction composed of 12 herbs, and loratadine tablet was the control oral ingestion intervention. External use of nitrofurazone, calamine, menthol, and CHM ointment were also provided to both groups.
The Xue 2011 study used Shengxue Runfu decoction composed of 15 herbs. The formula could be modified depending upon an individual's condition, and loratadine was the control oral ingestion intervention for an 8‐week treatment. There were 63 boys and girls ranged from 2 to 12 years old (mean = 7 years) in this study. Topical application of CHM ointment and emollients were employed for both groups.
The Yang 2007 study used the same oral ingestion of CHM intervention as the Jin 2007 study. The two studies were conducted at the same department of a Chinese medicine hospital in Shenzhen, China. The Yang 2007 study however also used CHM ointment topically with a total of 64 participants from 5 to 25 years old (mean = 7 years) who were treated with Chinese herbs or oral ingestion of loratadine tablet and 1% hydrocortisone butyrate cream (a corticosteroid) for 4 weeks.
The Zhang 2005 study recruited 45 children under 16 years old (mean = 8 years) and compared the efficacy of a CHM decoction to chlorpheniramine tablet for 12 weeks in 3 groups of participants. In this study, CHM lotion or CHM ointment were also used topically according to an individual's condition in all the groups.
Finally, the Zhang 2009 study treated 61 children aged from 2 to 12 years old (mean not provided) with Xiao'er Huashi decoction (composed of 13 herbs) or loratadine granules for 4 weeks. External use of CHM lotion and CHM cream were provided to both groups.
3. Combination of oral and topical CHM interventions versus same oral CHM alone
We found two studies comparing the effects of a combination of oral and topical CHM to the same oral CHM formula alone (Lin 2010; Rao 2010). The Lin 2010 study used Runfu Xiaoyan lotion composed of 4 herbs applied externally on a randomly selected site of the limb (which had received no previous treatment with regard to the topical intervention) of 23 participants aged from 11 months to 27 years old (mean = 10 years) for 2 weeks. The Lin 2010 study also used oral ingestion of Qingxin Peitu decoction for moderate and severe cases.
The Rao 2010 study was a 3‐arm parallel controlled design of 12 weeks' treatment duration, which recruited 30 participants aged from 7 to 25 years old (mean = 15 years). The treatment group (the first arm) received Qingxin Peitu decoction with individualised modifications plus external use of Qingxin Peitu lotion. The second‐arm group was treated with the same oral ingestion of the intervention but no topical intervention, and the third‐arm group used oral ingestion of placebo plus oral ingestion of cetirizine hydrochloride tablet and topical application of mometasone furoate cream. We did not use data from the third‐arm group in this review as there was no appropriate comparator for this group.
Outcomes
With regard to our first primary outcome, the trial investigators in most of the included studies converted the measure score into effectiveness rate without reporting the actual score. Thus, we accepted that a 'recovery' was where there was > 90% reduction of the investigator global score, and a 'significant improvement' was > 70% reduction of the score as stated by the trial investigator(s). A total effectiveness rate was a sum of effectiveness rates expressed as 'recovery' and 'significant' by the trial investigator(s) of the included studies. A higher total effectiveness rate indicates better improvement of the condition.
With regard to our second primary outcome, most of the included studies measured severity of itching score and expressed this as a participant‐rated visual analogue score (VAS). Thereafter, we extracted continuous data in mean values, standard deviations (SD), and total numbers of events assessed at the end point of the trial as one of the primary outcome measures to replace the percentage of trial participants that we planned.
With regard to our third secondary outcome, we extracted adverse events in a data extraction form for all included studies. A severe adverse event was an adverse effect that led a participant to withdraw from the study. A minor adverse event was one reported by the participant or clinician but that was not serious and the person still completed the treatment.
With regard to short‐term or long‐term improvement of a relevant outcome, the short‐term improvement was an outcome measured within six weeks in the follow‐up period after stopping the treatment. The long‐term improvement was an outcome measured more than six weeks into the follow‐up period after stopping the treatment.
Excluded studies
We excluded four studies because their comparison interventions did not meet the inclusion criteria of this review. Please see the 'Characteristics of excluded studies' tables.
Risk of bias in included studies
Two authors (SG and AWY) independently assessed the risk of bias in the included studies and resolved discrepancies of the assessments by discussion. The other two team members, HCW and WZ, provided arbitrating advice when a consensus could not be achieved. We assessed risk of bias and provided a brief rationale for our judgment for each study (see the 'Risk of bias' tables, which are an extension of the 'Characteristics of included studies' tables). Overall, the risk of bias in the included studies was high for blinding of participants and research personnel and unclear for the other domains. Our judgements according to the published data about each 'Risk of bias' item presented as percentages across all included studies are shown in Figure 2. We summarised our judgements, which we based on The Cochrane Collaboration's domain‐based evaluation for "assessing risk of bias" about each 'Risk of bias' item for each included study, in Figure 3.
2.
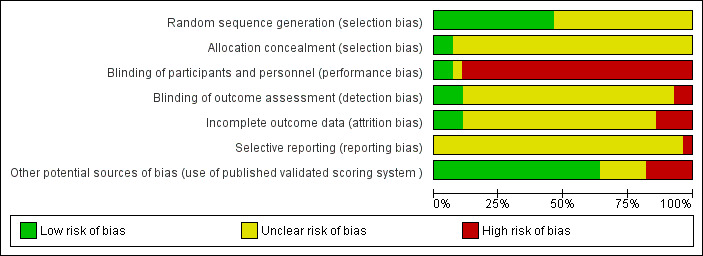
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies
3.
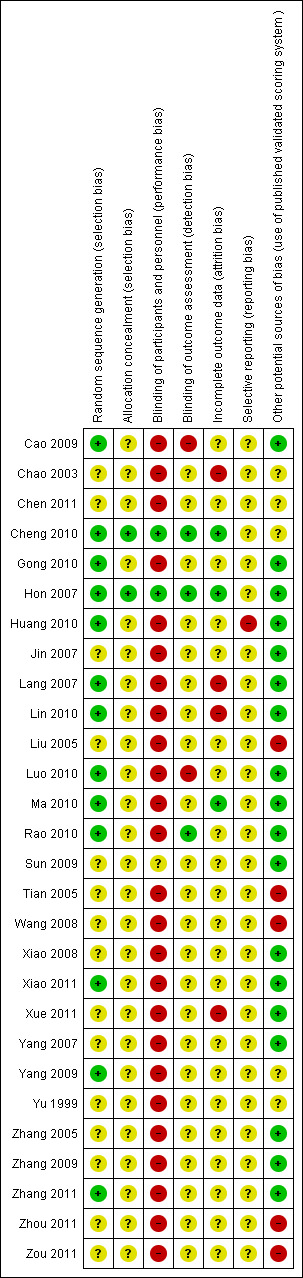
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study
Allocation
Almost half of the included studies (13/28) did not state how they generated allocation sequences (Chao 2003; Chen 2011; Jin 2007; Liu 2005; Sun 2009; Tian 2005; Wang 2008; Xiao 2008; Xue 2011; Yang 2007; Yu 1999; Zhang 2005; Zhang 2009). Of the 28 included studies, only 2 studies explicitly explained the procedures for allocation concealment of randomised codes for avoiding potential selection bias (Cheng 2010; Hon 2007). Both studies used an independent party to provide randomised codes, which were generated by a computer program. The Cheng 2010 study placed the random codes in an envelope. In the Hon 2007 study, the trial investigator did not break the codes of any participant until the trial was completed.
Blinding
Blinding of participants and personnel involved in direct contact with the participants is important for minimising bias from subjective outcome measures (Tal 2011).
One of the most common quoted subjective outcome measures in eczema was VAS for itching severity. About 89% of the included studies (25/28) did not use blinding either on the participants or on the trial investigators, which implied the highest risk of bias within the assessed domains. Although the Sun 2009 study claimed that the trial was a double‐blind design, there was only one author in the published paper with absence of acknowledgment of other personnel. We were not sure how the blinding was implemented in this study. Only two studies employed the double‐blind design and provided clear description of blinding methods (Cheng 2010; Hon 2007).
Blinding of the outcome assessors was another overall weakness of methodology in the included studies. Most of the included studies (82%; 23/28) did not state whether they had used blinding in assessments of outcomes. In many situations, the appearance and administration of the two compared interventions were different in the trial, e.g. Chinese herbal decoction versus Western medications, which made blinding impossible even though the study did not particularly state that it did not use blinding. The Cao 2009 and Luo 2010 studies declared that they did not require blinding. Only three studies appropriately blinded the chief investigators of the trials from awareness of the interventions used, when they performed outcome assessments or used a third party to carry out such assessments (Cheng 2010; Hon 2007; Rao 2010).
Incomplete outcome data
There was unclear risk of bias among the included studies as the numbers of participants randomised and analysed were identical in 75% of the included studies, and it seems that there were no incomplete outcome data in those studies. High risk of attrition bias (a bias associated with withdrawal or dropout of participants in a study) existed as there were withdrawals or dropouts in the studies of Chao 2003; Lang 2007; Lin 2010; and Xue 2011, and these studies did not use ITT. The Cheng 2010; Hon 2007; and Ma 2010 studies reported data for withdrawals and dropouts, and they used the ITT principle in the final statistical calculations. Therefore, we considered the risk of bias at a low level.
Selective reporting
In the Huang 2010 study, the trial investigators claimed full blood counts (they performed liver and renal function tests after the two‐week treatment period), but we could not find the results of those tests in their study. We were unable to assess the outcome reporting bias because of insufficient information in the rest of the 27 included studies.
Other potential sources of bias
We set "use of published validated scoring systems" to assess potential sources of bias and found that more than 64% (18/28) of the included studies used published and validated scoring systems, including EASI, SAASAD, or SCORAD, as outcome measures. Five included studies did not use any published and validated scoring system, and we considered these studies at a high risk of bias (Liu 2005; Tian 2005; Wang 2008; Zhou 2011; Zou 2011). Four studies used a scoring system developed by the trial investigator(s) for measurement of outcomes (Chao 2003; Chen 2011; Yang 2009; Yu 1999). We were not able to assess the validation of those trial investigators' self‐developed scoring systems; thus, we classed the risk of bias as unclear. The Cheng 2010 study claimed to use a "standardised scoring system"; again, we were unable to assess whether the system had been validated, although the scoring system had been previously used and published in other trials, so we classed the risk of bias as unclear in this study, too.
None of the included studies used POEM for scoring the severity of the condition.
Effects of interventions
See: Table 1; Table 2; Table 3
I. CHM versus placebo
1. Primary outcomes
a) Total effectiveness rate
The Chao 2003 study showed that there was a statistically significant increase in total effectiveness rate (those participants with 'recovery' or 'significant improvement') in the CHM group treated with 10% strength CHM cream compared to those in the control group using petroleum jelly (Vaseline) at the end of the 3‐week treatment period. We decided to include the full strength (10%) CHM cream for analysis in this review. The Sun 2009 study recorded no effect in the sum of 'recovery' and 'significant improvement' events in both groups at the end of the four‐week treatment period.
We pooled data from these 2 studies using the statistical method of inverse‐variance with the random‐effects analysis model and expressed an estimate of their overall effects as RR with 95% CI, which showed a statistically significant effect of the CHM intervention (RR 2.09, 95% CI 1.32 to 3.32; see Analysis 1.1).
The Chao 2003 study did not report short‐term or long‐term improvement. The Sun 2009 study reported long‐term improvement (24 weeks after stopping the treatment) assessed with 'Recurrence rate'. We did not perform further analysis of the data as the 'Recurrence rate' was not a prespecified outcome of this review.
The Cheng 2010 and Hon 2007 studies did not report the outcomes as 'effectiveness rate'.
b) Severity of itching score measured by VAS
The Cheng 2010 study reported the improvement of itching in scores (scale from 0 to 4). The score was expressed as least‐squares mean ± the standard error (SE) change from baseline for each intervention group following the eight‐week treatment period. The Cheng 2010 study also provided data of baseline median (interquartile range (IQ)) per group. We did not use the SEs provided as they were too narrow. We pooled the data by using an alternative SD estimated from the baseline data (calculation from baseline IQ range: SD = IQ/1.35) to ensure the least‐squares means did not receive too much weight in the meta‐analysis (Higgins 2011). The Sun 2009 study also used VAS (scale unknown) to assess the severity of itching at the end of the four‐week treatment period but did not report scale. We pooled the data and expressed as SMD with 95% CI due to different outcome scales being used in these 2 studies (SMD ‐1.53, 95% CI ‐2.64 to ‐0.41; see Analysis 1.2). As the Cheng 2010 study reported improvement of VAS without the actual score and the Sun 2009 study recorded decrease of VAS at end point, we multiplied the mean in the Cheng 2010 study by ‐1 to ensure the 2 outcomes were in the same direction (Deeks 2011). Both studies showed favourable results towards the CHM groups.
The Cheng 2010 study reported short‐term improvement (four weeks after stopping the treatment) and stated that better scores of itching were seen in the CHM group, but it did not provide details of data.
We found no record of severity of itching score in the Chao 2003 and Hon 2007 studies.
2. Secondary outcomes
a) Overall severity score measured by the scoring system (e.g. EASI, SAASAD, or SCORAD)
The Chao 2003 study used a self‐developed scoring system and recorded the score at end point in the CHM group (2nd arm) and control group (4th arm). The Cheng 2010 study reported improvement in clinical lesion scores, which were expressed as least‐squares means ± SE at the end of the eight‐week treatment period. We analysed the data by using an alternative SD as outlined above. The Hon 2007 study reported the SCORAD score at the end of the 12‐week treatment period in both groups and stated that there was no significant difference between the 2 groups. The Sun 2009 study also used SCORAD to measure the outcomes and claimed that a significant difference in the treatment and control groups at the end of the treatment period was observed, and the effect in the CHM group was superior to the control group. We pooled data from those 4 studies and recorded a significant difference (SMD ‐0.88, 95% CI ‐1.67 to ‐0.09; see Analysis 1.3).
The Cheng 2010 study reported short‐term improvement (four weeks after stopping the treatment) and stated that improved clinical lesion scores were seen in the CHM group; however, no data were provided. The Hon 2007 study reported that no short‐term improvement was observed as there was no difference between the 2 groups 4 weeks after stopping the treatment (MD 3.40, 95% CI ‐5.70 to 12.50; see Analysis 1.4). The Chao 2003 and Sun 2009 studies did not report short‐term or long‐term improvement in overall severity score.
1.4. Analysis.
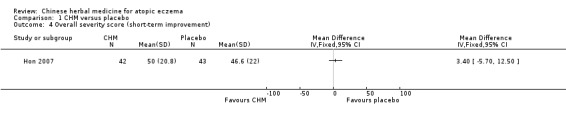
Comparison 1 CHM versus placebo, Outcome 4 Overall severity score (short‐term improvement).
b) QoL index
The Hon 2007 study reported improvement in CDLQI score in the CHM group at the end of the 12‐week treatment period (MD ‐2.50, 95% CI ‐4.77 to ‐0.23; see Analysis 1.5). The Hon 2007 study also stated that there was a short‐term improvement in CDLQI 4 weeks after stopping the treatment, but this claim was not supported by the statistical analysis (MD ‐1.30, 95% CI ‐3.51 to 0.91; see Analysis 1.6).
1.6. Analysis.
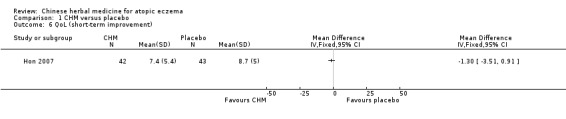
Comparison 1 CHM versus placebo, Outcome 6 QoL (short‐term improvement).
The Chao 2003; Cheng 2010; and Sun 2009 studies did not use a QoL index to measure the outcomes.
c) Adverse events
There were two minor adverse events in the CHM group in the Chao 2003 study. The Cheng 2010 study reported that one participant had transient elevation of aspartate aminotransferase (AST); the trial investigators did not state in which group the participant was assessed. There were two participants in the treatment group who complained of gastrointestinal upset in the first week of the treatment, but the participants were able to complete the whole trial (Cheng 2010). The Sun 2009 study stated that none of the trial participants reported adverse events.
We pooled data from the Chao 2003 and Cheng 2010 studies about minor adverse events; no significant difference was seen between the treatment and control groups (RR 0.71, 95% CI 0.06 to 8.67; 2 studies, n = 129; see Analysis 1.7). There were a total of 82 minor adverse events reported by participants in the CHM group and 47 minor adverse events reported by participants in the control group in the Hon 2007 study. The trial investigators claimed that there was no significant difference in terms of frequency of minor adverse events in the two groups. We treated the frequency of those adverse events as 'count data' and converted to risk ratio (Deeks 2011). It showed a statistically significant difference in the minor adverse events between the 2 groups, and the CHM group had a higher rate in the incident of the events (RR 1.77, 95% CI 1.24 to 2.53; see Analysis 1.8).
1.8. Analysis.
Comparison 1 CHM versus placebo, Outcome 8 Adverse events in one study.
Subgroup analysis and investigation of heterogeneity
We found substantial heterogeneity (I² statistic = 87%, see Figure 4) across the 4 studies in the outcome 'overall severity score'. We planned to perform subgroup analyses of "children (16 years old or under) with eczema versus adults with eczema" and "application of interventions based on Chinese medicine syndrome differentiation versus non‐individualisation formula" where there were at least moderate levels of heterogeneity across the included studies. However, only the Chao 2003 study recruited children aged from 1 to 38 months; the other 3 studies mixed children with adults, and these 3 studies used non‐individualised formulae. Thus, we did not conduct subgroup analyses.
4.
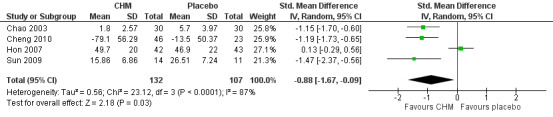
Forest plot of comparison: 1 CHM versus placebo, outcome: 1.3 Overall severity score
We could not explain such differences by further analysis of the sources of heterogeneity, which included the following:
participant factors, e.g. age (children versus adults, because we were not able to identify the difference for the reasons stated above), diagnosis (infantile eczema in the Chao 2003 study versus atopic eczema in the Cheng 2010; Hon 2007; and Sun 2009 studies), sex (mixed gender in all four studies), race (all Asians), and comorbidity (not able to identify because of insufficient data);
treatment factors, e.g. dosage (various CHM dosages applied across the four studies) and formulation (four different CHM formulae used in four studies); and
study factors, e.g. concordance rates (all four studies reported high compliance rates), quality of reporting (this was overcome by assessment of risk of bias in this review), and quality control for the Chinese herbal preparations, e.g. source, purity, and preparation facilities (all four studies reported quality control for the CHM interventions).
Sensitivity analysis
We planned to perform sensitivity analyses of the primary outcomes by excluding studies of low methodological quality. We found substantial heterogeneity (I² statistic = 74%; see Analysis 1.2) in the 2 studies that measured 1 of the primary outcomes, the severity of itching, by VAS. We could not perform sensitivity analysis as there were only two studies in the meta‐analysis.
II. CHM versus no treatment
None of the included studies compared CHM with no treatment.
III. CHM versus acupuncture
None of the included studies compared CHM with acupuncture treatment.
IV. CHM versus conventional medicines (drugs)
1. Primary outcomes
a) Total effectiveness rate
A total of 20 included studies employed total effectiveness rate as the outcome measure. In addition, we included one arm of the Chao 2003 study, which was a four‐arm design where CHM was used topically (second arm) compared to steroid cream (third arm) in the current category. We pooled data from the 21 included studies using the statistical method of inverse‐variance with the random‐effects analysis model and expressed an estimate of their overall effects as RR with 95% CI. The forest plot of comparison showed that application of CHM significantly improved the condition compared to control interventions (RR 1.43, 95% CI 1.27 to 1.61; see Analysis 2.1).
The Cao 2009; Chao 2003; Chen 2011; Lang 2007; Ma 2010; Tian 2005; Wang 2008; Xue 2011; Yang 2007; Yang 2009; and Zhang 2005 studies did not report short‐term or long‐term improvement. The Zhang 2009 study reported short‐term improvement assessed with 'Recurrence rate'. The Huang 2010; Liu 2005; Xiao 2011; Zhang 2011; Zhou 2011; and Zou 2011 studies also used 'Recurrence rate' to report long‐term improvement. All of them stated that the CHM groups had a lower recurrence rate than their comparators. The Luo 2010 study reported long‐term improvement, but provided no data. The Gong 2010 and Yu 1999 studies reported long‐term improvement and stated that CHM groups had a higher effectiveness rate than the control groups (RR 1.52, 95% CI 1.11 to 2.08; see Analysis 2.2).
2.2. Analysis.
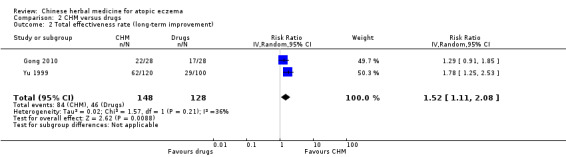
Comparison 2 CHM versus drugs, Outcome 2 Total effectiveness rate (long‐term improvement).
b) Severity of itching score measured by VAS
Seven included studies reported continuous VAS data to measure the severity of itching score. The scale was 0 to 10 in all studies except the Chen 2011 study where the scale of VAS was 0 to 3. We expressed the data as SMD with 95% CI as the included studies used different outcome scales. The forest plot figure showed that there was a statistically significant difference between the CHM group and control group in terms of reduction of the severity of itching, and overall effects were favourable to the CHM groups (SMD ‐0.83, 95% CI ‐1.43 to ‐0.22; see Analysis 2.3).
None of the seven included studies reported short‐term or long‐term improvement in terms of itching score (Chen 2011; Jin 2007; Lang 2007; Ma 2010; Xue 2011; Yang 2007; Zhang 2005).
2. Secondary outcomes
a) Overall severity score measured by the scoring system (e.g. EASI, SAASAD, or SCORAD)
The Liu 2005; Tian 2005; Wang 2008; Zhou 2011; and Zou 2011 studies did not report measurement of overall severity of the condition. The Yang 2009; Yu 1999; and Zhang 2009 studies did not provide data for the scores. We pooled data collected from the remaining 15 included studies and expressed them as SMD with 95% CI as the studies used different outcome scales. The Cao 2009; Luo 2010; and Zhang 2005 studies reported data measured at the end point as percentage of reduction of total SASSAD score and expressed the data as 'numbers ±'. We assumed unlabelled data in these three studies were 'mean and SD'. We multiplied the mean by ‐1 to ensure all scales were in the same direction in the meta‐analysis. The forest plot figure showed that application of CHM significantly reduced the severity of skin lesions measured by various scoring systems when compared to Western medications (SMD ‐0.97, 95% CI ‐1.23 to ‐0.71; see Analysis 2.4).
Cao 2009; Chao 2003; Chen 2011; Jin 2007; Lang 2007; Ma 2010; Xue 2011; Yang 2007; and Zhang 2005 reported no short‐term or long‐term improvement. The Gong 2010; Huang 2010; Luo 2010; Xiao 2008; Xiao 2011; and Zhang 2011 studies reported long‐term improvement. Only the Xiao 2008 study provided data to support a long‐term improvement observed in the CHM group (MD ‐8.50, 95% CI ‐13.40 to ‐3.60; see Analysis 2.5).
2.5. Analysis.
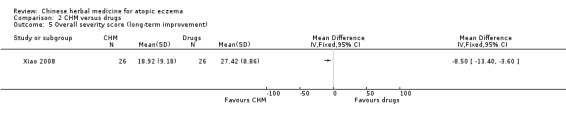
Comparison 2 CHM versus drugs, Outcome 5 Overall severity score (long‐term improvement).
b) QoL index
No studies in this group employed QoL questionnaires as outcome measures.
c) Adverse events
The Jin 2007; Xue 2011; Zhang 2009; and Zhang 2011 studies did not report adverse events. The Cao 2009; Luo 2010; Zhou 2011; and Zou 2011 studies stated that no adverse events were reported during the trial period. None of the studies reported withdrawals of participants due to any adverse event. When combined, the 15 studies indicated there were significantly less minor adverse events in the CHM than the control groups (RR 0.44, 95% CI 0.32 to 0.61; see Analysis 2.6).
Subgroup analysis and investigation of heterogeneity
There was substantial heterogeneity (I² statistic = 65%; see Analysis 2.1 and Figure 5) across the 21 included studies with the outcome measured by total effectiveness rate. We planned to conduct a subgroup analysis of the studies of "children (16 years old or under) with eczema versus adults with eczema" and identified 12 studies in which the participants were 16 years old or under. The other nine studies however recruited participants with a mix of children and adults; therefore, we were unable to conduct subgroup analysis under this heading.
5.
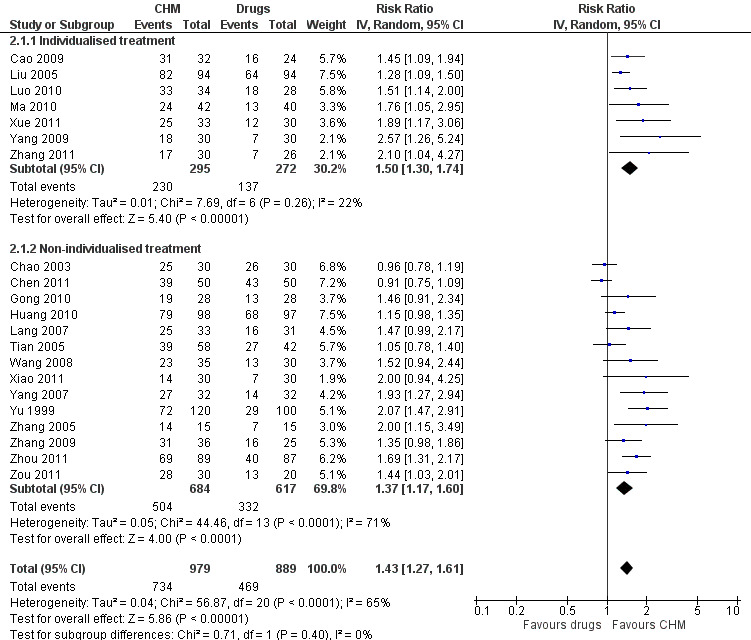
Forest plot of comparison: 2 CHM versus drugs, outcome: 2.1 Total effectiveness rate (number of participants recovered and significantly improved) with subgroup analysis
We also compared the difference in the total effectiveness rate between two groups where application of CHM was based on Chinese medicine syndrome differentiation or non‐individualised formula. There was low inconsistency (I² statistic = 22%) within the 7 subgrouped studies, which applied CHM based on Chinese medicine syndrome differentiation (individualised modifications) and showed that CHM was more effective than the Western medications (RR 1.50, 95% CI 1.30 to 1.74; see analysis 2.1.1 in Analysis 2.1). There were no subgroup differences (I² statistic = 0) when comparing the individualised treatment subgroup to the non‐individualised subgroup. Where non‐individualised formulae were used, there was a high level of heterogeneity between the studies in this subgroup (I² statistic = 71%; see analysis 2.1.2 in Figure 5).
We performed a posthoc subgroup analysis of 'CHM versus topical steroid', 'CHM versus antihistamines', and 'CHM versus other agents' as the different types of comparators could be a possible reason for heterogeneity in the studies. We found substantial heterogeneity in the subgroup of topical steroid (I² statistic = 72%). Although there were no inconsistencies in the subgroups of antihistamines or other agents, the total subgroup differences were statistically significant (P = 0.02; I² statistic = 74.4%; see Analysis 2.7).
2.7. Analysis.
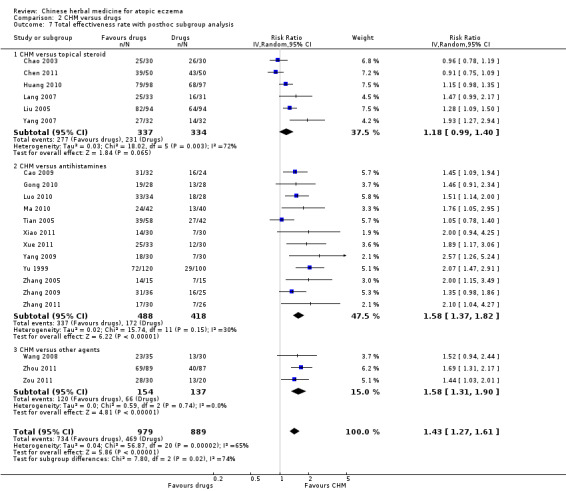
Comparison 2 CHM versus drugs, Outcome 7 Total effectiveness rate with posthoc subgroup analysis.
We were unable to further investigate the sources of the heterogeneity in this group from participant factors (e.g. age, diagnosis, sex, race, comorbidity), treatment factors (e.g. dosage, formulation), study factors (e.g. concordance rates, quality of reporting), and quality control for the Chinese herbal preparations as no data were available for appropriate comparisons.
Sensitivity analysis
We could not perform sensitivity analyses of the primary outcomes by further excluding studies of low methodological quality as all studies in this category had similar methodological weaknesses (e.g. high risk of bias in blinding of participants and research personnel).
Assessment of reporting bias
We generated a funnel plot (Figure 6) to inspect visually for evidence of potential reporting bias including publication bias across 15 included studies, which compared effects of CHM and Western medications (Cao 2009; Chao 2003; Chen 2011; Gong 2010; Huang 2010; Jin 2007; Lang 2007; Luo 2010; Ma 2010; Xiao 2008; Xiao 2011; Xue 2011; Yang 2007; Zhang 2005; Zhang 2011). We further assessed for any bias captured in the funnel plot with the test proposed by Egger 1997. The results of the assessment indicated that there were no statistically asymmetrical distributions among those 15 studies (Egger test P = 0.2021).
6.
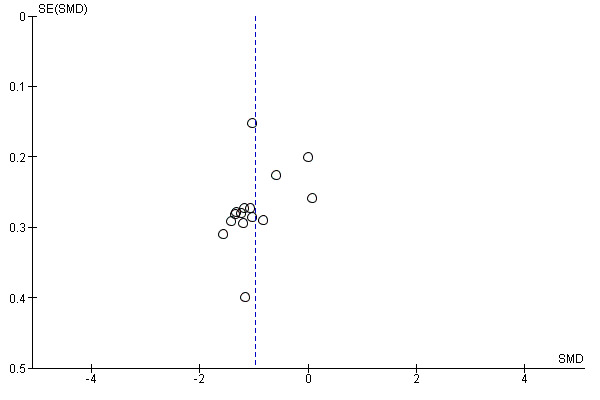
Funnel plot of comparison: 2 CHM vs drugs, outcome: 2.4 Overall severity score
V. Combination of oral and topical CHM interventions versus same oral CHM alone
1. Primary outcomes
a) Total effectiveness rate
The Lin 2010 study did not express the outcomes as 'effectiveness rate'. The Rao 2010 study reported no difference in the effects between the first arm (CHM used orally and topically) and second arm (CHM was used by oral ingestion only, but there was no topical intervention) at the end of the 12‐week treatment period (RR 1.13, 95% CI 0.78 to 1.63; see Analysis 3.1).
The Lin 2010 study did not report short‐term or long‐term improvement. The Rao 2010 study reported long‐term improvement (24 weeks after stopping the treatment), but no difference was observed between the 2 groups (RR 1.00, 95% CI 0.75 to 1.34; see Analysis 3.2).
3.2. Analysis.
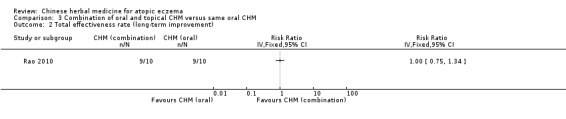
Comparison 3 Combination of oral and topical CHM versus same oral CHM, Outcome 2 Total effectiveness rate (long‐term improvement).
b) Severity of itching score measured by VAS
The Lin 2010 study reported that there was statistically significant improvement in terms of itching relief (scale from 0 to 10) in the treatment site compared to the control site of the limb at the end of 2 weeks of treatment (MD ‐1.05, 95% CI ‐1.75 to ‐0.35; see Analysis 3.3). The Lin 2010 study did not report short‐term or long‐term improvement. The Rao 2010 study did not report severity of itching score.
2. Secondary outcomes
a) Overall severity score measured by the scoring system (e.g. EASI, SAASAD, or SCORAD)
The Lin 2010 study used a self‐developed scale (scale 0 to 24) for scoring the severity of skin lesions and reported a statistically significant improvement in terms of skin lesions at the treatment site of the limb compared to the control site, at the end of the 2‐week treatment period (MD ‐1.59, 95% CI ‐2.92 to ‐0.26; see Analysis 3.4). We did not pool the score of SCORAD in the Lin 2010 study as the data provided were recorded at the baseline and the end of the treatment period rather than the treatment site and control site. The Rao 2010 study stated no difference in the reduction of SCORAD between the treatment group and control group at the end of the 12‐week treatment period (MD ‐3.43, 95% CI ‐7.01 to 0.15; see Analysis 3.5). We did not pool the data from the two studies for meta‐analysis as the Lin 2010 study was a within‐patient trial.
The two studies did not report short‐term or long‐term improvement.
b) QoL index
The Lin 2010 study did not use a QoL index for measurement of outcomes. The Rao 2010 study used CDLQI as the secondary outcome measure and recorded the scores at the end of the 12‐week treatment period, which indicated no difference between the 2 groups (MD 0.90, 95% CI ‐2.89 to 4.69; see Analysis 3.6).
The Rao 2010 study also used CDLQI scores for measuring long‐term improvement in 24 weeks after stopping the treatment, but provided no data.
c) Adverse events
There was one participant withdrawal (a severe adverse event) from the Lin 2010 study due to exacerbation of the skin condition after using the Chinese herbs for two days, and three participants complained of mild to moderate burning and pain sensations, but they still completed the two‐week treatment. The Rao 2010 study stated that there was 1 participant with increased serum alanine transaminase (ALT) each in the treatment and control group (RR 1.00, 95% CI 0.07 to 13.87; see Analysis 3.7).
We did not perform subgroup or sensitivity analyses for this comparison.
Number needed to treat (NNT) or number needed to benefit (NNTB)
Because of high risk of bias in most of the included studies, we decided not to express dichotomous data as NNT or continuous data as NNTB as these additional variations may have induced unnecessary misleading implications.
Discussion
Summary of main results
This review is an updated version with a new team of authors and a newly published protocol. We did not include the four studies that were included in the previous version of this review as they all investigated a Chinese herbal medicine (CHM) product, Zemaphyte, which the manufacturer withdrew from the market in 2004 (Zhang 2004). And we think it would skew the significance of systematically produced evidence‐based medicine if we incorporated data that is not linked to current clinical practice or research.
This review included 28 studies, with a total of 2306 participants. Chinese herbal medicines and comparators were taken orally or applied topically by children and adults with eczema. Four studies compared CHM to placebo. Two studies compared a combination of oral and topical CHM to the same oral CHM formula alone, and 22 studies and 1 arm of the Chao 2003 study compared CHM to Western medications.
We found evidence from one 12‐week study of moderate to severe eczema, comparing an oral CHM to placebo, of a statistically significant difference between the 2 groups with respect to QoL score (MD ‐2.50, 95% CI ‐4.77 to ‐0.23; see Analysis 1.5) (Hon 2007). The mean QoL score in the CHM groups was 2.5 lower than that in the placebo groups, which indicated that oral ingestion of CHM could improve QoL. Although the overall effect in the outcomes of 'total effectiveness rate', 'severity of itching score', and 'overall severity score' showed a statistically significant difference between the groups in favour of CHM, these findings were inconclusive because of the high risk of bias with regard to blinding of participants and research personnel, incomplete outcomes, or other unclear risk of bias that existed across these four studies (see Table 1). Unexplained high heterogeneity (I² statistic = 87%; see Figure 4) among the 4 studies in the outcome measured by 'overall severity score' further weakened the strength of the positive estimates.
The majority of the included studies (22 studies and 1 arm of the Chao 2003 study) used conventional medicines (Western medications) as comparators, which included oral ingestion of antihistamine tablets; topical use of corticosteroid cream; and other agents, such as antifungals, antiseptics, or emollients. Twenty‐one studies expressed their primary outcome as 'total effectiveness rate', and all reported that effectiveness of CHM interventions was superior to the comparators except the Chao 2003 and Chen 2011 studies, which used corticosteroid cream as the control intervention. In addition to these two studies, our meta‐analyses showed no statistically significant difference between the CHM and conventional medicine groups observed in the studies of Gong 2010; Huang 2010; Lang 2007; Tian 2005; Wang 2008; Xiao 2011; and Zhang 2009, although the overall effects of the 21 included studies favoured the CHM groups (RR 1.43, 95% CI 1.27 to 1.61; see Analysis 2.1).
The claim of positive effects with CHM intervention needs to be interpreted with caution because of substantial heterogeneity (I² statistic = 65%; see Figure 5) across the studies. The result from a posthoc subgroup analysis (subgroup differences I² statistic = 74.4%) also confirmed there was unexplained heterogeneity. We also found there was high risk of bias in the domains for blinding of participants and research personnel and blinding of outcome assessment, as well as other potential sources of bias (absence of usage of published and validated scoring systems for outcome measures) in this group of studies (see Table 2). All included studies in this group were associated with several major methodological weaknesses. For example, although all studies used randomisation for grouping of participants, none of them provided information of the procedure for allocation concealment (see Figure 3). Inadequate randomisation could give rise to an investigator's bias for grouping of participants, which consequently affects the outcomes (Liu 2006).
Two studies reported a statistically significant difference in outcomes of 'total effectiveness rate' or 'severity of itching score measured by VAS', respectively, and overall effects in the combination of oral and topical CHM groups were always superior to the oral CHM control groups (Lin 2010; Rao 2010). We did not pool data from the two studies as the Lin 2010 study was a within‐patient study. The Lin 2010 study had a high risk of performance bias and attrition bias. The Rao 2010 study had a high risk of bias in the domain of blinding of the participants and research personnel, and both studies had small sample sizes (a total of 42 participants in 2 studies evaluated). Their claims that overall effects in CHM groups were superior to the control groups were in doubt (see Table 3).
It is worth pointing out that nearly half of the included studies did not use published and validated scoring systems for measuring the severity of the condition. Some studies used the scoring system but did not provide continuous data for the scores. The absence of these data made quantifiable data analysis impossible and downgraded the credibility of the results (Eichenfield 2003). We were unable to further estimate if CHM has potential for short‐term or long‐term improvement of eczema because of limited data provided by the included studies.
Chinese herbal medicines' possible association with hepatotoxicity (liver toxicity) was discussed when 11 cases of liver damage following oral ingestion of some raw Chinese herbal mixtures for skin conditions were reported in the UK between 1991 to 1993 (Perharic 1995). The reporters indicated that the mechanism of toxicity was not clear. The adverse effects of those CHM mixtures seemed to not be dose‐related and were probably idiosyncratic. The safety issue of oral ingestion of CHM has been a concern of healthcare professionals and the public (Chitturi 2000). In this review, we evaluated both beneficial effects and adverse effects of interventions from the included studies. We found only a quarter (7/28) of the included studies had monitored the liver and renal function of the participants during the period of the trial (Cheng 2010; Hon 2007; Luo 2010; Rao 2010; Xiao 2008; Xiao 2011; Zou 2011).
With regard to adverse events including liver or kidney dysfunction, there was one withdrawal due to aggravation of the condition (a severe adverse event) after using CHM (Lin 2010), no severe adverse events were reported in 23 studies, and the remaining 4 studies did not report adverse events (Jin 2007; Xue 2011; Zhang 2009; Zhang 2011). Twenty‐four studies reported minor adverse events; 2 studies observed transient elevation of aspartate aminotransferase or alanine transaminase in the trial participants (Cheng 2010; Rao 2010). Apart from the Hon 2007 study, which recorded a statistically significant difference in minor adverse events with a higher incidence in the CHM group, pooled data from other included studies demonstrated significantly less minor adverse events with CHM interventions than their comparators. Nevertheless, the quality of evidence was low.
There were eight included studies (Cheng 2010; Gong 2010; Hon 2007; Ma 2010; Sun 2009; Xue 2011; Yang 2007; Yu 1999) that were funded by governments. In addition, 75% of the included studies, all conducted in mainland China, reported identical numbers of participants randomised and analysed. These studies reported no incomplete outcome data. We were not able to find out the underlying reasons for such unusually high compliance in RCTs.
Overall completeness and applicability of evidence
We included studies with CHM interventions administered orally or applied topically, or a combination of both, for children or adults diagnosed with eczema. All 28 included studies specifically focused on management of eczema with CHM. Based on a Chinese medicine description, the selected Chinese herbs in the included studies were under categories of "exterior‐releasing", "heat‐clearing", "purgative", "wind‐damp‐dispelling", "damp‐resolving", "damp‐draining", "interior‐warming", "Qi‐regulating", "digestant", "haemostatic", "blood‐activating and stasis‐resolving", "liver‐pacifying wind‐extinguishing", "resuscitative", "tonifying", "astringent", and "externally applied and miscellaneous" (Li 2008). The top seven most commonly used herbs were Gancao (Radix glycyrrhizae) (16 studies), Cangzhu (Rhizoma atractylodis) (13 studies), Danggui (Radix angelicae sinensis) (11 studies), Baizhu (Rhizoma atractylodis macrocephalae) (9 studies), Baixianpi (Cortex dictamni) (9 studies), Fuling (Poria) (9 studies), and Shengdihuang (Radix rehmanniae) (9 studies). We also included studies in which the CHM formulae were modified based on Chinese medicine syndrome differentiation, as well as the studies that only recruited people with eczema who had a prespecified Chinese medicine syndrome. Many of the included studies were conducted in Chinese medicine teaching hospitals or general medical teaching hospitals, which are expected to have standardised facilities and qualified personnel and represent the standard of clinical practice of the profession (MEPRC 1992). The results have reflected the up‐to‐date management of eczema with CHM. The findings of this review could provide a crucial reference for current evidence‐based Chinese medical practice and research.
Quality of the evidence
We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system, recommended by the Cochrane Handbook for Systematic Reviews of Interventions, to assess the level of evidence on outcome measures reported by the included studies (Schünemann 2011). Overall, the quality of the included studies was poor except the Hon 2007 study where the level of quality of the evidence was 'moderate' in the outcome measured by QoL. The majority of the included studies showed unclear risk of bias for allocation concealment and high risk of bias due to lack of blinding; thus, we had to downgrade the strength of evidence of those studies into 'low level' because of serious limitations in their design and implementation (absence of allocation concealment and blinding). The 2306 participants within the 28 included studies were diverse, with their ages ranging from newborn babies to 65 years, and most of the studies had mixed children with adults. There were heterogeneous Chinese herbs or formulae with regard to the ingredients, dosage, and administration in the included studies. This contributed to a high level of inconsistency of the outcomes across the studies although such underlying sources of heterogeneity have not been confirmed by statistical analyses because of insufficiency of data.
Potential biases in the review process
The randomised controlled trial is a gold standard to test efficacy of an intervention for a defined condition within a population (Kane 2004). It is debatable however whether results from RCTs can really reflect the intrinsic effect obtained from an individualised treatment, which is one of the essential features of Chinese medicine practice. For this reason, we scrupulously aimed to include studies using individualised treatments or studies only recruiting people with eczema who had a specific type of Chinese medicine syndrome as far as there was an appropriate control group, i.e. with balanced numbers of randomised participants, in the study. We further performed subgroup analysis in those included studies with individualised treatment. We tried our best to search for any studies that matched the inclusion criteria, but it could still be possible that we overlooked some papers, in particular those published in Chinese. This is because we had limited access to the printed Chinese medical journals that were not covered by the Chinese databases we had searched. We were unable to rule out the possibility of potential language bias in this review as Chinese medicine is also popularly used in other Asian countries, such as Japan, Vietnam, and Korea. We were not able to search databases developed by these countries.
The funnel plot in Figure 6 and Egger test did not show statistically asymmetrical distributions among those 15 studies that compared the effects of CHM and Western medications. However, we could not exclude reporting bias including publication bias in those 15 studies because of the relatively low power of the Egger test (Sterne 2011).
Agreements and disagreements with other studies or reviews
The first Cochrane systematic review of CHM for eczema was published in 2004 (Zhang 2004); it included only 4 studies with oral ingestion of a CHM product, which is no longer available on the market. We did not include these studies in this updated review. Poor trial quality and "small study effect" were found across the included studies in both the version published in 2004 and this review.
Authors' conclusions
Implications for practice.
We could not find conclusive evidence that oral ingestion of other Chinese herbs or Chinese herbal formulae used in the included studies could improve the condition. Furthermore, we could not find convincing evidence that topical application of CHM, whether used alone or in conjunction with oral ingestion of Chinese herbal formulae, could reduce the severity of eczema in children or adults. Even though in the included studies there were statistically significant differences in the outcome measures where CHM treatment groups were compared to those in the control groups, because of a low strength of evidence and high risk of bias, these claims cannot be regarded as reliable.
Implications for research.
There is evidence that CHM has been increasingly used for the management of eczema since the publication of the first Cochrane systematic review in this area, and many included studies were government‐funded research projects (almost one third of the included studies received funding). The following are our suggestions for conducting a randomised controlled trial of CHM for eczema in the future.
Recruitment of participants with similar ages or severity of their condition is needed to minimise heterogeneous outcomes within the study. Stratified randomisation is recommended if the study recruits both children and adults.
Sample size in the intervention group and control group should be balanced. Characteristics of participants in the two groups should be comparable. Methods for randomisation must be clearly described on the published paper.
Blinding should always be used, because in most cases, outcome measures for eczema are subjective. An open‐label design study could lead to risk of bias for outcome assessment.
Application of the intervention should be used alone, i.e. oral ingestion or topical application with appropriate comparator unless efficacy of the oral ingestion or topical application of the intervention has been confirmed respectively. Quality control, including appropriate toxicology studies and quality assurance of Chinese herbs to be investigated, should be performed prior to the conduct of clinical trials as contamination of any non‐CHM components detracts from the high standards and tradition of Chinese medicine.
Assessment of effectiveness of the intervention should rely on data from both objective and subjective outcome measures assessed at baseline and at the end point of the trial. Using published and validated scoring systems, such as EASI, SASSAD, or SCORAD as a primary outcome measure may help to achieve this, and continuous data should always be reported or provided upon request.
Adverse events should be adequately reported. Liver and renal function tests should be used as one of the safety parameters in a randomised controlled trial.
In summary, well‐designed, adequately powered, randomised placebo‐controlled clinical trials are required to evaluate the efficacy and safety of CHM for managing eczema.
What's new
| Date | Event | Description |
|---|---|---|
| 18 November 2015 | Review declared as stable | A search of MEDLINE and PubMed in November 2015 found only 1 RCT study, and a search by the lead author of CNKI yielded 3 potential studies, but he does not think the inclusion of these new findings could substantially change the conclusions made in 2013. An update has not been considered necessary for two successive years. Our Trials Search Co‐ordinator will run a new search in 2016 to re‐assess whether an update is needed. |
History
Protocol first published: Issue 8, 2010 Review first published: Issue 9, 2013
| Date | Event | Description |
|---|---|---|
| 15 October 2014 | Amended | A search of MEDLINE and PubMed in October 2014 found only 3 studies, which our Co‐ordinating Editor deemed small and not consequential. Thus, an update has not been considered necessary at this time. Our Trials Search Co‐ordinator will run a new search in 2015 to re‐assess whether an update is needed. |
| 24 June 2013 | New citation required and conclusions have changed | We did not include the four studies that were in the previous version of this review. We included 28 newly identified studies and rewrote the full review. |
Notes
A search of MEDLINE and PubMed in November 2015 found only 1 RCT study, and a search by the lead author of CNKI yielded 3 potential studies, but he does not think the inclusion of these new findings could substantially change the conclusions made in 2013. An update has not been considered necessary for two successive years. Our Trials Search Co‐ordinator will run a new search in 2016 to re‐assess whether an update is needed.
Acknowledgements
We would like to express our sincere thanks for those who provided help:
Dr Finola M Delamere, Managing Editor, Cochrane Skin Group, for co‐ordination of the project;
Ms Liz Doney, Trials Search Co‐ordinator, Cochrane Skin Group, for searching the databases and inputting the search results;
Miss Laura Prescott, Editorial Assistant, Cochrane Skin Group, for providing assistance;
Ms Miranda Cumpston, Systematic Review Trainer, Australasian Cochrane Centre, for providing author training and advice;
Dr Tony Zhang, Head, Discipline of Chinese Medicine, School of Health Sciences, Royal Melbourne Institute of Technology (RMIT) University, Australia, for providing advice on interpretation of statistical data;
Professor Chuanjian Lu, Deputy Director, Guangdong Provincial Academy of Chinese Medical Sciences, China, for providing expert advice;
Dr Chijing Liu, Director, Chi Herbal Australia P/L, for providing conference proceedings; and
Mr Kun Zou, PhD student, Division of Academic Rheumatology, School of Clinical Sciences, University of Nottingham, UK, for testing publication bias.
Our sincere thanks are also extended to those authors who made their contribution to the previous version of the review. They were Tina Leonard, Fiona Bath‐Hextall, Colette Chambers, Caroline Lee, and Rosemary Humphreys.
The Cochrane Skin Group editorial base wishes to thank Robert Dellavalle who was the Key Editor for this review; Jo Leonardi‐Bee and Ching‐Chi Chi who were the Statistical and Methods Editors, respectively; the clinical referees, Jerry Tan and Kam‐Lun Ellis Hon; and the consumer referee, the late Shirley Manknell.
Appendices
Appendix 1. CENTRAL (Cochrane Library) search strategy
#1 MeSH descriptor Eczema explode all trees #2 MeSH descriptor Dermatitis, Atopic explode all trees #3 MeSH descriptor Dermatitis explode all trees #4 eczema or dermatitis or "besnier* prurigo" #5 (#1 OR #2 OR #3 OR #4) #6 MeSH descriptor Medicine, Chinese Traditional explode all trees #7 MeSH descriptor Drugs, Chinese Herbal explode all trees #8 MeSH descriptor Plants, Medicinal explode all trees #9 MeSH descriptor Medicine, Traditional explode all trees #10 MeSH descriptor Plant Extracts explode all trees #11 MeSH descriptor Phytotherapy explode all trees #12 (phytopharmaceutic*) #13 (herb*) #14 (traditional or herbal) and (therap* or medicine*) #15 "aconite root" or camelia or cayenne or "chinese cucumber" or "chrysanthemum flower*" or "cocklebur fruit" or "cow dipper" or "croton seed" or ginger or ginkgo or ginseng or "goji berry" or "horny goat weed" or rhubarb or "thunder vine" or "strychnine tree" or "sweet wormwood" or "willow bark" #16 (#6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15) #17 (#5 AND #16)
Appendix 2. MEDLINE (OVID) search strategy
1. exp Eczema/ or eczema.mp. 2. atopic dermatitis.mp. or exp Dermatitis, Atopic/ 3. exp Dermatitis/ or dermatitis.mp. 4. Besnier$ prurigo.mp. 5. or/1‐4 6. exp drugs, chinese herbal/ or exp medicine, chinese traditional/ 7. exp Plants, Medicinal/ 8. exp Medicine, Traditional/ 9. exp Plant Extracts/ 10. exp Phytotherapy/ 11. phytopharmaceutic$.mp. 12. herb$.mp. 13. traditional medicine$.mp. 14. traditional therap$.mp. 15. herbal medicine$.mp. 16. herbal therap$.mp. 17. aconite root.mp. 18. camelia.mp. 19. cayenne.mp. 20. chinese cucumber.mp. 21. chrysanthemum flower$.mp. 22. cocklebur fruit.mp. 23. cow dipper.mp. 24. croton seed.mp. or exp Croton/ 25. ginger.mp. or exp Ginger/ 26. ginkgo.mp. or exp Ginkgo biloba/ 27. ginseng.mp. or exp Panax/ 28. goji berry.mp. 29. horny goat weed.mp. 30. rhubarb.mp. or exp Rheum/ 31. thunder vine.mp. 32. strychnine tree.mp. 33. sweet wormwood.mp. 34. willow bark.mp. 35. randomized controlled trial.pt. 36. controlled clinical trial.pt. 37. randomized.ab. 38. placebo.ab. 39. clinical trials as topic.sh. 40. randomly.ab. 41. trial.ti. 42. 35 or 36 or 37 or 38 or 39 or 40 or 41 43. (animals not (human and animals)).sh. 44. 42 not 43 45. 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 46. 5 and 44 and 45
Appendix 3. EMBASE (OVID) search strategy
1. eczema.ti,ab. or *eczema/ 2. exp *DERMATITIS/ or dermatitis.ti,ab. 3. atopic dermatitis.ti,ab. or *atopic dermatitis/ 4. Besnier$ prurigo.ti,ab. 5. or/1‐4 6. exp oriental medicine/ or exp medicinal plant/ or exp Chinese medicine/ or exp traditional medicine/ or exp Chinese drug/ 7. exp herb/ or exp Chinese herb/ 8. exp herbal medicine/ 9. (herb or herbs).mp. or herbal.ti,ab. 10. exp plant medicinal product/ or exp plant extract/ 11. exp phytotherapy/ 12. phytopharmaceutic$.ti,ab. 13. traditional medicine$.ti,ab. 14. traditional therap$.ti,ab. 15. herbal medicine$.ti,ab. 16. herbal therap$.ti,ab. 17. aconite root.ti,ab. 18. camelia.ti,ab. 19. cayenne.ti,ab. 20. chinese cucumber.ti,ab. 21. chrysanthemum flower$.ti,ab. 22. cocklebur fruit.ti,ab. 23. cow dipper.ti,ab. 24. croton seed.ti,ab. 25. ginger.ti,ab. 26. ginkgo.ti,ab. 27. ginseng.ti,ab. 28. goji berry.ti,ab. 29. horny goat weed.ti,ab. 30. rhubarb.ti,ab. 31. thunder vine.ti,ab. 32. strychnine tree.ti,ab. 33. sweet wormwood.ti,ab. 34. willow bark.ti,ab. 35. random$.mp. 36. factorial$.mp. 37. (crossover$ or cross‐over$).mp. 38. placebo$.mp. or PLACEBO/ 39. (doubl$ adj blind$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword] 40. (singl$ adj blind$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword] 41. (assign$ or allocat$).mp. 42. volunteer$.mp. or VOLUNTEER/ 43. Crossover Procedure/ 44. Double Blind Procedure/ 45. Randomized Controlled Trial/ 46. Single Blind Procedure/ 47. 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 48. or/6‐34 49. 5 and 47 and 48
Appendix 4. AMED (OVID) search strategy
1. exp Eczema/ or eczema.mp. 2. dermatitis.mp. 3. Dermatitis/ or exp Dermatitis atopic/ 4. besnier$ prurigo.mp. 5. or/1‐4 6. exp Drugs chinese herbal/ or exp Traditional medicine chinese/ 7. exp Plant extracts/ or exp Herbs/ or exp Herbal drugs/ or exp Plants medicinal/ 8. exp Traditional medicine/ 9. exp Herbalism/ 10. exp Phytotherapy/ 11. phytopharmaceutic$.mp. 12. traditional medicine$.mp. 13. traditional therap$.mp. 14. herbal medicine$.mp. 15. herbal therap$.mp. 16. aconite root.mp. 17. camelia.mp. 18. cayenne.mp. 19. chinese cucumber.mp. 20. chrysanthemum flower$.mp. 21. cocklebur fruit.mp. 22. cow dipper.mp. 23. croton seed.mp. 24. ginger.mp. 25. ginkgo.mp. or exp Ginkgo biloba/ 26. ginseng.mp. or exp Panax ginseng/ 27. goji berry.mp. 28. horny goat weed.mp. 29. rhubarb.mp. 30. thunder vine.mp. 31. strychnine tree.mp. 32. sweet wormwood.mp. 33. willow bark.mp. 34. (plant$1 or herb$).mp. [mp=abstract, heading words, title] 35. randomized controlled trial$/ 36. random allocation/ 37. double blind method/ 38. single blind method.mp. 39. exp Clinical trials/ 40. (clin$ adj25 trial$).mp. [mp=abstract, heading words, title] 41. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$ or dummy)).mp. [mp=abstract, heading words, title] 42. (placebo$ or random$).mp. [mp=abstract, heading words, title] 43. research design/ or clinical trials/ or comparative study/ or double blind method/ or random allocation/ 44. prospective studies.mp. 45. cross over studies.mp. 46. Follow up studies/ 47. control$.mp. 48. (multicent$ or multi‐cent$).mp. [mp=abstract, heading words, title] 49. ((stud or design$) adj25 (factorial or prospective or intervention or crossver or cross‐over or quasi‐experiment$)).mp. [mp=abstract, heading words, title] 50. 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 51. or/6‐34 52. 5 and 50 and 51
Appendix 5. LILACS search strategy
((Pt RANDOMIZED CONTROLLED TRIAL OR Pt CONTROLLED CLINICAL TRIAL OR Mh RANDOMIZED CONTROLLED TRIALS OR Mh RANDOM ALLOCATION OR Mh DOUBLE‐BLIND METHOD OR Mh SINGLE‐BLIND METHOD OR Pt MULTICENTER STUDY) OR ((tw ensaio or tw ensayo or tw trial) and (tw azar or tw acaso or tw placebo or tw control$ or tw aleat$ or tw random$ or (tw duplo and tw cego) or (tw doble and tw ciego) or (tw double and tw blind)) and tw clinic$)) AND NOT ((CT ANIMALS OR MH ANIMALS OR CT RABBITS OR CT MICE OR MH RATS OR MH PRIMATES OR MH DOGS OR MH RABBITS OR MH SWINE) AND NOT (CT HUMAN AND CT ANIMALS)) [Words] and chinese or herb$ or traditional [Words] and eczema or dermatitis [Words]
Appendix 6. CINAHL (EBSCO) search strategy
S1 (MM "Eczema") OR (MM "Dermatitis, Atopic") S2 (MH "Medicine, Chinese Traditional") OR (MH "Drugs, Chinese Herbal") S3 TI (Chinese and (herb* or medicin* or traditional or plant*)) S4 AB (Chinese and (herb* or medicin* or traditional or plant*)) S5 S2 or S3 or S4 S6 TI eczema or dermatitis S7 S1 or S6 S8 S5 and S7 S9 (MH "Clinical Trials+") S10 PT clinical trial S11 TX (clinic* n1 trial*) S12 (MH "Random Assignment") S13 TX random* allocat* S14 TX placebo* S15 (MH "Placebos") S16 (MH "Quantitative Studies") S17 TX allocat* random* S18 "randomi#ed control* trial*" S19 TX ( (singl* n1 blind*) or (singl* n1 mask*) ) or TX ( (doubl* n1 blind*) or (doubl* n1 mask*) ) or TX ( (tripl* n1 blind*) or (tripl* n1 mask*) ) or TX ( (trebl* n1 blind*) or (trebl* n1 mask*) ) S20 S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 S21 S8 and S20
Appendix 7. Chinese database CQVIP search strategy
“(Keyword_C=异位性皮炎)*((Keyword_C=(中医药)+Title_C=(中医药)))”,
“(Keyword_C=异位性湿疹)*((Keyword_C=(中医药)+Title_C=(中医药)))”,
“(Keyword_C=异位性湿疹)*((Keyword_C=(中药)+Title_C=(中药)))”,
“(Keyword_C=特应性皮炎)*((Keyword_C=(中医药)+Title_C=(中医药)))”,
“(Keyword_C=特应性皮炎)*((Keyword_C=(中药)+Title_C=(中药)))”,
“(Keyword_C=特异性湿疹)*((Keyword_C=(中医)+Title_C=(中医)))”
“(Keyword_C=四弯风)*((Keyword_C=(中医)+Title_C=(中医)))”,
“(Keyword_C=婴幼儿湿疹)*((Keyword_C=(中医药)+Title_C=(中医药)))”
“(Keyword_C=儿童湿疹)*((Keyword_C=(中医药)+Title_C=(中医药)))”
Appendix 8. Chinese database CNKI search strategy
(发表时间 between (1979,2011)) 并且 (( (题名=中英文扩展(异位性皮炎) 或者 题名=中英文扩展(异位性湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
(发表时间 between (2011, 2012)) 并且 (( (题名=中英文扩展(异位性皮炎) 或者 题名=中英文扩展(异位性湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
(发表时间 between (2012‐09‐14, 2013‐06‐12)) 并且 (( (题名=中英文扩展(异位性皮炎) 或者 题名=中英文扩展(异位性湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
(发表时间 between (1979,2011)) 并且 (( (题名=中英文扩展(特应性皮炎) 或者 题名=中英文扩展(特异性湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
(发表时间 between (2011, 2012)) 并且 (( (题名=中英文扩展(特应性皮炎) 或者 题名=中英文扩展(特异性湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
(发表时间 between (2012‐09‐14, 2013‐06‐12)) 并且 (( (题名=中英文扩展(特应性皮炎) 或者 题名=中英文扩展(特异性湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
(发表时间 between (1979,2011)) 并且 (( (题名=中英文扩展(婴幼儿湿疹) 或者 题名=中英文扩展(儿童湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
(发表时间 between (2011, 2012)) 并且 (( (题名=中英文扩展(婴幼儿湿疹) 或者 题名=中英文扩展(儿童湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
(发表时间 between (2012‐09‐14, 2013‐06‐12)) 并且 (( (题名=中英文扩展(婴幼儿湿疹) 或者 题名=中英文扩展(儿童湿疹))) 并且 全文=中英文扩展(中医药)) (精确匹配)
Appendix 9. Chinese database Wanfang data search strategy
title:异位性皮炎 keyword:中医药 date:1982‐2013
title:异位性湿疹 keyword:中医药 date:1982‐2013
title:特应性皮炎 keyword:中医药 date:1982‐2013
title:特应性湿疹 keyword:中医药 date:1982‐2013
title:四弯风date:1982‐2013
title:婴幼儿湿疹 keyword:中医药 date:1982‐2013
title:儿童湿疹 keyword:中医药 date:1982‐2013
Appendix 10. List of contacted Chinese medicine dermatologists or experts
Professor Rudi Ai, Professor Dacan Chen, Dr Chi Jing Liu, Professor Chuanjian Lu, Dr Xiumei Mo.
Data and analyses
Comparison 1. CHM versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total effectiveness rate (number of participants recovered and significantly improved) | 2 | 85 | Risk Ratio (IV, Random, 95% CI) | 2.09 [1.32, 3.32] |
| 2 Itching VAS | 2 | 94 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.53 [‐2.64, ‐0.41] |
| 3 Overall severity score | 4 | 239 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.67, ‐0.09] |
| 4 Overall severity score (short‐term improvement) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 QoL | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 QoL (short‐term improvement) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Adverse events | 2 | 129 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.06, 8.67] |
| 8 Adverse events in one study | 1 | Risk Ratio (Fixed, 95% CI) | Totals not selected |
Comparison 2. CHM versus drugs.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total effectiveness rate (number of participants recovered and significantly improved) with subgroup analysis | 21 | 1868 | Risk Ratio (IV, Random, 95% CI) | 1.43 [1.27, 1.61] |
| 1.1 Individualised treatment | 7 | 567 | Risk Ratio (IV, Random, 95% CI) | 1.50 [1.30, 1.74] |
| 1.2 Non‐individualised treatment | 14 | 1301 | Risk Ratio (IV, Random, 95% CI) | 1.37 [1.17, 1.60] |
| 2 Total effectiveness rate (long‐term improvement) | 2 | 276 | Risk Ratio (IV, Random, 95% CI) | 1.52 [1.11, 2.08] |
| 3 Itching VAS | 7 | 465 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.43, ‐0.22] |
| 4 Overall severity score | 15 | 1062 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.97 [‐1.23, ‐0.71] |
| 5 Overall severity score (long‐term improvement) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Adverse events | 15 | 1396 | Risk Ratio (IV, Random, 95% CI) | 0.44 [0.32, 0.61] |
| 7 Total effectiveness rate with posthoc subgroup analysis | 21 | 1868 | Risk Ratio (IV, Random, 95% CI) | 1.43 [1.27, 1.61] |
| 7.1 CHM versus topical steroid | 6 | 671 | Risk Ratio (IV, Random, 95% CI) | 1.18 [0.99, 1.40] |
| 7.2 CHM versus antihistamines | 12 | 906 | Risk Ratio (IV, Random, 95% CI) | 1.58 [1.37, 1.82] |
| 7.3 CHM versus other agents | 3 | 291 | Risk Ratio (IV, Random, 95% CI) | 1.58 [1.31, 1.90] |
Comparison 3. Combination of oral and topical CHM versus same oral CHM.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total effectiveness rate (number of participants recovered and significantly improved) | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Total effectiveness rate (long‐term improvement) | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Itching VAS | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 4 Skin lesion score | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 5 Overall severity score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 QoL | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Adverse events | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cao 2009.
| Methods | This was a randomised, non‐blinded, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of a university teaching hospital in Nanjing, China 2. Age: from 2 to 16 years of age 3. Sex (men/women): 32/24 4. Number of participants randomised: 56 5. T/C: 32/24 |
|
| Interventions |
I. Treatment group 1. Zhuling Jianpi Huashi decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group a. oral ingestion 2. Cetirizine hydrochloride drops 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ CHM lotion and cream (external use) were applied in both groups |
|
| Outcomes | 1. Percentage of reduction of total SASSAD score 2. Effectiveness rate 3. Adverse events All assessments were conducted at baseline, week 4, and at the end of the 8‐week treatment period, respectively |
|
| Notes | 1. The trial investigator claimed they included only those who were diagnosed with AD and identified as "spleen deficiency with accumulation of dampness" in Chinese medicine 2. Effectiveness rate = ((pre‐treatment score of SASSAD ‐ post‐treatment score of SASSAD)/pre‐treatment score of SASSAD) * 100% 3. The treatment intervention used was the same as the 1 orally used in Zhang 2005 4. The SASSAD scores were expressed as 'numbers ±' without labels, and we assumed they meant mean ± SD |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...used SPSS software for randomisation..." |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "...no blinding was required" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "...no blinding was required" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Those who were not compliant with the treatment were excluded" Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SASSAD |
Chao 2003.
| Methods | This was a randomised, controlled, 4‐arm parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from the outpatient dermatology department of hospitals in Qingdao, China 2. Age: from 1 to 38 months 3. Sex (men/women): 58/62 4. Number of participants randomised: 120 5. T/T/C/C: 30/30/30/30 |
|
| Interventions |
I. Treatment group (A) (1st arm) 1. Huangbai Zicao Diyu cream (5%). Data from this group were not used for comparison in this review as the trial investigator reported that the total effectiveness rate of the 2nd arm (group B) was superior to that in the 1st arm (group A) 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Treatment group (B) (2nd arm)
III. Control group (C) (3rd arm) 2. Compound Econazole nitrate cream (Pevisone) 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
IV. Control group (D) (4th arm) 2. Placebo 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ CHM lotion (external use) for washing the skin lesion was applied in all groups |
|
| Outcomes | 1. Skin lesion score. The trial investigators developed the scoring system. The trial investigators expressed data as "mean ±", and we assumed the "±" was SD 2. Effectiveness rate 3. Adverse events 4. Bacteriologic eradication rate on the skin lesions All assessments were conducted at baseline, weeks 1 and 2, and at the end of the 3‐week treatment period, respectively |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance of the treatment intervention and placebo were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Those who did not use the creams on time, or did not turn up for re‐assessment or drop out were excluded" Quote: "We recruited 132 participants and excluded 12 patients due to non compliance with the trial" Comment: The trial did not use ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Unclear risk | The trial used a scoring system developed by the trial investigators |
Chen 2011.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of a Chinese medicine hospital in Changshu, China 2. Age: from 58 days to 2 years of age 3. Sex (men/women): 59/41 4. Number of participants randomised: 100 5. T/C: 50/50 |
|
| Interventions |
I. Treatment group 1. Huanglian Qingdai ointment 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Mometasone furoate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. Severity of itching score (measured by participant‐rated score, scale 0 to 3) 2. Skin lesion (erythema and papule) score (measured by clinician‐rated score). The trial investigators developed the scoring system 3. Skin lesion area score (measured by clinician‐rated score). The trial investigators developed the scoring system 4. Effectiveness rate (the trial investigator developed the rating) 5. Adverse events All assessments were conducted at baseline and at the end of the 2‐week treatment period |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Unclear risk | The trial used a scoring system developed by the trial investigators |
Cheng 2010.
| Methods | This was a randomised, double‐blind, placebo‐controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from the department of Integration of Traditional Chinese and Western Medicine, in a university hospital in Taiwan 2. Age: from 8 to 23 years of age 3. Sex (men/women): 37/34 4. Number of participants randomised: 71 5. T/C: 47/24 |
|
| Interventions |
I. Treatment group 1. Xiao‐Feng‐San (XFS) 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Placebo 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. Improvement of clinical lesion score from baseline (the sum of erythema score and surface damage score measured by clinician‐rated score) 2. Improvement of itching relief score from baseline (measured by participant‐rated score) 3. Improvement of sleep score from baseline (measured by participant‐rated score) 4. Adverse events 5. Full blood count, serum bilirubin, aspartate aminotransferase, alkaline phosphatase, albumin, urea and electrolytes, creatinine, calcium, phosphate, glucose, creatine phosphokinase and immunologic markers (IgE, eosinophil count, eosinophil cationic protein, IL‐5, IL‐13) All assessments were conducted at baseline and weeks 4, 8, and 12 of the trial |
|
| Notes | 1. Outcomes 1 to 3 were expressed as least‐squares means ± SE at end points 2. There was a total of 15 withdrawals/dropouts. 69 participants (T/C: 46/23) were included in the ITT analysis 3. The final number of participants completing the entire trial was 56 (T/C: 35/21) 4. Ingredients of the treatment intervention were also used by Luo 2010 5. The trial was supported by the Department of Health, Committee on Chinese Medicine and Pharmacy, Taiwan |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible patients were randomized at a ratio of 2:1 to receive XFS or placebo for an 8‐week treatment period" |
| Allocation concealment (selection bias) | Low risk | Quote: "The computer generated randomisation list was drawn up by an independent statistician and placed in an envelope until the study was completed" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Both participants and evaluating physicians were unaware [of] the interventions used" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Both participants and evaluating physicians were unaware [of] the interventions used" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incomplete outcome data and ITT analysis were addressed |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Unclear risk | Quote: "...using a standardised scoring system" Comment: We found no evidence that the scoring system had been validated |
Gong 2010.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient and inpatient department of a Chinese medicine hospital in Changsha, China 2. Age: from 16 to 65 years of age 3. Sex (men/women): 31/25 4. Number of participants randomised: 56 5. T/C: 28/28 |
|
| Interventions |
I. Treatment group 1. Liangxue Xiaofeng decoction 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Desloratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ CHM lotion (external use) for washing the skin lesion was applied 3 times daily in both groups |
|
| Outcomes | 1. SCORAD score 2. Effectiveness rate 3. Adverse events All assessments were conducted at baseline, at the end of the 4‐week treatment period, and 12 weeks after the 4‐week treatment period |
|
| Notes | The trial was funded by the Department of Science and Technology, Hunan Province, China | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...random number table was used for stratified randomisation" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Hon 2007.
| Methods | This was a randomised, double‐blind placebo‐controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from the paediatric dermatology outpatient of a university teaching hospital in Hong Kong, China 2. Age: from 5 to 21 years of age 3. Sex (men/women): 46/39 4. Number of participants randomised: 85 5. T/C: 42/43 |
|
| Interventions |
I. Treatment group 1. TCHM capsules 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Placebo 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. SCORAD score 2. CDLQI score 3. Adverse events 4. Record of the usage of trial medications and primary Western medications All assessments were conducted at baseline, every 4 weeks during the trial period, and at the end of the 12‐week course (visit 4) 5. Complete blood counts; eosinophil counts; total IgE levels; liver and renal function were obtained before treatment (visit 1) and at the end of the 12‐week course (visit 4) |
|
| Notes | 1. There were 2 non‐compliant participants in the control group 2. The trial was reported again in February 2011 3. The trial was supported by the Health and Health Services Research Fund, Food and Health Bureau, Hong Kong SAR Government |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The Institute of Chinese Medicine (ICM) of the Chinese University of Hong Kong allocated TCHM or placebo treatment by using a computer generated randomization code" |
| Allocation concealment (selection bias) | Low risk | Quote: "The investigators were not allowed to break the code for any patient until the trial was completed" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The trial medications were supplied in containers labelled with the randomisation codes. The drugs were allocated to patients in strict numerical sequence. TCHM and placebo were provided in matching capsules" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Statistical analysis of the clinical and laboratory data was performed independently by a statistician not involved in the clinical trial" Quote: "...counting and weighing of unused trial medications and primary medications were performed by the research assistant and such information was blinded from the principal investigator" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis was performed |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Huang 2010.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from the a hospital in Mianyang, China 2. Age: from 3 months to 22 years of age 3. Sex (men/women): 96/99 4. Number of participants randomised: 195 5. T/C: 98/97 |
|
| Interventions |
I. Treatment group 1. Chushi Zhiyang ointment (a CHM product manufactured by a pharmaceutical company) 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Clobetasol propionate ointment 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Oral ingestion of phenergan syrup and moist dressing with 3% boric acid solution and infrared rays therapy for acute and subacute cases in both groups |
|
| Outcomes | 1. EASI score 2. Effectiveness rate 3. Adverse events (asessments were conducted at baseline, every week during the trial period, respectively, and follow‐up 3 months after the 2‐week treatment) 4. Full blood counts, liver and renal function tests Conducted after a 2‐week treatment period |
|
| Notes | The treatment intervention Chushi Zhiyang ointment was also used in Wang 2008 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...random number table was used" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | High risk | Quote: "...full blood counts, liver and renal function tests were performed after 2‐weeks treatment" Comment: The proposed outcomes were not reported |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used EASI |
Jin 2007.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a Chinese medicine hospital in Shenzhen, China 2. Age: from 10 to 52 years of age 3. Sex (men/women): 40/22 4. Number of participants randomised: 62 5. T/C: 32/30 |
|
| Interventions |
I. Treatment group 1. Jianpi Zhiyang granules 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. SCORAD score 2. Severity of itching score (measured by patient‐rated VAS, scale 0 to 10) 3. Serum IgE level and eosinophil count All assessments were conducted at baseline and at the end of the 4‐week treatment period |
|
| Notes | 1. The trial did not report adverse events 2. The treatment intervention was the same as that orally ingested in the Yang 2007 study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Those who did not completed the trial were excluded" Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Lang 2007.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from the dermatology department of a Chinese medicine hospital in Beijing, China 2. Age: from 3 to 34 years of age 3. Sex (men/women): 31/33 plus 8 dropouts without statement of gender 4. Number of participants randomised: 72 5. T/C: 36/36 |
|
| Interventions |
I. Treatment group a. Oral ingestion 1. Shengui decoction 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application 1. Shidu ointment 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group a. Oral ingestion 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Hydrocortisone cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. EASI score 2. Severity of itching score (measured by participant‐rated score, scale 0 to 3) 3. Effectiveness rate 4. Adverse events All measurements were performed at baseline and at the end of the 4‐week treatment period |
|
| Notes | The final number of participants evaluated was 64 (T/C: 33/31) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...random number table was used" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There were 8 dropouts/withdrawals (3 in the treatment group and 5 in the control group). The investigators did not report reasons for dropouts/withdrawals, and ITT analysis was not used |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used EASI |
Lin 2010.
| Methods | This was a randomised, controlled, within‐patient trial | |
| Participants | 1. Setting: The trial recruited participants from the dermatology department of a Chinese medicine teaching hospital in Guangzhou, China 2. Age: from 11 months to 27 years of age 3. Sex (men/women): 13/10 4. Number of participants randomised: 23 |
|
| Interventions |
I. Treatment group 1. Runfu Xiaoyan lotion 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. No external CHM lotion was used ‐ Basic moisturising cream was used topically for both groups and oral ingestion of Qingxin Peitu decoction for moderate and severe cases |
|
| Outcomes | 1. Skin lesion score (measured by clinician‐rated score) 2. Severity of itching score (measured by participant‐rated VAS, scale 0 to 10) 3. SCORAD 4. Adverse events All assessments were conducted at baseline, week 1, and at the end of the 2‐week treatment period |
|
| Notes | 1. This was a within‐patient trial. CHM was topically used on a randomised selected arm or leg of the participant for comparison with the other non‐treatment site of the same participant 2. There was 1 dropout due to exacerbation of the condition after using the intervention. The final number of participants evaluated was 22 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...computer generated random number table was used for selection of the involved site of the patients" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: It is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Five cases did not come back for assessment but last observation carried forward (LOCF) was performed" Comment: There was another 1 dropout, but ITT analysis was not used |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Liu 2005.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of a Chinese medicine teaching hospital in Changsha and a specialty outpatient department of a teaching hospital in Hong Kong, China 2. Age: from 3 months to 42 years of age 3. Sex (men/women): 98/86 4. Number of randomised: 184 5. T/C: 92/92 |
|
| Interventions |
I. Treatment group a. Oral ingestion 1. Cangyi decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application 1. Qingdai ointment and Huangbai lotion 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group a. Oral ingestion 2. Terfenadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Dexamethasone cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. Effectiveness rate 2. Adverse events Assessments were measured at baseline and at the end of the 4‐ to 8‐week treatment period 3. Recurrence rate Conducted at 24 weeks after the treatment period |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | High risk | The trial did not use a published validated scoring system |
Luo 2010.
| Methods | This was a randomised, non‐blind, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from the departments of Chinese medicine and dermatology in a teaching hospital in Taiwan 2. Age: from 7 to 14 years of age 3. Sex (men/women): 36/26 4. Number of participants randomised: 62 5. T/C: 34/28 |
|
| Interventions |
I. Treatment group 1. Xiao‐Feng‐San with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine tablet and antihistamine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. Percentage of reduction of total SASSAD score 2. Effectiveness rate 3. Adverse events Assessments were conducted at baseline and weeks 4, 8, 14, and 16 of the treatment period 4. Full counts of blood, routine tests of urine and stool 5. Electrocardiogram, liver and renal function tests Assessment time points were not stated |
|
| Notes | 1. The trial investigator claimed that they included only those who were diagnosed with AD and identified as "spleen deficiency with accumulation of dampness" in acute stage with wind, heat, or dampness in Chinese medicine 2. Effectiveness rate = ((pre‐treatment score of SASSAD ‐ post‐treatment score of SASSAD)/pre‐treatment score of SASSAD) * 100% 3. Ingredients of the treatment intervention were also used by Cheng 2010 4. The SASSAD scores were expressed as 'numbers ±' without labelled by the trial investigators, and we assumed they were mean ± SD |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...used SPSS software for randomisation" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "No blinding was required" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "No blinding was required" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SASSAD |
Ma 2010.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient and inpatient department of dermatology in a Chinese medicine teaching hospital in Beijing, China 2. Age: from 7 to 33 years of age 3. Sex (men/women): 42/40 4. Number of participants randomised: 82 5. T/C: 42/40 |
|
| Interventions |
I. Treatment group a. Oral ingestion 1. Jianpi Runfu decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application 1. Gancao oil 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group a. Oral ingestion 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Butyl flufenamate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. EASI score 2. Severity of itching score (measured by participant‐rated VAS, scale 0 to 10) 3. Adverse events All measurements were conducted at baseline and at the end of the 4‐week treatment period |
|
| Notes | 1. The trial investigator claimed they included only those who were diagnosed with AD and identified as "spleen deficiency with dryness of blood" in Chinese medicine 2. The trial was funded by the 51510 Science and technology project of Chinese medicine, Beijing ("the 11th of five‐year planning") and Zhao Bingnan renown expert research laboratory, passing on the heritage of Chinese medicine 3+3 project, Beijing, China |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...random number table was used" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "...one in treatment group and two in control group dropouts which were treated as no effects" |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used EASI |
Rao 2010.
| Methods | This was a randomised, placebo‐controlled, 3‐arm parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a Chinese medicine teaching hospital in Nanjing, China 2. Age: from 7 to 25 years of age 3. Sex (men/women): 20/10 4. Number of participants randomised: 30 5. T/C/C: 10/10/10 |
|
| Interventions |
I. Treatment group a. Oral ingestion 1. Qingxin Peitu decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application 1. Qingxin Peitu lotion 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group A
III. Control group B (Data of this group were not used for comparison in this review) a. Oral ingestion 2. Placebo plus cetirizine hydrochloride tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Mometasone furoate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. SCORAD score 2. Investigators' Global Assessment score (IGA) 3. Effectiveness rate Assessments were conducted at baseline, every 4 weeks during the trial period, at the end of the 12‐week treatment period, and 24 weeks after the 12‐week treatment period 4. Participant's self experience Assessment was conducted at baseline, every 2 weeks during the trial period, and at the end of the 12‐week treatment period 5. CDLQI or DLQI score Assessment was conducted at baseline, at the end of the 12‐week treatment period, and 24 weeks after the 12‐week treatment period 6. Full counts of blood, routine tests of urine and stool 7. Electrocardiogram, liver and renal function 8. Adverse events Assessments were conducted at baseline and at the end of the 12‐week treatment period |
|
| Notes | The interventions used in control group B were not comparable to other groups; thus, the outcome of this group was not included for evaluation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...used SPSS17.0 software for randomisation" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "...no blinding was required" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "...outcomes were evaluated by the third party person" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Sun 2009.
| Methods | This was a randomised, double‐blind, placebo‐controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a Chinese medicine teaching hospital in Guangzhou, China 2. Age: from 3 to 20 years of age 3. Sex (men/women): 12/13 4. Number of participants randomised: 25 5. T/C: 14/11 |
|
| Interventions |
I. Treatment group 1. Jianpi Shenshi granules 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Placebo 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Both groups applied non‐medicinal moisturising cream topically and oral ingestion of cyproheptadine tablets for cases with severe itchiness |
|
| Outcomes | 1. SCORAD score 2. Severity of itching score (measured by participant‐rated score, scale unknown) 3. Sleeping disturbance rate 4. Skin lesion area 5. Severity of skin lesion 6. Effectiveness rate 7. Adverse events All assessments were conducted at baseline and at the end of the 4‐week treatment period 8. Recurrence rate Conducted at 24 weeks after the 4‐week treatment period |
|
| Notes | 1. The trial investigator claimed that they included only those who were diagnosed with AD and identified as "spleen deficiency" in Chinese medicine 2. The trial was funded by Department of Science and Technology, Guangdong Provience, China |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "...double‐blind controlled trial" Comment: No details of blinding were provided, and the paper was published by only 1 author without acknowledgment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Tian 2005.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a hospital in Yingkou, China 2. Age: children (age not stated) 3. Sex (men/women): 71/29 4. Number of participants randomised: 100 5. T/C: 58/42 |
|
| Interventions |
I. Treatment group a. Oral ingestion 1. Fuyang granules 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application
II. Control group a. Oral ingestion 2. Cyproheptadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Sulphur cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. Effectiveness rate developed by the trial investigators 2. Adverse events Assessments were measured at baseline and at the end of the 5‐day treatment period |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | High risk | The trial did not use a published validated scoring system |
Wang 2008.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department in a teaching hospital in Yichang, China 2. Age: from 12 days to 11 months 3. Sex (men/women): 22/43 4. Number of participants randomised: 65 5. T/C: 35/30 |
|
| Interventions |
I. Treatment group 1. Chushi Zhiyang ointment (a CHM product manufactured by a pharmaceutical company) 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Vitamin B₆ cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. Effectiveness rate developed by the trial investigators 2. Adverse events Assessments were measured at baseline and at the end of the 1‐week treatment period |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The 2 interventions were made by the 2 pharmaceutical companies, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | High risk | The trial did not use a published validated scoring system |
Xiao 2008.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient and inpatient department of dermatology in a Chinese medicine teaching hospital in Chengdu, China 2. Age: from 3 to 23 years of age 3. Sex (men/women): 29/23 4. Number of participants randomised: 52 5. T/C: 26/26 |
|
| Interventions |
I. Treatment group a. Oral ingestion 1. Machixian decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application
II. Control group a. Oral ingestion 2. Chlorphenamine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Boric acid solution 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Sesame oil was used for cases with dry skin twice daily for both groups |
|
| Outcomes | 1. SCORAD score 2. Adverse events Assessments were conducted at baseline and at the end of the 8‐week treatment period 3. Full counts of blood, routine tests of urine and stool, liver and renal function tests, serum IgE level Assessments were conducted at baseline and at the end of the 8‐week treatment period 4. Recurrence rate Assessment was conducted at 12 weeks after the treatment period |
|
| Notes | The trial investigator claimed that they included only those who were diagnosed with AD and identified as "dampness‐heat" in Chinese medicine | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Xiao 2011.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a Chinese medicine teaching hospital in Guangzhou, China 2. Age: from 2 to 60 years of age 3. Sex: did not state 4. Number of participants randomised: 60 5. T/C: 30/30 |
|
| Interventions |
I. Treatment group 1. Huailian decoction 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ External use of nitrofurazone, calamine, menthol, and CHM ointment for both groups |
|
| Outcomes | 1. SCORAD score 2. Effectiveness rate 3. Adverse events Assessments were conducted at baseline, week 2, and at the end of the 4‐week treatment period 4. Full counts of blood, routine tests of urine and stool, liver and renal function tests Asssesments were conducted at baseline and after the 4‐week treatment period 5. Recurrence rate Conducted at 24 weeks after the 4‐week treatment period |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...computer generated random numbers were used" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Xue 2011.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from a Chinese medicine hospital in Jiangmen, China 2. Age: from 2 to 12 years of age 3. Sex (men/women): 37/26 4. Number of participants randomised: 63 5. T/C: 33/30 |
|
| Interventions |
I. Treatment group 1. Shengxue Runfu decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Topical application of CHM ointment and emollients for both groups |
|
| Outcomes | 1. SCORAD score 2. Severity of itching score (measured by participant‐rated score, scale 0 to 10) 3. Skin lesion area score 4. Severity of skin lesion score 5. Effectiveness rate 6. Chinese medicine clinical syndrome score All assessments were conducted at baseline, week 4, and at the end of the 8‐week treatment period |
|
| Notes | 1. The trial investigators claimed that they included only those who were diagnosed with AD and identified as "blood deficiency with wind‐dryness" in Chinese medicine 2. Did not report adverse event 3. The trial was funded by Guangdong Bureau of Chinese Medicine, China |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "...only those who took the herbal decoction for 20 days or more at week 4 of the trial were included for statistic analysis" Comment: ITT was not used for those who took herbal decoction for less than 20 days |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Yang 2007.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology of a Chinese medicine teaching hospital in Shenzhen, China 2. Age: from 5 to 25 years of age 3. Sex (men/women): 35/29 4. Number of participants randomised: 64 5. T/C: 32/32 |
|
| Interventions |
I. Treatment group a. Oral ingestion 1. Jianpi Zhiyang granules 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application 1. Pibao Xiaoyan Xuanshi ointment 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group a. Oral ingestion 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Hydrocortisone butyrate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. SCORAD score 2. Severity of itching score (measured by participant‐rated VAS, scale 0 to 10) 3. Effectiveness rate 4. Adverse events 5. Serum IgE level and eosinophil count All assessments were conducted at baseline and at the end of the 4‐week treatment period |
|
| Notes | 1. The oral ingestion treatment intervention was the same as that used in Jin 2007 2. The trial was funded by Shenzhen Science and Technology Planning Project, China |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 4 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insuficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Yang 2009.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of a Chinese medicine teaching hospital and dermatology and venereology outpatient department of a teaching hospital in Kunming, China 2. Age: from 4 to 27 years of age 3. Sex (men/women): 33/27 4. Number of participants randomised: 60 5. T/C: 30/30 |
|
| Interventions |
I. Treatment group 1. Jianpi Yangxue Qufeng decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. Skin lesion area score (measured by clinician‐rated score) 2. Skin lesion severity score (measured by clinician‐rated score) 3. Severity of itching score (measured by participant‐rated VAS, scale 0 to 3) 4. Erythema score (measured by clinician‐rated score) 5. Transepidermal water loss, skin oil, and skin elasticity (measured by a multifunctional skin testing equipment) 6. Effectiveness rate 7. Adverse events All assessments were conducted at baseline and at the end of the 4‐week treatment period |
|
| Notes | 1. The trial investigator claimed that they included only those who were diagnosed with AD and identified as "spleen deficiency with dryness of blood" in Chinese medicine 2. 30 healthy volunteers were also recruited for assessment of transepidermal water loss, skin oil, and skin elasticity 3. The paper did not provide continuous data of outcomes 1 to 4 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...random number table was used" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Unclear risk | The trial used a scoring system developed by the trial investigators |
Yu 1999.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient and inpatient department in 3 hospitals in Shanghai and Hangzhou, China 2. Age: from 5 to 53 years of age 3. Sex (men/women): 112/108 4. Number of participants randomised: 220 5. T/C: 120/100 |
|
| Interventions |
I. Treatment group 1. Piyan Xiaojingyin granules II 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine (Clarityne) tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Topical application of saline or zinc oxide cream for both groups |
|
| Outcomes | 1. Skin lesion severity score (measured by clinician‐rated score) 2. Skin lesion area score (measured by clinician‐rated score) 3. Severity of itching score (measured by participant‐rated VAS, scale 0 to 3) 4. Effectiveness rate 5. Adverse events Assessments were conducted at baseline, at the end of the 12‐week treatment period, and 52 weeks after the 12‐week treatment period 6. Serum CD4/CD8 ratio and IgE level Assessments were conducted at baseline and at the end of the 12‐week treatment period |
|
| Notes | 1. The trial investigator claimed they only included those who were diagnosed with AD and identified as "spleen deficiency with dryness of blood" in Chinese medicine 2. The trial did not provide continuous data of outcomes 1 to 3 3. The trial was funded and registered in the State Administration of Traditional Chinese Medicine, China 4. The trial passed the evaluation at the Ministerial level on 18 August 1998 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Unclear risk | The trial used a scoring system developed by the trial investigators |
Zhang 2005.
| Methods | This was a randomised, controlled, 3‐arm parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a Chinese medicine teaching hospital in Nanjing, China 2. Age: below or at 16 years of age 3. Sex (men/women): did not state 4. Number of participants randomised: 45 5. T/C/C: 15/15/15 |
|
| Interventions |
I. Treatment group 1. Jianpi Huashi decoction 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group A 2. Chlorpheniramine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
III. Control group B
‐ Topical application of CHM lotion or CHM ointment according to the condition of an individual in all groups |
|
| Outcomes | 1. Percentage of reduction of total SASSAD score 2. Severity of itching score from baseline (measured by participant‐rated VAS, scale 0 to 10) 3. IgE and EOS level 4. Effectiveness rate 5. Adverse events All measurements were conducted at baseline, 4 weeks, and at the end of the 12‐week treatment period |
|
| Notes | The SASSAD scores were expressed as 'numbers ±' without labels, and we assumed they meant mean ± SD | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SASSAD |
Zhang 2009.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a Chinese medicine teaching hospital in Jinan, China 2. Age: from 2 to 12 years of age 3. Sex (men/women): did not state 4. Number of participants randomised: 61 5. T/C: 36/25 |
|
| Interventions |
I. Treatment group 1. Xiao'er Huashi decoction 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine granules 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ External use of CHM lotion and CHM cream for both groups |
|
| Outcomes | 1. EASI score 2. Effectiveness rate Assessments were conducted at baseline and at the end of the 4‐week treatment period 3. Recurrence rate Conducted at 4 weeks after the 4‐week treatment period |
|
| Notes | 1. The trial did not report adverse events 2. The trial did not provide continuous data of EASI score |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not stated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used EASI |
Zhang 2011.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a Chinese medicine teaching hospital in Tianjin, China 2. Age: 2.5 to 14 years of age 3. Sex (men/women): 31/25 4. Number of randomised: 56 5. T/C: 30/26 |
|
| Interventions |
I. Treatment group 1. Self‐designed CHM decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Levocetirizine dihydrochloride tablets 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. SCORAD score 2. Effectiveness rate Assessments were conducted at baseline and at the end of the 8‐week treatment period 3. Recurrence rate Conducted at 24 weeks after the 8‐week treatment period |
|
| Notes | The trial did not report adverse events | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...random number table was used" |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | Low risk | The trial used SCORAD |
Zhou 2011.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in Jiangyong country Chinese medicine hospital in Hunan, China 2. Age: 3 to 38 months old 3. Sex (men/women): 95/81 4. Number of participants randomised: 176 5. T/C: 89/87 |
|
| Interventions |
I. Treatment group 1. Cang Er Kushen lotion 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Calamine lotion 2.1 Ingredients and dosage
2.2 Adminstration
2.3 Duration of treatment
2.4 Follow up
|
|
| Outcomes | 1. Effectiveness rate 2. Adverse events Assessments were conducted at baseline and at the end of the treatment period 3. Recurrence rate Conducted at 24 weeks after the 2‐week treatment period |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised into treatment or control group at a ratio of 1:1" Comment: The paper did not state how random sequence was generated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | High risk | The trial did not use a published validated scoring system |
Zou 2011.
| Methods | This was a randomised, controlled, parallel clinical trial | |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of dermatology in a Chinese medicine teaching hospital and another teaching hospital in Nanchang, China 2. Age: 3 to 36 months old 3. Sex (men/women): 27/23 4. Number of participants randomised: 50 5. T/C: 30/20 |
|
| Interventions |
I. Treatment group 1. Fufang Sanhuang lotion and oil 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Boric acid solution and zinc oxide cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow‐up
|
|
| Outcomes | 1. Effectiveness rate 2. Serum IgE, EOS, liver and renal function tests 3. Adverse events Assessments were conducted at baseline and at the end of the 2‐week treatment period 4. Recurrence rate Conducted at 12 weeks after the 2‐week treatment period |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised into treatment or control group at a ratio of 3:2 according to the proportion principle of ratio not less than 2:1" Comment: The paper did not state how random sequence was generated |
| Allocation concealment (selection bias) | Unclear risk | This was not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was not stated Comment: The appearance and administration of the 2 interventions were different, so it is unlikely that a blinding method was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This was not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This was not stated Comment: The numbers of participants randomised and analysed were equivalent. It seems that there were no withdrawals/dropouts in this study |
| Selective reporting (reporting bias) | Unclear risk | There was insufficient information |
| Other potential sources of bias (use of published validated scoring system ) | High risk | The trial did not use a published validated scoring system |
CDLQI: Children's Dermatology Life Quality Index CHM: Chinese herbal medicine DLQI: Dermatology Life Quality Index EASI: Eczema Area and Severity Index ITT: Intention‐to‐treat POEM: Patient‐oriented Eczema Measure SASSAD: Six Area, Six Sign Atopic Dermatitis severity score SCORAD: Severity Scoring of Atopic Dermatitis T/C: Treatment group/Control group VAS: Visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Li 2006 | The trial used inappropriate comparator interventions |
| Udompataikul 2011 | The trial used inappropriate treatment interventions |
| Zhang 2010 | The trial used inappropriate comparator interventions |
| Zhao 2008 | The trial used inappropriate comparator outcome measures |
Characteristics of studies awaiting assessment [ordered by study ID]
Cai 2012.
| Methods | This was a randomised, controlled, parallel clinical trial |
| Participants | 1. Setting: The trial recruited participants from an outpatient dermatology department of a Chinese medicine hospital in Zhangzhou, China 2. Age: from 1.5 to 13 years of age 3. Sex (men/women): 49/35 4. Number of participants randomised: 84 5. T/C: 43/41 |
| Interventions |
I. Treatment group 1. Shenling Baizhu decoction with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Topical application of triamcinolone acetonide acetate cream and vitamin B₆ cream were provided for both groups |
| Outcomes | 1. Effectiveness rate 2. Adverse events Assessed at the end of the 4‐week treatment period |
| Notes | 1. The trial investigator claimed that they included only those who were diagnosed with AD and identified as "spleen deficiency with dryness of blood" in Chinese medicine 2. We contacted the corresponding trial investigator for further information (such as the randomisation method, whether the study was a prospective design, etc). We received no reply |
Chi 2012.
| Methods | This was a randomised, controlled, parallel, multicentre clinical trial |
| Participants | 1. Setting: The trial recruited participants from 2 Chinese medicine teaching hospitals and 3 teaching hospitals in Beijing, Changsha, and Shanghai, China 2. Age: from 7 to 60 years of age 3. Sex (men/women): 89/103 4. Number of participants randomised: 201 5. T/C: 96/96 |
| Interventions |
I. Treatment group a. Oral ingestion 1. No. 1 Longmu formula for subgroups with "retention of wind dampness on the skin" 1.1 Ingredients and dosage No. 1 Longmu formula:
No. 2 Longmu formula for subgroups with "blood deficiency with dryness wind":
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application
II. Control group a. Oral ingestion 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Hydrocortisone butyrate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
| Outcomes | 1. Effectiveness rate 2. SCORAD 3. CDLQI or DLQI 4. Adverse events Assessments were conducted at baseline; weeks 1, 2, and 4; and at the end of the 8‐week treatment period 5. Complete blood cell count (CBC), urine analysis, liver and kidney function, serum eosinophil count, IgE, eosinophil cationic protein (ECP) Assessments were conducted at baseline and at the end of the 8‐week treatment period 6. Recurrence rate Conducted at 12 weeks after the 8‐week treatment period |
| Notes | 1. There were 9 dropouts in the treatment group and 9 dropouts in the control group; 2 were excluded from the control group because of non‐compliance 2. The trial investigators claimed they included only those who were diagnosed with AD and identified as "retention of wind dampness on the skin" or "blood deficiency with dryness wind" in Chinese medicine 3. The corresponding trial investigator was contacted for further information, such as whether the trial was the same one in Zhao 2011 (as both trials were under the same funding and used the same interventions). We received no reply 4. The trial was funded by Science and Technology National Suppport Scheme ‐ Research on Chinese medicine for common diseases, China |
Dong 2012.
| Methods | This was a randomised, controlled, parallel clinical trial |
| Participants | 1. Setting: The trial recruited participants from the outpatient dermatology department of a general hospital in Rizhao, China 2. Age: from 0.5 to 5.5 years of age 3. Sex (men/women): 52/43 4. Number of participants randomised: 95 5. T/C: 48/47 |
| Interventions |
I. Treatment group 1. Jingfang mixture 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Hydrocortisone butyrate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Topical use of Vitamin E cream for both groups |
| Outcomes | 1. Percentage of reduction of total EASI score 2. Effectiveness rate 3. Adverse events Assessments were conducted at baseline, day 3, week 1, week 7, and at the end of the 2‐week treatment period, respectively |
| Notes | 1. Effectiveness rate = ((pre‐treatment score of EASI ‐ post‐treatment score of EASI)/pre‐treatment score of EASI) * 100% 2. We contacted the corresponding trial investigator for further information (such as the randomisation method, whether the study was a prospective design, etc). We received no reply |
Shi 2012.
| Methods | This was a randomised, controlled, parallel clinical trial |
| Participants | 1. Setting: The trial recruited participants from a women's and children's hospital in Guangzhou, China 2. Age: from 5 to 25 years of age 3. Sex (men/women): 45/66 4. Number of participants randomised: 110 5. T/C: 54/56 |
| Interventions |
I. Treatment group 1. Chinese herbal decoction 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Cetirizine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
| Outcomes | 1. Percentage of reduction of total SASSAD score 2. Effectiveness rate 3. QoL 4. Serum CD3+CD4+T cells and CD3+CD8+T cells, immunoglobulin A (IgA), immunoglobulin G (IgG), immunoglobulin M (IgM), and IgE Assessments were conducted at baseline and at the end of the 3‐week treatment period, respectively |
| Notes | 1. Effectiveness rate = ((pre‐treatment score of SASSAD ‐ post‐treatment score of SASSAD)/pre‐treatment score of SASSAD) * 100% 2. We contacted the corresponding trial investigator for further information (such as why there was discrepancy in the number of participants and sum of the genders, and randomisation method, diagnostic criteria, report of adverse events, and data on QoL). We received no reply |
Tian 2011.
| Methods | This was a randomised, controlled, parallel clinical trial |
| Participants | 1. Setting: The trial recruited participants from an outpatient department of a general hospital in Shenyang, China 2. Age: from 39 days to 20 months old 3. Sex (men/women): 28/22 4. Number of participants randomised: 60 5. T/C: 30/30 |
| Interventions |
I. Treatment group a. Oral ingestion 1. Qushi Zhiyang formula with individualised modifications 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application
II. Control group a. Oral ingestion 2. Chlorpheniramine tablet, diphenhydramine syrup, antibiotics, vitamin E, and vitamin C 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Hydrocortisone butyrate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
| Outcomes | 1. Effectiveness rate assessed at the end of the 8‐week treatment period |
| Notes | We contacted the corresponding trial investigator for further information (such as the randomisation method, a report of adverse events, and whether the study was a prospective design). We received no reply |
Xu 2012.
| Methods | This was a randomised, controlled, parallel clinical trial |
| Participants | 1. Setting: The trial recruited participants from the inpatient paediatric department of a Chinese medicine hospital in Zhangzhou, China 2. Age: from 35 days to 2 years of age 3. Sex (men/women): 56/48 4. Number of participants randomised: 104 5. T/C: 53/51 |
| Interventions |
I. Treatment group 1. Kouqiang Xiaoyan powder 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Triamcinolone acetonide acetate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
| Outcomes | 1. Effectiveness rate 2. Adverse events Assessed at the end of the 2‐week treatment period |
| Notes | We contacted the corresponding trial investigator for further information (such as the randomisation method, a report of adverse events, and whether the study was a prospective design). We received no reply |
Yang 2012.
| Methods | This was a randomised, controlled, parallel clinical trial |
| Participants | 1. Setting: The trial recruited participants from an outpatient dermatology department of a Chinese medicine teaching hospital in Harbin, China 2. Age: did not state age range 3. Sex (men/women): 45/39 4. Number of participants randomised: 84 5. T/C: 42/42 |
| Interventions |
I. Treatment group 1. Shirun Shaoshang ointment 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Zinc oxide ointment (15%) 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
| Outcomes | 1. Effectiveness rate assessed at the end of the 4‐week treatment period |
| Notes | We contacted the corresponding trial investigator for further information (such as the randomisation method, whether the study was a prospective design, and the safety issues of the interventions). We received no reply |
Zhao 2011.
| Methods | This was a randomised, controlled, parallel clinical trial |
| Participants | 1. Setting: The trial recruited participants from an outpatient dermatology department of a Chinese medicine hospital in Beijing, China 2. Age: from 12 to 41 years of age 3. Sex (men/women): 51/71 4. Number of participants randomised: 122 5. T/C: 62/60 |
| Interventions |
I. Treatment group a. Oral ingestion 1. No. 1 Longmu formula for subgroups with "retention of wind dampness on the skin" 1.1 Ingredients and dosage No. 1 Longmu formula:
No. 2 Longmu formula for subgroups with "blood deficiency with dryness wind":
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application
II. Control group a. Oral ingestion 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application 2. Hydrocortisone butyrate cream 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Silicone creams were used externally for both groups |
| Outcomes | 1. Skin lesion score 2. Severity of itching score 3. SCORAD 4. DLQI 5. Adverse events Assessments were conducted at baseline; weeks 1, 2, and 4; and at the end of the 8‐week treatment period 6. Complete blood cell count (CBC), urine analysis, liver and kidney function Assessments were conducted at baseline and at the end of the 8‐week treatment period |
| Notes | 1. The trial investigators claimed that they included only those who were diagnosed with AD and identified as "retention of wind dampness on the skin" or "blood deficiency with dryness wind" in Chinese medicine 2. We contacted the corresponding trial investigator for further information (such as the randomisation method, data on the scores for the outcome measures, etc). We received no reply 3. The trial was funded by Science and Technology National Suppport Scheme ‐ Research on Chinese medicine for common diseases, China |
Zheng 2012.
| Methods | This was a randomised, controlled, parallel clinical trial |
| Participants | 1. Setting: The trial recruited participants from an outpatient and inpatient department of a Chinese medicine hospital in Zhongshan, China 2. Age: did not state 3. Sex (men/women): 58/43 4. Number of participants randomised: 101 5. T/C: 50/51 |
| Interventions |
I. Treatment group 1. Bupi Qufeng granules 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Loratadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Topical application of CHM cream was used in both groups |
| Outcomes | 1. Effectiveness rate 2. Reduction of total SASSAD score 3. Reduction of itching score (measured by participant‐rated score, scale unknown) 4. Adverse events 5. Full counts of blood, routine tests of urine and stool, fecal occult blood 6. Liver and renal function tests Outcome 1 was measured at the end of the trial Outcomes 2 to 4 were assessed at baseline, at 2 weeks, and at the end of the 4‐week treatment period Outcomes 5 and 6 were assessed before and after the treatment period, respectively |
| Notes | 1. The trial investigator claimed that they only included those who were diagnosed with AD and identified as "spleen deficiency" in Chinese medicine 2. Effectiveness rate = ((pre‐treatment score of SASSAD ‐ post‐treatment score of SASSAD)/pre‐treatment score of SASSAD) * 100% 3. We contacted the corresponding trial investigator for further information (such as the randomisation method, the age range of the participants, whether the study was a prospective design, etc). We received no reply 4. The trial was funded by Science and Technology Program, Science and Technology Bureau, Zhongshan, China |
AD: Atopic dermatitis DLQI: Dermatology Life Quality Index EASI: Eczema Area and Severity Index SASSAD: Six Area, Six Sign Atopic Dermatitis severity score SCORAD: Severity Scoring of Atopic Dermatitis
Characteristics of ongoing studies [ordered by study ID]
ChiCTR‐TRC‐08000156.
| Trial name or title | The clincal trial of the traditional Chinese formula of Hilling and Clearing Away Heart‐fire (HCAH) for atopic dermatitis |
| Methods | This is a randomised, non‐blind, controlled, 3‐arm parallel, multicentre clinical trial |
| Participants | 1. Setting: The trial recruited participants from 3 Chinese medicine teaching hospitals and 2 teaching hospitals in Guangzhou, Chengdu, Nanjing, Haikou, and Luzhou, China 2. Age: from 7 to 25 years of age 3. Sex (men/women): ‐ 4. Target number of participants for randomisation: 249 |
| Interventions |
I. Treatment group a. Oral ingestion 1. Peitu Qingxin formula 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
b. Topical application
II. Control group A a. Oral ingestion 2. Cyproheptadine tablet 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
b. Topical application
III. Control group B
|
| Outcomes | 1. SCORAD 2. DLQI 3. Index of curative effect Did not state assessment points |
| Starting date | 1st October 2008 |
| Contact information | Dr Xiumei Mo, Department of Dermatology, Guangdong Provincial Hospital, No.111 Dade Road, Guangzhou, Guangdong, China 510120 Email: moxiumeilsamay@163.com |
| Notes | 1. The trial has been registered on http://www.chictr.org/cn. Registration number: ChiCTR‐TRC‐08000156 2. The trial was completed, and the report of the trial has not been published 3. We contacted the corresponding investigator on 12 December 2011, who indicated that no protocol of the trial has been published 4. The trial was funded by the '11.5 Key Projects', the Ministry of Science and Technique, China 5. We contacted the corresponding investigator again on 17 September 2012 for the publication status of the trial. The corresponding investigator replied that the report of the trial has not been published yet 6. We contacted the corresponding investigator again on 21 June 2013 for the publication status of the trial as we found a title and abstract of a PhD thesis with a report of a clinical trial published by the corresponding investigator in 2012. We assumed the trial reported in the PhD thesis was the one started in 2008, but we were unable to retrieve the full text of the report for further assessment. We have received no reply |
ChiCTR‐TRC‐09000562.
| Trial name or title | Clinical trial of Bu Shen Yi Qi Fang on treating atopic dermatitis in deficiency of Kidney Yang and Qi |
| Methods | This is a randomised, double‐blind, placebo‐controlled, parallel, multicentre clinical trial |
| Participants | 1. Setting: Participants will be recruited from 3 teaching hospitals in Shanghai, Nanjing, and Chengdu, China 2. Age: from 18 to 70 years of age 3. Sex (men/women): ‐ 4. Target number of participants for randomisation: 320 |
| Interventions |
I. Treatment group 1. Bu Shen Yi Qi Fang formula 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Placebo 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Desloratadine tablet will be used for 2 groups |
| Outcomes | 1. Traditional Chinese medicine symptom scores 2. Severity of itching score measured by VAS 3. Numbers of sleep disturbance by skin itching 4. DLQI 5. SCORAD 6. Full blood counts, routine tests of urine, liver and renal function tests, electrocardiogram 7. Serum IgE, IFN‐γ, TNF‐α, IL‐4, IL‐6, IL‐10, TGF‐β, c‐reactive protein (CRP), CORT, adrenocorticotrophin (ACTH) Did not state assessment points |
| Starting date | Not started yet |
| Contact information | Dr. Liu Runhong, Lab of integrative medicine for Lung inflammation and cancer, Number 12 of Middle Wu Lu Mu Qi Lu, Shanghai, China 200040 Email: liurunhong@163.com |
| Notes | 1. The trial has been registered on http://www.chictr.org/cn. Registration number: ChiCTR‐TRC‐09000562 2. We contacted the corresponding investigator on 30 January 2012 and received no reply 3. The trial was funded by Ministry of Science and Technology, China 4. We contacted the corresponding investigator again on 17 September 2012 for the publication status of the trial and received no reply |
ChiCTR‐TRC‐12003174.
| Trial name or title | Effectiveness of PeiTu QingXin (PTQX) Granules adds on usual care to reduce the accumulated relapse of the atopic dermatitis in children: a protocol for a multi‐center, double‐blind, randomized controlled trial |
| Methods | This is a randomised, double‐blind, placebo‐controlled, parallel, multicentre clinical trial |
| Participants | 1. Setting: Participants will be recruited from 4 Chinese medicine teaching hospitals and 5 general hospitals in Guangzhou, Xi'an, Haikou, Nanjing, Beijing, Hangzhou, Shanghai, and Zhengzhou, China 2. Age: from 2 to 12 years of age 3. Sex (men/women): ‐ 4. Target number of participants for randomisation: 380 |
| Interventions |
I. Treatment group 1. Oral ingestion of Peitu Qingxin formula (CHM granules) 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Placebo 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
‐ Conventional medicines will be provided in both groups |
| Outcomes | 1. The starting time of a relapse 2. SCORAD 3. The Dermatitis Family Impact Questionnaire 4. Total usage of topical fluticasone propionate cream Did not state assessment points |
| Starting date | 1 March 2013 |
| Contact information | Dr Chi Liu, Department of Dermatology, Second Affiliated Hospital of Guangzhou University of Chinese Medicine. No.111 Dade Road, Guangzhou, Guangdong, China 510120 Email: ich008@163.com |
| Notes | 1. The trial has been registered on http://www.chictr.org/cn. Registration number: ChiCTR‐TRC‐12003174 2. The trial has been funded by the State Administration of Traditional Chinese Medicine, China 3. We contacted the corresponding investigator on 17 June 2013 for details of interventions. We received no reply |
ISRCTN26218532.
| Trial name or title | A clinical study of Hwangryunhaedoktang in adult atopic dermatitis: a randomised, double‐blind, placebo‐controlled, multicenter trial |
| Methods | This is a randomised, double‐blind, placebo‐controlled, parallel, multicentre clinical trial |
| Participants | 1. Setting: The trial recruited participants from South Korea 2. Age: more than 19 years of age 3. Sex (men/women): ‐ 4. Target number of participants for randomisation: 100 |
| Interventions |
I. Treatment group 1. Hwangryunhaedoktang extracted granules 1.1 Ingredients and dosage
1.2 Administration
1.3 Duration of treatment
1.4 Follow up
II. Control group 2. Placebo 2.1 Ingredients and dosage
2.2 Administration
2.3 Duration of treatment
2.4 Follow up
|
| Outcomes | 1. SCORAD Measured at treatment period (treatment initiation; 2, 4, and 8 weeks after the first medication) 2. Complete blood cell count (CBC), erythrocyte sedimentation rate (ESR), blood chemistry, urine analysis 3. Chest‐PA film Measured at baseline and 8 weeks after first medication 4. Vital signs Measured at baseline and treatment period (treatment initiation; 2, 4, and 8 weeks after the first medication) 5. Total IgE, eosinophil count Measured at treatment initiation and 4 and 8 weeks after the first medication 6. EuroQol 5‐Dimension (EQ‐5D) 7. Health Utilities Index Mark 3 (HUI‐3) 8. DLQI Measured at treatment initiation and 8 weeks after first medication |
| Starting date | 21 June 2010 |
| Contact information | Dr Namkwen Kim Wonkwang University Oriental Medical Center 1126‐1 Sanbon‐dong, Gunpo, Korea, South 435‐040 Email: drkim@wonkwang.ac.kr |
| Notes | 1. The trial has been registered on http://www.controlled‐trials.com/ISRCTN26218532. The protocol of the trial was published in 2011 2. The trial was completed, and a report of the trial has not been identified via electronic searches 3. We contacted the corresponding investigator on 30 January 2012 and received no reply 4. The trial was funded by Korea Health Industry Development Institute (KHIDI) (South Korea) ‐ The Traditional Korean Medicine Research and Development Project 5. We contacted the corresponding investigator again on 17 September 2012 for the publication status of the trial and received no reply |
DLQI: Dermatology Life Quality Index SCORAD: Severity Scoring of Atopic Dermatitis
Differences between protocol and review
We added "in children and adults" under the heading of 'Objectives' to define the participants in this review.
In the Methods section under 'Type of interventions', we found in the protocol that the words "or formula" were missing and CHM had been listed as one of the control interventions, which was inappropriate. We changed the wording to: "Oral ingestion and topical applications of a single Chinese medicinal herb or formula, manufactured or clinician self‐designed Chinese medicinal formulae, (a clinician self‐designed formula is usually composed of different types of Chinese herbs prescribed by a Chinese medicine practitioner who determines the selection of herbs based on a patient’s condition) compared to the following control interventions: placebo, no intervention, and active controls, including acupuncture or conventional medicines."
To make the meaning of the statement more precise, in the Methods section under 'Measures of treatment effect' and then the subheading 'Studies with multiple treatment groups', we rephrased the wording to: "For studies with more than two interventions, we selected the comparison group that met the inclusion criteria."
To reflect the actual process of the review, in the Methods section under 'Data collection and analysis' and then the subheading 'Data synthesis', we deleted the following sentence: "In the presence of substantial heterogeneity that cannot be explained, we would not undertake statistical pooling." We replaced it with, "We performed the meta‐analyses irrespective of the level of heterogeneity for the purpose of explanation of potential inconsistency across the included studies. When substantial heterogeneity was found (I² statistic greater than 50%), then we explored the sources of such heterogeneity by rechecking the data, and by subgroup analysis based on clinical and methodological diversity factors."
We performed a posthoc subgroup analysis to further investigate heterogeneity across the included studies where Western medications were used as comparators.
Contributions of authors
SG was the contact person with the editorial base. SG co‐ordinated contributions from the co‐authors and wrote the final draft of the review. SG and AWY screened papers against eligibility criteria. SG and AWY obtained data on ongoing and unpublished studies. HCW, WZ, CCX, and CGL appraised the quality of papers. SG and AWY extracted data for the review and sought additional information about papers. SG and AWY entered data into RevMan. SG, AWY, HCW, WZ, CCX, and CGL analysed and interpreted data. SG, AWY, HCW, WZ, CCX, and CGL worked on the methods sections. SG, AWY, HCW, and WZ drafted the clinical sections of the background and responded to the clinical comments of the referees. SG, AWY, HCW, and WZ responded to the methodology and statistics comments of the referees. CP was the consumer co‐author and checked the review for readability and clarity, as well as ensuring outcomes are relevant to consumers. SG is the guarantor of the update.
The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health, UK.
Sources of support
Internal sources
Discipline of Chinese Medicine, School of Health Sciences, RMIT University, Australia.
External sources
Centre of Evidence Based Dermatology, Nottingham University, UK.
-
The National Institute for Health Research (NIHR), UK.
The NIHR, UK, is the largest single funder of the Cochrane Skin Group.
Declarations of interest
Kam‐Lun Ellis Hon, who peer‐reviewed this review as a clinical referee, was also the Principal Investigator in the following included study:
Hon KL, Leung TF, Ng PC, Lam MCA, Kam WYC, Wong KY, et al. Efficacy and tolerability of a Chinese herbal medicine concoction for treatment of atopic dermatitis: a randomized, double‐blind, placebo‐controlled study. British Journal of Dermatology 2007;157(2):357‐63. [MEDLINE: 17501956]
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Cao 2009 {published data only}
- Cao M, Wei YG. Clinical study of Zhuling Jianpi Huashi decoction for atopic dermatitis. Nanjing University of Chinese Medicine, Nanjing [Masters thesis] 2009.
Chao 2003 {published data only}
- Chao Q, Xiao JG. Research of Chinese herbal medicines for infantile eczema. Qingdao University, Qingdao [Masters thesis] 2003.
Chen 2011 {published data only}
- Chen H. Clinical observation of Huanglian Qingdai cream for infantile eczema. Journal of Sichuan of Traditional Chinese Medicine 2011;29(6):88‐9. [Google Scholar]
Cheng 2010 {published data only}
- Cheng HM, Chiang LC, Jan YM, Chen GW, Li TC. The efficacy and safety of a Chinese herbal product (Xiao‐Feng‐San) for the treatment of refractory atopic dermatitis: a randomized, double‐blind, placebo‐controlled trial. International Archives of Allergy & Immunology 2011;155(2):141‐8. [DOI: 10.1159/000318861] [DOI] [PubMed] [Google Scholar]
Gong 2010 {published data only}
- Gong XH, Kuang L, Liu X. Clinical observation of Liangxue Xiaofeng formula for adult atopic dermatitis. Journal of TCM University of Hunan 2010;30(3):61‐3. [Google Scholar]
Hon 2007 {published data only}
- Hon KL, Leung TF, Ng PC, Lam MCA, Kam WYC, Wong KY, et al. Efficacy and tolerability of a Chinese herbal medicine concoction for treatment of atopic dermatitis: a randomized, double‐blind, placebo‐controlled study. British Journal of Dermatology 2007;157(2):357‐63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Hon KLE, Leung TF, Ng PC, Lam MCA, Kam WYC, Wong KY, et al. Therapeutic effect and safety of a traditional Chinese medicine for atopic dermatitis in children: a randomised, double‐blind, placebo‐controlled study. Hong Kong Medical Journal 2011;17(1 Suppl 2):38‐40. [PubMed] [Google Scholar]
Huang 2010 {published data only}
- Huang ZK, Chen P, Wei WN. Observation of efficacy of Chushi Zhiyang cream for atopic dermatitis. Modern Journal of Integrated Traditional Chinese & Western Medicine 2010;19(21):2647‐8. [Google Scholar]
Jin 2007 {published data only}
- Jin PZ, Ye QH, Shen M. Observation of efficacy of Jianpi Zhiyang granules for 32 cases with atopic dermatitis. Henan Traditional Chinese Medicine 2007;27(12):61‐2. [Google Scholar]
Lang 2007 {published data only}
- Lang N, Yao CH, Bo YJ, Chi HY, Tu YY, Huang YZ. Treatment of blood deficiency with wind dryness type of atopic dermatitis with combination of Shengui decoction and Shidu ointment. Chinese Journal of Dermatovenerology Integrated Traditional & West Medicine 2007;6(1):22‐3. [Google Scholar]
Lin 2010 {published data only}
- Lin Y, Chen DC. Efficacy of anti‐inflammatory moisturising washing formula for atopic dermatitis and its biological evaluation. Guangzhou University of Chinese Medicine, Guangzhou [PhD thesis] 2010.
Liu 2005 {published data only}
- Liu HC. Investigation of efficacy of Chinese medicine for atopic dermatitis. Hua‐xia Medicine 2005;25(3):208‐9. [Google Scholar]
Luo 2010 {published data only}
- Luo FJ, Wei YG. Evaluation of efficacy of Xiaofengsan with modifications for atopic dermatitis. Nanjing University of Chinese Medicine, Nanjing [Masters thesis] 2010.
Ma 2010 {published data only}
- Ma YB, Sun LY, Wang P, Zhang GZ, Cai NN. Clinical observation of combination of Jianpi Runfu decoction and topical application of Gancao oil for atopic dermatitis with syndrome of spleen deficiency and blood dryness. Beijing Journal of Traditional Chinese Medicine 2010;29(9):680‐2. [Google Scholar]
Rao 2010 {published data only}
- Rao MR, Wei YG. Clinical study of Qingxin Peitu method for atopic dermatitis. Nanjing University of Chinese Medicine, Nanjing [Masters thesis] 2010.
Sun 2009 {published data only}
- Sun XD. Evaluation of efficacy and affect of reoccurrence of Jianpi Shenshi granules for atopic dermatitis [Clinical effect of invigorating spleen and excreting dampness granules in treating atopic dermatitis and its influence for recurrence of the patient]. Chinese Journal of Dermatovenerology Integrated Traditional and Western Medicine 2009;8(6):335‐7. [Google Scholar]
Tian 2005 {published data only}
- Tian F, He T. Observation of efficacy of Fuyang granules for infantile eczema. Liaoning Journal of Traditional Chinese Medicine 2005;32(8):810‐1. [Google Scholar]
Wang 2008 {published data only}
- Wang P, Cai L, Xu JJ. Observation of efficacy of Chushi Zhiyang ointment for infantile eczema. Journal of Sichuan of Traditional Chinese Medicine 2008;26(9):92‐3. [Google Scholar]
Xiao 2008 {published data only}
- Xiao M, Ai RD. Observation of clinical efficacy of combination of Machixian decoction and topical application of Chinese herbs for atopic dermatitis and evaluation of IgE level in serum. Chengdu University of Chinese Medicine, Chengdu [Masters thesis] 2008.
Xiao 2011 {published data only}
- Xiao WM, Li G, Luo B, Zhu QJ. Observation of efficacy of Huailian decoction for atopic dermatitis. Journal of China Traditional Chinese Medicine Information 2011;3(3):37‐9. [Google Scholar]
Xue 2011 {published data only}
- Xue SQ, Tan JH. Clinical observation of Shengxue Runfu decoction with modifications for childhood atopic dermatitis. Journal of New Chinese Medicine 2011;43(2):94‐5. [Google Scholar]
Yang 2007 {published data only}
- Yang Y, Sun JL, Feng YL, Yang YF, Wang LX. Analysis of efficacy of Chinese herbs Jianpi Zhiyang granules with Pibo Xiaoyan Xuanshi ointment for atopic dermatitis. Chinese Journal of Dermatovenerology Integrated Traditional & Western Medicine 2007;6(3):135‐7. [Google Scholar]
Yang 2009 {published data only}
- Yang XS, Ye JZ, Li K. Clinical efficacy of Jianpi Yangxue Qufeng method for atopic dermatitis and its affect for skin barrier function [The effects of the clinical efficacy of method of strengthening spleen and enriching blood eliminating wind in treatment of chronic atopic dermatitis]. Journal of Yunnan University of Traditional Chinese Medicine 2009;32(3):5‐7. [Google Scholar]
Yu 1999 {published data only}
- Yu TG, Zhu JT, Xu JL, Zhuang YR, Shen B, Wu BL, et al. Clincial and laboratory study of Piyan Xiaojingyin granules II for atopic dermatitis. Journal of Traditional Chinese Medicine 1999;40(3):165‐7. [Google Scholar]
Zhang 2005 {published data only}
- Zhang QS, Wei YG. Clinical study of Jianpi Huashi formula for childhood atopic dermatitis. Nanjing University of Chinese Medicine, Nanjing [Masters thesis] 2005.
Zhang 2009 {published data only}
- Zhang XJ, Song XL. Observation of clinical efficacy of Xiao'er Huashi decoction for infantile eczema. Proceedings of the First International Dermatology Academic Symposium of TCM and Integrated TCM‐WM. Beijing: World Federation of Chinese Medicine Societies, 2009:297‐9.
Zhang 2011 {published data only}
- Zhang CJ. Clinical observation of Zhiyin Qingre method for 30 cases with atopic dermatitis. Guiding Journal of Traditional Chinese Medicine & Pharmacy 2011;17(8):22‐4. [Google Scholar]
Zhou 2011 {published data only}
- Zhou YZ. Observation of clinical efficacy of Canger Kushen lotion for 88 cases with infantile eczema. Guide of China Medicine 2011;9(25):115‐6. [Google Scholar]
Zou 2011 {published data only}
- Zou GM, Xie B. Clincial study of Fufang Sanhuang lotion for infantile eczema. Liaoning Journal of Traditional Chinese Medicine 2011;38(2):297‐9. [Google Scholar]
References to studies excluded from this review
Li 2006 {published data only}
- Li DH, Mu DS, Liu J, Song WY. Observation of efficacy of Jianpi Qufeng method for atopic dermatitis. Jilin Journal of Traditional Chinese Medicine 2006;26(8):18‐9. [Google Scholar]
Udompataikul 2011 {published data only}
- Udompataikul M, Srisatwaja W. Comparative trial of moisturizer containing licochalcone A vs. hydrocortisone lotion in the treatment of childhood atopic dermatitis: a pilot study. Journal of the European Academy of Dermatology & Venereology 2011;25(6):660‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zhang 2010 {published data only}
- Zhang YF, Lin ZS. Observation of clinical efficacy of Chinese medicine for 30 cases with infantile eczema. Journal of Pediatrics of Traditional Chinese Medicine 2010;6(5):18‐20. [Google Scholar]
Zhao 2008 {published data only}
- Zhao BJ. Clinical observation of Jianpi Hewei Xiaoshi Daozhi method for infantile eczema. Guangming Journal of Chinese Medicine 2008;23(5):623. [Google Scholar]
References to studies awaiting assessment
Cai 2012 {published data only}
- Cai XZ. Modified Shenling Baizhu formula for 43 cases with atopic dermatitis in spleen deficiency and blood dryness. Hebei Journal of Traditional Chinese Medicine 2012;34(10):1499‐500. [Google Scholar]
Chi 2012 {published data only}
- Chi HY, Huang YZ. A clinical evaluation of treating atopic dermatitis with traditional Chinese medicine. A muti‐center randomized controlled trial on the treatment of AD with suppress the heart and calm the mind method. China Academy of Chinese Medical Sciences, Beijing [PhD thesis] 2012.
Dong 2012 {published data only}
- Dong M. Efficacy of external use of Jingfang mixture in the treatment of children with eczema. Medical Journal of Qilu 2012;27(1):75‐8. [Google Scholar]
Shi 2012 {published data only}
- Shi J, Diao YT, Li XW. Compound Chinese medicine treatment for patients with atopic dermatitis and curative effect of the immune function of regulatory role. Chinese Journal of Dermatovenerology Integrated Traditional & Western Medicine 2012;11(3):143‐5. [Google Scholar]
Tian 2011 {published data only}
- Tian Y. Clinical observation of modified Qushi Zhiyang decoction for infantile eczema. Journal of China Traditional Chinese Medicine Information 2011;3(2):38‐9. [Google Scholar]
Xu 2012 {published data only}
- Xu XC, Guo YC. Clinical observation of Kouqiang Xiaoyan powder for infantile eczema. Strait Pharmaceutical Journal 2012;24(10):210. [Google Scholar]
Yang 2012 {published data only}
- Yang SQ, Yan JD. Clincial observation of Shirun Shaoshang ointment for atopic dermatitis in children. Proceedings of the 8th Academic Conference for External Therapy. Nanning: China Association of Chinese Medicine, 2012:151‐5.
Zhao 2011 {published data only}
- Zhao YD, Yao CH, Lang N, She YY, Chi HY, Tian FY, et al. Clinical observation of Longmu liquid in treatment of atopic dermatitis in youths and adults and the investigation of quality of life. Chinese Journal of Dermatovenerology Integrated Traditional & Western Medicine 2011;10(4):215‐8. [Google Scholar]
Zheng 2012 {published data only}
- Zheng YP, Xie RB, Chen GF, Zhang L. Clinical observation of efficacy of Bupi Qufeng formula for atopic dermatitis. Guangming Journal of Chinese Medicine 2012;27(7):1365‐6. [Google Scholar]
References to ongoing studies
ChiCTR‐TRC‐08000156 {published data only}
- ChiCTR‐TRC‐08000156. The clinical trial of the traditional Chinese formula of hilling and clearing away heart‐fire (HCAH) for atopic dermatitis. chictr.clinicaltrialecrf.org/en/proj/show.aspx?proj=1232 (accessed 25 April 2012).
- Mo XM, Chen DC. Clinical research with multiple dimensions in efficacy of Peitu Qingxin method for atopic dermatitis [Clinical Research on multi‐dimension evaluation treated by the traditional Chinese formula of Qingxinpeitu for atopic dermatitis]. Guangzhou Univeristy of Chinese Medicine, Guangzhou [PhD thesis] 2012.
ChiCTR‐TRC‐09000562 {published data only}
- ChiCTR‐TRC‐09000562. Clinical trial of Bu Shen Yi Qi Fang on treating atopic dermatitis in deficiency of kidney Yang and Qi. chictr.clinicaltrialecrf.org/en/proj/show.aspx?proj=838 (accessed 25 April 2012).
ChiCTR‐TRC‐12003174 {published data only}
- ChiCTR‐TRC‐12003174. Effectiveness of PeiTu QingXin (PTQX) Granules adds on usual care to reduce the accumulated relapse of the atopic dermatitis in children: A protocol for a multi‐center, double‐blind, randomized controlled trial. http://www.chictr.org/en/proj/show.aspx?proj=3241 (accessed 15 June 2013).
ISRCTN26218532 {published data only}
- ISRCTN26218532. A clinical study of Hwangryunhaedoktang in adult atopic dermatitis : a randomised, double‐blind, placebo‐controlled, multicentre trial. controlled‐trials.com/ISRCTN26218532 (accessed 25 April 2012).
- Kim NK, Lee DH, Seo HS, Sun SH, Oh YL, Kim JE, et al. Hwangryunhaedoktang in adult patients with atopic dermatitis: a randomised, double‐blind,placebo‐controlled, two‐centre trial ‐ study protocol. Complementary & Alternative Medicine 2011;11(8):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
CDER 2005
- Centre for Drug Evaluation and Research. Alert for healthcare professionals: pimecrolimus (marketed as Elidel) / tacrolimus (marketed as Protopic). Food & Drug Administration 2005.
Charman 2000
- Charman CR, Morris AD, Williams HC. Topical corticosteroid phobia in patients with atopic eczema. British Journal of Dermatology 2000;142(5):931‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chen 1991
- Chen GT, Yang SS. Practical diagnostics and therapeutics of integrated traditional Chinese and western medicine. Beijing: Medical and Pharmaceutical Science and Technology Press, 1991. [Google Scholar]
Chen 2001
- Chen DC, Xuan GW. Chinese medicine diagnosis and treatment in dermatosis and venereal diseases. Beijing: People's Medical Publishing House, 2001. [Google Scholar]
Chitturi 2000
- Chitturi S, Farrell GC. Herbal hepatotoxicity: an expanding but poorly defined problem. Journal of Gastroenterology & Hepatology 2000;15(10):1093‐9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. British Medical Journal 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eichenfield 2003
- Eichenfield LF, Hanifin JM, Luger TA, Stevens SR, Pride HB. Consensus conference on paediatric atopic dermatitis. Journal of the American Academy of Dermatology 2003;49(6):1088‐95. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Flohr 2008
- Flohr C, Weiland SK, Weinmayr G, Björkstén B, Bråbäck L, Brunekreef B, et al. The role of atopic sensitization in flexural eczema: Findings from the international study of asthma and allergies in childhood phase two. Journal of Allergy & Clinical Immunology 2008;121(1):141‐7 e4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Guo 2007
- Guo W, Yu TG. Research of Chinese medicine treatments for atopic dermatitis [Zhongyiyao zhiliao teyingxing piyan yanjiu jinzhan]. Henan Traditional Chinese Medicine 2007;27(4):83‐5. [Google Scholar]
Hanifin 1980
- Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Dermato‐Venereologica 1980;59(Suppl 92):44‐7. [Google Scholar]
Hanifin 2004
- Hanifin JM, Cooper KD, Ho VC, Kang S, Krafchik BR, Margolis DJ, et al. Guidelines of care for atopic dermatitis. Journal of the American Academy of Dermatology 2004;50(3):391‐404. [EMBASE: 2004116938] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. Available from www.cochrane‐handbook.org. The Cochrane Collaboration. Available from www.cochrane‐handbook.org.
Hon 2005
- Hon KL, Ma KC, Wong Y, Leung TF, Fok TF. A survey of traditional Chinese medicine use in children with atopic dermatitis attending a paediatric dermatology clinic. Journal of Dermatological Treatment 2005;16(3):154‐7. [EMBASE: 2005434025] [DOI] [PubMed] [Google Scholar]
Johansson 2004
- Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the nomenclature review committee of the world allergy organization, October 2003. Journal of Allergy & Clinical Immunology 2004;113(5):832‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kane 2004
- Kane M. Research Made Easy in Complementary & Alternative Medicine. Edinburgh: Churchill Livingstone, 2004. [Google Scholar]
Kerdel 2003
- Kerdel F, Jimenez‐Acosta F. Dermatology: Just the facts. New York: McGraw‐Hill Medical, 2003. [Google Scholar]
Li 2008
- Li, ZJ. International Standard Chinese‐English Basic Nomenclature of Chinese Medicine. Beijing: People's Medical Publishing House, 2008. [Google Scholar]
Liu 2006
- Liu, JP. Clinical research methodology for evidence‐based Chinese medicine. Clinical Research Methodology for Evidence‐based Chinese Medicine. Beijing: People's Medical Publishing House, 2006. [Google Scholar]
MEPRC 1992
- Ministry of Education of the People's Republic of China. Interim provisions for management of general tertiary medical education clinical teaching base. http://202.205.177.9/edoas/website18/41/info5941.htm (accessed 1 May 2012).
Odhiambo 2009
- Odhiambo JA, Williams HC, Clayton TO, Robertson CF, Asher MI, ISAAC Phase Three Study Group. Global variations in prevalence of eczema symptoms in children from ISAAC Phase Three. Journal of Allergy & Clinical Immunology 2009;124(6):1251‐8 e23. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Perharic 1995
- Perharic L, Shaw D, Leon C, Smet PA, Murray VS. Possible association of liver damage with the use of Chinese herbal medicine for skin disease. Veterinary & Human Toxicology 1995;37(6):562‐6. [MEDLINE: ] [PubMed] [Google Scholar]
SATCM 1994
- State Administration of Traditional Chinese Medicine of the People's Republic of China. Criteria of diagnosis and therapeutic effect of diseases and syndromes in traditional Chinese medicine. Chinese Medicine Profession Standards of the People's Republic of China 1994; Vol. ZY/T001.8, issue 94:147.
Schmid‐Ott 2003
- Schmid‐Ott G, Burchard R, Niederauer HH, Lamprecht F, Künsebeck HW. Stigmatization and quality of life of patients with psoriasis and atopic dermatitis [Stigmatisierungsgefühl und Lebensqualität bei Patienten mit Psoriasis und Neurodermitis]. Hautarzt 2003;54(9):852‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schmitt 2007
- Schmitt J, Langan S, Williams HC, European Dermato‐Epidemiology Network. What are the best outcome measurements for atopic eczema? A systematic review. Journal of Allergy & Clinical Immunology 2007;120(6):1389‐98. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schultz‐Larsen 2002
- Schultz‐Larsen F, Hanifin JM. Epidemiology of atopic dermatitis. Immunology & Allergy Clinics of North America 2002;22(1):1‐24. [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Sterne 2011
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Tal 2011
- Tal J. Strategy and statistics in clinical trials: a non‐statisticians guide to thinking, designing and executing. Amsterdam: Elsevier, 2011. [Google Scholar]
Williams 1994
- Williams HC, Burney PG, Hay RJ, Archer CB, Shipley MJ, Hunter JJ, et al. The U.K. Working Party's diagnostic criteria for atopic dermatitis. I. Derivation of a minimum set of discriminators for atopic dermatitis. British Journal of Dermatology 1994;131(3):383‐96. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Williams 2000
- Williams HC, Wüthrich B. The natural history of atopic dermatitis. In: Williams HC editor(s). Atopic Dermatitis: The epidemiology, causes and prevention of atopic eczema. Cambridge: Cambridge University Press, 2000:41‐59. [Google Scholar]
Williams 2008
- Williams H, Stewart A, Mutius E, Cookson W, Anderson HR, International Study of Asthma and Allergies in Childhood (ISAAC) Phase One and Three Study Groups. Is eczema really on the increase worldwide?. Journal of Allergy & Clinical Immunology 2008;121(4):947‐54 e15. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zhao 1983
- Zhao BN, Zhang ZL. Concise Chinese Medicine Dermatology. Beijing: China Prospects Publisher, 1983. [Google Scholar]
Zhou 2008
- Zhou F, Li P. Progress in treatment of atopic dermatitis by traditional Chinese medicine. Shaanxi Journal of Traditional Chinese Medicine 2008;42(10):83‐6. [Google Scholar]
References to other published versions of this review
Zhang 2004
- Zhang W, Leonard T, Bath‐Hextall F, Chambers CA, Lee C, Humphreys R, et al. Chinese herbal medicine for atopic eczema. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD002291] [DOI] [PubMed] [Google Scholar]


